870e8957020b33217047e3f68006f548.ppt
- Количество слайдов: 31
What was different about the Fall. Safe approach? 1. 2. 3. 4. It was evidence-based It prioritised the things we struggle with It was multidisciplinary The basic equipment they would need was made available

What was different about the Fall. Safe approach? 1. 2. 3. 4. 5. It was evidence-based It prioritised the things we struggle with It was multidisciplinary Basic equipment available The care bundle was implemented in stages rather than all at once 6. We measured delivery at least every month
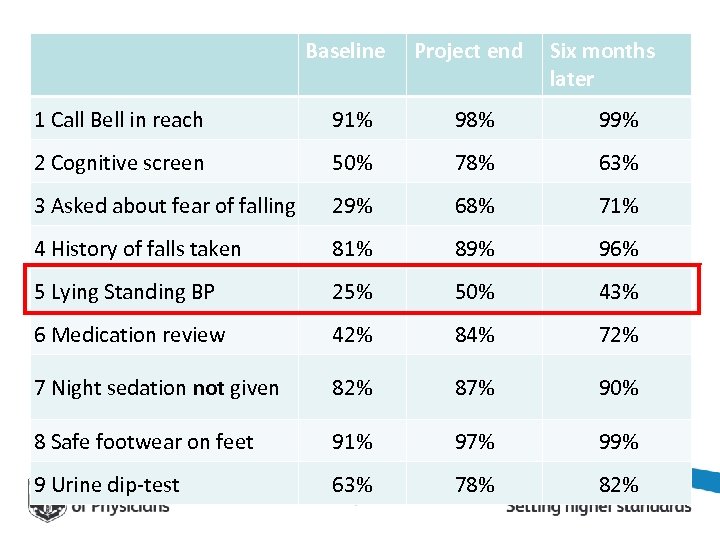
Baseline Project end Six months later 1 Call Bell in reach 91% 98% 99% 2 Cognitive screen 50% 78% 63% 3 Asked about fear of falling 29% 68% 71% 4 History of falls taken 81% 89% 96% 5 Lying Standing BP 25% 50% 43% 6 Medication review 42% 84% 72% 7 Night sedation not given 82% 87% 90% 8 Safe footwear on feet 91% 97% 99% 9 Urine dip-test 63% 78% 82%

