956c2b63383a04ff54070fdd118fee6f.ppt
- Количество слайдов: 81
Welcome to the NQF Safe Practices for Better Healthcare 2009 Update Webinar: Important Condition and Common Safety Issues (Safe Practices 26 -34) Hosted by NQF and TMIT Attendee dial-in instructions: Toll-free Call-in number (US/Canada): 1 -866 -764 -6260 (direct number, no code needed) To join the online webinar, go to: www. safetyleaders. org Online Access Password: Webinar 1 (case-sensitive) 1
Welcome and Updates and Developments on the 9 Practices Peter B. Angood, MD, FRCS(C), FACS, FCCM Senior Advisor, Patient Safety, National Quality Forum Toll-free Call-in number: 1 -866 -764 -6260 Safe Practices Webinar September 17, 2009 2

Panelists Peter Angood Charles Denham Donald Kennerly Welcome and Updates and Developments on the 9 Practices Charles Denham: Safe Practice Implementation from 30, 000 Feet Donald Kennerly: Prioritizing the Focus of Institutional Effort Donald Moorman: Correct Site Surgery – It Becomes More Than Just the OR Dan Ford: Patient Perspective on Prioritizing Safety Donald Moorman Peter Angood: Toll-free Call-in number: 1 -866 -764 -6260 Dan Ford 3
4
5
6
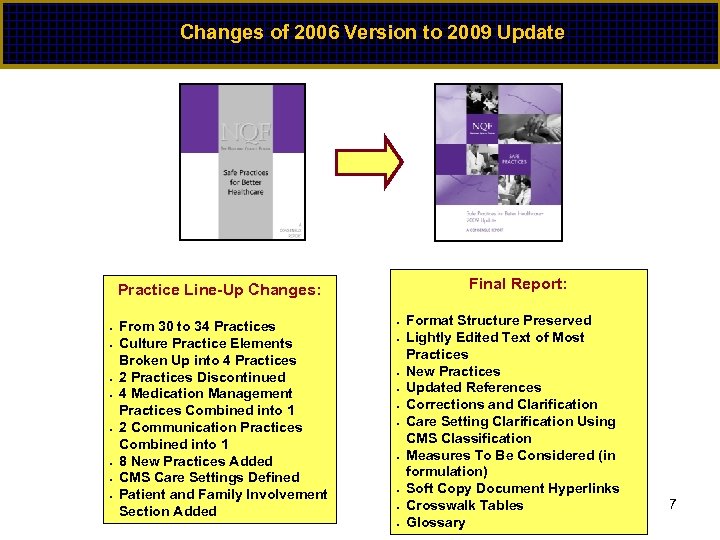
Changes of 2006 Version to 2009 Update Final Report: Practice Line-Up Changes: • • From 30 to 34 Practices Culture Practice Elements Broken Up into 4 Practices 2 Practices Discontinued 4 Medication Management Practices Combined into 1 2 Communication Practices Combined into 1 8 New Practices Added CMS Care Settings Defined Patient and Family Involvement Section Added • • • Format Structure Preserved Lightly Edited Text of Most Practices New Practices Updated References Corrections and Clarification Care Setting Clarification Using CMS Classification Measures To Be Considered (in formulation) Soft Copy Document Hyperlinks Crosswalk Tables Glossary 7
Toll-free Call-in number: 1 -866 -764 -6260 8

Harmonization – The Quality Choir Toll-free Call-in number: 1 -866 -764 -6260 9
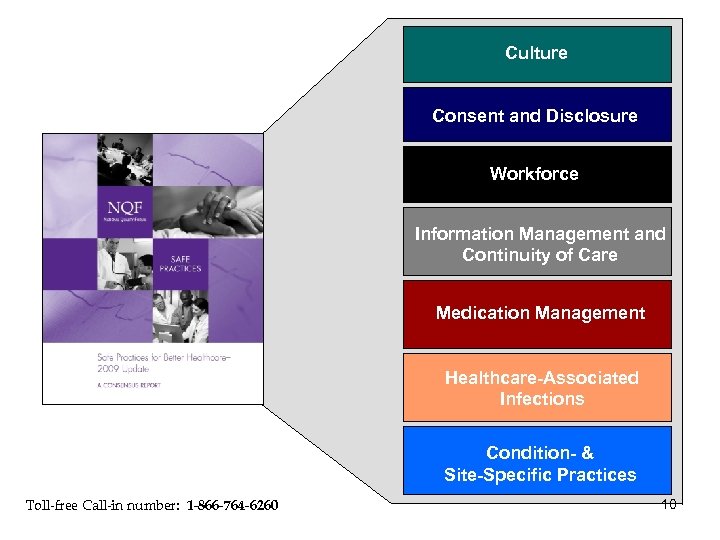
Culture Consent & Disclosure Consent and Disclosure Workforce Information Management and Continuity of Care Medication Management Healthcare-Associated Infections Condition- & Site-Specific Practices Toll-free Call-in number: 1 -866 -764 -6260 10
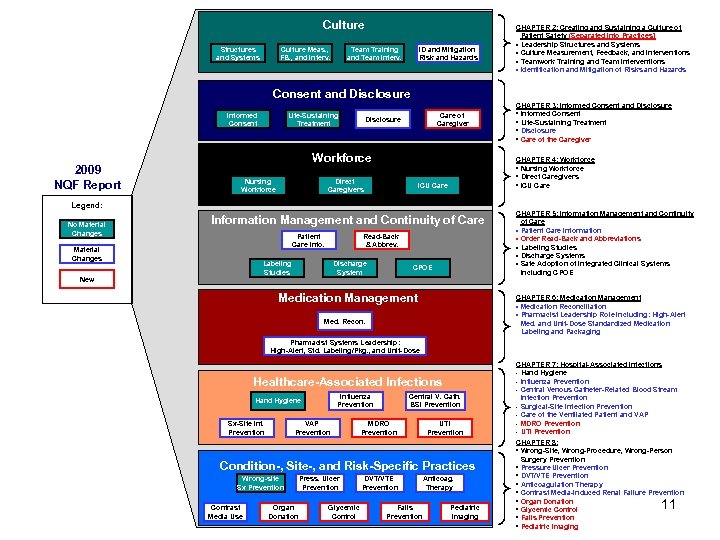
Culture Structures and Systems Culture Meas. , FB. , and Interv. Team Training and Team Interv. ID and Mitigation Risk and Hazards CHAPTER 2: Creating and Sustaining a Culture of Patient Safety (Separated into Practices] § Leadership Structures and Systems § Culture Measurement, Feedback, and Interventions § Teamwork Training and Team Interventions § Identification and Mitigation of Risks and Hazards Consent & Consent and Disclosure Informed Consent 2009 NQF Report Life-Sustaining Treatment Care of Caregiver Disclosure Workforce Nursing Workforce Direct Caregivers CHAPTER 3: Informed Consent and Disclosure • Informed Consent • Life-Sustaining Treatment • Disclosure • Care of the Caregiver CHAPTER 4: Workforce • Nursing Workforce • Direct Caregivers • ICU Care Legend: No Material Changes Information Management and Continuity of Care Patient Care Info. Material Changes Read-Back & Abbrev. Labeling