0461a4455812f7125adfdf12c6fba79f.ppt
- Количество слайдов: 74
 Wound Healing and Suture Knowledge ASR Certification Prep Kim Bayer, SRS, BS, CVT, LATg
Wound Healing and Suture Knowledge ASR Certification Prep Kim Bayer, SRS, BS, CVT, LATg
 Tissue Handling / Technique Goal is to minimize trauma ¬ Gentle use minimal tension with tissue Retractors should be placed to avoid excessive tension ¬ Proper use of instruments DO NOT CRUSH ¬ Use Proper Technique ¬ Keep Tissue Moist Dry tissue is dead tissue ¬ Minimize Time
Tissue Handling / Technique Goal is to minimize trauma ¬ Gentle use minimal tension with tissue Retractors should be placed to avoid excessive tension ¬ Proper use of instruments DO NOT CRUSH ¬ Use Proper Technique ¬ Keep Tissue Moist Dry tissue is dead tissue ¬ Minimize Time
 Incisions n Heal side-to-side, not end-to-end – There is little advantage to making an incision too small to easily view the surgical site
Incisions n Heal side-to-side, not end-to-end – There is little advantage to making an incision too small to easily view the surgical site
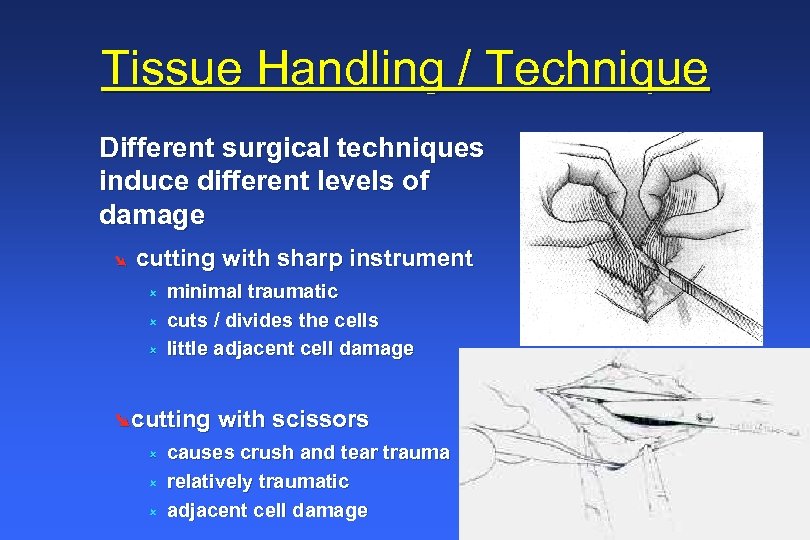 Tissue Handling / Technique Different surgical techniques induce different levels of damage Ø cutting with sharp instrument û û û minimal traumatic cuts / divides the cells little adjacent cell damage Øcutting with scissors û û û causes crush and tear trauma relatively traumatic adjacent cell damage
Tissue Handling / Technique Different surgical techniques induce different levels of damage Ø cutting with sharp instrument û û û minimal traumatic cuts / divides the cells little adjacent cell damage Øcutting with scissors û û û causes crush and tear trauma relatively traumatic adjacent cell damage
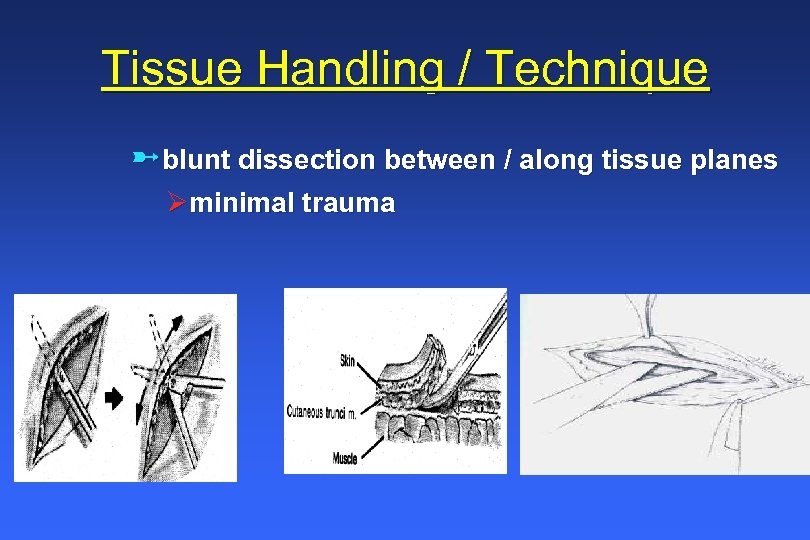 Tissue Handling / Technique üblunt dissection between / along tissue planes Øminimal trauma
Tissue Handling / Technique üblunt dissection between / along tissue planes Øminimal trauma
 Tissue Handling / Technique clamping tissue with hemostats / etc. û causes crushing of the cells û very traumatic û causes release of vasoconstrictors, clotting factors û proper for clamping vessels for ligation / hemostasis
Tissue Handling / Technique clamping tissue with hemostats / etc. û causes crushing of the cells û very traumatic û causes release of vasoconstrictors, clotting factors û proper for clamping vessels for ligation / hemostasis
 Tissue Handling / Technique provide gentle retraction with proper instruments
Tissue Handling / Technique provide gentle retraction with proper instruments
 Tissue Handling / Technique Keep Tissue Moist “The solution to pollution is dilution” þIrrigate, rinse the incision surgery site þLavage, irrigate body cavities
Tissue Handling / Technique Keep Tissue Moist “The solution to pollution is dilution” þIrrigate, rinse the incision surgery site þLavage, irrigate body cavities
 Hemostasis n Bleeding should be stopped whenever possible – Excessive bleeding may cause hematomas or increase dead space – Hematomas prevent wound apposition and retard healing – Blood is a natural food for micro-organisms and a large clot will help protect them from the body’s immune system » Bacteria inside the clot will be protected n Bleeding may be slowed or stopped by applying pressure, clamping, electro/thermocautery, and with various chemicals – Excessive pressure may lead to tissue necrosis
Hemostasis n Bleeding should be stopped whenever possible – Excessive bleeding may cause hematomas or increase dead space – Hematomas prevent wound apposition and retard healing – Blood is a natural food for micro-organisms and a large clot will help protect them from the body’s immune system » Bacteria inside the clot will be protected n Bleeding may be slowed or stopped by applying pressure, clamping, electro/thermocautery, and with various chemicals – Excessive pressure may lead to tissue necrosis
 Dead Space and a Clean Wound n n n Remove all non-essential material Wounds with excessive debris should be thoroughly lavaged with an appropriate sterile fluid (isotonic saline, LRS, Tis-U-Sol, etc. ) to flush them away Dead Space is an open area in closed tissue – Filled with room air, it prevents tissue apposition, provides a space for blood and other fluid influx, and may harbor micro-organisms
Dead Space and a Clean Wound n n n Remove all non-essential material Wounds with excessive debris should be thoroughly lavaged with an appropriate sterile fluid (isotonic saline, LRS, Tis-U-Sol, etc. ) to flush them away Dead Space is an open area in closed tissue – Filled with room air, it prevents tissue apposition, provides a space for blood and other fluid influx, and may harbor micro-organisms
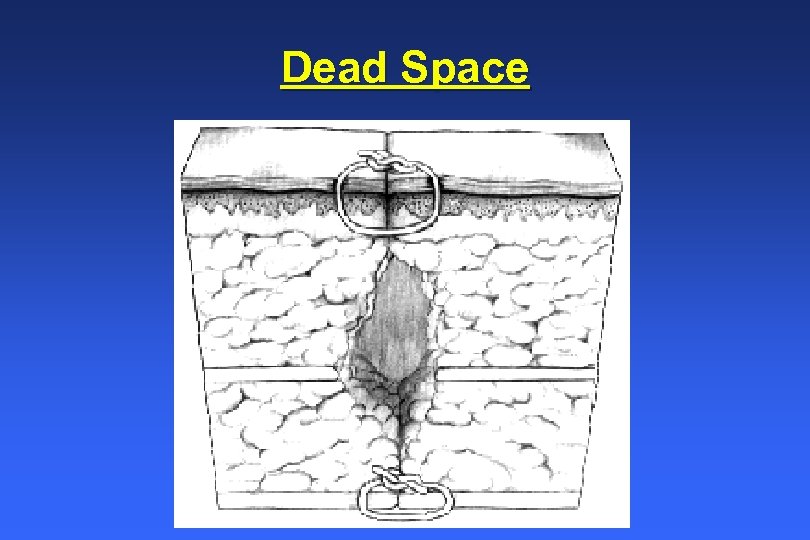 Dead Space
Dead Space
 Classification of Wounds n Clean – Standard surgical wound n Clean-contaminated – Clean wounds that are contaminated by entry into a viscus resulting in minimal spillage of contents n Contaminated – Lacerations, fractures, gross spillage from the GI tract, resulting from a break in aseptic technique – Within 6 hours of initial colonization a wound can be infected
Classification of Wounds n Clean – Standard surgical wound n Clean-contaminated – Clean wounds that are contaminated by entry into a viscus resulting in minimal spillage of contents n Contaminated – Lacerations, fractures, gross spillage from the GI tract, resulting from a break in aseptic technique – Within 6 hours of initial colonization a wound can be infected