What was different about the Fall. Safe approach? 1. 2. 3. 4. 5. 6. 7. It was evidence-based It prioritised the things we struggle with It was multidisciplinary Basic equipment available The care bundle was implemented in stages We measured delivery at least every month We didn’t expect results to show overnight
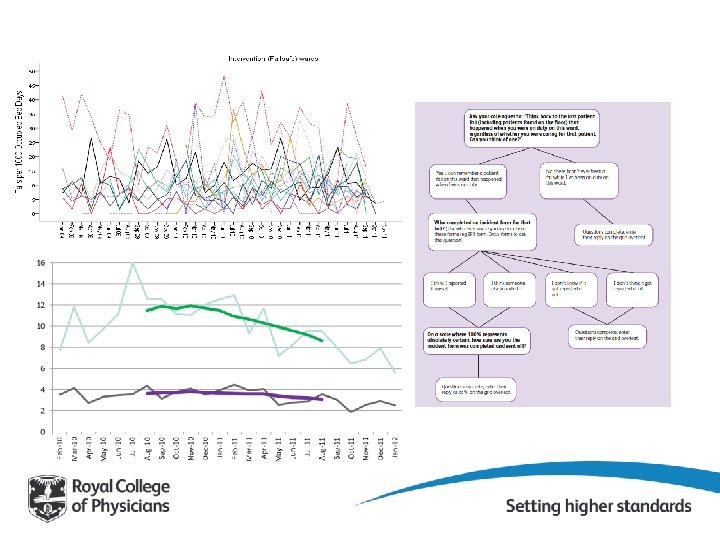
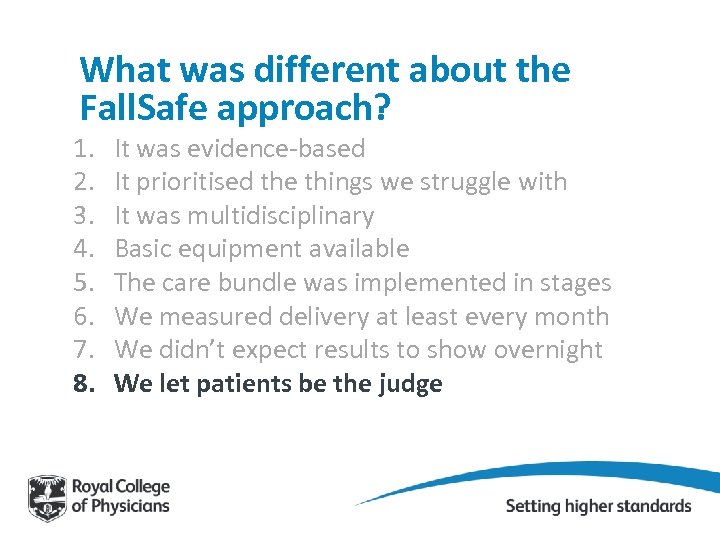
What was different about the Fall. Safe approach? 1. 2. 3. 4. 5. 6. 7. 8. It was evidence-based It prioritised the things we struggle with It was multidisciplinary Basic equipment available The care bundle was implemented in stages We measured delivery at least every month We didn’t expect results to show overnight We let patients be the judge


What was different about the Fall. Safe approach? 1. 2. 3. 4. 5. 6. 7. 8. 9. It was evidence-based It prioritised the things we struggle with It was multidisciplinary Basic equipment available The care bundle was implemented in stages We measured delivery at least every month We didn’t expect results to show overnight We let patients be the judge We created a ‘safe space’
