ccc74ee6d4fc907d53ac3ab988481b47.ppt
- Количество слайдов: 42
 YOUR VOICE 4: “Collecting and Using Patient Demographic Data to Create Equitable Health Care Systems: Perspectives from a Community of Practice” Kathryn Coltin, MPH Cheri Wilson, MA, MHS, CPHQ Catherine West, MS, RN Boris Kalanj, LISW, Moderator Diversity. Rx: 7 th National Conference on Quality Health Care for Culturally Diverse Populations, Baltimore, MD October 20, 2010
YOUR VOICE 4: “Collecting and Using Patient Demographic Data to Create Equitable Health Care Systems: Perspectives from a Community of Practice” Kathryn Coltin, MPH Cheri Wilson, MA, MHS, CPHQ Catherine West, MS, RN Boris Kalanj, LISW, Moderator Diversity. Rx: 7 th National Conference on Quality Health Care for Culturally Diverse Populations, Baltimore, MD October 20, 2010
 Community of Practice (Co. P) #3: Participant Introductions Name Work Setting
Community of Practice (Co. P) #3: Participant Introductions Name Work Setting
 Session Objectives Provide audience members with meaningful, replicable information and best practices related to REAL data collection and use; Outline barriers and best practices that are relevant to a variety of health care organizations (hospitals, clinics, health plans, etc. ) at varying points on the continuum of implementation; Discuss larger regulatory and HIT-related developments that impact this area of work; Problem solve with audience members; and Highlight key benefits/outcomes of the Co. P.
Session Objectives Provide audience members with meaningful, replicable information and best practices related to REAL data collection and use; Outline barriers and best practices that are relevant to a variety of health care organizations (hospitals, clinics, health plans, etc. ) at varying points on the continuum of implementation; Discuss larger regulatory and HIT-related developments that impact this area of work; Problem solve with audience members; and Highlight key benefits/outcomes of the Co. P.
 Goals of a Co. P To create an informative and supportive environment for people to learn more about the topic, share their expertise, get advice, and create a base of knowledge that will benefit others.
Goals of a Co. P To create an informative and supportive environment for people to learn more about the topic, share their expertise, get advice, and create a base of knowledge that will benefit others.
 What is a Co. P? A small group (12 -20 participants) of professional colleagues ‘Meet’ monthly on a specific topic Via teleconference or virtual learning platforms Purpose: to discuss common practice challenges and share information about strategies and resources. Supported by a listserv for ongoing dialogue between meetings and a wiki where the information base developed over the course of the project is documented for use by others. Initial meeting period is 12 months—groups may continue to meet as interest and funding permit. Co. P expectations—attendance, participation, contribution
What is a Co. P? A small group (12 -20 participants) of professional colleagues ‘Meet’ monthly on a specific topic Via teleconference or virtual learning platforms Purpose: to discuss common practice challenges and share information about strategies and resources. Supported by a listserv for ongoing dialogue between meetings and a wiki where the information base developed over the course of the project is documented for use by others. Initial meeting period is 12 months—groups may continue to meet as interest and funding permit. Co. P expectations—attendance, participation, contribution
 Why Focus on REAL Data? Minorities tend to receive a lower quality of healthcare than non-minorities. For LEP patients: increased medical errors, poorer follow-up and adherence to clinical instructions and poorer patient provider communication Race, ethnicity, and language data collected is often inadequate and not available for quality improvement Regulatory standards and HIT requirements
Why Focus on REAL Data? Minorities tend to receive a lower quality of healthcare than non-minorities. For LEP patients: increased medical errors, poorer follow-up and adherence to clinical instructions and poorer patient provider communication Race, ethnicity, and language data collected is often inadequate and not available for quality improvement Regulatory standards and HIT requirements
 Regulatory Standards and Healthcare IT Title VI of the Civil Rights Act of 1964 CLAS Standards (2001) The Joint Commission Standards (effective 1/1/2011) NCQA Multicultural Health Standards (effective 7/1/2010) Meaningful Use of Electronic Health Records (EHRs) (effective 1/1/2011) Healthcare Reform American Recovery and Reinvestment Act (ARRA) (2009) Patient Protection and Affordable Care Act (2010)
Regulatory Standards and Healthcare IT Title VI of the Civil Rights Act of 1964 CLAS Standards (2001) The Joint Commission Standards (effective 1/1/2011) NCQA Multicultural Health Standards (effective 7/1/2010) Meaningful Use of Electronic Health Records (EHRs) (effective 1/1/2011) Healthcare Reform American Recovery and Reinvestment Act (ARRA) (2009) Patient Protection and Affordable Care Act (2010)
 What Were Our Goals? 1. 2. 3. 4. 5. 6. 7. Consensus on standardized data collection methods Best practices that ultimately improve the health of our communities (improved data collection and validity, strategies to address disparities) Peer support and networking Support in encouraging government entities to standardize (and support) data collection and use Discussion of technical challenges of collecting granular data Sharing outcomes of Co. P with national/international audience An analysis of the ROI of conducting this work
What Were Our Goals? 1. 2. 3. 4. 5. 6. 7. Consensus on standardized data collection methods Best practices that ultimately improve the health of our communities (improved data collection and validity, strategies to address disparities) Peer support and networking Support in encouraging government entities to standardize (and support) data collection and use Discussion of technical challenges of collecting granular data Sharing outcomes of Co. P with national/international audience An analysis of the ROI of conducting this work
 Co. P Topics/Speakers Erin Bowman, California Health Care Safety Net Institute and Its REAL Data Efforts Dr. David Nerenz, Chair, IOM Subcommittee on Standardized Collection of Race/Ethnicity Data for Healthcare Quality Improvement Nuts and Bolts of REAL Data Collection Disparities Solutions Center, (Massachusetts General) Creating Equity Reports National Association of Public Hospitals and Health Systems, Assuring Healthcare Equity HRET Toolkit
Co. P Topics/Speakers Erin Bowman, California Health Care Safety Net Institute and Its REAL Data Efforts Dr. David Nerenz, Chair, IOM Subcommittee on Standardized Collection of Race/Ethnicity Data for Healthcare Quality Improvement Nuts and Bolts of REAL Data Collection Disparities Solutions Center, (Massachusetts General) Creating Equity Reports National Association of Public Hospitals and Health Systems, Assuring Healthcare Equity HRET Toolkit
 Topics Covered during the Co. P Dr. Geniene Wilson, New Tools for Eliminating Health Disparities: Collecting Demographic Data in an Electronic Health Record (Institute for Family Health) Dr. Barrie Baker, Collecting Member Race/Ethnicity (Keystone Mercy Health System) Kathryn Coltin, Harvard Pilgrim’s Equity Report: An Evolving Initiative Cheri Wilson, REAL Data Quality Issues (Johns Hopkins Hospital) Maria Moreno, Collecting REAL Data and EPIC Upgrade (Sutter Health Institute for Research and Education) EPIC Vendor and Standardization
Topics Covered during the Co. P Dr. Geniene Wilson, New Tools for Eliminating Health Disparities: Collecting Demographic Data in an Electronic Health Record (Institute for Family Health) Dr. Barrie Baker, Collecting Member Race/Ethnicity (Keystone Mercy Health System) Kathryn Coltin, Harvard Pilgrim’s Equity Report: An Evolving Initiative Cheri Wilson, REAL Data Quality Issues (Johns Hopkins Hospital) Maria Moreno, Collecting REAL Data and EPIC Upgrade (Sutter Health Institute for Research and Education) EPIC Vendor and Standardization
 Community of Practice (Co. P) #3 Participants Why applied to participate in the Co. P? What we each brought to the Co. P?
