c9368d7d4f92cb611dc8f1460a4c1030.ppt
- Количество слайдов: 43
 WHO Growth Grids/ 2012 Risk Changes Diane Traver Joyce Bryant
WHO Growth Grids/ 2012 Risk Changes Diane Traver Joyce Bryant
 Overview CDC vs WHO Growth Charts. Why Change? Transition from <24 mo to 24 -59 mo charts Risks Definition Justifications/Implications
Overview CDC vs WHO Growth Charts. Why Change? Transition from <24 mo to 24 -59 mo charts Risks Definition Justifications/Implications
 Shift in Population Growth Concern for underweight has been replaced with concerns of overweight and obesity Re-examination of methodologies used in establishing CDC charts reveal improvements needed USDA requiring implementation by Oct ’ 12 (will be in Aug release)
Shift in Population Growth Concern for underweight has been replaced with concerns of overweight and obesity Re-examination of methodologies used in establishing CDC charts reveal improvements needed USDA requiring implementation by Oct ’ 12 (will be in Aug release)
 CDC Charts Based on only on US data from 1960’s-90’s No exclusion criteria Composition of formula has changed in last 35 years since first data collected Growth of formula fed infants may not be same now as those used in creation of charts, as a result Little data available for infants < 2 months old Several data sets combined to generate the charts Reference- description of how certain children grew in a particular place and time
CDC Charts Based on only on US data from 1960’s-90’s No exclusion criteria Composition of formula has changed in last 35 years since first data collected Growth of formula fed infants may not be same now as those used in creation of charts, as a result Little data available for infants < 2 months old Several data sets combined to generate the charts Reference- description of how certain children grew in a particular place and time
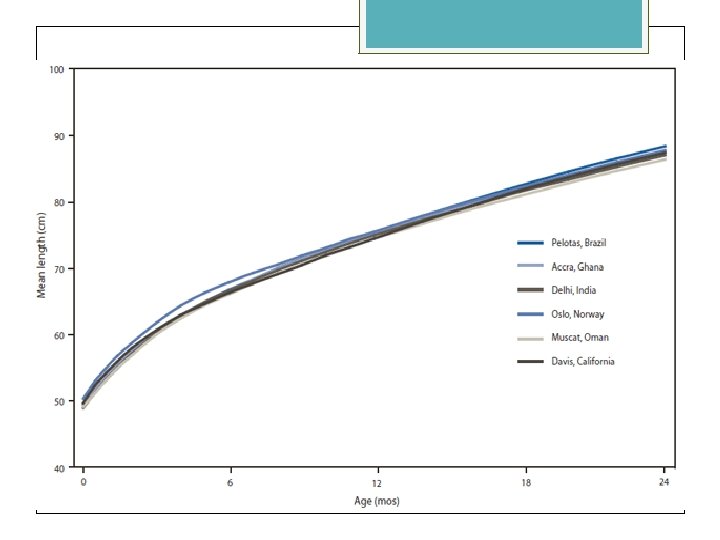
 WHO Premise All young children have the potential to grow similarly, regardless of ethnic group or place of birth, if they are in a healthy environment and have adequate nutrition In order to identify abnormal growth, healthy growth must be defined and adopting a standard would identify and address environmental conditions negatively affecting growth
WHO Premise All young children have the potential to grow similarly, regardless of ethnic group or place of birth, if they are in a healthy environment and have adequate nutrition In order to identify abnormal growth, healthy growth must be defined and adopting a standard would identify and address environmental conditions negatively affecting growth
 WHO Charts International study Participants willing to follow international feeding guidelines 100% BF for 12 months Adherence to many exclusion criteria Longitudinal data collected over 2 year period Premise confirmed Standard- how healthy children should grow under optimal conditions
WHO Charts International study Participants willing to follow international feeding guidelines 100% BF for 12 months Adherence to many exclusion criteria Longitudinal data collected over 2 year period Premise confirmed Standard- how healthy children should grow under optimal conditions
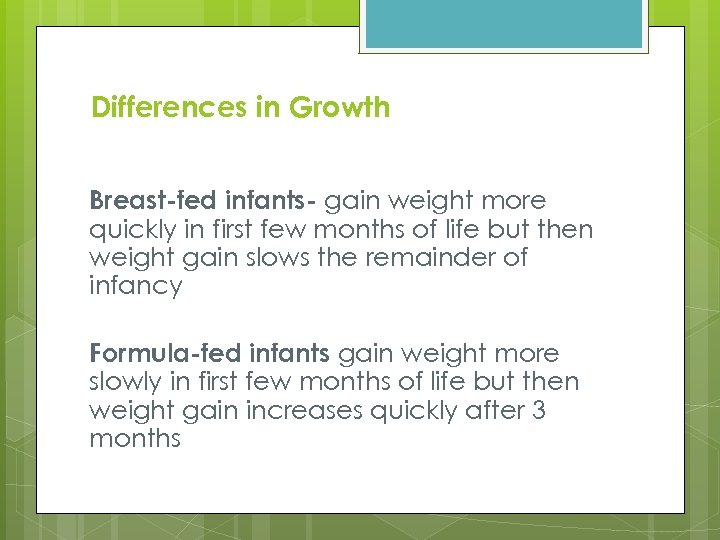 Differences in Growth Breast-fed infants- gain weight more quickly in first few months of life but then weight gain slows the remainder of infancy Formula-fed infants gain weight more slowly in first few months of life but then weight gain increases quickly after 3 months
Differences in Growth Breast-fed infants- gain weight more quickly in first few months of life but then weight gain slows the remainder of infancy Formula-fed infants gain weight more slowly in first few months of life but then weight gain increases quickly after 3 months
 Case Examples
Case Examples
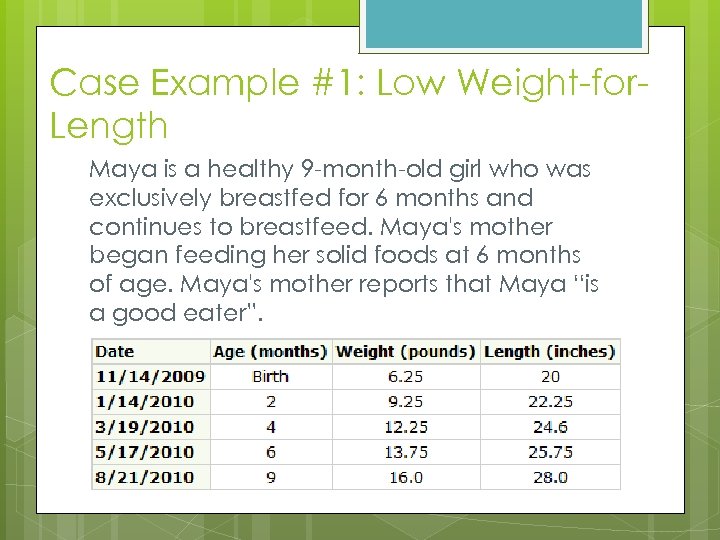 Case Example #1: Low Weight-for. Length Maya is a healthy 9 -month-old girl who was exclusively breastfed for 6 months and continues to breastfeed. Maya's mother began feeding her solid foods at 6 months of age. Maya's mother reports that Maya “is a good eater”.