Peer support and challenge “It’s a safe environment to talk about it – no one is standing over you saying ‘why have you had ten falls? ’ – so you can really think about what can prevent them” “Where do you buy your slippersocks? ” “If we can do it, surely you can!”
Changing mindsets “It used to be just one of those things you expected to happen; now it’s a big deal if a patient does fall and everyone will be thinking, ok, let’s try this or that – we know we can do something about it”
What was different about the Fall. Safe approach? 1. It was evidence-based 2. It prioritised the things we struggle with 3. It was multidisciplinary 4. Basic equipment available 5. The care bundle was implemented in stages 6. We measured delivery at least every month 7. We didn’t expect results to show overnight 8. We let patients be the judge 9. We created a ‘safe space’ 10. We gave each Fall. Safe lead enough education and support to make them confident and knowledgeable
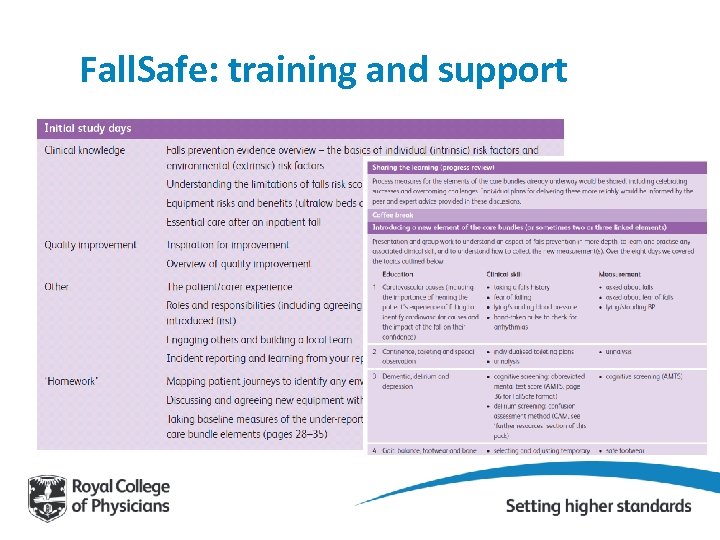
Fall. Safe: training and support
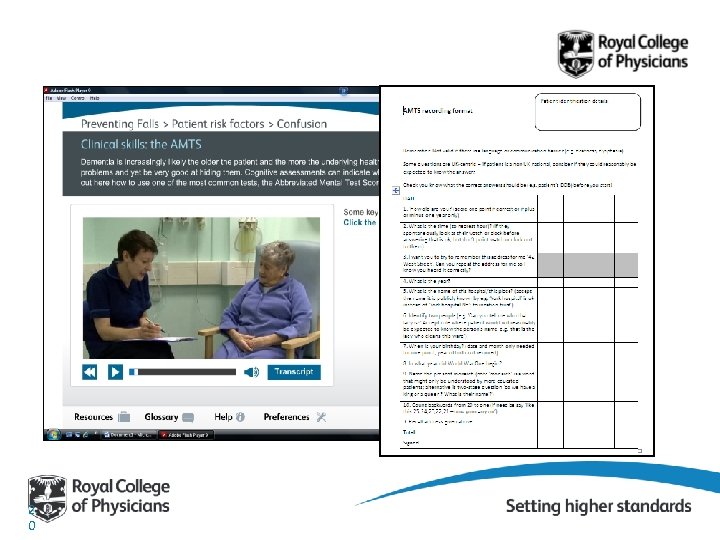
