Zabolotnikova Daria Clinical Case: Saccular cerebral aneurysm СНК

Zabolotnikova Daria Clinical Case: Saccular cerebral aneurysm СНК РНЦХ «Лучевая диагностика в хирургии»
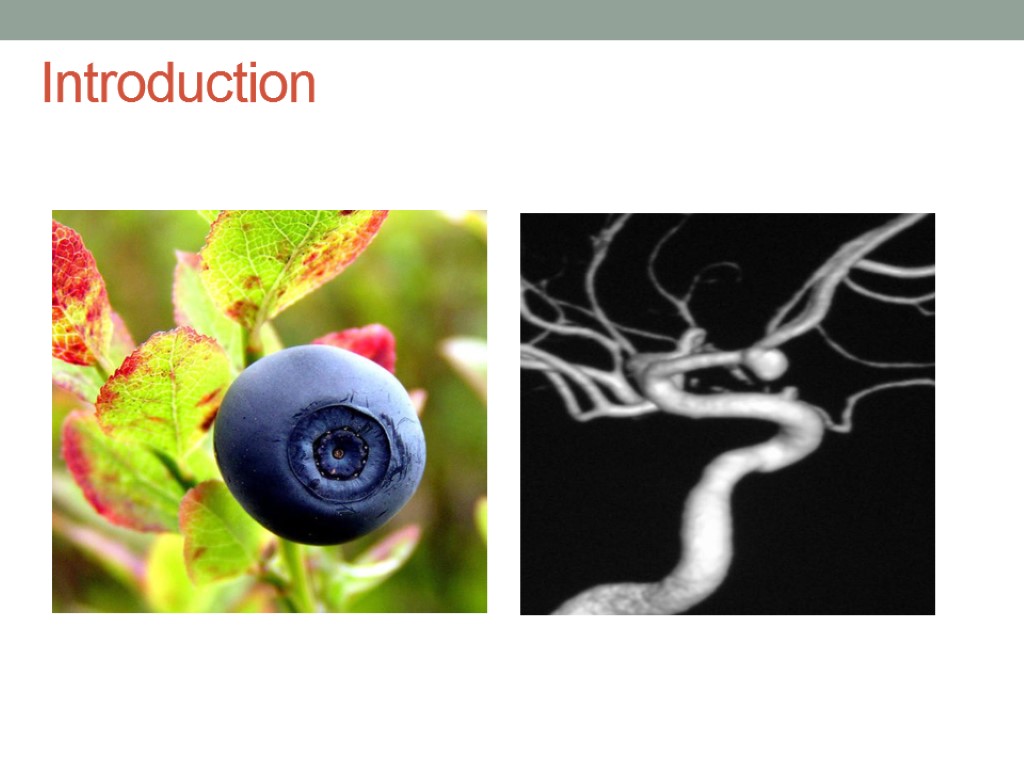
Introduction The word aneurysm comes from the Greek word aneurysma ("dilatation"). An aneurysm is an abnormal local dilatation in the wall of a blood vessel, usually an artery, that develops as a consequence of a defect, disease, or injury. The common causes of intracranial aneurysm include hemodynamically induced or degenerative vascular injury, atherosclerosis (typically leading to fusiform aneurysms), underlying vasculopathy (fibromuscular dysplasia [FMD]), and high-flow states, as in arteriovenous malformation (AVM) and fistula. Uncommon causes include trauma, infection, drugs, and neoplasms (primary or metastatic). Aneurysms can be true or false. A false aneurysm is a cavity lined by blood clot. The three major types of true intracranial aneurysms are as follows: Saccular aneurysms (Degenerative or developmental; traumatic; mycotic; oncotic; flow-related; vasculopathy-related; and drug-related) Fusiform aneurysms Dissecting aneurysms
Introduction
Etiology Family history. People who have a family history of brain aneurysms are more likely to have an aneurysm than those who don't. Previous aneurysm. People who have had a brain aneurysm are more likely to have another. Gender. Women are more likely to develop a brain aneurysm or to suffer a subarachnoid hemorrhage. Race. African Americans are more likely than whites to have a subarachnoid hemorrhage. High blood pressure. The risk of subarachnoid hemorrhage is greater in people who have a history of high blood pressure. Smoking. In addition to being a cause of high blood pressure, the use of cigarettes may greatly increase the chances of a brain aneurysm rupturing.
