0d796e9d5f1a05ccbf1fd173aa2f6b59.ppt
- Количество слайдов: 30
 Workshop on Country Perspectives on Decision Making for control of chronic diseases Institute of Medicine of the National Academies July 19 -21, 2011 One. Health for Strategic Planning and Costing A tool developed by the UN Inter-Agency Working Group on Costing Karin Stenberg WHO Health Systems Financing Department (WHO/HSF)
Workshop on Country Perspectives on Decision Making for control of chronic diseases Institute of Medicine of the National Academies July 19 -21, 2011 One. Health for Strategic Planning and Costing A tool developed by the UN Inter-Agency Working Group on Costing Karin Stenberg WHO Health Systems Financing Department (WHO/HSF)
 UN costing tools: Background l To date UN agencies have supported the development of numerous costing tools for health programmes. l Inter-Agency Working Group on Costing established in 2008 (WHO, UNICEF, WB, UNAIDS, UNFPA, UNDP) l A User's meeting in Senegal reviewed 13 commonly used tools. Recommendations from countries (users): – Request for standardised approaches across UN agencies – Request for joint UN tools for MDG planning – Harmonised technical support
UN costing tools: Background l To date UN agencies have supported the development of numerous costing tools for health programmes. l Inter-Agency Working Group on Costing established in 2008 (WHO, UNICEF, WB, UNAIDS, UNFPA, UNDP) l A User's meeting in Senegal reviewed 13 commonly used tools. Recommendations from countries (users): – Request for standardised approaches across UN agencies – Request for joint UN tools for MDG planning – Harmonised technical support
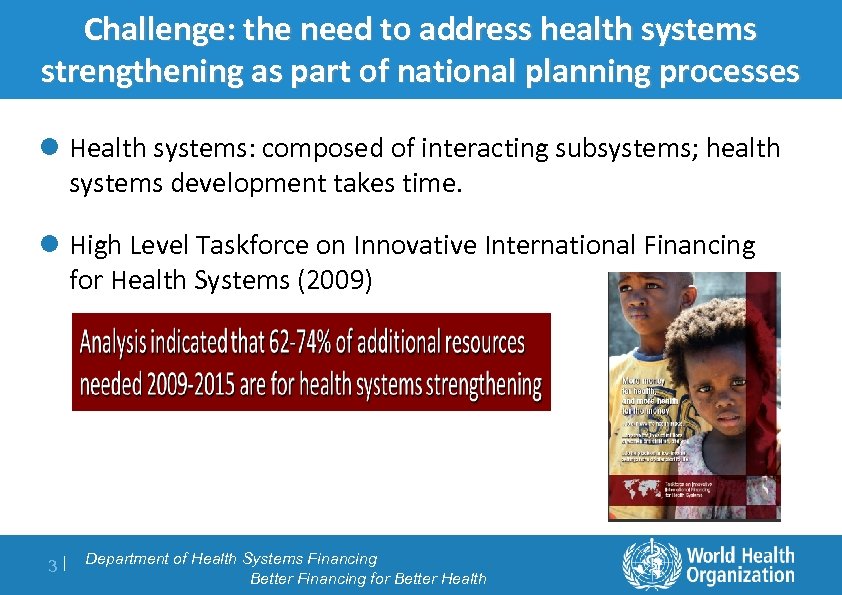 Challenge: the need to address health systems Context planning processes strengthening as part of national l Health systems: composed of interacting subsystems; health systems development takes time. l High Level Taskforce on Innovative International Financing for Health Systems (2009) 3| Department of Health Systems Financing Better Financing for Better Health
Challenge: the need to address health systems Context planning processes strengthening as part of national l Health systems: composed of interacting subsystems; health systems development takes time. l High Level Taskforce on Innovative International Financing for Health Systems (2009) 3| Department of Health Systems Financing Better Financing for Better Health
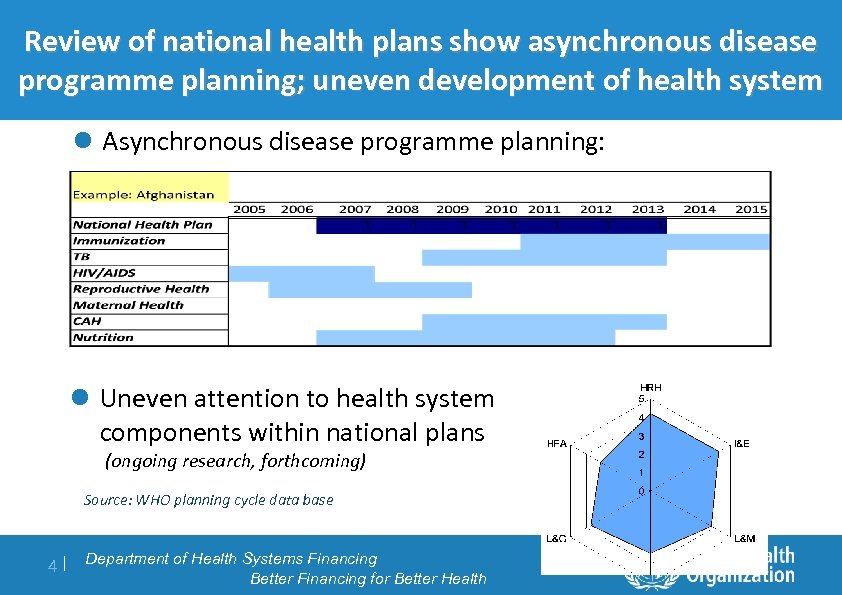 Review of national health. Context asynchronous disease plans show programme planning; uneven development of health system l Asynchronous disease programme planning: l Uneven attention to health system components within national plans (ongoing research, forthcoming) Source: WHO planning cycle data base 4| Department of Health Systems Financing Better Financing for Better Health