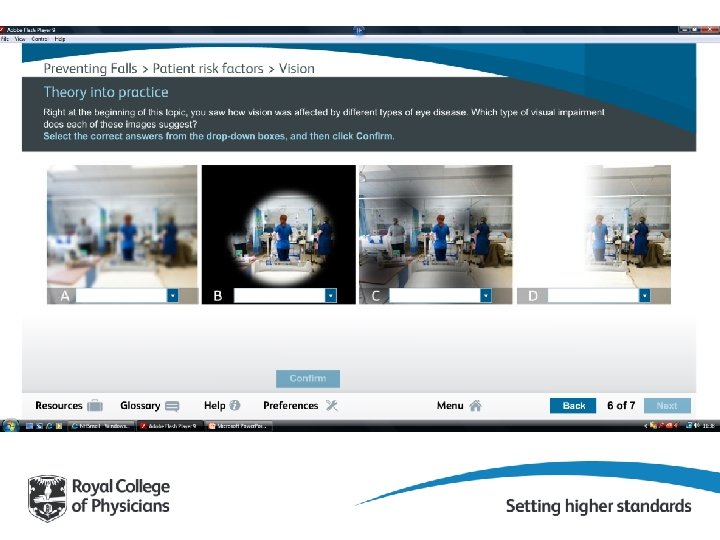
e. Learning focused on nurses’ role
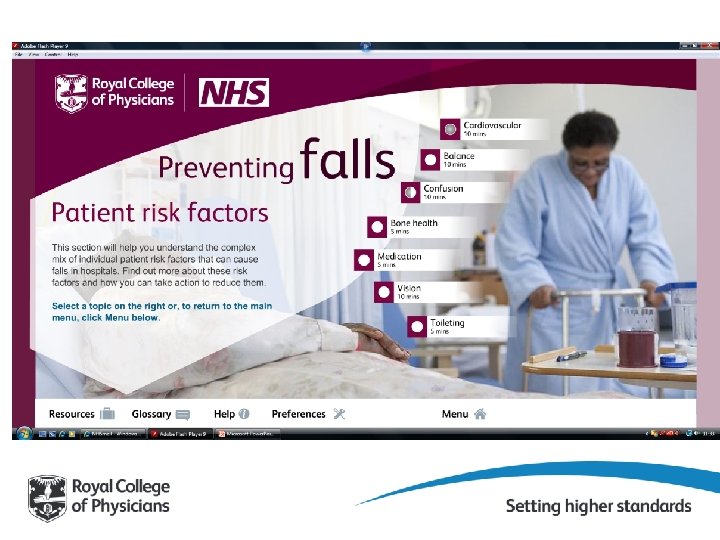
Starting point for some Fall. Safe units “ Oh yes, the Occupational Therapists always do MMSE – they’ll be in the OT notes in their office somewhere” “That’s a doctors’ job” “We would do an AMTS when we notice that a patient’s confused…. . ” 1 9
2 0
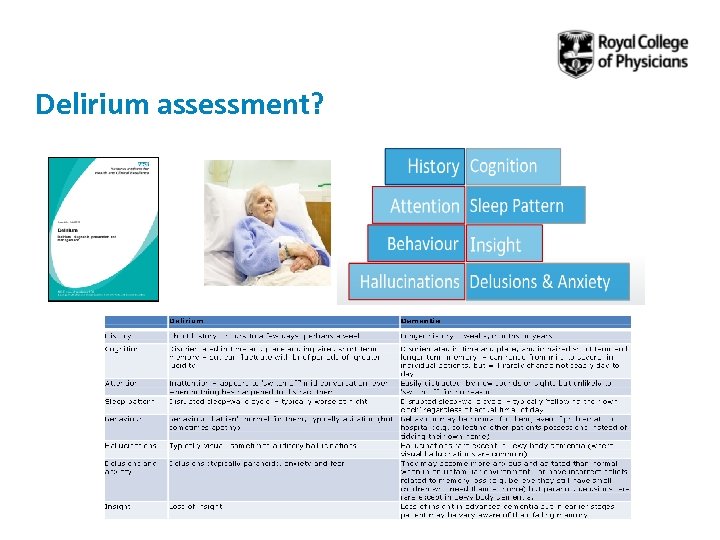
Delirium assessment?
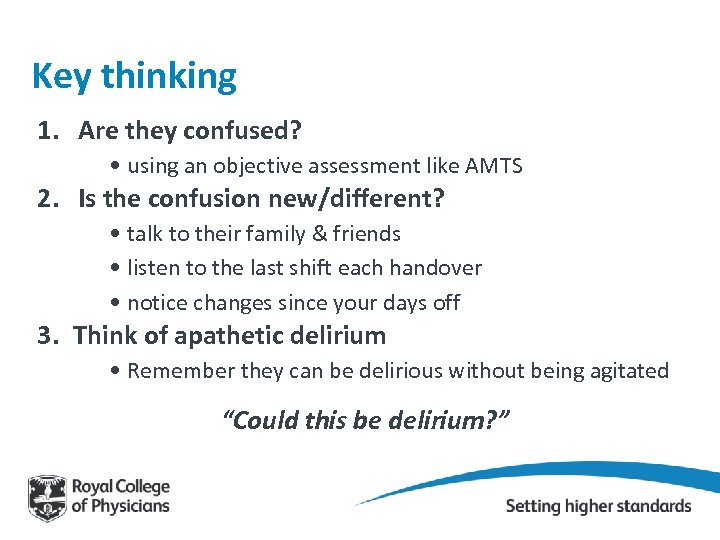
Key thinking 1. Are they confused? • using an objective assessment like AMTS 2. Is the confusion new/different? • talk to their family & friends • listen to the last shift each handover • notice changes since your days off 3. Think of apathetic delirium • Remember they can be delirious without being agitated “Could this be delirium? ”
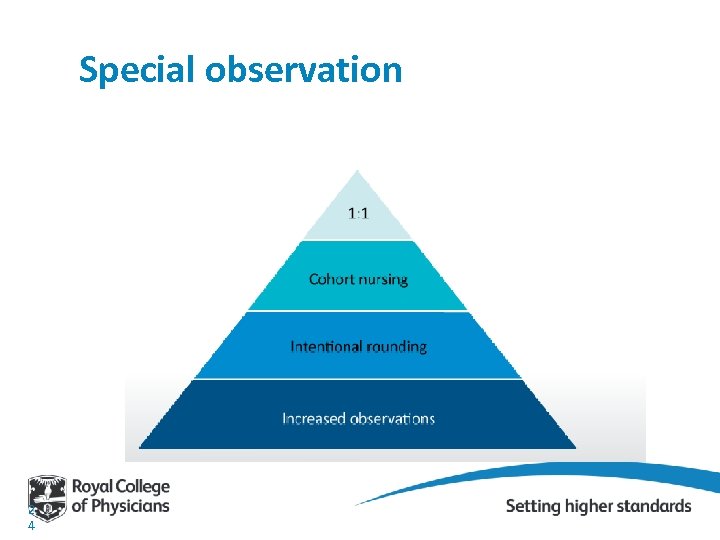
Special observation 2 4
Intentional rounding: if you do use Don’t standardise, individualise Minimise documentation Remember: – Communication skills in dementia – An hour is a long time
