4ba7a4911633dbac58d3a96234406f8b.ppt
- Количество слайдов: 24
Who can really move the needle? Elizabeth C. Wick, M. D. © The Johns Hopkins University and The Johns Hopkins Health System Corporation, 2011
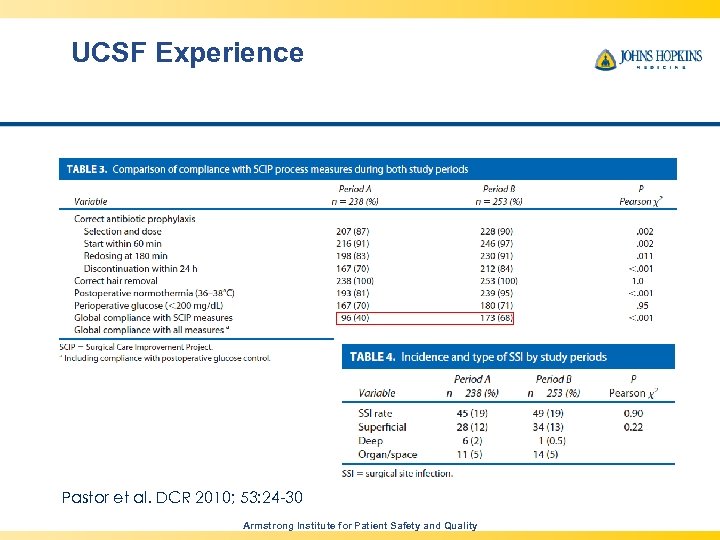
UCSF Experience Pastor et al. DCR 2010; 53: 24 -30 Armstrong Institute for Patient Safety and Quality
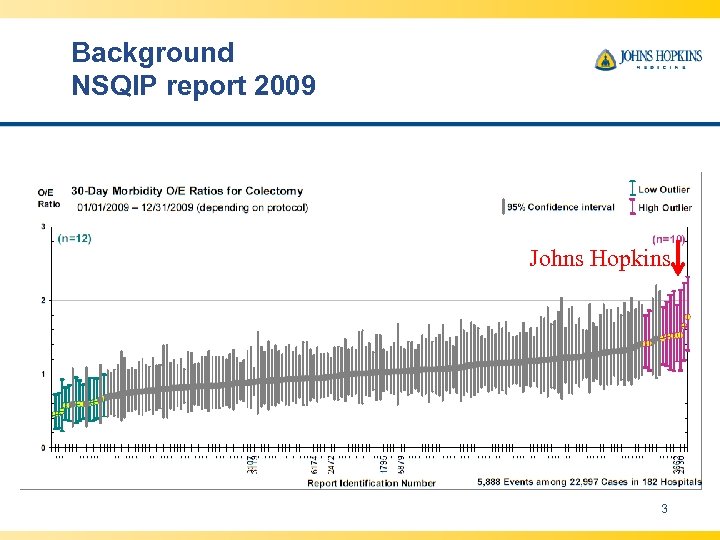
Background NSQIP report 2009 Johns Hopkins 3
The Vision of CUSP The Comprehensive Unit-based Safety Program is designed to: – Improve patient safety awareness and systems thinking at the unit level – Mobilize staff to identify and resolve patient safety issues – Create a patient safety partnership between executives and frontline caregivers – Provide tools to help CUSP teams investigate and learn from defects and improve teamwork and safety culture 4
Successful Efforts to Reduce Preventable Harm Johns Hopkins ICU program 1 Michigan Keystone ICU program 2, 3 National On the CUSP: Stop BSI program Reductions in central line-associated blood stream infections (CLABSI) 1. 2. 3. Crit Care Med. 2004; 32: 2014 -20. N Engl J Med 2006; 355: 2725 -32. BMJ 2010; 340: c 309.