Review of national health. Context asynchronous disease plans show programme planning; uneven development of health system l Asynchronous disease programme planning: l Uneven attention to health system components within national plans (ongoing research, forthcoming) Source: WHO planning cycle data base 4| Department of Health Systems Financing Better Financing for Better Health
 One. Health: purpose and audience l A tool to support processes for medium term (3 -10 years) health systems to planning at country level l Covers the national health sector, with focus on public sector health interventions. Allows for incorporating activities in private sector and costing of selected non-health sector activities that may have health impacts. l Intended audience: – Health Sector planners (department of planning, Ministry of Health) – Disease-specific programme planners (e. g. EPI, Malaria) , Health System component (e. g. , Human Resource Department in Mo. H) – NGOs and other agencies in countries – Donors, academe and UN agencies 5| Department of Health Systems Financing Better Financing for Better Health
One. Health: purpose and audience l A tool to support processes for medium term (3 -10 years) health systems to planning at country level l Covers the national health sector, with focus on public sector health interventions. Allows for incorporating activities in private sector and costing of selected non-health sector activities that may have health impacts. l Intended audience: – Health Sector planners (department of planning, Ministry of Health) – Disease-specific programme planners (e. g. EPI, Malaria) , Health System component (e. g. , Human Resource Department in Mo. H) – NGOs and other agencies in countries – Donors, academe and UN agencies 5| Department of Health Systems Financing Better Financing for Better Health
 One. Health development process Wide stakeholder engagement process l Inter-Agency Working Group on Costing (IAWG-COSTING) established in 2008 (WHO, UNICEF, WB, UNAIDS, UNFPA, UNDP). l The Global Fund to fight Aids, TB and Malaria, The Global Health Workforce Alliance, The Health Metrics Network, Bilateral agencies, IHP+, have provided funding and technical support; other partners: UNIFEM and projects like USAID deliver, Optimize provide technical inputs l Health Planners in Country Reference Group provide technical and user related inputs into model development (Burkina Faso, Cap Vert, Ghana, Mali, Mauretania). 6| Department of Health Systems Financing Better Financing for Better Health
One. Health development process Wide stakeholder engagement process l Inter-Agency Working Group on Costing (IAWG-COSTING) established in 2008 (WHO, UNICEF, WB, UNAIDS, UNFPA, UNDP). l The Global Fund to fight Aids, TB and Malaria, The Global Health Workforce Alliance, The Health Metrics Network, Bilateral agencies, IHP+, have provided funding and technical support; other partners: UNIFEM and projects like USAID deliver, Optimize provide technical inputs l Health Planners in Country Reference Group provide technical and user related inputs into model development (Burkina Faso, Cap Vert, Ghana, Mali, Mauretania). 6| Department of Health Systems Financing Better Financing for Better Health
