cd0d44d701e9d353063ce8739f845be1.ppt
- Количество слайдов: 70
口腔病理科 Wound Healing 傷口癒合 陳玉昆教授: 高雄醫學大學 口腔病理科 07 -3121101~2755 yukkwa@kmu. edu. tw

學習目標 1. Regeneration & repair 2. Epithelium & connective tissue 3. Tooth extraction wound 4. Bone fracture
References 參考資料 1. Ibsen OAC: Oral Pathology for the dental hygienist. 4 th ed. , pp. 36 - 52 2. Avery JK: Oral Development & Histology, pp. 192 -212 3. Horwitz AF: Integrins and Health. Sci Am 1997; May, 68 -75 4. Singer AF et al: Evaluation and management of traumatic lacerations. New Eng Med J 1997; 337: 1142 -8 5. Habeck M: Wound-healing genes promote cancer progression. Lancet Oncol 2004; 5: 138 6. Epstein FH: Cutaneous wound healing. New Eng Med J 1999; 341: 738 -46 7. Kaohsiung Medical University, Oral Pathology Department 8. Sompayrac L. How the immune works Lecture 1. An overview 1999: p. 5 -16 9. www. mybiology. com/archive_movies 10. http: //www. bu. edu/woundbiotech/Wound. Healing. Process/ 11. http: //connection. lww. com/products/taylor/documents/cc 37 figure 37 -1. jpg 12. http: //ls. berkeley. edu/bio/gallery_mcb/wound. html 13. www. nchmd. org 14. http: //www. ma. hw. ac. uk/~jas/researchinterests/scartissueformation. html 15. http: //www. malp-research. de/ 16. http: //www. imakenews. com/mvius/e_article 000210982. cfm 17. Awang MN. The aetiology of dry socket: a review. Int Dent J 1989; 39: 236 -40 18. 徐博文、謝耀東 拔牙後齒槽骨傷口之癒合 中華民國口腔植體學會會訊1997; 5月第 4期 p. 27 -30 19. Shafer WG. A textbook of oral pathology. 1 st edition, p. 609 -10 20. www. unireptile. com/amphibian/newt_web. htm 21. Nanci A. Ten Cate’s Oral Histology 7 th ed. , pp. 388 -9
Wound Healing (再生) Regeneration Slight tissue damage: inflamed area returns completely to its normal structure & function 2 Most favorable end to acute inflammation & involves: 1. Complete removal of all cells, by-products inflammatory exudate that enter tissue 2. Return of microcirculation to its preinflammatory state 蠑螈 Ref. 20
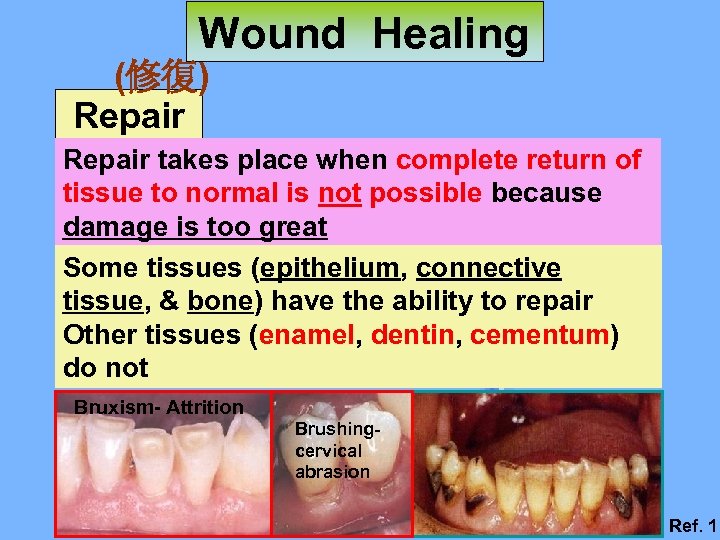
Wound Healing (修復) Repair takes place when complete return of tissue to normal is not possible because damage is too great Some tissues (epithelium, connective tissue, & bone) have the ability to repair Other tissues (enamel, dentin, cementum) do not Bruxism- Attrition Brushingcervical abrasion Ref. 1
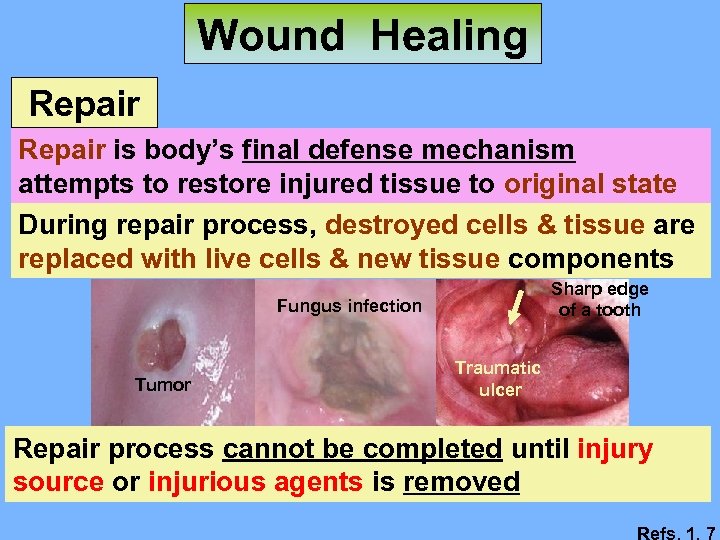