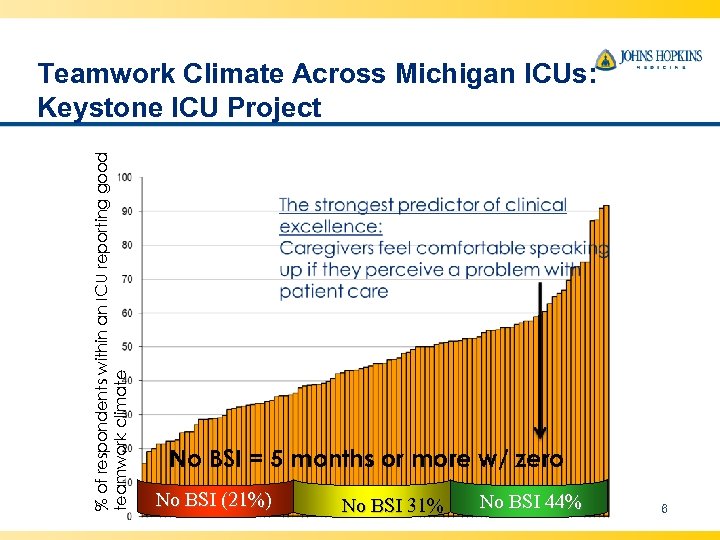
% of respondents within an ICU reporting good teamwork climate Teamwork Climate Across Michigan ICUs: Keystone ICU Project No BSI = 5 months or more w/ zero No BSI (21%) No BSI 31% No BSI 44% 6
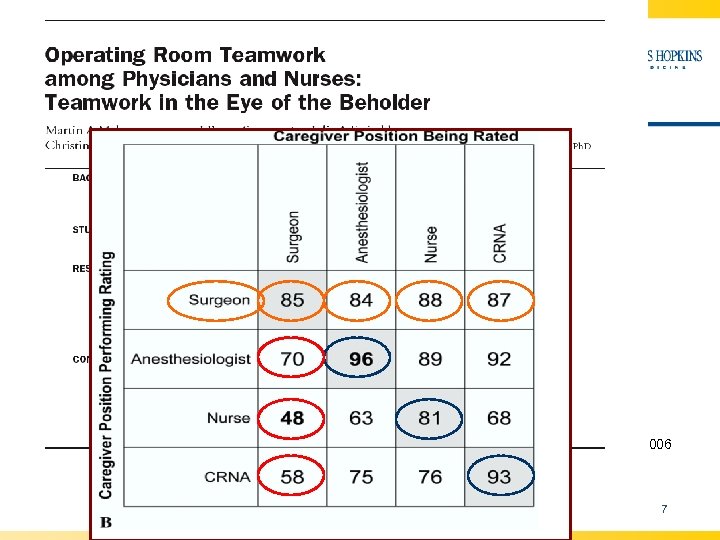
Perceptions of Teamwork Vary Among Operating Room Providers Makary et al. JACS 2006 7 Armstrong Institute for Patient Safety and Quality
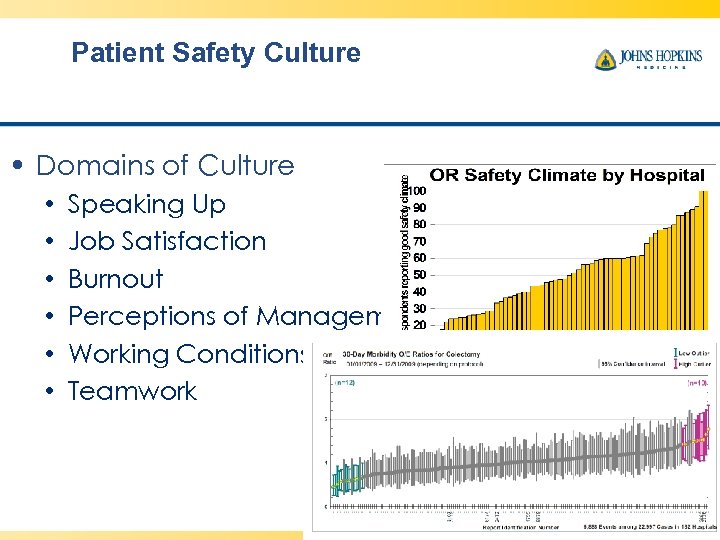
Patient Safety Culture • Domains of Culture • • • Speaking Up Job Satisfaction Burnout Perceptions of Management Working Conditions Teamwork Makary M, et al. , Annals of Surgery, 2006
COLORECTAL SURGERY CUSP Armstrong Institute for Patient Safety and Quality
CUSP Steps 1. Educate everyone in the Science of Safety 2. Identify defects 3. Recruit executive as active SUSP team member 4. Learn from one defect per quarter 5. Implement teamwork tools Timmel, et al. 2010.
