97432138145b6866be90b21dc60ce6a3.ppt
- Количество слайдов: 70

Welcome to CHA’s Catholic Health Strategy Webinar Integrating Services for Seniors – Parish-based Programs May 31, 2011 | Noon – 1: 30 p. m. ET The webinar will start shortly. Thank you for joining us. © 2011 by the Catholic Health Association of the United States
Catholic Health Strategy Webinar: Integrating Services for Seniors – Parish-based Programs Your Presenter for Today’s Program Julie Trocchio is senior director of community benefit and continuing care at the Catholic Health Association of the United States. She is based in CHA's Washington, D. C. , office. Ms. Trocchio carries out programmatic and advocacy activities related to community benefit, tax exemption, environmental sustainability and long-term care. She also is the CHA liaison to the executives of state Catholic health associations and conferences. © 2011 by the Catholic Health Association of the United States May 31, 2011 2
Catholic Health Strategy Webinar: Integrating Services for Seniors – Parish-based Programs Reflection “The foundational ethic of love of neighbor has its basis in both Old and New Testament texts such as Leviticus 19: 18 and Matthew 22: 34 - 40. The injunction to help the poor and needy is not seen as optional, and the Christian’s salvation is predicated on it (1 John 3: 17). Through this personal involvement, the church has a continuing presence in these communities…” From Setting the Agenda: Meditations for the Organization’s Soul By Edgar Stoesz and Rick Stiffney © 2011 by the Catholic Health Association of the United States May 31, 2011 3
Catholic Health Strategy Webinar: Integrating Services for Seniors – Parish-based Programs Your Presenter for Today’s Program Howard Gleckman is the author of Caring for Our Parents: Inspiring Stories of Families Seeking New Solutions to America's Most Urgent Health Care Crisis, published by St. Martin's Press in June 2009. He is a resident fellow at the Urban Institute. He writes a column on longterm care issues for Kaiser Health News and a blog at http: //blog. howardgleckman. com/. He is a member of the Board of Trustees and co-chair of the Medical Quality Committee at Suburban Hospital (Bethesda, Md. ), a unit of Johns Hopkins Medicine. He is also a member of the Board of the Jewish Council for the Aging of Greater Washington and senior advisor to Caring from a Distance, a nonprofit organization that provides Web-based and telephone assistance to longdistance caregivers. A veteran journalist, Mr. Gleckman was senior correspondent in the Washington bureau of Business Week, where he covered health and elder care, as well as tax and budget issues, for nearly 20 years. He was a 2003 National Magazine Award finalist for a series of Business Week articles entitled The Coming Revolution in Health Care. He began the research for Caring for Our Parents as a 2006 -2007 Media Fellow at the Kaiser Family Foundation, and was a 20062008 Visiting Fellow at the Center for Retirement Research at Boston College. © 2011 by the Catholic Health Association of the United States May 31, 2011 4
