1762a1b6e5cc5404bfb725bc2d323892.ppt
- Количество слайдов: 101
 Welcome to: Understanding the SAMHSA FAQs: Part 2 TO HEAR this webinar, you must dial the number emailed to you in your registration confirmation and use the access code also provided in the same email. The audio pin is on the panel to the right of this screen. The webinar will begin at 3: 00 p. m. EDT Thank you for your patience. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 1
Welcome to: Understanding the SAMHSA FAQs: Part 2 TO HEAR this webinar, you must dial the number emailed to you in your registration confirmation and use the access code also provided in the same email. The audio pin is on the panel to the right of this screen. The webinar will begin at 3: 00 p. m. EDT Thank you for your patience. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 1
 Can’t hear the presentation? Using your telephone, dial the number emailed to you in your registration. When prompted, use the access code also provided in the same email. The audio pin is on the panel to the right of this screen. Having trouble with the phone number? Call 212 -243 -1313. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 2
Can’t hear the presentation? Using your telephone, dial the number emailed to you in your registration. When prompted, use the access code also provided in the same email. The audio pin is on the panel to the right of this screen. Having trouble with the phone number? Call 212 -243 -1313. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 2
 Four-Part Webinar Series on… Confidentiality, Substance Use Treatment, and Health Information Technology (HIT) First 3 Webinars Presented by the Legal Action Center. Today’s presenter is Anita Marton, Esq. 4 th Webinar Presented by SAMHSA Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 3
Four-Part Webinar Series on… Confidentiality, Substance Use Treatment, and Health Information Technology (HIT) First 3 Webinars Presented by the Legal Action Center. Today’s presenter is Anita Marton, Esq. 4 th Webinar Presented by SAMHSA Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 3
 Who is the Legal Action Center? Ø Ø National law & policy non-profit organization Policy and legal work on anti-discrimination & privacy issues affecting people with § Substance Use Disorders § Criminal records or § HIV/AIDS Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 4
Who is the Legal Action Center? Ø Ø National law & policy non-profit organization Policy and legal work on anti-discrimination & privacy issues affecting people with § Substance Use Disorders § Criminal records or § HIV/AIDS Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 4
 Have a Question During this Presentation? Use the “Question(s)” feature on the upper right-hand corner of your screens to type in your question(s). Will stop for Q&A about every 20 minutes. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 5
Have a Question During this Presentation? Use the “Question(s)” feature on the upper right-hand corner of your screens to type in your question(s). Will stop for Q&A about every 20 minutes. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 5
 Today’s Materials This Power. Point presentation FAQs by SAMHSA & ONC: Applying the Substance Abuse Confidentiality Regulations to Health Information Exchange (HIE) (2010) http: //www. samhsa. gov/health. Privacy/docs/EHRFAQs. pdf Applying the Substance Abuse Confidentiality Regulations 42 C. F. R. Part 2 (REVISED) 12. 14. 11 http: //www. samhsa. gov/about/laws/SAMHSA_42 C FRPART 2 FAQII_Revised. pdf 42 C. F. R. Part 2 – the regulations Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 6
Today’s Materials This Power. Point presentation FAQs by SAMHSA & ONC: Applying the Substance Abuse Confidentiality Regulations to Health Information Exchange (HIE) (2010) http: //www. samhsa. gov/health. Privacy/docs/EHRFAQs. pdf Applying the Substance Abuse Confidentiality Regulations 42 C. F. R. Part 2 (REVISED) 12. 14. 11 http: //www. samhsa. gov/about/laws/SAMHSA_42 C FRPART 2 FAQII_Revised. pdf 42 C. F. R. Part 2 – the regulations Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 6
 Today’s Materials Download them on: • www. lac. org – click on “Free Webinars” • www. pfr. samhsa. gov Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 7
Today’s Materials Download them on: • www. lac. org – click on “Free Webinars” • www. pfr. samhsa. gov Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 7
 Recording of this webinar • will be available soon at www. lac. org and www. pfr. samhsa. gov Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 8
Recording of this webinar • will be available soon at www. lac. org and www. pfr. samhsa. gov Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 8
 Who’s today’s audience? This training is for. . . State Government agencies overseeing/providing treatment for substance use and mental health disorders SAMHSA representatives who oversee drug/alcohol treatment and mental health programs Providers treating people with substance use/mental health disorders Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 9
Who’s today’s audience? This training is for. . . State Government agencies overseeing/providing treatment for substance use and mental health disorders SAMHSA representatives who oversee drug/alcohol treatment and mental health programs Providers treating people with substance use/mental health disorders Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 9
 This series is about. . . How to apply the Federal alcohol/drug confidentiality regulations – 42 C. F. R. Part 2 – to Health Information Technology (HIT) Understanding the 2 sets of FAQs issued by SAMSHA Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 10
This series is about. . . How to apply the Federal alcohol/drug confidentiality regulations – 42 C. F. R. Part 2 – to Health Information Technology (HIT) Understanding the 2 sets of FAQs issued by SAMSHA Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 10
 This series is about. . . Why now? Use of HIT is growing rapidly across U. S. – due to technological advances, incentives through the Health Information Technology for Economic and Clinical Health Act (HITECH) enacted as part of American Recovery and Reinvestment Act of 2009. In 2010 and 2011, SAMHSA released 2 sets of FAQs addressing how alcohol/drug treatment records can be incorporated into HIT environment without violating federal alcohol/drug confidentiality regulations. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 11
This series is about. . . Why now? Use of HIT is growing rapidly across U. S. – due to technological advances, incentives through the Health Information Technology for Economic and Clinical Health Act (HITECH) enacted as part of American Recovery and Reinvestment Act of 2009. In 2010 and 2011, SAMHSA released 2 sets of FAQs addressing how alcohol/drug treatment records can be incorporated into HIT environment without violating federal alcohol/drug confidentiality regulations. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 11
 This series is about. . . Why now? (cont. ) Even after the release of the FAQs, many have questions about how to integrate alcohol/drug treatment records into HIT systems. Goal of these webinars is to advance understanding of how to do this. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 12
This series is about. . . Why now? (cont. ) Even after the release of the FAQs, many have questions about how to integrate alcohol/drug treatment records into HIT systems. Goal of these webinars is to advance understanding of how to do this. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 12
 Summary of Webinar #1 Ø Ø Provided general overview of HIPAA Provided general overview of 42 C. F. R. Part 2, with a focus on the provisions of Part 2 that are most relevant to an e-health environment, including: • which programs are covered by Part 2; • what patient information is protected; and • provisions that allow for the disclosure of patient identifying information. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 13
Summary of Webinar #1 Ø Ø Provided general overview of HIPAA Provided general overview of 42 C. F. R. Part 2, with a focus on the provisions of Part 2 that are most relevant to an e-health environment, including: • which programs are covered by Part 2; • what patient information is protected; and • provisions that allow for the disclosure of patient identifying information. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 13
 Summary of Webinar #2 Ø Discussed SAMHSA FAQs Relating To: q Patient choice models q Consent issues, including: § consent forms; § redisclosure issues; and § minors and consent Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 14
Summary of Webinar #2 Ø Discussed SAMHSA FAQs Relating To: q Patient choice models q Consent issues, including: § consent forms; § redisclosure issues; and § minors and consent Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 14
 Today’s Presentation Ø Will Discuss SAMHSA FAQs Relating To: • • Qualified Service Organization Agreements (“QSOAs”); Medical emergencies; Immediate threats to health or safety of an individual or the public; and Screening, Brief Intervention and Referral to Treatment (“SBIRT”) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 15
Today’s Presentation Ø Will Discuss SAMHSA FAQs Relating To: • • Qualified Service Organization Agreements (“QSOAs”); Medical emergencies; Immediate threats to health or safety of an individual or the public; and Screening, Brief Intervention and Referral to Treatment (“SBIRT”) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 15
 Save the Date! Upcoming Webinar: SAMHSA’s Investment to Support of HIT Adoption – May 25, 2012 Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 16