Community of Practice (Co. P) #3 Participants Why applied to participate in the Co. P? What we each brought to the Co. P?
 The Johns Hopkins Hospital (JHH): REAL Data Quality Issues Cheri Wilson, MA, MHS, CPHQ Faculty Research Associate Program Director, Culture-Quality. Collaborative (CQC)
The Johns Hopkins Hospital (JHH): REAL Data Quality Issues Cheri Wilson, MA, MHS, CPHQ Faculty Research Associate Program Director, Culture-Quality. Collaborative (CQC)
 Outline About JHH Project background Data quality issues Recommendations
Outline About JHH Project background Data quality issues Recommendations
 About JHH founded in 1889 1, 085 licensed patient beds 46, 775 inpatient admissions 421, 933 outpatient encounters 1, 714 full-time attending physicians 9, 294 employees
About JHH founded in 1889 1, 085 licensed patient beds 46, 775 inpatient admissions 421, 933 outpatient encounters 1, 714 full-time attending physicians 9, 294 employees
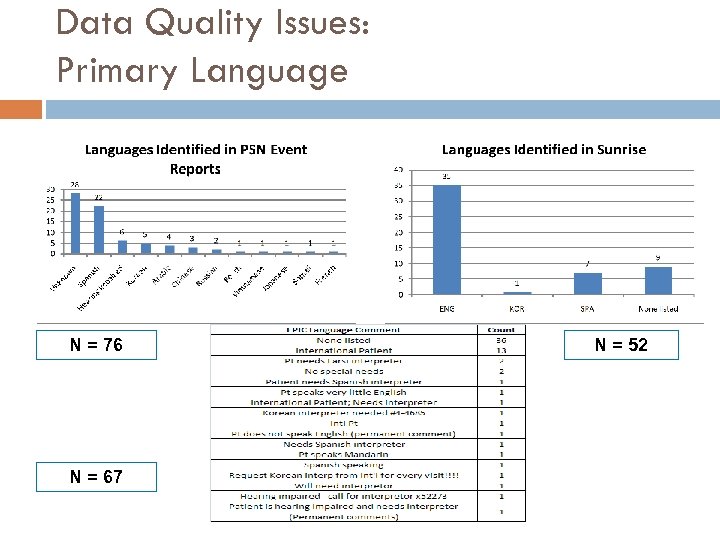 Data Quality Issues: Primary Language N = 76 N = 67 N = 52
Data Quality Issues: Primary Language N = 76 N = 67 N = 52
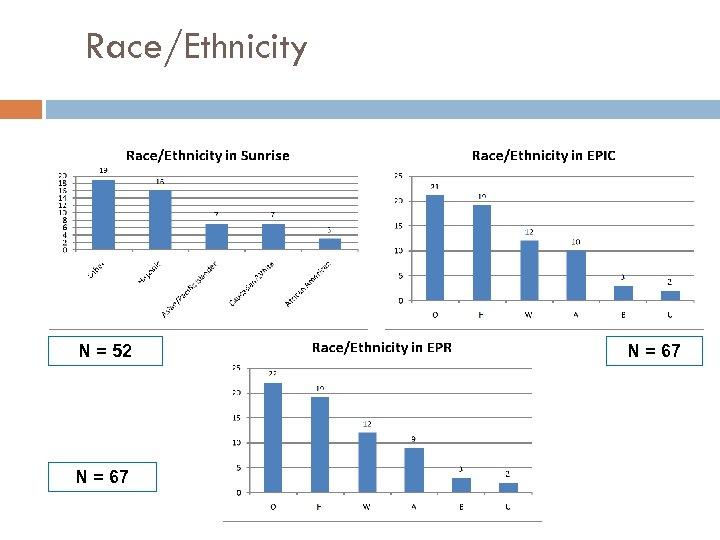 Race/Ethnicity N = 52 N = 67
Race/Ethnicity N = 52 N = 67
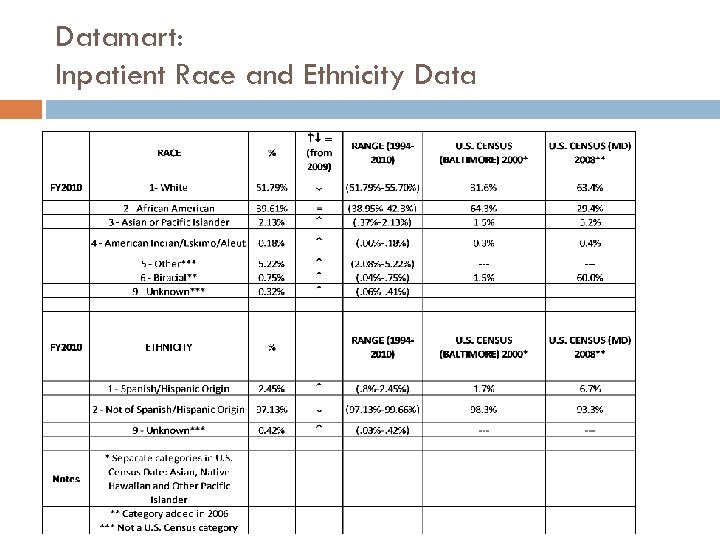 Datamart: Inpatient Race and Ethnicity Data
Datamart: Inpatient Race and Ethnicity Data
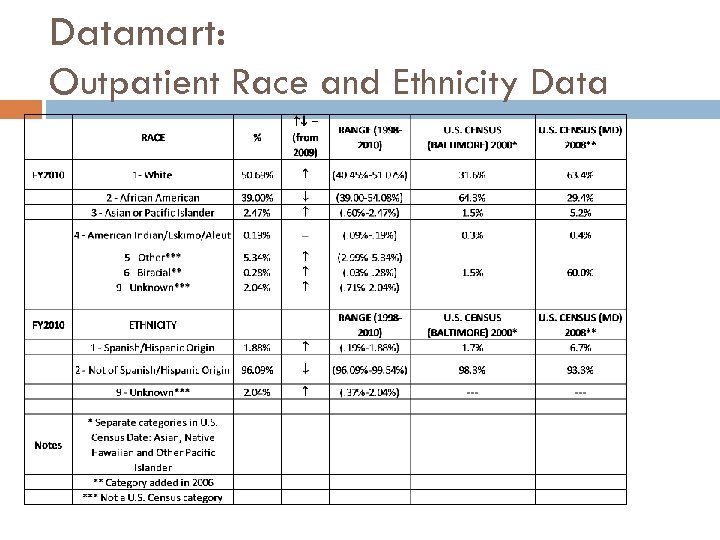 Datamart: Outpatient Race and Ethnicity Data
Datamart: Outpatient Race and Ethnicity Data
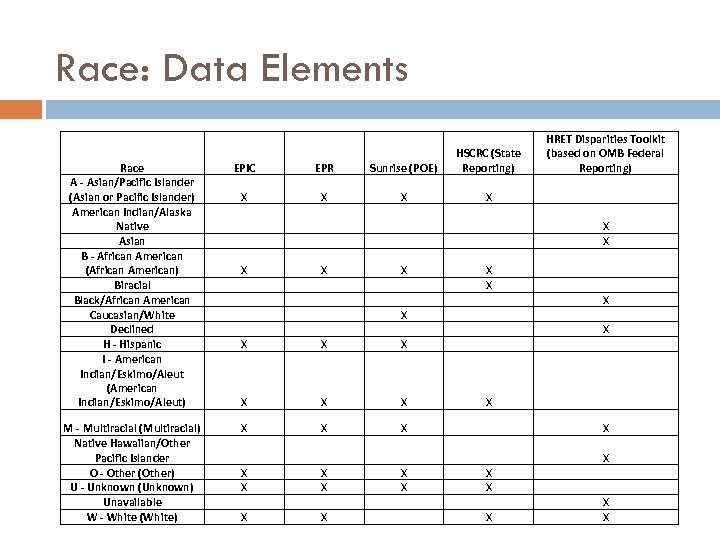 Race: Data Elements Race A - Asian/Pacific Islander (Asian or Pacific Islander) American Indian/Alaska Native Asian B - African American (African American) Biracial Black/African American Caucasian/White Declined H - Hispanic I - American Indian/Eskimo/Aleut (American Indian/Eskimo/Aleut) M - Multiracial (Multiracial) Native Hawaiian/Other Pacific Islander O - Other (Other) U - Unknown (Unknown) Unavailable W - White (White) EPIC EPR Sunrise (POE) HSCRC (State Reporting) HRET Disparities Toolkit (based on OMB Federal Reporting) X X X X X X X X X X X X X X
Race: Data Elements Race A - Asian/Pacific Islander (Asian or Pacific Islander) American Indian/Alaska Native Asian B - African American (African American) Biracial Black/African American Caucasian/White Declined H - Hispanic I - American Indian/Eskimo/Aleut (American Indian/Eskimo/Aleut) M - Multiracial (Multiracial) Native Hawaiian/Other Pacific Islander O - Other (Other) U - Unknown (Unknown) Unavailable W - White (White) EPIC EPR Sunrise (POE) HSCRC (State Reporting) HRET Disparities Toolkit (based on OMB Federal Reporting) X X X X X X X X X X X X X X
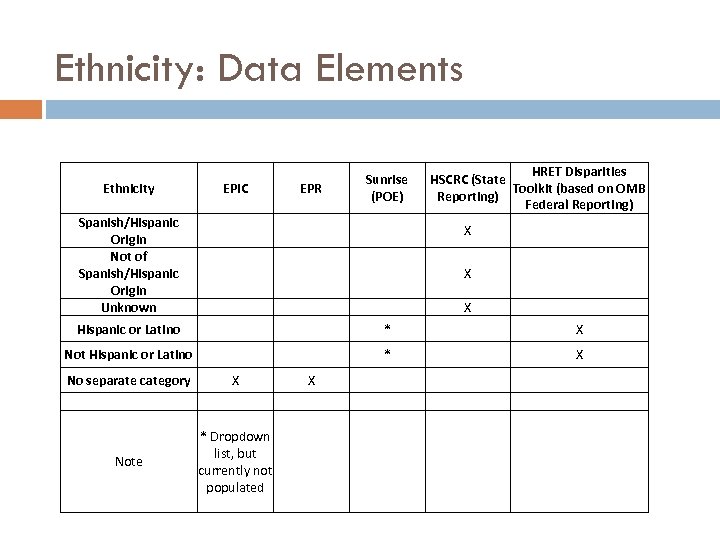 Ethnicity: Data Elements HRET Disparities HSCRC (State Toolkit (based on OMB Reporting) Federal Reporting) EPIC EPR Sunrise (POE) X X Hispanic or Latino * X Not Hispanic or Latino * X No separate category X X Note * Dropdown list, but currently not populated Ethnicity Spanish/Hispanic Origin Not of Spanish/Hispanic Origin Unknown
Ethnicity: Data Elements HRET Disparities HSCRC (State Toolkit (based on OMB Reporting) Federal Reporting) EPIC EPR Sunrise (POE) X X Hispanic or Latino * X Not Hispanic or Latino * X No separate category X X Note * Dropdown list, but currently not populated Ethnicity Spanish/Hispanic Origin Not of Spanish/Hispanic Origin Unknown
