dbc22231d99862dcf23edb48cac1bdb5.ppt
- Количество слайдов: 77
 What’s killing kids – AAPCC Death Cases Michael Wahl MD, FACEP, FACMT Medical Director, Illinois Poison Center Emergency Physician, Northshore University Healthsystems
What’s killing kids – AAPCC Death Cases Michael Wahl MD, FACEP, FACMT Medical Director, Illinois Poison Center Emergency Physician, Northshore University Healthsystems
 Disclosure • No financial interest • No business relationships with manufacturers, distributors or retailers of these products • No off-label use of products to be discussed
Disclosure • No financial interest • No business relationships with manufacturers, distributors or retailers of these products • No off-label use of products to be discussed
 AAPCC • Poison Control Centers provide treatment recommendations and follow up assessment for over 2. 4 million poison exposures per year. • All deaths reported to AAPCC are abstracted and the deaths with clear cause of death are published annually as short case reports
AAPCC • Poison Control Centers provide treatment recommendations and follow up assessment for over 2. 4 million poison exposures per year. • All deaths reported to AAPCC are abstracted and the deaths with clear cause of death are published annually as short case reports
 Hydrocarbons • 2 age groups affected • Route of exposure for each age group • Cause for morbidity and mortality for each age group
Hydrocarbons • 2 age groups affected • Route of exposure for each age group • Cause for morbidity and mortality for each age group
 Hydrocarbons - Toddlers (Garage and Kitchen Sink Tox) • 15 month old female found vomiting, cyanotic and in respiratory distress in the garage. The odor of gasoline was on the child
Hydrocarbons - Toddlers (Garage and Kitchen Sink Tox) • 15 month old female found vomiting, cyanotic and in respiratory distress in the garage. The odor of gasoline was on the child
 Hydrocarbons - Toddlers • 2 yo child ingested unknown amount of cigarette lighter fluid (Zippo)
Hydrocarbons - Toddlers • 2 yo child ingested unknown amount of cigarette lighter fluid (Zippo)
 Hydrocarbons - Toddlers • 18 month old child brought to ED after ingestion of pyrethrin insecticide that was >90% petroleum distillates
Hydrocarbons - Toddlers • 18 month old child brought to ED after ingestion of pyrethrin insecticide that was >90% petroleum distillates
 Hydrocarbons - Toddlers • 15 mo male ingested and aspirated tiki torch oil at home
Hydrocarbons - Toddlers • 15 mo male ingested and aspirated tiki torch oil at home
 Hydrocarbons • 33, 000 exposures reported to AAPCC (2013) • 10, 000 involved children • Low rate of admission and death
Hydrocarbons • 33, 000 exposures reported to AAPCC (2013) • 10, 000 involved children • Low rate of admission and death
 Acute Clinical Effects • CNS • GI • Respiratory
Acute Clinical Effects • CNS • GI • Respiratory
 Hydrocarbons • Important History: – Type of hydrocarbon (volatility, surface tension and viscosity) – When – How much (often unreliable) – Coughing – Vomiting (increases aspiration potential) – Behavior changes (lethargy, drowsiness)
Hydrocarbons • Important History: – Type of hydrocarbon (volatility, surface tension and viscosity) – When – How much (often unreliable) – Coughing – Vomiting (increases aspiration potential) – Behavior changes (lethargy, drowsiness)
 Hydrocarbons • Important signs and diagnostic exam results – Mental status – Respiratory status • Cough • Tachypnea • Grunting/Flaring/Retractions • Fever • Pulse ox • CXR