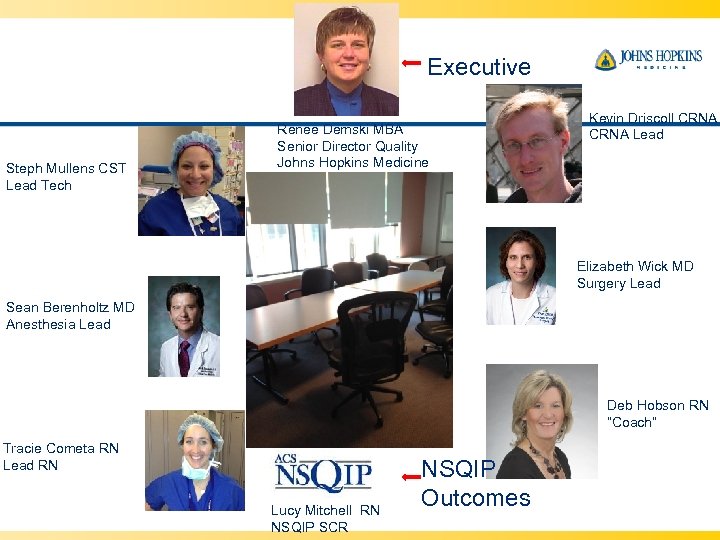
Executive Steph Mullens CST Lead Tech Renee Demski MBA Senior Director Quality Johns Hopkins Medicine Kevin Driscoll CRNA Lead Elizabeth Wick MD Surgery Lead Sean Berenholtz MD Anesthesia Lead Deb Hobson RN “Coach” Tracie Cometa RN Lead RN Lucy Mitchell RN NSQIP SCR NSQIP Outcomes
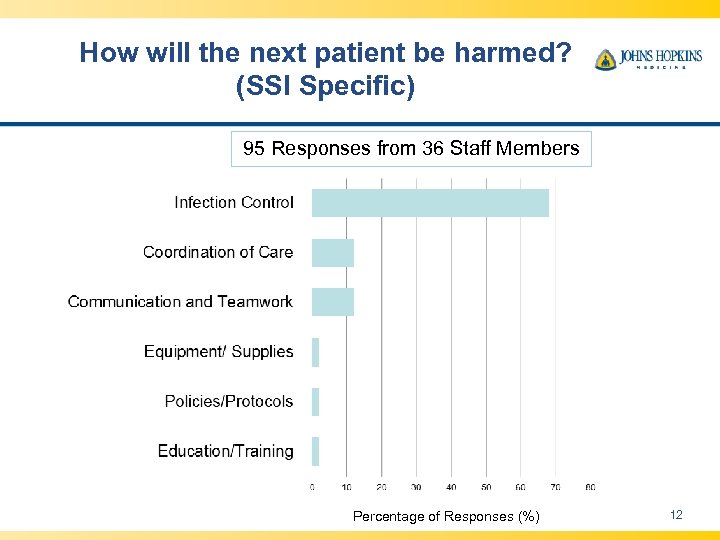
How will the next patient be harmed? (SSI Specific) 95 Responses from 36 Staff Members Percentage of Responses (%) 12
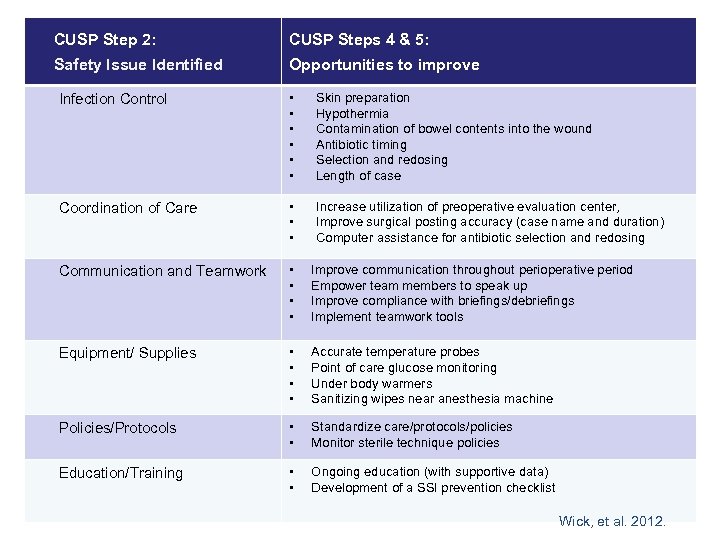
CUSP Step 2: CUSP Steps 4 & 5: Safety Issue Identified Opportunities to improve Infection Control • • • Skin preparation Hypothermia Contamination of bowel contents into the wound Antibiotic timing Selection and redosing Length of case Coordination of Care • • • Increase utilization of preoperative evaluation center, Improve surgical posting accuracy (case name and duration) Computer assistance for antibiotic selection and redosing Communication and Teamwork • • Improve communication throughout perioperative period Empower team members to speak up Improve compliance with briefings/debriefings Implement teamwork tools Equipment/ Supplies • • Accurate temperature probes Point of care glucose