Case Example #1: Low Weight-for. Length Maya is a healthy 9 -month-old girl who was exclusively breastfed for 6 months and continues to breastfeed. Maya's mother began feeding her solid foods at 6 months of age. Maya's mother reports that Maya “is a good eater”.
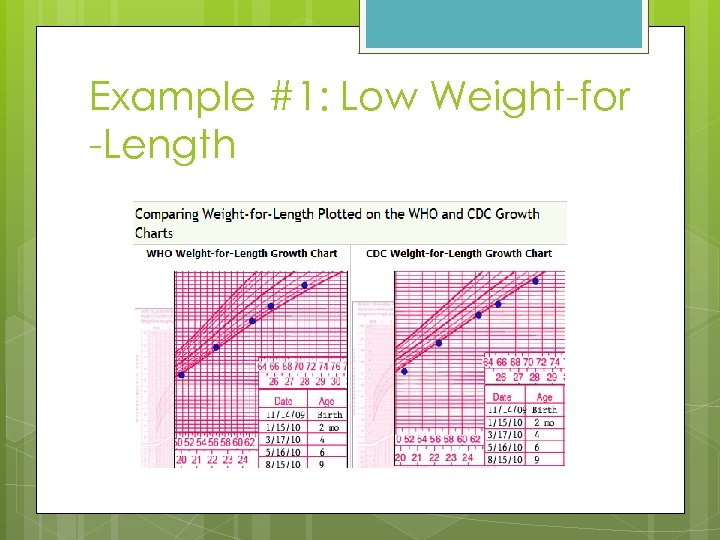 Example #1: Low Weight-for -Length
Example #1: Low Weight-for -Length
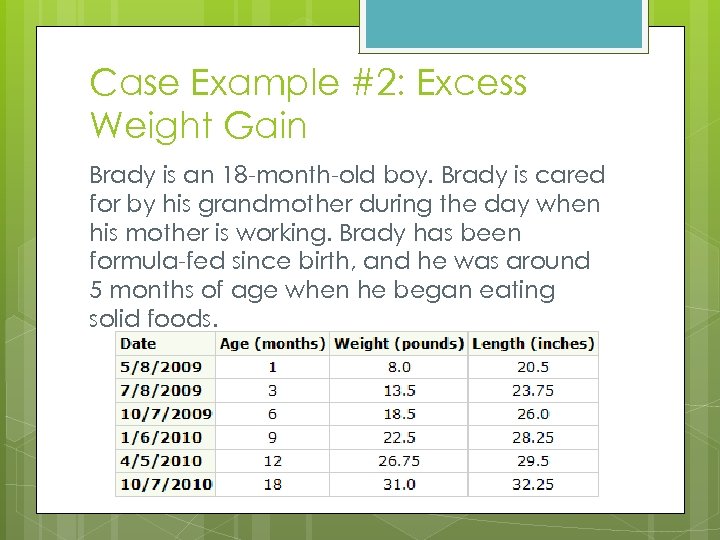 Case Example #2: Excess Weight Gain Brady is an 18 -month-old boy. Brady is cared for by his grandmother during the day when his mother is working. Brady has been formula-fed since birth, and he was around 5 months of age when he began eating solid foods.
Case Example #2: Excess Weight Gain Brady is an 18 -month-old boy. Brady is cared for by his grandmother during the day when his mother is working. Brady has been formula-fed since birth, and he was around 5 months of age when he began eating solid foods.