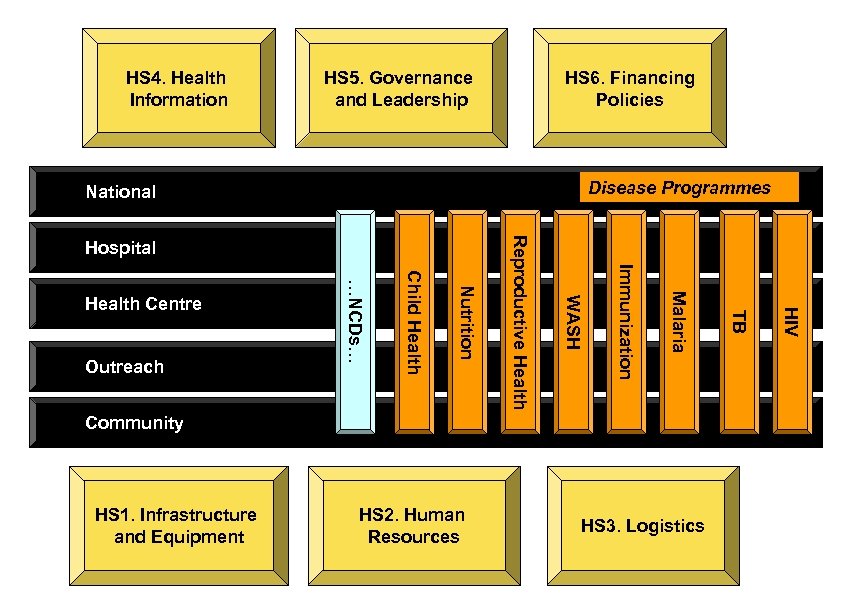 HS 4. Health Information HS 5. Governance and Leadership HS 6. Financing Policies Disease Programmes National HS 1. Infrastructure and Equipment HS 2. Human Resources HS 3. Logistics HIV Community TB Malaria Immunization WASH Nutrition Child Health Outreach …NCDs… Health Centre Reproductive Health Hospital
HS 4. Health Information HS 5. Governance and Leadership HS 6. Financing Policies Disease Programmes National HS 1. Infrastructure and Equipment HS 2. Human Resources HS 3. Logistics HIV Community TB Malaria Immunization WASH Nutrition Child Health Outreach …NCDs… Health Centre Reproductive Health Hospital
 One. Health : what is new and better? #1 l Unified model in 3 aspects: – Planning, Costing, Budgeting, impact analysis, financial space analysis. – Bringing disease programme planning and health systems planning together – One UN l Aligned with Joint Assessment of National Strategies (JANS) principles on situation analysis, informed priority setting, and financial sustainability considerations. l Incorporates UN epidemiology impact models to demonstrate the achievable health gains, e. g. , Lives Saved Tool (Li. ST), AIM; with new modules developed where there was previously a gap, e. g. , TB impact. l Programme planning is carried out within a framework of: – Health system capacity assessment – Financial sustainability assessment 8| Department of Health Systems Financing Better Financing for Better Health
One. Health : what is new and better? #1 l Unified model in 3 aspects: – Planning, Costing, Budgeting, impact analysis, financial space analysis. – Bringing disease programme planning and health systems planning together – One UN l Aligned with Joint Assessment of National Strategies (JANS) principles on situation analysis, informed priority setting, and financial sustainability considerations. l Incorporates UN epidemiology impact models to demonstrate the achievable health gains, e. g. , Lives Saved Tool (Li. ST), AIM; with new modules developed where there was previously a gap, e. g. , TB impact. l Programme planning is carried out within a framework of: – Health system capacity assessment – Financial sustainability assessment 8| Department of Health Systems Financing Better Financing for Better Health
 One. Health : what is new and better? #2 l User friendly interface closely resembles the formats and structures of existing tools, thus allowing transfer of skills from old tools l The tool is modular in format and can easily be adapted to different country contexts l Allowing for flexibility within a structure and language that corresponds to the ways in which real world health care system planning is performed. l User can choose the level of detail for planning, down to ingredients based, population-based costing; provided with default values from UN health statistics databases l Software updated on a regular basis including recent updates of epidemiology impact models. l Direct links and checks are built in between different modules, allowing for real time integrated planning discussions. 9| Department of Health Systems Financing Better Financing for Better Health