monitoring Under body warmers Sanitizing wipes near anesthesia machine Policies/Protocols • • Standardize care/protocols/policies Monitor sterile technique policies Education/Training • • Ongoing education (with supportive data) Development of a SSI prevention checklist Wick, et al. 2012. 13
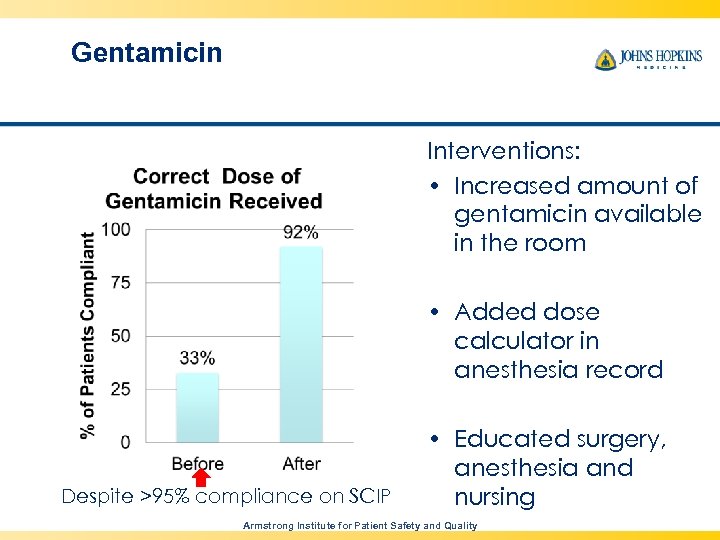
Gentamicin Interventions: • Increased amount of gentamicin available in the room • Added dose calculator in anesthesia record Despite >95% compliance on SCIP • Educated surgery, anesthesia and nursing in grand rounds Armstrong Institute for Patient Safety and Quality
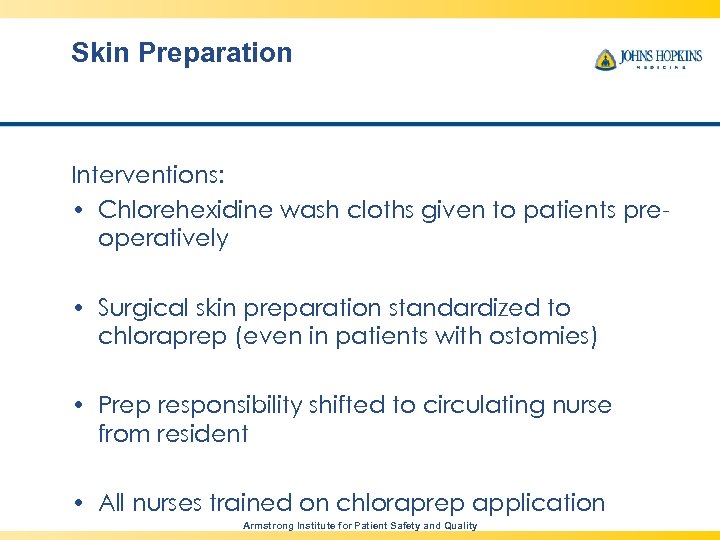
Skin Preparation Interventions: • Chlorehexidine wash cloths given to patients preoperatively • Surgical skin preparation standardized to chloraprep (even in patients with ostomies) • Prep responsibility shifted to circulating nurse from resident • All nurses trained on chloraprep application Armstrong Institute for Patient Safety and Quality
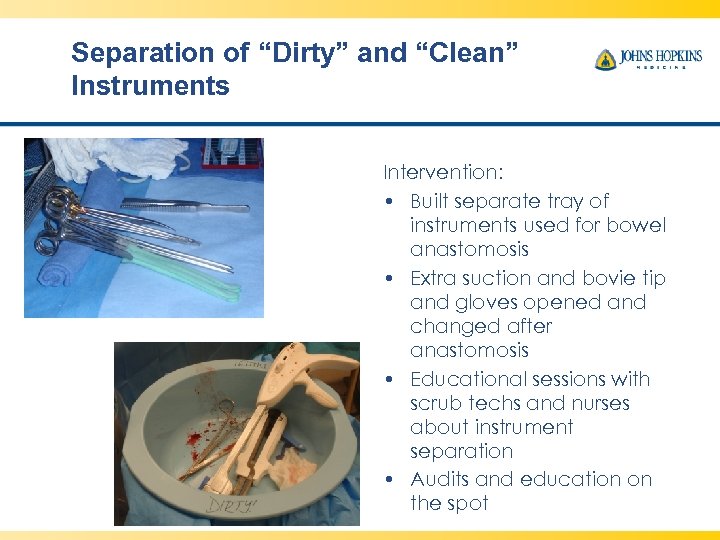
Separation of “Dirty” and “Clean” Instruments Intervention: • Built separate tray of instruments used for bowel anastomosis • Extra suction and bovie tip and gloves opened and changed after anastomosis • Educational sessions with scrub techs and nurses about instrument separation • Audits and education on the spot