Catholic Health Strategy Webinar: Integrating Services for Seniors – Parish-based Programs Your Presenter for Today’s Program Gary R. Gunderson, D. Min. , M. Div. , is senior vice president of Health and Welfare Ministries for Methodist Healthcare and the director for the Interfaith Health Program at Rollins School of Public Health at Emory University, focusing on building the capacity of religious institutions to advance health and wholeness. He is the author of several books, including Deeply Woven Roots and Boundary Leaders (Fortress Press, 1997 and 2004), many articles and hundreds of speeches and presentations to religious and science groups. His most recent book, Leading Causes of Life, with Larry Pray, was published in 2006. Gunderson serves on a range of national and international advisory boards. He served on the Institute of Medicine panel examining the role of U. S. voluntary human resources in the expanded response to HIV/AIDS. He is an advisor to the Duke Divinity School Center on Sustaining Pastoral Excellence, the Chicago Theological Seminary Center for Community Transformation and Wesley Seminary’s Doctor of Ministry program. He was the co-chair of the 2006 Congress on Urban Ministry of The Seminary Consortium for Urban Pastoral Education (SCUPE). He continues to serve as faculty for the Department of Global Health of the Rollins School of Public Health and for the Candler School of Theology at Emory University. Gunderson is a commissioned deacon in the United Methodist Church. He is a graduate of Wake Forest University, Candler School of Theology and the Interdenominational Theological Center. © 2011 by the Catholic Health Association of the United States May 31, 2011 5
Catholic Health Strategy Webinar: Integrating Services for Seniors – Parish-based Programs Your Presenter for Today’s Program Rev. Bobby Baker is director of faith & community partnerships at Methodist Le Bonheur Healthcare. He earned a bachelor of science degree in computer science from Jackson State University and completed a master of divinity at Memphis Theological Seminary. Rev. Baker was awarded the distinction of Certified Chaplain by the Association of Professional Chaplains in July 2000. © 2011 by the Catholic Health Association of the United States May 31, 2011 6
Catholic Health Strategy Webinar: Integrating Services for Seniors – Parish-based Programs Your Presenter for Today’s Program Dr. Teresa Cutts is director of research and innovative practice at Methodist Le Bonheur Healthcare. She earned a bachelor of arts degree in psychology, a master of arts degree in clinical psychology and a Ph. D. in clinical psychology from the University of Mississippi. Dr. Cutts currently serves as an Arkwings Board Member, is on the Assisi Foundation Healthcare Advisory Board and Assisi Foundation Healthy Memphis Advisory Board. She holds adjunct privileges at Baptist Memorial Hospital and clinical privileges at the University of Tennessee and Charter Lakeside. She serves as credentialing officer for psychology at Baptist Memorial Hospital and is on the Harbor of Health Advisory Board. © 2011 by the Catholic Health Association of the United States May 31, 2011 7