Hydrocarbons • Important signs and diagnostic exam results – Mental status – Respiratory status • Cough • Tachypnea • Grunting/Flaring/Retractions • Fever • Pulse ox • CXR
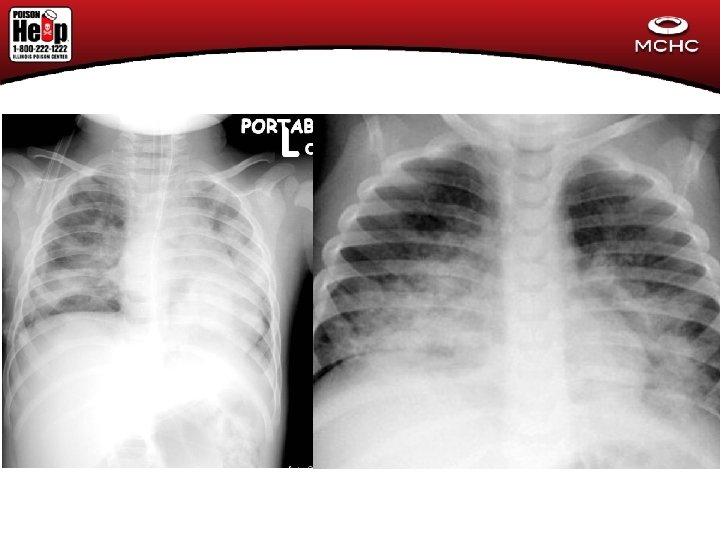
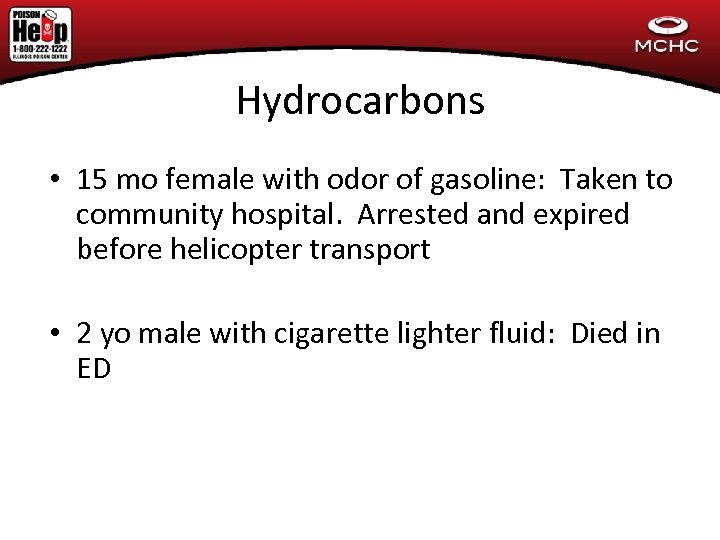 Hydrocarbons • 15 mo female with odor of gasoline: Taken to community hospital. Arrested and expired before helicopter transport • 2 yo male with cigarette lighter fluid: Died in ED
Hydrocarbons • 15 mo female with odor of gasoline: Taken to community hospital. Arrested and expired before helicopter transport • 2 yo male with cigarette lighter fluid: Died in ED
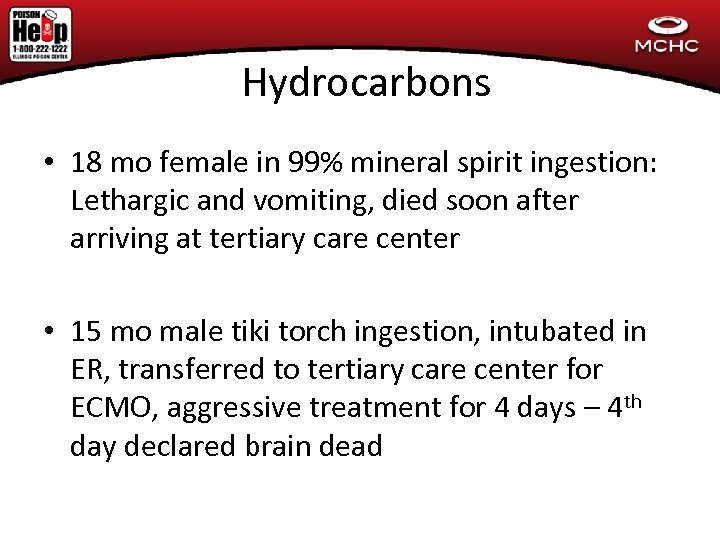 Hydrocarbons • 18 mo female in 99% mineral spirit ingestion: Lethargic and vomiting, died soon after arriving at tertiary care center • 15 mo male tiki torch ingestion, intubated in ER, transferred to tertiary care center for ECMO, aggressive treatment for 4 days – 4 th day declared brain dead
Hydrocarbons • 18 mo female in 99% mineral spirit ingestion: Lethargic and vomiting, died soon after arriving at tertiary care center • 15 mo male tiki torch ingestion, intubated in ER, transferred to tertiary care center for ECMO, aggressive treatment for 4 days – 4 th day declared brain dead
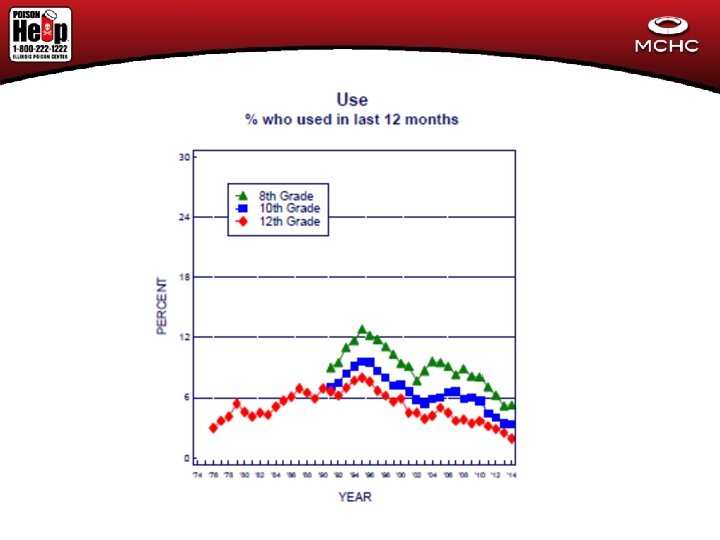
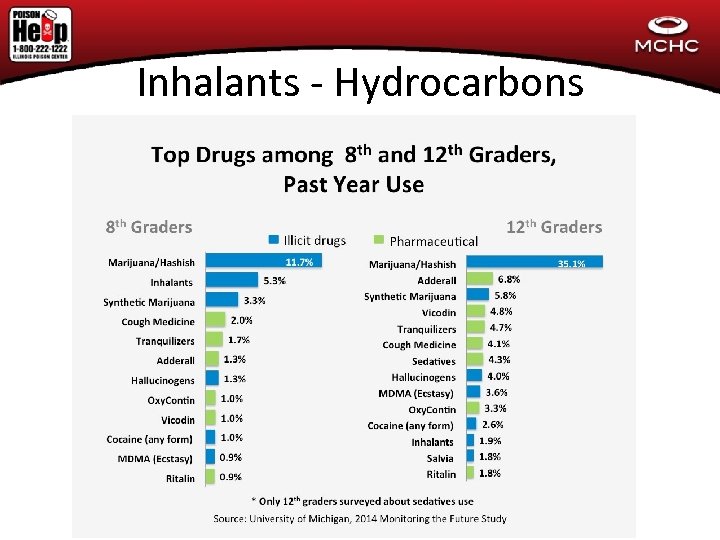 Inhalants - Hydrocarbons
Inhalants - Hydrocarbons
 Types of Abused Inhalants Hydrocarbons (examples out of 1000’s include) – Solvents/Volatile Chemicals • • – Gases Gasoline Strippers Lacquer Dry-cleaning fluids Carburetor Cleaners Correction Fluid Permanent Marker Model Glue www. mchc. org www. illinoispoisoncenter. org • Freon • Butane • Propane
Types of Abused Inhalants Hydrocarbons (examples out of 1000’s include) – Solvents/Volatile Chemicals • • – Gases Gasoline Strippers Lacquer Dry-cleaning fluids Carburetor Cleaners Correction Fluid Permanent Marker Model Glue www. mchc. org www. illinoispoisoncenter. org • Freon • Butane • Propane
 Hydrocarbons (Methylene Chloride, Toluene) www. mchc. org www. illinoispoisoncenter. org
Hydrocarbons (Methylene Chloride, Toluene) www. mchc. org www. illinoispoisoncenter. org
 Hydrocarbons www. mchc. org www. illinoispoisoncenter. org
Hydrocarbons www. mchc. org www. illinoispoisoncenter. org
 Hydrocarbons www. mchc. org www. illinoispoisoncenter. org
Hydrocarbons www. mchc. org www. illinoispoisoncenter. org
 Hydrocarbons www. mchc. org www. illinoispoisoncenter. org
Hydrocarbons www. mchc. org www. illinoispoisoncenter. org
 Hydrocarbons www. mchc. org www. illinoispoisoncenter. org
Hydrocarbons www. mchc. org www. illinoispoisoncenter. org
 Computer Dust Cleaner
Computer Dust Cleaner
 Why Inhalants Are Abused • Available – Home, school, groceries, hardware/home improvement stores • Legal purchased – No restriction to access (whipped cream cans) • Low Cost – Correction Fluid, butane lighters, nail polish remover, air freshener, cooking sprays, COMPUTER DUST CLEANER www. mchc. org www. illinoispoisoncenter. org
Why Inhalants Are Abused • Available – Home, school, groceries, hardware/home improvement stores • Legal purchased – No restriction to access (whipped cream cans) • Low Cost – Correction Fluid, butane lighters, nail polish remover, air freshener, cooking sprays, COMPUTER DUST CLEANER www. mchc. org www. illinoispoisoncenter. org
 Why Inhalants Are Abused • Immediate physiological effects – Works immediately unlike pills or alcohol • Short-acting Effects – Provides a short 1 to 5 minute high perfect for inbetween class breaks, bathroom use, school bus trips www. mchc. org www. illinoispoisoncenter. org