One. Health : what is new and better? #2 l User friendly interface closely resembles the formats and structures of existing tools, thus allowing transfer of skills from old tools l The tool is modular in format and can easily be adapted to different country contexts l Allowing for flexibility within a structure and language that corresponds to the ways in which real world health care system planning is performed. l User can choose the level of detail for planning, down to ingredients based, population-based costing; provided with default values from UN health statistics databases l Software updated on a regular basis including recent updates of epidemiology impact models. l Direct links and checks are built in between different modules, allowing for real time integrated planning discussions. 9| Department of Health Systems Financing Better Financing for Better Health
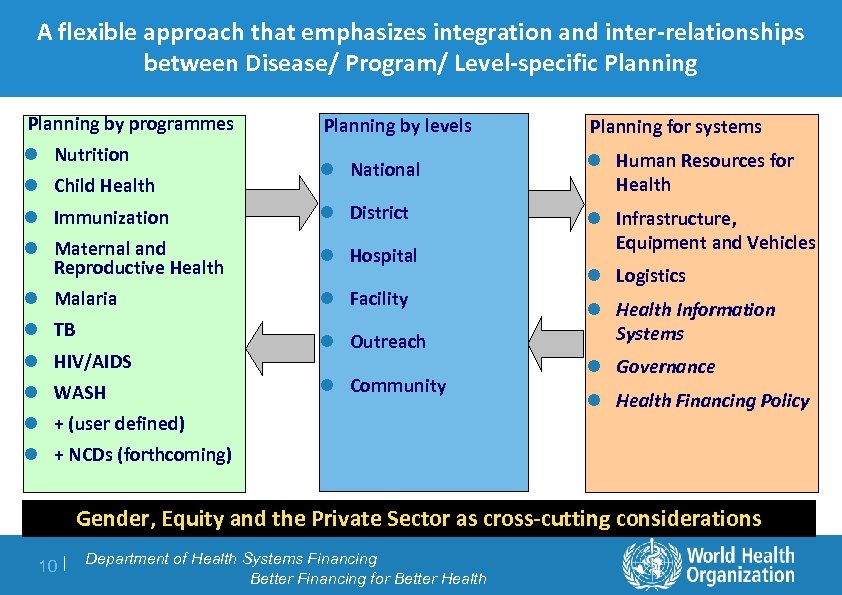 A flexible approach that emphasizes integration and inter-relationships between Disease/ Program/ Level-specific Planning by programmes Planning by levels Planning for systems l National l Human Resources for Health l Immunization l District l Maternal and Reproductive Health l Hospital l Infrastructure, Equipment and Vehicles l Malaria l Facility l Nutrition l Child Health l TB l HIV/AIDS l WASH l Outreach l Community l + (user defined) l Logistics l Health Information Systems l Governance l Health Financing Policy l + NCDs (forthcoming) Gender, Equity and the Private Sector as cross-cutting considerations 10 | Department of Health Systems Financing Better Financing for Better Health
A flexible approach that emphasizes integration and inter-relationships between Disease/ Program/ Level-specific Planning by programmes Planning by levels Planning for systems l National l Human Resources for Health l Immunization l District l Maternal and Reproductive Health l Hospital l Infrastructure, Equipment and Vehicles l Malaria l Facility l Nutrition l Child Health l TB l HIV/AIDS l WASH l Outreach l Community l + (user defined) l Logistics l Health Information Systems l Governance l Health Financing Policy l + NCDs (forthcoming) Gender, Equity and the Private Sector as cross-cutting considerations 10 | Department of Health Systems Financing Better Financing for Better Health
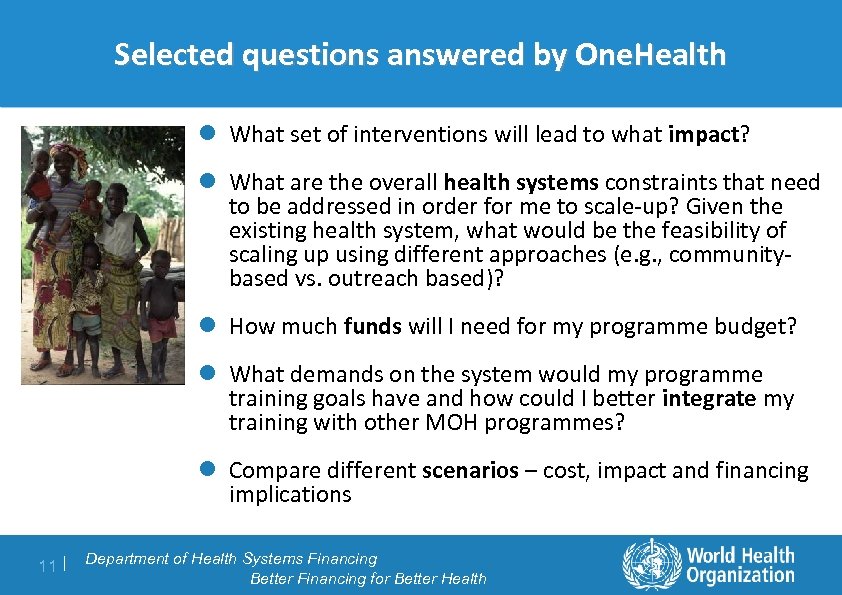 Selected questions answered by One. Health l What set of interventions will lead to what impact? l What are the overall health systems constraints that need to be addressed in order for me to scale-up? Given the existing health system, what would be the feasibility of scaling up using different approaches (e. g. , communitybased vs. outreach based)? l How much funds will I need for my programme budget? l What demands on the system would my programme training goals have and how could I better integrate my training with other MOH programmes? l Compare different scenarios – cost, impact and financing implications 11 | Department of Health Systems Financing Better Financing for Better Health