Integrating Services for Seniors Howard Gleckman The Urban Institute Catholic Health Association Webinar May 31, 2011
“If there is one hallmark, centering idea to achieve better care, better health, and lower cost without harming a single person, it is through integrated care…the awareness of their journey through their lives and through their illness instead of treating them in fragments. ” Donald Berwick Administrator CMS
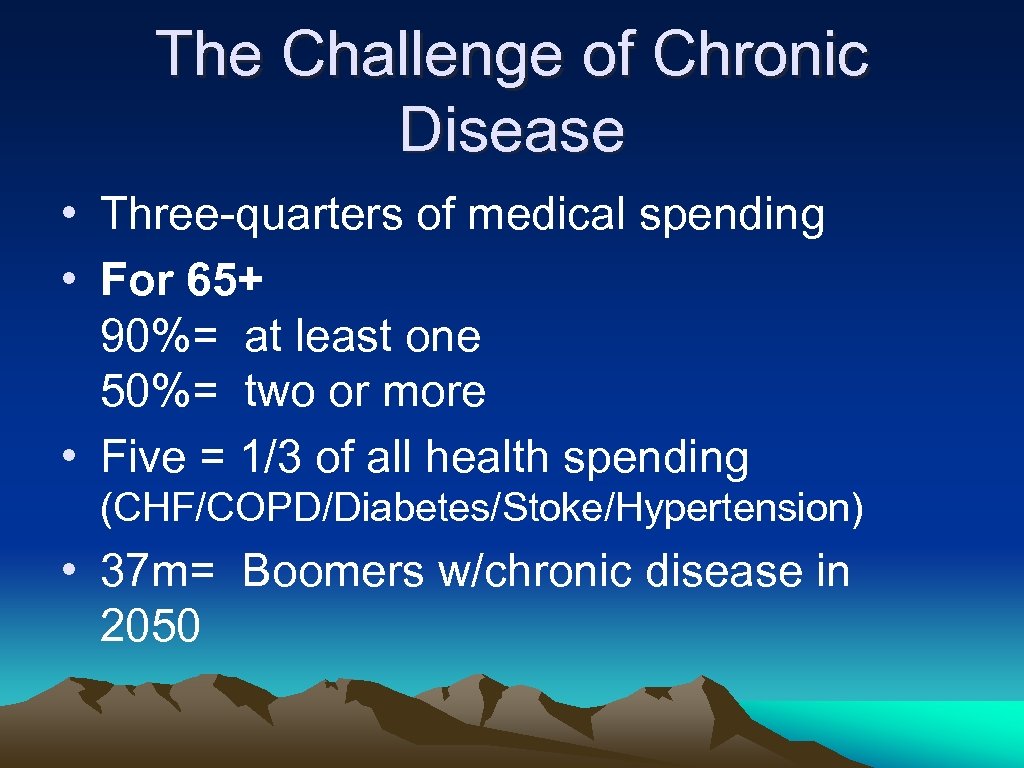
The Challenge of Chronic Disease • Three-quarters of medical spending • For 65+ 90%= at least one 50%= two or more • Five = 1/3 of all health spending (CHF/COPD/Diabetes/Stoke/Hypertension) • 37 m= Boomers w/chronic disease in 2050
Chronic Disease in an Acute Care World • • • Primary care In-patient risks Transitions/discharge planning Post-discharge compliance Balancing medical/personal/social/spiritual

The Mission & The Market • • • Demographics The economy Technology Payment systems State and federal fiscal pressures The Affordable Care Act
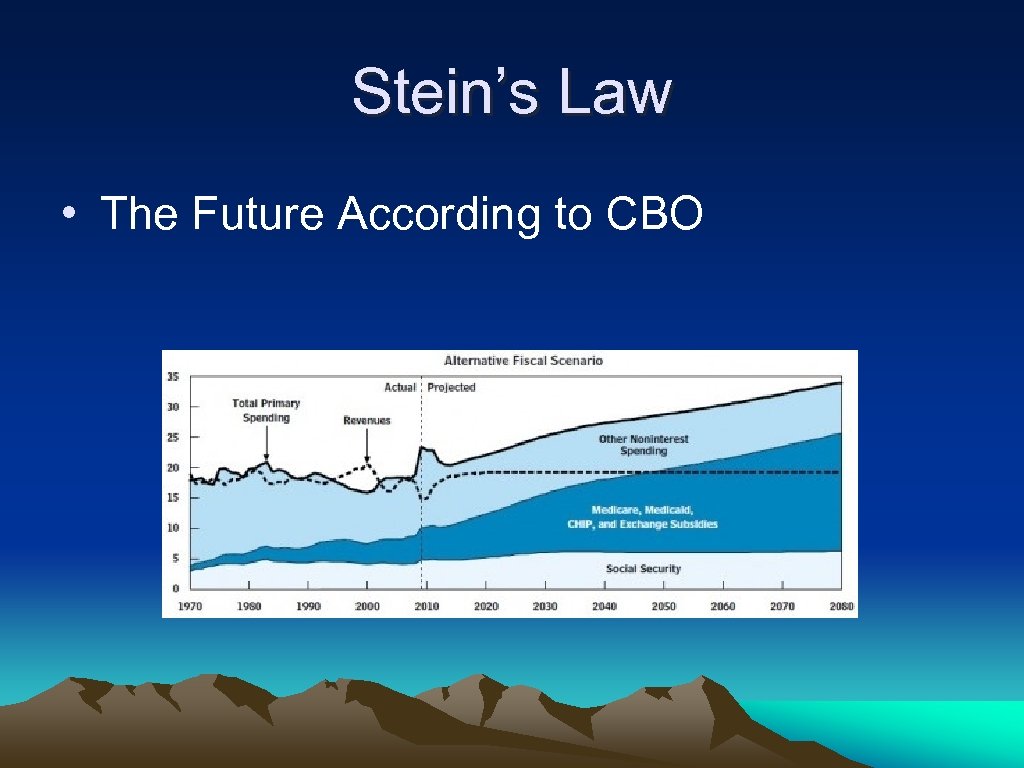
Stein’s Law • The Future According to CBO
The Budget War • Medicare • Medicaid • Non-Medicaid Services
The ACA: Good News and Bad News • The Bad: Less $ for traditional services Growing cost pressures Uncertainty • The Good: More flexibility/integrated care
The Bad… • $500 billion in Medicare provider reductions • 16 m new Medicaid acute patients • Political uncertainty • “All we have to do is provide better care to more people for less money. ”

The Opportunity… • Freedom from Golden Handcuffs • • Opportunities for Innovation: Accountable Care Organizations Bundled Payment Medical Homes
Models for Reform • Keeping patients healthy • Improving transitions • Hospital-quality care in new settings • Reducing Readmissions
Readmissions • Medicare payment cuts for readmissions • Effect on SNFs • Good for payers, but hospitals?

Building Community Relationships • • Congregational Health Network Senior Villages Parish Nursing PACE
Pulling It Together • Guided Care • Palliative Care • Siu’s Vision
Conclusions • A Turning Point for Care Delivery • Integrated Care is hard, but can be done. • Good for patients/Good for providers • Diminishing Gov’t, Growing Community
Thank You Howard Gleckman The Urban Institute 202 -261 -5420 www. urban. org www. caringforourparents. com
Building the Whole Health System : The Emerging Memphis Model Methodist Le. Bonheur Healthcare Center of Excellence in Faith and Health Congregational Health Network Rev. Bobby Baker, Dr. Teresa Cutts, Rev. Dr. Gary Gunderson May 31, 2011