 Classification of Wounds n Dirty-infected – Caused by perforated viscera, abscesses, or a prior clinical infection – Ongoing infection at time of surgery may lead to a 400% increase in infection rates
Classification of Wounds n Dirty-infected – Caused by perforated viscera, abscesses, or a prior clinical infection – Ongoing infection at time of surgery may lead to a 400% increase in infection rates
 Problems n Infection – The source of infection should always be determined – Before closure of an infected wound the wound should be drained, debrided, and a small opening or drain left in n Dehiscence – Wound reopens – May result from too much tension on tissue, improper suturing technique, or improper suture materials
Problems n Infection – The source of infection should always be determined – Before closure of an infected wound the wound should be drained, debrided, and a small opening or drain left in n Dehiscence – Wound reopens – May result from too much tension on tissue, improper suturing technique, or improper suture materials
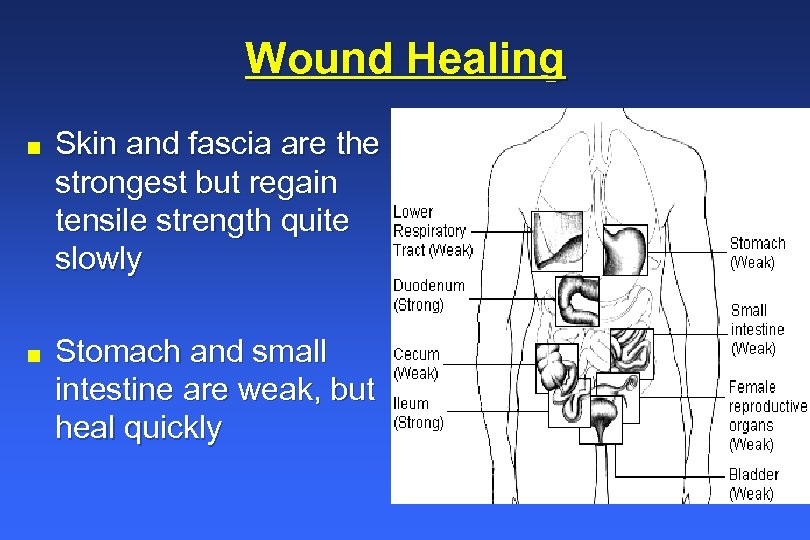 Wound Healing n n Skin and fascia are the strongest but regain tensile strength quite slowly Stomach and small intestine are weak, but heal quickly
Wound Healing n n Skin and fascia are the strongest but regain tensile strength quite slowly Stomach and small intestine are weak, but heal quickly
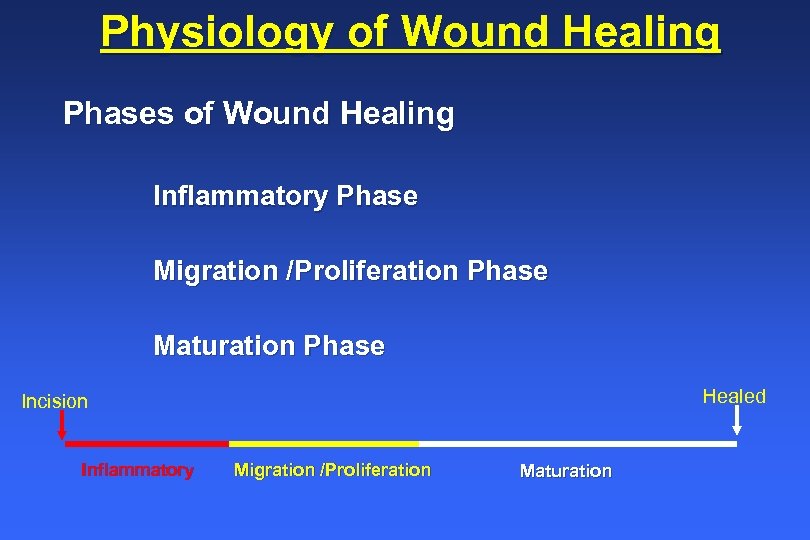 Physiology of Wound Healing Phases of Wound Healing Inflammatory Phase Migration /Proliferation Phase Maturation Phase Healed Incision Inflammatory Migration /Proliferation Maturation
Physiology of Wound Healing Phases of Wound Healing Inflammatory Phase Migration /Proliferation Phase Maturation Phase Healed Incision Inflammatory Migration /Proliferation Maturation
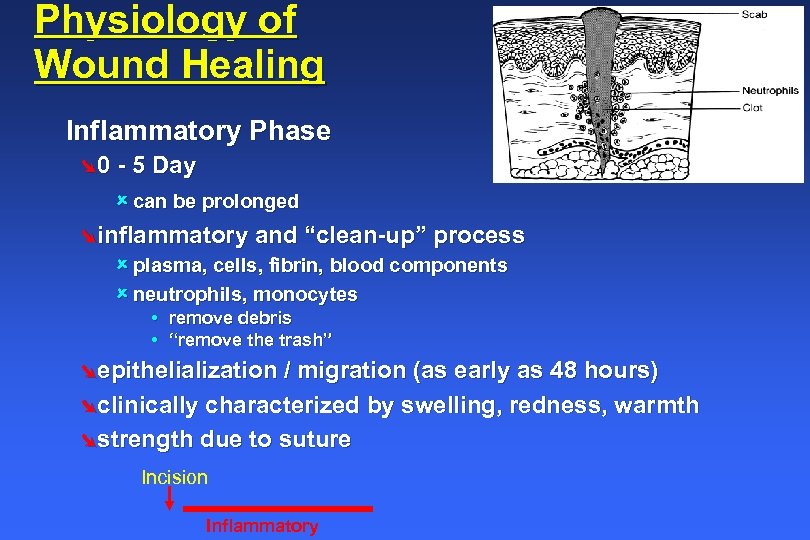 Physiology of Wound Healing Inflammatory Phase Ø 0 - 5 Day û can be prolonged Øinflammatory and “clean-up” process û plasma, cells, fibrin, blood components û neutrophils, monocytes • remove debris • “remove the trash” Øepithelialization / migration (as early as 48 hours) Øclinically characterized by swelling, redness, warmth Østrength due to suture Incision Inflammatory
Physiology of Wound Healing Inflammatory Phase Ø 0 - 5 Day û can be prolonged Øinflammatory and “clean-up” process û plasma, cells, fibrin, blood components û neutrophils, monocytes • remove debris • “remove the trash” Øepithelialization / migration (as early as 48 hours) Øclinically characterized by swelling, redness, warmth Østrength due to suture Incision Inflammatory
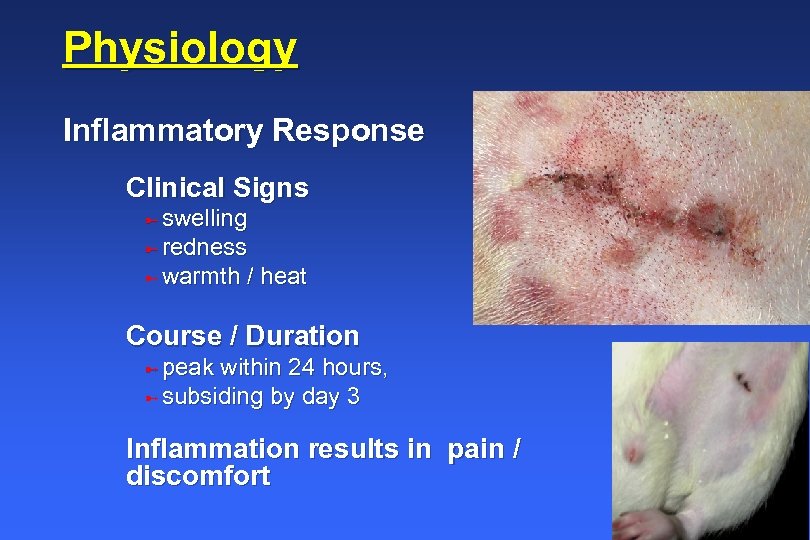 Physiology Inflammatory Response Clinical Signs ü swelling ü redness ü warmth / heat Course / Duration ü peak within 24 hours, ü subsiding by day 3 Inflammation results in pain / discomfort
Physiology Inflammatory Response Clinical Signs ü swelling ü redness ü warmth / heat Course / Duration ü peak within 24 hours, ü subsiding by day 3 Inflammation results in pain / discomfort
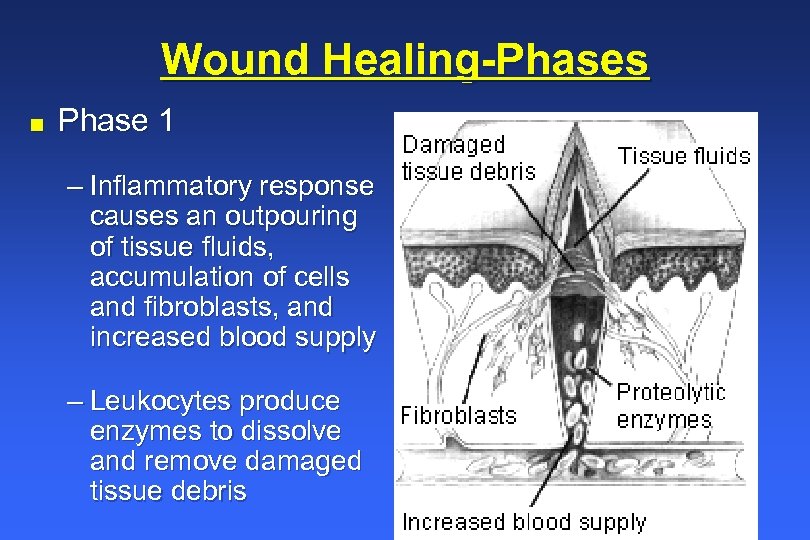 Wound Healing-Phases n Phase 1 – Inflammatory response causes an outpouring of tissue fluids, accumulation of cells and fibroblasts, and increased blood supply – Leukocytes produce enzymes to dissolve and remove damaged tissue debris
Wound Healing-Phases n Phase 1 – Inflammatory response causes an outpouring of tissue fluids, accumulation of cells and fibroblasts, and increased blood supply – Leukocytes produce enzymes to dissolve and remove damaged tissue debris
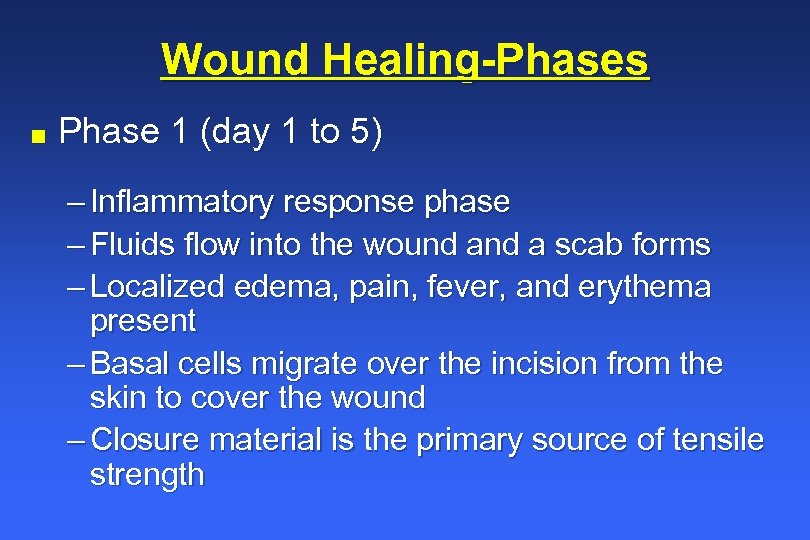 Wound Healing-Phases n Phase 1 (day 1 to 5) – Inflammatory response phase – Fluids flow into the wound a scab forms – Localized edema, pain, fever, and erythema present – Basal cells migrate over the incision from the skin to cover the wound – Closure material is the primary source of tensile strength
Wound Healing-Phases n Phase 1 (day 1 to 5) – Inflammatory response phase – Fluids flow into the wound a scab forms – Localized edema, pain, fever, and erythema present – Basal cells migrate over the incision from the skin to cover the wound – Closure material is the primary source of tensile strength
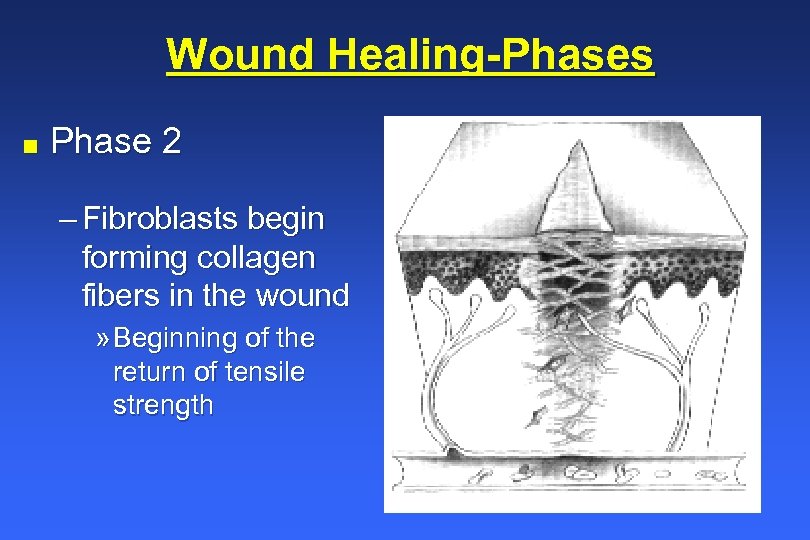 Wound Healing-Phases n Phase 2 – Fibroblasts begin forming collagen fibers in the wound » Beginning of the return of tensile strength
Wound Healing-Phases n Phase 2 – Fibroblasts begin forming collagen fibers in the wound » Beginning of the return of tensile strength
 Wound Healing-Phases n Phase 2 (day 5 to 14) – Fibroblasts migrate toward the wound site » Begin forming collagen fibers – Tensile strength rapidly increases – Lymphatics recanalize – Blood vessels bud – Granulation tissue forms – Capillaries develop
Wound Healing-Phases n Phase 2 (day 5 to 14) – Fibroblasts migrate toward the wound site » Begin forming collagen fibers – Tensile strength rapidly increases – Lymphatics recanalize – Blood vessels bud – Granulation tissue forms – Capillaries develop
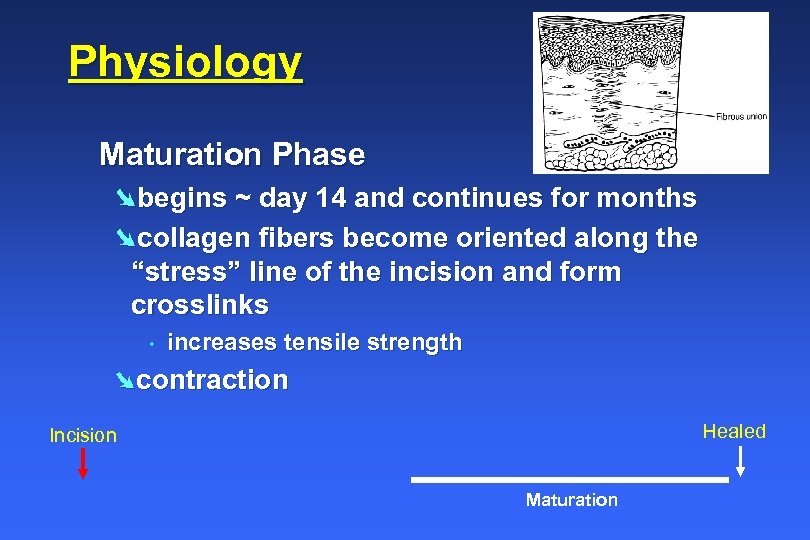 Physiology Maturation Phase Øbegins ~ day 14 and continues for months Øcollagen fibers become oriented along the “stress” line of the incision and form crosslinks • increases tensile strength Øcontraction Healed Incision Maturation
Physiology Maturation Phase Øbegins ~ day 14 and continues for months Øcollagen fibers become oriented along the “stress” line of the incision and form crosslinks • increases tensile strength Øcontraction Healed Incision Maturation