Selected questions answered by One. Health l What set of interventions will lead to what impact? l What are the overall health systems constraints that need to be addressed in order for me to scale-up? Given the existing health system, what would be the feasibility of scaling up using different approaches (e. g. , communitybased vs. outreach based)? l How much funds will I need for my programme budget? l What demands on the system would my programme training goals have and how could I better integrate my training with other MOH programmes? l Compare different scenarios – cost, impact and financing implications 11 | Department of Health Systems Financing Better Financing for Better Health
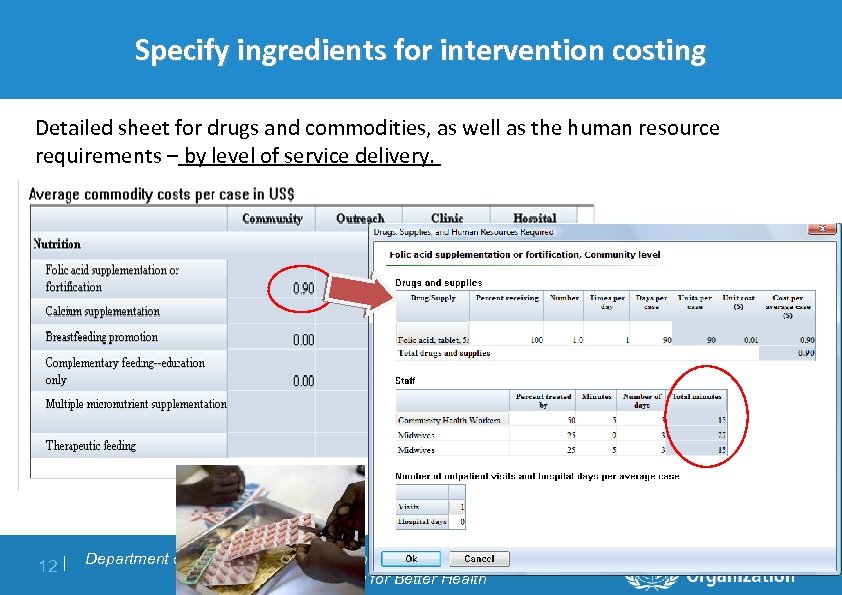 Specify ingredients for intervention costing Detailed sheet for drugs and commodities, as well as the human resource requirements – by level of service delivery. 12 | Department of Health Systems Financing Better Financing for Better Health
Specify ingredients for intervention costing Detailed sheet for drugs and commodities, as well as the human resource requirements – by level of service delivery. 12 | Department of Health Systems Financing Better Financing for Better Health
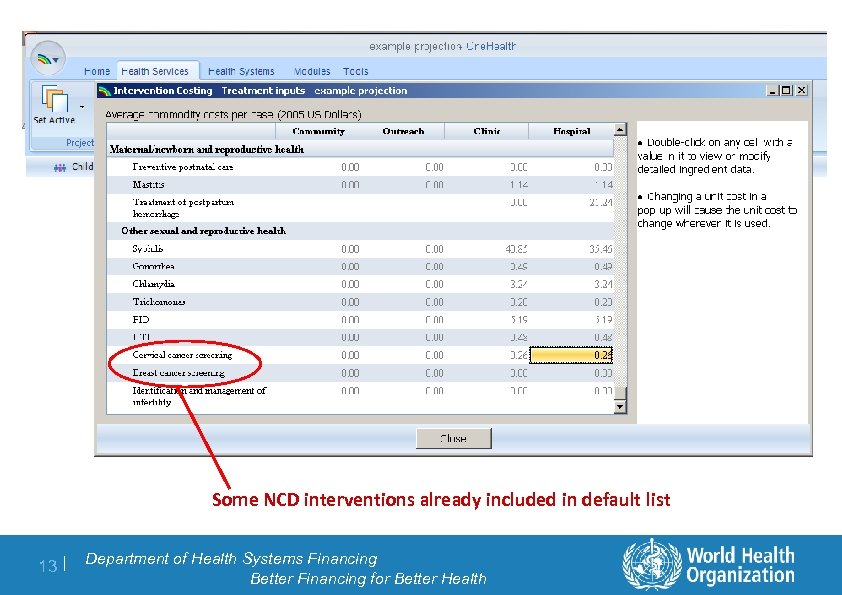 Some NCD interventions already included in default list 13 | Department of Health Systems Financing Better Financing for Better Health
Some NCD interventions already included in default list 13 | Department of Health Systems Financing Better Financing for Better Health
 Bottom-up detailed estimation of cost for activities to support the national programme l Programme-Specific staff l Training l Supervision l Monitoring & Evaluation l Infrastructure & Equipment l Transport l Communication, Media & Outreach l Demand generation l Advocacy l General Programme Management l Technical Assistance 14 | Department of Health Systems Financing Better Financing for Better Health
Bottom-up detailed estimation of cost for activities to support the national programme l Programme-Specific staff l Training l Supervision l Monitoring & Evaluation l Infrastructure & Equipment l Transport l Communication, Media & Outreach l Demand generation l Advocacy l General Programme Management l Technical Assistance 14 | Department of Health Systems Financing Better Financing for Better Health
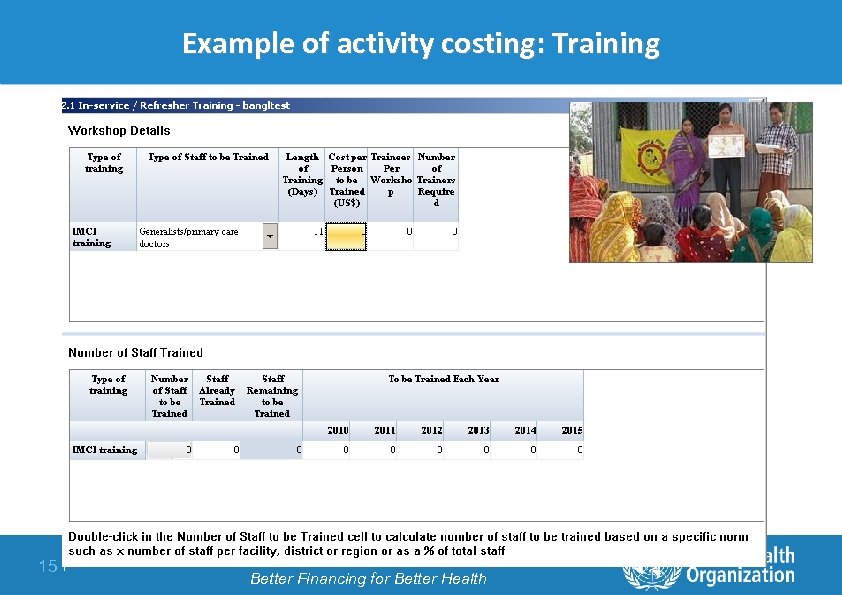 Example of activity costing: Training 15 | Department of Health Systems Financing Better Financing for Better Health
Example of activity costing: Training 15 | Department of Health Systems Financing Better Financing for Better Health
