b6135a0c2ffa212c74385d8ccd132cb0.ppt
- Количество слайдов: 46
 Workforce Development in Sexual Health Dr Anne Mc. Nall Senior Lecturer, Continuing Professional Development Pathway Leader – Sexual Health
Workforce Development in Sexual Health Dr Anne Mc. Nall Senior Lecturer, Continuing Professional Development Pathway Leader – Sexual Health
 The North East
The North East
 Newcastle Quayside
Newcastle Quayside
 Alnwick Castle
Alnwick Castle

 Aims • To summarise the national problem of sexual health nursing workforce development • To share the Sexual Health Integrated Nurse Education (SHINE) workforce development model to support service integration in sexual health – The SHINE model – The practice educator posts – Implementation of the SHINE model • To evaluate the usefulness and transferability of this model for your own area • To update you on plans and progress for workforce development in the South West
Aims • To summarise the national problem of sexual health nursing workforce development • To share the Sexual Health Integrated Nurse Education (SHINE) workforce development model to support service integration in sexual health – The SHINE model – The practice educator posts – Implementation of the SHINE model • To evaluate the usefulness and transferability of this model for your own area • To update you on plans and progress for workforce development in the South West
 The background and context
The background and context
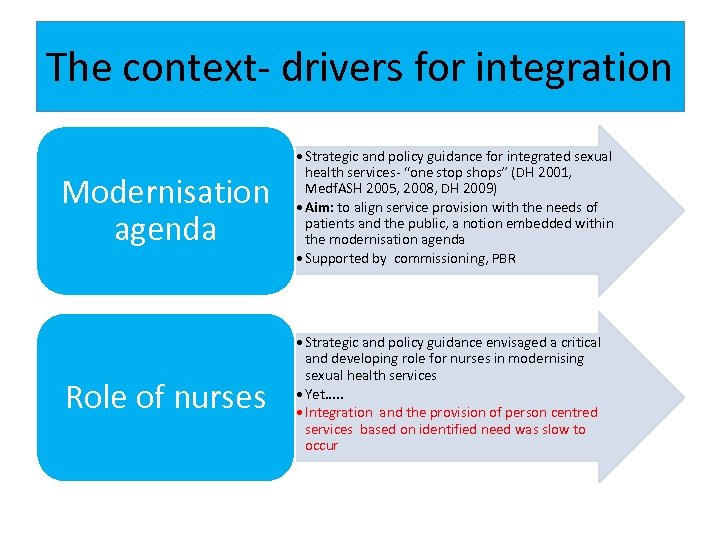 The context- drivers for integration Modernisation agenda • Strategic and policy guidance for integrated sexual health services- “one stop shops” (DH 2001, Medf. ASH 2005, 2008, DH 2009) • Aim: to align service provision with the needs of patients and the public, a notion embedded within the modernisation agenda • Supported by commissioning, PBR Role of nurses • Strategic and policy guidance envisaged a critical and developing role for nurses in modernising sexual health services • Yet. . . • Integration and the provision of person centred services based on identified need was slow to occur
The context- drivers for integration Modernisation agenda • Strategic and policy guidance for integrated sexual health services- “one stop shops” (DH 2001, Medf. ASH 2005, 2008, DH 2009) • Aim: to align service provision with the needs of patients and the public, a notion embedded within the modernisation agenda • Supported by commissioning, PBR Role of nurses • Strategic and policy guidance envisaged a critical and developing role for nurses in modernising sexual health services • Yet. . . • Integration and the provision of person centred services based on identified need was slow to occur
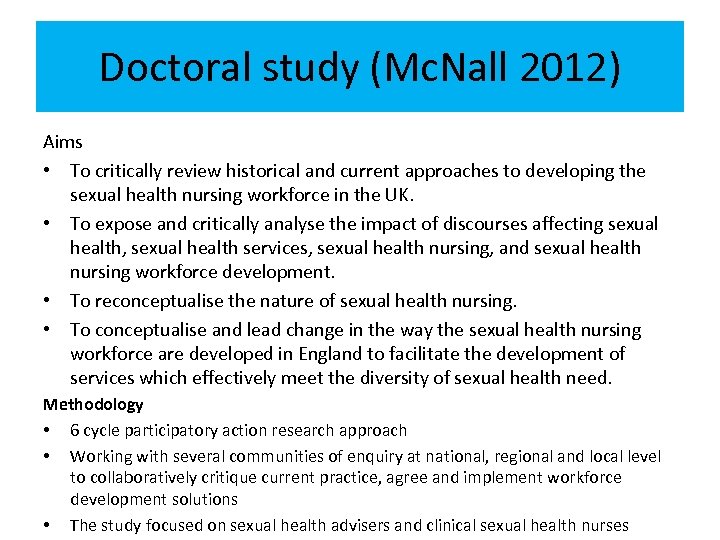 Doctoral study (Mc. Nall 2012) Aims • To critically review historical and current approaches to developing the sexual health nursing workforce in the UK. • To expose and critically analyse the impact of discourses affecting sexual health, sexual health services, sexual health nursing, and sexual health nursing workforce development. • To reconceptualise the nature of sexual health nursing. • To conceptualise and lead change in the way the sexual health nursing workforce are developed in England to facilitate the development of services which effectively meet the diversity of sexual health need. Methodology • 6 cycle participatory action research approach • Working with several communities of enquiry at national, regional and local level to collaboratively critique current practice, agree and implement workforce development solutions • The study focused on sexual health advisers and clinical sexual health nurses
Doctoral study (Mc. Nall 2012) Aims • To critically review historical and current approaches to developing the sexual health nursing workforce in the UK. • To expose and critically analyse the impact of discourses affecting sexual health, sexual health services, sexual health nursing, and sexual health nursing workforce development. • To reconceptualise the nature of sexual health nursing. • To conceptualise and lead change in the way the sexual health nursing workforce are developed in England to facilitate the development of services which effectively meet the diversity of sexual health need. Methodology • 6 cycle participatory action research approach • Working with several communities of enquiry at national, regional and local level to collaboratively critique current practice, agree and implement workforce development solutions • The study focused on sexual health advisers and clinical sexual health nurses
 Models of integration • 3 levels of integration – Integration at provider level (one practitioner providing a complete package of care) – Integration at facility level (internal referral, which may or not occur at the time of the visit) – Referral model ( no integration but effective referral linkages between services) – Church & Mayhew (2009) • Integration at provider level is the preferred model under QUIPP /PPI agenda- need the ability to holistically assess and respond to need
Models of integration • 3 levels of integration – Integration at provider level (one practitioner providing a complete package of care) – Integration at facility level (internal referral, which may or not occur at the time of the visit) – Referral model ( no integration but effective referral linkages between services) – Church & Mayhew (2009) • Integration at provider level is the preferred model under QUIPP /PPI agenda- need the ability to holistically assess and respond to need
 Barriers to integration • Lack of clarity and leadership to guide integration • Lack of integrated education and training for staff • Reliance on in-service training as opposed to education of staff prior to integration. • Medical hierarchies were identified as important constraints to the provision of integrated services and undermined attempts to shift from a task orientated model to a more holistic model of care (Church & Mayhew, 2009, pg 177, Mc. Nall , 2012)
Barriers to integration • Lack of clarity and leadership to guide integration • Lack of integrated education and training for staff • Reliance on in-service training as opposed to education of staff prior to integration. • Medical hierarchies were identified as important constraints to the provision of integrated services and undermined attempts to shift from a task orientated model to a more holistic model of care (Church & Mayhew, 2009, pg 177, Mc. Nall , 2012)
 Sexual health nursing • The art of nursing – “ the expert use and adaptation of empirical and metaphysical knowledge and values. It involves sensitively identifying need and adapting care to meet the needs of individual patients, and in the face of uncertainty, the discretionary use of creativity. It encompasses the ability to care for and care about the client, requiring an ability to work in partnership. ” (Fingfeld- Connett (2008) • Discourse analysis identified a need to move from the dominant medical model of sexual ill health to an emphasis on the nature and practice of sexual health nursing to assess and meet user need