Save the Date! Upcoming Webinar: SAMHSA’s Investment to Support of HIT Adoption – May 25, 2012 Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 16
 Let’s Get Started Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 17
Let’s Get Started Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 17
 Useful Terms & Definitions Ø Ø 42 C. F. R. Part 2 (“Part 2”): federal regulations protecting the confidentiality of drug/alcohol patient information Health Information Exchange (“HIE”): various methods & mechanisms through which information can be exchanged electronically via a computer network between health care providers and other health care stakeholders Health Information Organization (“HIO”): an organization that oversees and governs the exchange of health-related information among organizations HIO Affiliated Members: Entities that participate in a HIO network, including but not limited to participating health care providers Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 18
Useful Terms & Definitions Ø Ø 42 C. F. R. Part 2 (“Part 2”): federal regulations protecting the confidentiality of drug/alcohol patient information Health Information Exchange (“HIE”): various methods & mechanisms through which information can be exchanged electronically via a computer network between health care providers and other health care stakeholders Health Information Organization (“HIO”): an organization that oversees and governs the exchange of health-related information among organizations HIO Affiliated Members: Entities that participate in a HIO network, including but not limited to participating health care providers Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 18
 PART ONE QUALIFIED SERVICE ORGANIZATION AGREEMENTS (“QSOAs”) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 19
PART ONE QUALIFIED SERVICE ORGANIZATION AGREEMENTS (“QSOAs”) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 19
 QSOAs: Definition of QSOA Ø A Qualified Services Organization Agreement (“QSOA”) is a written agreement between a Part 2 program and a Qualified Service Organization (“QSO”), allowing two-way communication between the two parties. FAQ I(6) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 20
QSOAs: Definition of QSOA Ø A Qualified Services Organization Agreement (“QSOA”) is a written agreement between a Part 2 program and a Qualified Service Organization (“QSO”), allowing two-way communication between the two parties. FAQ I(6) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 20
 QSOAs: Definition of QSOA Ø Ø Ø A QSOA is similar to a Business Associate agreement under HIPAA. As a practical matter, Part 2 programs will have to enter into QSO/BA agreements to meet both the Part 2 and HIPAA requirements. The FAQs only address Part 2 requirements. As covered in Webinar #1, QSO/BA agreements will have to meet Part 2’s stricter requirement. Thus, this Webinar focuses on QSOAs under Part 2’s requirements. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 21
QSOAs: Definition of QSOA Ø Ø Ø A QSOA is similar to a Business Associate agreement under HIPAA. As a practical matter, Part 2 programs will have to enter into QSO/BA agreements to meet both the Part 2 and HIPAA requirements. The FAQs only address Part 2 requirements. As covered in Webinar #1, QSO/BA agreements will have to meet Part 2’s stricter requirement. Thus, this Webinar focuses on QSOAs under Part 2’s requirements. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 21
 QSOAs: Definition of QSO Under Part 2, a QSO is defined as a person or organization that: 1. Provides services to a Part 2 program (e. g. , data processing, bill collecting, dosage preparation, laboratory analyses, medical, etc. ) • In the HIE context, the services a HIO could provide to a Part 2 program could include: “holding and storing patient data, receiving and reviewing requests for disclosures to third parties, and facilitating the electronic exchange of patients’ information through the HIO network. ” AND more… Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 22
QSOAs: Definition of QSO Under Part 2, a QSO is defined as a person or organization that: 1. Provides services to a Part 2 program (e. g. , data processing, bill collecting, dosage preparation, laboratory analyses, medical, etc. ) • In the HIE context, the services a HIO could provide to a Part 2 program could include: “holding and storing patient data, receiving and reviewing requests for disclosures to third parties, and facilitating the electronic exchange of patients’ information through the HIO network. ” AND more… Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 22
 QSOAs: Definition of QSO 2. Has entered into a written agreement with a Part 2 program in which the QSO: a. acknowledges that in receiving, storing, processing or otherwise dealing with any patient records from the programs it is fully bound by the Part 2 regulations AND b. will resist in judicial proceedings any efforts to obtain access to patient records unless otherwise permitted by Part 2. FAQ I(5) and FAQ II(6) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 23
QSOAs: Definition of QSO 2. Has entered into a written agreement with a Part 2 program in which the QSO: a. acknowledges that in receiving, storing, processing or otherwise dealing with any patient records from the programs it is fully bound by the Part 2 regulations AND b. will resist in judicial proceedings any efforts to obtain access to patient records unless otherwise permitted by Part 2. FAQ I(5) and FAQ II(6) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 23
 QSOAs: No Patient Consent Needed Ø Can a Part 2 program give patient information to an entity that provides services to the Part 2 program (e. g. , a laboratory) pursuant to a QSOA without a patient’s consent? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 24
QSOAs: No Patient Consent Needed Ø Can a Part 2 program give patient information to an entity that provides services to the Part 2 program (e. g. , a laboratory) pursuant to a QSOA without a patient’s consent? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 24
 QSOAs: No Patient Consent Needed YES, but only when a Part 2 program has entered into a QSOA with the entity providing such services. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 25
QSOAs: No Patient Consent Needed YES, but only when a Part 2 program has entered into a QSOA with the entity providing such services. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 25
 QSOAs: HIOs Ø Is a Part 2 program allowed to enter into a QSOA with a HIO without the patient’s written consent? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 26
QSOAs: HIOs Ø Is a Part 2 program allowed to enter into a QSOA with a HIO without the patient’s written consent? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 26
 QSOAs: HIOs YES, if: 1. the HIO provides covered services to the Part 2 program, such as holding and storing patient data, etc. ; 2. the Part 2 program and the HIO enter into a two-way written QSOA; AND 3. the Part 2 patient information made available to the HIO is restricted to the information needed by the HIO to provide services to the Part 2 program. FAQ I(6), (7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 27
QSOAs: HIOs YES, if: 1. the HIO provides covered services to the Part 2 program, such as holding and storing patient data, etc. ; 2. the Part 2 program and the HIO enter into a two-way written QSOA; AND 3. the Part 2 patient information made available to the HIO is restricted to the information needed by the HIO to provide services to the Part 2 program. FAQ I(6), (7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 27
 QSOAs: HIOs Ø Ø The scope of a QSOA is limited. As discussed in previous slides, a QSOA is a twoway agreement between a Part 2 Program and the QSO. The QSOA only authorizes communications between the Part 2 program and the QSO. Information can flow back and forth between the parties. This is true even when the QSO is a HIO. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 28
QSOAs: HIOs Ø Ø The scope of a QSOA is limited. As discussed in previous slides, a QSOA is a twoway agreement between a Part 2 Program and the QSO. The QSOA only authorizes communications between the Part 2 program and the QSO. Information can flow back and forth between the parties. This is true even when the QSO is a HIO. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 28
 QSOAs: HIOs Case Study/Poll: Part 2 Program ABC has a written QSOA with a HIO. Pursuant to the QSOA, may the Part 2 Program upload (electronically transmit) information about its patients without the written consent of its patients? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 29
QSOAs: HIOs Case Study/Poll: Part 2 Program ABC has a written QSOA with a HIO. Pursuant to the QSOA, may the Part 2 Program upload (electronically transmit) information about its patients without the written consent of its patients? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 29
 QSOAs: HIOs Possible answers: 1. YES. No, not even with a QSOA in place, a program cannot upload information about its patients without consent. 2. NO. Patient consent is always needed when patient-identifying information is disclosed by a Part 2 program. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 30
QSOAs: HIOs Possible answers: 1. YES. No, not even with a QSOA in place, a program cannot upload information about its patients without consent. 2. NO. Patient consent is always needed when patient-identifying information is disclosed by a Part 2 program. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 30
 QSOAs: HIOs Answer: #1 - YES, if: 1. a QSOA is in place; AND 2. the HIO’s choice model (discussed in Webinar 2) does not require patient consent before information can be disclosed to the HIO. For example, if the HIO uses an “Opt-In” choice model, a QSOA cannot be used because patient consent is required before a Part 2 program can disclose patient information to the HIO. FAQ I(6 and 7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 31