Wound Healing Repair is body’s final defense mechanism attempts to restore injured tissue to original state During repair process, destroyed cells & tissue are replaced with live cells & new tissue components Sharp edge of a tooth Fungus infection Tumor Traumatic ulcer Repair process cannot be completed until injury source or injurious agents is removed Refs. 1, 7
Wound Healing Repair Epithelium and connective tissue Tooth extraction wound Bone fracture
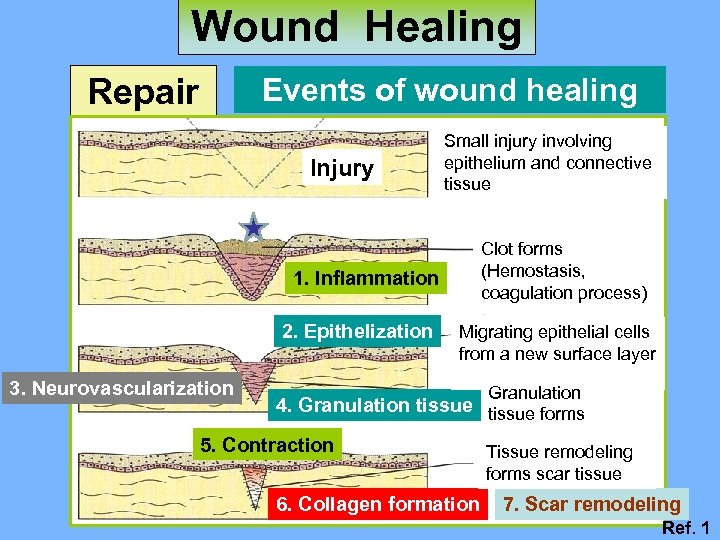
Wound Healing Repair Events of wound healing Injury Small injury involving epithelium and connective tissue Clot forms (Hemostasis, coagulation process) 1. Inflammation 2. Epithelization 3. Neurovascularization Migrating epithelial cells from a new surface layer Granulation 4. Granulation tissue forms 5. Contraction 6. Collagen formation Tissue remodeling forms scar tissue 7. Scar remodeling Ref. 1
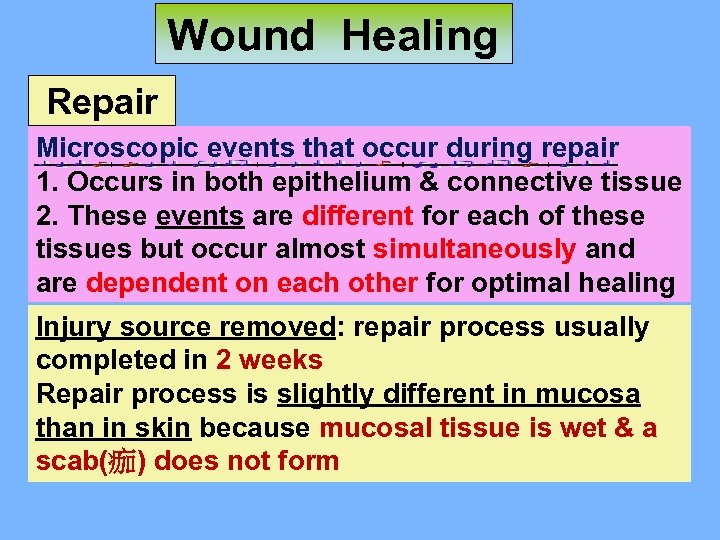
Wound Healing Repair Microscopic events that occur during repair 1. Occurs in both epithelium & connective tissue 2. These events are different for each of these tissues but occur almost simultaneously and are dependent on each other for optimal healing Injury source removed: repair process usually completed in 2 weeks Repair process is slightly different in mucosa than in skin because mucosal tissue is wet & a scab(痂) does not form
Wound Healing Repair Day of Injury. A clot [凝塊 meshwork of fibrin clumped(成塊) red blood cells & platelets (thrombocytes)] forms as blood flows into injured tissue due to activation of clotting mechanism Platelets are found in blood: important in clot formation
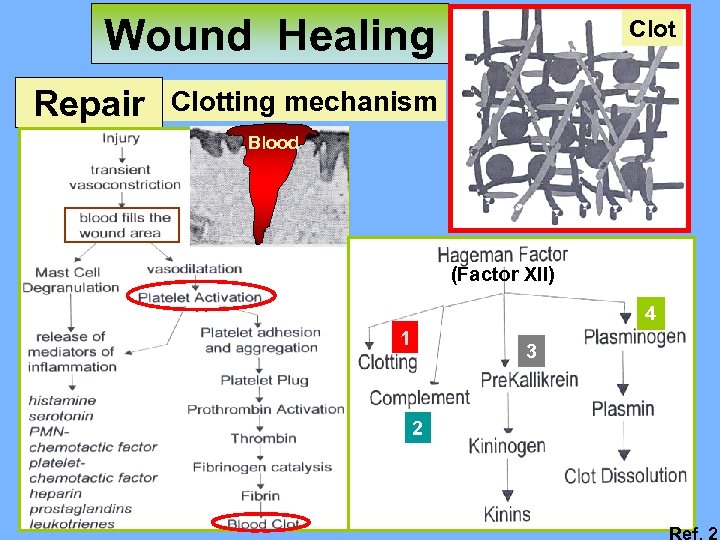
Wound Healing Repair Clotting mechanism Blood (Factor XII) 4 1 3 2 Ref. 2
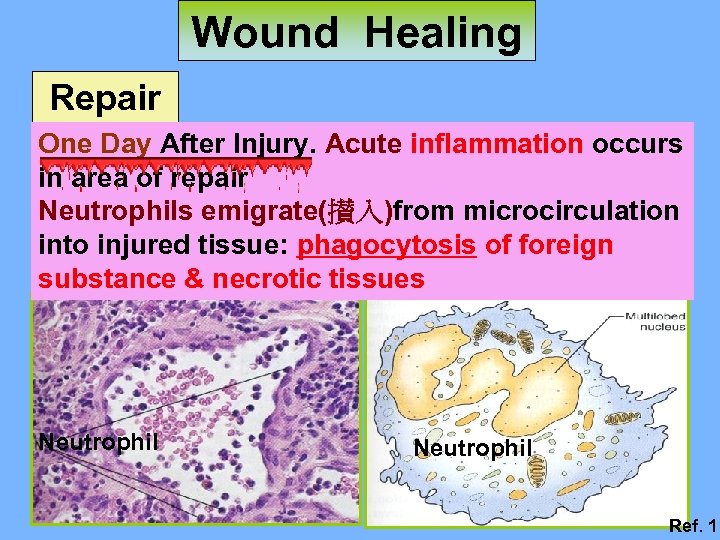
Wound Healing Repair One Day After Injury. Acute inflammation occurs in area of repair Neutrophils emigrate(攅入)from microcirculation into injured tissue: phagocytosis of foreign substance & necrotic tissues Neutrophil Ref. 1
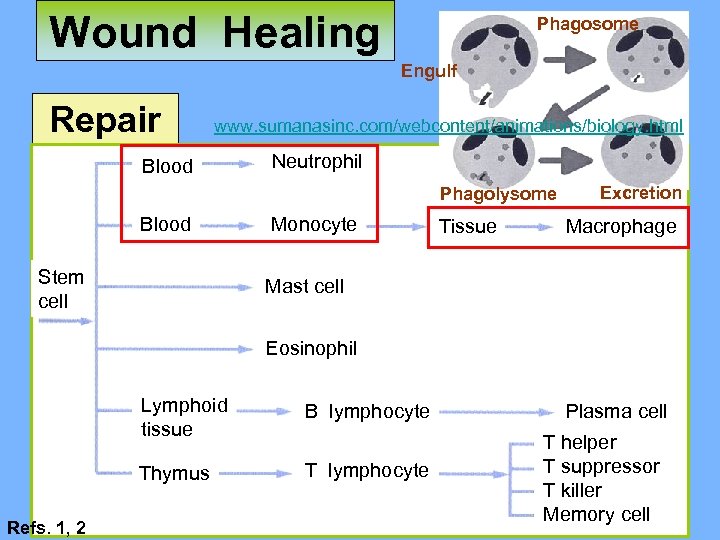
Wound Healing Phagosome Engulf Repair www. sumanasinc. com/webcontent/animations/biology. html Blood Neutrophil Phagolysome Blood Stem cell Monocyte Tissue Excretion Macrophage Mast cell Eosinophil Lymphoid tissue Thymus Refs. 1, 2 B lymphocyte T lymphocyte Plasma cell T helper T suppressor T killer Memory cell
Wound Healing Repair Stem Cell Differentiation