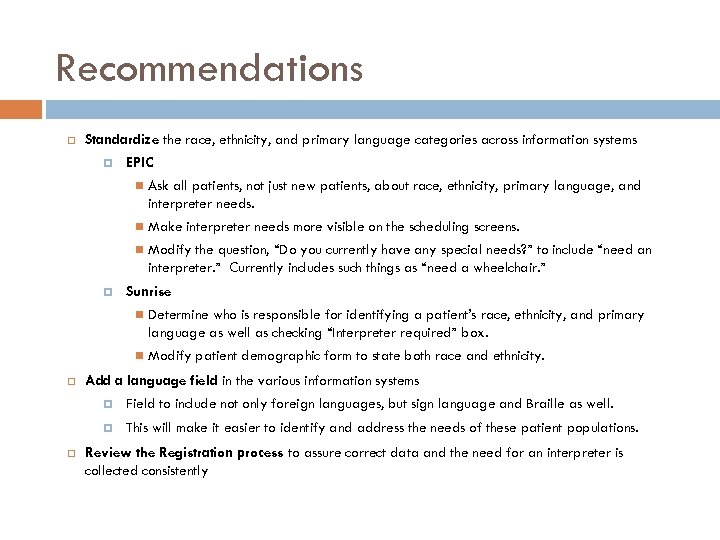 Recommendations Standardize the race, ethnicity, and primary language categories across information systems EPIC Make interpreter needs more visible on the scheduling screens. Ask all patients, not just new patients, about race, ethnicity, primary language, and interpreter needs. Modify the question, “Do you currently have any special needs? ” to include “need an interpreter. ” Currently includes such things as “need a wheelchair. ” Sunrise Determine who is responsible for identifying a patient’s race, ethnicity, and primary language as well as checking “Interpreter required” box. Modify patient demographic form to state both race and ethnicity. Add a language field in the various information systems Field to include not only foreign languages, but sign language and Braille as well. This will make it easier to identify and address the needs of these patient populations. Review the Registration process to assure correct data and the need for an interpreter is collected consistently
Recommendations Standardize the race, ethnicity, and primary language categories across information systems EPIC Make interpreter needs more visible on the scheduling screens. Ask all patients, not just new patients, about race, ethnicity, primary language, and interpreter needs. Modify the question, “Do you currently have any special needs? ” to include “need an interpreter. ” Currently includes such things as “need a wheelchair. ” Sunrise Determine who is responsible for identifying a patient’s race, ethnicity, and primary language as well as checking “Interpreter required” box. Modify patient demographic form to state both race and ethnicity. Add a language field in the various information systems Field to include not only foreign languages, but sign language and Braille as well. This will make it easier to identify and address the needs of these patient populations. Review the Registration process to assure correct data and the need for an interpreter is collected consistently
 Collecting, Reporting and Using REa. L Data To Reduce Health Care Disparities Kathryn Coltin Harvard Pilgrim Health Care Diversity Rx Community of Practice 3 October 2010
Collecting, Reporting and Using REa. L Data To Reduce Health Care Disparities Kathryn Coltin Harvard Pilgrim Health Care Diversity Rx Community of Practice 3 October 2010
 Harvard Pilgrim Health Care Background and Context Harvard Pilgrim Health Care is a non-profit health plan serving over 1 million commercially-insured members in MA, ME, NH and RI. Of these, almost 70% reside in Massachusetts In 2004 Harvard Pilgrim became one of ten founding members of the National Health Plan Collaborative to reduce racial & ethnic disparities. This step fueled a steadily growing initiative to measure, report and reduce disparities in the care and service our members receive. Harvard Pilgrim has been ranked the #1 health plan in the U. S. based on quality since 2005*. Even so, disparities exist in the care some of our members receive. The Commonwealth of Massachusetts mandated collection and reporting of patients’ race, ethnicity and language by acute care hospitals in January 2007 and extended this mandate to health plan collection of enrollees’ REa. L data beginning July 2010. $$$ Penalties are tied to non-compliance in achieving specified reporting thresholds. *Based on NCQA’s U. S. News and World Report and Consumer Reports Best U. S. Health Plan Rankings