Studies New Discharge System CPOE Medication Management CHAPTER 5: Information Management and Continuity of Care § Patient Care Information § Order Read-Back and Abbreviations § Labeling Studies § Discharge Systems § Safe Adoption of Integrated Clinical Systems including CPOE CHAPTER 6: Medication Management § Medication Reconciliation § Pharmacist Leadership Role Including: High-Alert Med. and Unit-Dose Standardized Medication Labeling and Packaging Med. Recon. Pharmacist Systems Leadership: High-Alert, Std. Labeling/Pkg. , and Unit-Dose Healthcare-Associated Infections Influenza Prevention Hand Hygiene Sx-Site Inf. Prevention VAP Prevention Central V. Cath. BSI Prevention MDRO Prevention UTI Prevention Condition-, Site-, and Risk-Specific Practices Wrong-site Sx Prevention Contrast Media Use Organ Donation Press. Ulcer Prevention Glycemic Control DVT/VTE Prevention Anticoag. Therapy Falls Prevention Pediatric Imaging CHAPTER 7: Hospital-Associated Infections • Hand Hygiene • Influenza Prevention • Central Venous Catheter-Related Blood Stream Infection Prevention • Surgical-Site Infection Prevention • Care of the Ventilated Patient and VAP • MDRO Prevention • UTI Prevention CHAPTER 8: • Wrong-Site, Wrong-Procedure, Wrong-Person Surgery Prevention • Pressure Ulcer Prevention • DVT/VTE Prevention • Anticoagulation Therapy • Contrast Media-Induced Renal Failure Prevention • Organ Donation • Glycemic Control • Falls Prevention • Pediatric Imaging 11
Safe Practice Implementation from 30, 000 Feet Charles Denham, MD Chairman, TMIT; Co-chairman, NQF Safe Practices Consensus Committee; Chairman, Leapfrog Safe Practices Program Safe Practices Webinar September 17, 2009 Toll-free Call-in number: 1 -866 -764 -6260 12
© 2009 TMIT 13
14
15
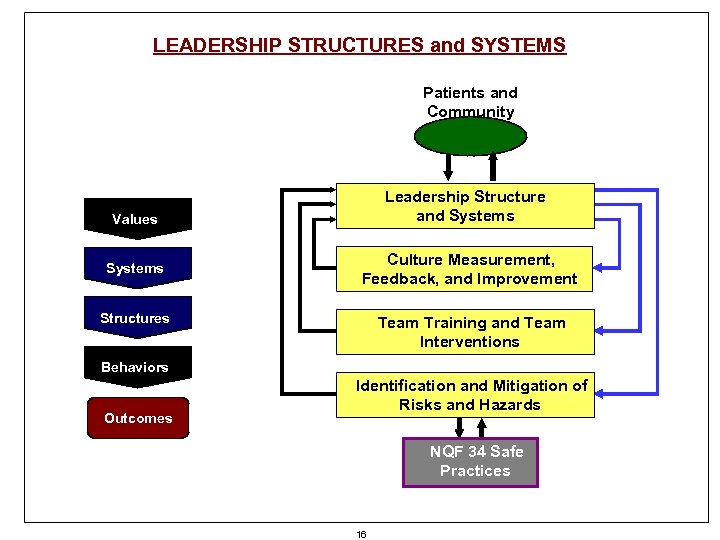
LEADERSHIP STRUCTURES and SYSTEMS Patients and Community Leadership Structure and Systems Values Systems Culture Measurement, Feedback, and Improvement Structures Team Training and Team Interventions Behaviors Outcomes Identification and Mitigation of Risks and Hazards NQF 34 Safe Practices 16
17
Leadership Collaborative 18
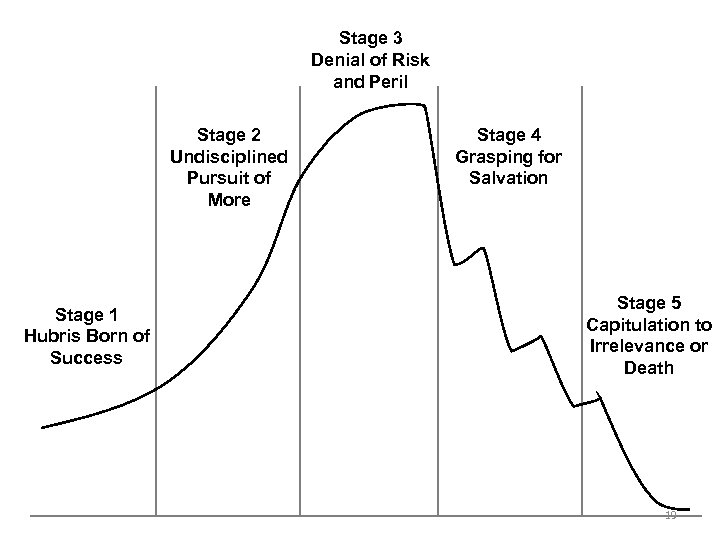
Stage 3 Denial of Risk and Peril Stage 2 Undisciplined Pursuit of More Stage 1 Hubris Born of Success Stage 4 Grasping for Salvation Stage 5 Capitulation to Irrelevance or Death 19
The Power of Stories Chip and Dan Heath © 2008 TMIT © 2006 HCC, Inc. CD 000000 -0000 XX 20 20
21
22
Prioritizing the Focus of Institutional Effort: Developing Short- & Long-Term Priorities in Patient Safety Donald Kennerly, MD, Ph. D Vice President of Patient Safety; Chief Patient Safety Officer, Baylor Health Care System Toll-free Call-in number: 1 -866 -764 -6260 Safe Practices Webinar September 17, 2009 23
Overview • Organizational overview/biases • Conceptual framework • Structural initiatives • Selecting improvement targets to: – Reduce risk-adjusted inpatient mortality – Reduce patient injury from adverse events • Balance: culture vs. processes vs. HIT Toll-free Call-in number: 1 -866 -764 -6260 24
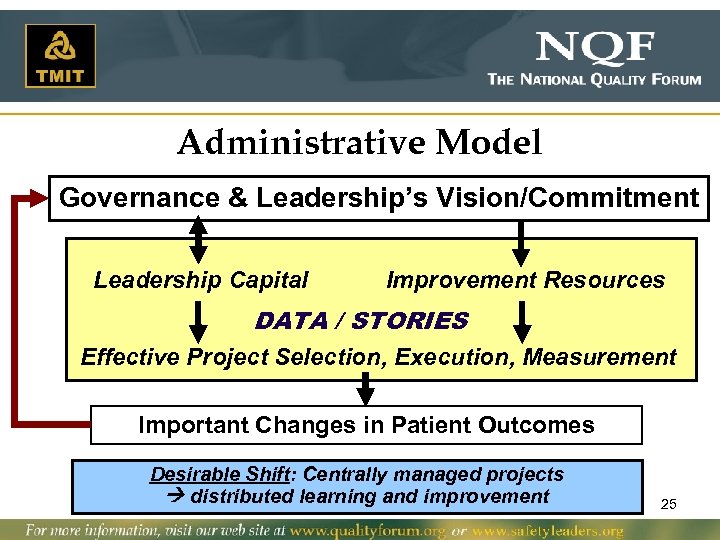