Sexual health nursing • The art of nursing – “ the expert use and adaptation of empirical and metaphysical knowledge and values. It involves sensitively identifying need and adapting care to meet the needs of individual patients, and in the face of uncertainty, the discretionary use of creativity. It encompasses the ability to care for and care about the client, requiring an ability to work in partnership. ” (Fingfeld- Connett (2008) • Discourse analysis identified a need to move from the dominant medical model of sexual ill health to an emphasis on the nature and practice of sexual health nursing to assess and meet user need
 Analysis of the focus of previous CPD for SH • No national standard or benchmark; difficult to know what you are getting as an employer • Analysis of existing preparation; – Multiple modules required to cover all aspects of SH – time/ cost/ release issues – Many modular courses focused on knowledge with no practice competence – Where practice competence was included, reliance on practitioners to find their own assessor –quality and clinical governance issue? – Many in- house training courses developed - no accreditation/ quality assurance of learning – not transferable to other areas – Many courses do not meet DH (2002) Standards for SH education – attitudes, values, comfort, interpersonal skills • Need for preparation that develops competent practitioners – fit for practice • Most were theory only courses • Again, there was an emphasis in existing CPD on dominant medical model of sexual ill health
Analysis of the focus of previous CPD for SH • No national standard or benchmark; difficult to know what you are getting as an employer • Analysis of existing preparation; – Multiple modules required to cover all aspects of SH – time/ cost/ release issues – Many modular courses focused on knowledge with no practice competence – Where practice competence was included, reliance on practitioners to find their own assessor –quality and clinical governance issue? – Many in- house training courses developed - no accreditation/ quality assurance of learning – not transferable to other areas – Many courses do not meet DH (2002) Standards for SH education – attitudes, values, comfort, interpersonal skills • Need for preparation that develops competent practitioners – fit for practice • Most were theory only courses • Again, there was an emphasis in existing CPD on dominant medical model of sexual ill health
 Analysis of the current situation in practice. . . • Many skilled nurses employed in CASH, GUM, CSP • Most have specialist knowledge and skills in one (or more) aspect of sexual health practice • Some have dual qualifications/ competence but may not have used the skills in every day practice • Some primary care staff offering services, usually one aspect of sexual health • Some practitioners are coming new to the speciality • Highest academic level of practitioners very variable –some with little formal CPD in many years • Any new workforce development plan needed to accommodate all levels of knowledge/ experience, and recognise and accredit prior learning and competence.
Analysis of the current situation in practice. . . • Many skilled nurses employed in CASH, GUM, CSP • Most have specialist knowledge and skills in one (or more) aspect of sexual health practice • Some have dual qualifications/ competence but may not have used the skills in every day practice • Some primary care staff offering services, usually one aspect of sexual health • Some practitioners are coming new to the speciality • Highest academic level of practitioners very variable –some with little formal CPD in many years • Any new workforce development plan needed to accommodate all levels of knowledge/ experience, and recognise and accredit prior learning and competence.
 Is CPD effective? • Review of the literature on the effectiveness of continuing professional development programmes in nursing(Griscti & Jacono 2006) – Improved understanding – Often learning not implemented in practice – Deficit of evidence of effectiveness in developing practice and impact on practice outcomes • Need to think differently about preparation of the workforce
Is CPD effective? • Review of the literature on the effectiveness of continuing professional development programmes in nursing(Griscti & Jacono 2006) – Improved understanding – Often learning not implemented in practice – Deficit of evidence of effectiveness in developing practice and impact on practice outcomes • Need to think differently about preparation of the workforce
 Analysis of the current situation for universities • Want to provide CPD that both meets user need & is educationally robust • Essential to us in a competitive educational commissioning model • Many universities have had reduction or complete loss of CPD contracts • Needed partnership working to find a solution & maintain our business
Analysis of the current situation for universities • Want to provide CPD that both meets user need & is educationally robust • Essential to us in a competitive educational commissioning model • Many universities have had reduction or complete loss of CPD contracts • Needed partnership working to find a solution & maintain our business
 Workforce Development is. . “…a multi-faceted approach which addresses the range of factors impacting on the ability of the workforce to function with maximum effectiveness in responding to. . . problems. Workforce development should have a systems focus. Unlike traditional approaches, this is broad and comprehensive, targeting individual, organisational and structural factors, rather than just addressing education and training of individual mainstream workers”. Australia’s National Research Centre on Alcohol and other drugs Workforce Development (2002)
Workforce Development is. . “…a multi-faceted approach which addresses the range of factors impacting on the ability of the workforce to function with maximum effectiveness in responding to. . . problems. Workforce development should have a systems focus. Unlike traditional approaches, this is broad and comprehensive, targeting individual, organisational and structural factors, rather than just addressing education and training of individual mainstream workers”. Australia’s National Research Centre on Alcohol and other drugs Workforce Development (2002)