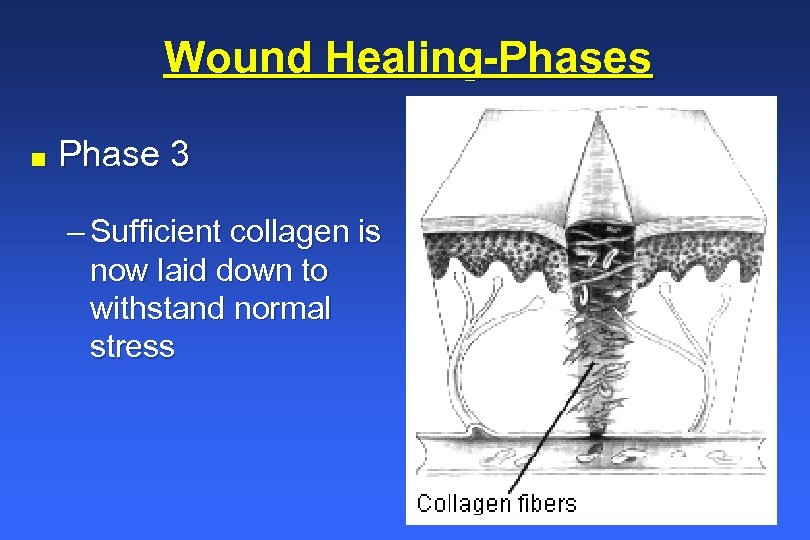 Wound Healing-Phases n Phase 3 – Sufficient collagen is now laid down to withstand normal stress
Wound Healing-Phases n Phase 3 – Sufficient collagen is now laid down to withstand normal stress
 Wound Healing-Phases n Phase 3 (day 14 until done) – Tensile strength continues to improve for as long as one year – Skin regains 70 to 90% of its original strength – Collagen content remains constant but crosslinks with other fibers – Scar is formed which grows paler as new vessel construction tapers off – Wound contraction occurs over a period of weeks or months
Wound Healing-Phases n Phase 3 (day 14 until done) – Tensile strength continues to improve for as long as one year – Skin regains 70 to 90% of its original strength – Collagen content remains constant but crosslinks with other fibers – Scar is formed which grows paler as new vessel construction tapers off – Wound contraction occurs over a period of weeks or months
 Wound Healing Types n First Intention – Wound edges brought together during closure at the time of surgery n Second Intention – Wound is left open and heals from the bottom up – Slower than first intention and creates more granulation and scar tissue n Third Intention – Wound is initially not closed and remains open until a granulation bed formed, then the granulated tissue is closed using standard techniques – Useful in infected wounds » Infected tissue should not be closed or it will dehiss » Infection is resolved naturally, or with topical and systemic treatments
Wound Healing Types n First Intention – Wound edges brought together during closure at the time of surgery n Second Intention – Wound is left open and heals from the bottom up – Slower than first intention and creates more granulation and scar tissue n Third Intention – Wound is initially not closed and remains open until a granulation bed formed, then the granulated tissue is closed using standard techniques – Useful in infected wounds » Infected tissue should not be closed or it will dehiss » Infection is resolved naturally, or with topical and systemic treatments
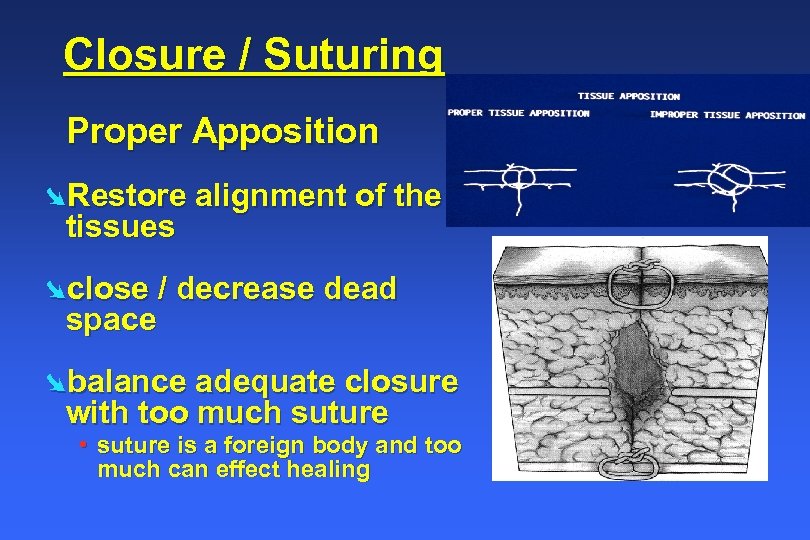 Closure / Suturing Proper Apposition ØRestore alignment of the tissues Øclose / decrease dead space Øbalance adequate closure with too much suture • suture is a foreign body and too much can effect healing
Closure / Suturing Proper Apposition ØRestore alignment of the tissues Øclose / decrease dead space Øbalance adequate closure with too much suture • suture is a foreign body and too much can effect healing
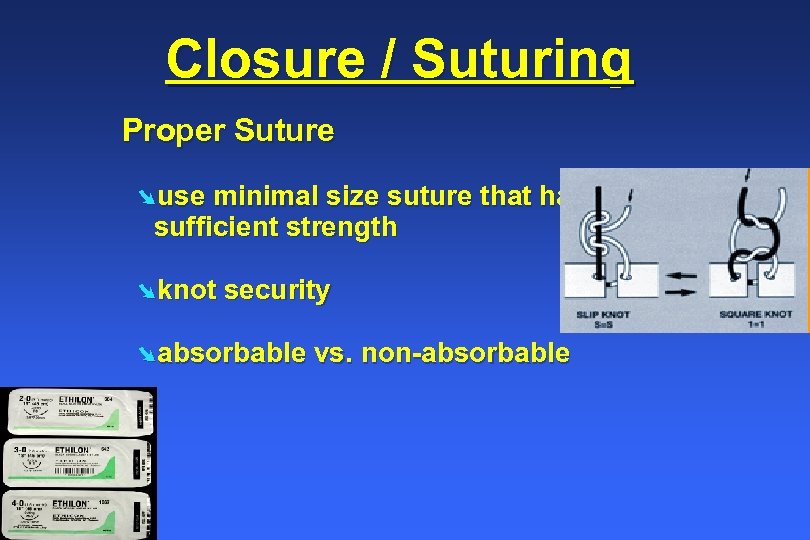 Closure / Suturing Proper Suture Øuse minimal size suture that has sufficient strength Øknot security Øabsorbable vs. non-absorbable
Closure / Suturing Proper Suture Øuse minimal size suture that has sufficient strength Øknot security Øabsorbable vs. non-absorbable
 Sutures n Ideal suture material · All-purpose, composed of material which could be used in any surgical procedure (the only variables being size and tensile strength) · Sterile · Nonelectrolytic, noncapillary, nonallergenic, and noncarcinogenic · Nonferromagnetic, as is the case with stainless steel sutures · Easy to handle
Sutures n Ideal suture material · All-purpose, composed of material which could be used in any surgical procedure (the only variables being size and tensile strength) · Sterile · Nonelectrolytic, noncapillary, nonallergenic, and noncarcinogenic · Nonferromagnetic, as is the case with stainless steel sutures · Easy to handle
 Sutures n Ideal suture material · Minimally reactive in tissue and not predisposed to bacterial growth · Capable of holding securely when knotted without fraying or cutting · Resistant to shrinking in tissues · Absorbed with minimal tissue reaction after serving its purpose · Doesn’t exist!
Sutures n Ideal suture material · Minimally reactive in tissue and not predisposed to bacterial growth · Capable of holding securely when knotted without fraying or cutting · Resistant to shrinking in tissues · Absorbed with minimal tissue reaction after serving its purpose · Doesn’t exist!
 Sutures n Surgeon should select suture materials for – High uniform tensile strength (quality) – Permitting use of finer sizes » Suture should be the smallest diameter that will do the job – Consistent uniform diameter – Sterile – Pliable for ease of handling and knot security – Freedom from irritating substances or impurities for optimum tissue acceptance – Predictable performance
Sutures n Surgeon should select suture materials for – High uniform tensile strength (quality) – Permitting use of finer sizes » Suture should be the smallest diameter that will do the job – Consistent uniform diameter – Sterile – Pliable for ease of handling and knot security – Freedom from irritating substances or impurities for optimum tissue acceptance – Predictable performance
 Sutures n Size – Generally stated in “oughts”; i. e. , 3 -0, 5 -0, etc. – 2 -0 is larger than 4 -0, 0 is larger than 2 -0, etc. – Some suture and wire is larger than 0, then numbered 1 and higher » 2 is larger than 1, 6 is larger than 1, etc. – From smallest to largest: » 7 -0, 3 -0, 0, 1, 3, 7, etc.
Sutures n Size – Generally stated in “oughts”; i. e. , 3 -0, 5 -0, etc. – 2 -0 is larger than 4 -0, 0 is larger than 2 -0, etc. – Some suture and wire is larger than 0, then numbered 1 and higher » 2 is larger than 1, 6 is larger than 1, etc. – From smallest to largest: » 7 -0, 3 -0, 0, 1, 3, 7, etc.