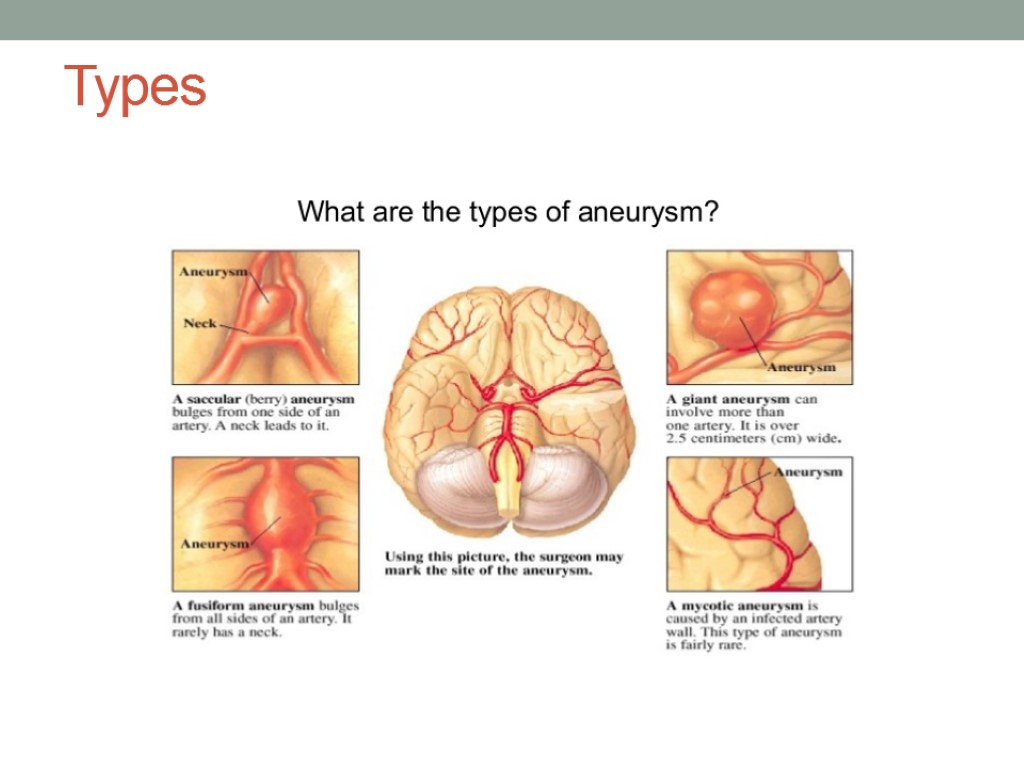
Types
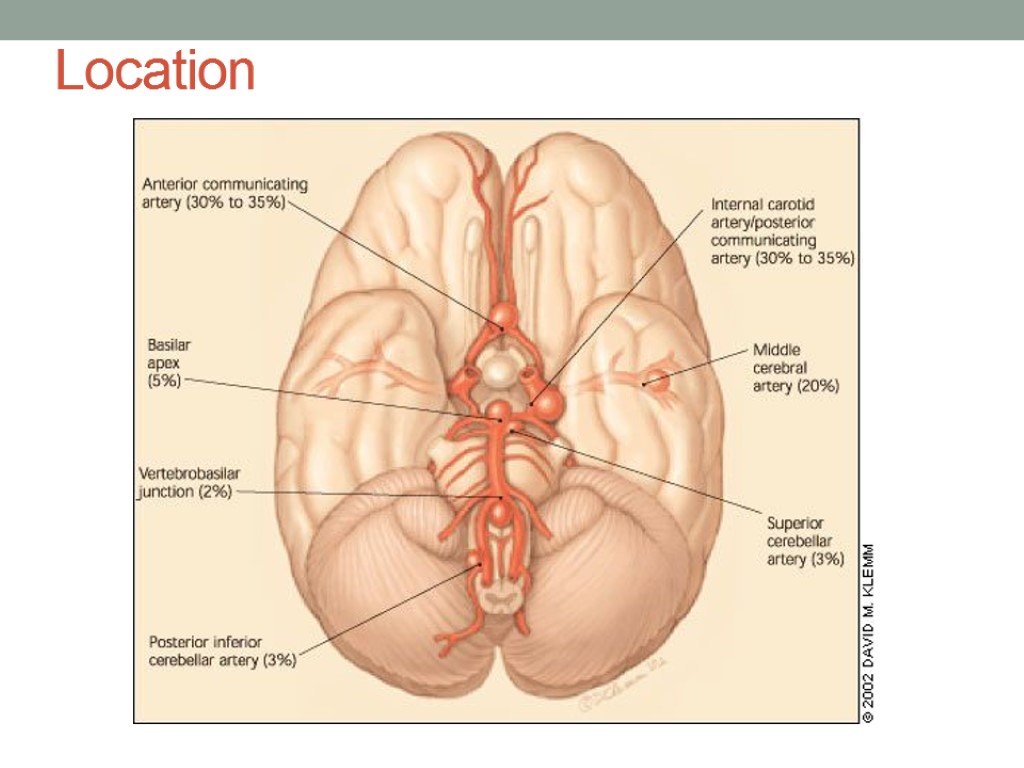
Location
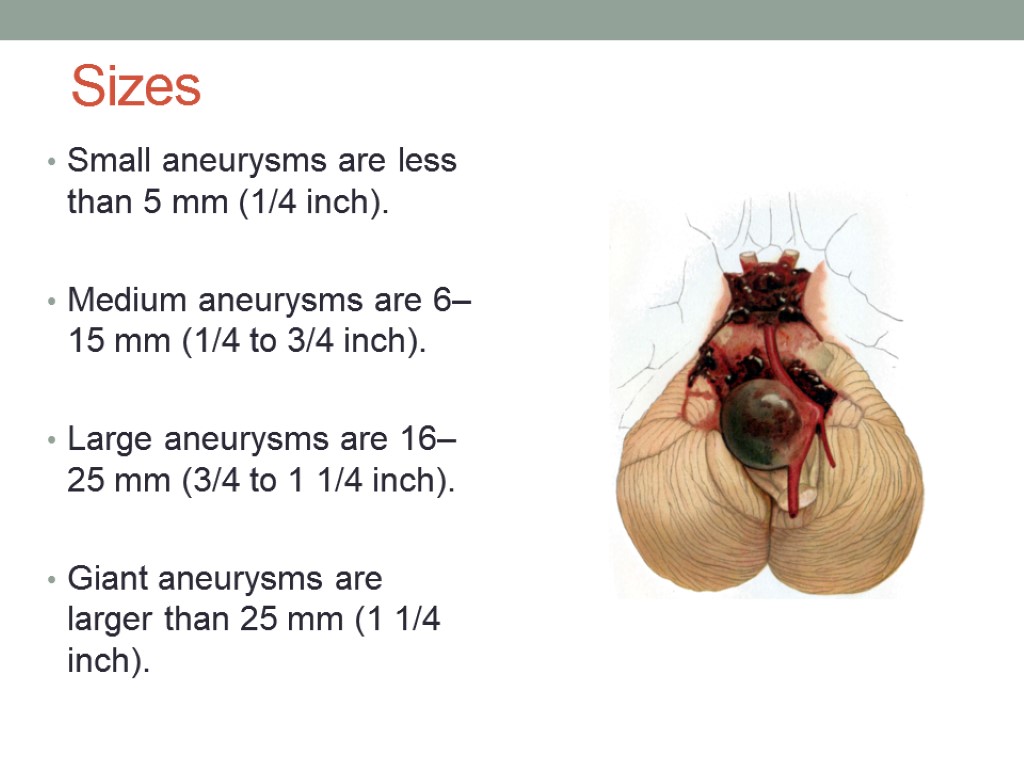
Sizes Small aneurysms are less than 5 mm (1/4 inch). Medium aneurysms are 6–15 mm (1/4 to 3/4 inch). Large aneurysms are 16–25 mm (3/4 to 1 1/4 inch). Giant aneurysms are larger than 25 mm (1 1/4 inch).