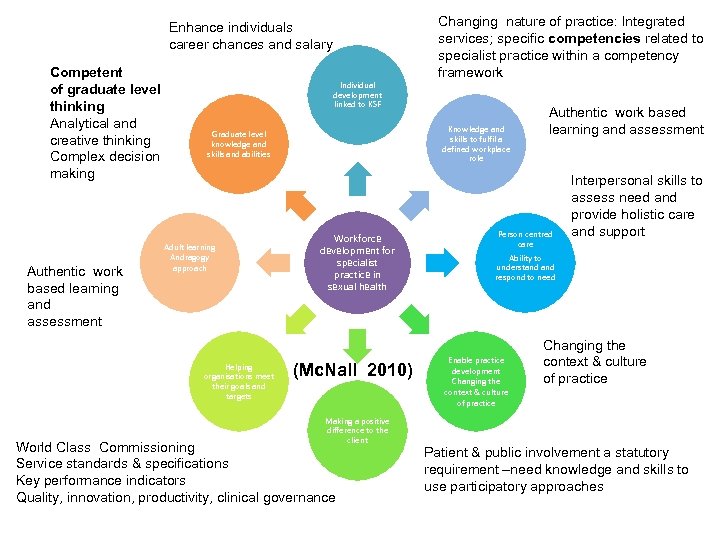 Enhance individuals career chances and salary Competent of graduate level thinking Analytical and creative thinking Complex decision making Authentic work based learning and assessment Individual development linked to KSF Knowledge and skills to fulfil a defined workplace role Graduate level knowledge and skills and abilities Adult learning Andragogy approach Helping organisations meet their goals and targets Changing nature of practice: Integrated services; specific competencies related to specialist practice within a competency framework Workforce development for specialist practice in sexual health (Mc. Nall 2010) Making a positive difference to the client World Class Commissioning Service standards & specifications Key performance indicators Quality, innovation, productivity, clinical governance Authentic work based learning and assessment Person centred care Interpersonal skills to assess need and provide holistic care and support Ability to understand respond to need Enable practice development Changing the context & culture of practice Patient & public involvement a statutory requirement –need knowledge and skills to use participatory approaches
Enhance individuals career chances and salary Competent of graduate level thinking Analytical and creative thinking Complex decision making Authentic work based learning and assessment Individual development linked to KSF Knowledge and skills to fulfil a defined workplace role Graduate level knowledge and skills and abilities Adult learning Andragogy approach Helping organisations meet their goals and targets Changing nature of practice: Integrated services; specific competencies related to specialist practice within a competency framework Workforce development for specialist practice in sexual health (Mc. Nall 2010) Making a positive difference to the client World Class Commissioning Service standards & specifications Key performance indicators Quality, innovation, productivity, clinical governance Authentic work based learning and assessment Person centred care Interpersonal skills to assess need and provide holistic care and support Ability to understand respond to need Enable practice development Changing the context & culture of practice Patient & public involvement a statutory requirement –need knowledge and skills to use participatory approaches
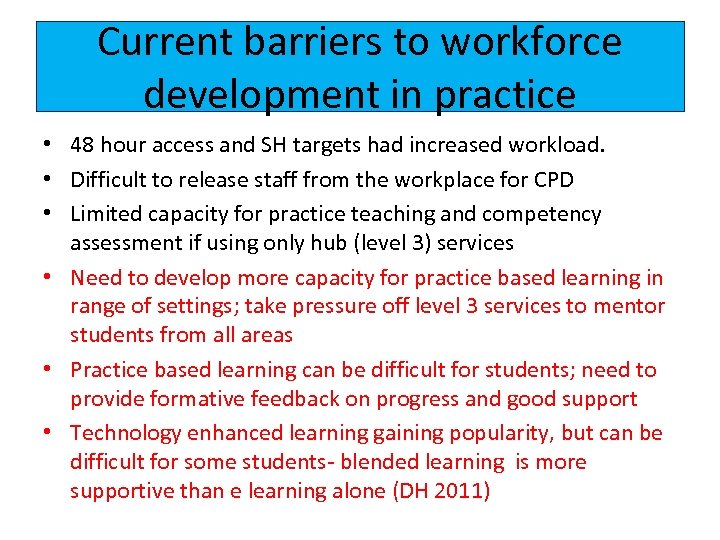 Current barriers to workforce development in practice • 48 hour access and SH targets had increased workload. • Difficult to release staff from the workplace for CPD • Limited capacity for practice teaching and competency assessment if using only hub (level 3) services • Need to develop more capacity for practice based learning in range of settings; take pressure off level 3 services to mentor students from all areas • Practice based learning can be difficult for students; need to provide formative feedback on progress and good support • Technology enhanced learning gaining popularity, but can be difficult for some students- blended learning is more supportive than e learning alone (DH 2011)
Current barriers to workforce development in practice • 48 hour access and SH targets had increased workload. • Difficult to release staff from the workplace for CPD • Limited capacity for practice teaching and competency assessment if using only hub (level 3) services • Need to develop more capacity for practice based learning in range of settings; take pressure off level 3 services to mentor students from all areas • Practice based learning can be difficult for students; need to provide formative feedback on progress and good support • Technology enhanced learning gaining popularity, but can be difficult for some students- blended learning is more supportive than e learning alone (DH 2011)
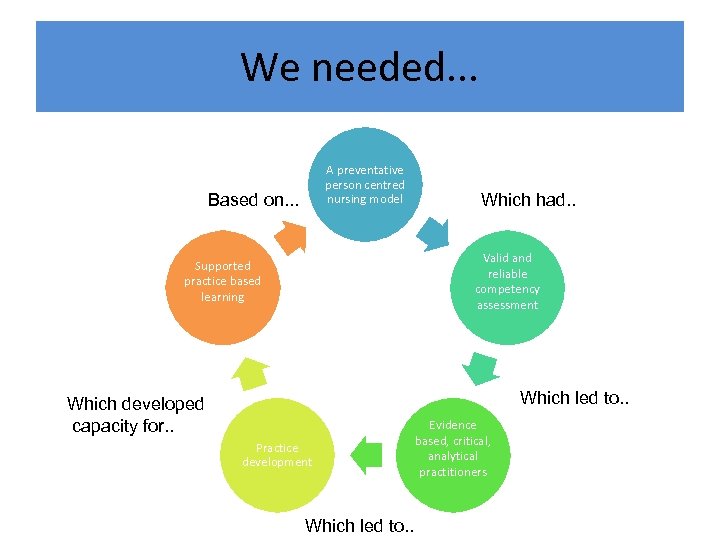 We needed. . . A preventative person centred nursing model Based on. . . Which had. . Valid and reliable competency assessment Supported practice based learning Which led to. . Which developed capacity for. . Practice development Which led to. . Evidence based, critical, analytical practitioners
We needed. . . A preventative person centred nursing model Based on. . . Which had. . Valid and reliable competency assessment Supported practice based learning Which led to. . Which developed capacity for. . Practice development Which led to. . Evidence based, critical, analytical practitioners
 The SHINE model
The SHINE model
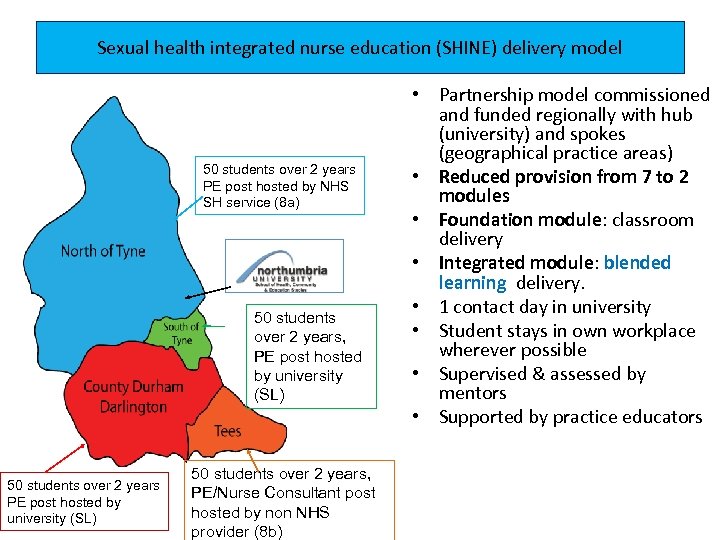 Sexual health integrated nurse education (SHINE) delivery model 50 students over 2 years PE post hosted by NHS SH service (8 a) 50 students over 2 years, PE post hosted by university (SL) 50 students over 2 years, PE/Nurse Consultant post hosted by non NHS provider (8 b) • Partnership model commissioned and funded regionally with hub (university) and spokes (geographical practice areas) • Reduced provision from 7 to 2 modules • Foundation module: classroom delivery • Integrated module: blended learning delivery. • 1 contact day in university • Student stays in own workplace wherever possible • Supervised & assessed by mentors • Supported by practice educators
Sexual health integrated nurse education (SHINE) delivery model 50 students over 2 years PE post hosted by NHS SH service (8 a) 50 students over 2 years, PE post hosted by university (SL) 50 students over 2 years, PE/Nurse Consultant post hosted by non NHS provider (8 b) • Partnership model commissioned and funded regionally with hub (university) and spokes (geographical practice areas) • Reduced provision from 7 to 2 modules • Foundation module: classroom delivery • Integrated module: blended learning delivery. • 1 contact day in university • Student stays in own workplace wherever possible • Supervised & assessed by mentors • Supported by practice educators
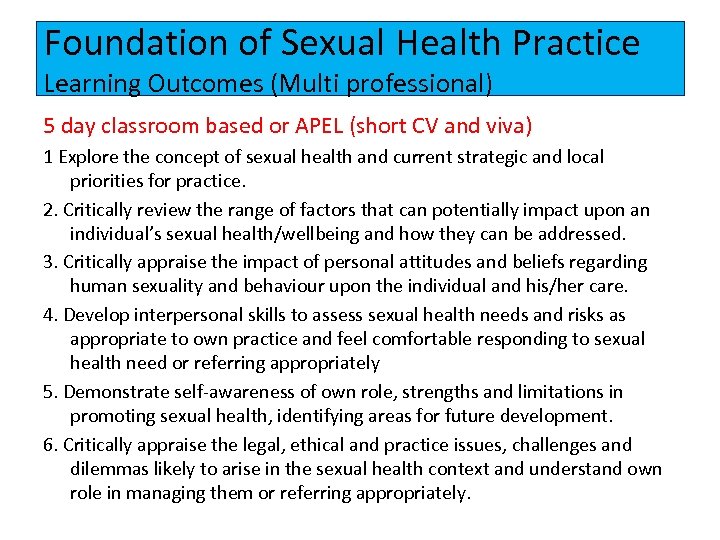 Foundation of Sexual Health Practice Learning Outcomes (Multi professional) 5 day classroom based or APEL (short CV and viva) 1 Explore the concept of sexual health and current strategic and local priorities for practice. 2. Critically review the range of factors that can potentially impact upon an individual’s sexual health/wellbeing and how they can be addressed. 3. Critically appraise the impact of personal attitudes and beliefs regarding human sexuality and behaviour upon the individual and his/her care. 4. Develop interpersonal skills to assess sexual health needs and risks as appropriate to own practice and feel comfortable responding to sexual health need or referring appropriately 5. Demonstrate self-awareness of own role, strengths and limitations in promoting sexual health, identifying areas for future development. 6. Critically appraise the legal, ethical and practice issues, challenges and dilemmas likely to arise in the sexual health context and understand own role in managing them or referring appropriately.