QSOAs: HIOs Answer: #1 - YES, if: 1. a QSOA is in place; AND 2. the HIO’s choice model (discussed in Webinar 2) does not require patient consent before information can be disclosed to the HIO. For example, if the HIO uses an “Opt-In” choice model, a QSOA cannot be used because patient consent is required before a Part 2 program can disclose patient information to the HIO. FAQ I(6 and 7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 31
 QSOAs: HIO Disclosures to Third Parties Ø Generally, a HIO that is holding or storing Part 2 patient data through a QSOA IS NOT ALLOWED to redisclose data from a Part 2 program to a third party without a patient’s written consent. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 32
QSOAs: HIO Disclosures to Third Parties Ø Generally, a HIO that is holding or storing Part 2 patient data through a QSOA IS NOT ALLOWED to redisclose data from a Part 2 program to a third party without a patient’s written consent. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 32
 QSOAs: HIO Disclosures to Third Parties However, a HIO IS PERMITTED to: 1. Disclose Part 2 information to a contract agent of the HIO when: a. a HIO needs to do so to provide the services described in the QSOA; AND b. as long as the agent only discloses the information back to the HIO or the originating Part 2 program more… Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 33
QSOAs: HIO Disclosures to Third Parties However, a HIO IS PERMITTED to: 1. Disclose Part 2 information to a contract agent of the HIO when: a. a HIO needs to do so to provide the services described in the QSOA; AND b. as long as the agent only discloses the information back to the HIO or the originating Part 2 program more… Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 33
 QSOAs: HIO Disclosures to Third Parties 2. Redisclose Part 2 information in a medical emergency situation. § We will address medical emergencies later on in this presentation. FAQ I(10) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 34
QSOAs: HIO Disclosures to Third Parties 2. Redisclose Part 2 information in a medical emergency situation. § We will address medical emergencies later on in this presentation. FAQ I(10) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 34
 QSOAs: HIO Disclosures to Third Parties Case Study/Poll: Part 2 Program ABC has a QSOA with a HIO and has uploaded information about Patient Nellie without her written consent. General Hospital XYZ is affiliated with that HIO network. Can the HIO redisclose Patient Nellie’s Part 2 information to General Hospital XYZ without her consent? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 35
QSOAs: HIO Disclosures to Third Parties Case Study/Poll: Part 2 Program ABC has a QSOA with a HIO and has uploaded information about Patient Nellie without her written consent. General Hospital XYZ is affiliated with that HIO network. Can the HIO redisclose Patient Nellie’s Part 2 information to General Hospital XYZ without her consent? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 35
 QSOAs: HIO Disclosures to Third Parties Possible Answers: 1. Yes, because a QSOA is in place, and General Hospital XYZ is providing medical services to Nellie, a Part 2 program ABC’s patient. 2. No, because a QSOA is a 2 -way agreement between the HIO and Part 2 program ABC, and since General Hospital XYZ is not an agent of the HIO, the HIO cannot disclose information about Nellie without consent unless there is a medical emergency. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 36
QSOAs: HIO Disclosures to Third Parties Possible Answers: 1. Yes, because a QSOA is in place, and General Hospital XYZ is providing medical services to Nellie, a Part 2 program ABC’s patient. 2. No, because a QSOA is a 2 -way agreement between the HIO and Part 2 program ABC, and since General Hospital XYZ is not an agent of the HIO, the HIO cannot disclose information about Nellie without consent unless there is a medical emergency. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 36
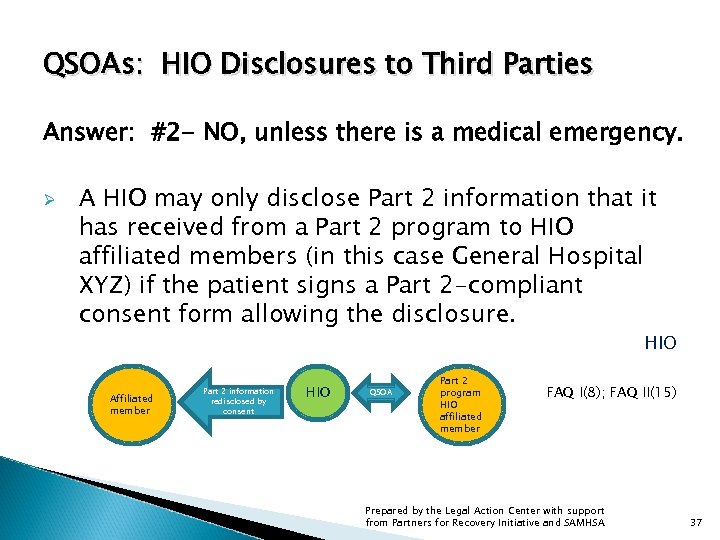 QSOAs: HIO Disclosures to Third Parties Answer: #2 - NO, unless there is a medical emergency. Ø A HIO may only disclose Part 2 information that it has received from a Part 2 program to HIO affiliated members (in this case General Hospital XYZ) if the patient signs a Part 2 -compliant consent form allowing the disclosure. HIO Affiliated member Part 2 information redisclosed by consent HIO QSOA Part 2 program HIO affiliated member FAQ I(8); FAQ II(15) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 37
QSOAs: HIO Disclosures to Third Parties Answer: #2 - NO, unless there is a medical emergency. Ø A HIO may only disclose Part 2 information that it has received from a Part 2 program to HIO affiliated members (in this case General Hospital XYZ) if the patient signs a Part 2 -compliant consent form allowing the disclosure. HIO Affiliated member Part 2 information redisclosed by consent HIO QSOA Part 2 program HIO affiliated member FAQ I(8); FAQ II(15) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 37
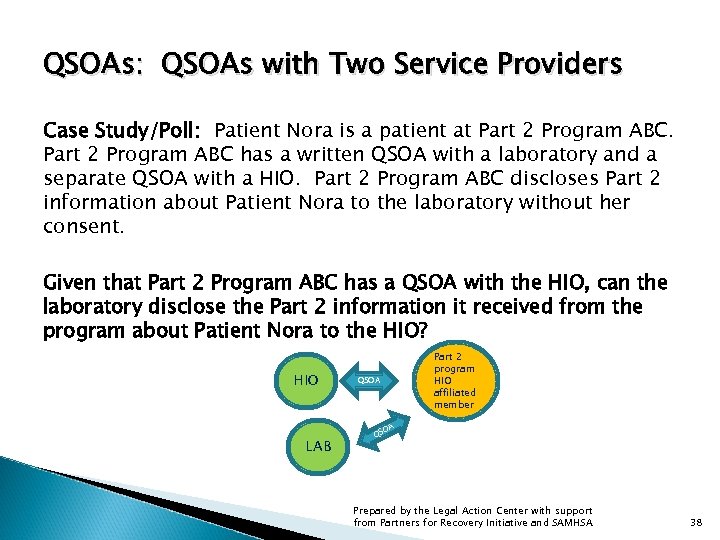 QSOAs: QSOAs with Two Service Providers Case Study/Poll: Patient Nora is a patient at Part 2 Program ABC has a written QSOA with a laboratory and a separate QSOA with a HIO. Part 2 Program ABC discloses Part 2 information about Patient Nora to the laboratory without her consent. Given that Part 2 Program ABC has a QSOA with the HIO, can the laboratory disclose the Part 2 information it received from the program about Patient Nora to the HIO? HIO LAB Part 2 program HIO affiliated member QSOA OA QS Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 38
QSOAs: QSOAs with Two Service Providers Case Study/Poll: Patient Nora is a patient at Part 2 Program ABC has a written QSOA with a laboratory and a separate QSOA with a HIO. Part 2 Program ABC discloses Part 2 information about Patient Nora to the laboratory without her consent. Given that Part 2 Program ABC has a QSOA with the HIO, can the laboratory disclose the Part 2 information it received from the program about Patient Nora to the HIO? HIO LAB Part 2 program HIO affiliated member QSOA OA QS Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 38
 QSOAs: QSOAs with Two Service Providers Possible Answers: 1. Yes, because the Part 2 program has QSOAs with both the lab and HIO. 2. No, not without Patient Nora’s written consent, because a QSOA is a two-way agreement between a Part 2 program and a service provider. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 39
QSOAs: QSOAs with Two Service Providers Possible Answers: 1. Yes, because the Part 2 program has QSOAs with both the lab and HIO. 2. No, not without Patient Nora’s written consent, because a QSOA is a two-way agreement between a Part 2 program and a service provider. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 39
 QSOAs: QSOAs with Two Service Providers ANSWER: #2 NO, not without Patient Nora’s written consent. As we learned in Webinar #2, one consent form could authorize: (1) Part 2 Program ABC to disclose information about Patient Nora to the lab; AND (2) the lab to redisclose Part 2 information to the HIO. more… FAQ II(14) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 40
QSOAs: QSOAs with Two Service Providers ANSWER: #2 NO, not without Patient Nora’s written consent. As we learned in Webinar #2, one consent form could authorize: (1) Part 2 Program ABC to disclose information about Patient Nora to the lab; AND (2) the lab to redisclose Part 2 information to the HIO. more… FAQ II(14) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 40
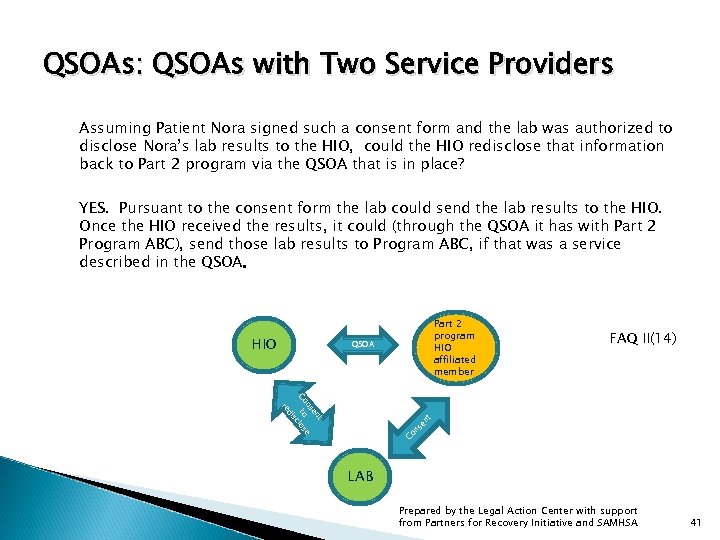 QSOAs: QSOAs with Two Service Providers Assuming Patient Nora signed such a consent form and the lab was authorized to disclose Nora’s lab results to the HIO, could the HIO redisclose that information back to Part 2 program via the QSOA that is in place? YES. Pursuant to the consent form the lab could send the lab results to the HIO. Once the HIO received the results, it could (through the QSOA it has with Part 2 Program ABC), send those lab results to Program ABC, if that was a service described in the QSOA. HIO Part 2 program HIO affiliated member QSOA FAQ II(14) t en ns e Co to los sc di Co ns en t re LAB Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 41
QSOAs: QSOAs with Two Service Providers Assuming Patient Nora signed such a consent form and the lab was authorized to disclose Nora’s lab results to the HIO, could the HIO redisclose that information back to Part 2 program via the QSOA that is in place? YES. Pursuant to the consent form the lab could send the lab results to the HIO. Once the HIO received the results, it could (through the QSOA it has with Part 2 Program ABC), send those lab results to Program ABC, if that was a service described in the QSOA. HIO Part 2 program HIO affiliated member QSOA FAQ II(14) t en ns e Co to los sc di Co ns en t re LAB Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 41
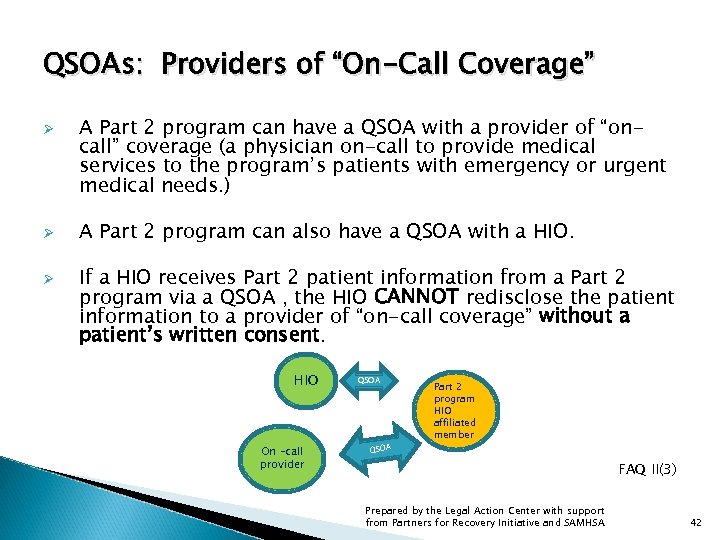 QSOAs: Providers of “On-Call Coverage” Ø Ø Ø A Part 2 program can have a QSOA with a provider of “oncall” coverage (a physician on-call to provide medical services to the program’s patients with emergency or urgent medical needs. ) A Part 2 program can also have a QSOA with a HIO. If a HIO receives Part 2 patient information from a Part 2 program via a QSOA , the HIO CANNOT redisclose the patient information to a provider of “on-call coverage” without a patient’s written consent. HIO On –call provider QSOA Part 2 program HIO affiliated member FAQ II(3) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 42