Signs and symptoms Symptoms associated with cerebral aneurysms and SAH are as follows: Headache Facial pain Alterations in consciousness Seizures Manifestations of meningeal irritation Autonomic disturbances Focal neurologic complaints Visual symptoms Respiratory dysfunction Cardiovascular instability Hormonal dysfunction Epistaxis
Epidemiology Prevalence of saccular cerebral aneurysms in the asymptomatic general population has been reported over a wide range (0.2-8.9%) when examined angiographically, and in 15-30% of these patients, multiple aneurysms are found A familial tendency to aneurysms is also well recognised, with patients who have more than one first-degree relative affected, having a ~30% (range 17-44%) chance of themselves having an aneurysm
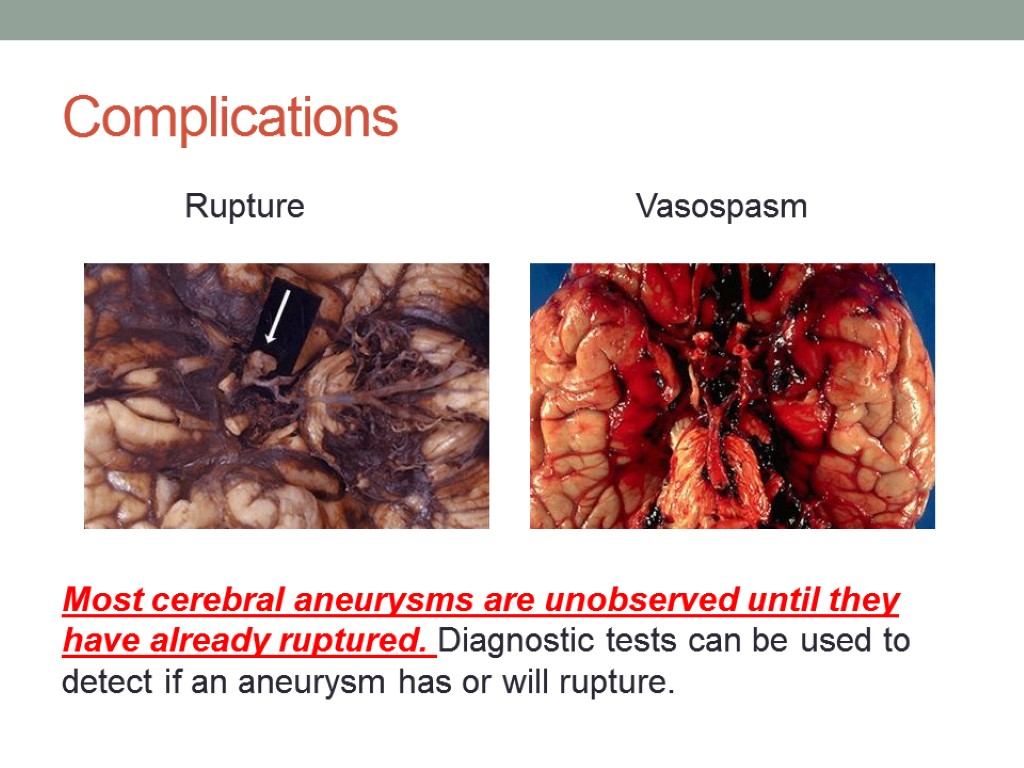
Complications Rupture Vasospasm Most cerebral aneurysms are unobserved until they have already ruptured. Diagnostic tests can be used to detect if an aneurysm has or will rupture.