Foundation of Sexual Health Practice Learning Outcomes (Multi professional) 5 day classroom based or APEL (short CV and viva) 1 Explore the concept of sexual health and current strategic and local priorities for practice. 2. Critically review the range of factors that can potentially impact upon an individual’s sexual health/wellbeing and how they can be addressed. 3. Critically appraise the impact of personal attitudes and beliefs regarding human sexuality and behaviour upon the individual and his/her care. 4. Develop interpersonal skills to assess sexual health needs and risks as appropriate to own practice and feel comfortable responding to sexual health need or referring appropriately 5. Demonstrate self-awareness of own role, strengths and limitations in promoting sexual health, identifying areas for future development. 6. Critically appraise the legal, ethical and practice issues, challenges and dilemmas likely to arise in the sexual health context and understand own role in managing them or referring appropriately.
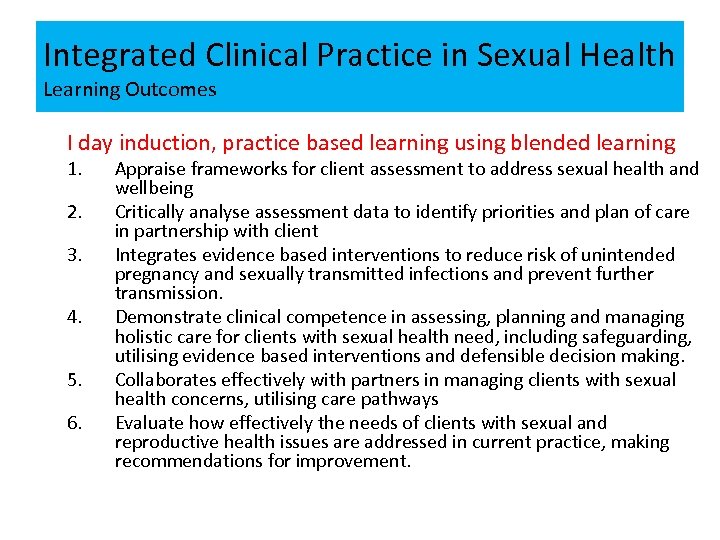 Integrated Clinical Practice in Sexual Health Learning Outcomes I day induction, practice based learning using blended learning 1. 2. 3. 4. 5. 6. Appraise frameworks for client assessment to address sexual health and wellbeing Critically analyse assessment data to identify priorities and plan of care in partnership with client Integrates evidence based interventions to reduce risk of unintended pregnancy and sexually transmitted infections and prevent further transmission. Demonstrate clinical competence in assessing, planning and managing holistic care for clients with sexual health need, including safeguarding, utilising evidence based interventions and defensible decision making. Collaborates effectively with partners in managing clients with sexual health concerns, utilising care pathways Evaluate how effectively the needs of clients with sexual and reproductive health issues are addressed in current practice, making recommendations for improvement.
Integrated Clinical Practice in Sexual Health Learning Outcomes I day induction, practice based learning using blended learning 1. 2. 3. 4. 5. 6. Appraise frameworks for client assessment to address sexual health and wellbeing Critically analyse assessment data to identify priorities and plan of care in partnership with client Integrates evidence based interventions to reduce risk of unintended pregnancy and sexually transmitted infections and prevent further transmission. Demonstrate clinical competence in assessing, planning and managing holistic care for clients with sexual health need, including safeguarding, utilising evidence based interventions and defensible decision making. Collaborates effectively with partners in managing clients with sexual health concerns, utilising care pathways Evaluate how effectively the needs of clients with sexual and reproductive health issues are addressed in current practice, making recommendations for improvement.