QSOAs: Providers of “On-Call Coverage” Ø Ø Ø A Part 2 program can have a QSOA with a provider of “oncall” coverage (a physician on-call to provide medical services to the program’s patients with emergency or urgent medical needs. ) A Part 2 program can also have a QSOA with a HIO. If a HIO receives Part 2 patient information from a Part 2 program via a QSOA , the HIO CANNOT redisclose the patient information to a provider of “on-call coverage” without a patient’s written consent. HIO On –call provider QSOA Part 2 program HIO affiliated member FAQ II(3) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 42
 QSOAs: Providers of “On-Call Coverage” Ø As previously mentioned, a QSOA between a Part 2 program and a HIO is a two-way agreement between those parties. Generally, a HIO cannot redisclose Part 2 information that it receives from a Part 2 program to a third party unless there is a medical emergency or the third party is a contract agent of the HIO. Therefore, a HIO is not allowed to redisclose Part 2 information to a provider of “on-call coverage” without a patient’s written consent. FAQ II(3) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 43
QSOAs: Providers of “On-Call Coverage” Ø As previously mentioned, a QSOA between a Part 2 program and a HIO is a two-way agreement between those parties. Generally, a HIO cannot redisclose Part 2 information that it receives from a Part 2 program to a third party unless there is a medical emergency or the third party is a contract agent of the HIO. Therefore, a HIO is not allowed to redisclose Part 2 information to a provider of “on-call coverage” without a patient’s written consent. FAQ II(3) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 43
 QSOAs: Providers of “On-Call Coverage” Ø HOWEVER, patient consent IS NOT needed for a HIO to redisclose patient information to providers “on-call coverage” when: (1) the providers are part of the Part 2 program; or (2) the providers are part of an entity that has direct administrative control over the program Note: In both circumstances, the on-call providers must need the information in connection with their duties that arise out of the provision of diagnosis, treatment or referral for treatment services. FAQ II(3) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 44
QSOAs: Providers of “On-Call Coverage” Ø HOWEVER, patient consent IS NOT needed for a HIO to redisclose patient information to providers “on-call coverage” when: (1) the providers are part of the Part 2 program; or (2) the providers are part of an entity that has direct administrative control over the program Note: In both circumstances, the on-call providers must need the information in connection with their duties that arise out of the provision of diagnosis, treatment or referral for treatment services. FAQ II(3) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 44
 HAVE QUESTIONS? Now for your questions. . . Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 45
HAVE QUESTIONS? Now for your questions. . . Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 45
 PART TWO MEDICAL EMERGENCY ISSUES Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 46
PART TWO MEDICAL EMERGENCY ISSUES Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 46
 Medical Emergency: Definition The Part 2 medical emergency provision states: “Patient identifying information may be disclosed to medical personnel who have a need for information about a patient for the purpose of treating a condition which poses an immediate threat to the health of any individual and which requires immediate medical intervention. ” 42 C. F. R. § 2. 51(a) FAQ I(24); FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 47
Medical Emergency: Definition The Part 2 medical emergency provision states: “Patient identifying information may be disclosed to medical personnel who have a need for information about a patient for the purpose of treating a condition which poses an immediate threat to the health of any individual and which requires immediate medical intervention. ” 42 C. F. R. § 2. 51(a) FAQ I(24); FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 47
 Medical Emergency: Definition Ø A medical emergency includes both physical and mental health emergencies under Part 2. FAQ I(29) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 48
Medical Emergency: Definition Ø A medical emergency includes both physical and mental health emergencies under Part 2. FAQ I(29) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 48
 Medical Emergency: Exception to Consent Ø When a medical emergency exists, patient consent IS NOT required under Part 2 in order to disclose Part 2 patient information to medical personnel treating the emergency. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 49
Medical Emergency: Exception to Consent Ø When a medical emergency exists, patient consent IS NOT required under Part 2 in order to disclose Part 2 patient information to medical personnel treating the emergency. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 49
 Medical Emergency: The Determination Case Study/Poll: Does a Part 2 program have to make the decision that a medical emergency exists? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 50
Medical Emergency: The Determination Case Study/Poll: Does a Part 2 program have to make the decision that a medical emergency exists? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 50
 Medical Emergency: The Determination Possible Answers: 1. Yes. 2. No. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 51
Medical Emergency: The Determination Possible Answers: 1. Yes. 2. No. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 51
 Medical Emergency: The Determination Answer: NO. Ø Ø A Part 2 program is not the only provider permitted to make the determination that a medical emergency exists. ANY health care provider who is treating a patient for a medical emergency IS ALLOWED to make the determination that a medical emergency exists warranting “breaking the glass, ” in order to obtain access to a patient’s Part 2 records through a HIO without the patient’s consent. FAQ I(24) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 52
Medical Emergency: The Determination Answer: NO. Ø Ø A Part 2 program is not the only provider permitted to make the determination that a medical emergency exists. ANY health care provider who is treating a patient for a medical emergency IS ALLOWED to make the determination that a medical emergency exists warranting “breaking the glass, ” in order to obtain access to a patient’s Part 2 records through a HIO without the patient’s consent. FAQ I(24) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 52
 Medical Emergency: The Determination Ø Ø A computer system cannot make the determination that a medical emergency exists under Part 2. The treating health care provider must use their professional judgment to determine whether the situation meets the definition of medical emergency under Part 2. FAQ I(25) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 53
Medical Emergency: The Determination Ø Ø A computer system cannot make the determination that a medical emergency exists under Part 2. The treating health care provider must use their professional judgment to determine whether the situation meets the definition of medical emergency under Part 2. FAQ I(25) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 53
 Medical Emergency: The Determination Ø Once the health care provider determines that a true medical emergency exits, then the HIO may make clinical decision support functions, including without limitation, showing a patient’s medications to clinicians when they write prescriptions, automatically ordering medications, and/or alerting clinicians about potential drug interactions, available to the health care provider. FAQ I(28) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 54
Medical Emergency: The Determination Ø Once the health care provider determines that a true medical emergency exits, then the HIO may make clinical decision support functions, including without limitation, showing a patient’s medications to clinicians when they write prescriptions, automatically ordering medications, and/or alerting clinicians about potential drug interactions, available to the health care provider. FAQ I(28) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 54
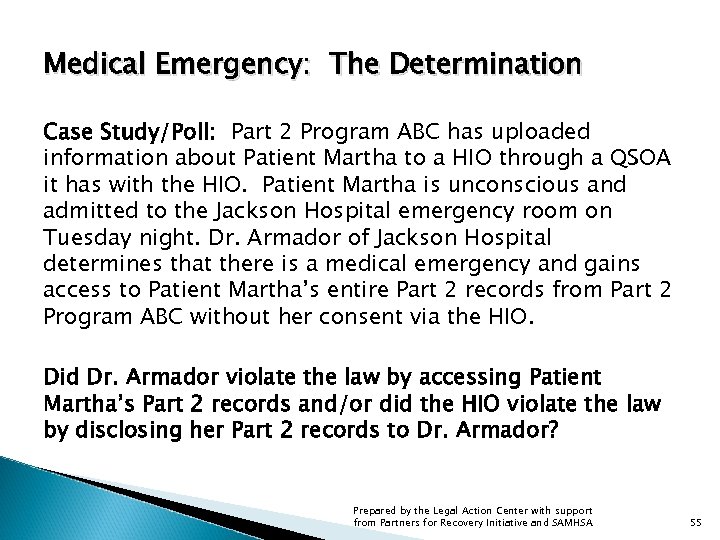 Medical Emergency: The Determination Case Study/Poll: Part 2 Program ABC has uploaded information about Patient Martha to a HIO through a QSOA it has with the HIO. Patient Martha is unconscious and admitted to the Jackson Hospital emergency room on Tuesday night. Dr. Armador of Jackson Hospital determines that there is a medical emergency and gains access to Patient Martha’s entire Part 2 records from Part 2 Program ABC without her consent via the HIO. Did Dr. Armador violate the law by accessing Patient Martha’s Part 2 records and/or did the HIO violate the law by disclosing her Part 2 records to Dr. Armador? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 55
Medical Emergency: The Determination Case Study/Poll: Part 2 Program ABC has uploaded information about Patient Martha to a HIO through a QSOA it has with the HIO. Patient Martha is unconscious and admitted to the Jackson Hospital emergency room on Tuesday night. Dr. Armador of Jackson Hospital determines that there is a medical emergency and gains access to Patient Martha’s entire Part 2 records from Part 2 Program ABC without her consent via the HIO. Did Dr. Armador violate the law by accessing Patient Martha’s Part 2 records and/or did the HIO violate the law by disclosing her Part 2 records to Dr. Armador? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 55