Radiographic features CT angiography (CTA) MR angiography (MRA) digital subtraction (catheter) angiography (DSA) Each of these confers certain advantages and disadvantages, although in general digital subtraction catheter angiography, especially with 3D acquisitions, is considered the gold standard in most institutions.
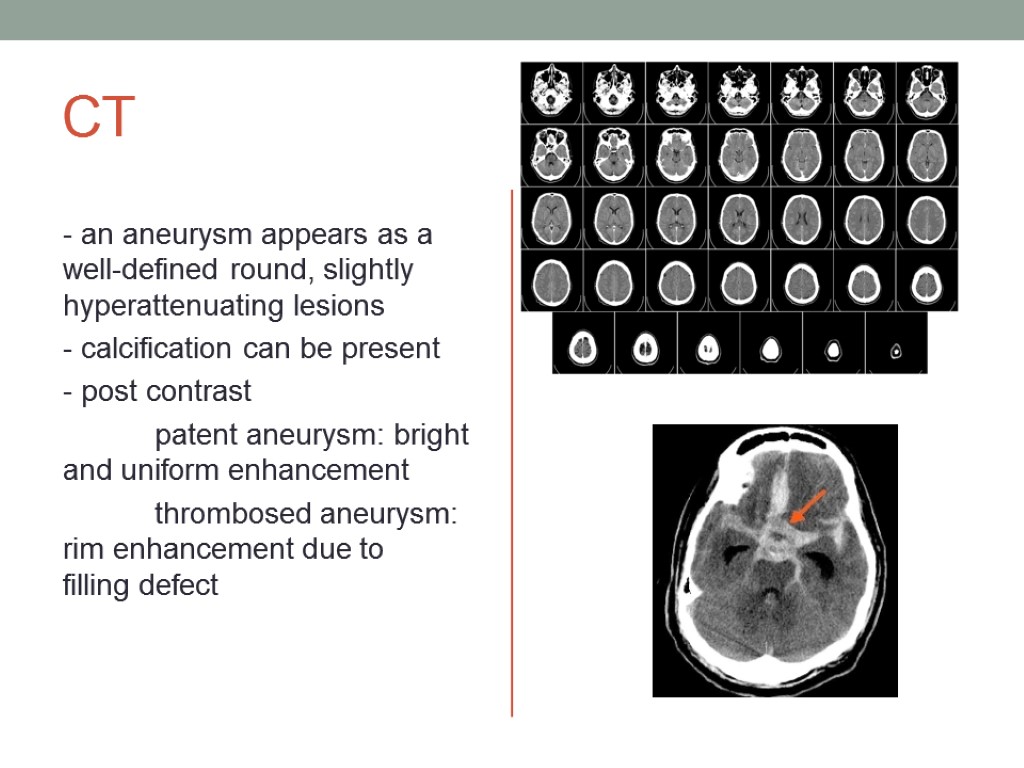
CT - an aneurysm appears as a well-defined round, slightly hyperattenuating lesions - calcification can be present - post contrast patent aneurysm: bright and uniform enhancement thrombosed aneurysm: rim enhancement due to filling defect
MRI On MRI also the patent and thrombosed aneurysm display different imaging features: T1 most of the patent aneurysm appears as flow void, or they may show heterogeneous signal intensity in thrombosed aneurysm appearance depends on the age of clot within the lumen T2 typically hypointense laminated thrombus may show a hyperintense rim
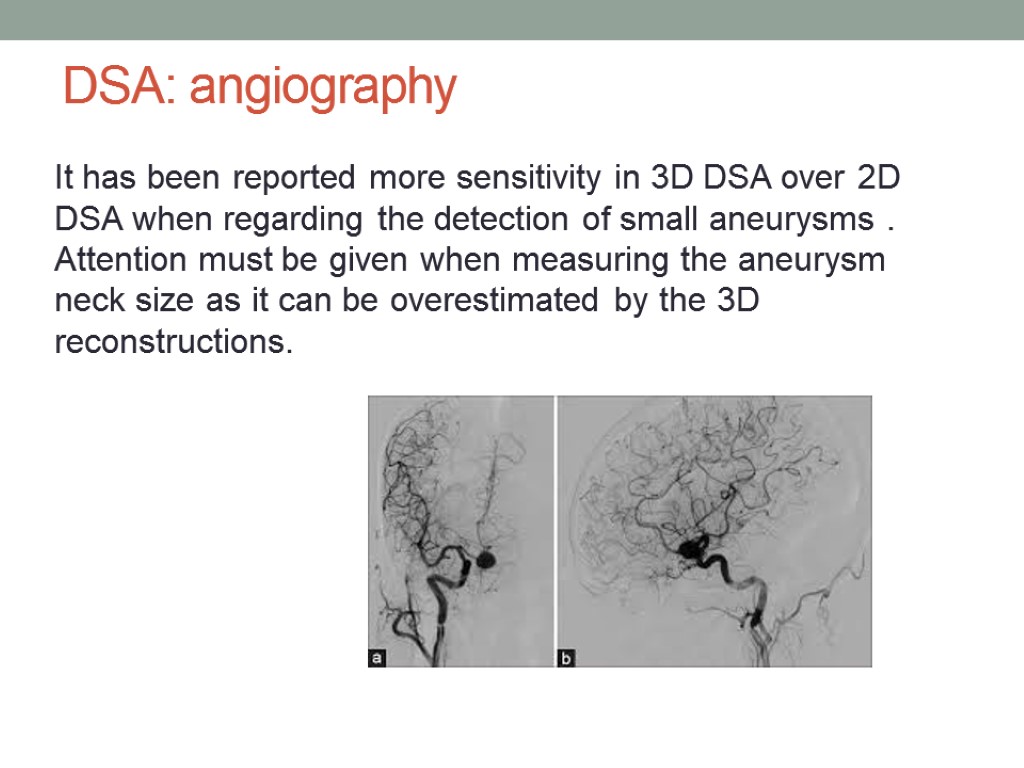
DSA: angiography It has been reported more sensitivity in 3D DSA over 2D DSA when regarding the detection of small aneurysms . Attention must be given when measuring the aneurysm neck size as it can be overestimated by the 3D reconstructions.