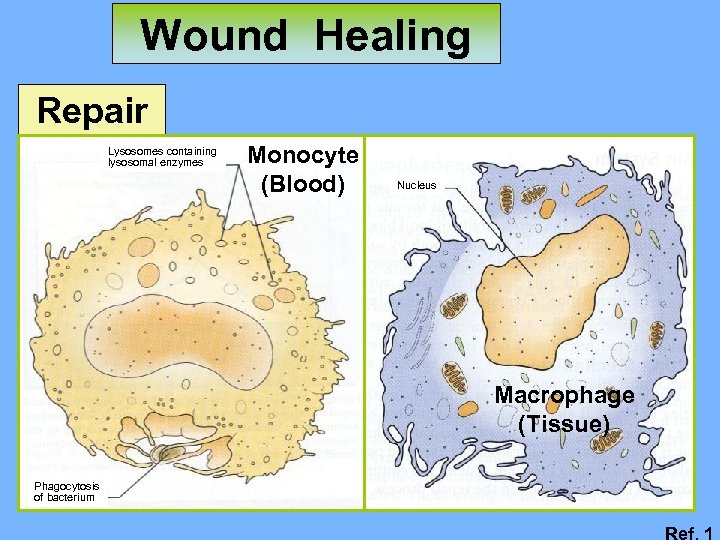
Wound Healing Repair Lysosomes containing lysosomal enzymes Monocyte (Blood) Nucleus Macrophage (Tissue) Phagocytosis of bacterium Ref. 1
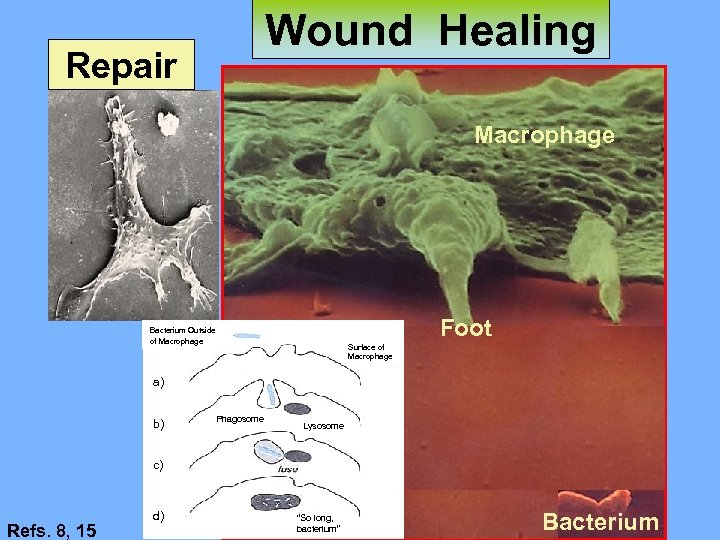
Wound Healing Repair Macrophage Foot Bacterium Outside of Macrophage Surface of Macrophage a) b) Phagosome Lysosome c) Refs. 8, 15 d) “So long, bacterium” Bacterium

Wound Healing Repair
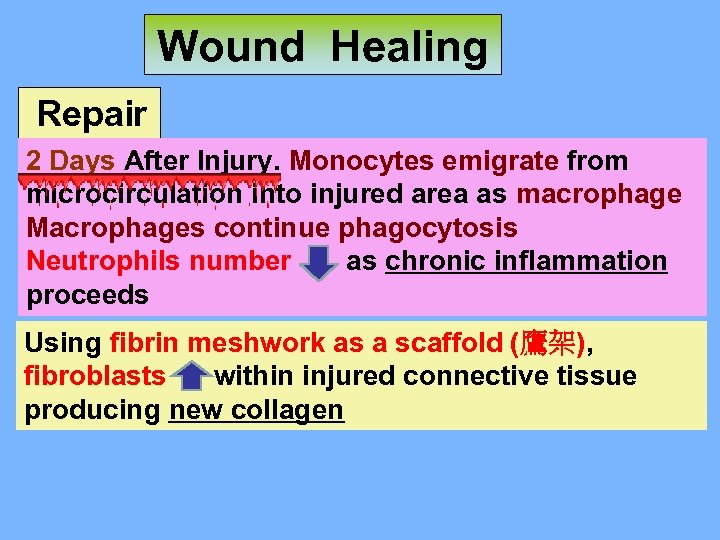
Wound Healing Repair 2 Days After Injury. Monocytes emigrate from microcirculation into injured area as macrophage Macrophages continue phagocytosis Neutrophils number as chronic inflammation proceeds Using fibrin meshwork as a scaffold (鷹架), fibroblasts within injured connective tissue producing new collagen
Wound Healing Repair Initial tissue formed in connective tissue is granulation tissue: More capillaries & fibroblasts Sometimes the growth is excessive Need removal for proper healing
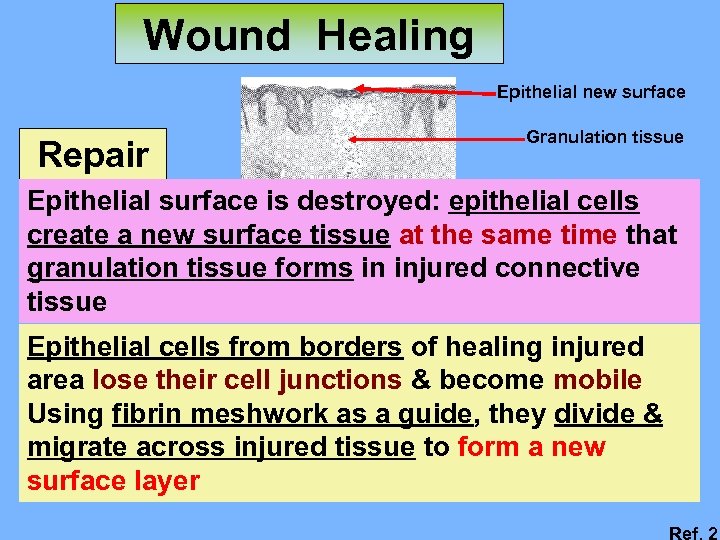
Wound Healing Epithelial new surface Repair Granulation tissue Epithelial surface is destroyed: epithelial cells create a new surface tissue at the same time that granulation tissue forms in injured connective tissue Epithelial cells from borders of healing injured area lose their cell junctions & become mobile Using fibrin meshwork as a guide, they divide & migrate across injured tissue to form a new surface layer Ref. 2
Wound Healing Repair Functions of fibrin meshwork 1. Guide for migrating epithelial cells 2. Scaffold forming connective tissue 3. Protect the two newly formed tissues Clot remains in place is important: 1. Allow optimal repair in both tissues 2. Dressing placed over the clot is beneficial to healing process
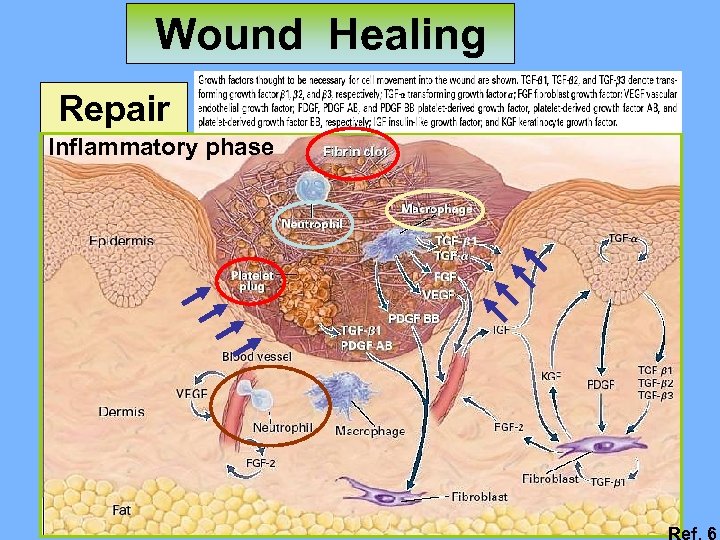
Wound Healing Repair Inflammatory phase Ref. 6
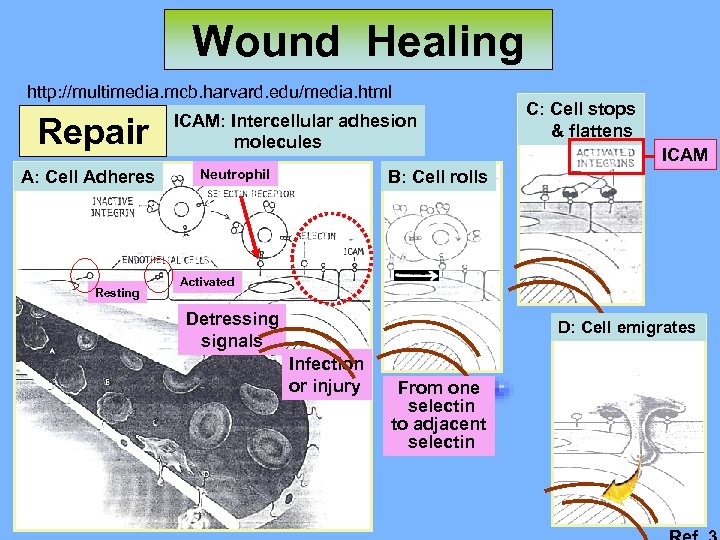
Wound Healing http: //multimedia. mcb. harvard. edu/media. html Repair A: Cell Adheres Resting ICAM: Intercellular adhesion molecules Neutrophil C: Cell stops & flattens ICAM B: Cell rolls Activated Detressing signals D: Cell emigrates Infection or injury From one selectin to adjacent selectin

Wound Healing Repair Reepithelization & neovascularization 1. Guide for migrating epithelial cells 2. Scaffold for collagen 3. Protection Ref. 6
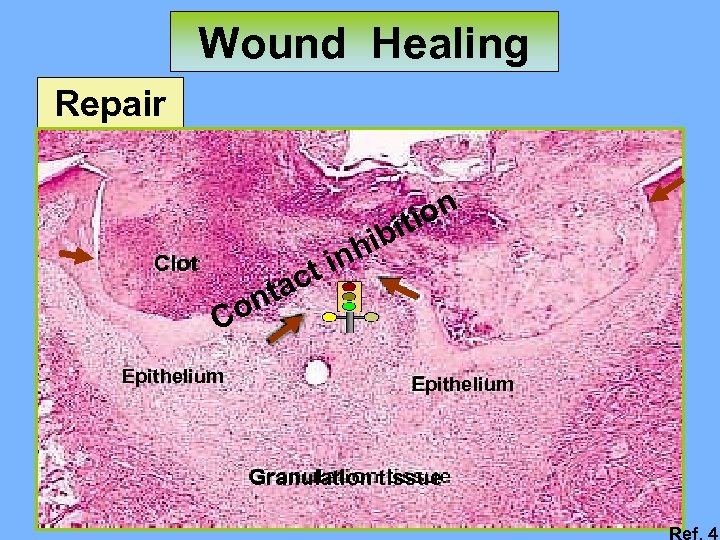