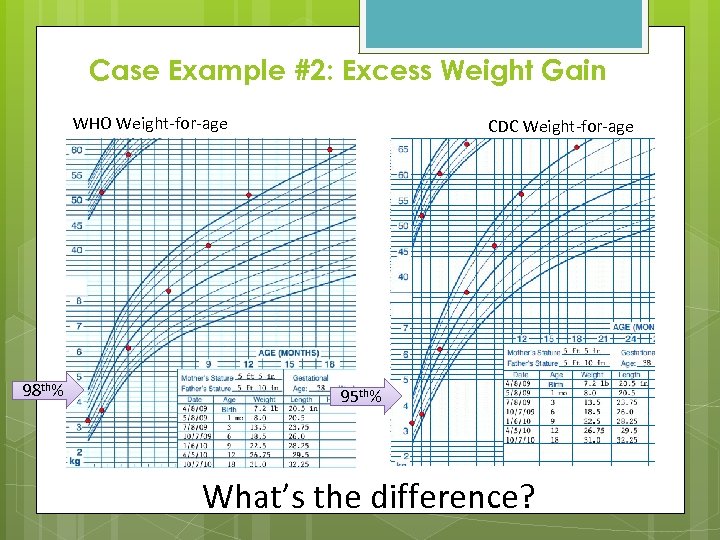 Case Example #2: Excess Weight Gain WHO Weight-for-age 98 th% CDC Weight-for-age 95 th% What’s the difference?
Case Example #2: Excess Weight Gain WHO Weight-for-age 98 th% CDC Weight-for-age 95 th% What’s the difference?
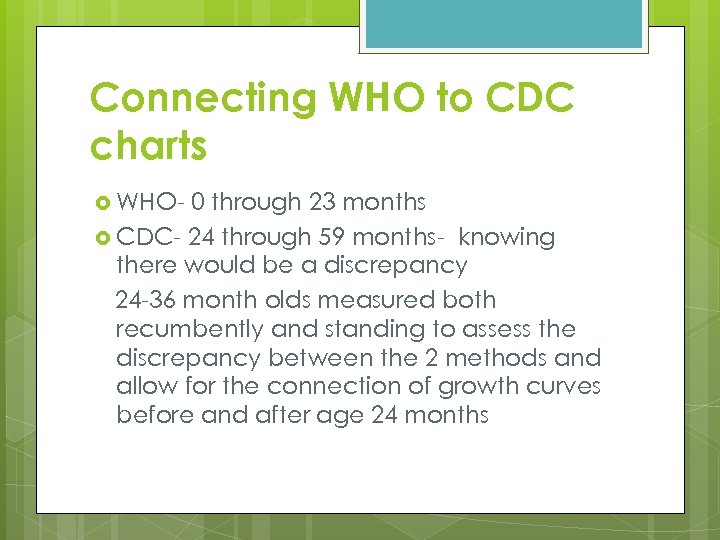 Connecting WHO to CDC charts WHO- 0 through 23 months CDC- 24 through 59 months- knowing there would be a discrepancy 24 -36 month olds measured both recumbently and standing to assess the discrepancy between the 2 methods and allow for the connection of growth curves before and after age 24 months
Connecting WHO to CDC charts WHO- 0 through 23 months CDC- 24 through 59 months- knowing there would be a discrepancy 24 -36 month olds measured both recumbently and standing to assess the discrepancy between the 2 methods and allow for the connection of growth curves before and after age 24 months
 Transitioning from WHO to CDC WHO Growth Grids- 0 through 23 monthsrecumbent CDC Growth Grids- 24 -59 months - stature MI-WIC- Will no longer have ‘R/S’ option If C-2 cannot be measured standing, click ‘Unknown’ and add measurement in ‘Comment’
Transitioning from WHO to CDC WHO Growth Grids- 0 through 23 monthsrecumbent CDC Growth Grids- 24 -59 months - stature MI-WIC- Will no longer have ‘R/S’ option If C-2 cannot be measured standing, click ‘Unknown’ and add measurement in ‘Comment’
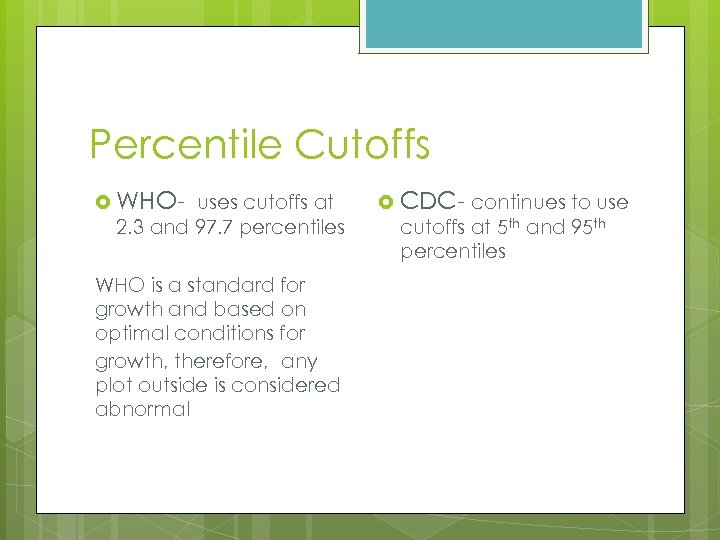 Percentile Cutoffs WHO- uses cutoffs at 2. 3 and 97. 7 percentiles WHO is a standard for growth and based on optimal conditions for growth, therefore, any plot outside is considered abnormal CDC- continues to use cutoffs at 5 th and 95 th percentiles
Percentile Cutoffs WHO- uses cutoffs at 2. 3 and 97. 7 percentiles WHO is a standard for growth and based on optimal conditions for growth, therefore, any plot outside is considered abnormal CDC- continues to use cutoffs at 5 th and 95 th percentiles
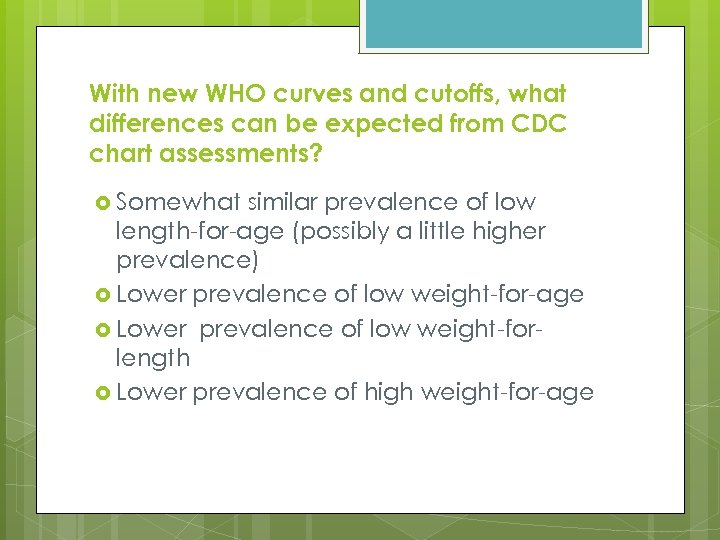 With new WHO curves and cutoffs, what differences can be expected from CDC chart assessments? Somewhat similar prevalence of low length-for-age (possibly a little higher prevalence) Lower prevalence of low weight-for-age Lower prevalence of low weight-forlength Lower prevalence of high weight-for-age