Clinical Case The patient F. is a 50-year-old female is brought by her husband to Emergency Center after experiencing sudden onset of severe headache associated with vomiting, neck stiffness, and weakness. Two weeks ago she returned from jogging noting a moderate headache with nausea and photophobia Did not have head trauma Has a history of hypertension(180/90Hhmg) and tobacco use (pack/years index – 15)
WHAT IS THE MOST LIKELY DIAGNOSIS? WHAT IS THE NEXT DIAGNOSTIC STEP? WHAT IS THE NEXT STEP IN THERAPY?
Considerations This 50-year-old woman has multiple risk factors for subarachnoid hemorrhage caused by an underlying aneurysm, including: HER AGE(mean age for subarachnoid hemorrhage is 50 years of age) HER SEX(slightly higher risk for females) HYPERTENSION(180/90 Hhmg) TOBACCO USE HER RECENT MODERATE HEADACHE AFTER JOGGING (physical strain) NEUROLOGIC SYMPTOMS
Answers The most likely diagnosis: subarachnoid hemorrhage Next diagnostic step: non-contrast CT of the head Next step in therapy: сerebral angiography
Objectives ! Identify the epidemiology and risk factors for subarachnoid hemorrhage ! Understand the prognosis and complications of subarachnoid hemorrhage ! Know a diagnostic and therapeutic approach to this condition

Diagnosis and prognosis Head CT without contrast is the most sensitive neuroimaging study for detecting subarachnoid bleeding, appearing as hyperdensity within the cerebral convexities, cisterns, and parenchyma Sensitivity of CT is greatest 24 hours after the event with 50% still detectable after 1 week Negative head CT occurs in 10-15% of cases, and should be further evaluated with lumber puncture looking for xanthochromia(yellowish discoloration of CSF) and increased red blood cells. Cerebrospinal fluid(CSF) studies are most sensitive 12 hours after onset, but can be negative in 10-15% of patients as well, in which case the prognosis is better