Why Inhalants Are Abused • Immediate physiological effects – Works immediately unlike pills or alcohol • Short-acting Effects – Provides a short 1 to 5 minute high perfect for inbetween class breaks, bathroom use, school bus trips www. mchc. org www. illinoispoisoncenter. org
 Why Inhalants Are Abused • Social Activity – Usually done in groups • Hard to detect – No easy “drug test” • Easy to Conceal – Butane lighter, small vials www. mchc. org www. illinoispoisoncenter. org
Why Inhalants Are Abused • Social Activity – Usually done in groups • Hard to detect – No easy “drug test” • Easy to Conceal – Butane lighter, small vials www. mchc. org www. illinoispoisoncenter. org
 Why Inhalants Are Abused • Unrecognized Dangers – Products are legal and the dangers were not well publicized • Paraphernalia – No needles, crack pipes, bongs needed. Plastic bags, rags, socks, bandanas and balloons are easily obtainable and not easily recognized as warning signs by adults www. mchc. org www. illinoispoisoncenter. org
Why Inhalants Are Abused • Unrecognized Dangers – Products are legal and the dangers were not well publicized • Paraphernalia – No needles, crack pipes, bongs needed. Plastic bags, rags, socks, bandanas and balloons are easily obtainable and not easily recognized as warning signs by adults www. mchc. org www. illinoispoisoncenter. org
 • Sniffing Methods of Abuse – Inhaling vapors directly from an open container (lowest concentration) • Huffing – Inhaling vapors from a volatile-soaked cloth held over face (medium concentration) • Bagging – Placing volatile substance in a bag and breathing into the bag (highest concentration) • Ballooning – Inhaling the contents of a balloon • Dusting – Inhaling the contents of computer dust cleaner www. mchc. org www. illinoispoisoncenter. org
• Sniffing Methods of Abuse – Inhaling vapors directly from an open container (lowest concentration) • Huffing – Inhaling vapors from a volatile-soaked cloth held over face (medium concentration) • Bagging – Placing volatile substance in a bag and breathing into the bag (highest concentration) • Ballooning – Inhaling the contents of a balloon • Dusting – Inhaling the contents of computer dust cleaner www. mchc. org www. illinoispoisoncenter. org
 Ballooning remnants www. mchc. org www. illinoispoisoncenter. org
Ballooning remnants www. mchc. org www. illinoispoisoncenter. org
 Huffing www. mchc. org www. illinoispoisoncenter. org
Huffing www. mchc. org www. illinoispoisoncenter. org
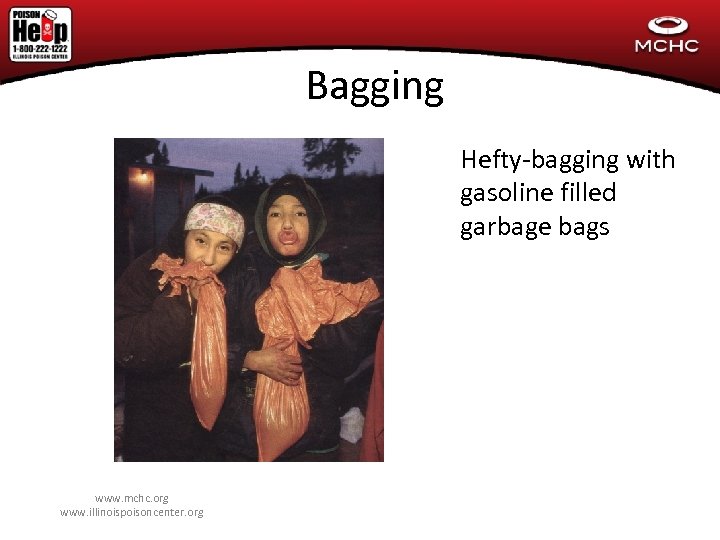 Bagging Hefty-bagging with gasoline filled garbage bags www. mchc. org www. illinoispoisoncenter. org
Bagging Hefty-bagging with gasoline filled garbage bags www. mchc. org www. illinoispoisoncenter. org
 Dusting
Dusting
 Types of Abused Inhalants • Hydrocarbons – Easily cross the blood brain barrier – Have “general anesthetic” qualities – Euphoria, intoxication www. mchc. org www. illinoispoisoncenter. org
Types of Abused Inhalants • Hydrocarbons – Easily cross the blood brain barrier – Have “general anesthetic” qualities – Euphoria, intoxication www. mchc. org www. illinoispoisoncenter. org
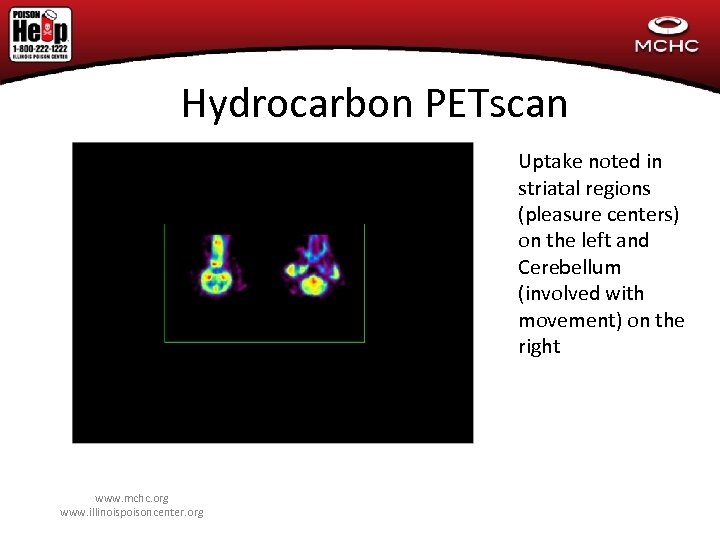 Hydrocarbon PETscan Uptake noted in striatal regions (pleasure centers) on the left and Cerebellum (involved with movement) on the right www. mchc. org www. illinoispoisoncenter. org
Hydrocarbon PETscan Uptake noted in striatal regions (pleasure centers) on the left and Cerebellum (involved with movement) on the right www. mchc. org www. illinoispoisoncenter. org
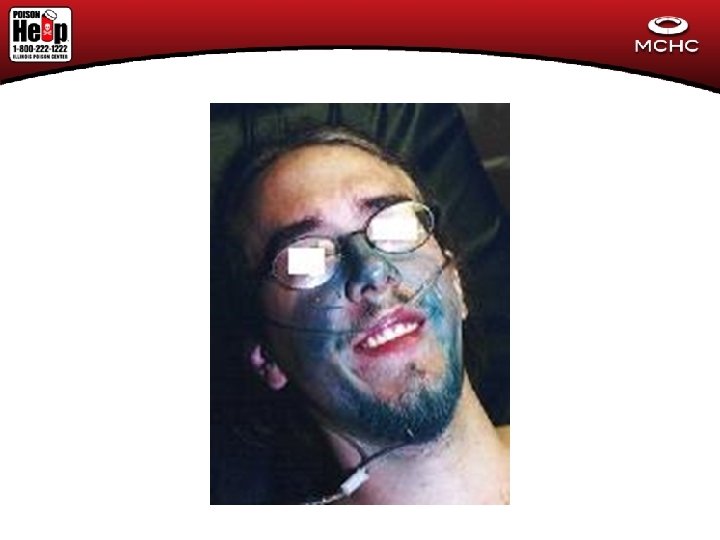