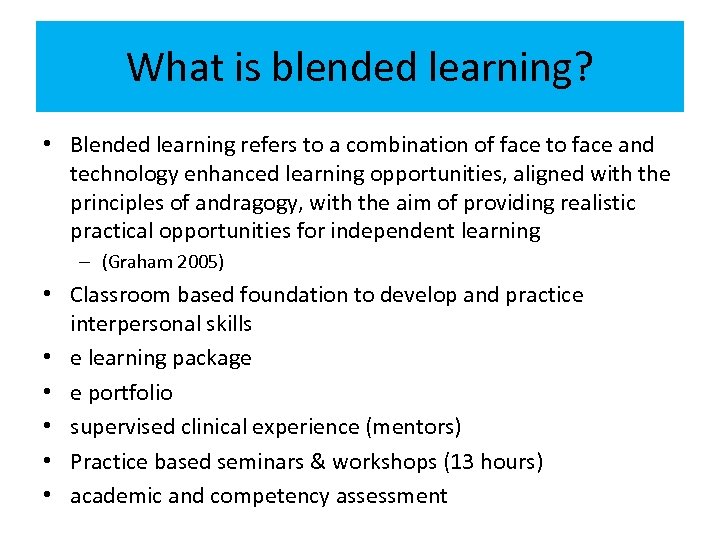 What is blended learning? • Blended learning refers to a combination of face to face and technology enhanced learning opportunities, aligned with the principles of andragogy, with the aim of providing realistic practical opportunities for independent learning – (Graham 2005) • Classroom based foundation to develop and practice interpersonal skills • e learning package • e portfolio • supervised clinical experience (mentors) • Practice based seminars & workshops (13 hours) • academic and competency assessment
What is blended learning? • Blended learning refers to a combination of face to face and technology enhanced learning opportunities, aligned with the principles of andragogy, with the aim of providing realistic practical opportunities for independent learning – (Graham 2005) • Classroom based foundation to develop and practice interpersonal skills • e learning package • e portfolio • supervised clinical experience (mentors) • Practice based seminars & workshops (13 hours) • academic and competency assessment
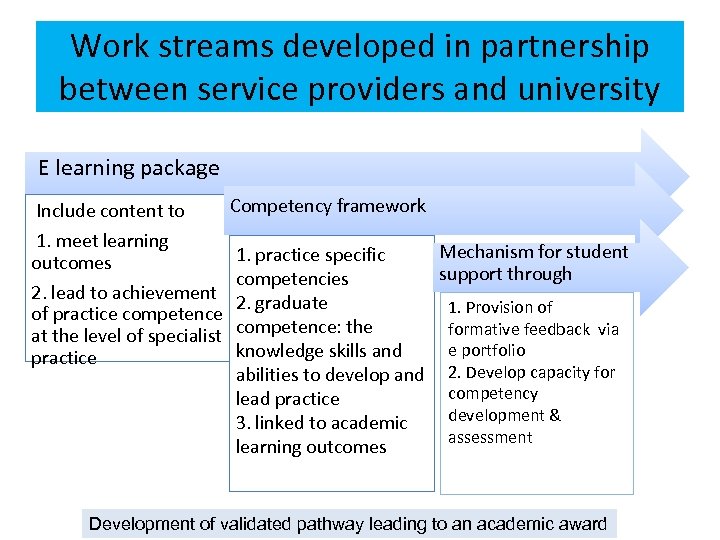 Work streams developed in partnership between service providers and university E learning package Include content to 1. meet learning outcomes 2. lead to achievement of practice competence at the level of specialist practice Competency framework 1. practice specific competencies 2. graduate competence: the knowledge skills and abilities to develop and lead practice 3. linked to academic learning outcomes Mechanism for student support through 1. Provision of formative feedback via e portfolio 2. Develop capacity for competency development & assessment Development of validated pathway leading to an academic award
Work streams developed in partnership between service providers and university E learning package Include content to 1. meet learning outcomes 2. lead to achievement of practice competence at the level of specialist practice Competency framework 1. practice specific competencies 2. graduate competence: the knowledge skills and abilities to develop and lead practice 3. linked to academic learning outcomes Mechanism for student support through 1. Provision of formative feedback via e portfolio 2. Develop capacity for competency development & assessment Development of validated pathway leading to an academic award
 The competency framework • Informed by the notion of competence referred to as professional capability by Eraut (1998) which includes – Individual competencies aligned with the service specifications – PLUS – competence linked to graduate outcomes (QAA 2012) to enable nurses to lead practice development. • This requires a partnership approach to ensure both competencies and competence are adequately reflected from practitioner and educational perspectives. Anema & Mc. Coy (2010)
The competency framework • Informed by the notion of competence referred to as professional capability by Eraut (1998) which includes – Individual competencies aligned with the service specifications – PLUS – competence linked to graduate outcomes (QAA 2012) to enable nurses to lead practice development. • This requires a partnership approach to ensure both competencies and competence are adequately reflected from practitioner and educational perspectives. Anema & Mc. Coy (2010)
 The e learning package • Adult learning takes place whilst solving complex and authentic tasks and problems based on issues of relevance to the student, often in collaboration and through interaction with others. • Case based learning has high relevance in this context, and can provide an effective means of engaging students with their own learning as they analyse not only how they might practice but are also required to articulate their decision making in particular scenarios (Knowles 2011) • But. . . • Many e-learning packages lack pedagogical principles and theoretical foundations • Therefore the “active learning” potential of much e learning is not realised (Schroeder & Spannagel 2006)
The e learning package • Adult learning takes place whilst solving complex and authentic tasks and problems based on issues of relevance to the student, often in collaboration and through interaction with others. • Case based learning has high relevance in this context, and can provide an effective means of engaging students with their own learning as they analyse not only how they might practice but are also required to articulate their decision making in particular scenarios (Knowles 2011) • But. . . • Many e-learning packages lack pedagogical principles and theoretical foundations • Therefore the “active learning” potential of much e learning is not realised (Schroeder & Spannagel 2006)
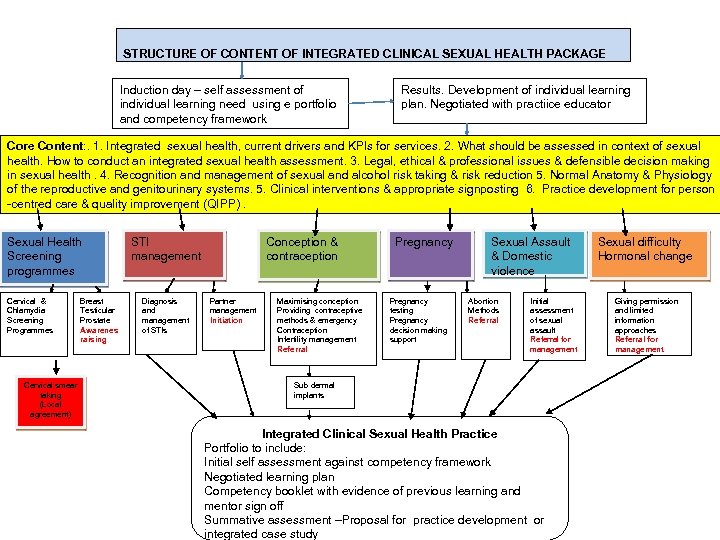 STRUCTURE OF CONTENT OF INTEGRATED CLINICAL SEXUAL HEALTH PACKAGE Induction day – self assessment of individual learning need using e portfolio and competency framework Results. Development of individual learning plan. Negotiated with practiice educator Core Content: . 1. Integrated sexual health, current drivers and KPIs for services. 2. What should be assessed in context of sexual health. How to conduct an integrated sexual health assessment. 3. Legal, ethical & professional issues & defensible decision making in sexual health. 4. Recognition and management of sexual and alcohol risk taking & risk reduction 5. Normal Anatomy & Physiology of the reproductive and genitourinary systems. 5. Clinical interventions & appropriate signposting 6. Practice development for person -centred care & quality improvement (QIPP). Sexual Health Screening programmes Cervical & Chlamydia Screening Programmes Cervical smear taking (Local agreement) Breast Testicular Prostate Awarenes raising STI management Diagnosis and management of STIs Conception & contraception Partner management Initiation Maximising conception Providing contraceptive methods & emergency Contraception Infertility management Referral Pregnancy testing Pregnancy decision making support Sexual Assault & Domestic violence Abortion Methods Referral Initial assessment of sexual assault Referral for management Sub dermal implants Integrated Clinical Sexual Health Practice Portfolio to include: Initial self assessment against competency framework Negotiated learning plan Competency booklet with evidence of previous learning and mentor sign off Summative assessment –Proposal for practice development or integrated case study Sexual difficulty Hormonal change Giving permission and limited information approaches Referral for management