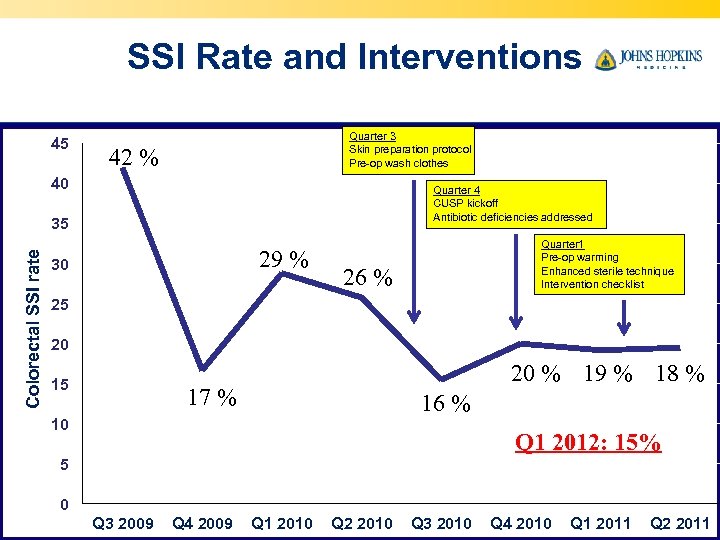
SSI Rate and Interventions 45 Quarter 3 Skin preparation protocol Pre-op wash clothes 42 % 40 Quarter 4 CUSP kickoff Antibiotic deficiencies addressed Colorectal SSI rate 35 29 % 30 Quarter 1 Pre-op warming Enhanced sterile technique Intervention checklist 26 % 25 20 15 20 % 19 % 18 % 17 % 16 % 10 Q 1 2012: 15% 5 0 Q 3 2009 Q 4 2009 Q 1 2010 Q 2 2010 Q 3 2010 Q 4 2010 Q 1 2011 Q 2 2011
HIGHLIGHTS FROM YEAR 2 EXPANDING THE SCOPE 18 Armstrong Institute for Patient Safety and Quality
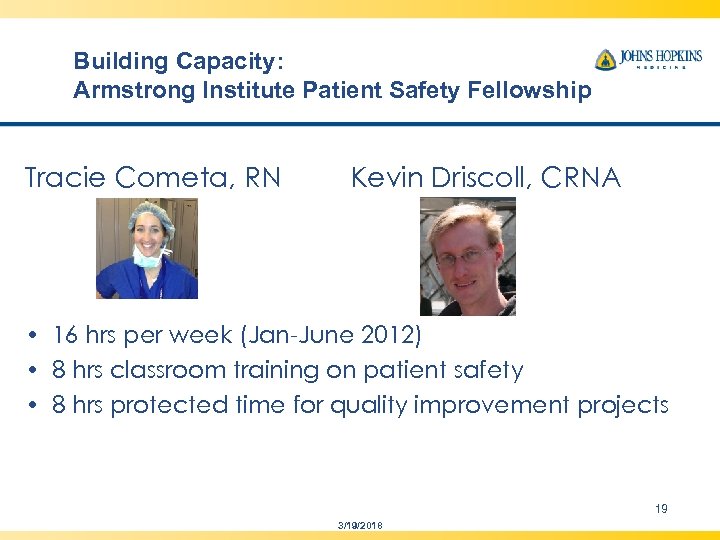
Building Capacity: Armstrong Institute Patient Safety Fellowship Tracie Cometa, RN Kevin Driscoll, CRNA • 16 hrs per week (Jan-June 2012) • 8 hrs classroom training on patient safety • 8 hrs protected time for quality improvement projects 19 3/19/2018
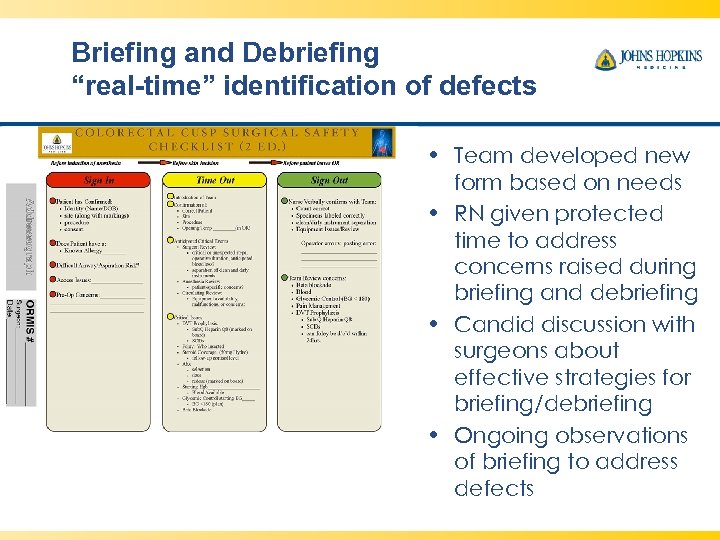
Briefing and Debriefing “real-time” identification of defects • Team developed new form based on needs • RN given protected time to address concerns raised during briefing and debriefing • Candid discussion with surgeons about effective strategies for briefing/debriefing • Ongoing observations of briefing to address defects