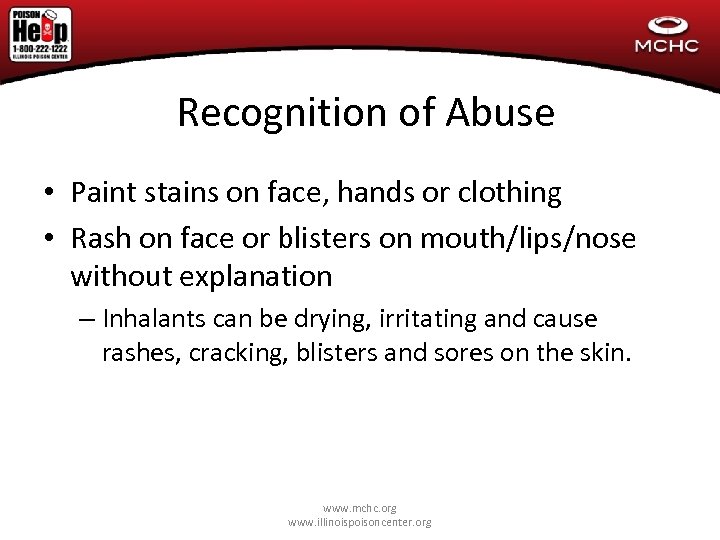 Recognition of Abuse • Paint stains on face, hands or clothing • Rash on face or blisters on mouth/lips/nose without explanation – Inhalants can be drying, irritating and cause rashes, cracking, blisters and sores on the skin. www. mchc. org www. illinoispoisoncenter. org
Recognition of Abuse • Paint stains on face, hands or clothing • Rash on face or blisters on mouth/lips/nose without explanation – Inhalants can be drying, irritating and cause rashes, cracking, blisters and sores on the skin. www. mchc. org www. illinoispoisoncenter. org
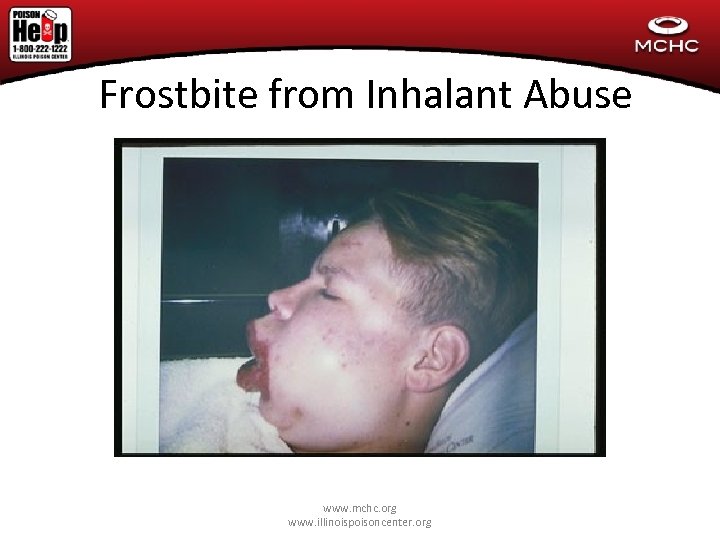 Frostbite from Inhalant Abuse www. mchc. org www. illinoispoisoncenter. org
Frostbite from Inhalant Abuse www. mchc. org www. illinoispoisoncenter. org
 Localized Frostbite from Freon sniffing www. mchc. org www. illinoispoisoncenter. org
Localized Frostbite from Freon sniffing www. mchc. org www. illinoispoisoncenter. org
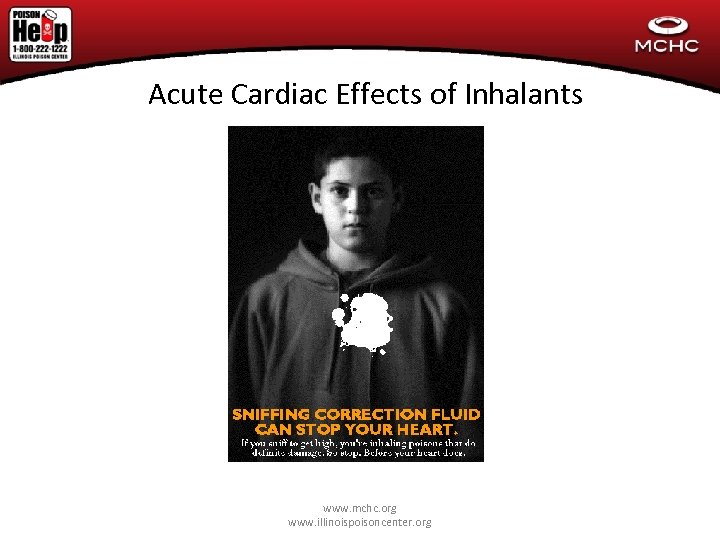 Acute Cardiac Effects of Inhalants www. mchc. org www. illinoispoisoncenter. org
Acute Cardiac Effects of Inhalants www. mchc. org www. illinoispoisoncenter. org
 • 17 yo female presents to ED by EMS in cardiac arrest after huffing computer cleaner that contained difluoroethane. • Intubated by EMS in the field • ROSC post resuscitation with atropine, CPR, IVF – no Epinephrine given • CT Head: Brain edema, severe anoxic injury • Expired within 24 hours
• 17 yo female presents to ED by EMS in cardiac arrest after huffing computer cleaner that contained difluoroethane. • Intubated by EMS in the field • ROSC post resuscitation with atropine, CPR, IVF – no Epinephrine given • CT Head: Brain edema, severe anoxic injury • Expired within 24 hours
 Calcium Channel Blockers (Medicine Cabinet Or Purse Tox Or Visiting Grandparents Tox) • 19 month old male found with mother’s Nifedipine 90 mg SR tablets. By pill count may have ingested 5 pills.
Calcium Channel Blockers (Medicine Cabinet Or Purse Tox Or Visiting Grandparents Tox) • 19 month old male found with mother’s Nifedipine 90 mg SR tablets. By pill count may have ingested 5 pills.
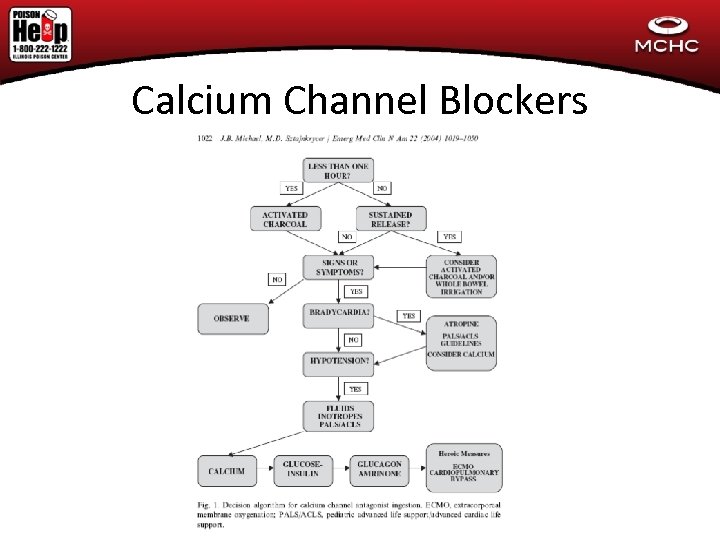 Calcium Channel Blockers
Calcium Channel Blockers
 Calcium Channel Blockers Hyperglycemia is a calling card of this drug overdose • Calcium Channel blockers in the pancreatic B islet cells • Decreased release of insulin • Can lead to HYPERGLYCEMIA
Calcium Channel Blockers Hyperglycemia is a calling card of this drug overdose • Calcium Channel blockers in the pancreatic B islet cells • Decreased release of insulin • Can lead to HYPERGLYCEMIA
 Calcium Channel blockers • 2 yo male with ingestion of up to 450 mg sustained release nifedipine • Unremarkable vitals initially. Glucose 253 • Upon arrival to tertiary care center, resting tachycardia 150 to 170. Patient monitored, tachycardic, hyperglycemic for up to 24 hours. • Arrested the day after admission to tertiary care center, unable to resuscitate
Calcium Channel blockers • 2 yo male with ingestion of up to 450 mg sustained release nifedipine • Unremarkable vitals initially. Glucose 253 • Upon arrival to tertiary care center, resting tachycardia 150 to 170. Patient monitored, tachycardic, hyperglycemic for up to 24 hours. • Arrested the day after admission to tertiary care center, unable to resuscitate
 The acidotic patient • 17 yo female presents to community hospital with SOB and fatigue. Has a sz and given versed and intubated. Transferred to tertiary care hospital • p. H 6. 8/p. CO 2 10/ HCO 3 6 (has anion gap of >25) • CT mild cerebral edema • Bicarb drip started, Continuous Renal Replacement Therapy started • Differential of anion gap metabolic acidosis?