Leadership commitment…… “I’d like to do Fall. Safe in my hospital, but we won’t be able to give staff for any training” “ Two hours of e. Learning is a bit much – can’t you do a version that covers everything in 15 minutes? ”
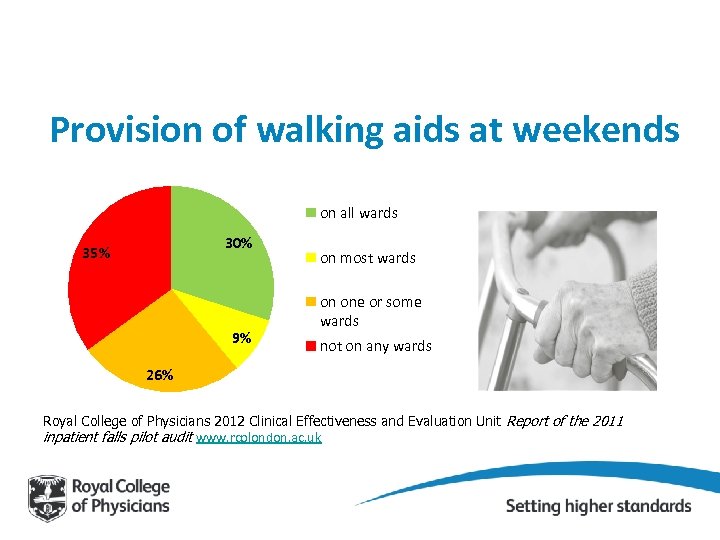
Provision of walking aids at weekends on all wards 30% 35% 9% on most wards on one or some wards not on any wards 26% Royal College of Physicians 2012 Clinical Effectiveness and Evaluation Unit Report of the 2011 inpatient falls pilot audit www. rcplondon. ac. uk
Sometimes falls is not the priority • • 50 bed unit No permanent unit manager in post 30 -40% temporary staff Three Fall. Safe leads left in quick succession
You will meet most of your patients again…. . 2001 census People aged 75 years or more 3, 704, 945 Hospital admission statistics 2006 People aged 75 years or more admitted as inpatients 3, 174, 676
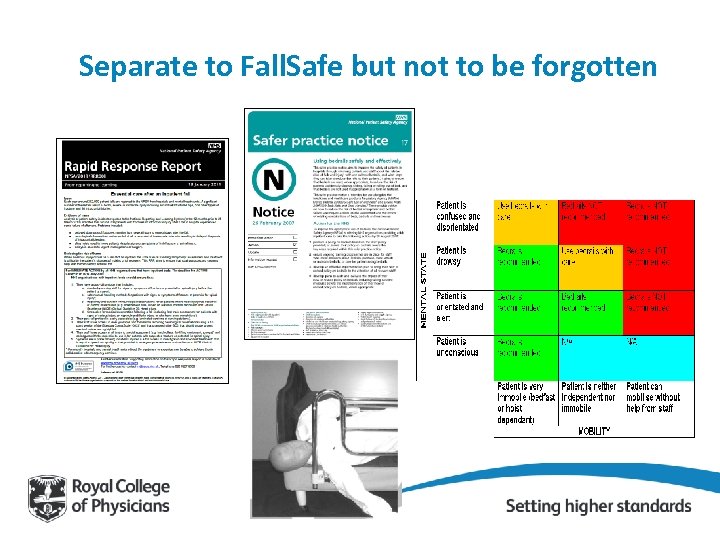
Separate to Fall. Safe but not to be forgotten
Last words Questions and comment? frances. healey@nhs. net @Frances. Healey
870e8957020b33217047e3f68006f548.ppt