Diagnosis and prognosis(2) Up to 60% patients die in the 1st 30 days after a SAH ! 10% instantly without warning 40% 1st month mortality for hospitalized patients
Diagnosis and prognosis(3) Severity of cases and their prognoses can be graded based upon alertness and presence of local signs. GRADE I SAH-patients are alert with mild headache and nuchal rigidity and have a 5 % chance of deteriorating with a 3-5% mortality risk GRADE II patients have moderate-to-severe headache and nuchal rigidity, and a 6-10% mortality GRADE III patients have added confusion GRADE IV patients have stupor and moderate hemiparesis GRADE V patients are comatose with signs of severe increased intracranial pressure, they have the worst prognosis
Treatment GRADE I & GRADE II SAH may be observed after diagnostic measures Emergent conventional angiography is warranted if ruptured aneurysm is suspected and neurosurgical intervention is required. Endovascular coiling is indicated to reduce rebleeding in low-grade cases and has been shown to be superior to clipping. Clipping should be performed in the 1st 48 hours after onset or be delayed for 2 weeks to avoid the window of greatest risk of vasospasm, especially with complicated high-grade cases.
Treatment(2) The mainstay of medical management is to reduce vasospasm through Triple H therapy (hypertensive hypervolemic hemodilution) to maintain cerebral perfusion, and nimodipine, a calcium channel blocker
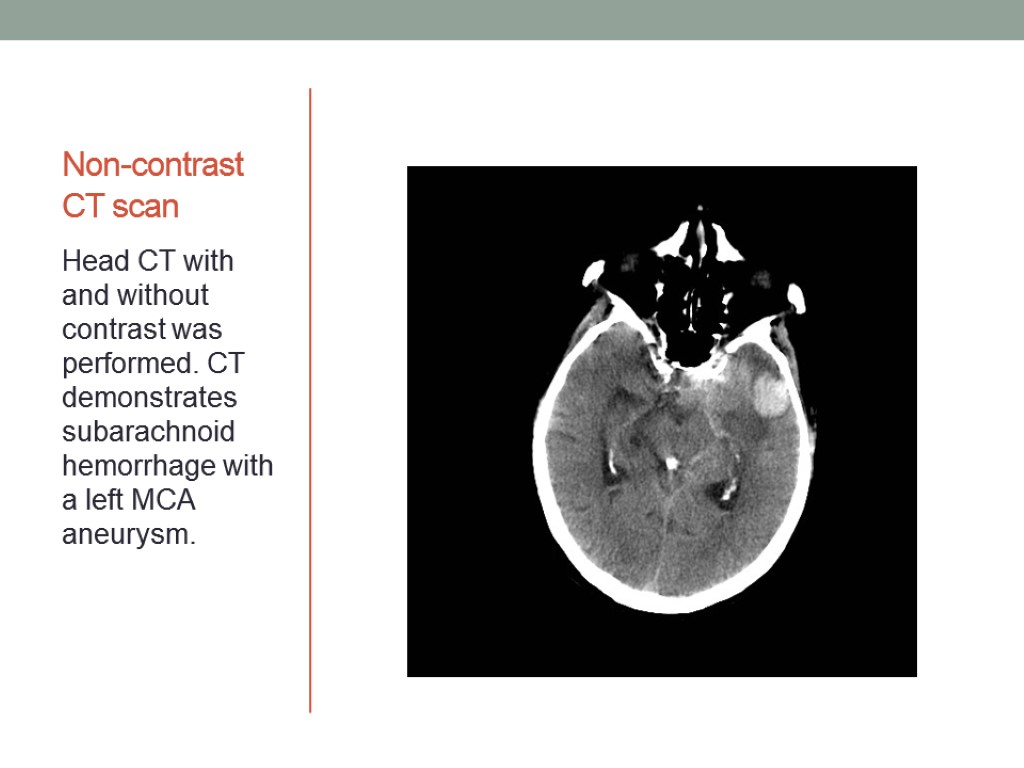
Non-contrast CT scan Head CT with and without contrast was performed. CT demonstrates subarachnoid hemorrhage with a left MCA aneurysm.
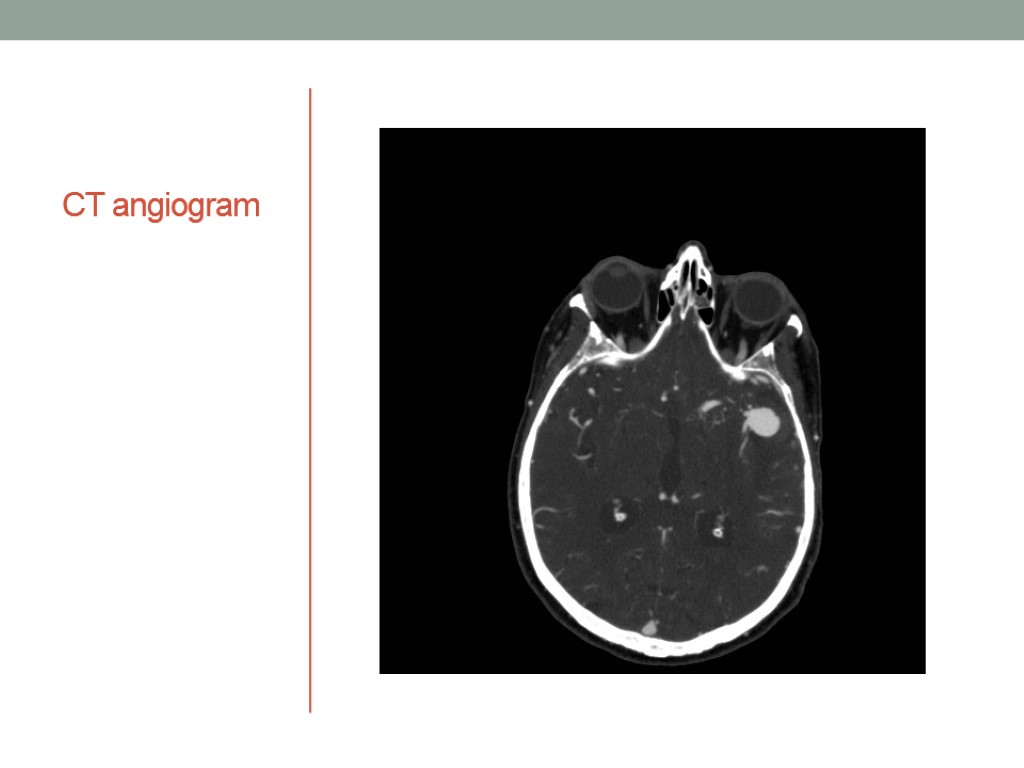
CT angiogram

3D RTA reformat