With new WHO curves and cutoffs, what differences can be expected from CDC chart assessments? Somewhat similar prevalence of low length-for-age (possibly a little higher prevalence) Lower prevalence of low weight-for-age Lower prevalence of low weight-forlength Lower prevalence of high weight-for-age
 In transitioning between WHO and CDC charts Remember that a series of measurements establishes a growth pattern Use measurements in conjunction with medical and family history Caution should be used in interpreting any changes
In transitioning between WHO and CDC charts Remember that a series of measurements establishes a growth pattern Use measurements in conjunction with medical and family history Caution should be used in interpreting any changes
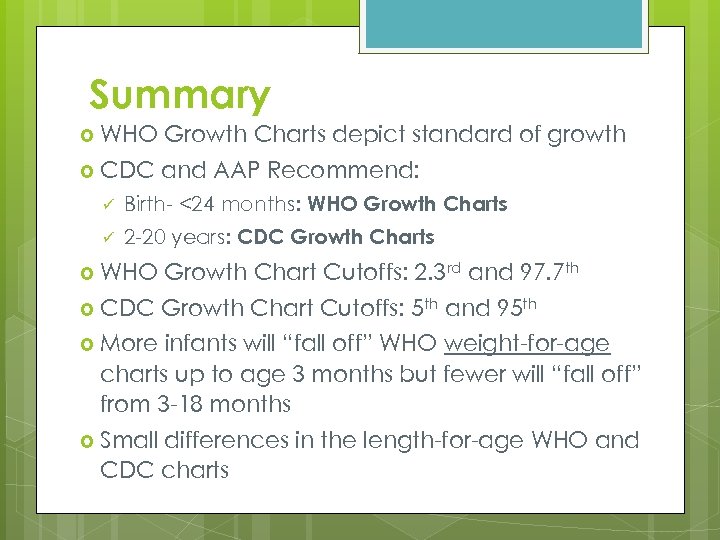 Summary WHO Growth Charts depict standard of growth CDC and AAP Recommend: ü Birth- <24 months: WHO Growth Charts ü 2 -20 years: CDC Growth Charts WHO Growth Chart Cutoffs: 2. 3 rd and 97. 7 th CDC Growth Chart Cutoffs: 5 th and 95 th More infants will “fall off” WHO weight-for-age charts up to age 3 months but fewer will “fall off” from 3 -18 months Small differences in the length-for-age WHO and CDC charts
Summary WHO Growth Charts depict standard of growth CDC and AAP Recommend: ü Birth- <24 months: WHO Growth Charts ü 2 -20 years: CDC Growth Charts WHO Growth Chart Cutoffs: 2. 3 rd and 97. 7 th CDC Growth Chart Cutoffs: 5 th and 95 th More infants will “fall off” WHO weight-for-age charts up to age 3 months but fewer will “fall off” from 3 -18 months Small differences in the length-for-age WHO and CDC charts
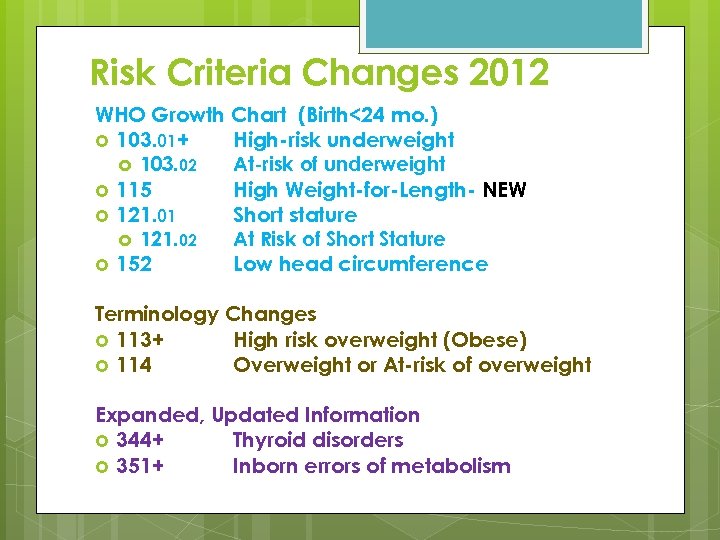 Risk Criteria Changes 2012 WHO Growth Chart (Birth<24 mo. ) 103. 01+ High-risk underweight 103. 02 At-risk of underweight 115 High Weight-for-Length- NEW 121. 01 Short stature 121. 02 At Risk of Short Stature 152 Low head circumference Terminology Changes 113+ High risk overweight (Obese) 114 Overweight or At-risk of overweight Expanded, Updated Information 344+ Thyroid disorders 351+ Inborn errors of metabolism
Risk Criteria Changes 2012 WHO Growth Chart (Birth<24 mo. ) 103. 01+ High-risk underweight 103. 02 At-risk of underweight 115 High Weight-for-Length- NEW 121. 01 Short stature 121. 02 At Risk of Short Stature 152 Low head circumference Terminology Changes 113+ High risk overweight (Obese) 114 Overweight or At-risk of overweight Expanded, Updated Information 344+ Thyroid disorders 351+ Inborn errors of metabolism