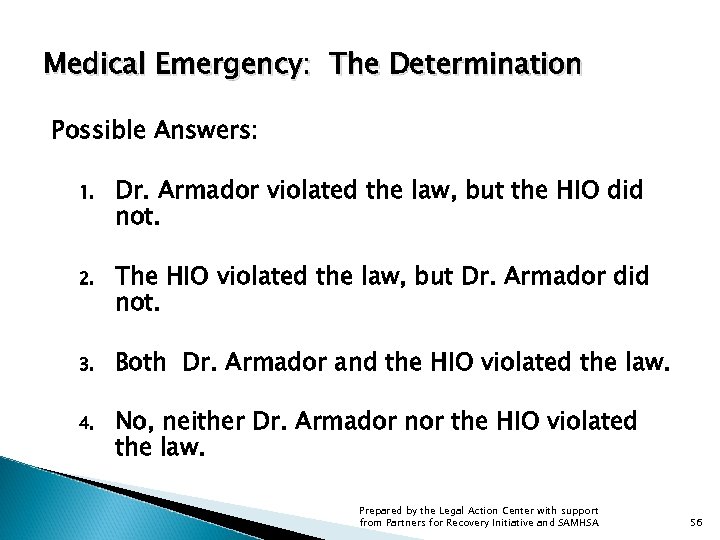 Medical Emergency: The Determination Possible Answers: 1. Dr. Armador violated the law, but the HIO did not. 2. The HIO violated the law, but Dr. Armador did not. 3. Both Dr. Armador and the HIO violated the law. 4. No, neither Dr. Armador nor the HIO violated the law. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 56
Medical Emergency: The Determination Possible Answers: 1. Dr. Armador violated the law, but the HIO did not. 2. The HIO violated the law, but Dr. Armador did not. 3. Both Dr. Armador and the HIO violated the law. 4. No, neither Dr. Armador nor the HIO violated the law. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 56
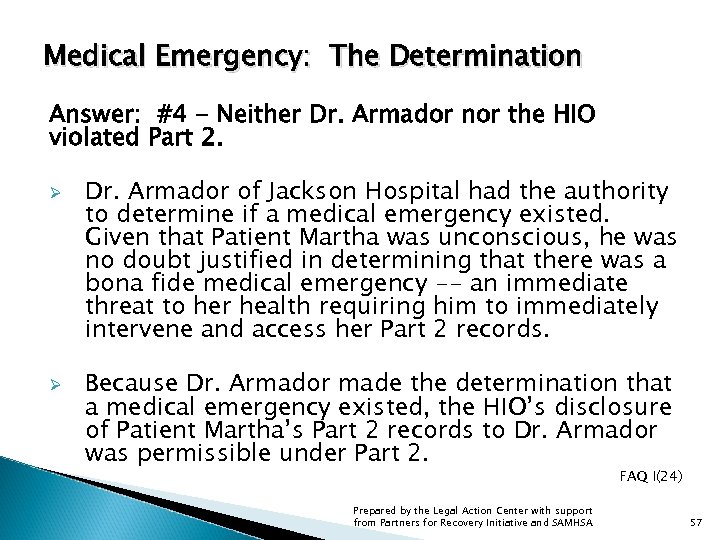 Medical Emergency: The Determination Answer: #4 - Neither Dr. Armador nor the HIO violated Part 2. Ø Ø Dr. Armador of Jackson Hospital had the authority to determine if a medical emergency existed. Given that Patient Martha was unconscious, he was no doubt justified in determining that there was a bona fide medical emergency -- an immediate threat to her health requiring him to immediately intervene and access her Part 2 records. Because Dr. Armador made the determination that a medical emergency existed, the HIO’s disclosure of Patient Martha’s Part 2 records to Dr. Armador was permissible under Part 2. FAQ I(24) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 57
Medical Emergency: The Determination Answer: #4 - Neither Dr. Armador nor the HIO violated Part 2. Ø Ø Dr. Armador of Jackson Hospital had the authority to determine if a medical emergency existed. Given that Patient Martha was unconscious, he was no doubt justified in determining that there was a bona fide medical emergency -- an immediate threat to her health requiring him to immediately intervene and access her Part 2 records. Because Dr. Armador made the determination that a medical emergency existed, the HIO’s disclosure of Patient Martha’s Part 2 records to Dr. Armador was permissible under Part 2. FAQ I(24) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 57
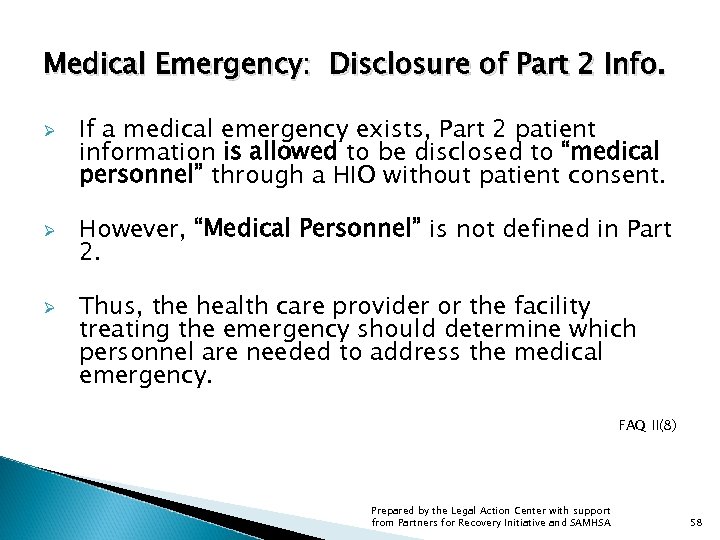 Medical Emergency: Disclosure of Part 2 Info. Ø Ø Ø If a medical emergency exists, Part 2 patient information is allowed to be disclosed to “medical personnel” through a HIO without patient consent. However, “Medical Personnel” is not defined in Part 2. Thus, the health care provider or the facility treating the emergency should determine which personnel are needed to address the medical emergency. FAQ II(8) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 58
Medical Emergency: Disclosure of Part 2 Info. Ø Ø Ø If a medical emergency exists, Part 2 patient information is allowed to be disclosed to “medical personnel” through a HIO without patient consent. However, “Medical Personnel” is not defined in Part 2. Thus, the health care provider or the facility treating the emergency should determine which personnel are needed to address the medical emergency. FAQ II(8) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 58
 Medical Emergency: Disclosure of Part 2 Info. Ø Ø Under Part 2, all disclosures made must be limited to the information necessary to carry out the purpose of the disclosure. When a medical emergency exists, a patient’s entire Part 2 record can be released to a treating health care provider without the patient’s consent if needed to treat the condition. FAQ I(26); FAQ I(33) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 59
Medical Emergency: Disclosure of Part 2 Info. Ø Ø Under Part 2, all disclosures made must be limited to the information necessary to carry out the purpose of the disclosure. When a medical emergency exists, a patient’s entire Part 2 record can be released to a treating health care provider without the patient’s consent if needed to treat the condition. FAQ I(26); FAQ I(33) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 59
 Medical Emergency: Disclosure of Part 2 Info. Ø HIO Disclosures in a Medical Emergency: § Ø A HIO system IS PERMITTED to show the treating provider the information that is needed to treat the emergency, including Part 2 patient information without patient consent. HIO Disclosures in a Non-Medical Emergency: § The HIO system MAY NOT disclose any Part 2 data to the treating provider absent patient consent. FAQ I (28) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 60
Medical Emergency: Disclosure of Part 2 Info. Ø HIO Disclosures in a Medical Emergency: § Ø A HIO system IS PERMITTED to show the treating provider the information that is needed to treat the emergency, including Part 2 patient information without patient consent. HIO Disclosures in a Non-Medical Emergency: § The HIO system MAY NOT disclose any Part 2 data to the treating provider absent patient consent. FAQ I (28) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 60
 Medical Emergency: Disclosure of Part 2 Info. Ø Ø Ø Redisclosure of Part 2 information IS NOT prohibited once it is released in a medical emergency situation. Medical personnel treating a patient for a medical emergency who are HIO affiliated providers are allowed to download and include in their own records the information they obtained in treating the emergency, and may then redisclose that information to others without obtaining patient consent. However, the information still remains protected within the HIO and the HIO will need consent to release the Part 2 information in a non-medical emergency. FAQ I(33) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 61
Medical Emergency: Disclosure of Part 2 Info. Ø Ø Ø Redisclosure of Part 2 information IS NOT prohibited once it is released in a medical emergency situation. Medical personnel treating a patient for a medical emergency who are HIO affiliated providers are allowed to download and include in their own records the information they obtained in treating the emergency, and may then redisclose that information to others without obtaining patient consent. However, the information still remains protected within the HIO and the HIO will need consent to release the Part 2 information in a non-medical emergency. FAQ I(33) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 61
 Medical Emergency: Disclosure of Part 2 Info. Ø Ø Under Part 2, even if a patient previously refused to consent to the release of her Part 2 records to a particular HIO affiliated health care provider, it would still be permissible for her records to be released to that provider in a medical emergency. However, HIO policies or State laws may prohibit HIOs from redisclosing Part 2 records to a HIO affiliated health care provider when a patient has previously refused to consent to the release of her records even in an medical emergency situation. FAQ I(34) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 62
Medical Emergency: Disclosure of Part 2 Info. Ø Ø Under Part 2, even if a patient previously refused to consent to the release of her Part 2 records to a particular HIO affiliated health care provider, it would still be permissible for her records to be released to that provider in a medical emergency. However, HIO policies or State laws may prohibit HIOs from redisclosing Part 2 records to a HIO affiliated health care provider when a patient has previously refused to consent to the release of her records even in an medical emergency situation. FAQ I(34) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 62
 Medical Emergency: Disclosure of Part 2 Info. Case Study/Poll: Patient Tim goes to Dr. Smith because his back is in excruciating pain. Dr. Smith is unwilling to prescribe any medications to Patient Tim without knowing the medications that Tim is taking for fear of a drug interaction. Dr. Smith may: Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 63
Medical Emergency: Disclosure of Part 2 Info. Case Study/Poll: Patient Tim goes to Dr. Smith because his back is in excruciating pain. Dr. Smith is unwilling to prescribe any medications to Patient Tim without knowing the medications that Tim is taking for fear of a drug interaction. Dr. Smith may: Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 63
 Medical Emergency: Disclosure of Part 2 Info. Possible Answers: 1. Ask Patient Tim about the medications he is taking and obtain his written consent to obtain additional information. 2. Declare a medical emergency and “break the glass” in order to obtain any Part 2 information about Patient Tim that may be useful. 3. Neither 1 nor 2. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 64
Medical Emergency: Disclosure of Part 2 Info. Possible Answers: 1. Ask Patient Tim about the medications he is taking and obtain his written consent to obtain additional information. 2. Declare a medical emergency and “break the glass” in order to obtain any Part 2 information about Patient Tim that may be useful. 3. Neither 1 nor 2. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 64
 Medical Emergency: Disclosure of Part 2 Info. Answer: #1. Because the situation is not a medical emergency, Dr. Smith can only ask Patient Tim about the medications he is taking and try to obtain his written consent to obtain additional information. Ø In this situation, a HIO system is not allowed to disclose any Part 2 data to Dr. Smith about Patient Tim UNLESS: (1) there is a medical emergency; (2) Patient Tim provides written consent to the disclosure; or (3) a consent form authorizing disclosure to Dr. Smith already exists in the HIE environment. § Ø The HIO system could notify Dr. Smith that consent from Patient Tim is needed, but such notice cannot reveal that Part 2 information about Patient Tim exists. If Dr. Smith knew that Patient Tim was in a Part 2 program and had a QSOA with that Part 2 Program, he would be able to obtain Part 2 information about Tim directly from the program. FAQ I(28) ; FAQ II(9) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 65