Harvard Pilgrim Health Care Background and Context Harvard Pilgrim Health Care is a non-profit health plan serving over 1 million commercially-insured members in MA, ME, NH and RI. Of these, almost 70% reside in Massachusetts In 2004 Harvard Pilgrim became one of ten founding members of the National Health Plan Collaborative to reduce racial & ethnic disparities. This step fueled a steadily growing initiative to measure, report and reduce disparities in the care and service our members receive. Harvard Pilgrim has been ranked the #1 health plan in the U. S. based on quality since 2005*. Even so, disparities exist in the care some of our members receive. The Commonwealth of Massachusetts mandated collection and reporting of patients’ race, ethnicity and language by acute care hospitals in January 2007 and extended this mandate to health plan collection of enrollees’ REa. L data beginning July 2010. $$$ Penalties are tied to non-compliance in achieving specified reporting thresholds. *Based on NCQA’s U. S. News and World Report and Consumer Reports Best U. S. Health Plan Rankings
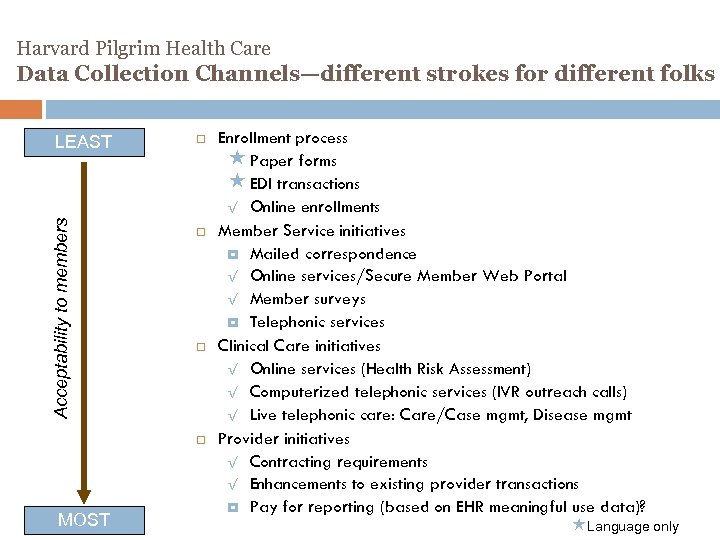 Harvard Pilgrim Health Care Data Collection Channels—different strokes for different folks Acceptability to members LEAST MOST Enrollment process « Paper forms « EDI transactions √ Online enrollments Member Service initiatives Mailed correspondence √ Online services/Secure Member Web Portal √ Member surveys Telephonic services Clinical Care initiatives √ Online services (Health Risk Assessment) √ Computerized telephonic services (IVR outreach calls) √ Live telephonic care: Care/Case mgmt, Disease mgmt Provider initiatives √ Contracting requirements √ Enhancements to existing provider transactions Pay for reporting (based on EHR meaningful use data)? «Language only
Harvard Pilgrim Health Care Data Collection Channels—different strokes for different folks Acceptability to members LEAST MOST Enrollment process « Paper forms « EDI transactions √ Online enrollments Member Service initiatives Mailed correspondence √ Online services/Secure Member Web Portal √ Member surveys Telephonic services Clinical Care initiatives √ Online services (Health Risk Assessment) √ Computerized telephonic services (IVR outreach calls) √ Live telephonic care: Care/Case mgmt, Disease mgmt Provider initiatives √ Contracting requirements √ Enhancements to existing provider transactions Pay for reporting (based on EHR meaningful use data)? «Language only
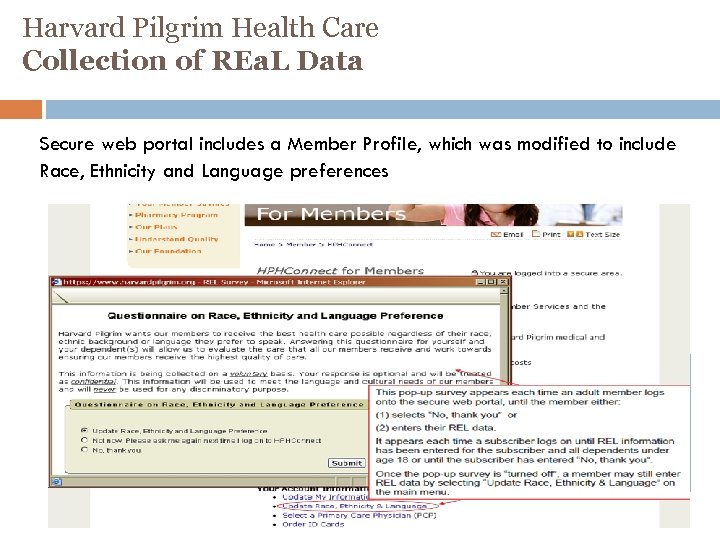 Harvard Pilgrim Health Care Collection of REa. L Data Secure web portal includes a Member Profile, which was modified to include Race, Ethnicity and Language preferences 25
Harvard Pilgrim Health Care Collection of REa. L Data Secure web portal includes a Member Profile, which was modified to include Race, Ethnicity and Language preferences 25
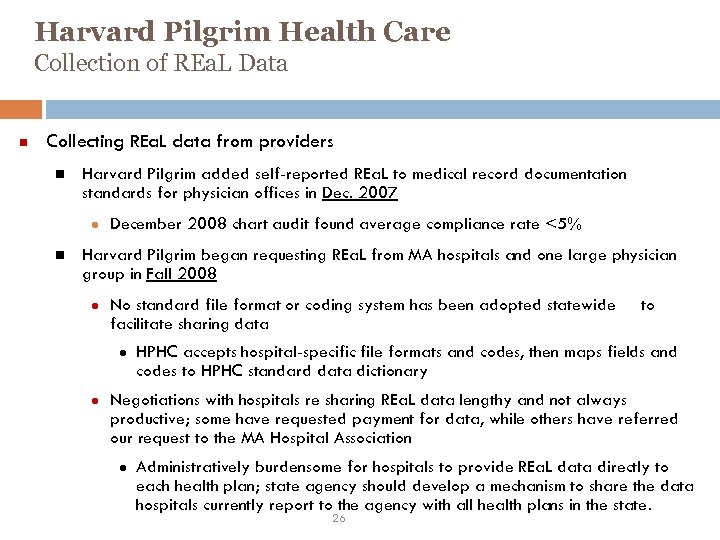 Harvard Pilgrim Health Care Collection of REa. L Data Collecting REa. L data from providers Harvard Pilgrim added self-reported REa. L to medical record documentation standards for physician offices in Dec. 2007 ● December 2008 chart audit found average compliance rate <5% Harvard Pilgrim began requesting REa. L from MA hospitals and one large physician group in Fall 2008 ● No standard file format or coding system has been adopted statewide facilitate sharing data ● ● to HPHC accepts hospital-specific file formats and codes, then maps fields and codes to HPHC standard data dictionary Negotiations with hospitals re sharing REa. L data lengthy and not always productive; some have requested payment for data, while others have referred our request to the MA Hospital Association ● Administratively burdensome for hospitals to provide REa. L data directly to each health plan; state agency should develop a mechanism to share the data hospitals currently report to the agency with all health plans in the state. 26