The acidotic patient • 17 yo female presents to community hospital with SOB and fatigue. Has a sz and given versed and intubated. Transferred to tertiary care hospital • p. H 6. 8/p. CO 2 10/ HCO 3 6 (has anion gap of >25) • CT mild cerebral edema • Bicarb drip started, Continuous Renal Replacement Therapy started • Differential of anion gap metabolic acidosis?
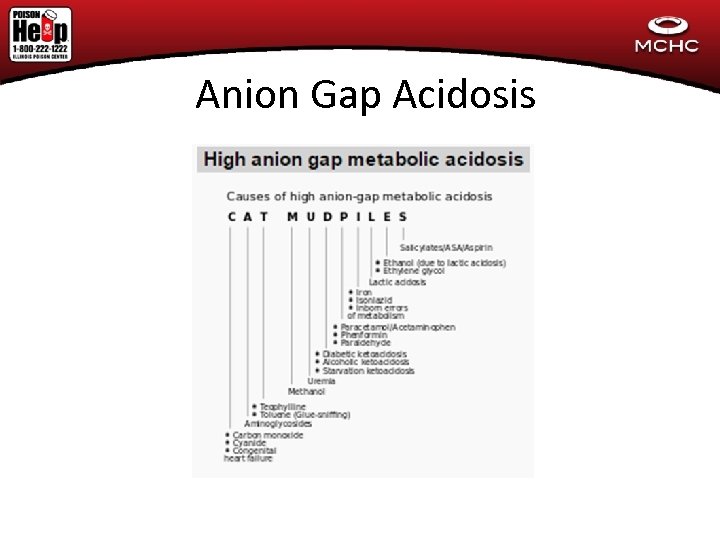 Anion Gap Acidosis
Anion Gap Acidosis
 w/u After bicarbonate drip and CRRT: Na – 141, Cl – 111, HCO 3 – 15 BUN/CR – nl Lactate 2. 2 Persistent elevated ammonia over 160 Metabolic service consulted and w/u for late presenting inborn error of metabolism started • Toxicology service consulted 16 to 18 hours into admission • • •
w/u After bicarbonate drip and CRRT: Na – 141, Cl – 111, HCO 3 – 15 BUN/CR – nl Lactate 2. 2 Persistent elevated ammonia over 160 Metabolic service consulted and w/u for late presenting inborn error of metabolism started • Toxicology service consulted 16 to 18 hours into admission • • •
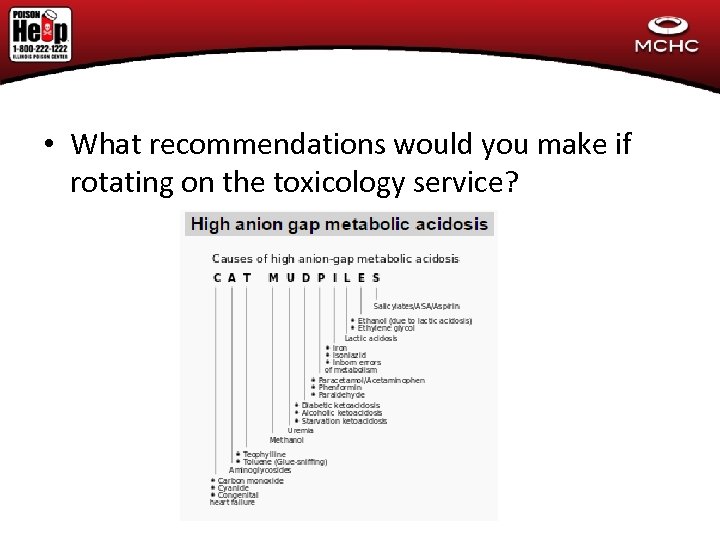 • What recommendations would you make if rotating on the toxicology service?
• What recommendations would you make if rotating on the toxicology service?