Medical Emergency: Disclosure of Part 2 Info. Answer: #1. Because the situation is not a medical emergency, Dr. Smith can only ask Patient Tim about the medications he is taking and try to obtain his written consent to obtain additional information. Ø In this situation, a HIO system is not allowed to disclose any Part 2 data to Dr. Smith about Patient Tim UNLESS: (1) there is a medical emergency; (2) Patient Tim provides written consent to the disclosure; or (3) a consent form authorizing disclosure to Dr. Smith already exists in the HIE environment. § Ø The HIO system could notify Dr. Smith that consent from Patient Tim is needed, but such notice cannot reveal that Part 2 information about Patient Tim exists. If Dr. Smith knew that Patient Tim was in a Part 2 program and had a QSOA with that Part 2 Program, he would be able to obtain Part 2 information about Tim directly from the program. FAQ I(28) ; FAQ II(9) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 65
 Medical Emergency: Disclosure of Part 2 Info. Ø Ø Concern alone about potential drug interaction may be insufficient to meet the standard of a medical emergency. SAMHSA recommends obtaining patient consent in such circumstances. “If a health care provider treating an individual determines that a medical emergency exists as defined in Part 2. . . and in treating the medical emergency the health care provider needs information about potential drug interactions, then that information and any other information contained in the Part 2 record that the treating health care provider determines he or she needs to treat the medical emergency can be disclosed. ” FAQ II(9) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 66
Medical Emergency: Disclosure of Part 2 Info. Ø Ø Concern alone about potential drug interaction may be insufficient to meet the standard of a medical emergency. SAMHSA recommends obtaining patient consent in such circumstances. “If a health care provider treating an individual determines that a medical emergency exists as defined in Part 2. . . and in treating the medical emergency the health care provider needs information about potential drug interactions, then that information and any other information contained in the Part 2 record that the treating health care provider determines he or she needs to treat the medical emergency can be disclosed. ” FAQ II(9) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 66
 Medical Emergency: Documenting the Disclosure Ø A Part 2 program IS REQUIRED to document in writing the disclosure made in a medical emergency in the patient’s records, including: (1) The name of the medical personnel who received the disclosure and their affiliation with any health care facility; (2) The name of the person who made the disclosure (3) The date and time of the disclosure; AND (4) The nature of the emergency. FAQ I(27); FAQ II(7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 67
Medical Emergency: Documenting the Disclosure Ø A Part 2 program IS REQUIRED to document in writing the disclosure made in a medical emergency in the patient’s records, including: (1) The name of the medical personnel who received the disclosure and their affiliation with any health care facility; (2) The name of the person who made the disclosure (3) The date and time of the disclosure; AND (4) The nature of the emergency. FAQ I(27); FAQ II(7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 67
 Medical Emergency: Documenting the Disclosure Ø One of the policy reasons behind Part 2’s documentation requirements is to hold individuals accountable for their decisions when Part 2 patient information is disclosed without patient consent in a medical emergency situation. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 68
Medical Emergency: Documenting the Disclosure Ø One of the policy reasons behind Part 2’s documentation requirements is to hold individuals accountable for their decisions when Part 2 patient information is disclosed without patient consent in a medical emergency situation. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 68
 Medical Emergency: Documenting the Disclosure Ø Consistent with that policy, when Part 2 records are disclosed via a HIO in a medical emergency situation, the Part 2 documentation requirements still apply to Part 2 programs. FAQ II(7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 69
Medical Emergency: Documenting the Disclosure Ø Consistent with that policy, when Part 2 records are disclosed via a HIO in a medical emergency situation, the Part 2 documentation requirements still apply to Part 2 programs. FAQ II(7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 69
 Medical Emergency: Documenting the Disclosure Ø Thus, “SAMHSA recommends that HIE data systems be designed to ensure that a Part 2 program is notified when a disclosure occurs and Part 2 records are released pursuant to a medical emergency. ” § § Notification should include all the information that the Part 2 program is required to document in the patient’s records. SAMHSA suggests that the information about the disclosures also be kept in the HIO’s electronic system and protected using appropriate safeguards. FAQ I(30); FAQ II(7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 70
Medical Emergency: Documenting the Disclosure Ø Thus, “SAMHSA recommends that HIE data systems be designed to ensure that a Part 2 program is notified when a disclosure occurs and Part 2 records are released pursuant to a medical emergency. ” § § Notification should include all the information that the Part 2 program is required to document in the patient’s records. SAMHSA suggests that the information about the disclosures also be kept in the HIO’s electronic system and protected using appropriate safeguards. FAQ I(30); FAQ II(7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 70
 Medical Emergency: Documenting the Disclosure Ø A Part 2 program SHOULD ENSURE that a HIO that it affiliates itself with can comply with all of Part 2 requirements, including the ability to notify the Part 2 program when its records have been disclosed because of a medical emergency. FAQ II(7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 71
Medical Emergency: Documenting the Disclosure Ø A Part 2 program SHOULD ENSURE that a HIO that it affiliates itself with can comply with all of Part 2 requirements, including the ability to notify the Part 2 program when its records have been disclosed because of a medical emergency. FAQ II(7) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 71
 Medical Emergency: Documenting the Disclosure Ø In a medical emergency, a treating provider should also record the same information that a Part 2 program is required to record and that information should be conveyed to the Part 2 program. § § A treating provider is permitted to check a drop down box to signify that a medical emergency exists. In a medical emergency situation, such documentation in and of itself is not sufficient to meet the four documentation requirements under Part 2. Automated electronic systems may be used to generate information necessary for a provider: (1) to make a determination of a medical emergency; (2) to enable a provider’s entry of emergency information; and/or (3) to generate a report documenting the emergency. FAQ I(27) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 72
Medical Emergency: Documenting the Disclosure Ø In a medical emergency, a treating provider should also record the same information that a Part 2 program is required to record and that information should be conveyed to the Part 2 program. § § A treating provider is permitted to check a drop down box to signify that a medical emergency exists. In a medical emergency situation, such documentation in and of itself is not sufficient to meet the four documentation requirements under Part 2. Automated electronic systems may be used to generate information necessary for a provider: (1) to make a determination of a medical emergency; (2) to enable a provider’s entry of emergency information; and/or (3) to generate a report documenting the emergency. FAQ I(27) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 72
 Medical Emergency: Documenting the Disclosure Example: Patient Mike’s Part 2 records were disclosed to Dr. Apple of Madison Hospital via a HIO in a situation that constituted a medical emergency situation. The HIO maintained an electronic record of the Part 2 disclosures that were made. However, Part 2 Program ABC (the originating program) did not record the medical emergency in Patient Mike’s records. Is the HIO’s electronic record of the medical emergency sufficient to meet Part 2’s requirement? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 73
Medical Emergency: Documenting the Disclosure Example: Patient Mike’s Part 2 records were disclosed to Dr. Apple of Madison Hospital via a HIO in a situation that constituted a medical emergency situation. The HIO maintained an electronic record of the Part 2 disclosures that were made. However, Part 2 Program ABC (the originating program) did not record the medical emergency in Patient Mike’s records. Is the HIO’s electronic record of the medical emergency sufficient to meet Part 2’s requirement? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 73
 Medical Emergency: Documenting the Disclosure Answer: No. Program ABC is required to document the disclosure in the patient’s records pursuant to 42 C. F. R. 2. 51(c). Ø Ø It is good practice for the disclosure information to be kept in the HIO’s electronic system. The HIO should be capable of notifying the Part 2 program that the disclosure took place in a medical emergency. FAQ I(30) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 74