 Sutures Monofilament is a single strand » Passes through tissue easily, won’t harbor microorganisms » Ties easily » May be weakened by crushing (clamping in forceps or needle holders) » Has more “memory” n Continues to hold the shape as it lay in the package » Good for percutaneous sutures » Knots may slip over time due to the slipperiness of the suture
Sutures Monofilament is a single strand » Passes through tissue easily, won’t harbor microorganisms » Ties easily » May be weakened by crushing (clamping in forceps or needle holders) » Has more “memory” n Continues to hold the shape as it lay in the package » Good for percutaneous sutures » Knots may slip over time due to the slipperiness of the suture
 Sutures Multifilament is a bundle of strands, like rope » Affords greater tensile strength, pliability, flexibility, and knot security » May harbor micro-organisms and “wick” them down the suture n Should not be used for percutaneous sutures
Sutures Multifilament is a bundle of strands, like rope » Affords greater tensile strength, pliability, flexibility, and knot security » May harbor micro-organisms and “wick” them down the suture n Should not be used for percutaneous sutures
 Sutures Absorbable suture holds temporarily but gradually loses tensile strength and is eventually mostly or completely absorbed
Sutures Absorbable suture holds temporarily but gradually loses tensile strength and is eventually mostly or completely absorbed
 Absorbable Sutures Surgical Catgut: Plain or Chromic Absorbed by proleolytic enzymatic digestive process. Polyglactin 910 : Vicryl® Polyglycolic acid: Dexon® Poliglecaprone 25: Monocryl® Polydixanone: PDSII® Polyglyconate: Maxon® Absorbed by Hydrolysis
Absorbable Sutures Surgical Catgut: Plain or Chromic Absorbed by proleolytic enzymatic digestive process. Polyglactin 910 : Vicryl® Polyglycolic acid: Dexon® Poliglecaprone 25: Monocryl® Polydixanone: PDSII® Polyglyconate: Maxon® Absorbed by Hydrolysis
 Sutures Nonabsorbable suture will retain tensile strength and not be absorbed » Many nonabsorbable sutures (silk) will lose some tensile strength over time » Useful for device fixation, areas of extreme tension, slow healing areas, or percutaneous skin sutures » Selected for procedures where the suture should be permanent
Sutures Nonabsorbable suture will retain tensile strength and not be absorbed » Many nonabsorbable sutures (silk) will lose some tensile strength over time » Useful for device fixation, areas of extreme tension, slow healing areas, or percutaneous skin sutures » Selected for procedures where the suture should be permanent
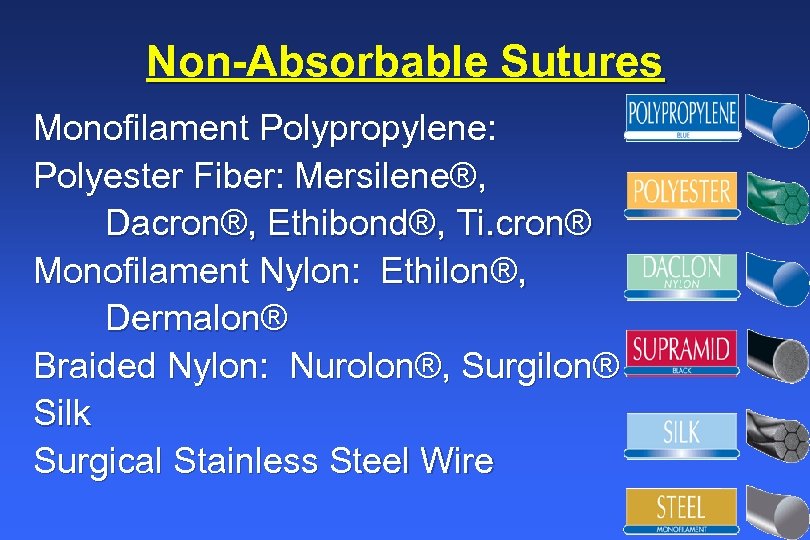 Non-Absorbable Sutures Monofilament Polypropylene: Polyester Fiber: Mersilene®, Dacron®, Ethibond®, Ti. cron® Monofilament Nylon: Ethilon®, Dermalon® Braided Nylon: Nurolon®, Surgilon® Silk Surgical Stainless Steel Wire
Non-Absorbable Sutures Monofilament Polypropylene: Polyester Fiber: Mersilene®, Dacron®, Ethibond®, Ti. cron® Monofilament Nylon: Ethilon®, Dermalon® Braided Nylon: Nurolon®, Surgilon® Silk Surgical Stainless Steel Wire
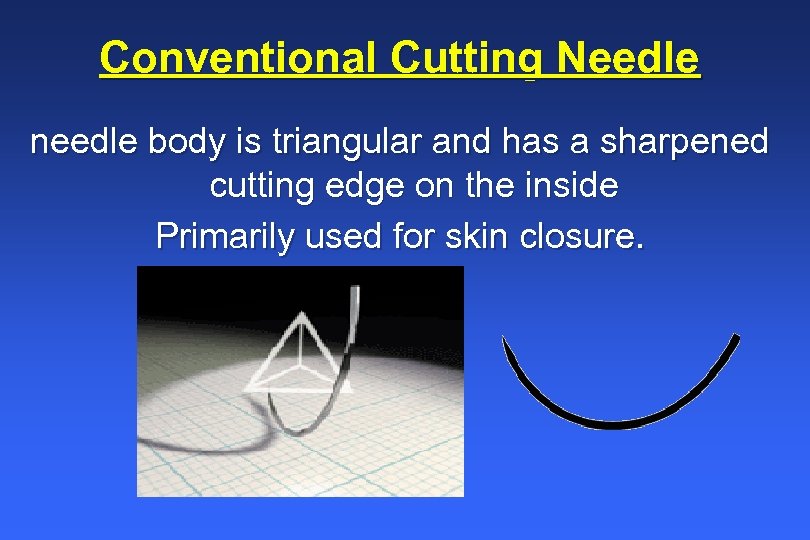 Conventional Cutting Needle needle body is triangular and has a sharpened cutting edge on the inside Primarily used for skin closure.
Conventional Cutting Needle needle body is triangular and has a sharpened cutting edge on the inside Primarily used for skin closure.