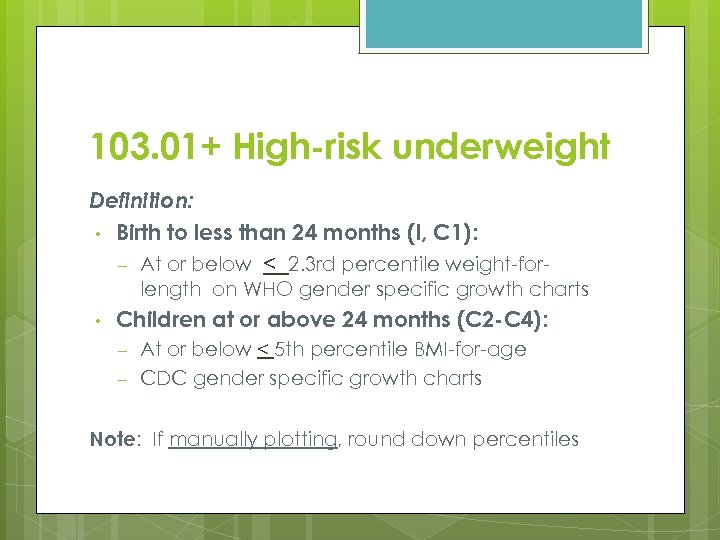 103. 01+ High-risk underweight Definition: • Birth to less than 24 months (I, C 1): – At or below < 2. 3 rd percentile weight-forlength on WHO gender specific growth charts • Children at or above 24 months (C 2 -C 4): – – At or below < 5 th percentile BMI-for-age CDC gender specific growth charts Note: If manually plotting, round down percentiles
103. 01+ High-risk underweight Definition: • Birth to less than 24 months (I, C 1): – At or below < 2. 3 rd percentile weight-forlength on WHO gender specific growth charts • Children at or above 24 months (C 2 -C 4): – – At or below < 5 th percentile BMI-for-age CDC gender specific growth charts Note: If manually plotting, round down percentiles
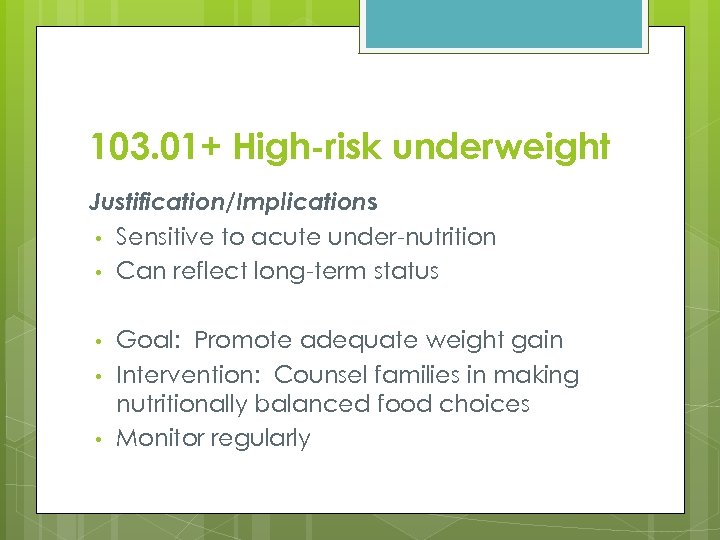 103. 01+ High-risk underweight Justification/Implications • Sensitive to acute under-nutrition • Can reflect long-term status • • • Goal: Promote adequate weight gain Intervention: Counsel families in making nutritionally balanced food choices Monitor regularly
103. 01+ High-risk underweight Justification/Implications • Sensitive to acute under-nutrition • Can reflect long-term status • • • Goal: Promote adequate weight gain Intervention: Counsel families in making nutritionally balanced food choices Monitor regularly
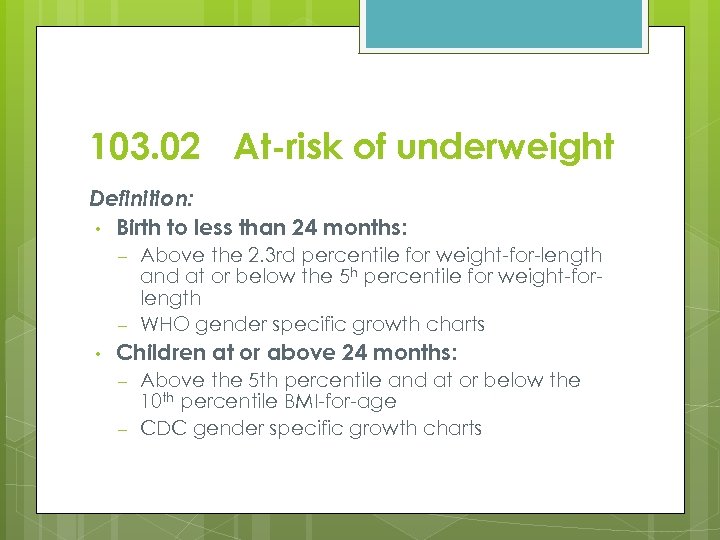 103. 02 At-risk of underweight Definition: • Birth to less than 24 months: – – • Above the 2. 3 rd percentile for weight-for-length and at or below the 5 h percentile for weight-forlength WHO gender specific growth charts Children at or above 24 months: – – Above the 5 th percentile and at or below the 10 th percentile BMI-for-age CDC gender specific growth charts
103. 02 At-risk of underweight Definition: • Birth to less than 24 months: – – • Above the 2. 3 rd percentile for weight-for-length and at or below the 5 h percentile for weight-forlength WHO gender specific growth charts Children at or above 24 months: – – Above the 5 th percentile and at or below the 10 th percentile BMI-for-age CDC gender specific growth charts
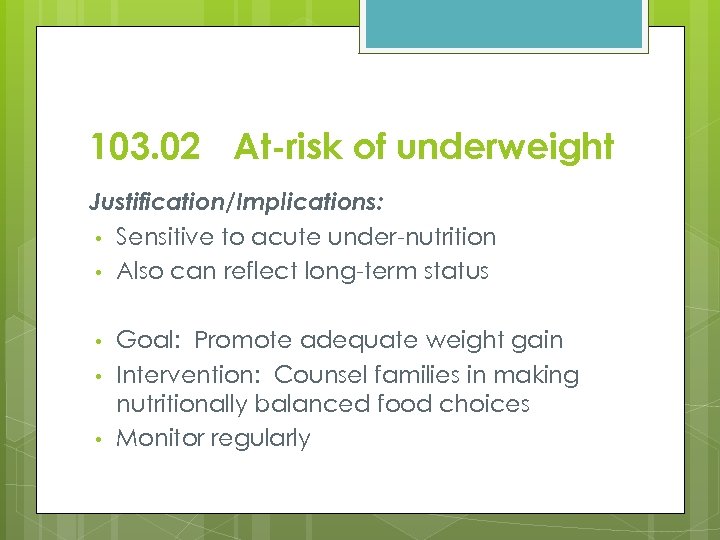 103. 02 At-risk of underweight Justification/Implications: • Sensitive to acute under-nutrition • Also can reflect long-term status • • • Goal: Promote adequate weight gain Intervention: Counsel families in making nutritionally balanced food choices Monitor regularly