Hidden Cost-Savings Antibiotic Irrigation • Frontline providers questioned the inconsistency in use of antibiotic irrigation between surgeons • Solution: if effective, advocate for consistent use and if not proven stop using • NO EVIDENCE TO SUPPORT USE • $537, 000/ year on antibiotic irrigation • Obtained surgeon and leadership buy-in for removing it from hospital formulary Armstrong Institute for Patient Safety and Quality
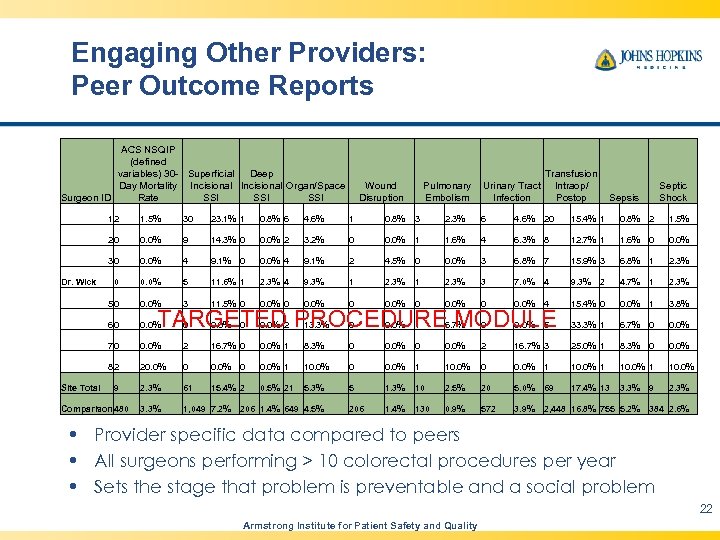
Engaging Other Providers: Peer Outcome Reports ACS NSQIP (defined variables) 30 - Superficial Deep Day Mortality Incisional Organ/Space Surgeon ID Rate SSI SSI Wound Disruption Pulmonary Embolism Urinary Tract Infection Transfusion Intraop/ Postop Sepsis Septic Shock 12 23. 1% 1 0. 8% 6 4. 6% 1 0. 8% 3 2. 3% 6 4. 6% 20 15. 4% 1 0. 8% 2 1. 5% 0. 0% 9 14. 3% 0 0. 0% 2 3. 2% 0 0. 0% 1 1. 6% 4 6. 3% 8 12. 7% 1 1. 6% 0 0. 0% 30 0. 0% 4 9. 1% 2 4. 5% 0 0. 0% 3 6. 8% 7 15. 9% 3 6. 8% 1 2. 3% 0 0. 0% 5 11. 6% 1 2. 3% 4 9. 3% 1 2. 3% 3 7. 0% 4 9. 3% 2 4. 7% 1 2. 3% 50 0. 0% 3 11. 5% 0 0. 0% 4 15. 4% 0 0. 0% 1 3. 8% 60 0. 0% 2 13. 3% 0 0. 0% 1 6. 7% 0 0. 0% 5 33. 3% 1 6. 7% 0 0. 0% 70 0. 