Wound Healing Repair ion it Clot ct ta hib in on C Epithelium Granulation tissue Ref. 4

Wound Healing Repair Clot Mitosis Capillary spouts Ref. 4
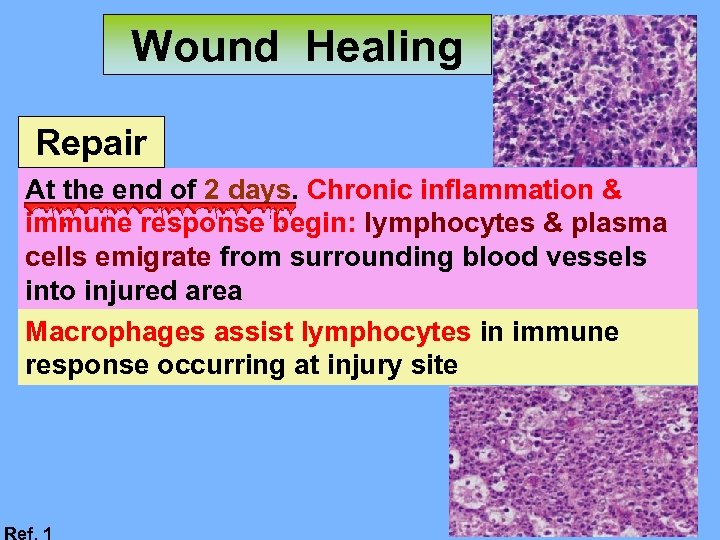
Wound Healing Repair At the end of 2 days. Chronic inflammation & immune response begin: lymphocytes & plasma cells emigrate from surrounding blood vessels into injured area Macrophages assist lymphocytes in immune response occurring at injury site Ref. 1
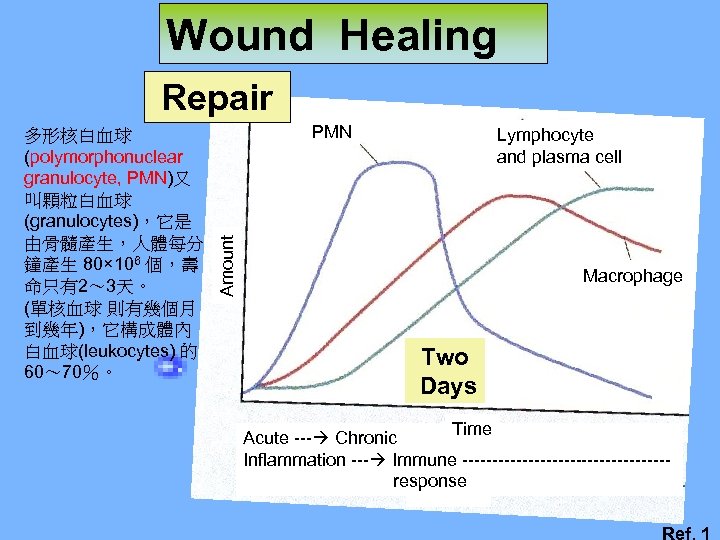
Wound Healing Repair PMN Lymphocyte and plasma cell Amount 多形核白血球 (polymorphonuclear granulocyte, PMN)又 叫顆粒白血球 (granulocytes),它是 由骨髓產生,人體每分 鐘產生 80× 106 個,壽 命只有2~ 3天。 (單核血球 則有幾個月 到幾年),它構成體內 白血球(leukocytes) 的 60~ 70%。 Macrophage Two Days Time Acute --- Chronic Inflammation --- Immune -----------------response Ref. 1
Wound Healing Repair 7 Days After Injury. Fibrin is digested by collagenase & sloughs off, & initial repair is completed Repaired injury surface remains redder: thinness of new epithelium & vascularity of new connective tissue

Wound Healing Repair Lymphocyte and plasma cell Amount PMN Macrophage Two Days Time Acute --- Chronic Inflammation --- Immune -----------------response Seven Days Ref. 1
Wound Healing Repair Contraction 2 Wks After Injury. Initial granulation tissue & its fibers are remodeled, giving full tissue strength New tissue is called scar tissue & appears whiter or paler at repaired injury surface due to collagen & vascularity

Wound Healing Repair Ref. 9
Wound Healing Repair Scar tissue amount depends on: heredity, strength & flexibility needed, repair type Oral mucosa is lesser scar formation than skin
Wound Healing Repair Types of repair: Healing by primarily intention Little tissue loss, clean edges joined with sutures to form a small clot, & little granulation tissue Less scar tissue & higher retention
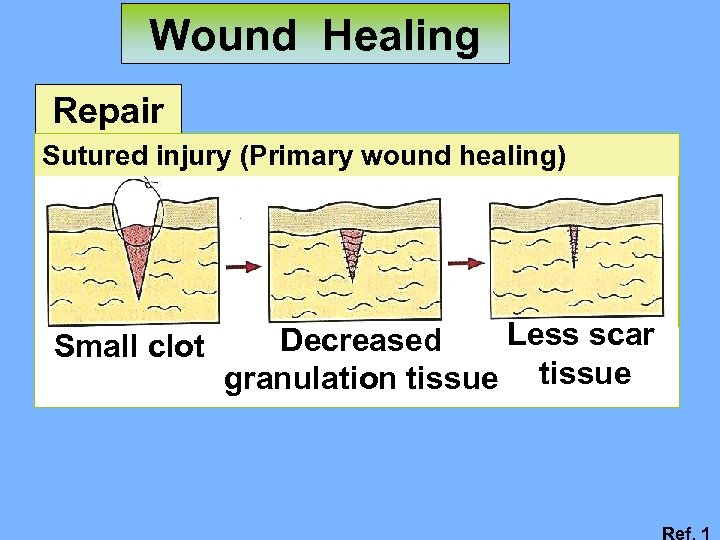
Wound Healing Repair Sutured injury (Primary wound healing) Small clot Less scar Decreased granulation tissue Ref. 1
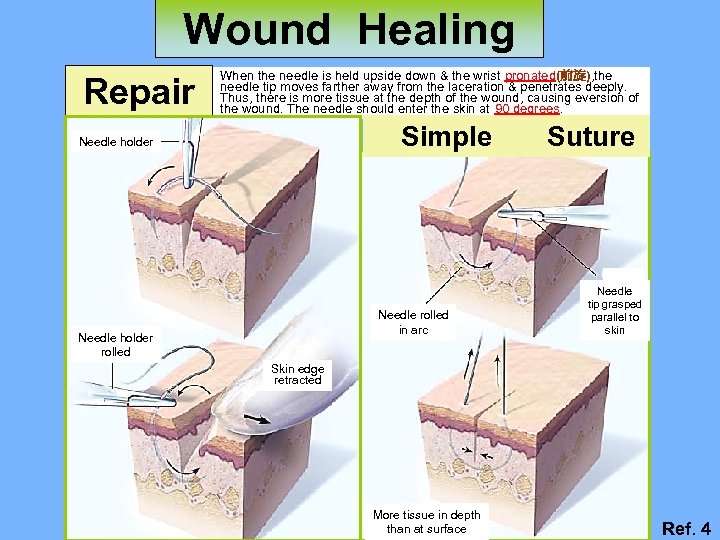
Wound Healing Repair When the needle is held upside down & the wrist pronated(前旋), the needle tip moves farther away from the laceration & penetrates deeply. Thus, there is more tissue at the depth of the wound, causing eversion of the wound. The needle should enter the skin at 90 degrees. Simple Needle holder Needle rolled in arc Needle holder rolled Suture Needle tip grasped parallel to skin Skin edge retracted More tissue in depth than at surface Ref. 4