Administrative Model Governance & Leadership’s Vision/Commitment Leadership Capital Improvement Resources DATA / STORIES Effective Project Selection, Execution, Measurement Important Changes in Patient Outcomes Desirable Shift: Centrally managed projects distributed learning and improvement 25
Organizational Snapshot • Integrated health system in north Texas • Component entities – 9 acute care hospitals in DFW metroplex – 2 specialty heart hospitals – 1 rehab hospital/2 LTACs – 105 primary and specialty care centers (450 employed physicians in BHCS’s PHO, Health. Texas) • 18, 000+ employees; 3, 000+ affiliated physicians • ~125, 000 inpatient admissions annually • >$4 B net operating revenue (FY 09) • Early/mid level of clinical integration 26
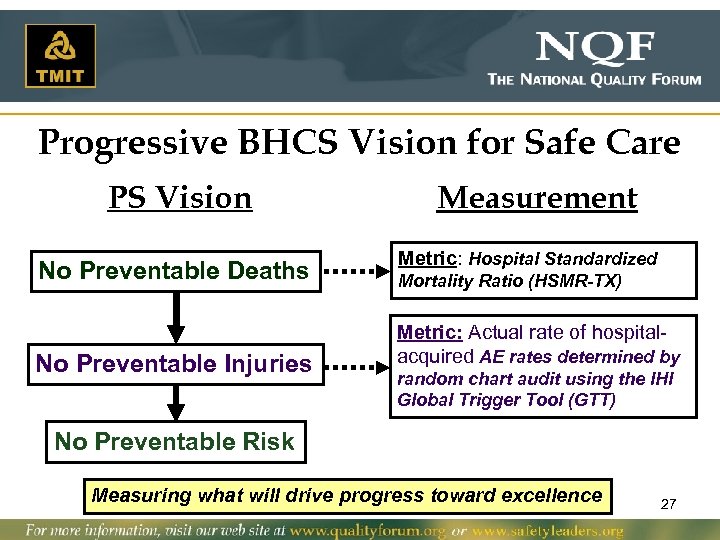
Progressive BHCS Vision for Safe Care PS Vision No Preventable Deaths No Preventable Injuries Measurement Metric: Hospital Standardized Mortality Ratio (HSMR-TX) Metric: Actual rate of hospitalacquired AE rates determined by random chart audit using the IHI Global Trigger Tool (GTT) No Preventable Risk Measuring what will drive progress toward excellence 27
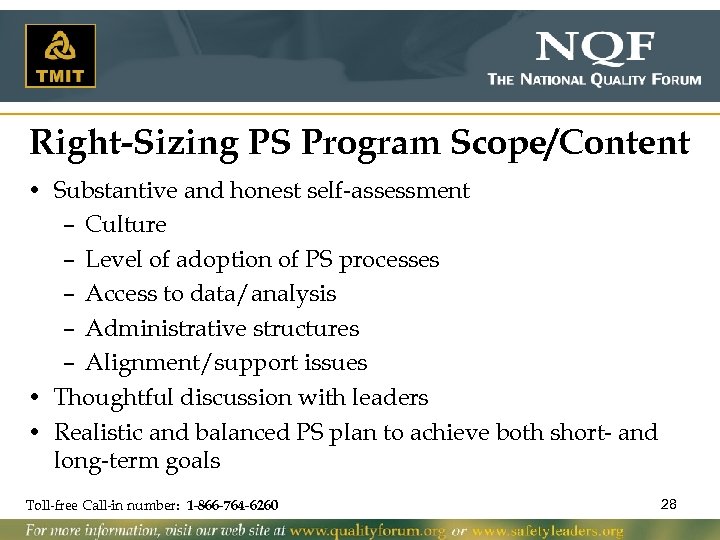
Right-Sizing PS Program Scope/Content • Substantive and honest self-assessment – Culture – Level of adoption of PS processes – Access to data/analysis – Administrative structures – Alignment/support issues • Thoughtful discussion with leaders • Realistic and balanced PS plan to achieve both short- and long-term goals Toll-free Call-in number: 1 -866 -764 -6260 28
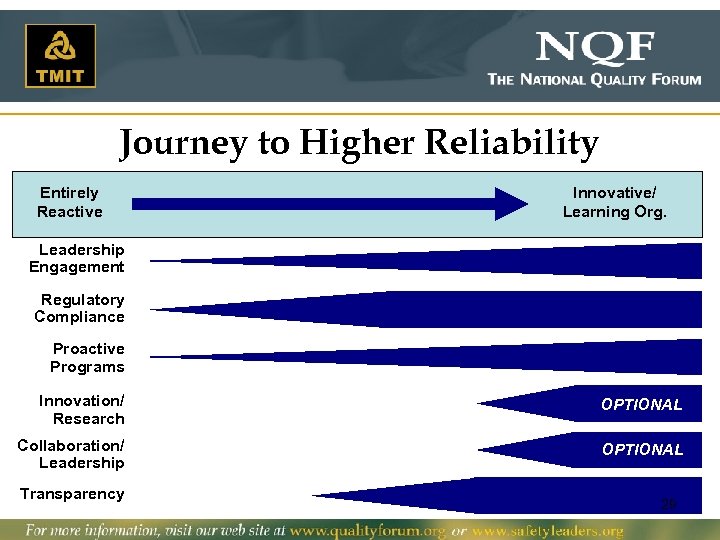
Journey to Higher Reliability Entirely Reactive Innovative/ Learning Org. Leadership Engagement Regulatory Compliance Proactive Programs Innovation/ Research OPTIONAL Collaboration/ Leadership OPTIONAL Transparency 29
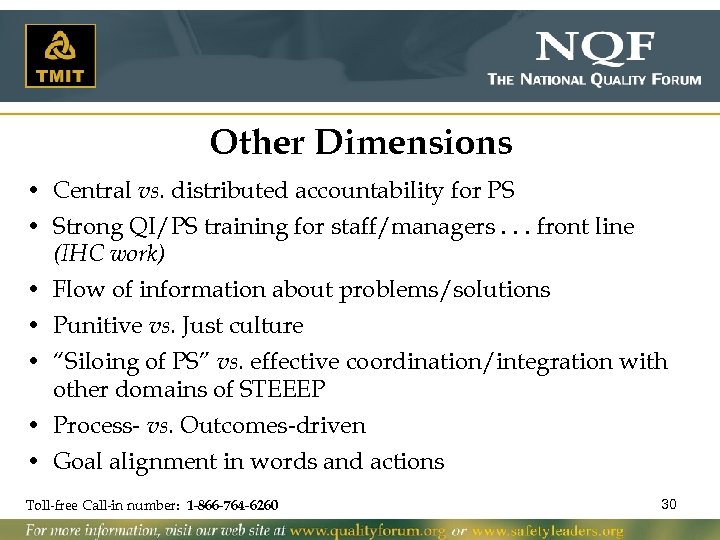
Other Dimensions • Central vs. distributed accountability for PS • Strong QI/PS training for staff/managers. . . front line (IHC work) • Flow of information about problems/solutions • Punitive vs. Just culture • “Siloing of PS” vs. effective coordination/integration with other domains of STEEEP • Process- vs. Outcomes-driven • Goal alignment in words and actions Toll-free Call-in number: 1 -866 -764 -6260 30
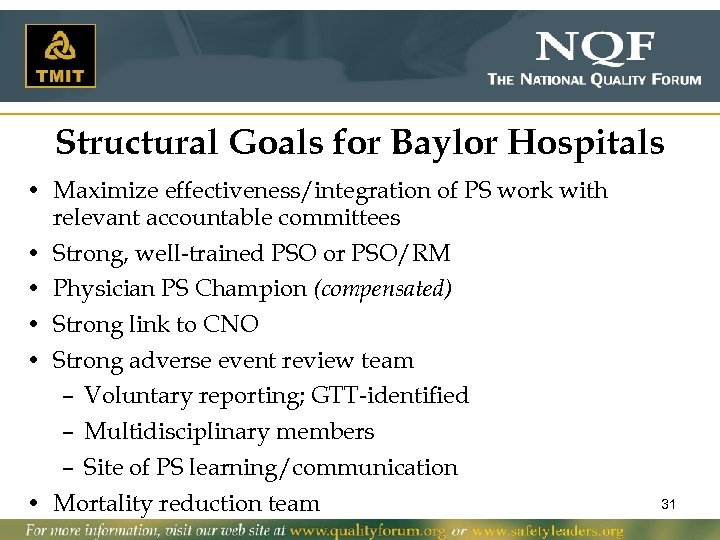
Structural Goals for Baylor Hospitals • Maximize effectiveness/integration of PS work with relevant accountable committees • Strong, well-trained PSO or PSO/RM • Physician PS Champion (compensated) • Strong link to CNO • Strong adverse event review team – Voluntary reporting; GTT-identified – Multidisciplinary members – Site of PS learning/communication • Mortality reduction team 31
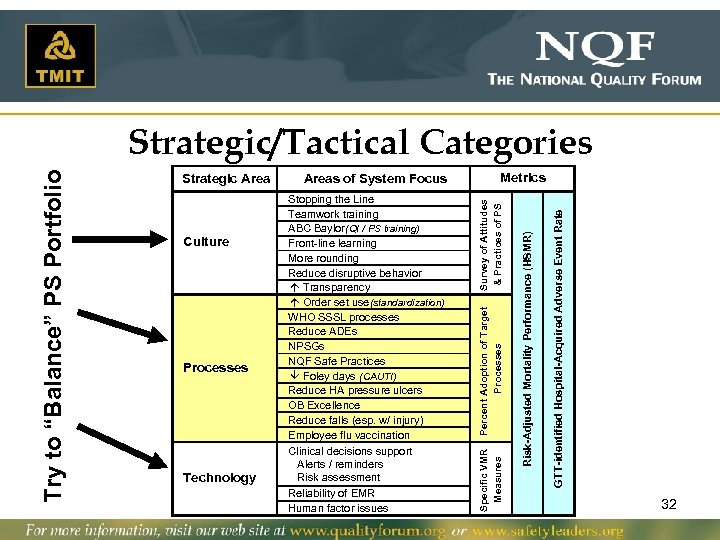
GTT-identified Hospital-Acquired Adverse Event Rate Technology Risk-Adjusted Mortality Performance (HSMR) Processes Stopping the Line Teamwork training ABC Baylor (QI / PS training) Front-line learning More rounding Reduce disruptive behavior á Transparency á Order set use (standardization) WHO SSSL processes Reduce ADEs NPSGs NQF Safe Practices â Foley days (CAUTI) Reduce HA pressure ulcers OB Excellence Reduce falls (esp. w/ injury) Employee flu vaccination Clinical decisions support Alerts / reminders Risk assessment Reliability of EMR Human factor issues Metrics Survey of Attitudes & Practices of PS Culture Areas of System Focus Percent Adoption of Target Processes Strategic Area Specific VMR Measures Try to “Balance” PS Portfolio Strategic/Tactical Categories 32