Medical Emergency: Documenting the Disclosure Answer: No. Program ABC is required to document the disclosure in the patient’s records pursuant to 42 C. F. R. 2. 51(c). Ø Ø It is good practice for the disclosure information to be kept in the HIO’s electronic system. The HIO should be capable of notifying the Part 2 program that the disclosure took place in a medical emergency. FAQ I(30) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 74
 Medical Emergency: Documenting the Disclosure Ø Ø Ø As previously noted, Part 2 requires the name of the person who made the disclosure to be documented in writing in the patient’s records. It is INSUFFICIENT to document the name of the DISCLOSER as “electronically disclosed through the system administered by HIO” under Part 2’s requirements. The name of the person who makes the determination that the situation was in fact a medical emergency and “documentation of disclosure made electronically through a system administered by the HIO should be recorded in the HIO’s electronic system. FAQ I(31) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 75
Medical Emergency: Documenting the Disclosure Ø Ø Ø As previously noted, Part 2 requires the name of the person who made the disclosure to be documented in writing in the patient’s records. It is INSUFFICIENT to document the name of the DISCLOSER as “electronically disclosed through the system administered by HIO” under Part 2’s requirements. The name of the person who makes the determination that the situation was in fact a medical emergency and “documentation of disclosure made electronically through a system administered by the HIO should be recorded in the HIO’s electronic system. FAQ I(31) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 75
 Medical Emergency: Documenting the Disclosure Ø Ø Ø As previously noted, Part 2 requires “the name of the medical personnel who received the disclosure and their affiliation with any health care facility” to be documented in writing in the patient’s records. Documenting the name of the medical personnel to whom the disclosure was made as “the printer in the emergency department” IS INSUFFICIENT to meet Part 2’s requirement. This is true even if a HIO’s electronic system sends Part 2 data in a medical emergency to a printer or fax machine in the emergency room. FAQ I(32) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 76
Medical Emergency: Documenting the Disclosure Ø Ø Ø As previously noted, Part 2 requires “the name of the medical personnel who received the disclosure and their affiliation with any health care facility” to be documented in writing in the patient’s records. Documenting the name of the medical personnel to whom the disclosure was made as “the printer in the emergency department” IS INSUFFICIENT to meet Part 2’s requirement. This is true even if a HIO’s electronic system sends Part 2 data in a medical emergency to a printer or fax machine in the emergency room. FAQ I(32) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 76
 HAVE QUESTIONS? Now for your questions. . . Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 77
HAVE QUESTIONS? Now for your questions. . . Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 77
 PART THREE Immediate Threats to Health or Safety of an Individual or the Public Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 78
PART THREE Immediate Threats to Health or Safety of an Individual or the Public Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 78
 Immediate Threats: Disclosures If there is an immediate threat to the health or safety of an individual or the public, Part 2 may permit the disclosure of information under certain circumstances without a patient’s consent. Those circumstances may be: Ø in a medical emergency situation as we just discussed; OR Ø in other limited situations, which we will discuss now. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 79
Immediate Threats: Disclosures If there is an immediate threat to the health or safety of an individual or the public, Part 2 may permit the disclosure of information under certain circumstances without a patient’s consent. Those circumstances may be: Ø in a medical emergency situation as we just discussed; OR Ø in other limited situations, which we will discuss now. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 79
 Immediate Threats: Disclosures Notifications to Law Enforcement: A Part 2 program is permitted to notify law enforcement if an immediate threat to the health or safety of an individual exists due to a crime on program premises OR against program personnel. Ø In either of these circumstances, A Part 2 program is allowed to disclose information relating to the incident without patient consent, including: (1) the name of the suspect (even if a Program 2 patient); (2) address; (3) last known whereabouts; and (4) status as a patient in the program. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 80
Immediate Threats: Disclosures Notifications to Law Enforcement: A Part 2 program is permitted to notify law enforcement if an immediate threat to the health or safety of an individual exists due to a crime on program premises OR against program personnel. Ø In either of these circumstances, A Part 2 program is allowed to disclose information relating to the incident without patient consent, including: (1) the name of the suspect (even if a Program 2 patient); (2) address; (3) last known whereabouts; and (4) status as a patient in the program. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 80
 Immediate Threats: Disclosures Immediate Threat to Health or Safety (Not Medical Emergencies or Crimes on Program Premises or Against Program Personnel): Part 2 programs, health care providers and HIOs, who have received Part 2 information, are allowed to make reports to law enforcement about an immediate threat to the health or safety of an individual or the public if patientidentifying information is not disclosed. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 81
Immediate Threats: Disclosures Immediate Threat to Health or Safety (Not Medical Emergencies or Crimes on Program Premises or Against Program Personnel): Part 2 programs, health care providers and HIOs, who have received Part 2 information, are allowed to make reports to law enforcement about an immediate threat to the health or safety of an individual or the public if patientidentifying information is not disclosed. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 81
 Immediate Threats: Disclosures Reports of Child Abuse and Neglect: The restrictions on disclosure are not applicable to the reporting under State law of incidents of suspected child abuse and neglect to the appropriate State or local authorities. Ø Ø Part 2 restrictions still apply to the original alcohol or drug abuse patient records that are maintained by the Part 2 program, including their disclosure and use for civil or criminal proceedings which may arise out of the report of suspected child abuse and neglect. A court order may authorize disclosure of confidential communications made by a patient to a Part 2 program if the disclosure is necessary to protect against an existing threat of life or of serious bodily injury, including circumstances which constitute suspected child abuse and neglect. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 82
Immediate Threats: Disclosures Reports of Child Abuse and Neglect: The restrictions on disclosure are not applicable to the reporting under State law of incidents of suspected child abuse and neglect to the appropriate State or local authorities. Ø Ø Part 2 restrictions still apply to the original alcohol or drug abuse patient records that are maintained by the Part 2 program, including their disclosure and use for civil or criminal proceedings which may arise out of the report of suspected child abuse and neglect. A court order may authorize disclosure of confidential communications made by a patient to a Part 2 program if the disclosure is necessary to protect against an existing threat of life or of serious bodily injury, including circumstances which constitute suspected child abuse and neglect. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 82
 Immediate Threats: Disclosures Court Ordered Disclosures: Under Part 2, Part 2 programs or “any person having a legally recognized interest in the disclosure which is sought” may apply to a court for an order authorizing disclosure of protected patient information. If the court order is granted, the information may be disclosed. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 83
Immediate Threats: Disclosures Court Ordered Disclosures: Under Part 2, Part 2 programs or “any person having a legally recognized interest in the disclosure which is sought” may apply to a court for an order authorizing disclosure of protected patient information. If the court order is granted, the information may be disclosed. FAQ II(5) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 83
 PART FOUR Screening, Brief Intervention and Referral to Treatment (“SBIRT”) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 84
PART FOUR Screening, Brief Intervention and Referral to Treatment (“SBIRT”) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 84
 SBIRT: Definition Ø Ø Screening, Brief Intervention and Referral to Treatment (“SBIRT”): “a comprehensive, integrated, public health, approach to the screening and identification of individuals who are practicing risky alcohol and drug use, and the timely delivery of early brief interventions to the people in order to reduce risky use, if not successful, leads to their timely referral to move intensive substance abuse interventions. ” For more information on “SBIRT” visit www. samhsa. gov/grants/2011 ti_11_014. aspx FAQ II (11) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 85