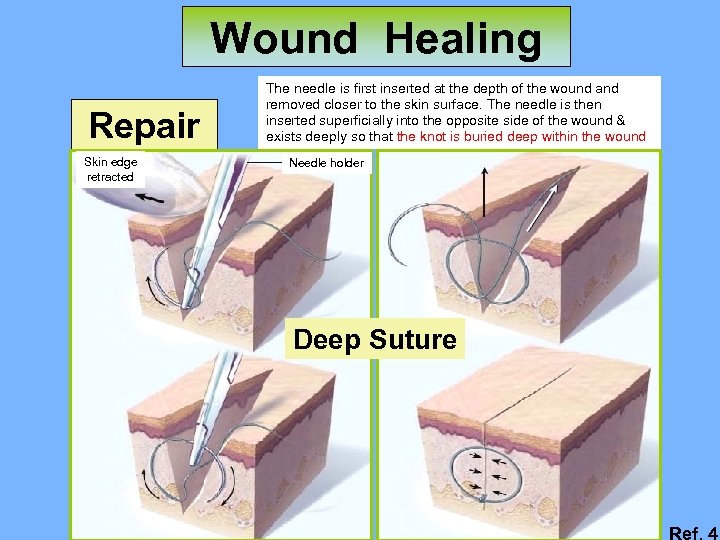
Wound Healing Repair Skin edge retracted The needle is first inserted at the depth of the wound and removed closer to the skin surface. The needle is then inserted superficially into the opposite side of the wound & exists deeply so that the knot is buried deep within the wound Needle holder Deep Suture Ref. 4
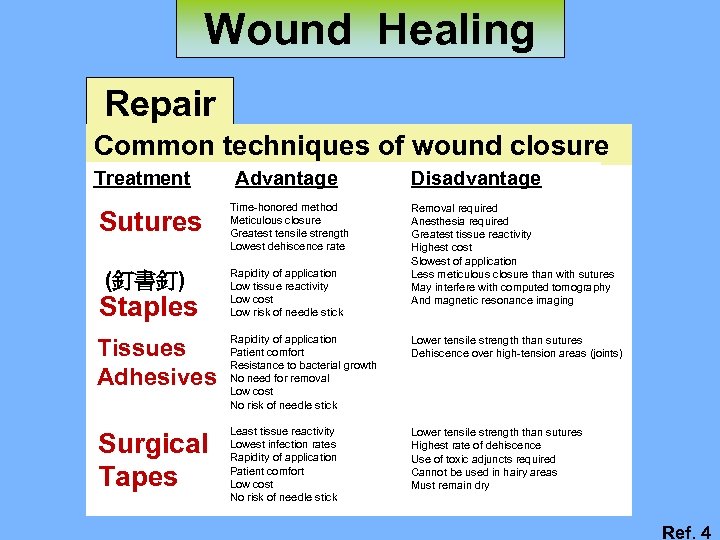
Wound Healing Repair Common techniques of wound closure Treatment Sutures (釘書釘) Staples Advantage Time-honored method Meticulous closure Greatest tensile strength Lowest dehiscence rate Rapidity of application Low tissue reactivity Low cost Low risk of needle stick Disadvantage Removal required Anesthesia required Greatest tissue reactivity Highest cost Slowest of application Less meticulous closure than with sutures May interfere with computed tomography And magnetic resonance imaging Tissues Adhesives Rapidity of application Patient comfort Resistance to bacterial growth No need for removal Low cost No risk of needle stick Lower tensile strength than sutures Dehiscence over high-tension areas (joints) Surgical Tapes Least tissue reactivity Lowest infection rates Rapidity of application Patient comfort Low cost No risk of needle stick Lower tensile strength than sutures Highest rate of dehiscence Use of toxic adjuncts required Cannot be used in hairy areas Must remain dry Ref. 4
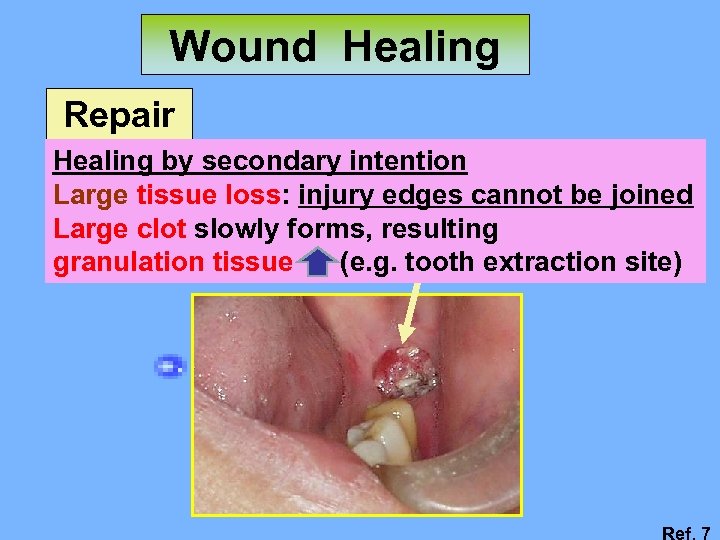
Wound Healing Repair Healing by secondary intention Large tissue loss: injury edges cannot be joined Large clot slowly forms, resulting granulation tissue (e. g. tooth extraction site) Ref. 7
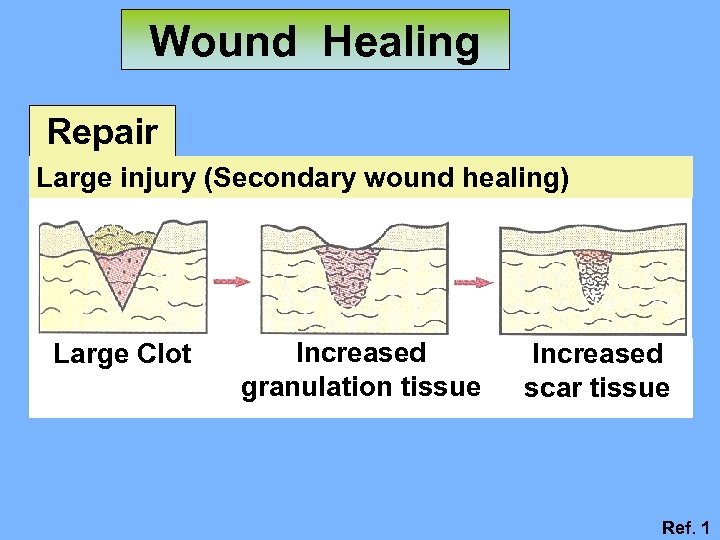
Wound Healing Repair Large injury (Secondary wound healing) Large Clot Increased granulation tissue Increased scar tissue Ref. 1
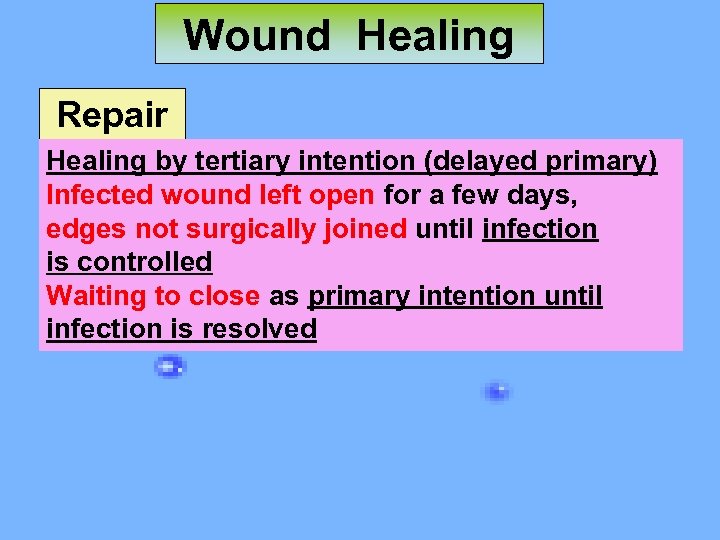
Wound Healing Repair Healing by tertiary intention (delayed primary) Infected wound left open for a few days, edges not surgically joined until infection is controlled Waiting to close as primary intention until infection is resolved
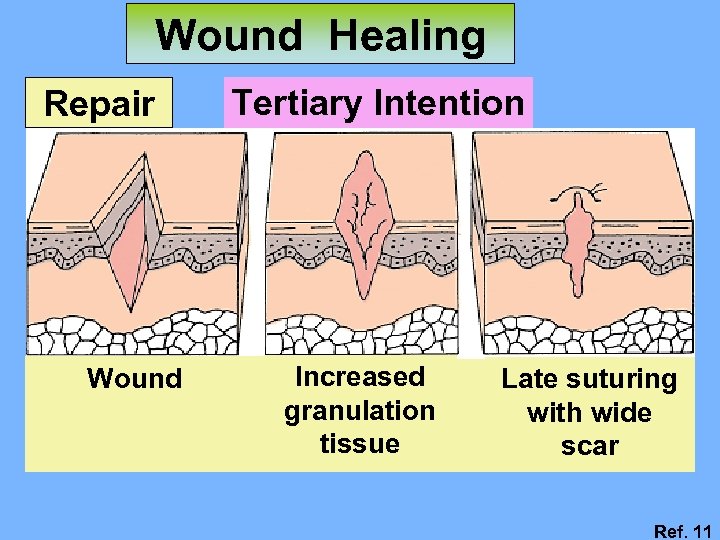
Wound Healing Repair Wound Tertiary Intention Increased granulation tissue Late suturing with wide scar Ref. 11

Wound Healing Repair Keloid Excess scarring in skin: surgically removed keloid Ref. 1