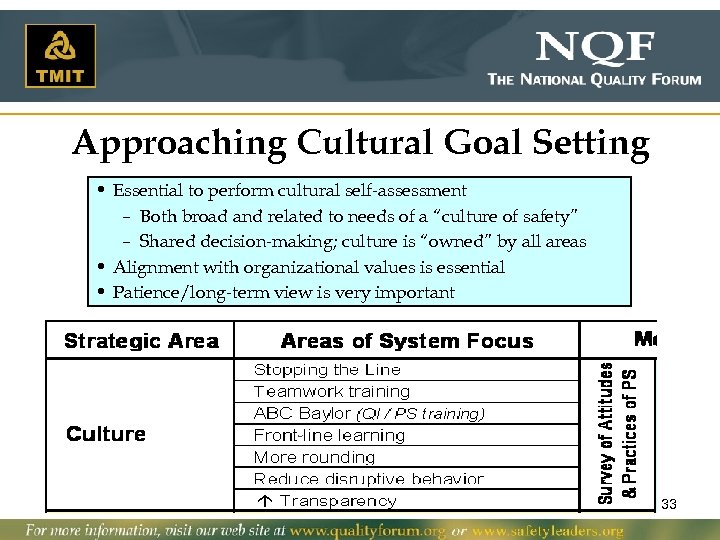
Approaching Cultural Goal Setting • Essential to perform cultural self-assessment – Both broad and related to needs of a “culture of safety” – Shared decision-making; culture is “owned” by all areas • Alignment with organizational values is essential • Patience/long-term view is very important - 33
Approaching Goal Setting for PS Processes • Alignment with regulators/payers (both now and in future) • Alignment with other existing and/or planned programs • Amount of “leadership capital” needed . 34
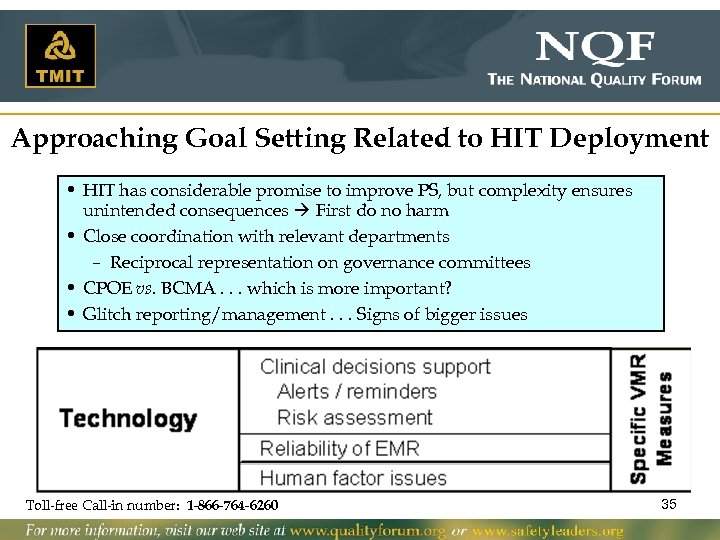
Approaching Goal Setting Related to HIT Deployment • HIT has considerable promise to improve PS, but complexity ensures unintended consequences First do no harm • Close coordination with relevant departments – Reciprocal representation on governance committees • CPOE vs. BCMA. . . which is more important? • Glitch reporting/management. . . Signs of bigger issues Toll-free Call-in number: 1 -866 -764 -6260 35
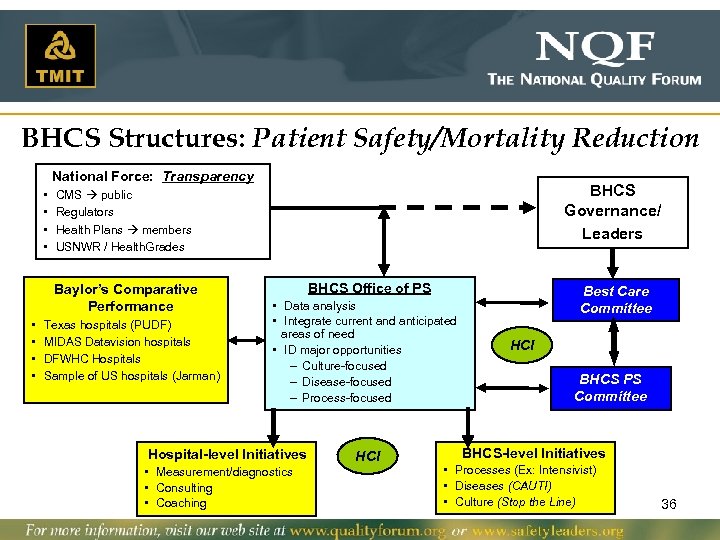
BHCS Structures: Patient Safety/Mortality Reduction National Force: Transparency • • Baylor’s Comparative Performance • • BHCS Governance/ Leaders CMS public Regulators Health Plans members USNWR / Health. Grades Texas hospitals (PUDF) MIDAS Datavision hospitals DFWHC Hospitals Sample of US hospitals (Jarman) BHCS Office of PS • Data analysis • Integrate current and anticipated areas of need • ID major opportunities – Culture-focused – Disease-focused – Process-focused Hospital-level Initiatives • Measurement/diagnostics • Consulting • Coaching HCI Best Care Committee HCI BHCS PS Committee BHCS-level Initiatives • Processes (Ex: Intensivist) • Diseases (CAUTI) • Culture (Stop the Line) 36
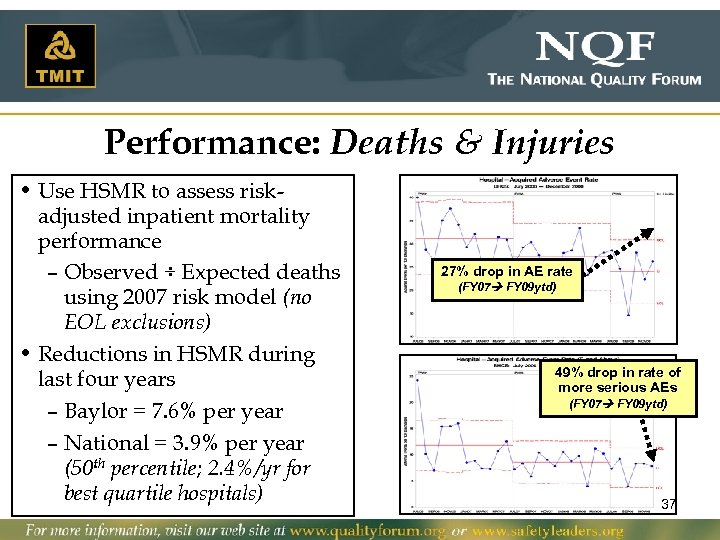
Performance: Deaths & Injuries • Use HSMR to assess riskadjusted inpatient mortality performance – Observed ÷ Expected deaths using 2007 risk model (no EOL exclusions) • Reductions in HSMR during last four years – Baylor = 7. 6% per year – National = 3. 9% per year (50 th percentile; 2. 4%/yr for best quartile hospitals) 27% drop in AE rate (FY 07 FY 09 ytd) 49% drop in rate of more serious AEs (FY 07 FY 09 ytd) 37
Processes for Today ü Wrong-site/-procedure/-person surgery ü Pressure ulcer prevention ü VTE prophylaxis ü Anticoagulation therapy ü Contrast media-induced renal injury q Organ donation ü Glycemic control ü Falls prevention q Pediatric imaging Toll-free Call-in number: 1 -866 -764 -6260 38
Correct Site Surgery – It Becomes More Than Just the OR Donald W. Moorman, M. D. Associate Professor of Surgery, Harvard Medical School; Associate Surgeon-in-Chief, Beth Israel Deaconess Medical Center Toll-free Call-in number: 1 -866 -764 -6260 Safe Practices Webinar September 17, 2009 39
Building More Effective and Safe Teams in Surgery Donald W. Moorman, MD Associate Professor of Surgery, Harvard Medical School; Associate Surgeon-in-Chief, Beth Israel Deaconess Medical Center Toll-free Call-in number: 1 -866 -764 -6260 40