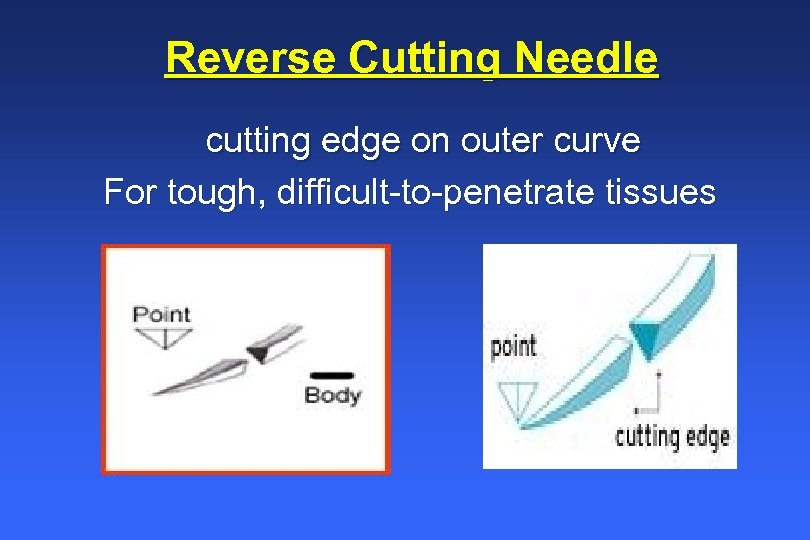 Reverse Cutting Needle cutting edge on outer curve For tough, difficult-to-penetrate tissues
Reverse Cutting Needle cutting edge on outer curve For tough, difficult-to-penetrate tissues
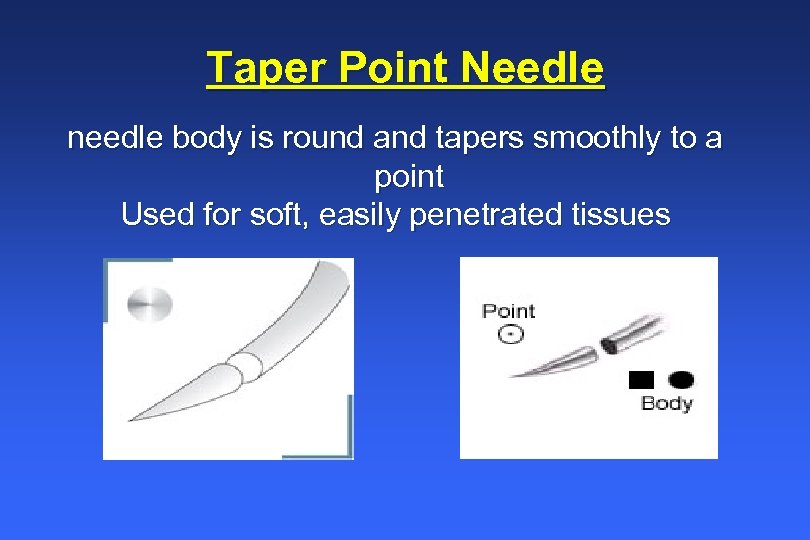 Taper Point Needle needle body is round and tapers smoothly to a point Used for soft, easily penetrated tissues
Taper Point Needle needle body is round and tapers smoothly to a point Used for soft, easily penetrated tissues
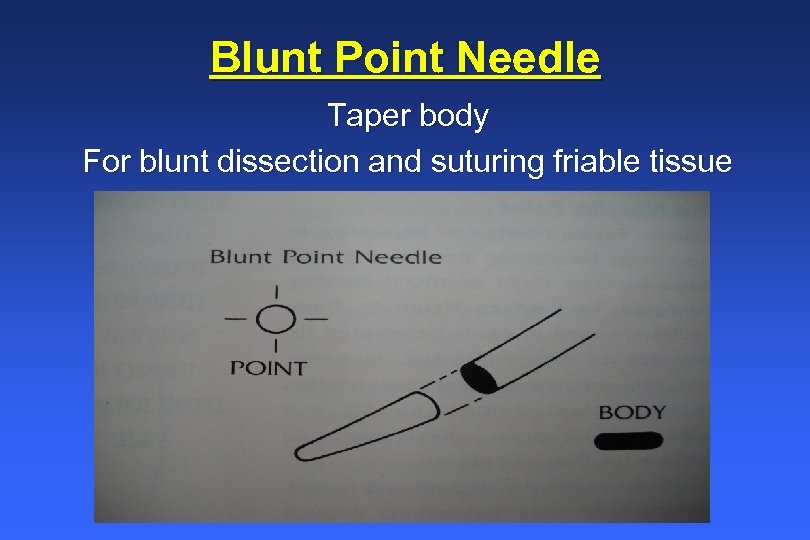 Blunt Point Needle Taper body For blunt dissection and suturing friable tissue
Blunt Point Needle Taper body For blunt dissection and suturing friable tissue
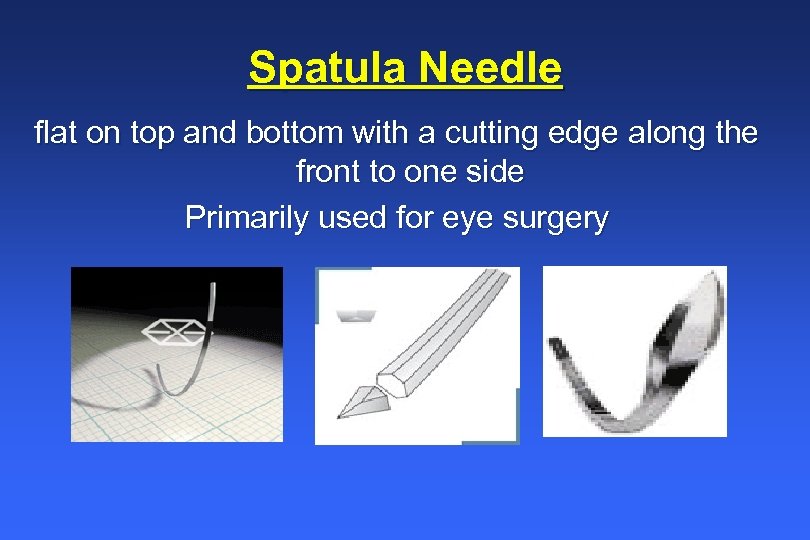 Spatula Needle flat on top and bottom with a cutting edge along the front to one side Primarily used for eye surgery
Spatula Needle flat on top and bottom with a cutting edge along the front to one side Primarily used for eye surgery
 Surgeon’s Knot n Extra throws do not add appreciable strength to the knot and may, in fact, weaken it while adding extra bulk – An initial double throw followed by one or two single throws is more than sufficient – The exception is nylon monofilament sutures, where two successive double throws are useful to prevent slippage
Surgeon’s Knot n Extra throws do not add appreciable strength to the knot and may, in fact, weaken it while adding extra bulk – An initial double throw followed by one or two single throws is more than sufficient – The exception is nylon monofilament sutures, where two successive double throws are useful to prevent slippage
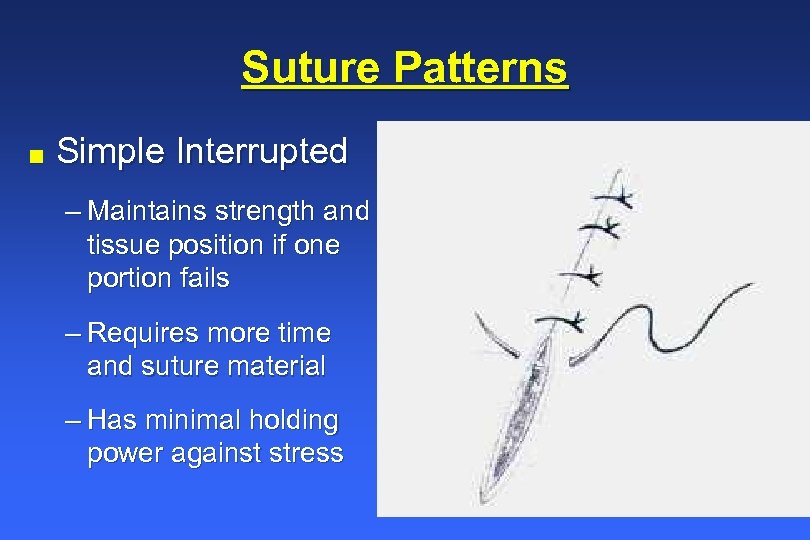 Suture Patterns n Simple Interrupted – Maintains strength and tissue position if one portion fails – Requires more time and suture material – Has minimal holding power against stress
Suture Patterns n Simple Interrupted – Maintains strength and tissue position if one portion fails – Requires more time and suture material – Has minimal holding power against stress
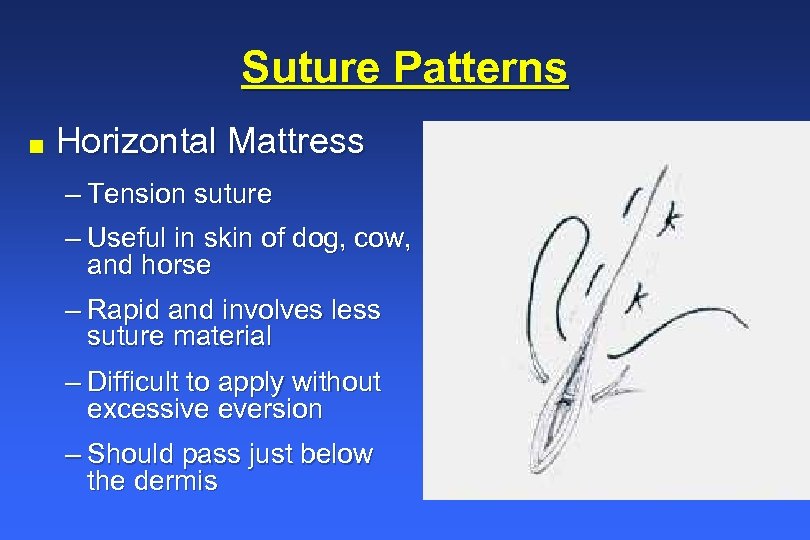 Suture Patterns n Horizontal Mattress – Tension suture – Useful in skin of dog, cow, and horse – Rapid and involves less suture material – Difficult to apply without excessive eversion – Should pass just below the dermis
Suture Patterns n Horizontal Mattress – Tension suture – Useful in skin of dog, cow, and horse – Rapid and involves less suture material – Difficult to apply without excessive eversion – Should pass just below the dermis
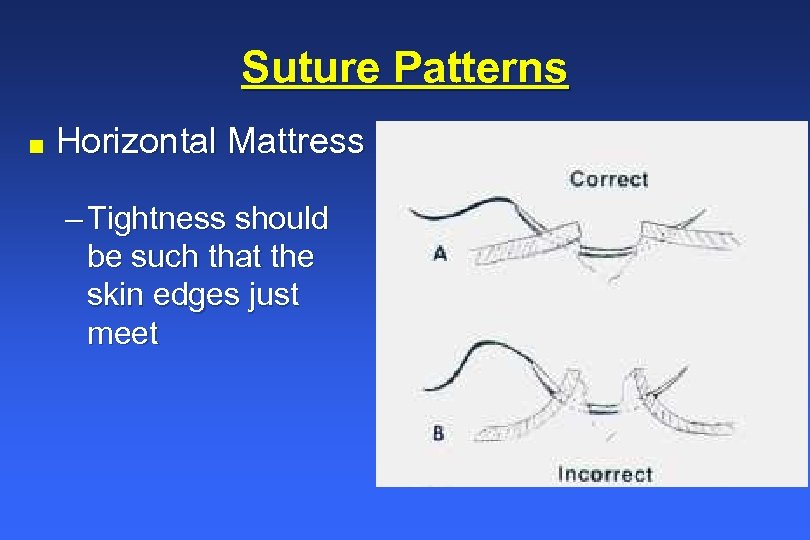 Suture Patterns n Horizontal Mattress – Tightness should be such that the skin edges just meet
Suture Patterns n Horizontal Mattress – Tightness should be such that the skin edges just meet
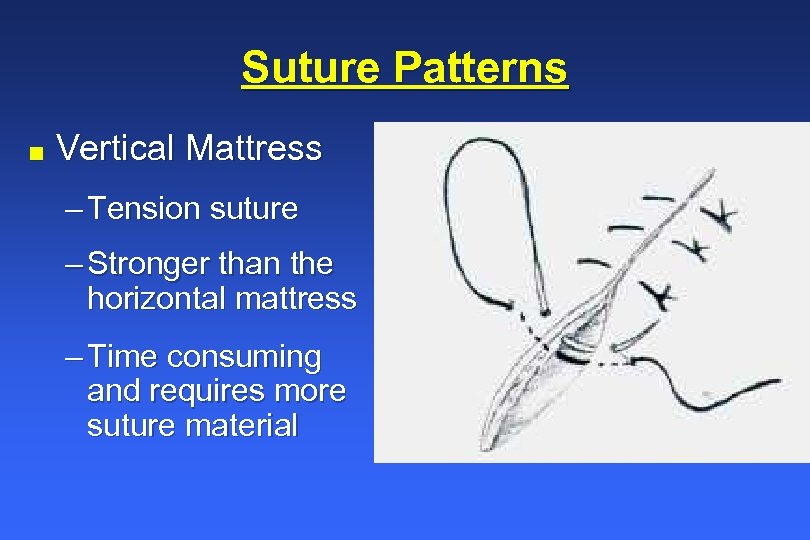 Suture Patterns n Vertical Mattress – Tension suture – Stronger than the horizontal mattress – Time consuming and requires more suture material
Suture Patterns n Vertical Mattress – Tension suture – Stronger than the horizontal mattress – Time consuming and requires more suture material
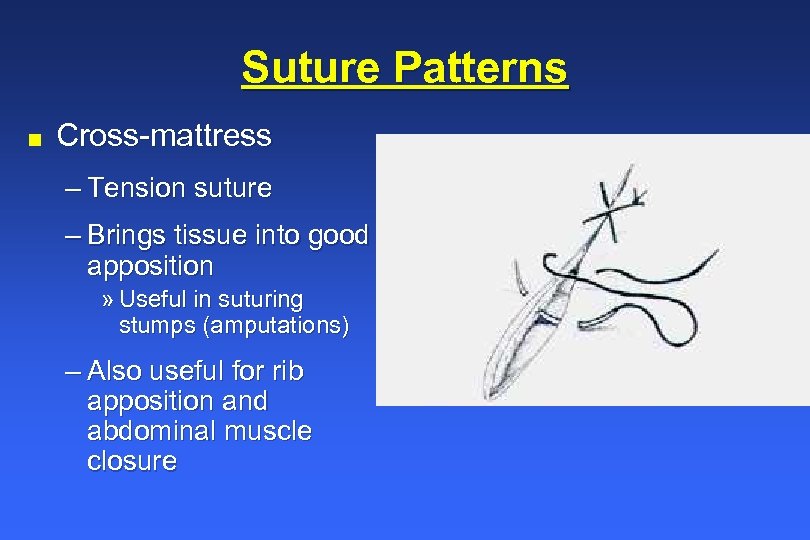 Suture Patterns n Cross-mattress – Tension suture – Brings tissue into good apposition » Useful in suturing stumps (amputations) – Also useful for rib apposition and abdominal muscle closure