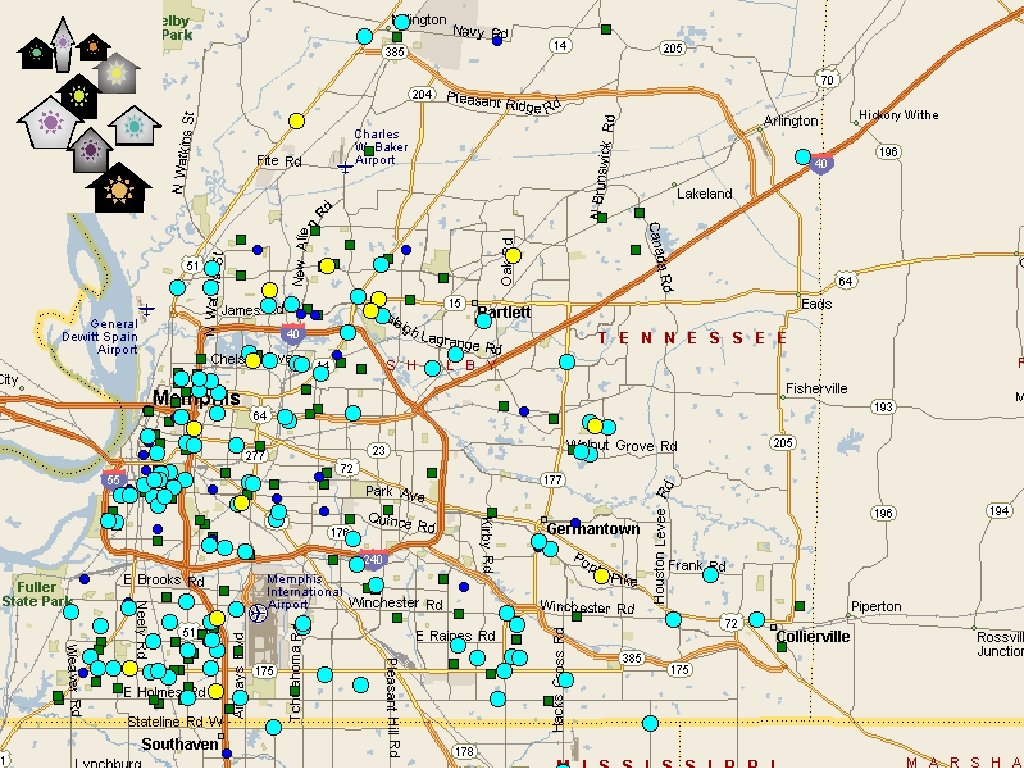
The Memphis Model • • • Methodist Le. Bonheur Healthcare Church Health Center (privately funded) Christ Community Health Services (FQHC) A large array of other faith-based organizations Surrounded by 400 congregations Continually more connected and aligned, strengthening each others’ capacities to improve access and health status of the whole community. • Fueled by intelligences near, global and multidisciplinary • All the assets are real and visible. And the connections are emerging constantly, drawn by common values and vision as they do. • (Big caveat: it’s not actually very pretty)
The goal • Build a trusted care delivery system that integrates traditional clinical care and community-based caregiving • Align and leverage religious and community health assets to improve health outcomes and access for all by 2020 • IHI Triple Aims: Improve population health, improve patient care experience (including quality, access and reliability), reduce and/or control per capita cost of care
What We’ll Talk About The “Memphis Model” • How this relates to integration of a faith-based community health center and other health assets • Community health assets mapping • What it looks and feels like in one congregation • Early outcomes data suggesting positive impact for connecting the congregations • Whether this is unique to one odd city, or adaptable to other communities

Memphis: Land of Disparity Egregious disparity exists: Income, Heart Disease, Diabetes, Cancer, Suicide/Homicide, Limb Amputation

Memphis: Land of the Blues and Lots of Church/Faith
Systems Challenge $1. 5 billion faith-based healthcare system, 43% market share with community mission. • 7 Hospital system • Anchor of “Memphis Model” • One hub of primary care clinics for poor • Unique: 324 congregational partners held together by a system-minded covenant
Church Health Center founded 1987: Safety Net

Christ Community Health Service Neighborhood Clinic Opens 1995: Safety Net
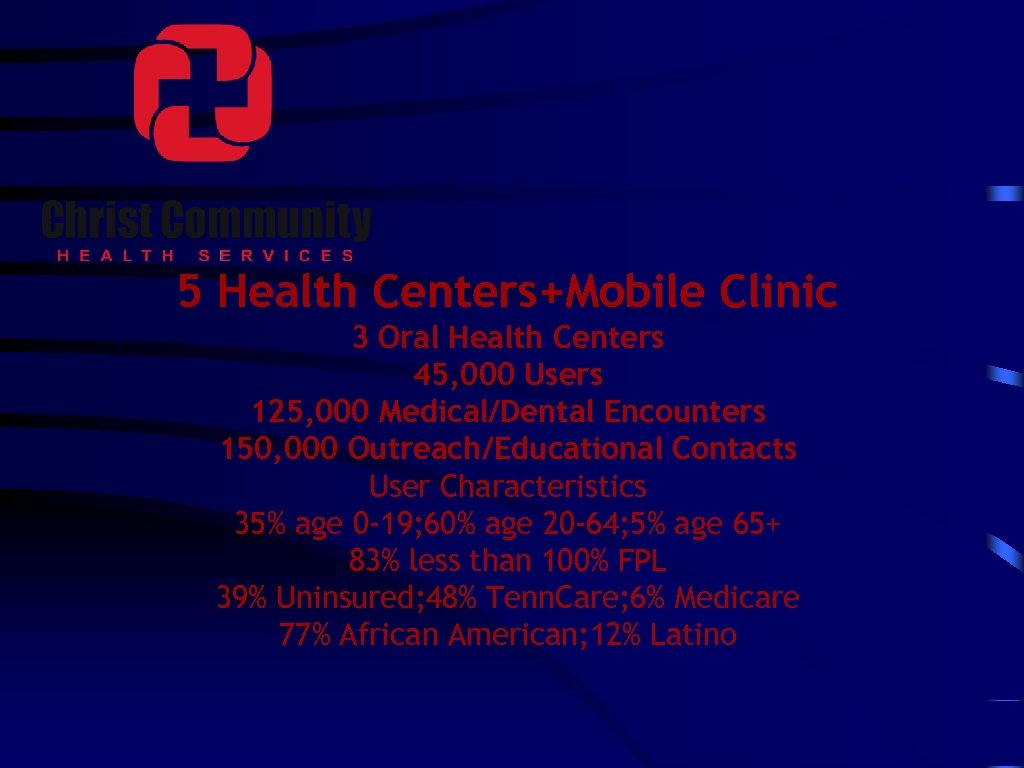
5 Health Centers+Mobile Clinic 3 Oral Health Centers 45, 000 Users 125, 000 Medical/Dental Encounters 150, 000 Outreach/Educational Contacts User Characteristics 35% age 0 -19; 60% age 20 -64; 5% age 65+ 83% less than 100% FPL 39% Uninsured; 48% Tenn. Care; 6% Medicare 77% African American; 12% Latino
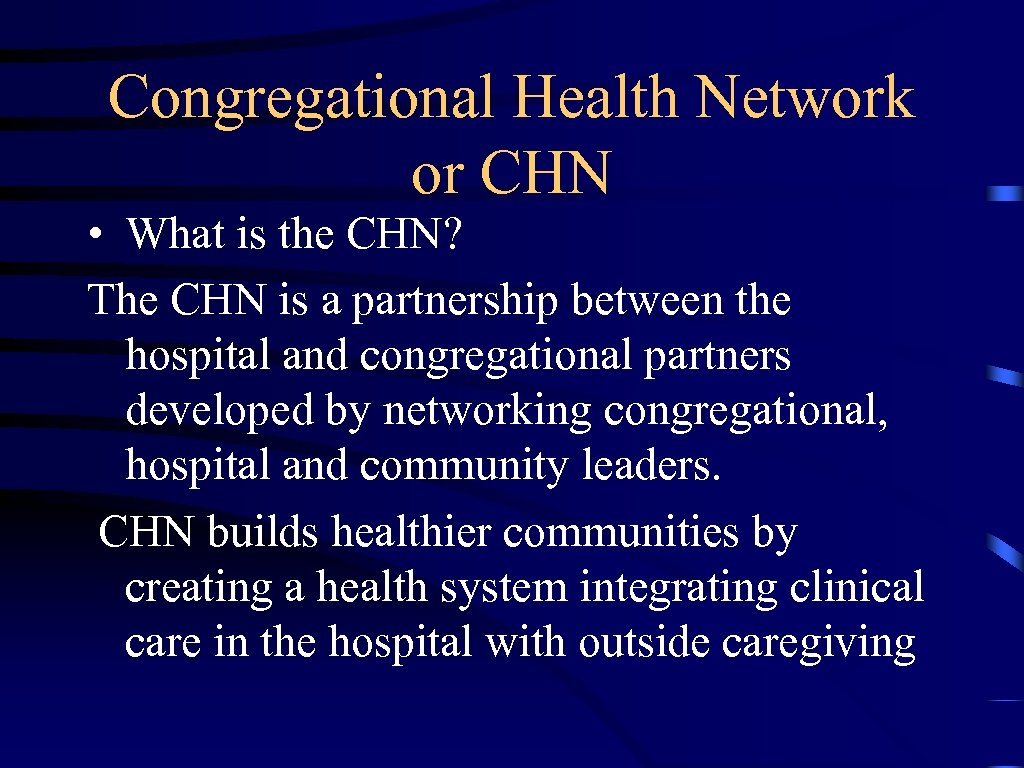
Congregational Health Network or CHN • What is the CHN? The CHN is a partnership between the hospital and congregational partners developed by networking congregational, hospital and community leaders. CHN builds healthier communities by creating a health system integrating clinical care in the hospital with outside caregiving
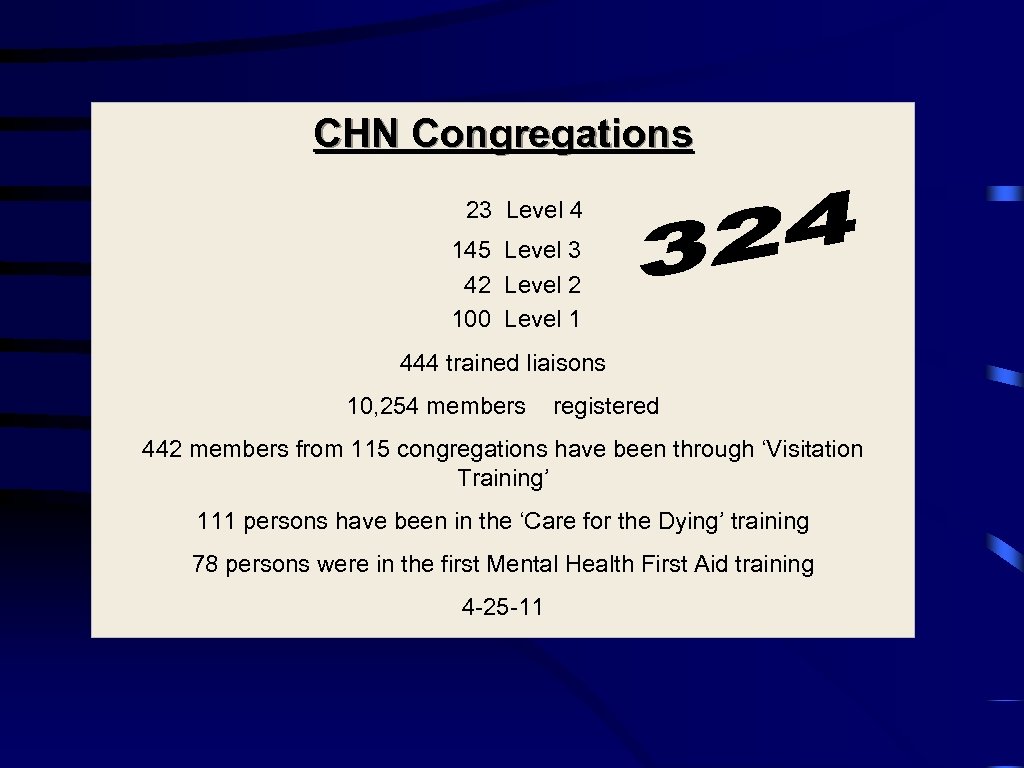
