27fe9c9b24e0dc18a404f379a791f32f.ppt
- Количество слайдов: 16
 What are we trying to do?
What are we trying to do?
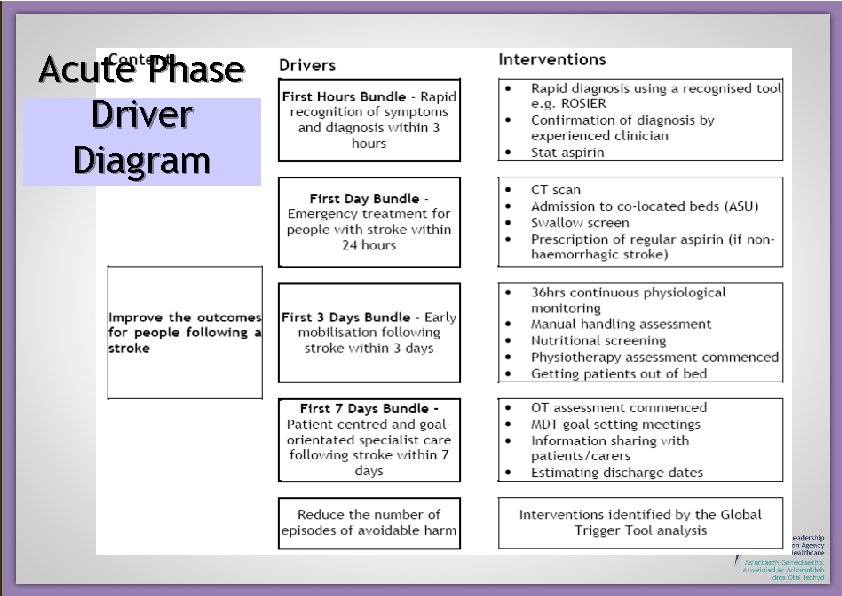 Acute Phase Driver Diagram
Acute Phase Driver Diagram
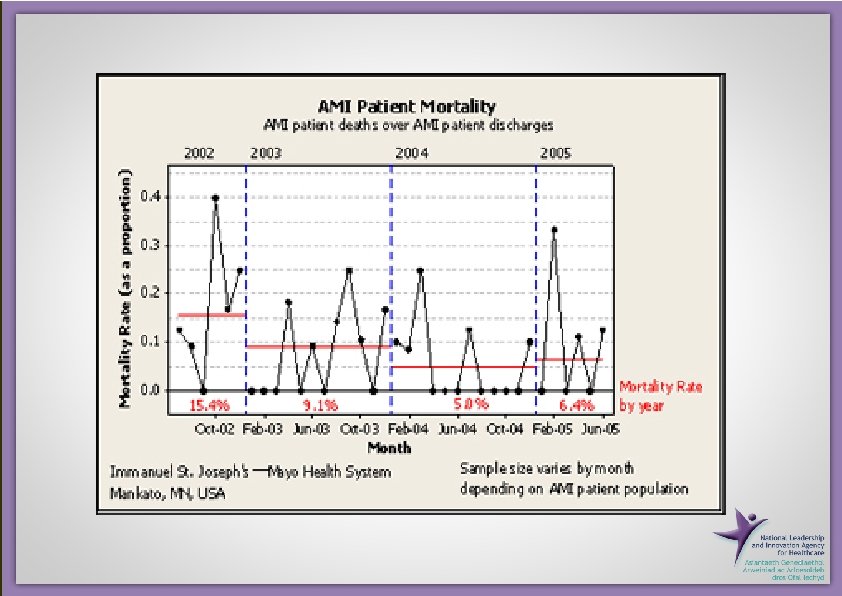
 An example from another setting Acute MI Care in US • • • Aspirin at discharge ACEI for LVSD Beta-blocker at arrival Beta-blocker at discharge Door to lytic Door to PCI Smoking cessation advice Composite and all-or-none scores Survival rate/index Aspirin at arrival
An example from another setting Acute MI Care in US • • • Aspirin at discharge ACEI for LVSD Beta-blocker at arrival Beta-blocker at discharge Door to lytic Door to PCI Smoking cessation advice Composite and all-or-none scores Survival rate/index Aspirin at arrival
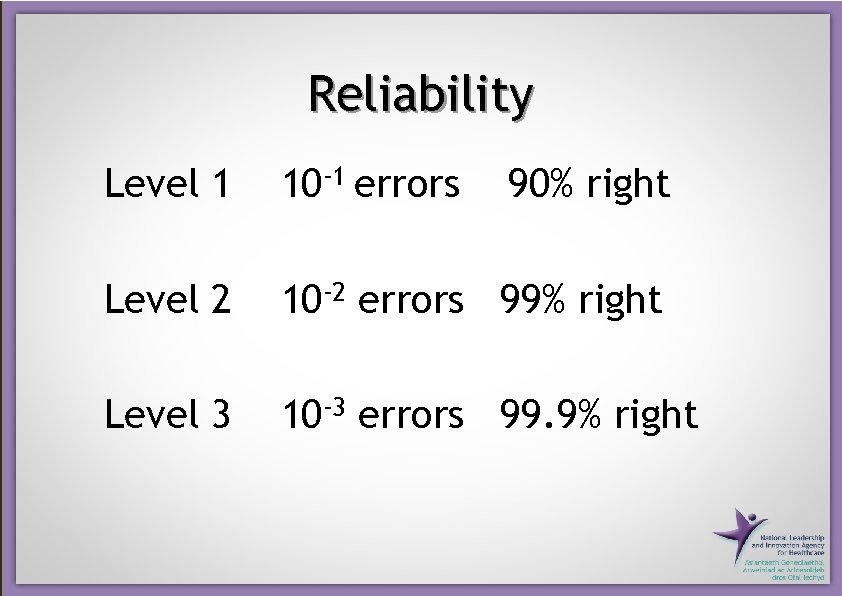 Reliability Level 1 10 -1 errors 90% right Level 2 10 -2 errors 99% right Level 3 10 -3 errors 99. 9% right