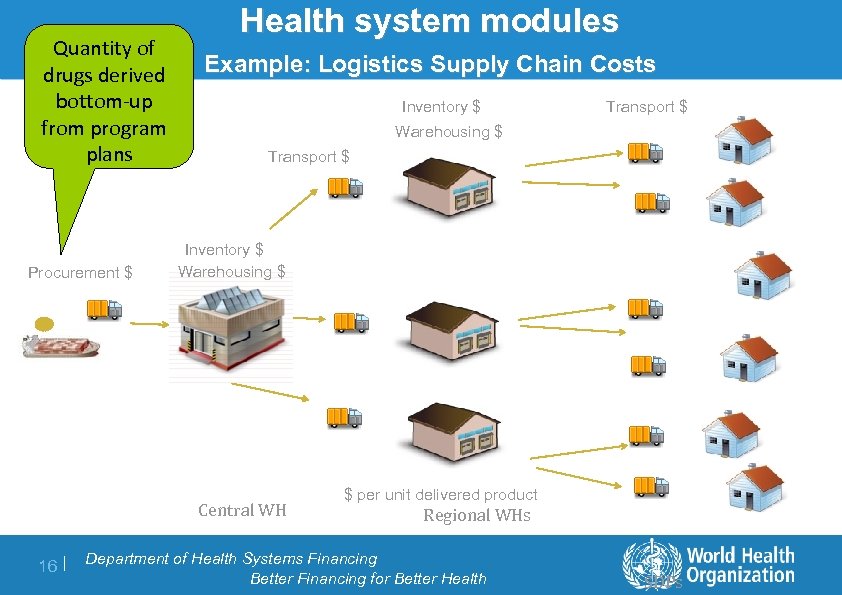 Quantity of drugs derived bottom-up from program plans Procurement $ Health system modules Example: Logistics Supply Chain Costs Inventory $ Warehousing $ Transport $ Inventory $ Warehousing $ Central WH 16 | Transport $ $ per unit delivered product Regional WHs Department of Health Systems Financing Better Financing for Better Health SDPs
Quantity of drugs derived bottom-up from program plans Procurement $ Health system modules Example: Logistics Supply Chain Costs Inventory $ Warehousing $ Transport $ Inventory $ Warehousing $ Central WH 16 | Transport $ $ per unit delivered product Regional WHs Department of Health Systems Financing Better Financing for Better Health SDPs
 Assessing impact on health systems and opportunities for integration 17 | Department of Health Systems Financing Better Financing for Better Health
Assessing impact on health systems and opportunities for integration 17 | Department of Health Systems Financing Better Financing for Better Health
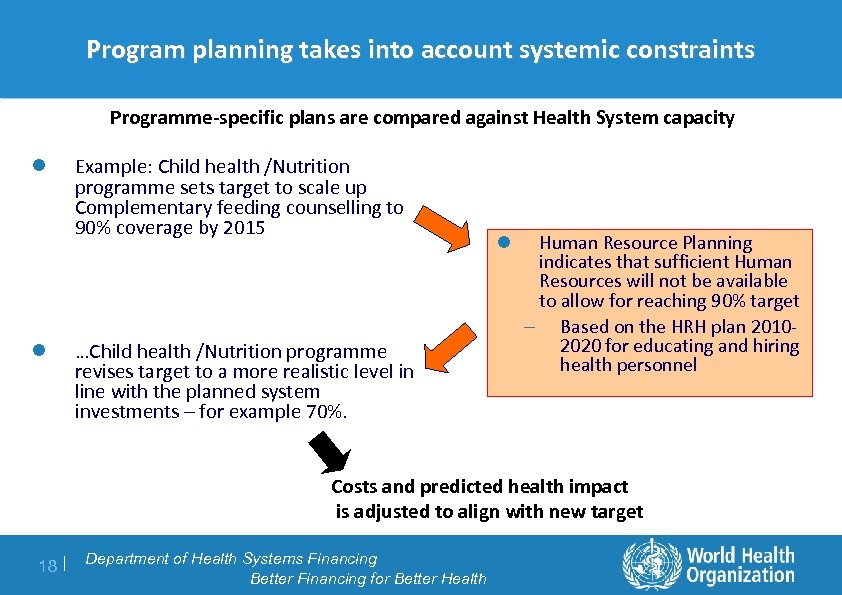 Program planning takes into account systemic constraints Programme-specific plans are compared against Health System capacity l l Example: Child health /Nutrition programme sets target to scale up Complementary feeding counselling to 90% coverage by 2015 …Child health /Nutrition programme revises target to a more realistic level in line with the planned system investments – for example 70%. l Human Resource Planning indicates that sufficient Human Resources will not be available to allow for reaching 90% target – Based on the HRH plan 20102020 for educating and hiring health personnel Costs and predicted health impact is adjusted to align with new target 18 | Department of Health Systems Financing Better Financing for Better Health
Program planning takes into account systemic constraints Programme-specific plans are compared against Health System capacity l l Example: Child health /Nutrition programme sets target to scale up Complementary feeding counselling to 90% coverage by 2015 …Child health /Nutrition programme revises target to a more realistic level in line with the planned system investments – for example 70%. l Human Resource Planning indicates that sufficient Human Resources will not be available to allow for reaching 90% target – Based on the HRH plan 20102020 for educating and hiring health personnel Costs and predicted health impact is adjusted to align with new target 18 | Department of Health Systems Financing Better Financing for Better Health
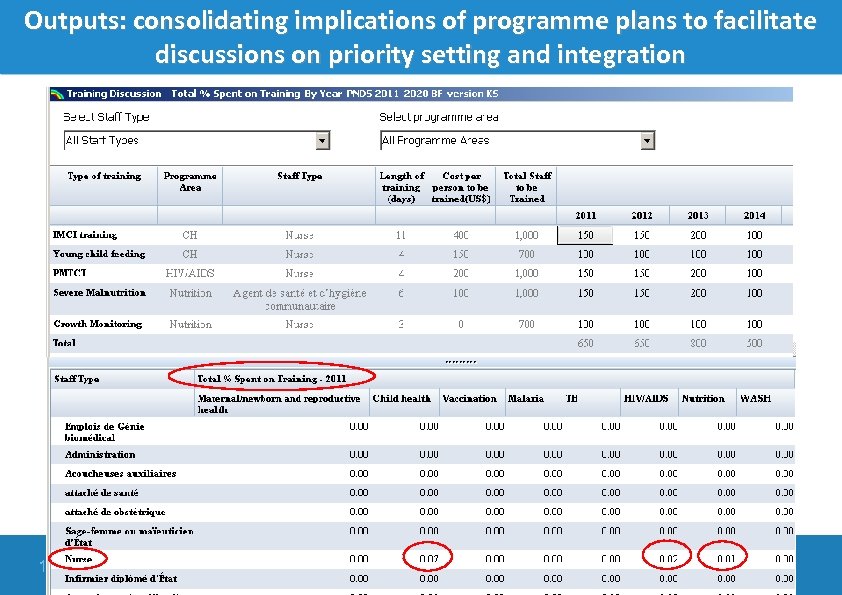 Outputs: consolidating implications of programme plans to facilitate discussions on priority setting and integration 19 | Department of Health Systems Financing Better Financing for Better Health
Outputs: consolidating implications of programme plans to facilitate discussions on priority setting and integration 19 | Department of Health Systems Financing Better Financing for Better Health
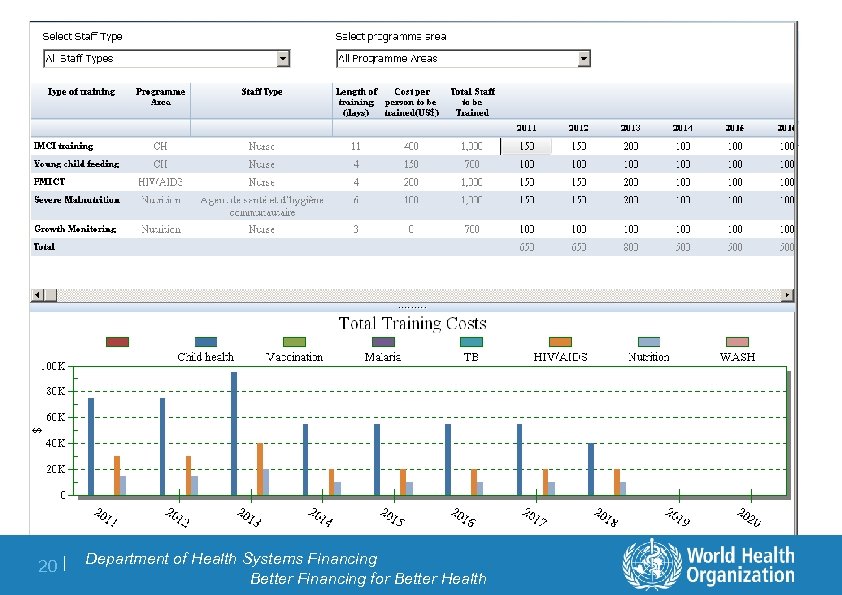 20 | Department of Health Systems Financing Better Financing for Better Health