103. 02 At-risk of underweight Justification/Implications: • Sensitive to acute under-nutrition • Also can reflect long-term status • • • Goal: Promote adequate weight gain Intervention: Counsel families in making nutritionally balanced food choices Monitor regularly
 113+ High risk overweight/obese Definition (C 2 -C 4) • At or above > 95 th percentile BMI-for-age OR >95 th percentile weight-for-stature CDC gender specific growth charts Problematic feeding practices – Excessive energy intake – Decreased energy expenditure, lifestyle – Impaired regulation of energy metabolism LANGUAGE: Provide sensitivity, compassion, and a conviction that this is an important, treatable chronic medical problem. Focus on future benefit shown to be effective. AMA recommends use of ‘obese & overweight’ in assessment & documentation only. –
113+ High risk overweight/obese Definition (C 2 -C 4) • At or above > 95 th percentile BMI-for-age OR >95 th percentile weight-for-stature CDC gender specific growth charts Problematic feeding practices – Excessive energy intake – Decreased energy expenditure, lifestyle – Impaired regulation of energy metabolism LANGUAGE: Provide sensitivity, compassion, and a conviction that this is an important, treatable chronic medical problem. Focus on future benefit shown to be effective. AMA recommends use of ‘obese & overweight’ in assessment & documentation only. –
 113+ High risk overweight/obese Justification/Implications • Goals: Achieve normal growth and development • Reduce risk of adolescent and adult obesity and obesity-related chronic disease • Intervention: – Choose food high in nutritional quality – Avoid unnecessary or excessive amounts of calorie rich foods and beverages – Increase age-appropriate physical activity/ Reduce inactivity Remember: Overweight is a chronic medical problem that can be treated.
113+ High risk overweight/obese Justification/Implications • Goals: Achieve normal growth and development • Reduce risk of adolescent and adult obesity and obesity-related chronic disease • Intervention: – Choose food high in nutritional quality – Avoid unnecessary or excessive amounts of calorie rich foods and beverages – Increase age-appropriate physical activity/ Reduce inactivity Remember: Overweight is a chronic medical problem that can be treated.