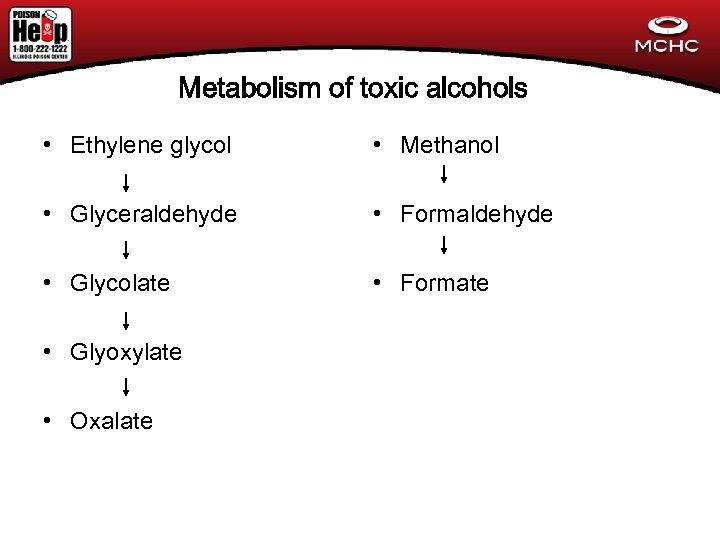 Metabolism of toxic alcohols • Ethylene glycol • Methanol • Glyceraldehyde • Formaldehyde • Glycolate • Formate • Glyoxylate • Oxalate
Metabolism of toxic alcohols • Ethylene glycol • Methanol • Glyceraldehyde • Formaldehyde • Glycolate • Formate • Glyoxylate • Oxalate
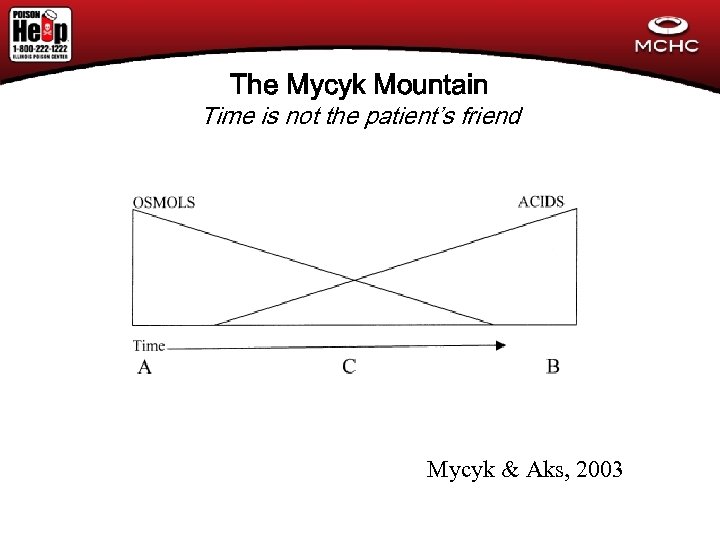 The Mycyk Mountain Time is not the patient’s friend Mycyk & Aks, 2003
The Mycyk Mountain Time is not the patient’s friend Mycyk & Aks, 2003
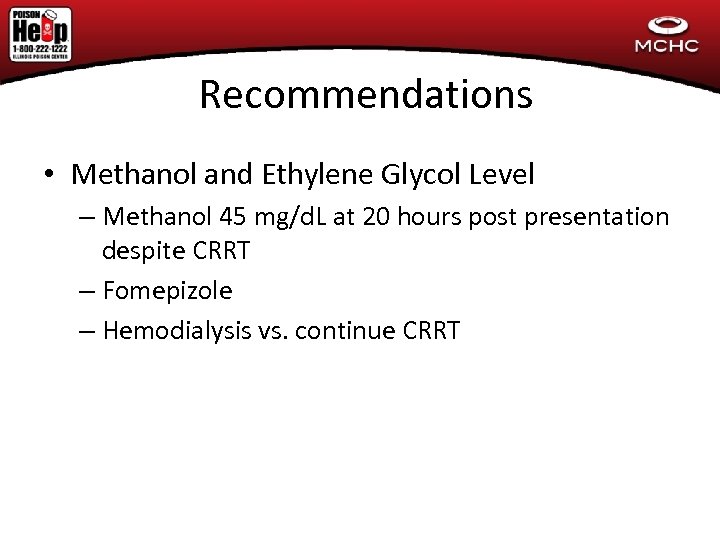 Recommendations • Methanol and Ethylene Glycol Level – Methanol 45 mg/d. L at 20 hours post presentation despite CRRT – Fomepizole – Hemodialysis vs. continue CRRT
Recommendations • Methanol and Ethylene Glycol Level – Methanol 45 mg/d. L at 20 hours post presentation despite CRRT – Fomepizole – Hemodialysis vs. continue CRRT
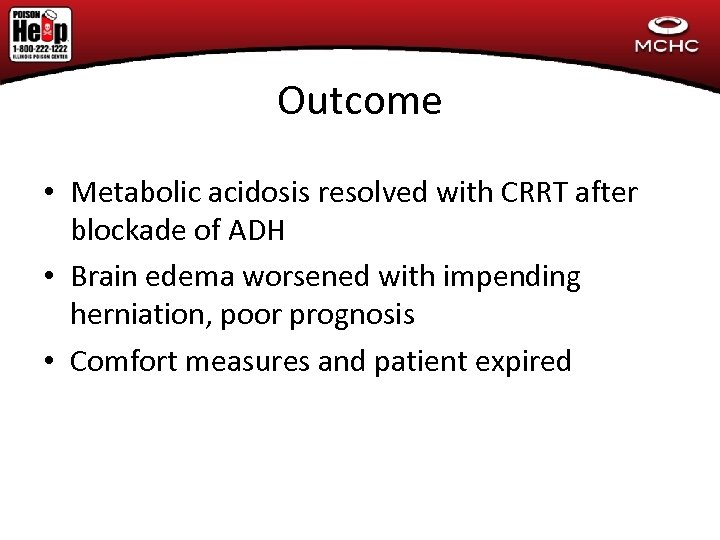 Outcome • Metabolic acidosis resolved with CRRT after blockade of ADH • Brain edema worsened with impending herniation, poor prognosis • Comfort measures and patient expired
Outcome • Metabolic acidosis resolved with CRRT after blockade of ADH • Brain edema worsened with impending herniation, poor prognosis • Comfort measures and patient expired
 Case #1 (Christmas Tox) • 18 month old child thought to have a respiratory infection (cough and vomiting) by family comes to ED for evaluaton. • CXR shows FB in esophagus
Case #1 (Christmas Tox) • 18 month old child thought to have a respiratory infection (cough and vomiting) by family comes to ED for evaluaton. • CXR shows FB in esophagus
 Button Battery # 2 • 4 yo female found pulseless and apneic with blood around mouth and nares • Initially thought to be trauma • CXR with Foreign Body in esophagus
Button Battery # 2 • 4 yo female found pulseless and apneic with blood around mouth and nares • Initially thought to be trauma • CXR with Foreign Body in esophagus
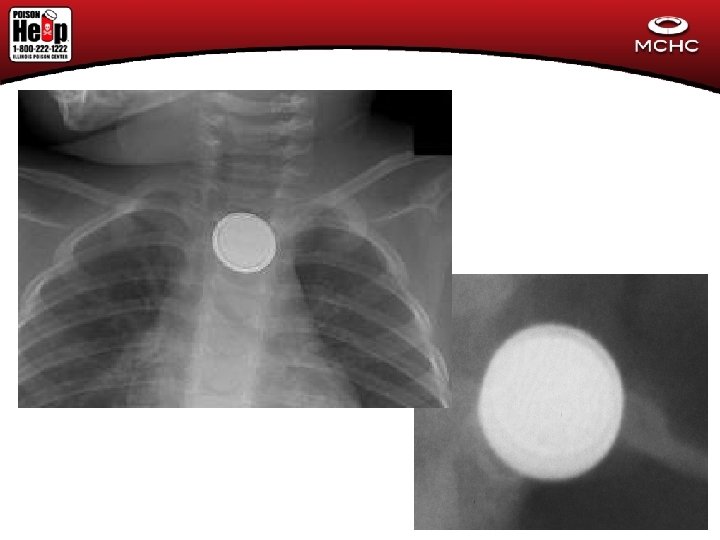
 Button Battery Case #3 • 4 yo cough for over a week. May have been treated with acetaminophen. • CXR showed a 20 mm disc in esophagus
Button Battery Case #3 • 4 yo cough for over a week. May have been treated with acetaminophen. • CXR showed a 20 mm disc in esophagus
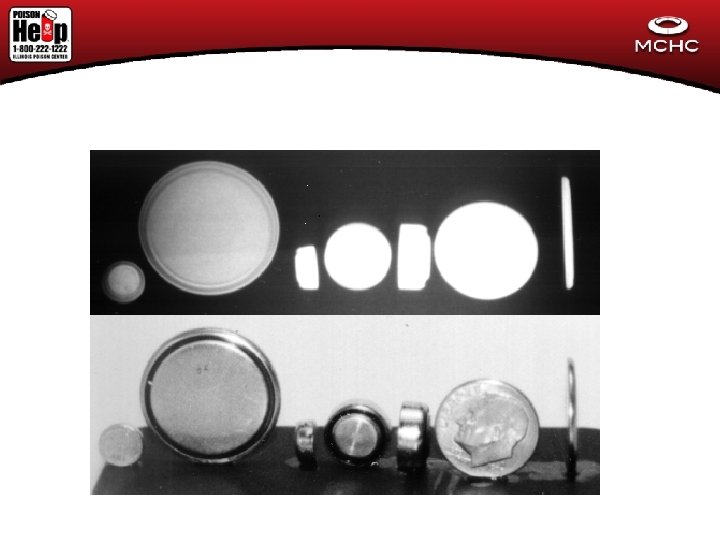
 Button Battery Case #1 • Time delay in transfer to appropriate facility • Both batteries removed endoscopically • Admitted for 4 days. Barium swallow with undefined esophageal deviation • Discharged with fever on abx and medication for acid reflux • 4 days later found cyanotic and in shock • Death Certificate with aorto-esophageal ulcer/fistula
Button Battery Case #1 • Time delay in transfer to appropriate facility • Both batteries removed endoscopically • Admitted for 4 days. Barium swallow with undefined esophageal deviation • Discharged with fever on abx and medication for acid reflux • 4 days later found cyanotic and in shock • Death Certificate with aorto-esophageal ulcer/fistula
 Button Battery # 2 • 4 yo female found pulseless and apneic with blood around mouth and nares • Initially thought to be trauma • CXR with button battery in esophagus Rest of Story • Taken to operating room • Unable to resuscitate • Intra-operative finding?