Beth Israel Deaconess Medical Center 41
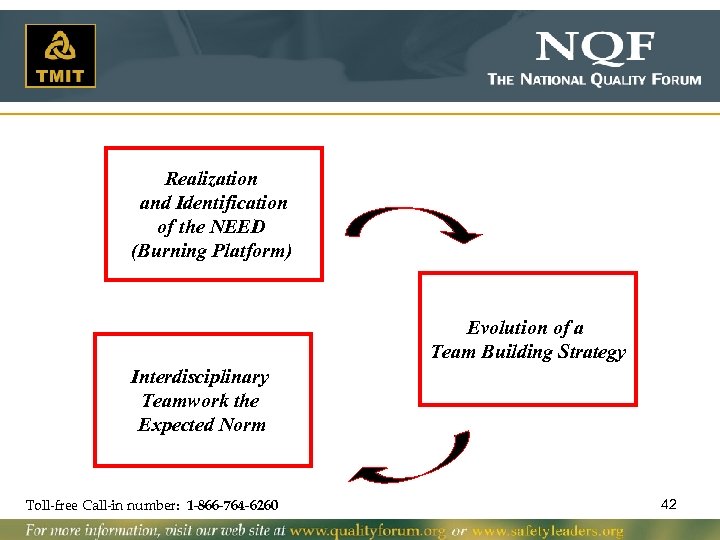
Realization and Identification of the NEED (Burning Platform) Evolution of a Team Building Strategy Interdisciplinary Teamwork the Expected Norm Toll-free Call-in number: 1 -866 -764 -6260 42
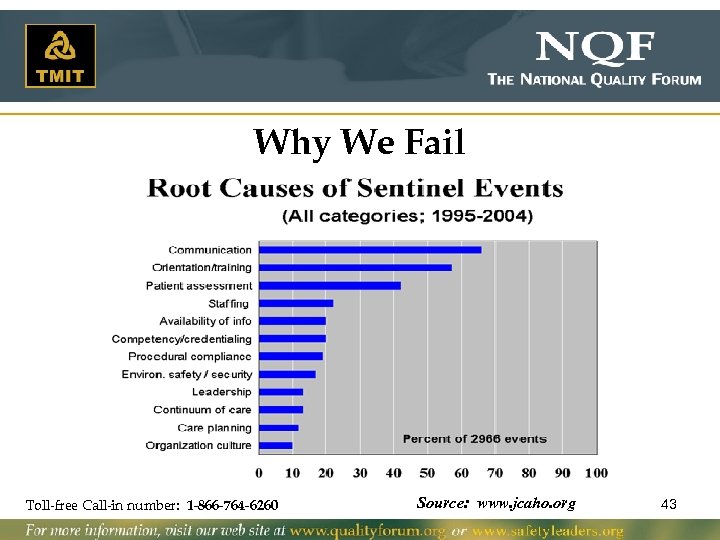
Why We Fail Toll-free Call-in number: 1 -866 -764 -6260 Source: www. jcaho. org 43
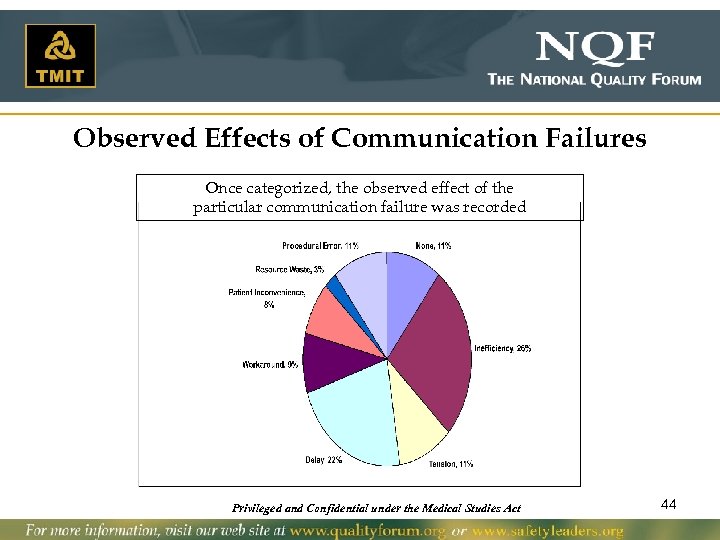
Observed Effects of Communication Failures Once categorized, the observed effect of the particular communication failure was recorded Privileged and Confidential under the Medical Studies Act 44
TEAM DYNAMICS in SURGERY Beth Israel Deaconess Surgical Safety Team And Harvard Risk Management Foundation Copyright: Donald W. Moorman, M. D. and BIDMC Surgery, 2004 45
Team Dynamics 5 Modules • Why Teams: Define and understand how and why teams function • Error Science, Error Sources, Shared MENTAL MODELS and Just Accountability • COMMUNICATION: – Realizing the expectations – Understanding the difficulty – Techniques for preventing miscommunication and misunderstanding • Maintaining Situational Awareness, and Work Load, Stress and FATIGUE management • Improving our personal performance on teams Toll-free Call-in number: 1 -866 -764 -6260 46
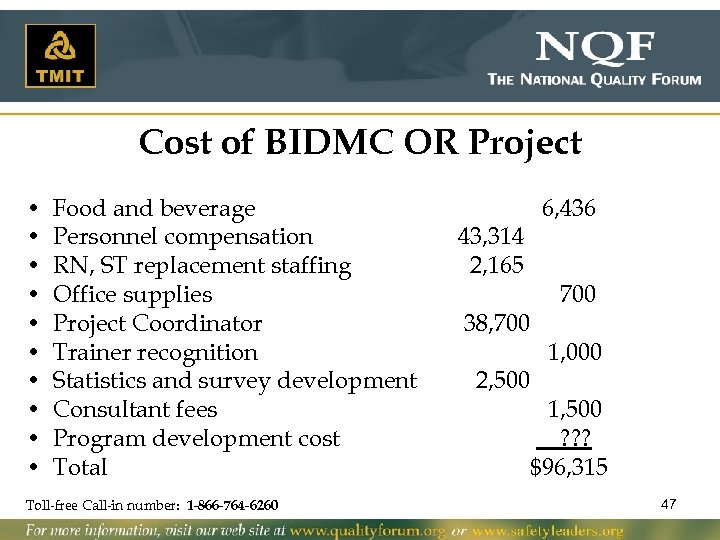
Cost of BIDMC OR Project • • • Food and beverage Personnel compensation RN, ST replacement staffing Office supplies Project Coordinator Trainer recognition Statistics and survey development Consultant fees Program development cost Total Toll-free Call-in number: 1 -866 -764 -6260 43, 314 2, 165 6, 436 38, 700 2, 500 1, 000 1, 500 ? ? ? $96, 315 47
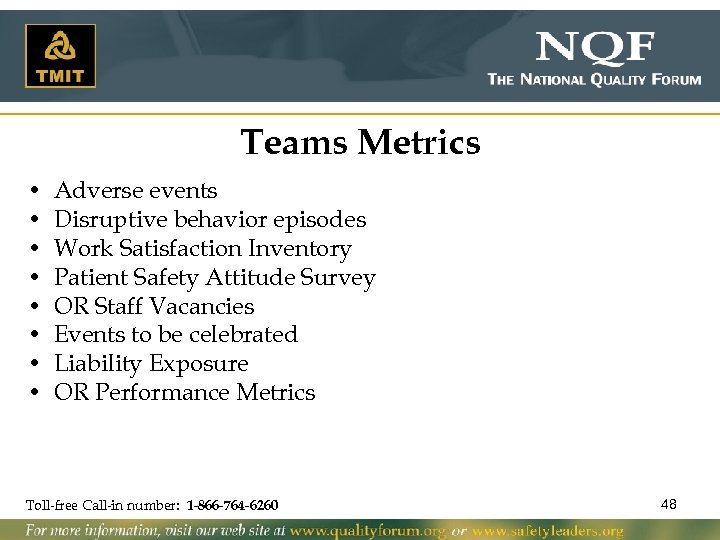
Teams Metrics • • Adverse events Disruptive behavior episodes Work Satisfaction Inventory Patient Safety Attitude Survey OR Staff Vacancies Events to be celebrated Liability Exposure OR Performance Metrics Toll-free Call-in number: 1 -866 -764 -6260 48
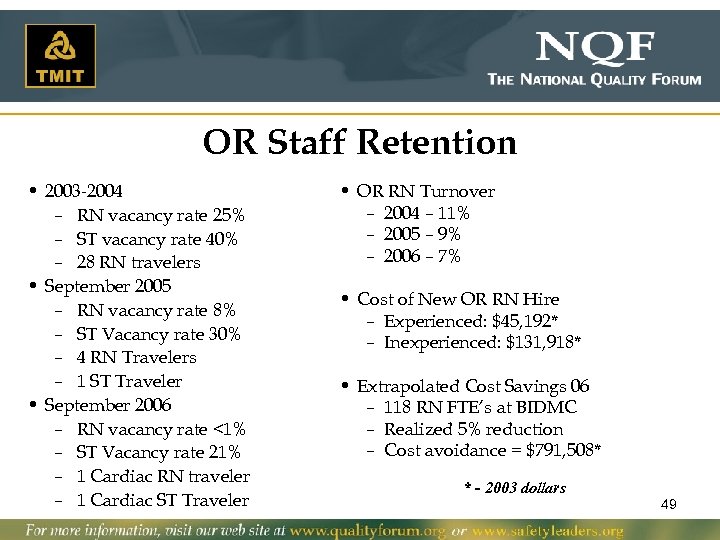
OR Staff Retention • 2003 -2004 – RN vacancy rate 25% – ST vacancy rate 40% – 28 RN travelers • September 2005 – RN vacancy rate 8% – ST Vacancy rate 30% – 4 RN Travelers – 1 ST Traveler • September 2006 – RN vacancy rate <1% – ST Vacancy rate 21% – 1 Cardiac RN traveler – 1 Cardiac ST Traveler • OR RN Turnover – 2004 – 11% – 2005 – 9% – 2006 – 7% • Cost of New OR RN Hire – Experienced: $45, 192* – Inexperienced: $131, 918* • Extrapolated Cost Savings 06 – 118 RN FTE’s at BIDMC – Realized 5% reduction – Cost avoidance = $791, 508* * - 2003 dollars 49
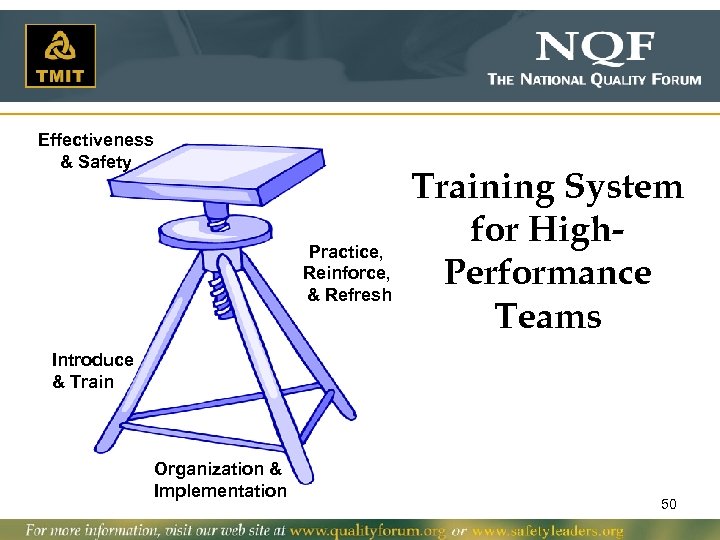
Effectiveness & Safety Practice, Reinforce, & Refresh Training System for High. Performance Teams Introduce & Train Organization & Implementation 50
Can Team Paradigm Extend Beyond the OR? Toll-free Call-in number: 1 -866 -764 -6260 51
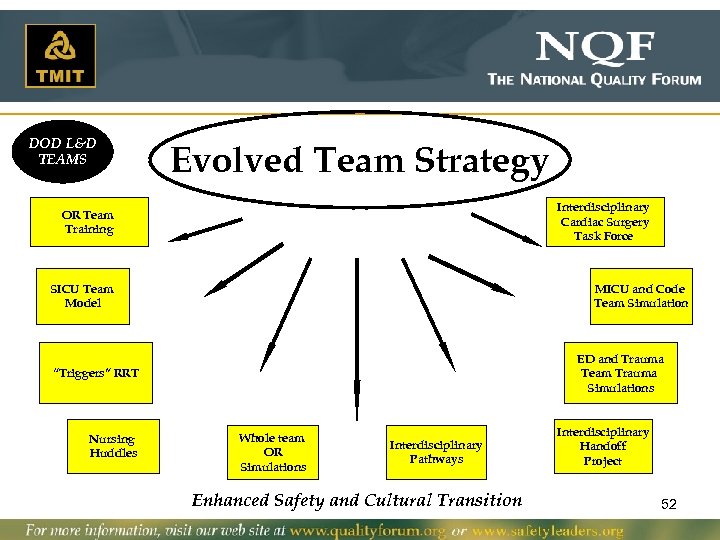
DOD L&D TEAMS Evolved Team Strategy Interdisciplinary Cardiac Surgery Task Force OR Team Training SICU Team Model MICU and Code Team Simulation ED and Trauma Team Trauma Simulations “Triggers” RRT Nursing Huddles Whole team OR Simulations Interdisciplinary Pathways Enhanced Safety and Cultural Transition Interdisciplinary Handoff Project 52