Harvard Pilgrim Health Care Collection of REa. L Data Collecting REa. L data from providers Harvard Pilgrim added self-reported REa. L to medical record documentation standards for physician offices in Dec. 2007 ● December 2008 chart audit found average compliance rate <5% Harvard Pilgrim began requesting REa. L from MA hospitals and one large physician group in Fall 2008 ● No standard file format or coding system has been adopted statewide facilitate sharing data ● ● to HPHC accepts hospital-specific file formats and codes, then maps fields and codes to HPHC standard data dictionary Negotiations with hospitals re sharing REa. L data lengthy and not always productive; some have requested payment for data, while others have referred our request to the MA Hospital Association ● Administratively burdensome for hospitals to provide REa. L data directly to each health plan; state agency should develop a mechanism to share the data hospitals currently report to the agency with all health plans in the state. 26
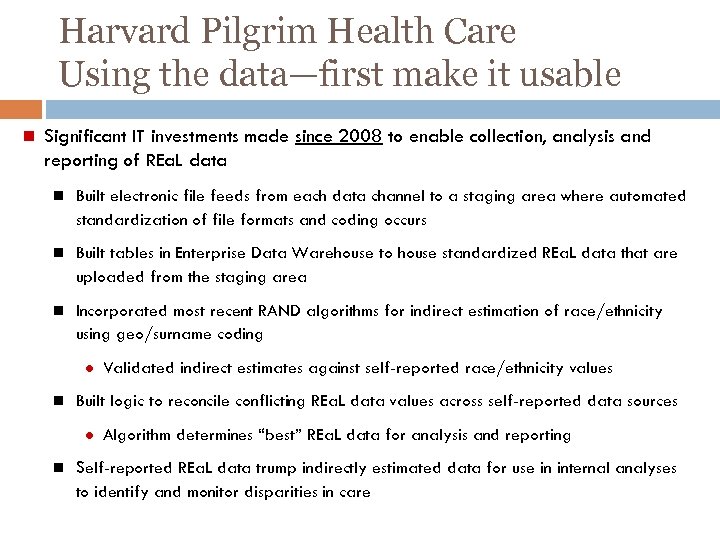 Harvard Pilgrim Health Care Using the data—first make it usable Significant IT investments made since 2008 to enable collection, analysis and reporting of REa. L data Built electronic file feeds from each data channel to a staging area where automated standardization of file formats and coding occurs Built tables in Enterprise Data Warehouse to house standardized REa. L data that are uploaded from the staging area Incorporated most recent RAND algorithms for indirect estimation of race/ethnicity using geo/surname coding ● Validated indirect estimates against self-reported race/ethnicity values Built logic to reconcile conflicting REa. L data values across self-reported data sources ● Algorithm determines “best” REa. L data for analysis and reporting Self-reported REa. L data trump indirectly estimated data for use in internal analyses to identify and monitor disparities in care
Harvard Pilgrim Health Care Using the data—first make it usable Significant IT investments made since 2008 to enable collection, analysis and reporting of REa. L data Built electronic file feeds from each data channel to a staging area where automated standardization of file formats and coding occurs Built tables in Enterprise Data Warehouse to house standardized REa. L data that are uploaded from the staging area Incorporated most recent RAND algorithms for indirect estimation of race/ethnicity using geo/surname coding ● Validated indirect estimates against self-reported race/ethnicity values Built logic to reconcile conflicting REa. L data values across self-reported data sources ● Algorithm determines “best” REa. L data for analysis and reporting Self-reported REa. L data trump indirectly estimated data for use in internal analyses to identify and monitor disparities in care