 114 Overweight or At-risk of overweight Definition: Overweight - Children ≥ 24 months of age, at or above the 85 th and below the 95 th percentile BMI-for-age (CDC) At Risk of Overweight: Have 1+ risk factors for at-risk of overweight Infants˂ 12 months Biological mother BMI ≥ 30 at conception or 1 st trimester, Self-reported or HCP measurement • Children ≥ 12 months Biological mother BMI ≥ 30 at certification, Self-reported pre-pregnancy BMI or staff measures taken at certification (not PG or delivered in past 6 mo. ) • Infants or Children, Biological father with BMI ≥ 30 at certification, Self-reported BMI or staff measurements taken at certification
114 Overweight or At-risk of overweight Definition: Overweight - Children ≥ 24 months of age, at or above the 85 th and below the 95 th percentile BMI-for-age (CDC) At Risk of Overweight: Have 1+ risk factors for at-risk of overweight Infants˂ 12 months Biological mother BMI ≥ 30 at conception or 1 st trimester, Self-reported or HCP measurement • Children ≥ 12 months Biological mother BMI ≥ 30 at certification, Self-reported pre-pregnancy BMI or staff measures taken at certification (not PG or delivered in past 6 mo. ) • Infants or Children, Biological father with BMI ≥ 30 at certification, Self-reported BMI or staff measurements taken at certification
 114 Overweight or At-risk of overweight Justification/Implications Parental obesity +/or genetic predisposition increases risk of overweight in preschoolers, even in the absence of other overt signs of increasing body mass – – BUT is Not inevitable Environmental and other factors mediate the relationship Intervention: – – – Positive Encouragement Food choices, family fun activities Appropriate referrals for entire family
114 Overweight or At-risk of overweight Justification/Implications Parental obesity +/or genetic predisposition increases risk of overweight in preschoolers, even in the absence of other overt signs of increasing body mass – – BUT is Not inevitable Environmental and other factors mediate the relationship Intervention: – – – Positive Encouragement Food choices, family fun activities Appropriate referrals for entire family
 115 High Weight-for-Length-New Definition: Infants and children less than 24 months of age, ≥ 97. 7 th percentile weight-for-length WHO gender specific growth charts
115 High Weight-for-Length-New Definition: Infants and children less than 24 months of age, ≥ 97. 7 th percentile weight-for-length WHO gender specific growth charts
 115 High Weight-for-Length Justification/Implication • Client-Centered Counseling – – Supportive, empathetic, nonjudgmental, and culturally appropriate Suggested language (AMA Expert Committee Report): • • – High weight-for-length ? Weight disproportional to height, Excess weight Evaluate & assist: • • • Recognition of satiety cues Non-Food Ways to comfort a child Behavior modeling
115 High Weight-for-Length Justification/Implication • Client-Centered Counseling – – Supportive, empathetic, nonjudgmental, and culturally appropriate Suggested language (AMA Expert Committee Report): • • – High weight-for-length ? Weight disproportional to height, Excess weight Evaluate & assist: • • • Recognition of satiety cues Non-Food Ways to comfort a child Behavior modeling
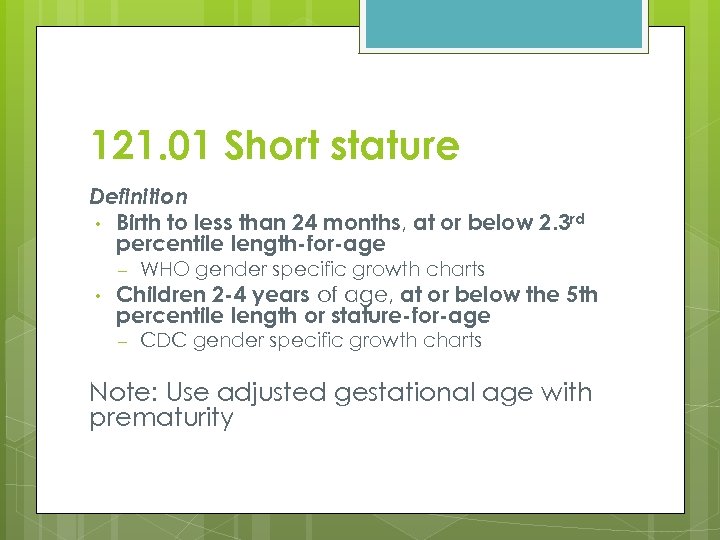 121. 01 Short stature Definition • Birth to less than 24 months, at or below 2. 3 rd percentile length-for-age – • WHO gender specific growth charts Children 2 -4 years of age, at or below the 5 th percentile length or stature-for-age – CDC gender specific growth charts Note: Use adjusted gestational age with prematurity
121. 01 Short stature Definition • Birth to less than 24 months, at or below 2. 3 rd percentile length-for-age – • WHO gender specific growth charts Children 2 -4 years of age, at or below the 5 th percentile length or stature-for-age – CDC gender specific growth charts Note: Use adjusted gestational age with prematurity
 121. 01 Short stature Justification/Implications – Abnormally low – – Prolonged undernutrition or repeated illness Inadequate protein, with poor diet quality Metabolic conditions, FAS NOTE per WHO study: Ethnic & racial differences
121. 01 Short stature Justification/Implications – Abnormally low – – Prolonged undernutrition or repeated illness Inadequate protein, with poor diet quality Metabolic conditions, FAS NOTE per WHO study: Ethnic & racial differences
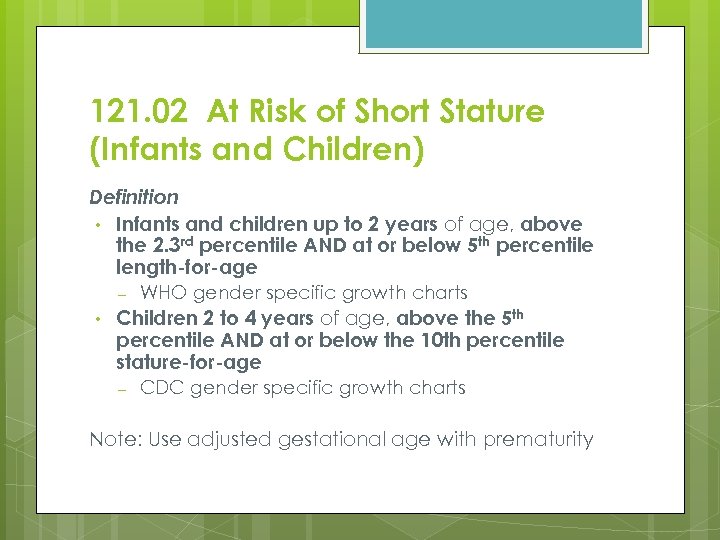 121. 02 At Risk of Short Stature (Infants and Children) Definition • Infants and children up to 2 years of age, above the 2. 3 rd percentile AND at or below 5 th percentile length-for-age – • WHO gender specific growth charts Children 2 to 4 years of age, above the 5 th percentile AND at or below the 10 th percentile stature-for-age – CDC gender specific growth charts Note: Use adjusted gestational age with prematurity
121. 02 At Risk of Short Stature (Infants and Children) Definition • Infants and children up to 2 years of age, above the 2. 3 rd percentile AND at or below 5 th percentile length-for-age – • WHO gender specific growth charts Children 2 to 4 years of age, above the 5 th percentile AND at or below the 10 th percentile stature-for-age – CDC gender specific growth charts Note: Use adjusted gestational age with prematurity