Reliability Level 1 10 -1 errors 90% right Level 2 10 -2 errors 99% right Level 3 10 -3 errors 99. 9% right
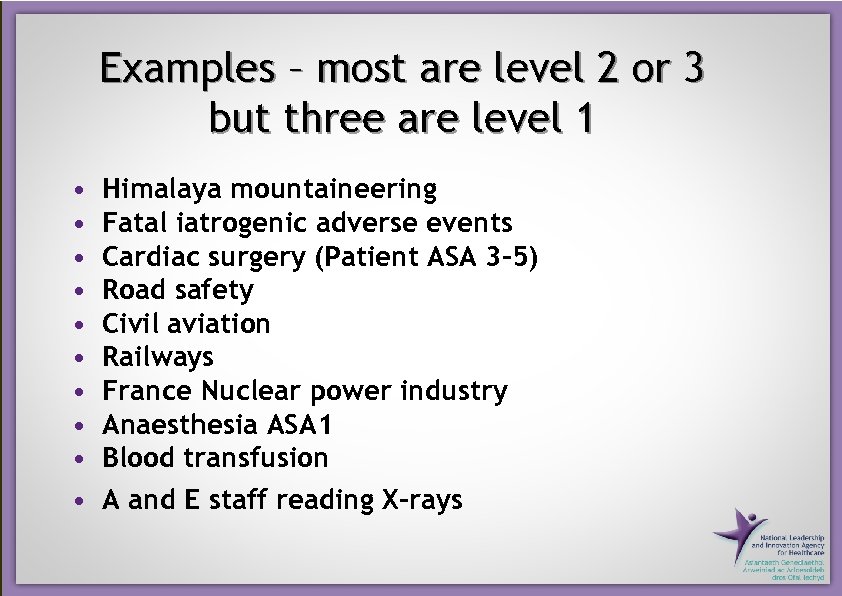 Examples – most are level 2 or 3 but three are level 1 • • • Himalaya mountaineering Fatal iatrogenic adverse events Cardiac surgery (Patient ASA 3 -5) Road safety Civil aviation Railways France Nuclear power industry Anaesthesia ASA 1 Blood transfusion A and E staff reading X-rays
Examples – most are level 2 or 3 but three are level 1 • • • Himalaya mountaineering Fatal iatrogenic adverse events Cardiac surgery (Patient ASA 3 -5) Road safety Civil aviation Railways France Nuclear power industry Anaesthesia ASA 1 Blood transfusion A and E staff reading X-rays
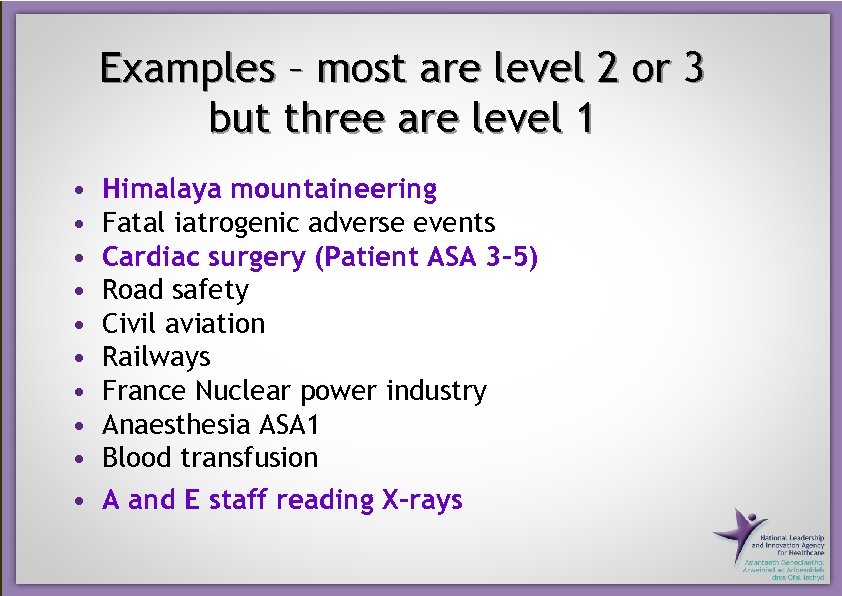 Examples – most are level 2 or 3 but three are level 1 • • • Himalaya mountaineering Fatal iatrogenic adverse events