SBIRT: Definition Ø Ø Screening, Brief Intervention and Referral to Treatment (“SBIRT”): “a comprehensive, integrated, public health, approach to the screening and identification of individuals who are practicing risky alcohol and drug use, and the timely delivery of early brief interventions to the people in order to reduce risky use, if not successful, leads to their timely referral to move intensive substance abuse interventions. ” For more information on “SBIRT” visit www. samhsa. gov/grants/2011 ti_11_014. aspx FAQ II (11) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 85
 SBIRT: Who Conducts SBIRT? Examples: Ø Part 2 programs Ø Federally qualified health centers Ø Hospital emergency rooms Ø Trauma centers Ø Other community programs Ø Physicians’ offices Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 86
SBIRT: Who Conducts SBIRT? Examples: Ø Part 2 programs Ø Federally qualified health centers Ø Hospital emergency rooms Ø Trauma centers Ø Other community programs Ø Physicians’ offices Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 86
 SBIRT: Part 2 Protections Whether patient information is protected by Part 2 when SBIRT services are conducted depends on whether the entity conducting the SBIRT activities is a Part 2 program as defined in the regulations. Ø Part 2 Program: COVERED Ø Not A Part 2 Program: NOT COVERED FAQ II(11) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 87
SBIRT: Part 2 Protections Whether patient information is protected by Part 2 when SBIRT services are conducted depends on whether the entity conducting the SBIRT activities is a Part 2 program as defined in the regulations. Ø Part 2 Program: COVERED Ø Not A Part 2 Program: NOT COVERED FAQ II(11) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 87
 Who must follow 42 C. F. R Part 2? To be covered by Part 2, a provider must meet the definition of “program” and be federally assisted. Definition of a program: 1. individual/entity other than general medical facility which holds itself out as providing and provides alcohol/drug diagnosis, treatment, or referral for treatment; or more… Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 88
Who must follow 42 C. F. R Part 2? To be covered by Part 2, a provider must meet the definition of “program” and be federally assisted. Definition of a program: 1. individual/entity other than general medical facility which holds itself out as providing and provides alcohol/drug diagnosis, treatment, or referral for treatment; or more… Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 88
 Who must follow 42 C. F. R Part 2? Definition 1. 2. of a program continued: an identified unit within a general medical facility which holds itself out as providing and provides alcohol/drug diagnosis, treatment, or referral for treatment; or Medical personnel or other staff in a general medical care facility whose primary function is the provision of alcohol/drug diagnosis, treatment, or referral for treatment and who are identified as such. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 89
Who must follow 42 C. F. R Part 2? Definition 1. 2. of a program continued: an identified unit within a general medical facility which holds itself out as providing and provides alcohol/drug diagnosis, treatment, or referral for treatment; or Medical personnel or other staff in a general medical care facility whose primary function is the provision of alcohol/drug diagnosis, treatment, or referral for treatment and who are identified as such. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 89
 SBIRT: Part 2 Protections Case Study/Poll: Tim is admitted to Madison Hospital’s Emergency Room for alcohol poisoning. During his time in the emergency room, he is brought to a unit of the hospital that holds itself out as providing and provides alcohol and drug treatment, where SBIRT services are conducted. He is told that he should seek treatment for his alcohol use. He refuses treatment. Are Tim’s SBIRT patient records subject to Part 2? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 90
SBIRT: Part 2 Protections Case Study/Poll: Tim is admitted to Madison Hospital’s Emergency Room for alcohol poisoning. During his time in the emergency room, he is brought to a unit of the hospital that holds itself out as providing and provides alcohol and drug treatment, where SBIRT services are conducted. He is told that he should seek treatment for his alcohol use. He refuses treatment. Are Tim’s SBIRT patient records subject to Part 2? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 90
 SBIRT: Part 2 Protections Possible Answers: 1. Yes. 2. No. 3. Not enough information. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 91
SBIRT: Part 2 Protections Possible Answers: 1. Yes. 2. No. 3. Not enough information. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 91
 SBIRT: Part 2 Protections Answer: YES. Tim received services from a unit in a general medical facility that holds itself out as providing and provides alcohol and drug treatment. Because the unit conducted the SBIRT services, the patient records are covered under Part 2. FAQ II(11) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 92
SBIRT: Part 2 Protections Answer: YES. Tim received services from a unit in a general medical facility that holds itself out as providing and provides alcohol and drug treatment. Because the unit conducted the SBIRT services, the patient records are covered under Part 2. FAQ II(11) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 92
 SBIRT: Part 2 Protections Case Study/Poll: Would your answer to the prior question change if the emergency room physician treating Patient Tim had conducted the SBIRT and that physician’s primary function was not the provision of alcohol/drug diagnosis, treatment, or referral for treatment? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 93
SBIRT: Part 2 Protections Case Study/Poll: Would your answer to the prior question change if the emergency room physician treating Patient Tim had conducted the SBIRT and that physician’s primary function was not the provision of alcohol/drug diagnosis, treatment, or referral for treatment? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 93
 SBIRT: Part 2 Protections Possible Answers: 1. Yes, my answer would change. 2. No, same answer. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 94
SBIRT: Part 2 Protections Possible Answers: 1. Yes, my answer would change. 2. No, same answer. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 94
 SBIRT: Part 2 Protections Answer: Yes, my answer would change. The emergency room physician is not considered a Part 2 program and Patient Tim’s SBIRT records would not be covered under Part 2. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 95
SBIRT: Part 2 Protections Answer: Yes, my answer would change. The emergency room physician is not considered a Part 2 program and Patient Tim’s SBIRT records would not be covered under Part 2. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 95
 SBIRT: Part 2 Protections Case Study/Poll: If Ms. Jones (whose primary function at Madison Hospital is to provide alcohol or drug abuse diagnosis, treatment or referral for treatment and she is identified as a provider of such services) conducted the SBIRT services for Patient Tim in the emergency room of Madison Hospital, would Tim’s SBIRT patient records be subject to Part 2 regulations? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 96
SBIRT: Part 2 Protections Case Study/Poll: If Ms. Jones (whose primary function at Madison Hospital is to provide alcohol or drug abuse diagnosis, treatment or referral for treatment and she is identified as a provider of such services) conducted the SBIRT services for Patient Tim in the emergency room of Madison Hospital, would Tim’s SBIRT patient records be subject to Part 2 regulations? Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 96
 SBIRT: Part 2 Protections Possible Answers: 1. Yes. 2. No. 3. Not enough information. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 97
SBIRT: Part 2 Protections Possible Answers: 1. Yes. 2. No. 3. Not enough information. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 97
 SBIRT: Part 2 Protections Answer: #1 YES. Patient Tim’s SBIRT records would be protected under Part 2 because Ms. Jones’s primary function at Madison Hospital is to provide alcohol or drug abuse diagnosis, treatment or referral for treatment and she is identified as a provider of such services. FAQ II(10 and 11) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 98
SBIRT: Part 2 Protections Answer: #1 YES. Patient Tim’s SBIRT records would be protected under Part 2 because Ms. Jones’s primary function at Madison Hospital is to provide alcohol or drug abuse diagnosis, treatment or referral for treatment and she is identified as a provider of such services. FAQ II(10 and 11) Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 98
 HAVE QUESTIONS? Now for your questions. . . Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 99
HAVE QUESTIONS? Now for your questions. . . Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 99
 Your feedback How did you like this webinar? We welcome your feedback. Please complete the survey that will appear when you exit this webinar. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 100
Your feedback How did you like this webinar? We welcome your feedback. Please complete the survey that will appear when you exit this webinar. Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 100
 Thank you Prepared in 2012 by – the Legal Action Center, under a subcontract from Partners for Recovery Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 101
Thank you Prepared in 2012 by – the Legal Action Center, under a subcontract from Partners for Recovery Prepared by the Legal Action Center with support from Partners for Recovery Initiative and SAMHSA 101