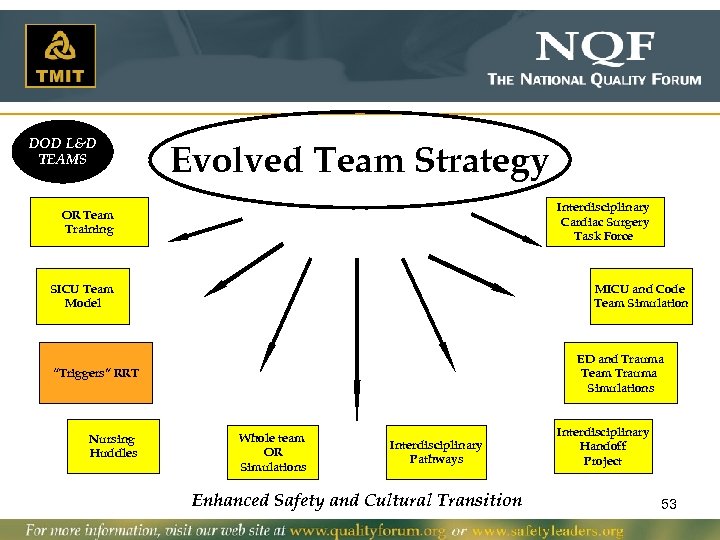
DOD L&D TEAMS Evolved Team Strategy Interdisciplinary Cardiac Surgery Task Force OR Team Training SICU Team Model MICU and Code Team Simulation ED and Trauma Team Trauma Simulations “Triggers” RRT Nursing Huddles Whole team OR Simulations Interdisciplinary Pathways Interdisciplinary Handoff Project Enhanced Safety and Cultural Transition 53
54
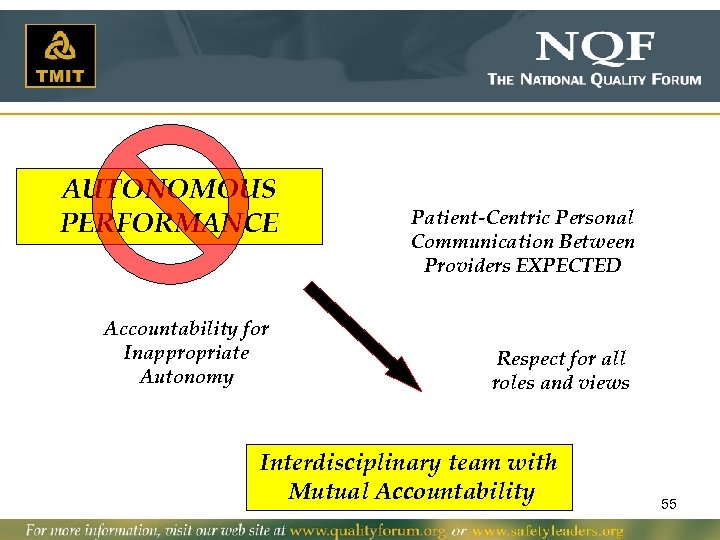
AUTONOMOUS PERFORMANCE Accountability for Inappropriate Autonomy Patient-Centric Personal Communication Between Providers EXPECTED Respect for all roles and views Interdisciplinary team with Mutual Accountability 55
“Many are stubborn in the pursuit of the path they have chosen, few in pursuit of the goal. ” Friedrich Nietzsche Toll-free Call-in number: 1 -866 -764 -6260 56
Did you guys hear… WE had a WRONG-SITE SURGERY at BIDMC! And we learned a lot! Toll-free Call-in number: 1 -866 -764 -6260 57
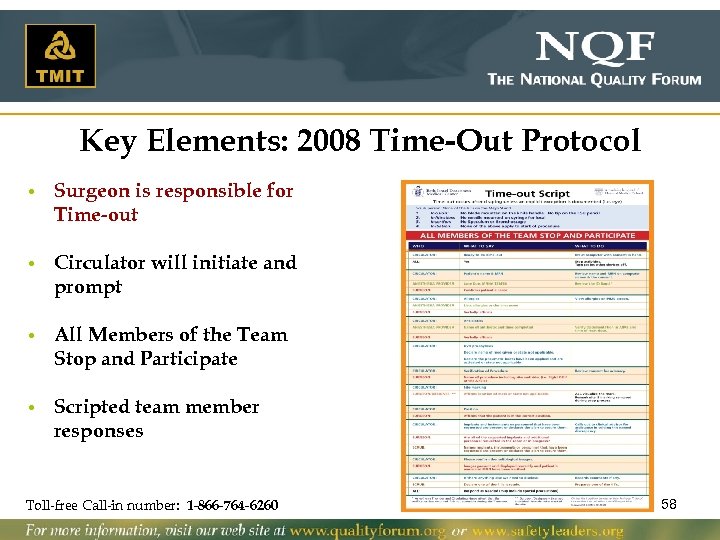
Key Elements: 2008 Time-Out Protocol • Surgeon is responsible for Time-out • Circulator will initiate and prompt • All Members of the Team Stop and Participate • Scripted team member responses Toll-free Call-in number: 1 -866 -764 -6260 58
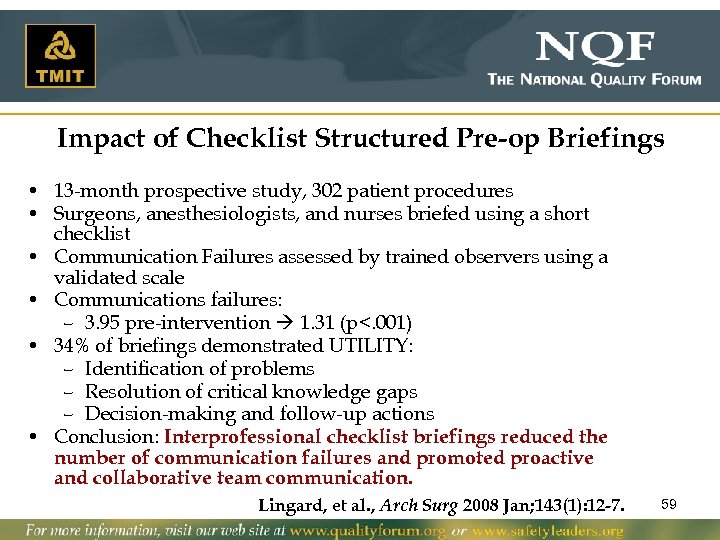
Impact of Checklist Structured Pre-op Briefings • 13 -month prospective study, 302 patient procedures • Surgeons, anesthesiologists, and nurses briefed using a short checklist • Communication Failures assessed by trained observers using a validated scale • Communications failures: – 3. 95 pre-intervention 1. 31 (p<. 001) • 34% of briefings demonstrated UTILITY: – Identification of problems – Resolution of critical knowledge gaps – Decision-making and follow-up actions • Conclusion: Interprofessional checklist briefings reduced the number of communication failures and promoted proactive and collaborative team communication. Lingard, et al. , Arch Surg 2008 Jan; 143(1): 12 -7. 59
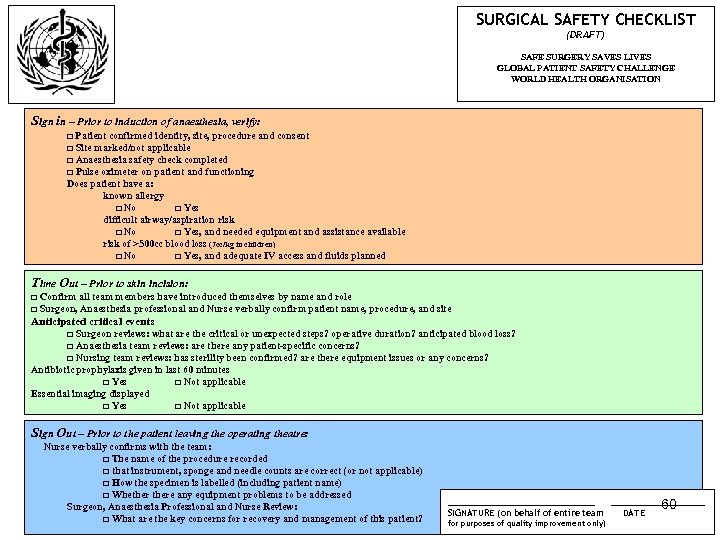
SURGICAL SAFETY CHECKLIST (DRAFT) SAFE SURGERY SAVES LIVES GLOBAL PATIENT SAFETY CHALLENGE WORLD HEALTH ORGANISATION Sign in – Prior to induction of anaesthesia, verify: □ Patient confirmed identity, site, procedure and consent □ Site marked/not applicable □ Anaesthesia safety check completed □ Pulse oximeter on patient and functioning Does patient have a: known allergy □ No □ Yes difficult airway/aspiration risk □ No □ Yes, and needed equipment and assistance available risk of >500 cc blood loss (7 cc/kg in children) □ No □ Yes, and adequate IV access and fluids planned Time Out – Prior to skin incision: □ Confirm all team members have introduced themselves by name and role □ Surgeon, Anaesthesia professional and Nurse verbally confirm patient name, procedure, and site Anticipated critical events □ Surgeon reviews: what are the critical or unexpected steps? operative duration? anticipated blood loss? □ Anaesthesia team reviews: are there any patient-specific concerns? □ Nursing team reviews: has sterility been confirmed? are there equipment issues or any concerns? Antibiotic prophylaxis given in last 60 minutes □ Yes □ Not applicable Essential imaging displayed □ Yes □ Not applicable Sign Out – Prior to the patient