CHN Congregations 23 Level 4 145 Level 3 42 Level 2 100 Level 1 444 trained liaisons 10, 254 members registered 442 members from 115 congregations have been through ‘Visitation Training’ 111 persons have been in the ‘Care for the Dying’ training 78 persons were in the first Mental Health First Aid training 4 -25 -11
CHN Congregational Partner Levels • Level I - Signed Covenant • Level II - Active Liaisons • Level III – CHN Functional • Level IV – Congregational Testimony
The CHN Covenant Agreement A signed document that spells out the partnership developed with clergy.
Four Clear Opportunities • Frail Elderly and End-of Life • Mental Health • Chronic Disease • Infant and Maternal Health
Five Phases in the Journey of Health Defined by Clergy • Education (constant, multi-faceted) • Prevention • Intervention (getting to the right place) • Treatment • Aftercare
Trained volunteer liaisons in every congregation are the functional link
Volunteer Liaison Roles: – ·Recruits congregational members into the network – ·Collects data on network members – ·Notifies CHN navigators of developments/changes – ·Follows network members into and out of the inpatient setting – ·Coordinates transition from hospital – ·Marshals community resources – ·Provides information and referral services – ·Facilitates wellness activity participation
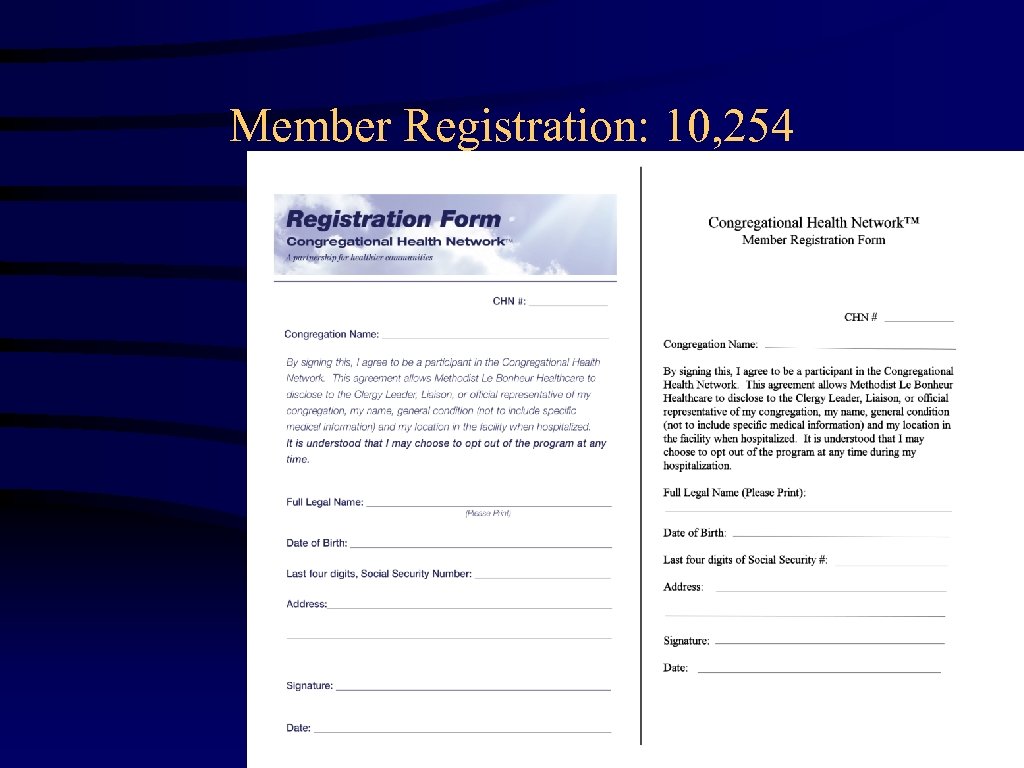
Member Registration: 10, 254
Navigator Roles: 9 Fulltime Hospital Employees – ·Develop a network of community resources ·Coordinate outpatient care ·Assist clients with navigating the service systems ·Provide avenues for prevention and education ·Maintain program documentation and participates in ongoing program evaluation and reporting – ·Participate in team and program staff meetings – ·Make appropriate client notes as required – –

CHN Training Builds Capacity: Over 500 Trained
Educational Trainings offered by CHN 7 Week Trainings, Integrated Education and “Church” • Hospital Visitation Training • Aftercare Training (Hands-On Caregiving) • Care for the Dying • Mental Health First Aid
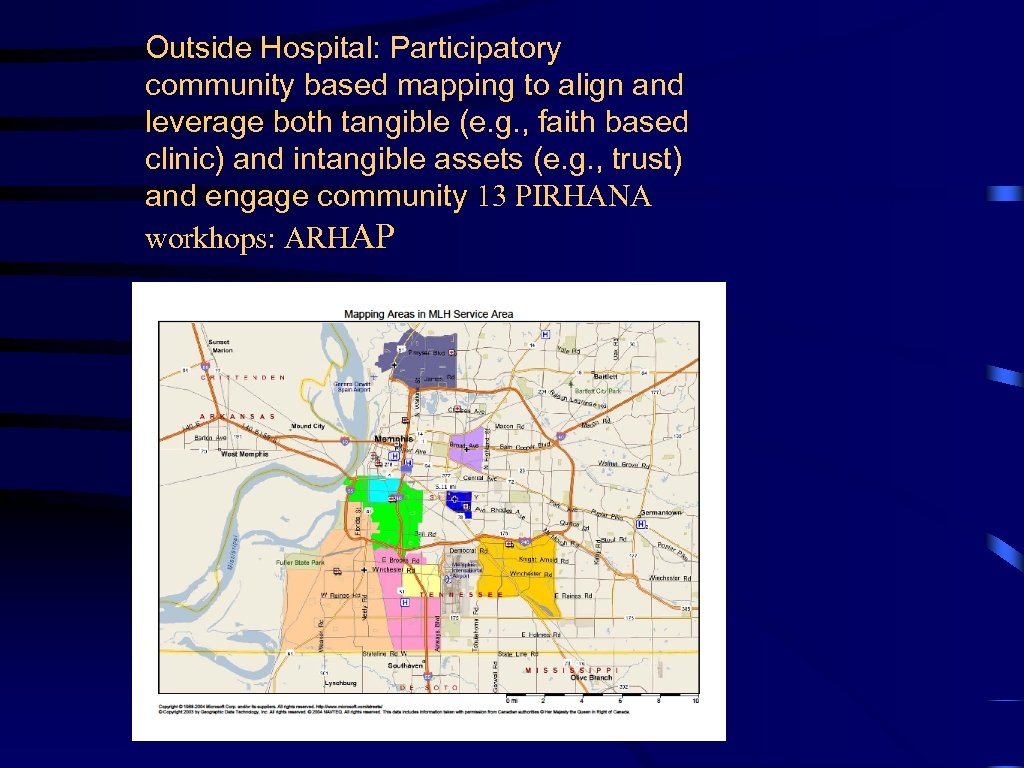
Outside Hospital: Participatory community based mapping to align and leverage both tangible (e. g. , faith based clinic) and intangible assets (e. g. , trust) and engage community 13 PIRHANA workhops: ARHAP
Data Inside the Hospital -Working with Case Management, Clinical Informatics, Policy, Social Work, Medical Staff, Nursing, Alliance Aftercare and Hospice to integrate their work with our CHN navigators to seamlessly build care pathways for members/patients CHN process measures through our Electronic Medical Record (EMR) -Preliminary CHN outcome and pre-post data tracked through EMR
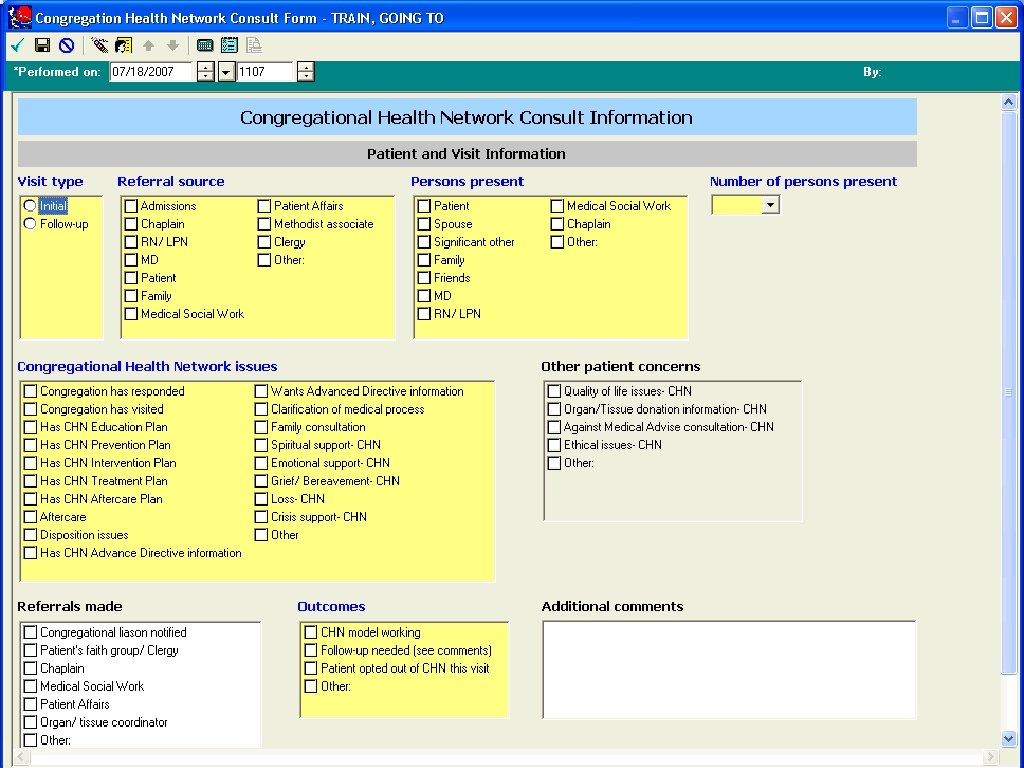
Navigator Consult Screen
Congregational Health Network: Outcome Measures • Impact measured in hospital from Electronic Medical Record (compare CHN vs. non-CHN patient on disease care piece of “health journey”) – Decreased length of stay? – Decreased recidivism (return within 30 days)? – Decreased total costs? – Decreased mortality rate?