Wound Healing Repair Wound closure Necessary for survival – reduces risk of infection etc. (REVIEW) Scarring Unnecessary for wound closure – may simply be a side-effect Ref. 10
Wound Healing Repair (REVIEW) HEALING PROGRESS: ACUTE WOUNDS l Sequence completed in continuous & expected time frame l Usually achieved with few or no complications l Overreaction in acute wound healing - Keloids - Hypertrophic scars Ref. 10

Wound Healing (REVIEW) Repair Phases of Wound Healing Hemostasis & Inflammation Fibroplasia 0 Injury 2 4 6 8 Days after injury Maturation 365 Ref. 10
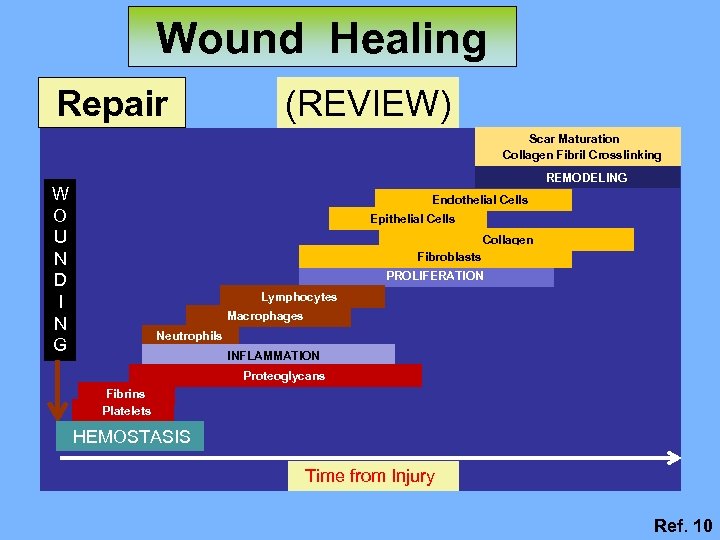
Wound Healing Repair (REVIEW) Scar Maturation Collagen Fibril Crosslinking REMODELING W O U N D I N G Endothelial Cells Epithelial Cells Collagen Fibroblasts PROLIFERATION Lymphocytes Macrophages Neutrophils INFLAMMATION Proteoglycans Fibrins Platelets HEMOSTASIS Time from Injury Ref. 10

Wound Healing (REVIEW) Repair COMPONENTS OF WOUND HEALING Cell Types Involved Coagulation Process Platelets Inflammation Process Platelet Macrophages Neutrophils Migratory Proliferative Process Macrophages Lymphocytes Fibroblasts Epithelial cells Endothelial cells Remodeling Process Fibroblasts Injury Hours Days Weeks Ref. 10
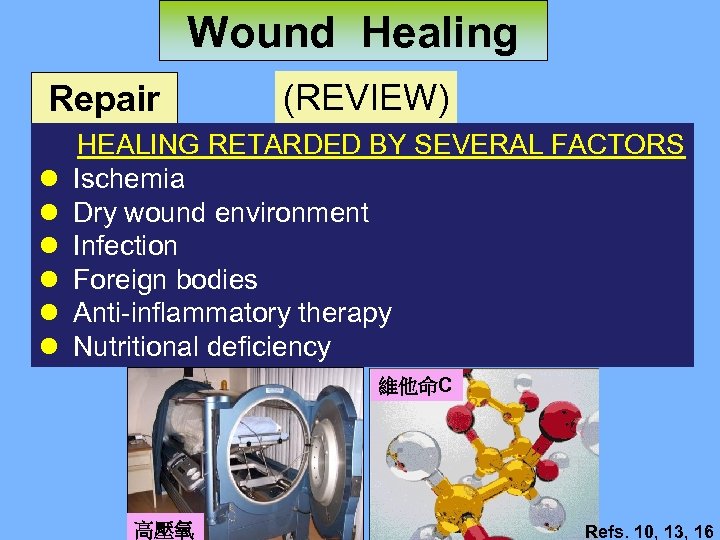
Wound Healing Repair l l l (REVIEW) HEALING RETARDED BY SEVERAL FACTORS Ischemia Dry wound environment Infection Foreign bodies Anti-inflammatory therapy Nutritional deficiency 維他命C 高壓氧 Refs. 10, 13, 16
Wound Healing Repair (REVIEW) EFFECTS OF BACTERIA ON WOUND HEALING l Quantitative bacterial cultures: >106 per gm l Presence of significant organisms - Staphylococcus aureus - Pseudomonas species - Streptococcus species Ref. 10
Wound Healing Repair (REVIEW) FUTURE OF WOUND HEALING l Continued research - Elucidation of signals/growth factors involved in: * Epithelization * Wound contraction and scarring * Angiogenesis l Tissue engineering l Gene therapy Ref. 10
Wound Healing Repair Tooth Extraction Wound
Wound Healing Repair Tooth Extraction Wound 拔牙後,齒槽癒合的程序:(一)血塊之形成,(二)血塊之 有機化,血管之再生,(三)肉芽組織出現,(四)噬骨細胞 (osteoclast)的出現、造骨細胞(osteoblast)的出現,(五)硬 組織修補。 癒合過程中除上述之機轉,局部因子與全身因子亦參與調 節傷口癒合。如 PTH、vitamin D、calcitonin、 glucocorticoid、sex steroid (estrogen、androgen)、 progestins、thyroid hormone、retinoid、GH、IGF、IGG、 IGF、TGFB I. III、BMP等cytokine。這些局部因子或全身 因子以局部癒合加速現象RAP (regional accelerate phenomenon) (Frost, 1983),或全身癒合加速現象SAP (systemic accelerate phenomenon),局部或全身,直接或 間接影響拔牙傷口癒合。 Ref. 18