Suture Patterns n Cross-mattress – Tension suture – Brings tissue into good apposition » Useful in suturing stumps (amputations) – Also useful for rib apposition and abdominal muscle closure
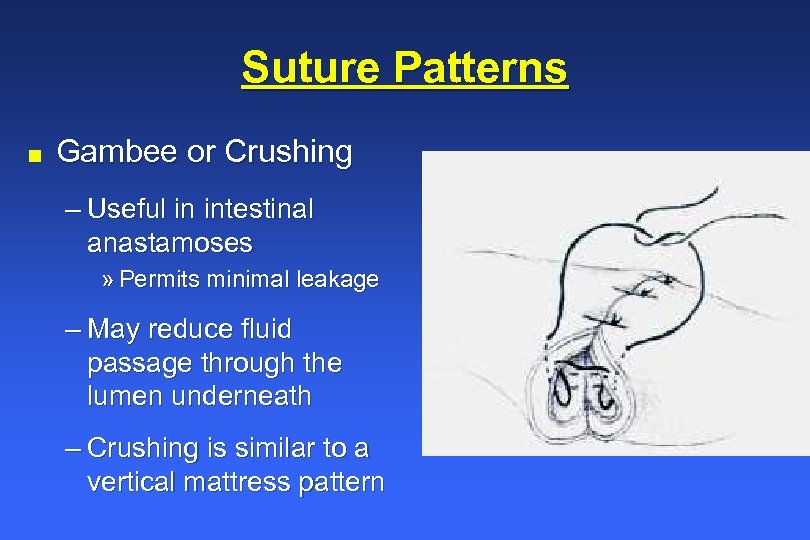 Suture Patterns n Gambee or Crushing – Useful in intestinal anastamoses » Permits minimal leakage – May reduce fluid passage through the lumen underneath – Crushing is similar to a vertical mattress pattern
Suture Patterns n Gambee or Crushing – Useful in intestinal anastamoses » Permits minimal leakage – May reduce fluid passage through the lumen underneath – Crushing is similar to a vertical mattress pattern
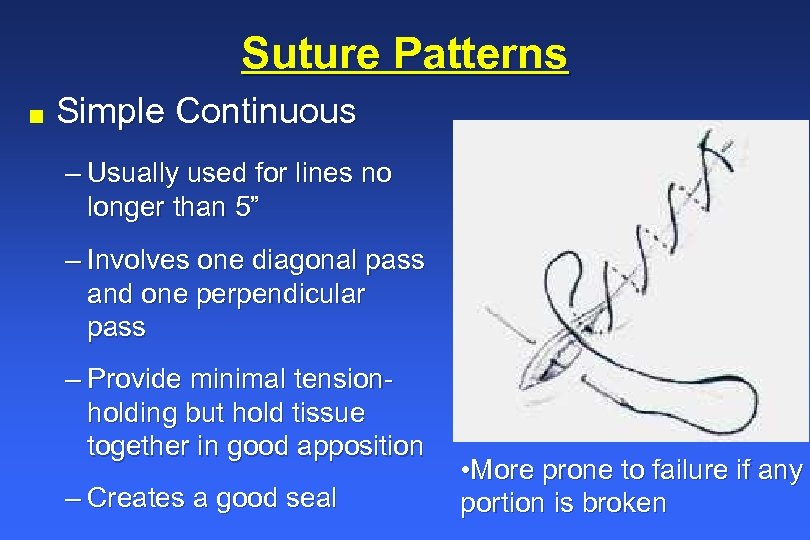 Suture Patterns n Simple Continuous – Usually used for lines no longer than 5” – Involves one diagonal pass and one perpendicular pass – Provide minimal tensionholding but hold tissue together in good apposition – Creates a good seal • More prone to failure if any portion is broken
Suture Patterns n Simple Continuous – Usually used for lines no longer than 5” – Involves one diagonal pass and one perpendicular pass – Provide minimal tensionholding but hold tissue together in good apposition – Creates a good seal • More prone to failure if any portion is broken
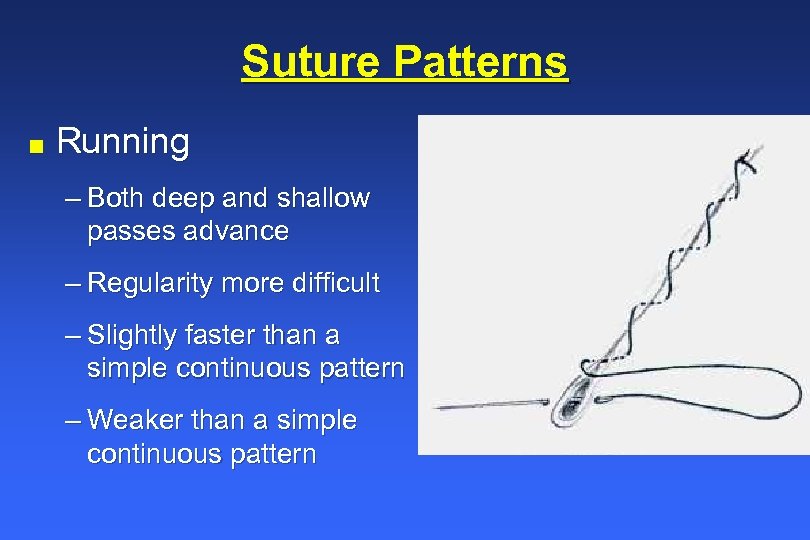 Suture Patterns n Running – Both deep and shallow passes advance – Regularity more difficult – Slightly faster than a simple continuous pattern – Weaker than a simple continuous pattern
Suture Patterns n Running – Both deep and shallow passes advance – Regularity more difficult – Slightly faster than a simple continuous pattern – Weaker than a simple continuous pattern
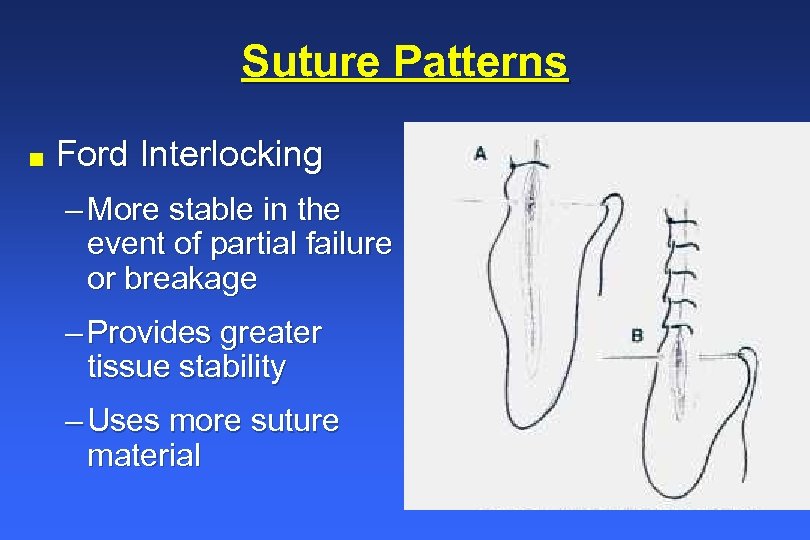 Suture Patterns n Ford Interlocking – More stable in the event of partial failure or breakage – Provides greater tissue stability – Uses more suture material
Suture Patterns n Ford Interlocking – More stable in the event of partial failure or breakage – Provides greater tissue stability – Uses more suture material
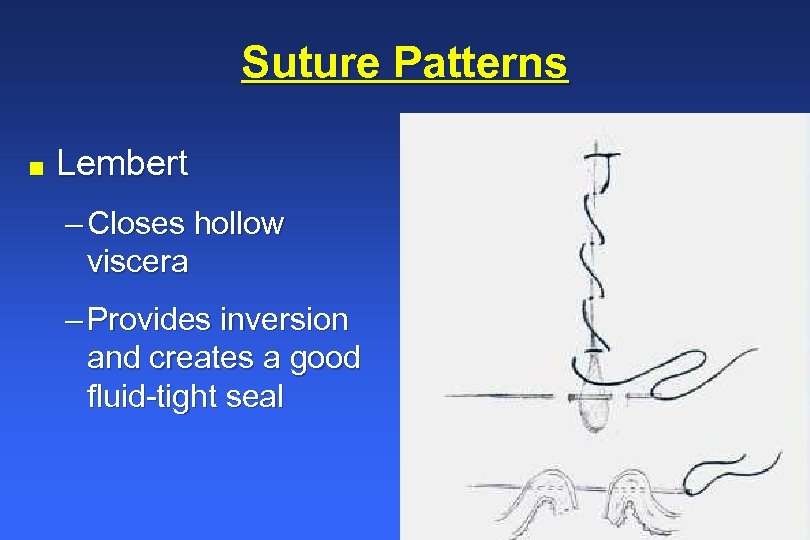 Suture Patterns n Lembert – Closes hollow viscera – Provides inversion and creates a good fluid-tight seal
Suture Patterns n Lembert – Closes hollow viscera – Provides inversion and creates a good fluid-tight seal
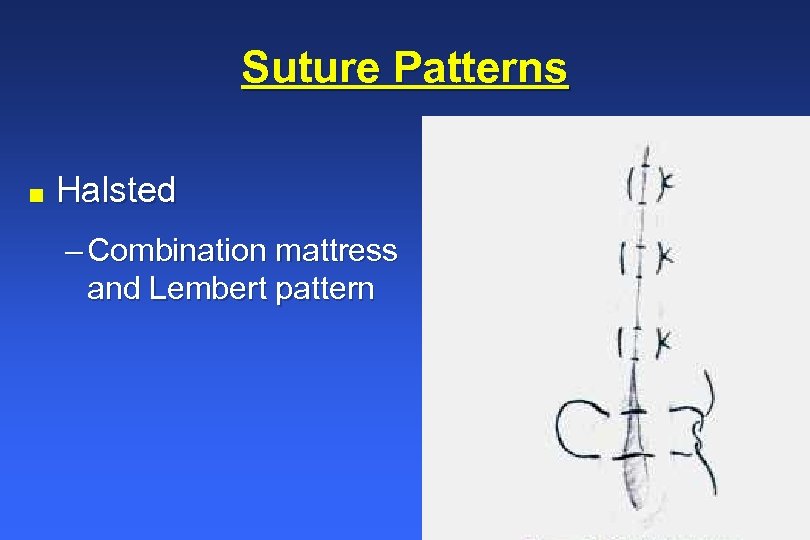 Suture Patterns n Halsted – Combination mattress and Lembert pattern
Suture Patterns n Halsted – Combination mattress and Lembert pattern
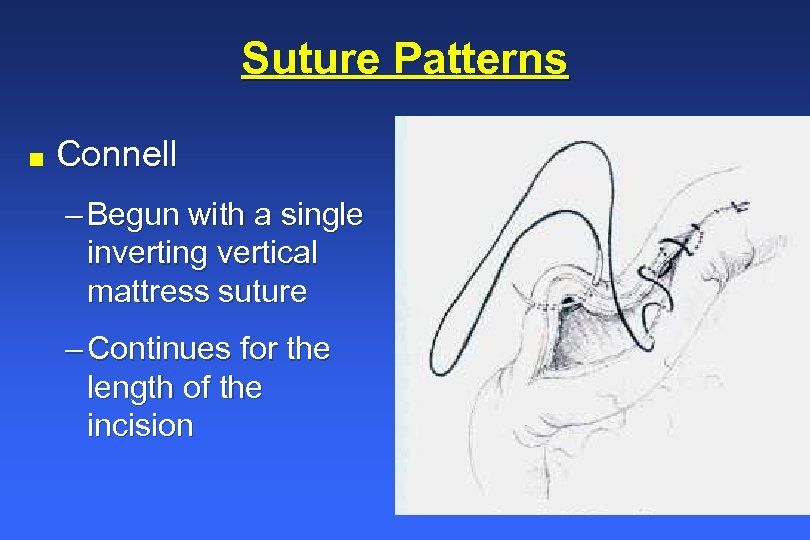 Suture Patterns n Connell – Begun with a single inverting vertical mattress suture – Continues for the length of the incision
Suture Patterns n Connell – Begun with a single inverting vertical mattress suture – Continues for the length of the incision
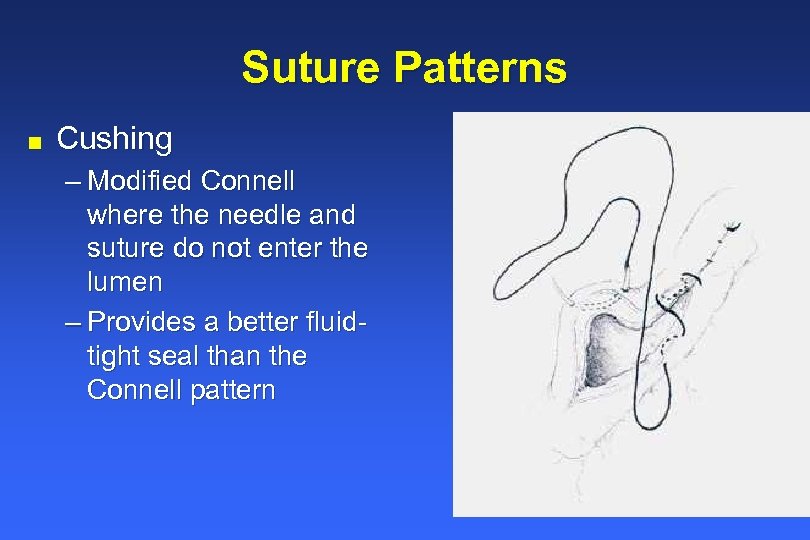 Suture Patterns n Cushing – Modified Connell where the needle and suture do not enter the lumen – Provides a better fluidtight seal than the Connell pattern
Suture Patterns n Cushing – Modified Connell where the needle and suture do not enter the lumen – Provides a better fluidtight seal than the Connell pattern
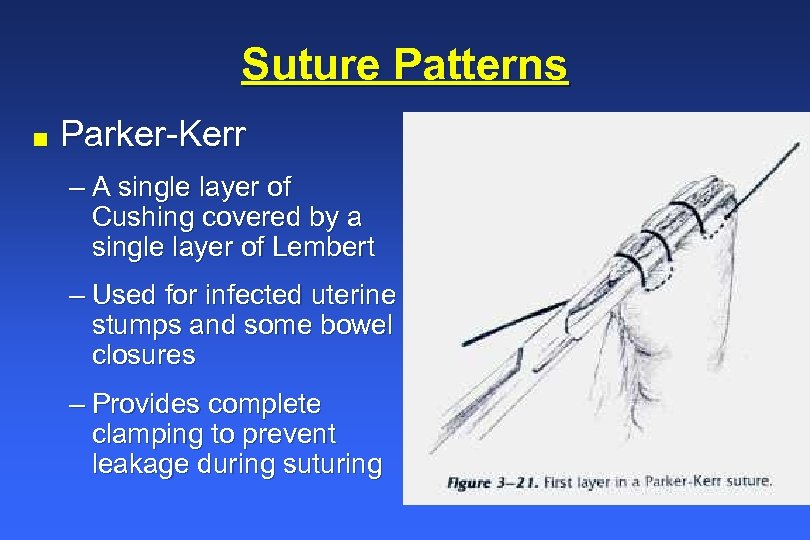 Suture Patterns n Parker-Kerr – A single layer of Cushing covered by a single layer of Lembert – Used for infected uterine stumps and some bowel closures – Provides complete clamping to prevent leakage during suturing