CHN Early Outcome Data (NOT a Research Project per se) Initial Data from first 25 months of build-out and operation of CHN: Nov. 2007 -Nov. 2009 Comparison of 473 CHN Members who came into MLH to controls who also were patients (matched on age, gender, ethnicity) in this timeframe Gross Hypothesis: CHN=social intervention; CHN and non-CHN receive standard care in hospital, CHN caregiving outside impacts outcomes in the hospital
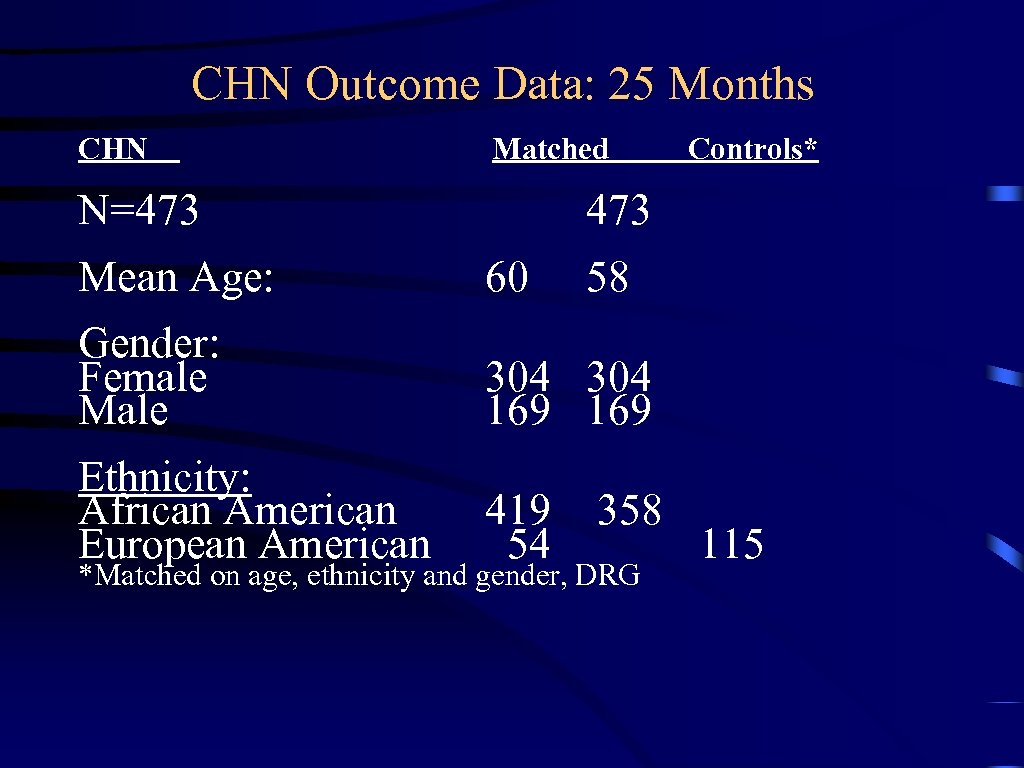
CHN Outcome Data: 25 Months CHN Matched N=473 Controls* 473 Mean Age: 60 58 Gender: Female Male 304 169 Ethnicity: African American European American 419 54 358 *Matched on age, ethnicity and gender, DRG 115
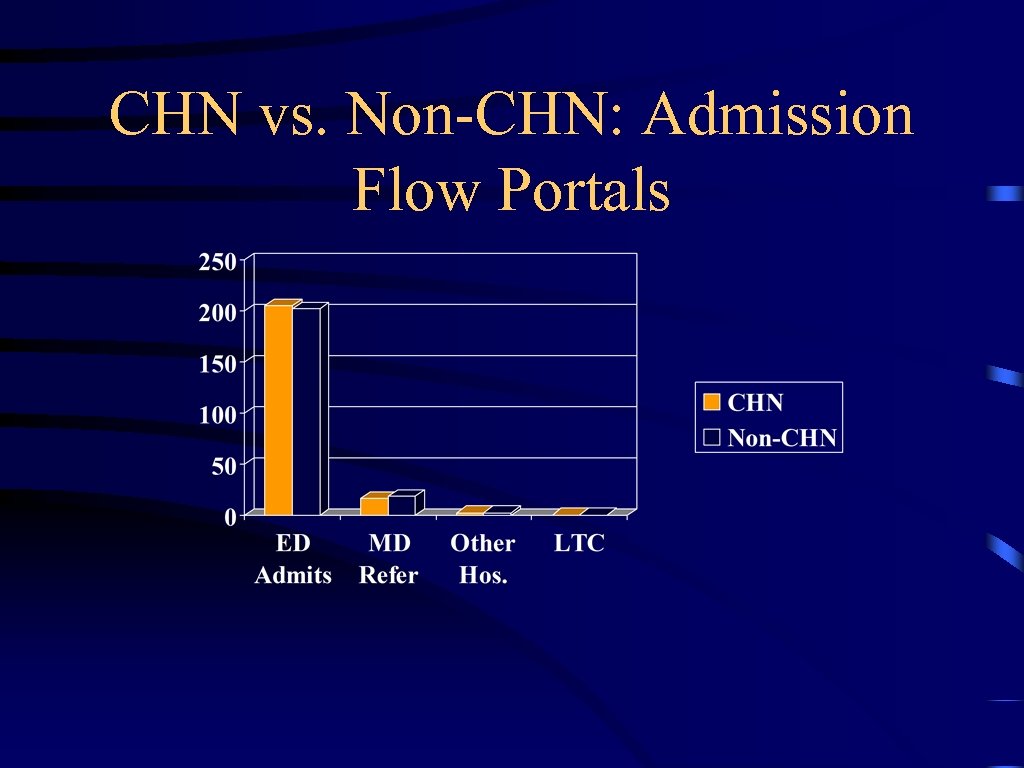