20 | Department of Health Systems Financing Better Financing for Better Health
 Mapping costs to the national budget classification 21 | Department of Health Systems Financing Better Financing for Better Health
Mapping costs to the national budget classification 21 | Department of Health Systems Financing Better Financing for Better Health
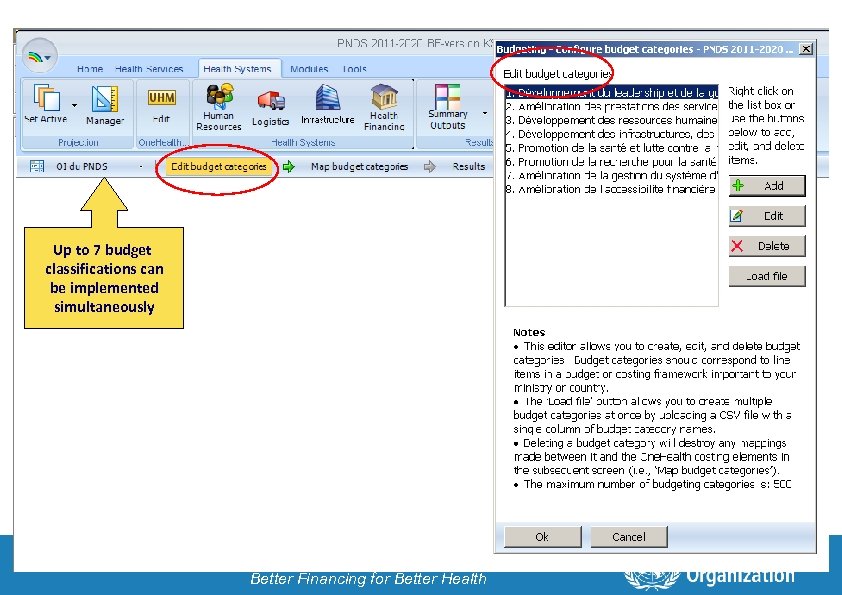 Up to 7 budget classifications can be implemented simultaneously 22 | Department of Health Systems Financing Better Financing for Better Health
Up to 7 budget classifications can be implemented simultaneously 22 | Department of Health Systems Financing Better Financing for Better Health
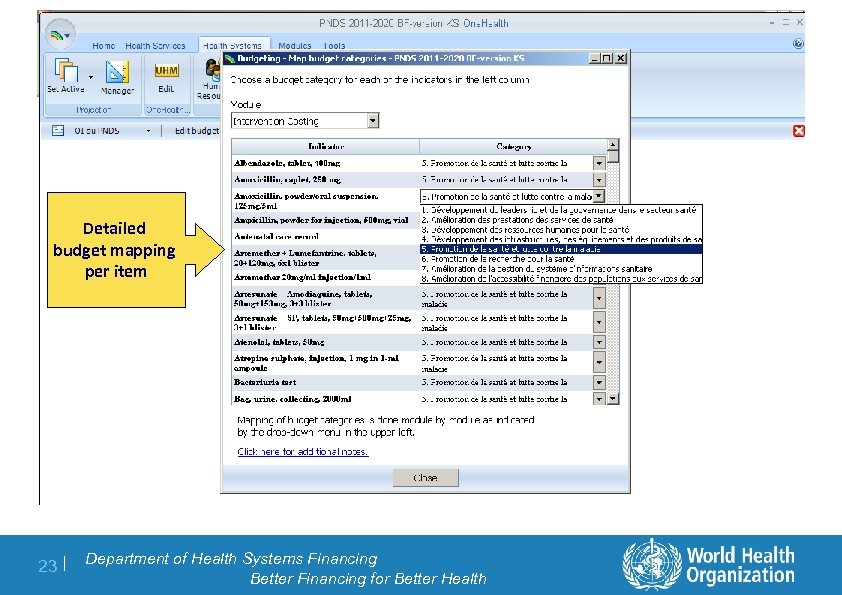 Detailed budget mapping per item 23 | Department of Health Systems Financing Better Financing for Better Health
Detailed budget mapping per item 23 | Department of Health Systems Financing Better Financing for Better Health
 Looking at financial sustainability and opportunities for increasing financial (and fiscal) space 24 | Department of Health Systems Financing Better Financing for Better Health
Looking at financial sustainability and opportunities for increasing financial (and fiscal) space 24 | Department of Health Systems Financing Better Financing for Better Health
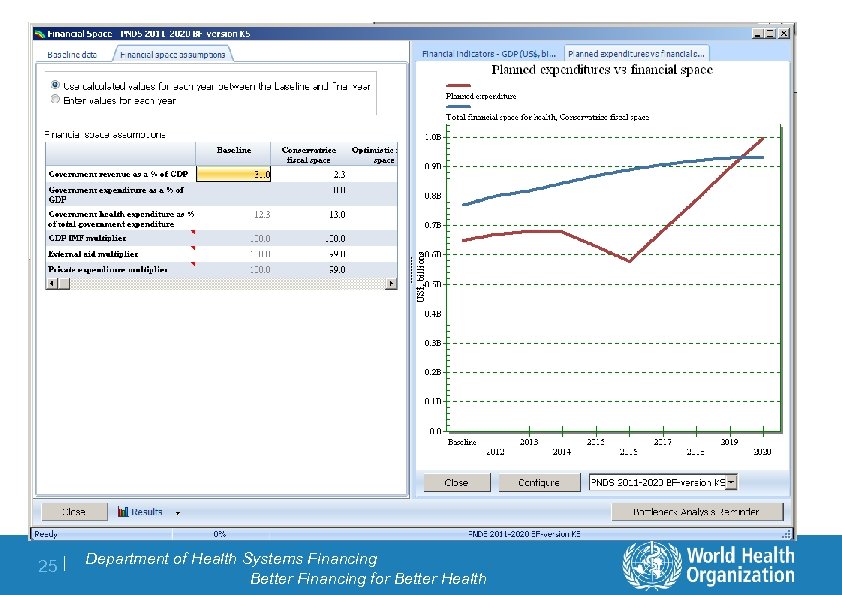 25 | Department of Health Systems Financing Better Financing for Better Health
25 | Department of Health Systems Financing Better Financing for Better Health
 Strengths and Opportunities: utility for policy makers l Giving national programmes a common platform where consistent methods are used across programme areas l Ensuring that health system capacity is driving the planning process, set realistic goals l Health impact and other criteria to drive priority setting process l Provides a check list function, promote comprehensiveness and inclusiveness l Bringing NCDs into the mainstream planning process for national strategic health plans 26 | Department of Health Systems Financing Better Financing for Better Health
Strengths and Opportunities: utility for policy makers l Giving national programmes a common platform where consistent methods are used across programme areas l Ensuring that health system capacity is driving the planning process, set realistic goals l Health impact and other criteria to drive priority setting process l Provides a check list function, promote comprehensiveness and inclusiveness l Bringing NCDs into the mainstream planning process for national strategic health plans 26 | Department of Health Systems Financing Better Financing for Better Health
 Challenges l Data requirements l Strengthening health information systems l Building capacity to use strategic planning tools to inform the decision making process 27 | Department of Health Systems Financing Better Financing for Better Health
Challenges l Data requirements l Strengthening health information systems l Building capacity to use strategic planning tools to inform the decision making process 27 | Department of Health Systems Financing Better Financing for Better Health