Cardiac surgery (Patient ASA 3 -5) Road safety Civil aviation Railways France Nuclear power industry Anaesthesia ASA 1 Blood transfusion A and E staff reading X-rays
Examples – most are level 2 or 3 but three are level 1 • • • Himalaya mountaineering Fatal iatrogenic adverse events Cardiac surgery (Patient ASA 3 -5) Road safety Civil aviation Railways France Nuclear power industry Anaesthesia ASA 1 Blood transfusion A and E staff reading X-rays
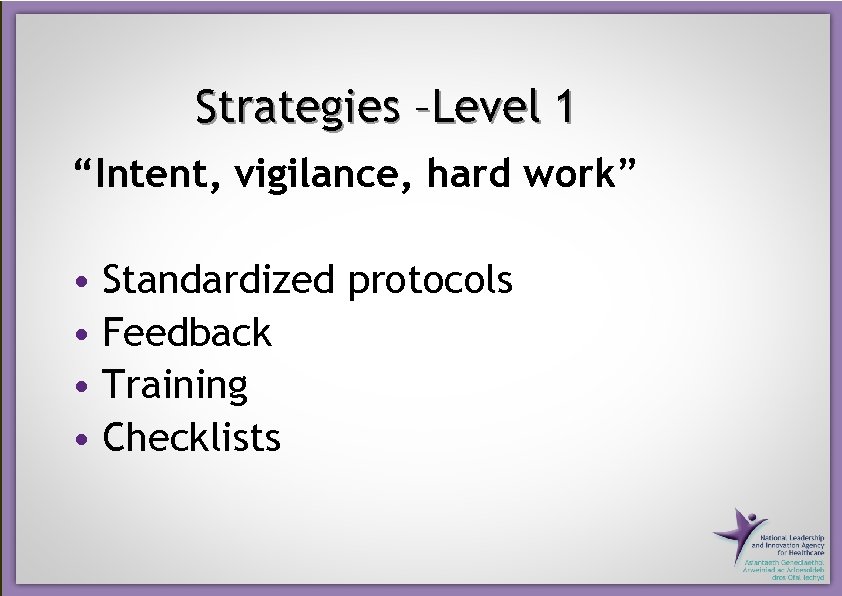 Strategies –Level 1 “Intent, vigilance, hard work” • Standardized protocols • Feedback • Training • Checklists
Strategies –Level 1 “Intent, vigilance, hard work” • Standardized protocols • Feedback • Training • Checklists
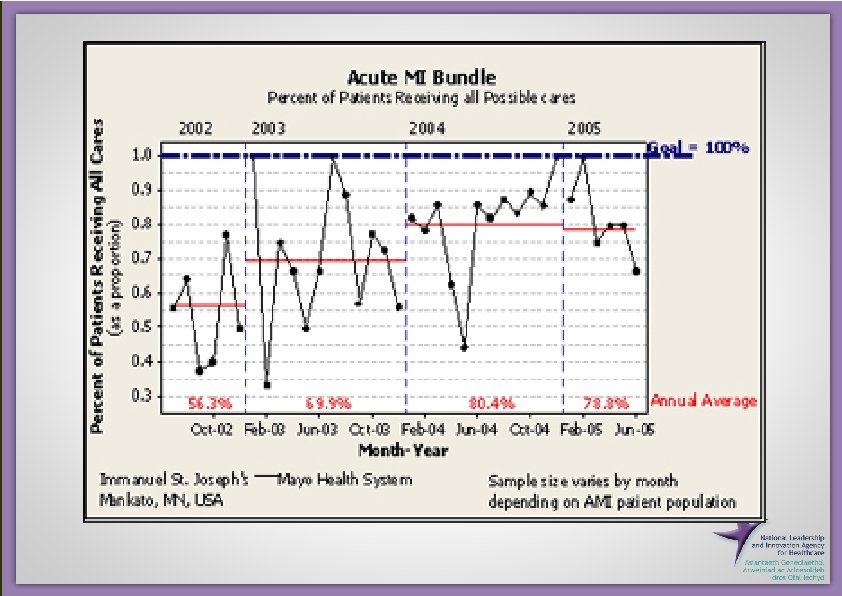
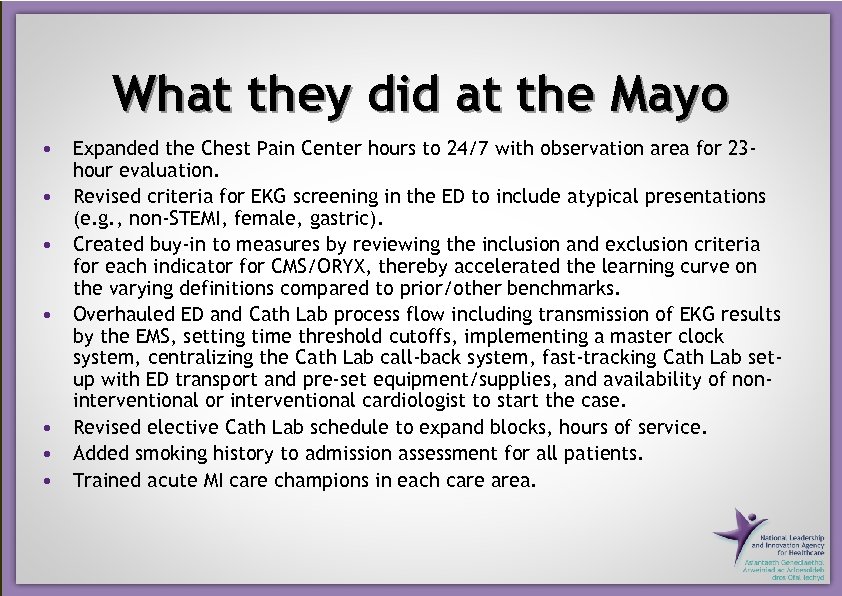 What they did at the Mayo • Expanded the Chest Pain Center hours to 24/7 with observation area for 23 hour evaluation. • Revised criteria for EKG screening in the ED to include atypical presentations (e. g. , non-STEMI, female, gastric). • Created buy-in to measures by reviewing the inclusion and exclusion criteria for each indicator for CMS/ORYX, thereby accelerated the learning curve on the varying definitions compared to prior/other benchmarks. • Overhauled ED and Cath Lab process flow including transmission of EKG results by the EMS, setting time threshold cutoffs, implementing a master clock system, centralizing the Cath Lab call-back system, fast-tracking Cath Lab setup with ED transport and pre-set equipment/supplies, and availability of noninterventional or interventional cardiologist to start the case. • Revised elective Cath Lab schedule to expand blocks, hours of service. • Added smoking history to admission assessment for all patients. • Trained acute MI care champions in each care area.