 121. 02 At Risk of Short Stature (Infants and Children) Justification/Implications (same as 121. 01 • Related to: – – Lack of total dietary energy Inadequate protein, due to poor diet quality Intervention: • Thorough dietary assessment • Possible HCP referral • Monitor growth with frequent F/U
121. 02 At Risk of Short Stature (Infants and Children) Justification/Implications (same as 121. 01 • Related to: – – Lack of total dietary energy Inadequate protein, due to poor diet quality Intervention: • Thorough dietary assessment • Possible HCP referral • Monitor growth with frequent F/U
 152 Low head circumference Definition • Birth to less than 24 months, at or below the 2. 3 rd percentile head circumferencefor-age – WHO gender specific growth charts
152 Low head circumference Definition • Birth to less than 24 months, at or below the 2. 3 rd percentile head circumferencefor-age – WHO gender specific growth charts
 152 Low head circumference Justification/Implications • Associated with: – Pre-term birth or Very low birth weight – Potential risk for neurocognitive abilities in light of other factors – – Genetic, nutrition, health, Socioeconomic status factors LHC not necessarily Abnormal head size Intervention: Consider medical referral when improvement is slow to respond to dietary interventions –
152 Low head circumference Justification/Implications • Associated with: – Pre-term birth or Very low birth weight – Potential risk for neurocognitive abilities in light of other factors – – Genetic, nutrition, health, Socioeconomic status factors LHC not necessarily Abnormal head size Intervention: Consider medical referral when improvement is slow to respond to dietary interventions –
 344+ Thyroid disorders Definition • Diagnosed hyperthyroidism (↑ levels) • Diagnosed hypothyroidism (↓ levels) • Diagnosed postpartum thyroiditis in 1 st year post-delivery (thyroid dysfunction)
344+ Thyroid disorders Definition • Diagnosed hyperthyroidism (↑ levels) • Diagnosed hypothyroidism (↓ levels) • Diagnosed postpartum thyroiditis in 1 st year post-delivery (thyroid dysfunction)
 344+ Thyroid disorders Justification/Implications -Hyperthyroidism: ↓ weight despite ↑ appetite -Hypothyroidism: ↑ weight For both : Monitor weight and diet Intervention: Reinforce & Support medical dietary therapy -Maternal needs for iodine increase PG hyperthyroidism relatively uncommon Encourage iodine sufficiency, Iodine-rich foods 150 mcg in prenatal supplements Promote breastfeeding, Discourage smoking Use soy with caution
344+ Thyroid disorders Justification/Implications -Hyperthyroidism: ↓ weight despite ↑ appetite -Hypothyroidism: ↑ weight For both : Monitor weight and diet Intervention: Reinforce & Support medical dietary therapy -Maternal needs for iodine increase PG hyperthyroidism relatively uncommon Encourage iodine sufficiency, Iodine-rich foods 150 mcg in prenatal supplements Promote breastfeeding, Discourage smoking Use soy with caution
 351+ Inborn errors of metabolism Definition: Gene mutations or deletions that alter metabolism of proteins, carbs, or fats • IEMS include, but are not limited to: Fructoaldolase deficiency Galactokinas deficiency Galactosemia Glutaric aciduria Glycogen storage disease Histidinemia Homocystinuria Hyperlipoproteinemia – – – – Hypermethioninemia Maple syrup urine disease Medium-chain acyl-Co. A dehydrogenase (MCAD), Methylmalonic academia, Phenylketonuria (PKU), Propionic academia Tyrosinemia Urea cycle disorders Additional information may be found at http: //rarediseases. onfo. nih. gov/GARD
351+ Inborn errors of metabolism Definition: Gene mutations or deletions that alter metabolism of proteins, carbs, or fats • IEMS include, but are not limited to: Fructoaldolase deficiency Galactokinas deficiency Galactosemia Glutaric aciduria Glycogen storage disease Histidinemia Homocystinuria Hyperlipoproteinemia – – – – Hypermethioninemia Maple syrup urine disease Medium-chain acyl-Co. A dehydrogenase (MCAD), Methylmalonic academia, Phenylketonuria (PKU), Propionic academia Tyrosinemia Urea cycle disorders Additional information may be found at http: //rarediseases. onfo. nih. gov/GARD
 351+ Inborn errors of metabolism Justification/Implications • Can manifest at any stage of life • Early identification important Goal: Achieve normal growth and development Intervention: Reinforce & Support medical dietary therapy – – • Correct metabolic imbalance Ensure adequate energy, protein, and nutrients Continual monitoring – – – Nutrient intake – Need to follow prescribed dietary regime! Laboratory values Growth
351+ Inborn errors of metabolism Justification/Implications • Can manifest at any stage of life • Early identification important Goal: Achieve normal growth and development Intervention: Reinforce & Support medical dietary therapy – – • Correct metabolic imbalance Ensure adequate energy, protein, and nutrients Continual monitoring – – – Nutrient intake – Need to follow prescribed dietary regime! Laboratory values Growth
 Release Webcast July 26, 2012
Release Webcast July 26, 2012
 Questions?
Questions?
 THANK YOU!
THANK YOU!