 Next steps: roll out and capacity building (a) Desk review; test application on costed national health plans (ongoing) (b) Roll out of One. Health version 1. 0 September 2011 • MDG programme planning • HSS modules for HRH, Infrastructure, Logistics + some financing and HIS • Budgeting and financial space • Health impact (c) Early Implementation (3 countries) (d) Roll out of One. Health version 2. 0 October/November 2011 – Added modules for NCD costing, Health Information Systems (e) Further development expected (2012 onwards) - Model to be continuously refined as new evidence available - Develop models for projecting health gains from NCDs, adult malaria 28 | Department of Health Systems Financing Better Financing for Better Health
Next steps: roll out and capacity building (a) Desk review; test application on costed national health plans (ongoing) (b) Roll out of One. Health version 1. 0 September 2011 • MDG programme planning • HSS modules for HRH, Infrastructure, Logistics + some financing and HIS • Budgeting and financial space • Health impact (c) Early Implementation (3 countries) (d) Roll out of One. Health version 2. 0 October/November 2011 – Added modules for NCD costing, Health Information Systems (e) Further development expected (2012 onwards) - Model to be continuously refined as new evidence available - Develop models for projecting health gains from NCDs, adult malaria 28 | Department of Health Systems Financing Better Financing for Better Health
 Summary recommendations for designing and applying a costing model as part of an NCD tool kit l Design: be clear on the specific policy question(s) to be answered; how the tool(s) will be used and by whom. l Design: opting out of a silo approach: consider broader health sector planning processes and how to cost integration across programmes. l Need to invest as much in training, application, validation, proof of concept studies, communication and advocacy as in development of tools; to ensure their use for the intended purpose. 29 | Department of Health Systems Financing Better Financing for Better Health
Summary recommendations for designing and applying a costing model as part of an NCD tool kit l Design: be clear on the specific policy question(s) to be answered; how the tool(s) will be used and by whom. l Design: opting out of a silo approach: consider broader health sector planning processes and how to cost integration across programmes. l Need to invest as much in training, application, validation, proof of concept studies, communication and advocacy as in development of tools; to ensure their use for the intended purpose. 29 | Department of Health Systems Financing Better Financing for Better Health
 Thank you 30 | Department of Health Systems Financing Better Financing for Better Health
Thank you 30 | Department of Health Systems Financing Better Financing for Better Health