STRUCTURE OF CONTENT OF INTEGRATED CLINICAL SEXUAL HEALTH PACKAGE Induction day – self assessment of individual learning need using e portfolio and competency framework Results. Development of individual learning plan. Negotiated with practiice educator Core Content: . 1. Integrated sexual health, current drivers and KPIs for services. 2. What should be assessed in context of sexual health. How to conduct an integrated sexual health assessment. 3. Legal, ethical & professional issues & defensible decision making in sexual health. 4. Recognition and management of sexual and alcohol risk taking & risk reduction 5. Normal Anatomy & Physiology of the reproductive and genitourinary systems. 5. Clinical interventions & appropriate signposting 6. Practice development for person -centred care & quality improvement (QIPP). Sexual Health Screening programmes Cervical & Chlamydia Screening Programmes Cervical smear taking (Local agreement) Breast Testicular Prostate Awarenes raising STI management Diagnosis and management of STIs Conception & contraception Partner management Initiation Maximising conception Providing contraceptive methods & emergency Contraception Infertility management Referral Pregnancy testing Pregnancy decision making support Sexual Assault & Domestic violence Abortion Methods Referral Initial assessment of sexual assault Referral for management Sub dermal implants Integrated Clinical Sexual Health Practice Portfolio to include: Initial self assessment against competency framework Negotiated learning plan Competency booklet with evidence of previous learning and mentor sign off Summative assessment –Proposal for practice development or integrated case study Sexual difficulty Hormonal change Giving permission and limited information approaches Referral for management
 The e learning package http: //hces-online. net/courses/sexual-health/front. html
The e learning package http: //hces-online. net/courses/sexual-health/front. html
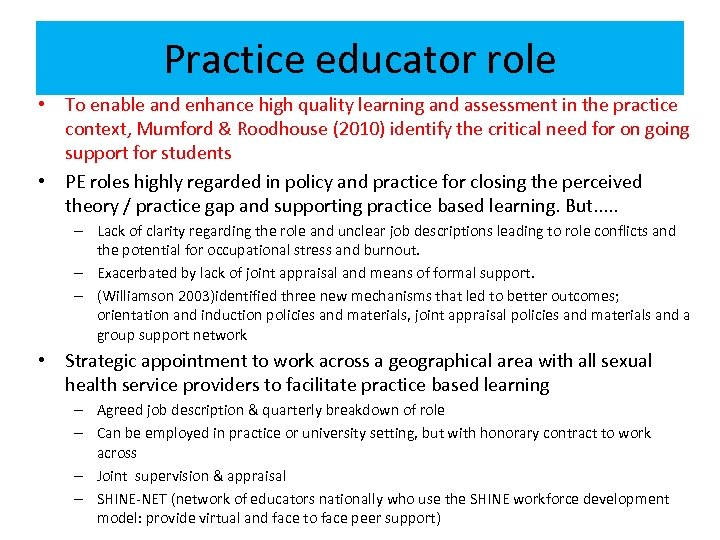 Practice educator role • To enable and enhance high quality learning and assessment in the practice context, Mumford & Roodhouse (2010) identify the critical need for on going support for students • PE roles highly regarded in policy and practice for closing the perceived theory / practice gap and supporting practice based learning. But. . . – Lack of clarity regarding the role and unclear job descriptions leading to role conflicts and the potential for occupational stress and burnout. – Exacerbated by lack of joint appraisal and means of formal support. – (Williamson 2003)identified three new mechanisms that led to better outcomes; orientation and induction policies and materials, joint appraisal policies and materials and a group support network • Strategic appointment to work across a geographical area with all sexual health service providers to facilitate practice based learning – Agreed job description & quarterly breakdown of role – Can be employed in practice or university setting, but with honorary contract to work across – Joint supervision & appraisal – SHINE-NET (network of educators nationally who use the SHINE workforce development model: provide virtual and face to face peer support)
Practice educator role • To enable and enhance high quality learning and assessment in the practice context, Mumford & Roodhouse (2010) identify the critical need for on going support for students • PE roles highly regarded in policy and practice for closing the perceived theory / practice gap and supporting practice based learning. But. . . – Lack of clarity regarding the role and unclear job descriptions leading to role conflicts and the potential for occupational stress and burnout. – Exacerbated by lack of joint appraisal and means of formal support. – (Williamson 2003)identified three new mechanisms that led to better outcomes; orientation and induction policies and materials, joint appraisal policies and materials and a group support network • Strategic appointment to work across a geographical area with all sexual health service providers to facilitate practice based learning – Agreed job description & quarterly breakdown of role – Can be employed in practice or university setting, but with honorary contract to work across – Joint supervision & appraisal – SHINE-NET (network of educators nationally who use the SHINE workforce development model: provide virtual and face to face peer support)
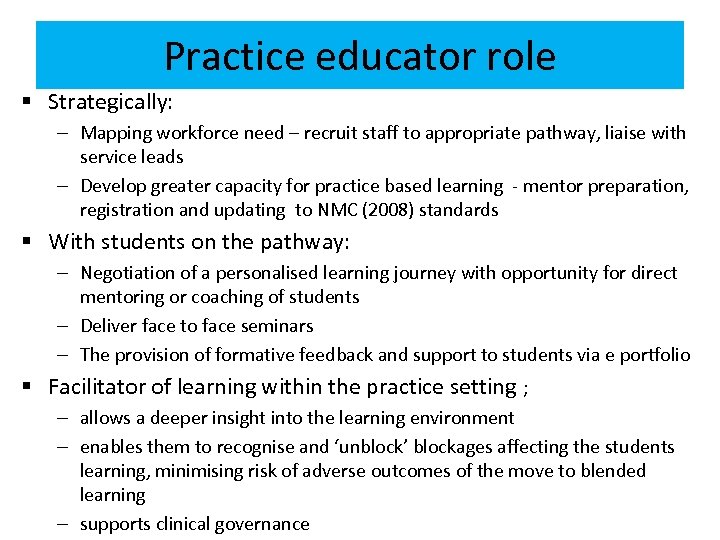 Practice educator role § Strategically: – Mapping workforce need – recruit staff to appropriate pathway, liaise with service leads – Develop greater capacity for practice based learning - mentor preparation, registration and updating to NMC (2008) standards § With students on the pathway: – Negotiation of a personalised learning journey with opportunity for direct mentoring or coaching of students – Deliver face to face seminars – The provision of formative feedback and support to students via e portfolio § Facilitator of learning within the practice setting ; – allows a deeper insight into the learning environment – enables them to recognise and ‘unblock’ blockages affecting the students learning, minimising risk of adverse outcomes of the move to blended learning – supports clinical governance
Practice educator role § Strategically: – Mapping workforce need – recruit staff to appropriate pathway, liaise with service leads – Develop greater capacity for practice based learning - mentor preparation, registration and updating to NMC (2008) standards § With students on the pathway: – Negotiation of a personalised learning journey with opportunity for direct mentoring or coaching of students – Deliver face to face seminars – The provision of formative feedback and support to students via e portfolio § Facilitator of learning within the practice setting ; – allows a deeper insight into the learning environment – enables them to recognise and ‘unblock’ blockages affecting the students learning, minimising risk of adverse outcomes of the move to blended learning – supports clinical governance
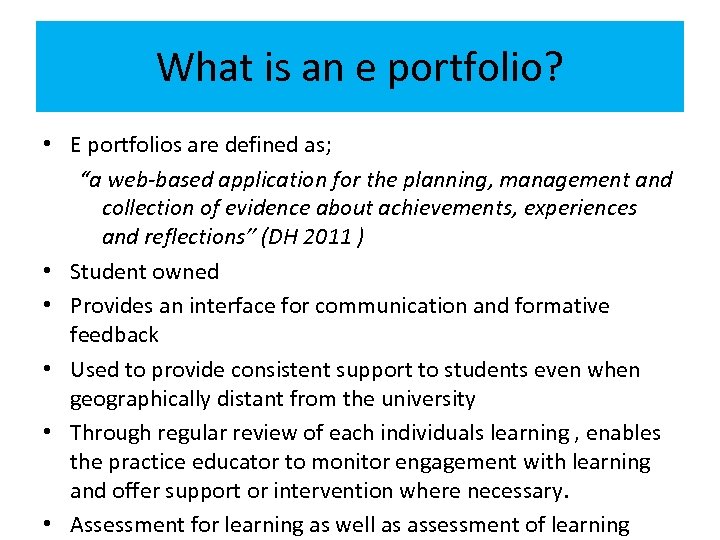 What is an e portfolio? • E portfolios are defined as; “a web-based application for the planning, management and collection of evidence about achievements, experiences and reflections” (DH 2011 ) • Student owned • Provides an interface for communication and formative feedback • Used to provide consistent support to students even when geographically distant from the university • Through regular review of each individuals learning , enables the practice educator to monitor engagement with learning and offer support or intervention where necessary. • Assessment for learning as well as assessment of learning
What is an e portfolio? • E portfolios are defined as; “a web-based application for the planning, management and collection of evidence about achievements, experiences and reflections” (DH 2011 ) • Student owned • Provides an interface for communication and formative feedback • Used to provide consistent support to students even when geographically distant from the university • Through regular review of each individuals learning , enables the practice educator to monitor engagement with learning and offer support or intervention where necessary. • Assessment for learning as well as assessment of learning