CHN vs. Non-CHN: Admission Flow Portals
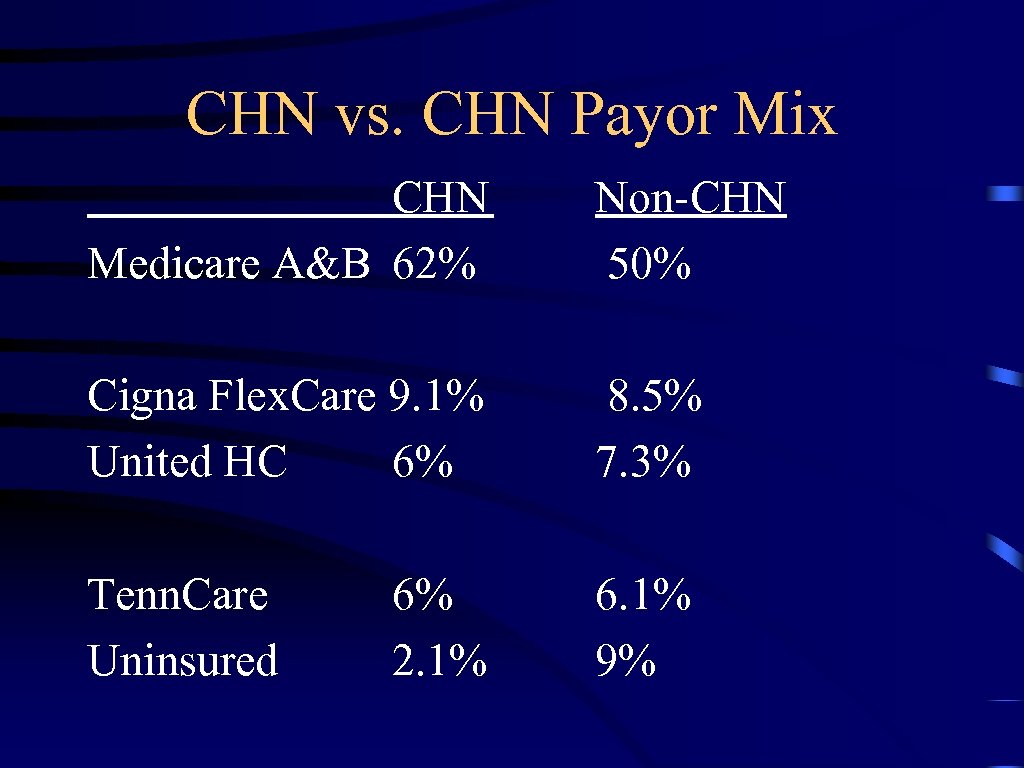
CHN vs. CHN Payor Mix CHN Medicare A&B 62% Non-CHN 50% Cigna Flex. Care 9. 1% United HC 6% 8. 5% 7. 3% Tenn. Care Uninsured 6. 1% 9% 6% 2. 1%
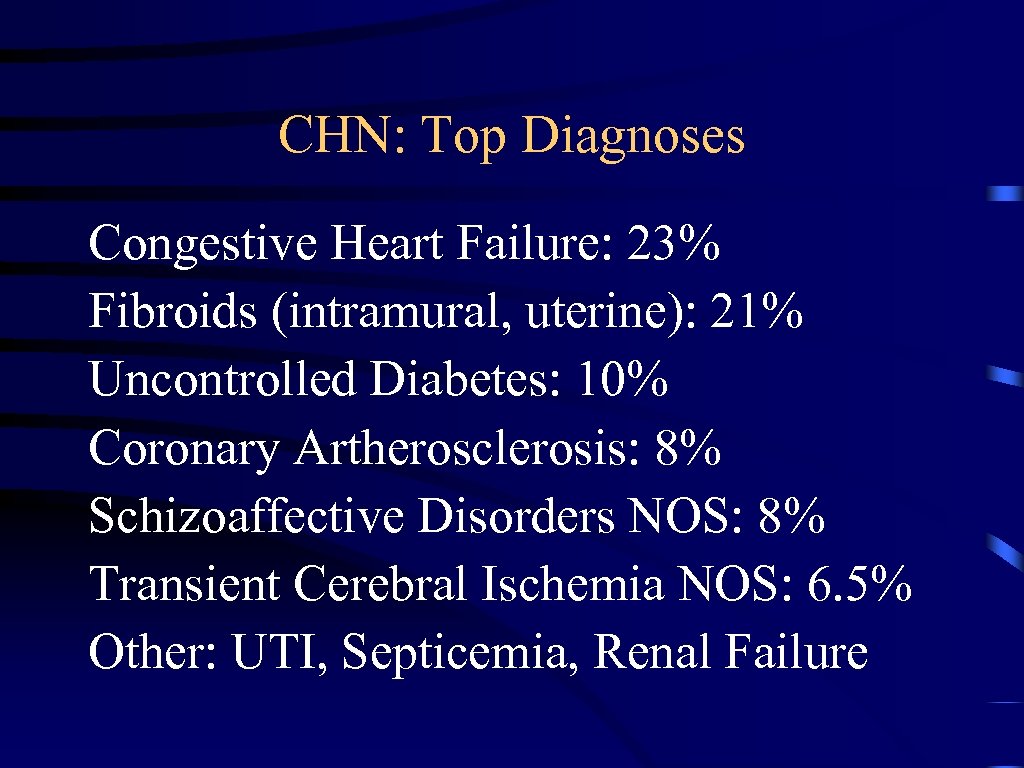
CHN: Top Diagnoses Congestive Heart Failure: 23% Fibroids (intramural, uterine): 21% Uncontrolled Diabetes: 10% Coronary Artherosclerosis: 8% Schizoaffective Disorders NOS: 8% Transient Cerebral Ischemia NOS: 6. 5% Other: UTI, Septicemia, Renal Failure
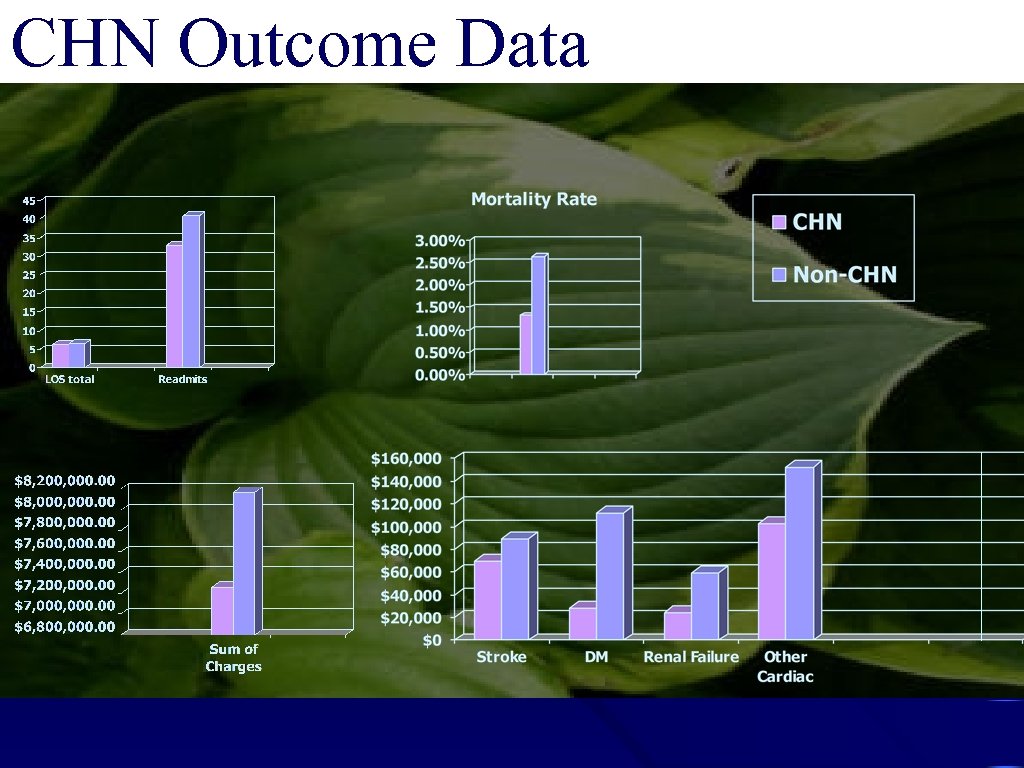
CHN Outcome Data
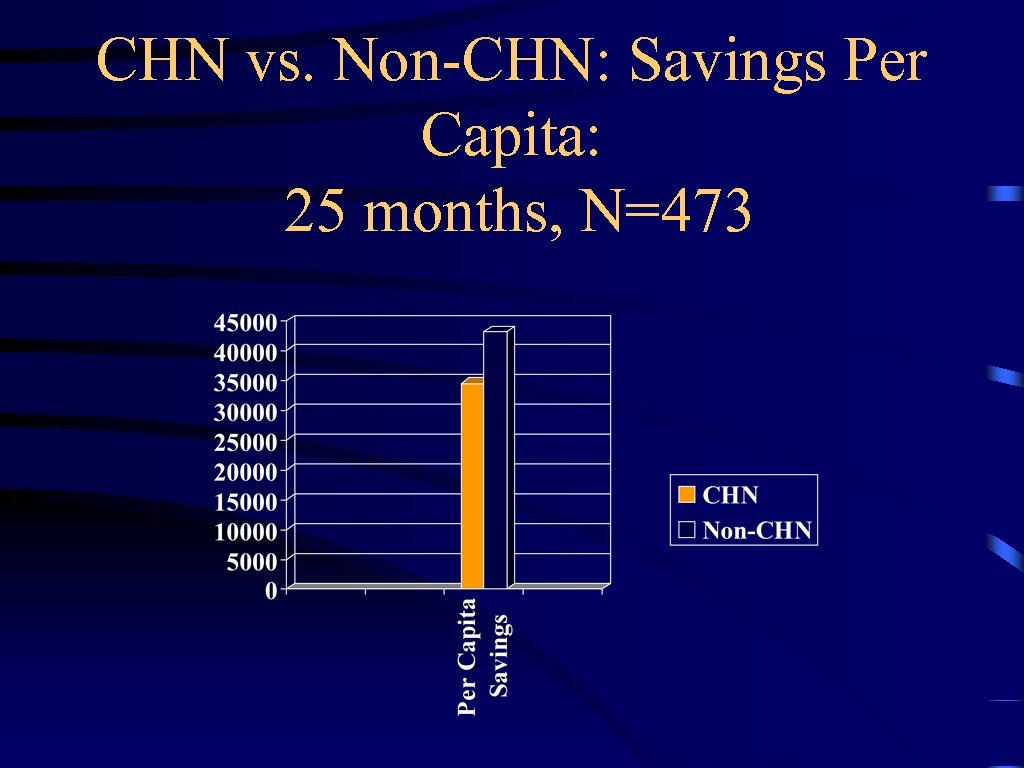
CHN vs. Non-CHN: Savings Per Capita: 25 months, N=473
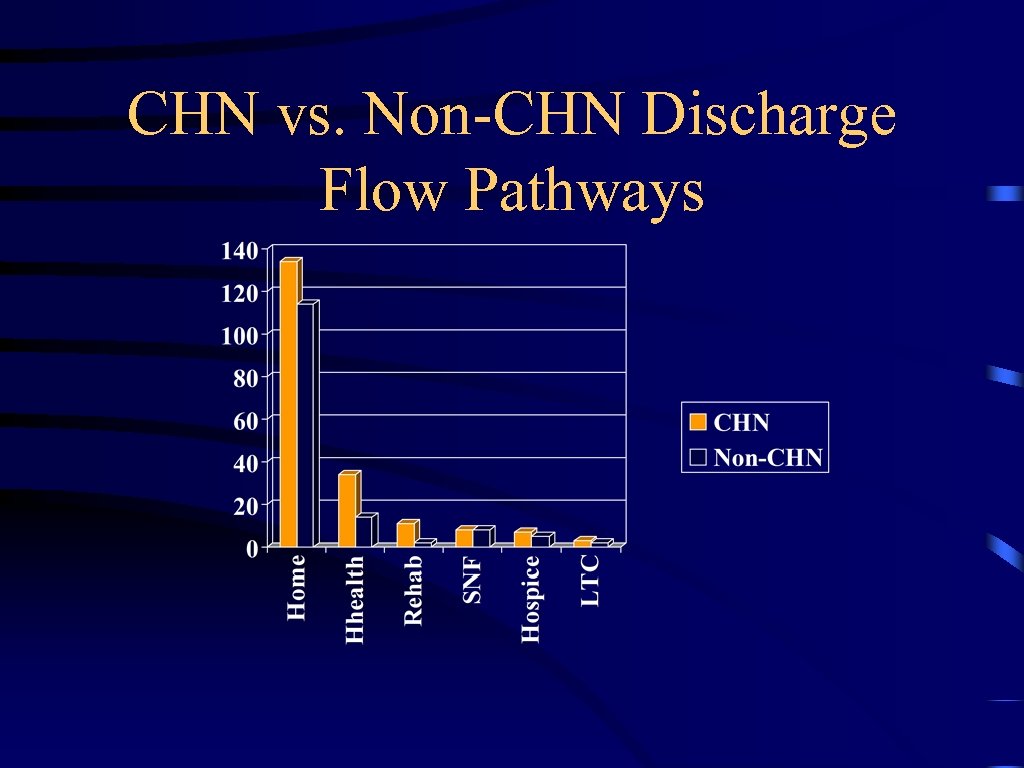