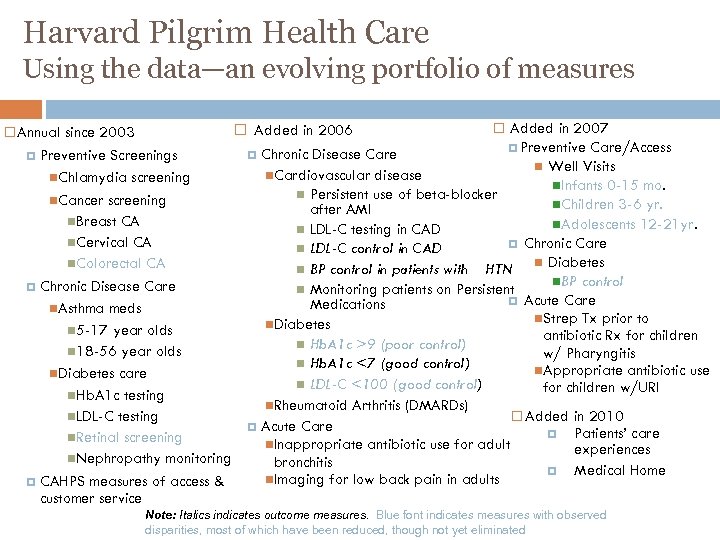 Harvard Pilgrim Health Care Using the data—an evolving portfolio of measures Added in 2006 Annual since 2003 Preventive Screenings Chlamydia screening Cancer screening Breast CA Cervical CA Colorectal CA Chronic Disease Care Asthma meds 5 -17 year olds 18 -56 year olds Diabetes care Hb. A 1 c testing LDL-C testing Retinal screening Nephropathy monitoring CAHPS measures of access & customer service Added in 2007 Preventive Care/Access Chronic Disease Care Well Visits Cardiovascular disease Infants 0 -15 mo. Persistent use of beta-blocker Children 3 -6 yr. after AMI Adolescents 12 -21 yr. LDL-C testing in CAD Chronic Care LDL-C control in CAD Diabetes BP control in patients with HTN BP control Monitoring patients on Persistent Acute Care Medications Strep Tx prior to Diabetes antibiotic Rx for children Hb. A 1 c >9 (poor control) w/ Pharyngitis Hb. A 1 c <7 (good control) Appropriate antibiotic use LDL-C <100 (good control) for children w/URI Rheumatoid Arthritis (DMARDs) Added in 2010 Acute Care Patients’ care Inappropriate antibiotic use for adult experiences bronchitis Medical Home Imaging for low back pain in adults Note: Italics indicates outcome measures. Blue font indicates measures with observed disparities, most of which have been reduced, though not yet eliminated
Harvard Pilgrim Health Care Using the data—an evolving portfolio of measures Added in 2006 Annual since 2003 Preventive Screenings Chlamydia screening Cancer screening Breast CA Cervical CA Colorectal CA Chronic Disease Care Asthma meds 5 -17 year olds 18 -56 year olds Diabetes care Hb. A 1 c testing LDL-C testing Retinal screening Nephropathy monitoring CAHPS measures of access & customer service Added in 2007 Preventive Care/Access Chronic Disease Care Well Visits Cardiovascular disease Infants 0 -15 mo. Persistent use of beta-blocker Children 3 -6 yr. after AMI Adolescents 12 -21 yr. LDL-C testing in CAD Chronic Care LDL-C control in CAD Diabetes BP control in patients with HTN BP control Monitoring patients on Persistent Acute Care Medications Strep Tx prior to Diabetes antibiotic Rx for children Hb. A 1 c >9 (poor control) w/ Pharyngitis Hb. A 1 c <7 (good control) Appropriate antibiotic use LDL-C <100 (good control) for children w/URI Rheumatoid Arthritis (DMARDs) Added in 2010 Acute Care Patients’ care Inappropriate antibiotic use for adult experiences bronchitis Medical Home Imaging for low back pain in adults Note: Italics indicates outcome measures. Blue font indicates measures with observed disparities, most of which have been reduced, though not yet eliminated
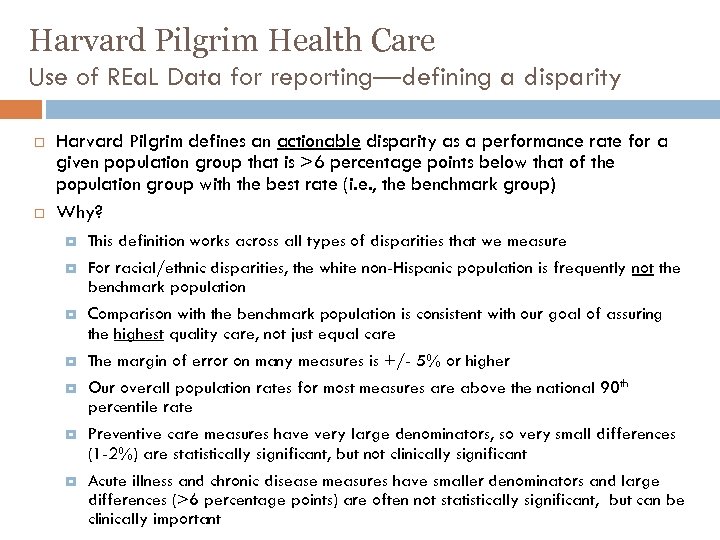 Harvard Pilgrim Health Care Use of REa. L Data for reporting—defining a disparity Harvard Pilgrim defines an actionable disparity as a performance rate for a given population group that is >6 percentage points below that of the population group with the best rate (i. e. , the benchmark group) Why? This definition works across all types of disparities that we measure For racial/ethnic disparities, the white non-Hispanic population is frequently not the benchmark population Comparison with the benchmark population is consistent with our goal of assuring the highest quality care, not just equal care The margin of error on many measures is +/- 5% or higher Our overall population rates for most measures are above the national 90 th percentile rate Preventive care measures have very large denominators, so very small differences (1 -2%) are statistically significant, but not clinically significant Acute illness and chronic disease measures have smaller denominators and large differences (>6 percentage points) are often not statistically significant, but can be clinically important