What they did at the Mayo • Expanded the Chest Pain Center hours to 24/7 with observation area for 23 hour evaluation. • Revised criteria for EKG screening in the ED to include atypical presentations (e. g. , non-STEMI, female, gastric). • Created buy-in to measures by reviewing the inclusion and exclusion criteria for each indicator for CMS/ORYX, thereby accelerated the learning curve on the varying definitions compared to prior/other benchmarks. • Overhauled ED and Cath Lab process flow including transmission of EKG results by the EMS, setting time threshold cutoffs, implementing a master clock system, centralizing the Cath Lab call-back system, fast-tracking Cath Lab setup with ED transport and pre-set equipment/supplies, and availability of noninterventional or interventional cardiologist to start the case. • Revised elective Cath Lab schedule to expand blocks, hours of service. • Added smoking history to admission assessment for all patients. • Trained acute MI care champions in each care area.
 Strategies –Level 2 “Redesign the system – don’t rely on checking” • Decision aids and reminders built into the system • Automation • Evidence as the default • Scheduling • Connection to habits
Strategies –Level 2 “Redesign the system – don’t rely on checking” • Decision aids and reminders built into the system • Automation • Evidence as the default • Scheduling • Connection to habits
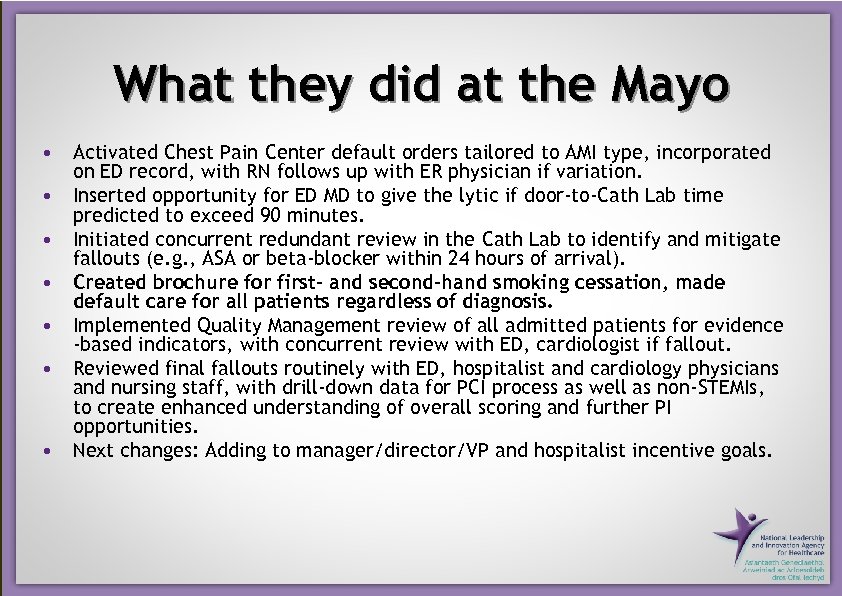 What they did at the Mayo • Activated Chest Pain Center default orders tailored to AMI type, incorporated on ED record, with RN follows up with ER physician if variation. • Inserted opportunity for ED MD to give the lytic if door-to-Cath Lab time predicted to exceed 90 minutes. • Initiated concurrent redundant review in the Cath Lab to identify and mitigate fallouts (e. g. , ASA or beta-blocker within 24 hours of arrival). • Created brochure for first- and second-hand smoking cessation, made default care for all patients regardless of diagnosis. • Implemented Quality Management review of all admitted patients for evidence -based indicators, with concurrent review with ED, cardiologist if fallout. • Reviewed final fallouts routinely with ED, hospitalist and cardiology physicians and nursing staff, with drill-down data for PCI process as well as non-STEMIs, to create enhanced understanding of overall scoring and further PI opportunities. • Next changes: Adding to manager/director/VP and hospitalist incentive goals.