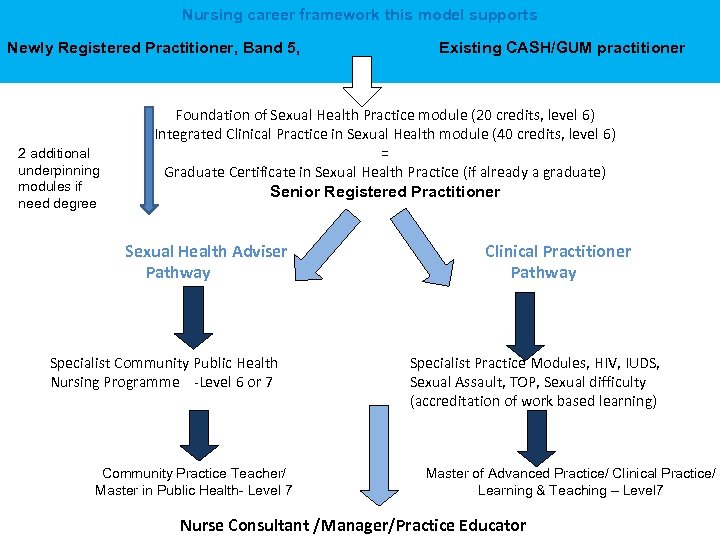 Nursing career framework this model supports Newly Registered Practitioner, Band 5, 2 additional underpinning modules if need degree Existing CASH/GUM practitioner Foundation of Sexual Health Practice module (20 credits, level 6) Integrated Clinical Practice in Sexual Health module (40 credits, level 6) = Graduate Certificate in Sexual Health Practice (if already a graduate) Senior Registered Practitioner Sexual Health Adviser Pathway Specialist Community Public Health Nursing Programme -Level 6 or 7 Clinical Practitioner Pathway Specialist Practice Modules, HIV, IUDS, Sexual Assault, TOP, Sexual difficulty (accreditation of work based learning) Community Practice Teacher/ Master in Public Health- Level 7 Master of Advanced Practice/ Clinical Practice/ Learning & Teaching – Level 7 Nurse Consultant /Manager/Practice Educator
Nursing career framework this model supports Newly Registered Practitioner, Band 5, 2 additional underpinning modules if need degree Existing CASH/GUM practitioner Foundation of Sexual Health Practice module (20 credits, level 6) Integrated Clinical Practice in Sexual Health module (40 credits, level 6) = Graduate Certificate in Sexual Health Practice (if already a graduate) Senior Registered Practitioner Sexual Health Adviser Pathway Specialist Community Public Health Nursing Programme -Level 6 or 7 Clinical Practitioner Pathway Specialist Practice Modules, HIV, IUDS, Sexual Assault, TOP, Sexual difficulty (accreditation of work based learning) Community Practice Teacher/ Master in Public Health- Level 7 Master of Advanced Practice/ Clinical Practice/ Learning & Teaching – Level 7 Nurse Consultant /Manager/Practice Educator
 Potential of SHINE model & practice educator posts to feed into development of advanced practice modules at masters level • Advanced LARCS (IUDs) – Fitting – Trainer • Management of sexual assault – nurse examiners • Management of sexual difficulty • Monitoring /Management of HIV • Management of unintended pregnancy
Potential of SHINE model & practice educator posts to feed into development of advanced practice modules at masters level • Advanced LARCS (IUDs) – Fitting – Trainer • Management of sexual assault – nurse examiners • Management of sexual difficulty • Monitoring /Management of HIV • Management of unintended pregnancy
 Public Health- Sexual Health Advisers • My doctoral study also influenced national policy and practice regarding the way Sexual Health Advisers are prepared • Each area should now commission a sexual health adviser pathway of the Specialist Community Public Health Nursing Programme, (SCPHN) alongside HVs, school nurses, occupational health. • Sexual health advisers undertake and develop capacity for sexual health needs assessment, moving beyond purely epidemiological need • Work at the level of individual and population health to deliver interventions to impact inequalities • Course 1 year 50% theory 50% practice - supported by community practice teachers
Public Health- Sexual Health Advisers • My doctoral study also influenced national policy and practice regarding the way Sexual Health Advisers are prepared • Each area should now commission a sexual health adviser pathway of the Specialist Community Public Health Nursing Programme, (SCPHN) alongside HVs, school nurses, occupational health. • Sexual health advisers undertake and develop capacity for sexual health needs assessment, moving beyond purely epidemiological need • Work at the level of individual and population health to deliver interventions to impact inequalities • Course 1 year 50% theory 50% practice - supported by community practice teachers
 Evaluation “Many congratulations to the Pathway leader, development team and IT colleagues. The use of all learning materials including Pebble Pad, Icons, Voiceover, Video, Case Studies, Care Scenarios, Contemporary literature, Policy, Guidelines and Reference Materials are presented in a professional polished, attractive and student friendly manner. This blended learning module reflects a great deal of work by colleagues; it is an excellent resource which reflects contemporary learning and teaching methodologies” University quality assurance reviewer 2010
Evaluation “Many congratulations to the Pathway leader, development team and IT colleagues. The use of all learning materials including Pebble Pad, Icons, Voiceover, Video, Case Studies, Care Scenarios, Contemporary literature, Policy, Guidelines and Reference Materials are presented in a professional polished, attractive and student friendly manner. This blended learning module reflects a great deal of work by colleagues; it is an excellent resource which reflects contemporary learning and teaching methodologies” University quality assurance reviewer 2010
 Evaluation • “ • I liked the structure - the package is really good” “You can pace your learning and study when convenient. • It is easy to pick up where you left off as the package 'files' your work for you” “Although there are deadlines for certain things, you can work through the package at your own speed. • It is good self learning with support. It is easier than travelling to a university base which is difficult to fit around work” Student evaluations, Cohort 1, Initial evaluation December 2010
Evaluation • “ • I liked the structure - the package is really good” “You can pace your learning and study when convenient. • It is easy to pick up where you left off as the package 'files' your work for you” “Although there are deadlines for certain things, you can work through the package at your own speed. • It is good self learning with support. It is easier than travelling to a university base which is difficult to fit around work” Student evaluations, Cohort 1, Initial evaluation December 2010
 Evaluation “I accessed the Foundation module over a weekend, reducing the time spent away from the workplace, and I found the a concentrated learning environment extremely beneficial. I attended this course with some colleagues new to Sexual Health and they all commented favourably on the approach and delivery, particularly subject matter that many of them had expressed unease discussing prior to the sessions. Sexual health nurse – outreach team 2011
Evaluation “I accessed the Foundation module over a weekend, reducing the time spent away from the workplace, and I found the a concentrated learning environment extremely beneficial. I attended this course with some colleagues new to Sexual Health and they all commented favourably on the approach and delivery, particularly subject matter that many of them had expressed unease discussing prior to the sessions. Sexual health nurse – outreach team 2011
 Evaluation The second module is delivered as an IT package and self directed learning in practice. Support from the practice educator was always available and there was a series of seminars to ensure everyone was happy with their progress through the package. Practice based mentors were arranged for each student to ensure the competencies could be practiced and achieved. From my experience this worked smoothly and efficiently. I felt encouraged to develop my own learning and practice linked to the knowledge and skills framework gateways and a career structure. ” Prison nurse leading the provision of sexual health services 2011