Suture Patterns n Parker-Kerr – A single layer of Cushing covered by a single layer of Lembert – Used for infected uterine stumps and some bowel closures – Provides complete clamping to prevent leakage during suturing
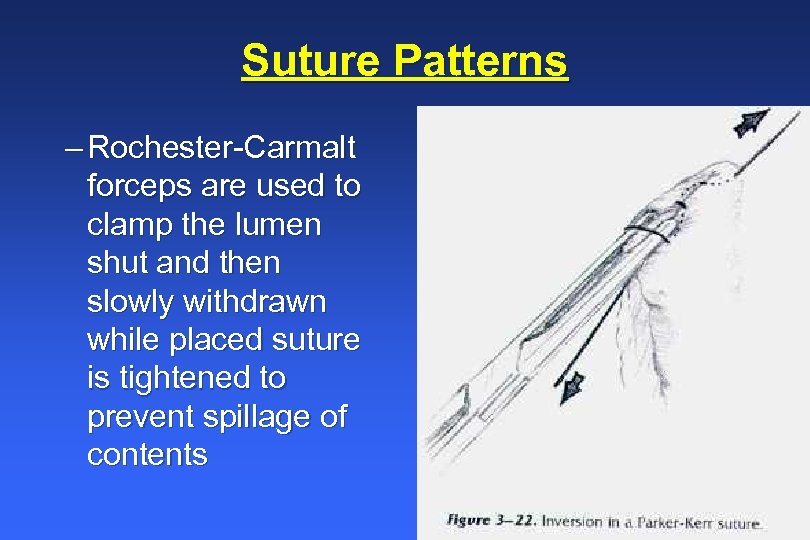 Suture Patterns – Rochester-Carmalt forceps are used to clamp the lumen shut and then slowly withdrawn while placed suture is tightened to prevent spillage of contents
Suture Patterns – Rochester-Carmalt forceps are used to clamp the lumen shut and then slowly withdrawn while placed suture is tightened to prevent spillage of contents
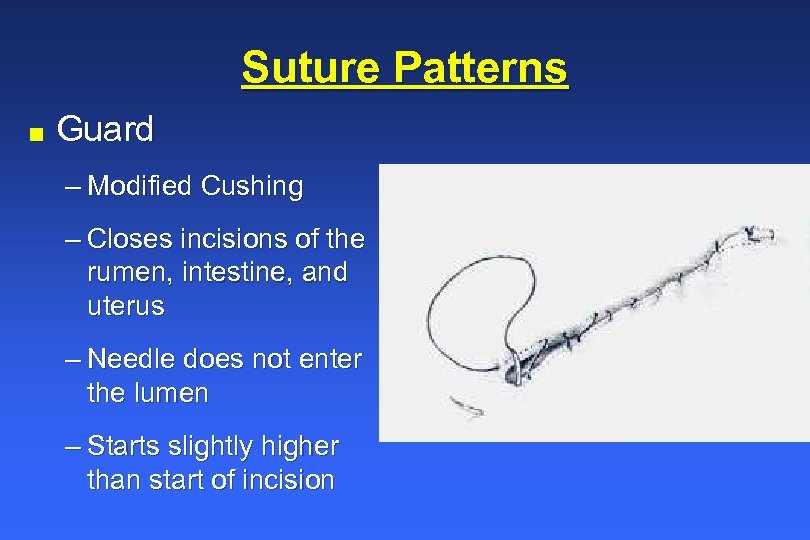 Suture Patterns n Guard – Modified Cushing – Closes incisions of the rumen, intestine, and uterus – Needle does not enter the lumen – Starts slightly higher than start of incision
Suture Patterns n Guard – Modified Cushing – Closes incisions of the rumen, intestine, and uterus – Needle does not enter the lumen – Starts slightly higher than start of incision
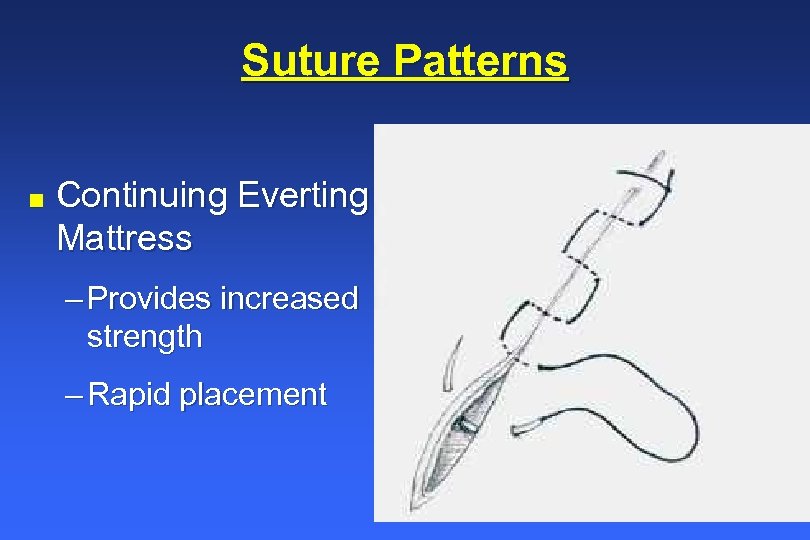 Suture Patterns n Continuing Everting Mattress – Provides increased strength – Rapid placement
Suture Patterns n Continuing Everting Mattress – Provides increased strength – Rapid placement
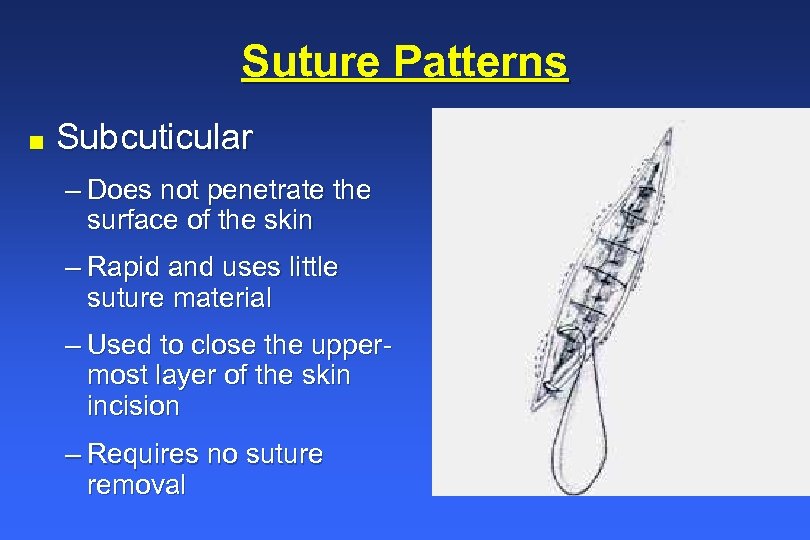 Suture Patterns n Subcuticular – Does not penetrate the surface of the skin – Rapid and uses little suture material – Used to close the uppermost layer of the skin incision – Requires no suture removal
Suture Patterns n Subcuticular – Does not penetrate the surface of the skin – Rapid and uses little suture material – Used to close the uppermost layer of the skin incision – Requires no suture removal
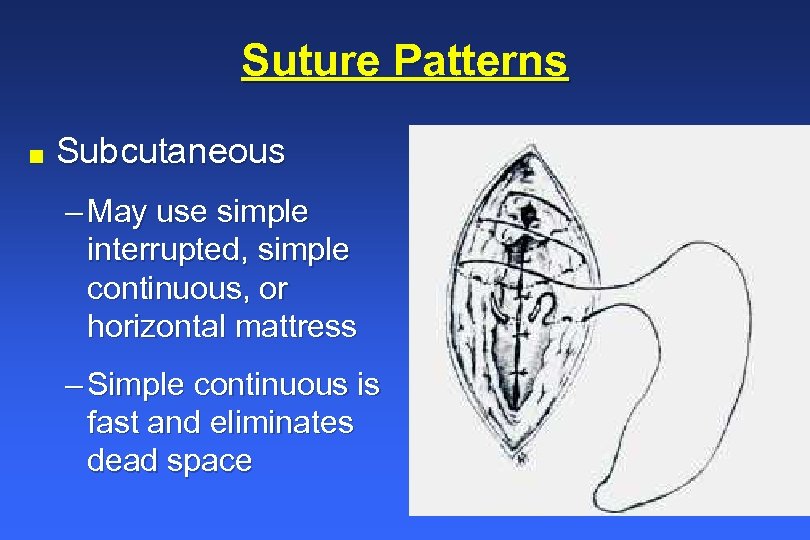 Suture Patterns n Subcutaneous – May use simple interrupted, simple continuous, or horizontal mattress – Simple continuous is fast and eliminates dead space
Suture Patterns n Subcutaneous – May use simple interrupted, simple continuous, or horizontal mattress – Simple continuous is fast and eliminates dead space
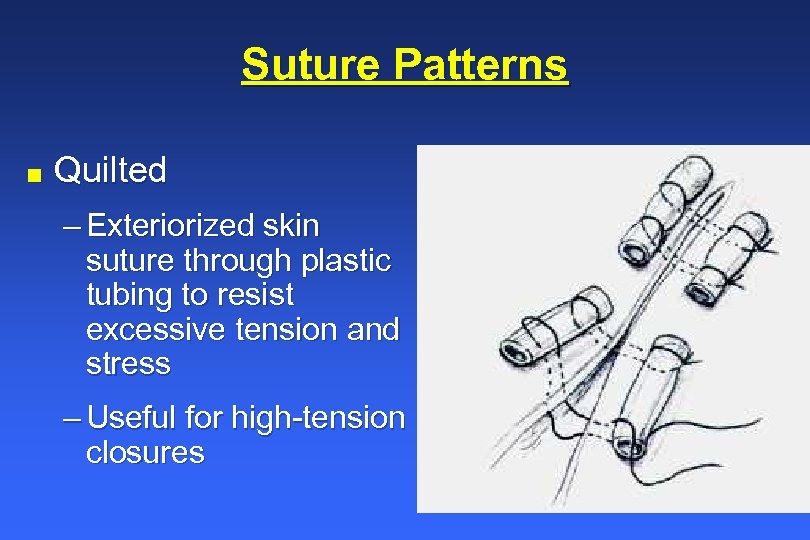 Suture Patterns n Quilted – Exteriorized skin suture through plastic tubing to resist excessive tension and stress – Useful for high-tension closures
Suture Patterns n Quilted – Exteriorized skin suture through plastic tubing to resist excessive tension and stress – Useful for high-tension closures
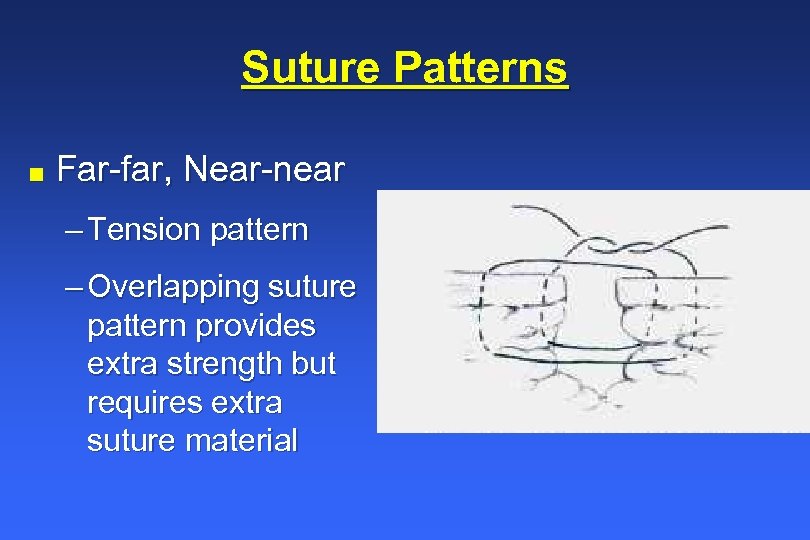 Suture Patterns n Far-far, Near-near – Tension pattern – Overlapping suture pattern provides extra strength but requires extra suture material
Suture Patterns n Far-far, Near-near – Tension pattern – Overlapping suture pattern provides extra strength but requires extra suture material
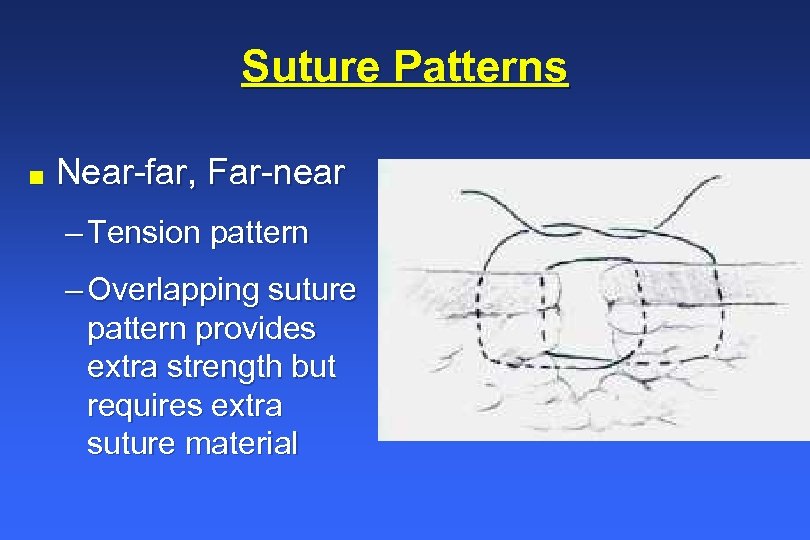 Suture Patterns n Near-far, Far-near – Tension pattern – Overlapping suture pattern provides extra strength but requires extra suture material
Suture Patterns n Near-far, Far-near – Tension pattern – Overlapping suture pattern provides extra strength but requires extra suture material
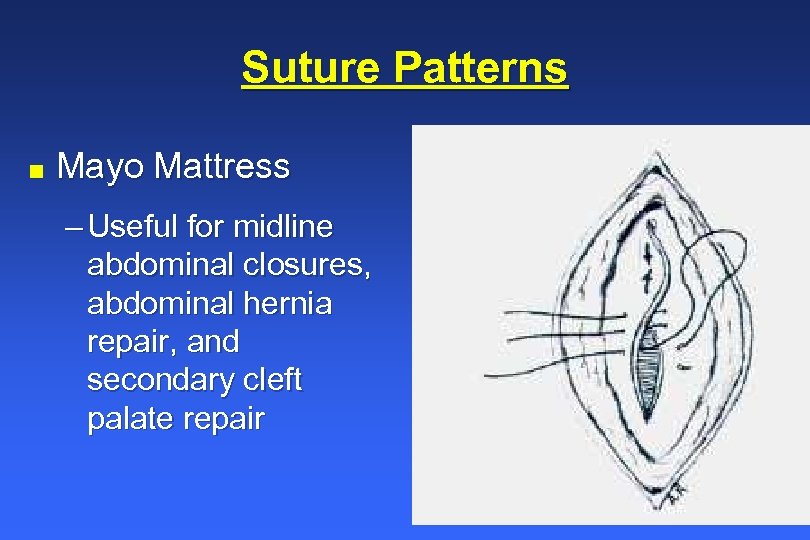 Suture Patterns n Mayo Mattress – Useful for midline abdominal closures, abdominal hernia repair, and secondary cleft palate repair
Suture Patterns n Mayo Mattress – Useful for midline abdominal closures, abdominal hernia repair, and secondary cleft palate repair