leaving the operating theatre: Nurse verbally confirms with the team: □ The name of the procedure recorded □ that instrument, sponge and needle counts are correct (or not applicable) □ How the specimen is labelled (including patient name) □ Whethere any equipment problems to be addressed Surgeon, Anaesthesia Professional and Nurse Review: □ What are the key concerns for recovery and management of this patient? ___________ SIGNATURE (on behalf of entire team for purposes of quality improvement only) _______ 60 DATE
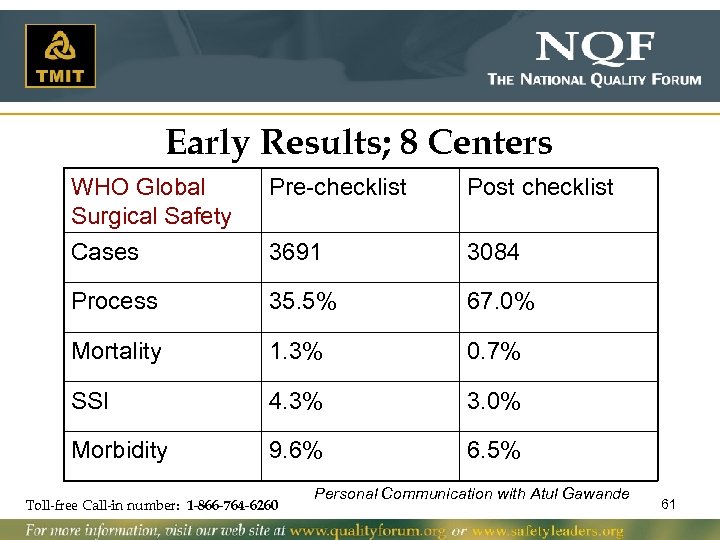
Early Results; 8 Centers WHO Global Surgical Safety Pre-checklist Post checklist Cases 3691 3084 Process 35. 5% 67. 0% Mortality 1. 3% 0. 7% SSI 4. 3% 3. 0% Morbidity 9. 6% 6. 5% Toll-free Call-in number: 1 -866 -764 -6260 Personal Communication with Atul Gawande 61
Team-based practice (K. Robert’s “heedful interrelating”) Toll-free Call-in number: 1 -866 -764 -6260 Courtesy of Concord Hospital Cardiac Care Team 62
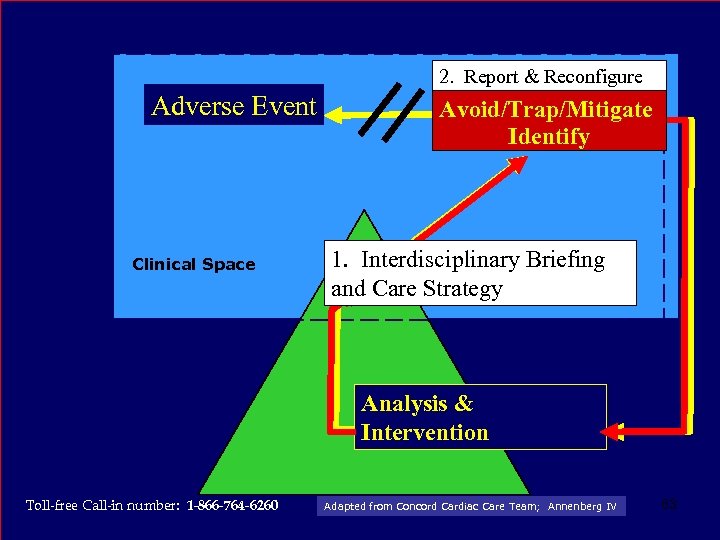
2. Report & Reconfigure Adverse Event Clinical Space Avoid/Trap/Mitigate Active Failure Identify 1. Interdisciplinary Briefing Provider and Care Strategy Analysis & Latent Failure Intervention Conditions Toll-free Call-in number: 1 -866 -764 -6260 Adapted from Concord Cardiac Care Team; Annenberg IV 63
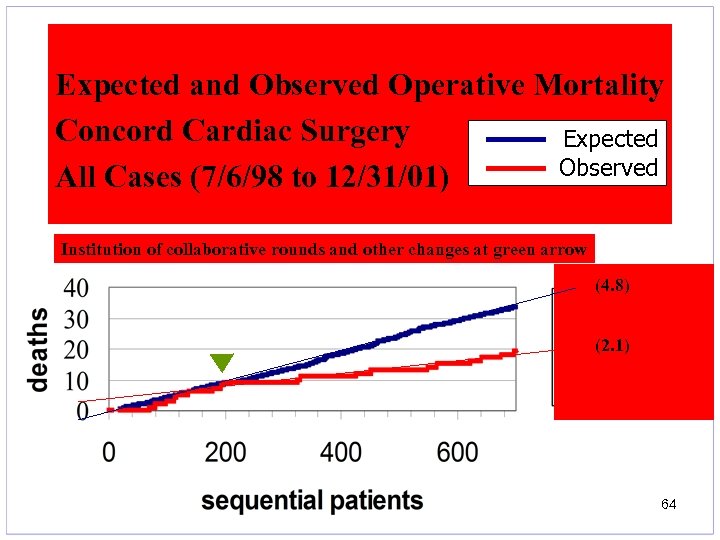
Expected and Observed Operative Mortality Concord Cardiac Surgery Expected Observed All Cases (7/6/98 to 12/31/01) Institution of collaborative rounds and other changes at green arrow (4. 8) (2. 1) 64
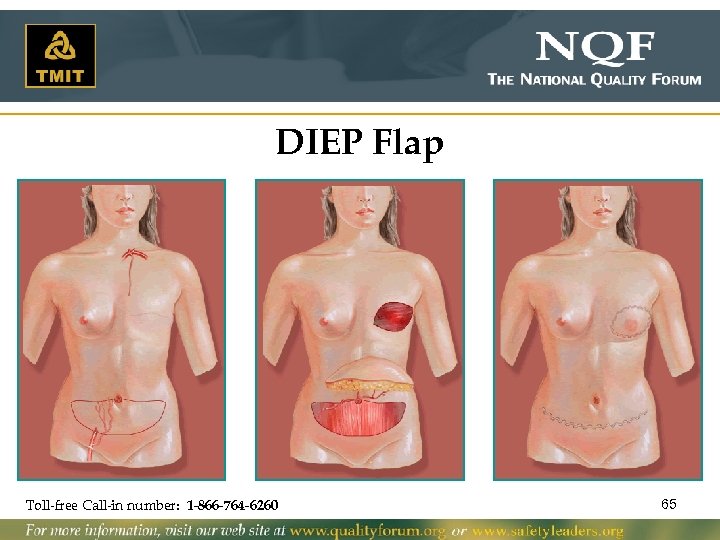
DIEP Flap Toll-free Call-in number: 1 -866 -764 -6260 65
Intra-operative Pathway Characteristics which Enhance Patient Safety • • • Effective coordination of multiple teams or fields Segmentation and standardization Structured communication Effective Hand-offs Management of task saturation and fatigue Toll-free Call-in number: 1 -866 -764 -6260 66
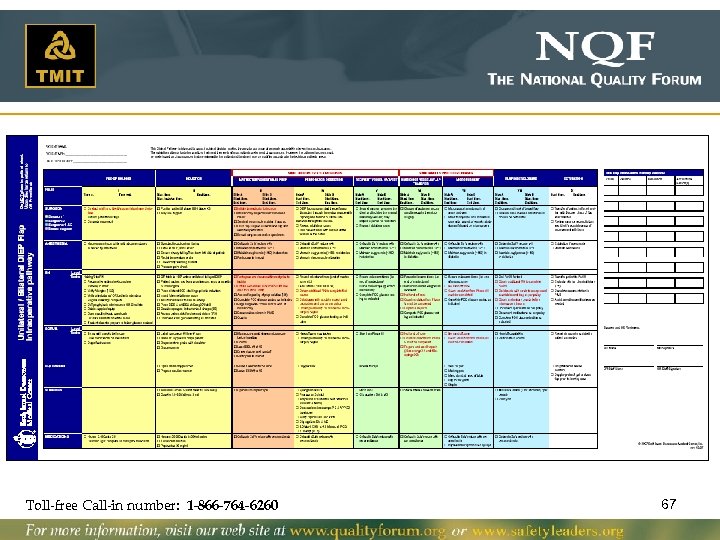
Toll-free Call-in number: 1 -866 -764 -6260 67
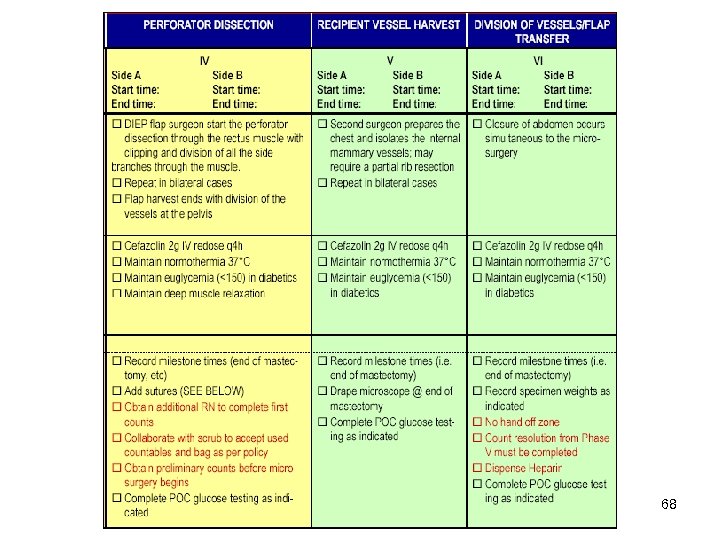
68
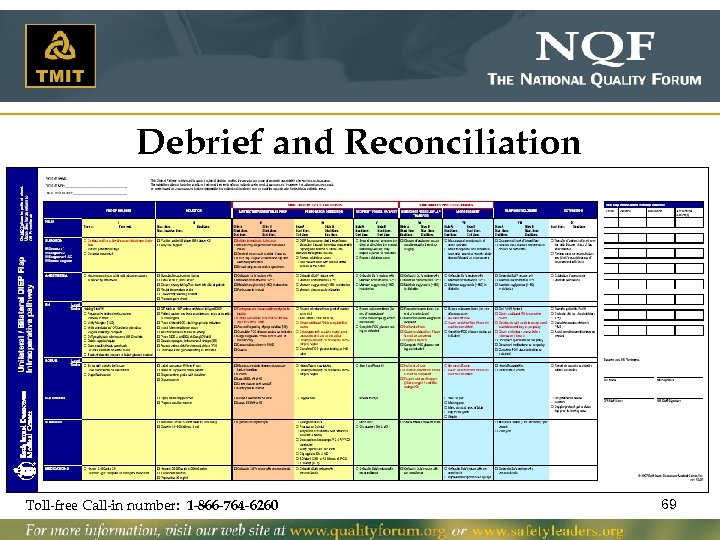
Debrief and Reconciliation Toll-free Call-in number: 1 -866 -764 -6260 69
The Early Results • 150 patients from 2005 to 2008 • Comparison Groups – Pre-pathway • 50 unilateral reconstructions • 50 bilateral reconstructions – Post-pathway • 25 unilateral reconstructions • 25 bilateral reconstructions Toll-free Call-in number: 1 -866 -764 -6260 70
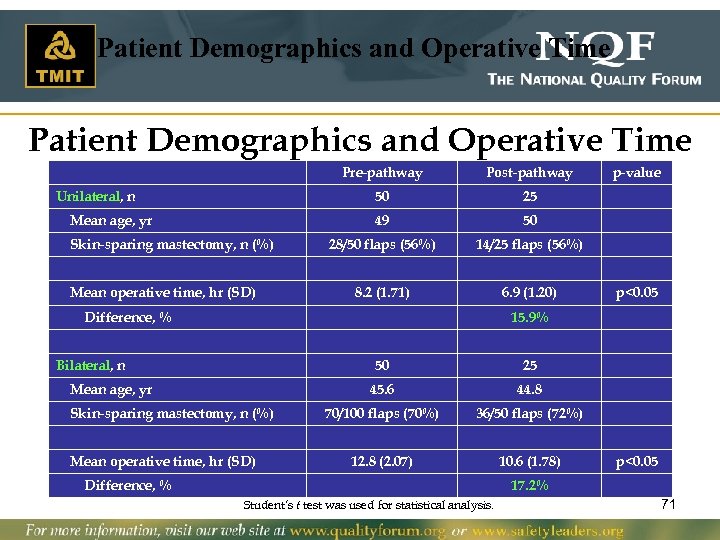
Patient Demographics and Operative Time Pre-pathway 50 Mean age, yr Skin-sparing mastectomy, n (%) Mean operative time, hr (SD) 25 49 Unilateral, n Post-pathway 50 28/50 flaps (56%) 14/25 flaps (56%) 8. 2 (1. 71) 6. 9 (1. 20) Difference, % p-value p<0. 05 15. 9% Bilateral, n 50 45. 6 Mean age, yr Skin-sparing mastectomy, n (%) Mean operative time, hr (SD) 25 44. 8 70/100 flaps (70%) 36/50 flaps (72%) 12. 8 (2. 07) 10. 6 (1. 78) Difference, % p<0. 05 17. 2% Student’s t test was used for statistical analysis. 71
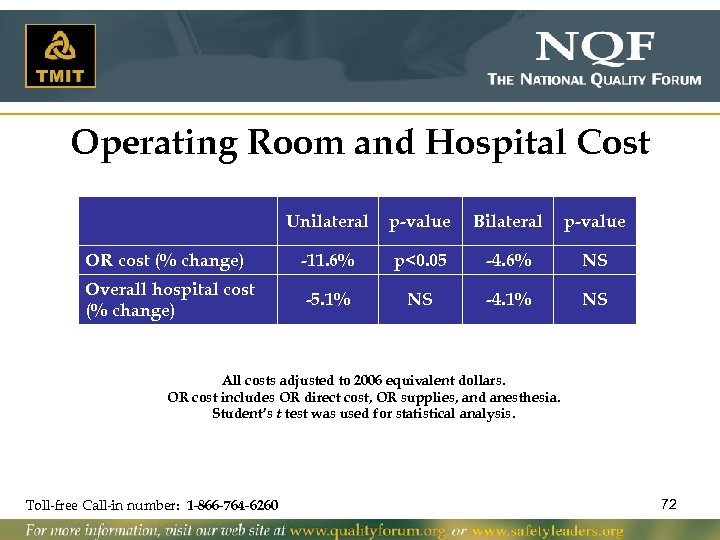