Button Battery # 2 • 4 yo female found pulseless and apneic with blood around mouth and nares • Initially thought to be trauma • CXR with button battery in esophagus Rest of Story • Taken to operating room • Unable to resuscitate • Intra-operative finding?
 Button Battery Case #3 • 4 yo cough for over a week. May have been treated with acetaminophen. • CXR showed a 20 mm disc in esophagus Rest of Story: • Transferred to tertiary care center, removed endoscopically • Admitted to ICU • Developed massive GI bleed, liver failure, renal failure • Child arrested during exploratory laparoscopy
Button Battery Case #3 • 4 yo cough for over a week. May have been treated with acetaminophen. • CXR showed a 20 mm disc in esophagus Rest of Story: • Transferred to tertiary care center, removed endoscopically • Admitted to ICU • Developed massive GI bleed, liver failure, renal failure • Child arrested during exploratory laparoscopy
 Button Batteries • • Fatal in rare cases Over 5, 500 ED visits in 2009 Larger, newer batteries most often implicated Burns can occur in 2 to 2. 5 hours
Button Batteries • • Fatal in rare cases Over 5, 500 ED visits in 2009 Larger, newer batteries most often implicated Burns can occur in 2 to 2. 5 hours
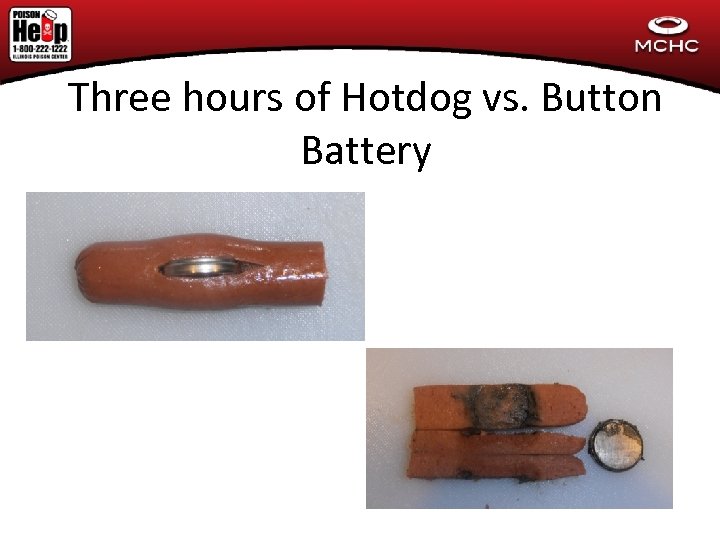 Three hours of Hotdog vs. Button Battery
Three hours of Hotdog vs. Button Battery
 December 2015
December 2015
 Toxidrome • 2 yo child found unarousable and blue, foaming at the mouth. Called pediatrician and then brought her to the ED. • Patient comatose, RR 6, pinpoint pupils • Tox Differential? • What antidote to give?
Toxidrome • 2 yo child found unarousable and blue, foaming at the mouth. Called pediatrician and then brought her to the ED. • Patient comatose, RR 6, pinpoint pupils • Tox Differential? • What antidote to give?
 • 12 hours earlier, found with Lomotil – atropine/diphenoxylate tabs, 16 removed from mouth • Went to ER, had 4 hour observation, awake and alert, active and was discharged • What do you think about that? – Contrast to methadone, buprenorphine, APAP/hydrocodone
• 12 hours earlier, found with Lomotil – atropine/diphenoxylate tabs, 16 removed from mouth • Went to ER, had 4 hour observation, awake and alert, active and was discharged • What do you think about that? – Contrast to methadone, buprenorphine, APAP/hydrocodone
 • The patient intubated • SBP 50 • Head CT: areas of low attenuation c/w infarction • Remained intubated, pinpoint pupils, unresponsive but over breathing ventilator • Expired from progressive cerebral edema and herniation
• The patient intubated • SBP 50 • Head CT: areas of low attenuation c/w infarction • Remained intubated, pinpoint pupils, unresponsive but over breathing ventilator • Expired from progressive cerebral edema and herniation
 Antidepressant pills • 16 yo female ingested 20 of her uncle’s Amitriptyline tabs – 150 mg each • Presents somnolent • VS: HR 126, RR 18, BP 90/60, Temp 99. 6 • Eyes: mid range to slightly wide • Chest: CTA, good AE • Car: Tachycardic regular • Abdo: decrease BS • Skin: Dry
Antidepressant pills • 16 yo female ingested 20 of her uncle’s Amitriptyline tabs – 150 mg each • Presents somnolent • VS: HR 126, RR 18, BP 90/60, Temp 99. 6 • Eyes: mid range to slightly wide • Chest: CTA, good AE • Car: Tachycardic regular • Abdo: decrease BS • Skin: Dry
 4 effects of TCA • Anticholinergic: Somnolence, tachycardia, Seizures • Alpha – blockade: hypotension and tachycardia • Re-uptake inhibition: serotonin syndrome risk • Sodium Channel Blockade: What is the concern?
4 effects of TCA • Anticholinergic: Somnolence, tachycardia, Seizures • Alpha – blockade: hypotension and tachycardia • Re-uptake inhibition: serotonin syndrome risk • Sodium Channel Blockade: What is the concern?