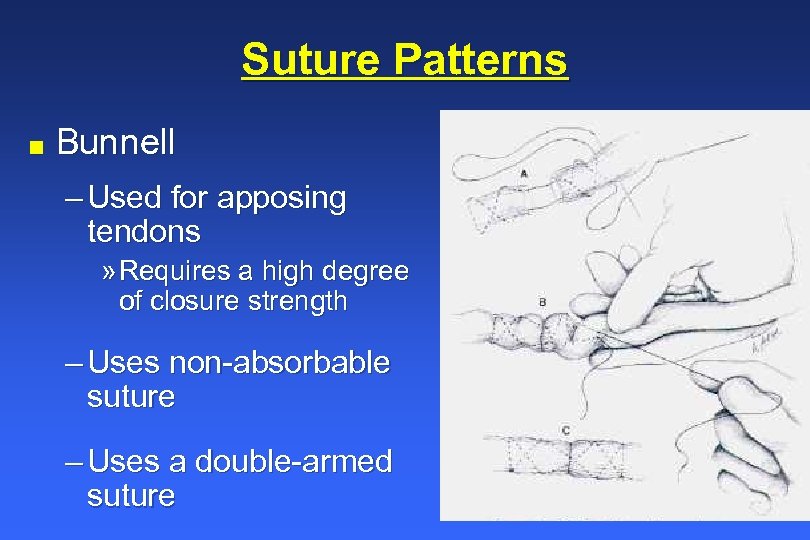 Suture Patterns n Bunnell – Used for apposing tendons » Requires a high degree of closure strength – Uses non-absorbable suture – Uses a double-armed suture
Suture Patterns n Bunnell – Used for apposing tendons » Requires a high degree of closure strength – Uses non-absorbable suture – Uses a double-armed suture
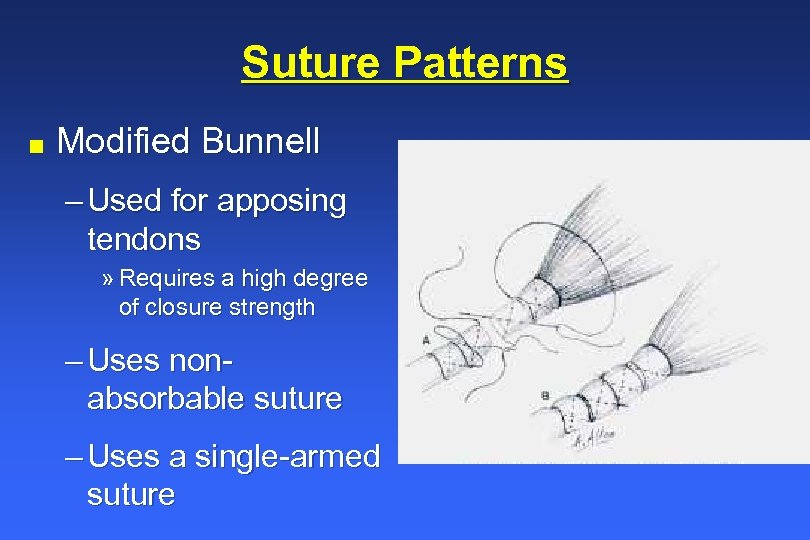 Suture Patterns n Modified Bunnell – Used for apposing tendons » Requires a high degree of closure strength – Uses nonabsorbable suture – Uses a single-armed suture
Suture Patterns n Modified Bunnell – Used for apposing tendons » Requires a high degree of closure strength – Uses nonabsorbable suture – Uses a single-armed suture
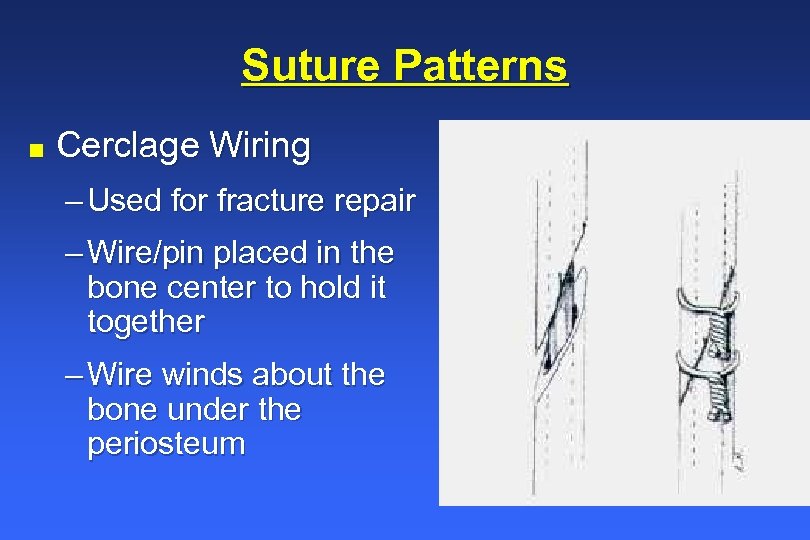 Suture Patterns n Cerclage Wiring – Used for fracture repair – Wire/pin placed in the bone center to hold it together – Wire winds about the bone under the periosteum
Suture Patterns n Cerclage Wiring – Used for fracture repair – Wire/pin placed in the bone center to hold it together – Wire winds about the bone under the periosteum
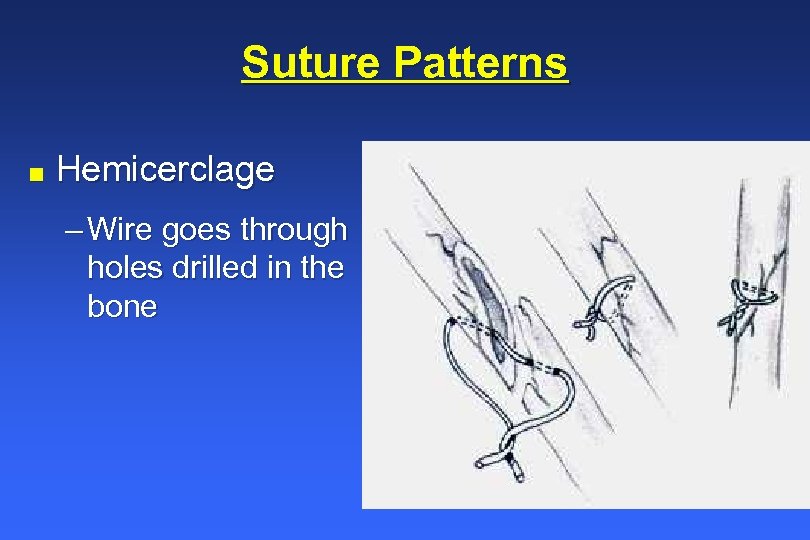 Suture Patterns n Hemicerclage – Wire goes through holes drilled in the bone
Suture Patterns n Hemicerclage – Wire goes through holes drilled in the bone
 Suture Patterns for Specific Tissues n n Skin- simple interrupted, horizontal mattress, vertical mattress, continuous apposing or everting Subcutaneous tissue- simple continuous Fascia- simple continuous (primary), simple interrupted, vertical mattress, far-near, near-far, Mayo mattress Peritoneum- simple continuous (two-layer), and simple interrupted – Very thin and fragile in horse, close muscle instead
Suture Patterns for Specific Tissues n n Skin- simple interrupted, horizontal mattress, vertical mattress, continuous apposing or everting Subcutaneous tissue- simple continuous Fascia- simple continuous (primary), simple interrupted, vertical mattress, far-near, near-far, Mayo mattress Peritoneum- simple continuous (two-layer), and simple interrupted – Very thin and fragile in horse, close muscle instead
 Suture Patterns n Vessels- simple interrupted and simple continuous n Viscera- direct appositional Cushing suture n Muscle- simple continuous, simple interrupted, and horizontal mattress n Tendons- Bunnell n Bone- hemicerclage and cerclage
Suture Patterns n Vessels- simple interrupted and simple continuous n Viscera- direct appositional Cushing suture n Muscle- simple continuous, simple interrupted, and horizontal mattress n Tendons- Bunnell n Bone- hemicerclage and cerclage
 References n § Clinical Textbook for Veterinary Technicians; Mc. Curnin, D. M. ; W. B. Saunders Co. , Philadelphia, 1994 Ethicon Wound Closure Manual; Available at http: //www. ethiconinc. com/wound_management/procedure/w ound/ Fundamental techniques in Veterinary Surgery; Knecht, C. D. ; Allen, A. R. ; Williams, D. J. : Johnson, J. H. ; W. B. Saunders Philadelphia, 1981 Davis + Geck Veterinary Suture Manual, 1991
References n § Clinical Textbook for Veterinary Technicians; Mc. Curnin, D. M. ; W. B. Saunders Co. , Philadelphia, 1994 Ethicon Wound Closure Manual; Available at http: //www. ethiconinc. com/wound_management/procedure/w ound/ Fundamental techniques in Veterinary Surgery; Knecht, C. D. ; Allen, A. R. ; Williams, D. J. : Johnson, J. H. ; W. B. Saunders Philadelphia, 1981 Davis + Geck Veterinary Suture Manual, 1991