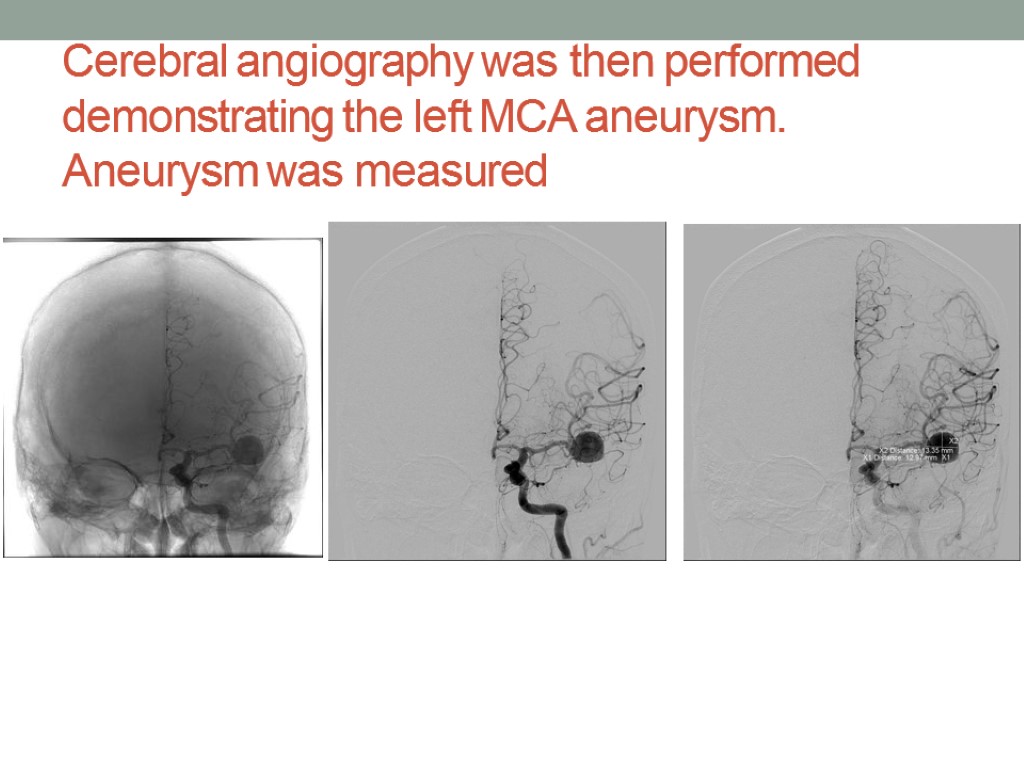
Cerebral angiography was then performed demonstrating the left MCA aneurysm. Aneurysm was measured

A microcatheter was advanced into the aneurysm and coils deployed Post procedure images demonstrates occlusion of the aneurysm.
In conclusion To sum up , I should say ,that it is very important to pay attention to screening programs ,which could probably reduce the cases of spontaneously ruptured aneurysms
References 1. Nahm AM, Henriquez DE, Ritz E. Renal cystic disease (ADPKD and ARPKD). Nephrol. Dial. Transplant. 2002;17 (2): 311-4. doi:10.1093/ndt/17.2.311 - Pubmed citation 2. Konen E, Merchant N, Provost Y et-al. Coarctation of the aorta before and after correction: the role of cardiovascular MRI. AJR Am J Roentgenol. 2004;182 (5): 1333-9. AJR Am J Roentgenol (full text) - Pubmed citation 3. Wardlaw JM, White PM. The detection and management of unruptured intracranial aneurysms. Brain. 2000;123 ( Pt 2) : 205-21. Brain (link) - Pubmed citation 4. Takahashi S. Neurovascular Imaging, MRI & Microangiography. Springer Verlag. (2010) ISBN:1848821336. Read it at Google Books - Find it at Amazon 5. Wiebers DO, Whisnant JP, Huston J et-al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362 (9378): 103-10. Lancet (link) - Pubmed citation 6. Cieściński J, Serafin Z, Strześniewski P et-al. DSA volumetric 3D reconstructions of intracranial aneurysms: A pictorial essay. Pol J Radiol. 2012;77 (2): 47-53. Free text at pubmed - Pubmed citation 7. Rouchaud A, Brandt MD, Rydberg AM et-al. Prevalence of Intracranial Aneurysms in Patients with Aortic Aneurysms. AJNR Am J Neuroradiol. doi:10.3174/ajnr.A4827 - Pubmed citation 8. Toy Simpson Pleitez Rosenfield Tintner Cases of neurology
THANKS FOR YOUR ATTENTION!
aneurysm_present.ppt
- Количество слайдов: 32