Wound Healing Repair Tooth Extraction Wound 關於齒槽骨於拔牙後傷口之癒合,Mangos(1941)於人 類拔牙傷口癒合組織學的研究,觀察到之變化: 術後3天,纖維細胞(fibroblast)出現於血塊邊緣。 術後7天,血管開始有機化。 上皮幾乎覆蓋拔牙傷口。 術後14天,上皮已覆蓋拔牙傷口,並有骨小樑 (trabeculae)出現。 術後40天,拔牙槽之上半部有明顯的纖維組織。 術後72天,上皮組織已很完整,皮下肉芽組織已不復見, 且已被緻密結締組織取代。 Ref. 18
Wound Healing Repair Tooth Extraction Wound Amler(1960)有類似發表,特別是在術後7天的拔牙傷口 有造骨纖維(osteogenic fiber)出現。 Amler的觀點被Carter等人(1991)證實,並說明此類造 骨纖維即是新生骨(woven bone or immature bone)生成 時的模板(template)架構,日後此骨塑形(bone modeling) 所生成的新生骨經過骨重塑形的過程轉為成熟的板狀骨 (lamellar bone)。 Ref. 18
Wound Healing Repair Tooth Extraction Wound 除了上面三篇外,Boyne(1996)以四環素(tetracycline) 作為骨骼螢光標記(Fluorochrome bone labels),認為拔牙 傷口內新生骨出現於術後10天,並且先出現於拔牙槽的側 壁(socket wall),而非過去認為齒槽底部(socket fundus)。 除人類外,其他動物拔牙傷口癒合過程也有大量研究報 告,如:Eyler(1920)、Dalogh(1932)、Meyer(1935)、 Claflin(1930)等人用狗;Huebsch(1952)、Smith(1974)、 Hsieh等人(1994, 1995)用大白鼠; Simpson(1958)、 Radden(1959)等人用猴子做拔牙傷口癒合之研究,基本癒 合模式(healing pattern)均類似,只因物種(species)不同, 生長代謝速率不同而有時間快慢之別。
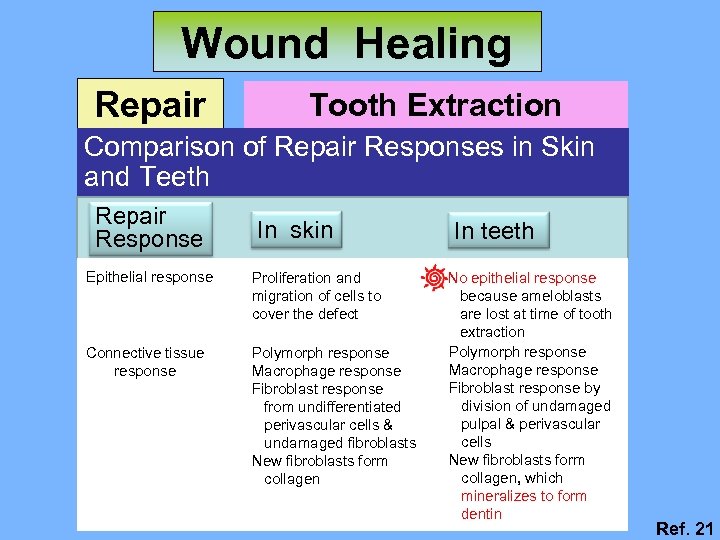
Wound Healing Repair Tooth Extraction Wound Comparison of Repair Responses in Skin and Teeth Repair Response In skin Epithelial response Proliferation and migration of cells to cover the defect Connective tissue response Polymorph response Macrophage response Fibroblast response from undifferentiated perivascular cells & undamaged fibroblasts New fibroblasts form collagen In teeth No epithelial response because ameloblasts are lost at time of tooth extraction Polymorph response Macrophage response Fibroblast response by division of undamaged pulpal & perivascular cells New fibroblasts form collagen, which mineralizes to form dentin Ref. 21
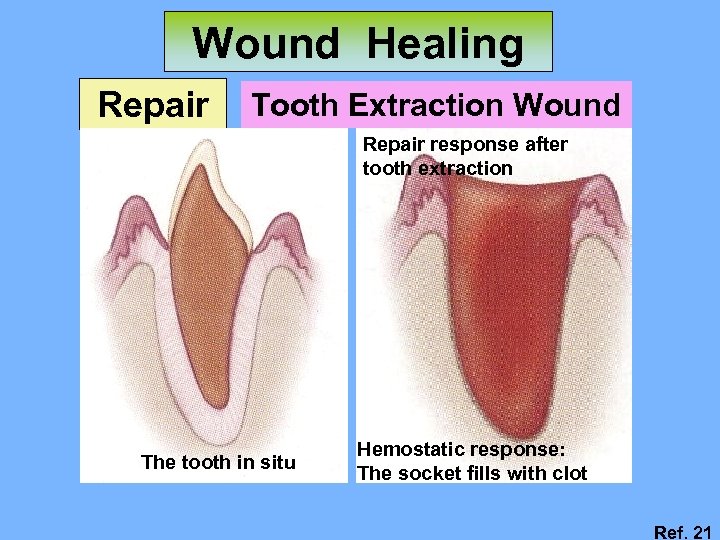
Wound Healing Repair Tooth Extraction Wound Repair response after tooth extraction The tooth in situ Hemostatic response: The socket fills with clot Ref. 21
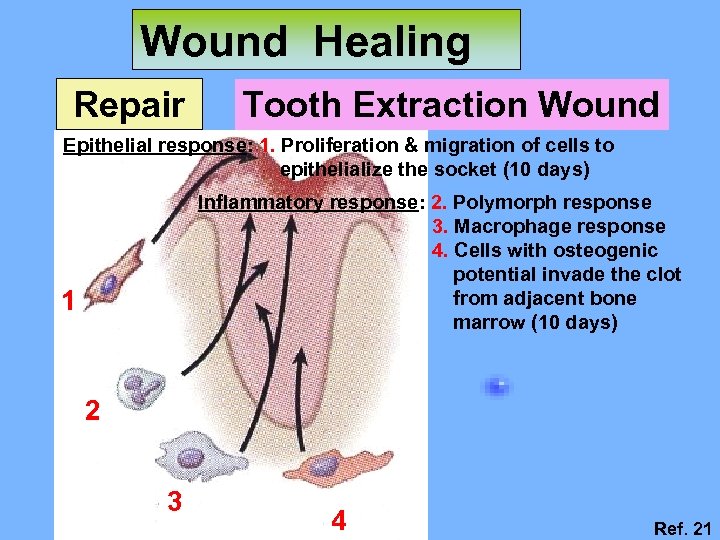
Wound Healing Repair Tooth Extraction Wound Epithelial response: 1. Proliferation & migration of cells to epithelialize the socket (10 days) Inflammatory response: 2. Polymorph response 3. Macrophage response 4. Cells with osteogenic potential invade the clot from adjacent bone marrow (10 days) 1 2 3 4 Ref. 21
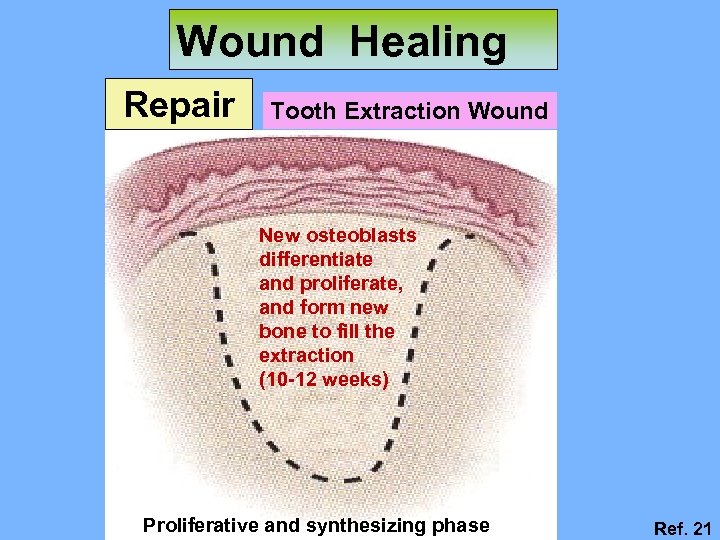