Harvard Pilgrim Health Care Use of REa. L Data for reporting—defining a disparity Harvard Pilgrim defines an actionable disparity as a performance rate for a given population group that is >6 percentage points below that of the population group with the best rate (i. e. , the benchmark group) Why? This definition works across all types of disparities that we measure For racial/ethnic disparities, the white non-Hispanic population is frequently not the benchmark population Comparison with the benchmark population is consistent with our goal of assuring the highest quality care, not just equal care The margin of error on many measures is +/- 5% or higher Our overall population rates for most measures are above the national 90 th percentile rate Preventive care measures have very large denominators, so very small differences (1 -2%) are statistically significant, but not clinically significant Acute illness and chronic disease measures have smaller denominators and large differences (>6 percentage points) are often not statistically significant, but can be clinically important
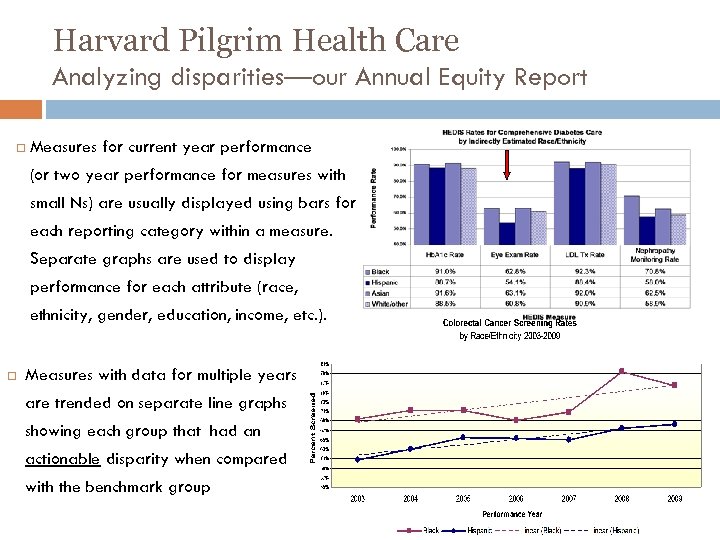 Harvard Pilgrim Health Care Analyzing disparities—our Annual Equity Report Measures for current year performance (or two year performance for measures with small Ns) are usually displayed using bars for each reporting category within a measure. Separate graphs are used to display performance for each attribute (race, ethnicity, gender, education, income, etc. ). Measures with data for multiple years are trended on separate line graphs showing each group that had an actionable disparity when compared with the benchmark group
Harvard Pilgrim Health Care Analyzing disparities—our Annual Equity Report Measures for current year performance (or two year performance for measures with small Ns) are usually displayed using bars for each reporting category within a measure. Separate graphs are used to display performance for each attribute (race, ethnicity, gender, education, income, etc. ). Measures with data for multiple years are trended on separate line graphs showing each group that had an actionable disparity when compared with the benchmark group
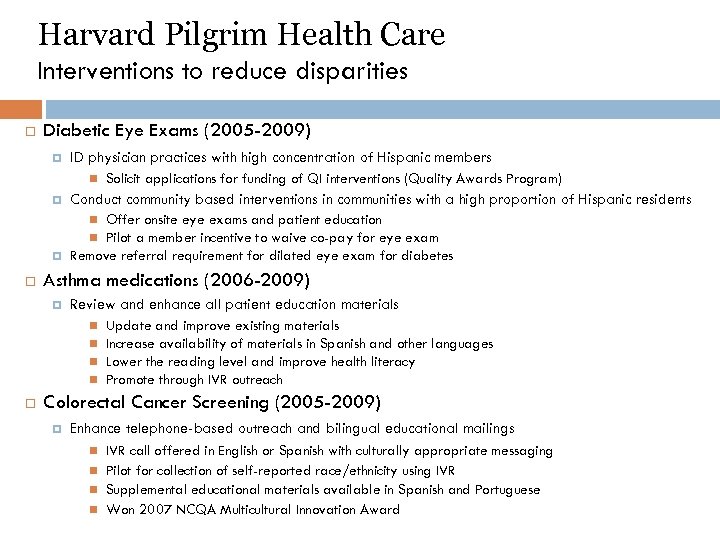 Harvard Pilgrim Health Care Interventions to reduce disparities Diabetic Eye Exams (2005 -2009) ID physician practices with high concentration of Hispanic members Solicit applications for funding of QI interventions (Quality Awards Program) Conduct community based interventions in communities with a high proportion of Hispanic residents Offer onsite eye exams and patient education Pilot a member incentive to waive co-pay for eye exam Remove referral requirement for dilated eye exam for diabetes Asthma medications (2006 -2009) Review and enhance all patient education materials Update and improve existing materials Increase availability of materials in Spanish and other languages Lower the reading level and improve health literacy Promote through IVR outreach Colorectal Cancer Screening (2005 -2009) Enhance telephone-based outreach and bilingual educational mailings IVR call offered in English or Spanish with culturally appropriate messaging Pilot for collection of self-reported race/ethnicity using IVR Supplemental educational materials available in Spanish and Portuguese Won 2007 NCQA Multicultural Innovation Award