0% 2 16. 7% 0 0. 0% 1 8. 3% 0 0. 0% 2 16. 7% 3 25. 0% 1 8. 3% 0 0. 0% 82 Site Total 30 20 Dr. Wick 1. 5% 20. 0% 0 0. 0% 1 10. 0% 2. 3% 61 15. 4% 2 0. 5% 21 5. 3% 5 1. 3% 10 2. 5% 20 5. 0% 69 17. 4% 13 3. 3% 9 2. 3% 3. 3% 1, 049 7. 2% 206 1. 4% 649 4. 5% 206 1. 4% 130 0. 9% 572 3. 9% 2, 448 16. 8% 755 5. 2% 384 2. 6% 9 Comparison 480 TARGETED PROCEDURE MODULE • Provider specific data compared to peers • All surgeons performing > 10 colorectal procedures per year • Sets the stage that problem is preventable and a social problem 22 Armstrong Institute for Patient Safety and Quality
Lessons Learned • Harm is preventable • Change can not be “top down” • CUSP sends a clear message, all provider opinions and ideas are important and essential for improvement • Better teamwork better outcomes better culture and teamwork • Positive culture empowers frontline staff to take ownership of patient safety and achieve unprecedented improvements • It takes time and commitment
Johns Hopkins Hospital Motto Our experience: hospital level interventions(SCIP) pale in comparison to interventions at the work unit level (CUSP) We embrace local wisdom in the Colorectal OR’s 24 © JHU and JHHS, 2009
4ba7a4911633dbac58d3a96234406f8b.ppt