Wound Healing Repair Tooth Extraction Wound New osteoblasts differentiate and proliferate, and form new bone to fill the extraction (10 -12 weeks) Proliferative and synthesizing phase Ref. 21
Wound Healing Repair Tooth Extraction Wound Normal Healing Extraction wound Delayed Healing (dry socket) Ref. 17
Wound Healing Repair Bone Tissue Repair Bone injury repair is similar to process that occurs in connective tissue except that it involves bone tissue creation, produced by osteoblasts
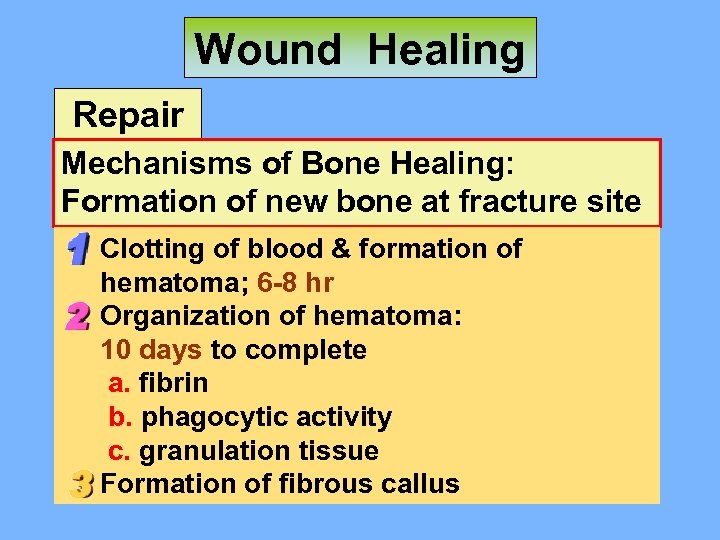
Wound Healing Repair Mechanisms of Bone Healing: Formation of new bone at fracture site Clotting of blood & formation of hematoma; 6 -8 hr Organization of hematoma: 10 days to complete a. fibrin b. phagocytic activity c. granulation tissue Formation of fibrous callus
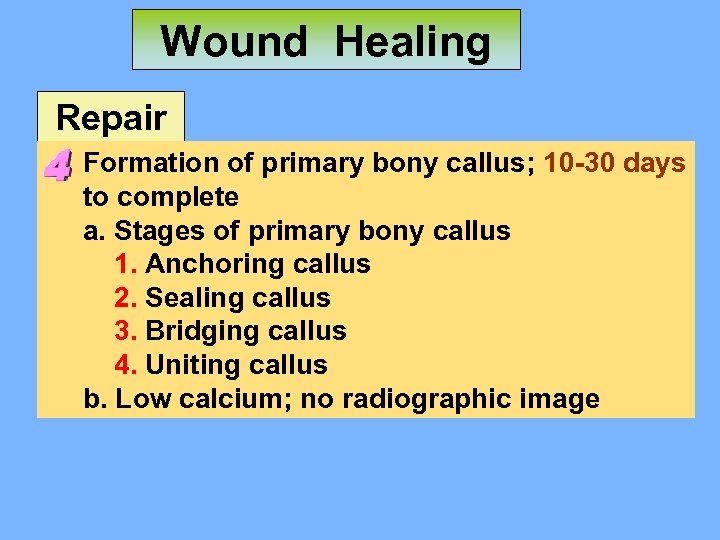
Wound Healing Repair Formation of primary bony callus; 10 -30 days to complete a. Stages of primary bony callus 1. Anchoring callus 2. Sealing callus 3. Bridging callus 4. Uniting callus b. Low calcium; no radiographic image
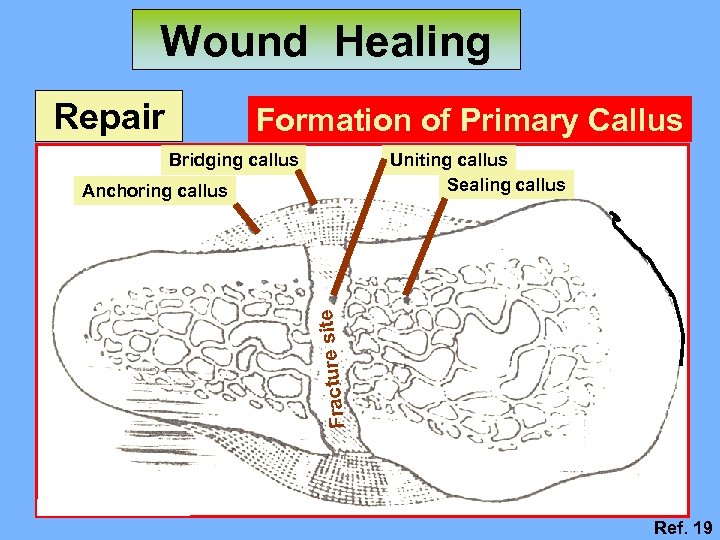
Wound Healing Repair Formation of Primary Callus Bridging callus Uniting callus Sealing callus Fracture s ite Anchoring callus Ref. 19
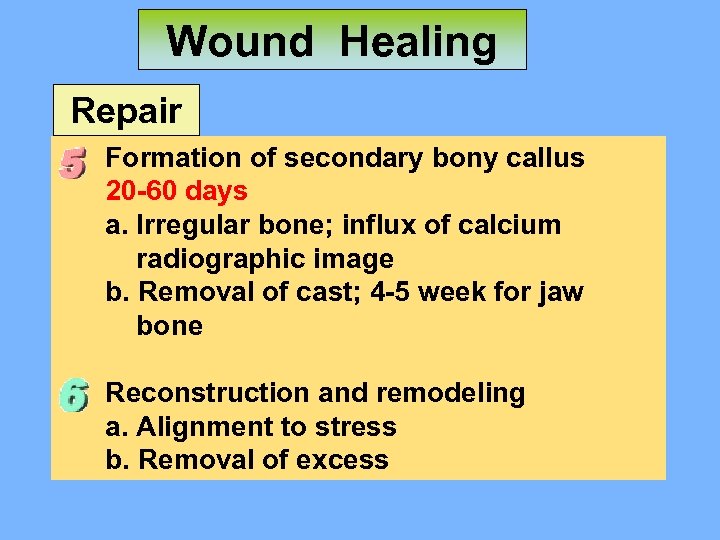
Wound Healing Repair Formation of secondary bony callus 20 -60 days a. Irregular bone; influx of calcium radiographic image b. Removal of cast; 4 -5 week for jaw bone Reconstruction and remodeling a. Alignment to stress b. Removal of excess
Wound Healing Repair Healing of bone depends on: Interrupted by removal of osteoblast-producing tissues Increased movement of bone Presence of edema or infection

Wound Healing Repair Fixation 1 Fixation 2
Wound Healing Repair Carcinoma cells & their surrounding stroma behave remarkably similar to cells in a healing wound with characteristics such as rapid division, migration, remodeling & invasion of connective tissue, & ability to induce angiogenesis Wound healing genes promote cancer progression In 1986, Harold Dvorak (Berth Israel Deaconess Medical Center, Boston, MA, USA) made the most graphic analogy between wound healing & cancer when he said that tumors are wounds that do not heal Ref. 7
口腔病理科 SUMMARIES 1. Regeneration & repair 2. Epithelium & connective tissue 3. Tooth extraction wound 4. Bone fracture Processes, types, characteristics
cd0d44d701e9d353063ce8739f845be1.ppt