Evaluation The second module is delivered as an IT package and self directed learning in practice. Support from the practice educator was always available and there was a series of seminars to ensure everyone was happy with their progress through the package. Practice based mentors were arranged for each student to ensure the competencies could be practiced and achieved. From my experience this worked smoothly and efficiently. I felt encouraged to develop my own learning and practice linked to the knowledge and skills framework gateways and a career structure. ” Prison nurse leading the provision of sexual health services 2011
 Nurse Education Provider of the Year (post-registration)
Nurse Education Provider of the Year (post-registration)
 Evaluation • We have the potential, in partnership with University of West of England to develop a bid for Higher Education Academy funding to research the SHINE model more thoroughly and include: • • Student perspective Commissioner perspective Clinical service lead perspective Practice educator perspective
Evaluation • We have the potential, in partnership with University of West of England to develop a bid for Higher Education Academy funding to research the SHINE model more thoroughly and include: • • Student perspective Commissioner perspective Clinical service lead perspective Practice educator perspective
 The current situation in South West • In the North East developing the support, infrastructure and resources to collaboratively agree and implement the SHINE model has been demanding • It has been supported and enabled by strong relationships between the HEI, commissioners, SH providers and students and willingness to work in partnership to achieve a mutually desirable goal. • Much of the complexity arises from the number of stakeholders involved, and the many organisational policies and boundaries that have to be acknowledged and respected in finding solutions to complex problems. • South Strategic Health authority have demonstrated an intent to commission the same approach in the South West with UWE as the delivery partner- currently at contract negotiation stage. • Sexual health provider nurse leads have driven the process (Ann Steele- Nicholson & colleagues) • Some mapping work has been undertaken (Peter Carter with service provider leads)
The current situation in South West • In the North East developing the support, infrastructure and resources to collaboratively agree and implement the SHINE model has been demanding • It has been supported and enabled by strong relationships between the HEI, commissioners, SH providers and students and willingness to work in partnership to achieve a mutually desirable goal. • Much of the complexity arises from the number of stakeholders involved, and the many organisational policies and boundaries that have to be acknowledged and respected in finding solutions to complex problems. • South Strategic Health authority have demonstrated an intent to commission the same approach in the South West with UWE as the delivery partner- currently at contract negotiation stage. • Sexual health provider nurse leads have driven the process (Ann Steele- Nicholson & colleagues) • Some mapping work has been undertaken (Peter Carter with service provider leads)
 • Thank you for your attention • Questions? • anne. mcnall@northumbria. ac. uk • 0191 215 6139
• Thank you for your attention • Questions? • anne. mcnall@northumbria. ac. uk • 0191 215 6139
 References • • • Anema, M. Mc. Coy, J. (2010) Competency-based nursing education: guide to achieving outstanding learner outcomes. New York: Springer Australia’s National Research Centre on Alcohol and other drugs Workforce development (2002) Models of Workforce Development http: //ncoss. org. au/projects/workforce-development-models. pdf accessed 10. 6. 10 Church, K. Mayhew, S. H. (2009) Integration of STI and HIV prevention, Care, and Treatment into Family Planning Services: A review of the literature. Studies in Family Planning. 40 (3) 171 -186 Eraut, M (1997) Concepts of competence. Journal of Inter-Professional care 12, 2 127 -139 Fingfeld-Connett, D. (2008) Concept synthesis of the art of nursing. Journal of Advanced Nursing, 62, 3 381 -388 Great Britain. Department of Health. (2011) A Framework for Technology enhanced learning. DH London Mc. Nall, A (2010) Workforce Development in Sexual Health: the way forward. Theme 7: Department of Health National Consultative Conference in Sexual Health- Celebrate - Innovate - Influence. 4 February 2010, London. Mc Nall, A (2012) An emancipatory practice development study: using critical discourse analysis to develop theory and practice of sexual health workforce development. Thesis submitted in partial fulfilment of the requirements for the award of Professional Doctorate. Northumbria University Roodhouse, S. Mumford, J. (2010) Understanding work based learning. Farnham. Gower Royal College of Nursing (2009) Sexual Health Competencies: An integrated career and competency framework for sexual and reproductive health nursing. RCN. London framework Schroeder, U. Spannagel, C (2006) Supporting the active learning process. International journal on e learning 5 (2) 245 -264
References • • • Anema, M. Mc. Coy, J. (2010) Competency-based nursing education: guide to achieving outstanding learner outcomes. New York: Springer Australia’s National Research Centre on Alcohol and other drugs Workforce development (2002) Models of Workforce Development http: //ncoss. org. au/projects/workforce-development-models. pdf accessed 10. 6. 10 Church, K. Mayhew, S. H. (2009) Integration of STI and HIV prevention, Care, and Treatment into Family Planning Services: A review of the literature. Studies in Family Planning. 40 (3) 171 -186 Eraut, M (1997) Concepts of competence. Journal of Inter-Professional care 12, 2 127 -139 Fingfeld-Connett, D. (2008) Concept synthesis of the art of nursing. Journal of Advanced Nursing, 62, 3 381 -388 Great Britain. Department of Health. (2011) A Framework for Technology enhanced learning. DH London Mc. Nall, A (2010) Workforce Development in Sexual Health: the way forward. Theme 7: Department of Health National Consultative Conference in Sexual Health- Celebrate - Innovate - Influence. 4 February 2010, London. Mc Nall, A (2012) An emancipatory practice development study: using critical discourse analysis to develop theory and practice of sexual health workforce development. Thesis submitted in partial fulfilment of the requirements for the award of Professional Doctorate. Northumbria University Roodhouse, S. Mumford, J. (2010) Understanding work based learning. Farnham. Gower Royal College of Nursing (2009) Sexual Health Competencies: An integrated career and competency framework for sexual and reproductive health nursing. RCN. London framework Schroeder, U. Spannagel, C (2006) Supporting the active learning process. International journal on e learning 5 (2) 245 -264