What they did at the Mayo • Activated Chest Pain Center default orders tailored to AMI type, incorporated on ED record, with RN follows up with ER physician if variation. • Inserted opportunity for ED MD to give the lytic if door-to-Cath Lab time predicted to exceed 90 minutes. • Initiated concurrent redundant review in the Cath Lab to identify and mitigate fallouts (e. g. , ASA or beta-blocker within 24 hours of arrival). • Created brochure for first- and second-hand smoking cessation, made default care for all patients regardless of diagnosis. • Implemented Quality Management review of all admitted patients for evidence -based indicators, with concurrent review with ED, cardiologist if fallout. • Reviewed final fallouts routinely with ED, hospitalist and cardiology physicians and nursing staff, with drill-down data for PCI process as well as non-STEMIs, to create enhanced understanding of overall scoring and further PI opportunities. • Next changes: Adding to manager/director/VP and hospitalist incentive goals.
 We can do this in Wales!
We can do this in Wales!
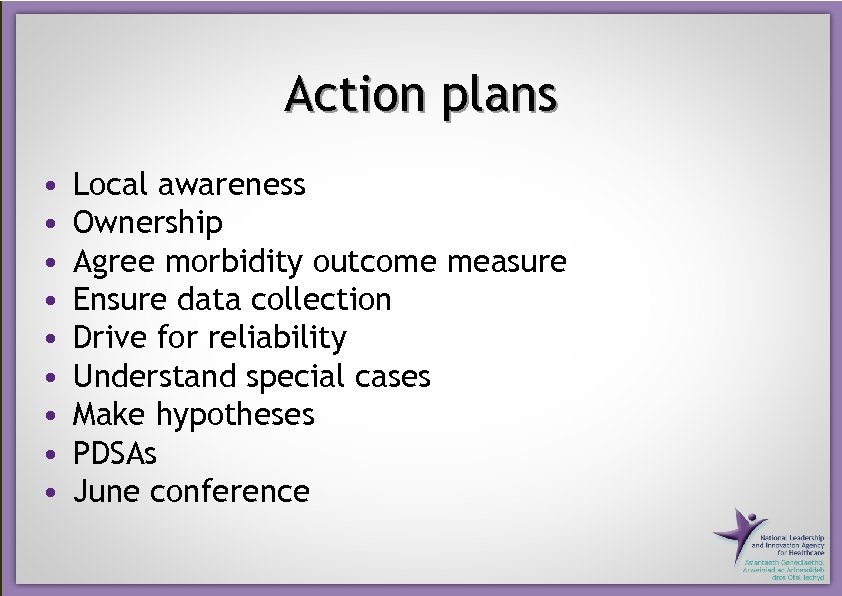 Action plans • • • Local awareness Ownership Agree morbidity outcome measure Ensure data collection Drive for reliability Understand special cases Make hypotheses PDSAs June conference
Action plans • • • Local awareness Ownership Agree morbidity outcome measure Ensure data collection Drive for reliability Understand special cases Make hypotheses PDSAs June conference