Operating Room and Hospital Cost Unilateral p-value Bilateral p-value OR cost (% change) -11. 6% p<0. 05 -4. 6% NS Overall hospital cost (% change) -5. 1% NS -4. 1% NS All costs adjusted to 2006 equivalent dollars. OR cost includes OR direct cost, OR supplies, and anesthesia. Student’s t test was used for statistical analysis. Toll-free Call-in number: 1 -866 -764 -6260 72
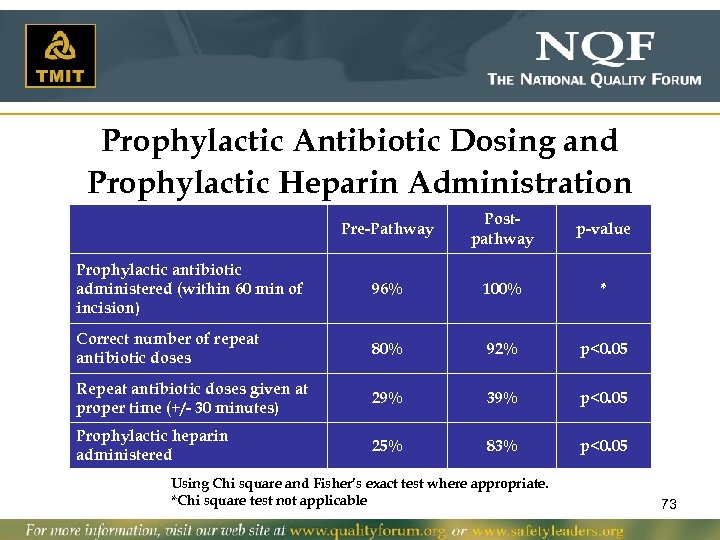
Prophylactic Antibiotic Dosing and Prophylactic Heparin Administration Pre-Pathway Postpathway p-value Prophylactic antibiotic administered (within 60 min of incision) 96% 100% * Correct number of repeat antibiotic doses 80% 92% p<0. 05 Repeat antibiotic doses given at proper time (+/- 30 minutes) 29% 39% p<0. 05 Prophylactic heparin administered 25% 83% p<0. 05 Using Chi square and Fisher’s exact test where appropriate. *Chi square test not applicable 73
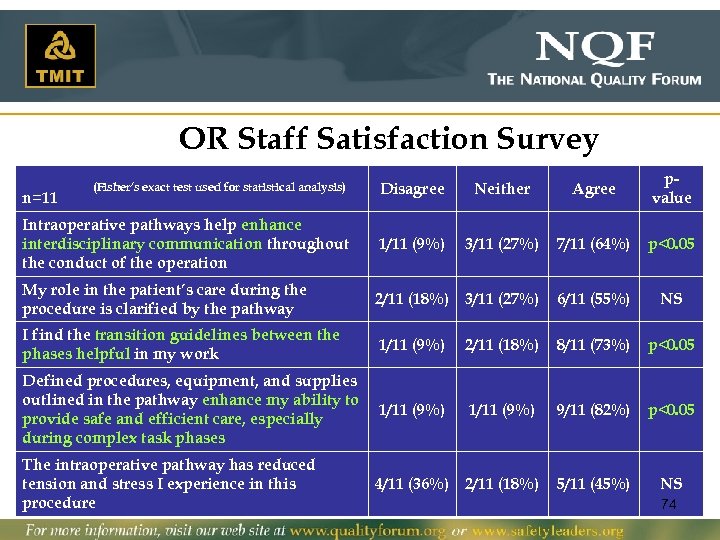
OR Staff Satisfaction Survey (Fisher’s exact test used for statistical analysis) Disagree Neither Agree pvalue Intraoperative pathways help enhance interdisciplinary communication throughout the conduct of the operation 1/11 (9%) 3/11 (27%) 7/11 (64%) p<0. 05 My role in the patient’s care during the procedure is clarified by the pathway 2/11 (18%) 3/11 (27%) 6/11 (55%) NS I find the transition guidelines between the phases helpful in my work 1/11 (9%) 2/11 (18%) 8/11 (73%) p<0. 05 Defined procedures, equipment, and supplies outlined in the pathway enhance my ability to provide safe and efficient care, especially during complex task phases 1/11 (9%) 9/11 (82%) p<0. 05 The intraoperative pathway has reduced tension and stress I experience in this procedure 4/11 (36%) 2/11 (18%) 5/11 (45%) NS n=11 74
The 5 Conditions for High Reliability Teams • Mutual Monitoring • Back-up Behaviors • Adaptability • Leadership promoting 1, 2, and 3 • Collective orientation of the members Toll-free Call-in number: 1 -866 -764 -6260 75
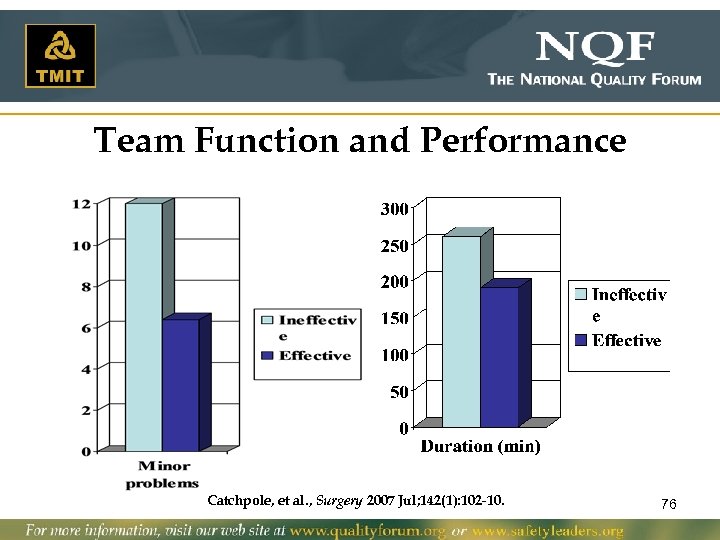
Team Function and Performance Catchpole, et al. , Surgery 2007 Jul; 142(1): 102 -10. 76
Team-Based Practice Strategy • Didactic Team Training – The Tools • Practice: Actions driven by values of effectiveness – Operating room-based whole team simulation – Practice in real time … coaches • Integrating team-based practice into work flow – Structured Communication – Standardization and systematized care process Toll-free Call-in number: 1 -866 -764 -6260 77
Change Requires Energy “Culture does not change because we desire to change it. Culture changes when the organization is transformed; the culture reflects the realities of people working together every day. ” Frances Hesselbein, The Key to Cultural Transformation, Leader to Leader (Spring 1999) Toll-free Call-in number: 1 -866 -764 -6260 78
Patient Perspective on Prioritizing Safety Dan Ford, MBA Vice President, Furst Group Member, Consumers Advancing Patient Safety (CAPS) Safe Practices Webinar September 17, 2009 Toll-free Call-in number: 1 -866 -764 -6260 79
80
Upcoming Safe Practices Webinars v October 22 – Creating Transparency, Openness, and Improved Safety (Safe Practices 5 -8) v November 19 – Healthier Communication and Safe Information Management (Safe Practices 12 -16) v December 17 – Optimizing a Workforce for Optimal Safe Care (Safe Practices 9 -11) 81
956c2b63383a04ff54070fdd118fee6f.ppt