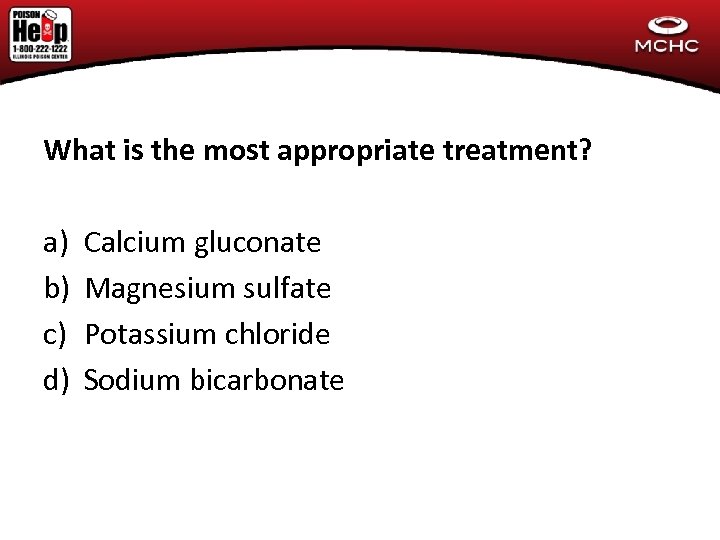 What is the most appropriate treatment? a) b) c) d) Calcium gluconate Magnesium sulfate Potassium chloride Sodium bicarbonate
What is the most appropriate treatment? a) b) c) d) Calcium gluconate Magnesium sulfate Potassium chloride Sodium bicarbonate
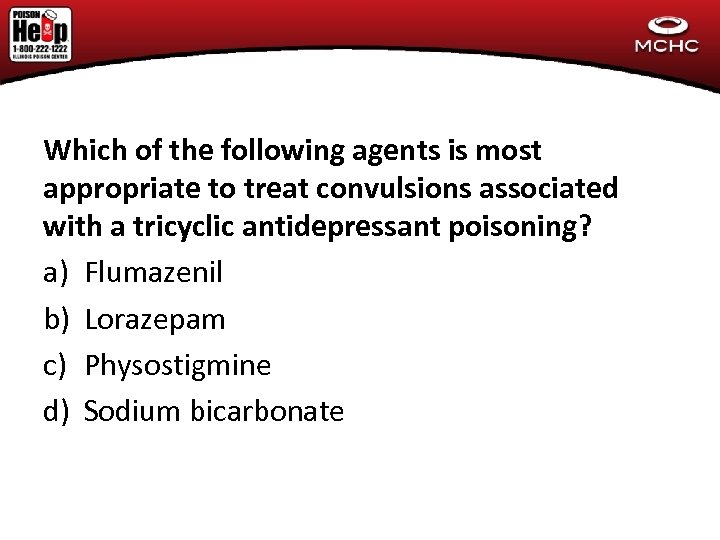 Which of the following agents is most appropriate to treat convulsions associated with a tricyclic antidepressant poisoning? a) Flumazenil b) Lorazepam c) Physostigmine d) Sodium bicarbonate
Which of the following agents is most appropriate to treat convulsions associated with a tricyclic antidepressant poisoning? a) Flumazenil b) Lorazepam c) Physostigmine d) Sodium bicarbonate
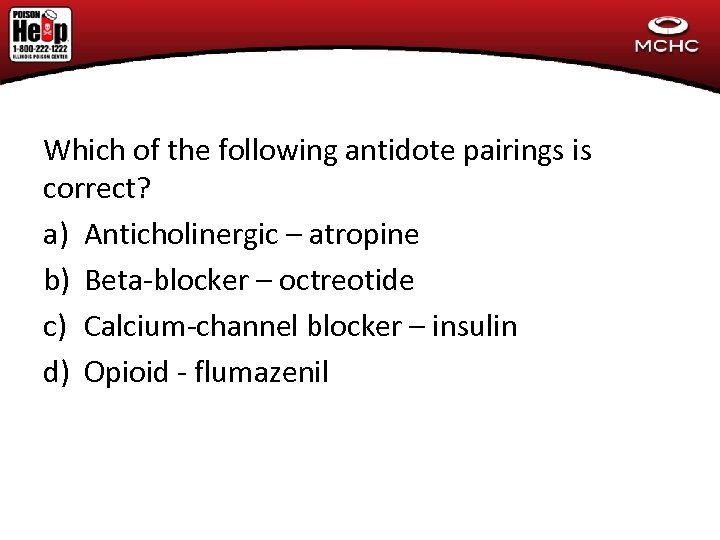 Which of the following antidote pairings is correct? a) Anticholinergic – atropine b) Beta-blocker – octreotide c) Calcium-channel blocker – insulin d) Opioid - flumazenil
Which of the following antidote pairings is correct? a) Anticholinergic – atropine b) Beta-blocker – octreotide c) Calcium-channel blocker – insulin d) Opioid - flumazenil
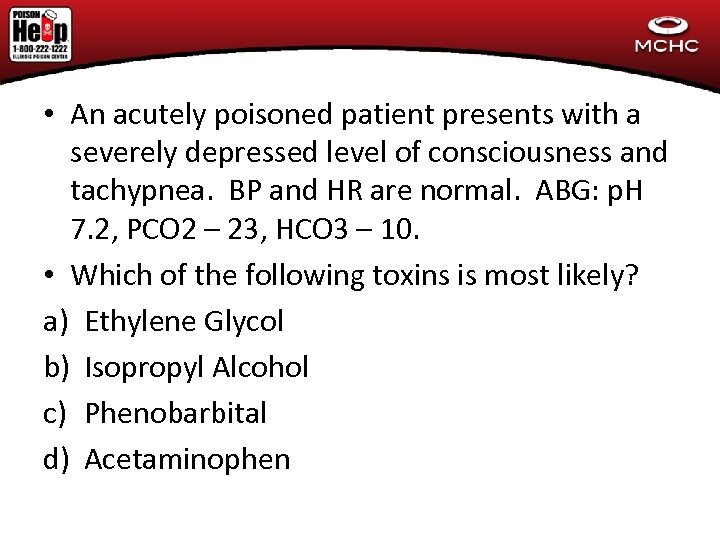 • An acutely poisoned patient presents with a severely depressed level of consciousness and tachypnea. BP and HR are normal. ABG: p. H 7. 2, PCO 2 – 23, HCO 3 – 10. • Which of the following toxins is most likely? a) Ethylene Glycol b) Isopropyl Alcohol c) Phenobarbital d) Acetaminophen
• An acutely poisoned patient presents with a severely depressed level of consciousness and tachypnea. BP and HR are normal. ABG: p. H 7. 2, PCO 2 – 23, HCO 3 – 10. • Which of the following toxins is most likely? a) Ethylene Glycol b) Isopropyl Alcohol c) Phenobarbital d) Acetaminophen
 • A patient is found in arrest next to cans of computer cleaner. A drug to consider avoiding during the resuscitation is: a) Atropine b) Amiodarone c) Epinephrine d) Adenosine
• A patient is found in arrest next to cans of computer cleaner. A drug to consider avoiding during the resuscitation is: a) Atropine b) Amiodarone c) Epinephrine d) Adenosine
 Which of the following agents in overdose most closely mimics opioid poisoning? a) Clonidine b) Diphenhydramine c) LSD d) Yohimbine
Which of the following agents in overdose most closely mimics opioid poisoning? a) Clonidine b) Diphenhydramine c) LSD d) Yohimbine
 Questions?
Questions?