Harvard Pilgrim Health Care Interventions to reduce disparities Diabetic Eye Exams (2005 -2009) ID physician practices with high concentration of Hispanic members Solicit applications for funding of QI interventions (Quality Awards Program) Conduct community based interventions in communities with a high proportion of Hispanic residents Offer onsite eye exams and patient education Pilot a member incentive to waive co-pay for eye exam Remove referral requirement for dilated eye exam for diabetes Asthma medications (2006 -2009) Review and enhance all patient education materials Update and improve existing materials Increase availability of materials in Spanish and other languages Lower the reading level and improve health literacy Promote through IVR outreach Colorectal Cancer Screening (2005 -2009) Enhance telephone-based outreach and bilingual educational mailings IVR call offered in English or Spanish with culturally appropriate messaging Pilot for collection of self-reported race/ethnicity using IVR Supplemental educational materials available in Spanish and Portuguese Won 2007 NCQA Multicultural Innovation Award
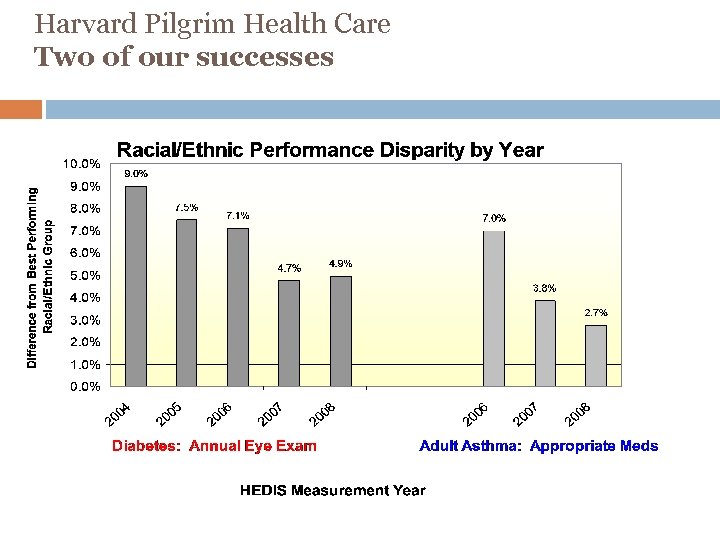 Harvard Pilgrim Health Care Two of our successes
Harvard Pilgrim Health Care Two of our successes
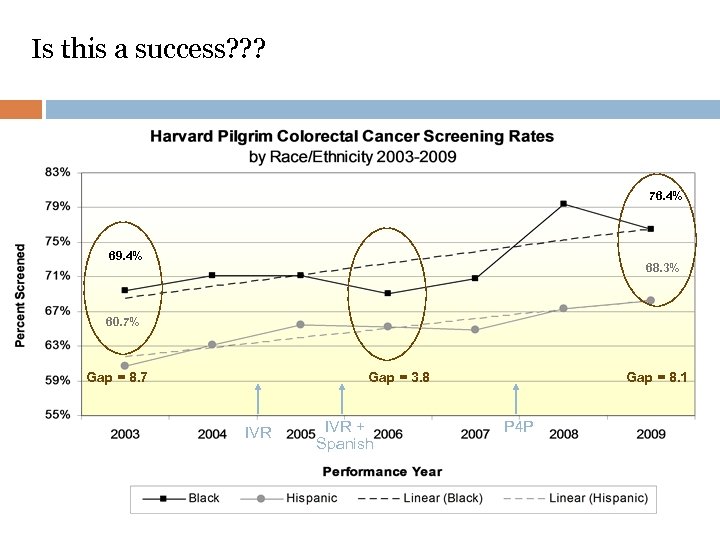 Is this a success? ? ? 76. 4% 69. 4% 68. 3% 60. 7% Gap = 8. 7 Gap = 3. 8 IVR + Spanish Gap = 8. 1 P 4 P
Is this a success? ? ? 76. 4% 69. 4% 68. 3% 60. 7% Gap = 8. 7 Gap = 3. 8 IVR + Spanish Gap = 8. 1 P 4 P
 Aligning Forces for Quality Using Stratified Data for Quality Improvement: Examples from Speaking Together National Language Services Network Catherine West, MS, RN October 20, 2010 34
Aligning Forces for Quality Using Stratified Data for Quality Improvement: Examples from Speaking Together National Language Services Network Catherine West, MS, RN October 20, 2010 34
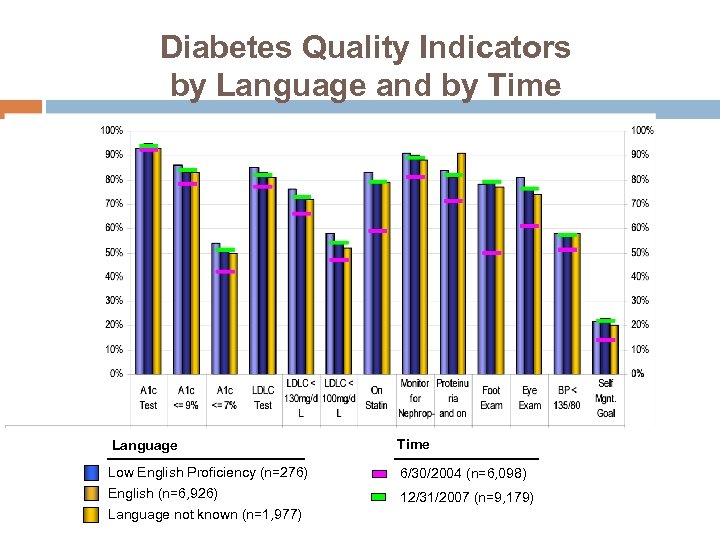 Diabetes Quality Indicators by Language and by Time Language Time Low English Proficiency (n=276) English (n=6, 926) 6/30/2004 (n=6, 098) Language not known (n=1, 977) 12/31/2007 (n=9, 179)
Diabetes Quality Indicators by Language and by Time Language Time Low English Proficiency (n=276) English (n=6, 926) 6/30/2004 (n=6, 098) Language not known (n=1, 977) 12/31/2007 (n=9, 179)
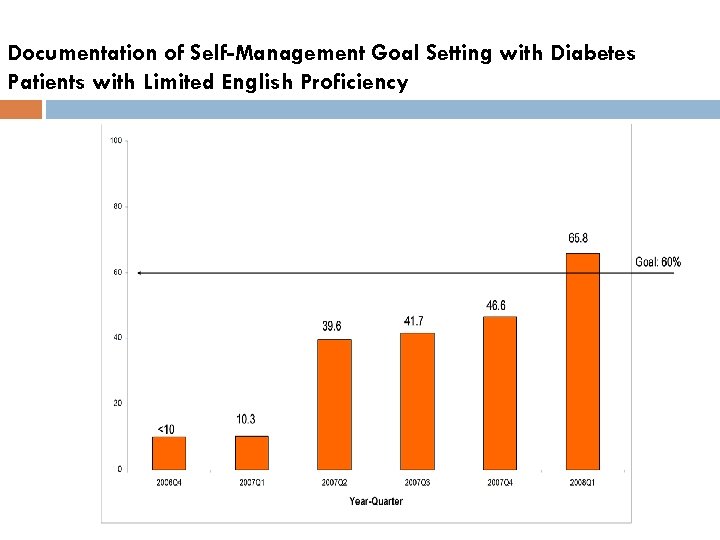 Documentation of Self-Management Goal Setting with Diabetes Patients with Limited English Proficiency
Documentation of Self-Management Goal Setting with Diabetes Patients with Limited English Proficiency
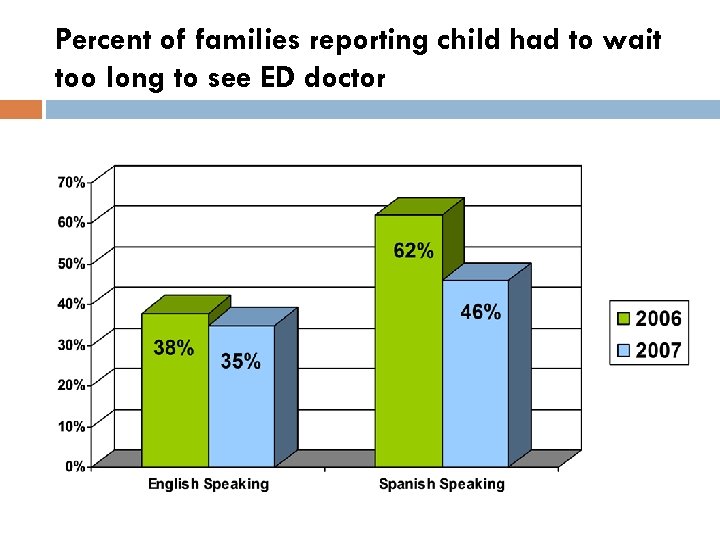 Percent of families reporting child had to wait too long to see ED doctor
Percent of families reporting child had to wait too long to see ED doctor
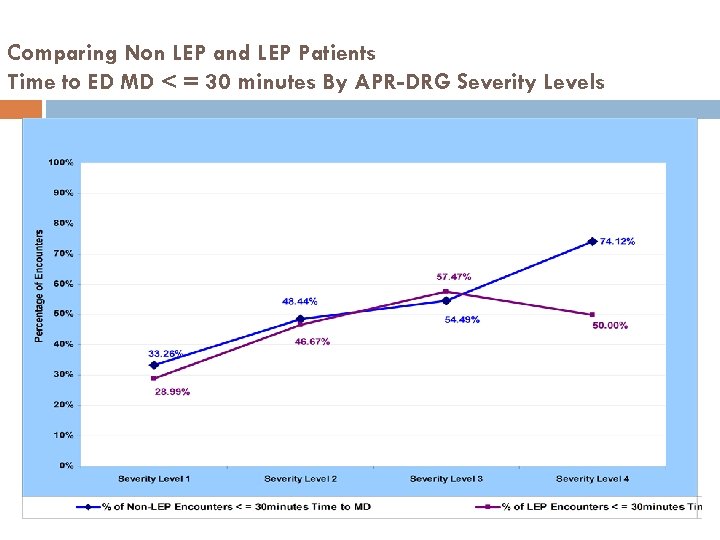 Comparing Non LEP and LEP Patients Time to ED MD < = 30 minutes By APR-DRG Severity Levels
Comparing Non LEP and LEP Patients Time to ED MD < = 30 minutes By APR-DRG Severity Levels
 Questions and Discussion
Questions and Discussion
 Small Group Discussion Each group please assign a scribe to capture themes discussed. Discuss: What have been your experiences in collecting and utilizing REa. L data? What successes have you had? Any strategies/resources you employed to get to these successes? What have been the challenges? What would you like to achieve in your organizations in the next 2 years?
Small Group Discussion Each group please assign a scribe to capture themes discussed. Discuss: What have been your experiences in collecting and utilizing REa. L data? What successes have you had? Any strategies/resources you employed to get to these successes? What have been the challenges? What would you like to achieve in your organizations in the next 2 years?
 Top 3 Issues from Small Groups
Top 3 Issues from Small Groups