CHN vs. Non-CHN Discharge Flow Pathways
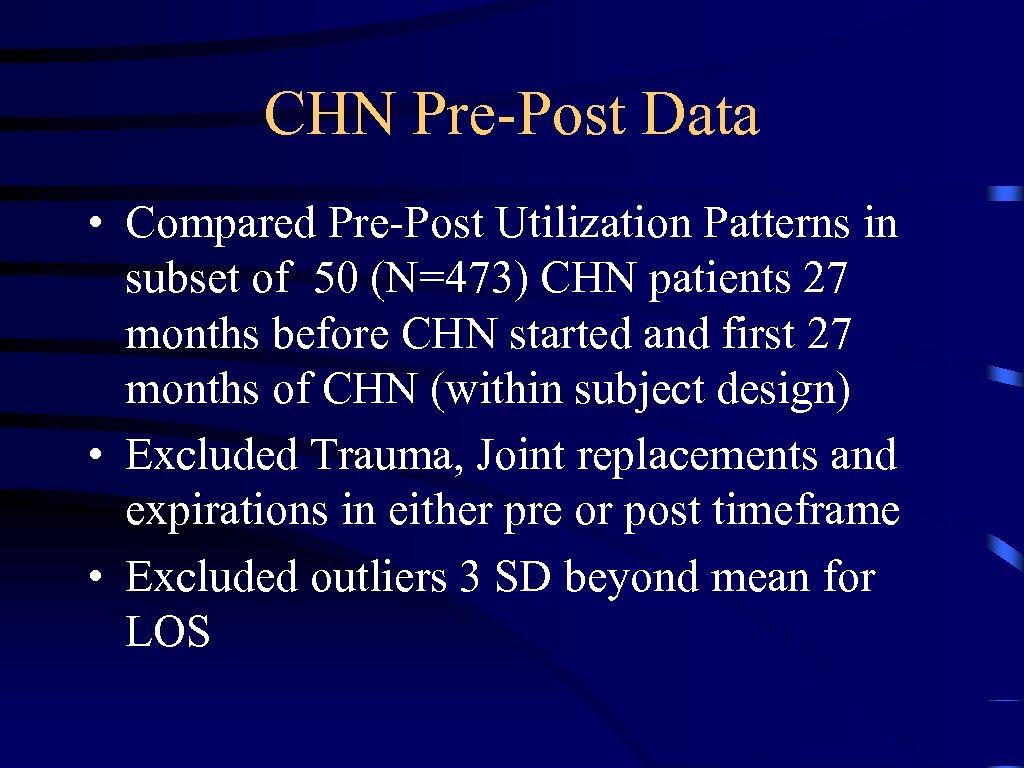
CHN Pre-Post Data • Compared Pre-Post Utilization Patterns in subset of 50 (N=473) CHN patients 27 months before CHN started and first 27 months of CHN (within subject design) • Excluded Trauma, Joint replacements and expirations in either pre or post timeframe • Excluded outliers 3 SD beyond mean for LOS
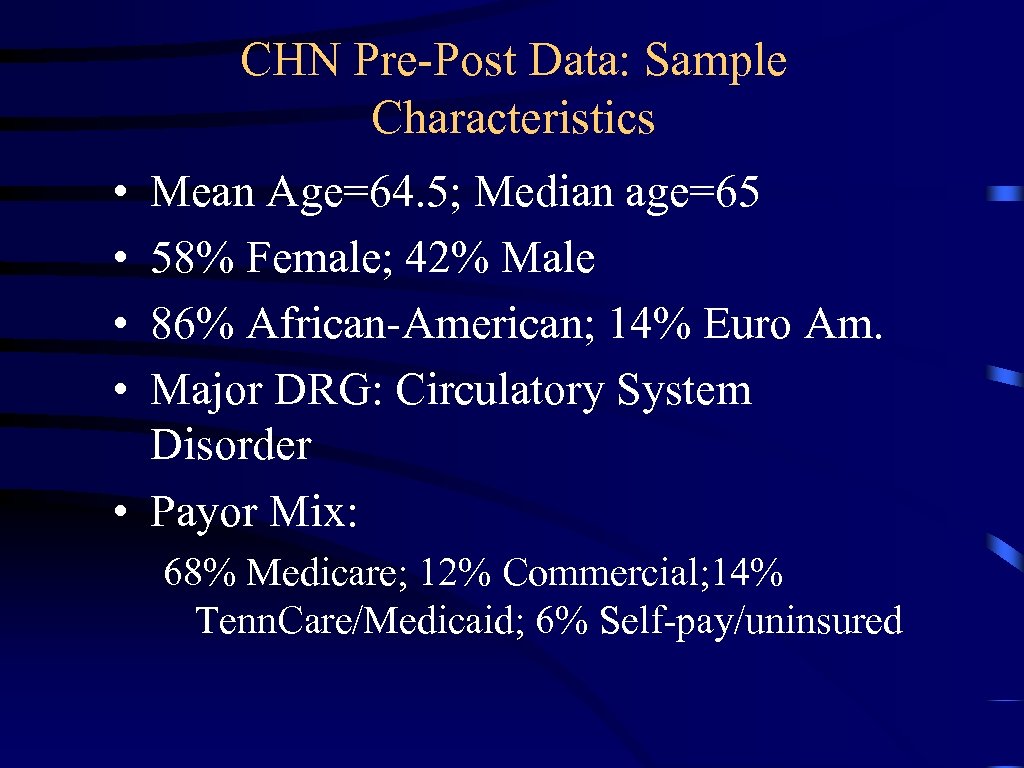
CHN Pre-Post Data: Sample Characteristics • • Mean Age=64. 5; Median age=65 58% Female; 42% Male 86% African-American; 14% Euro Am. Major DRG: Circulatory System Disorder • Payor Mix: 68% Medicare; 12% Commercial; 14% Tenn. Care/Medicaid; 6% Self-pay/uninsured
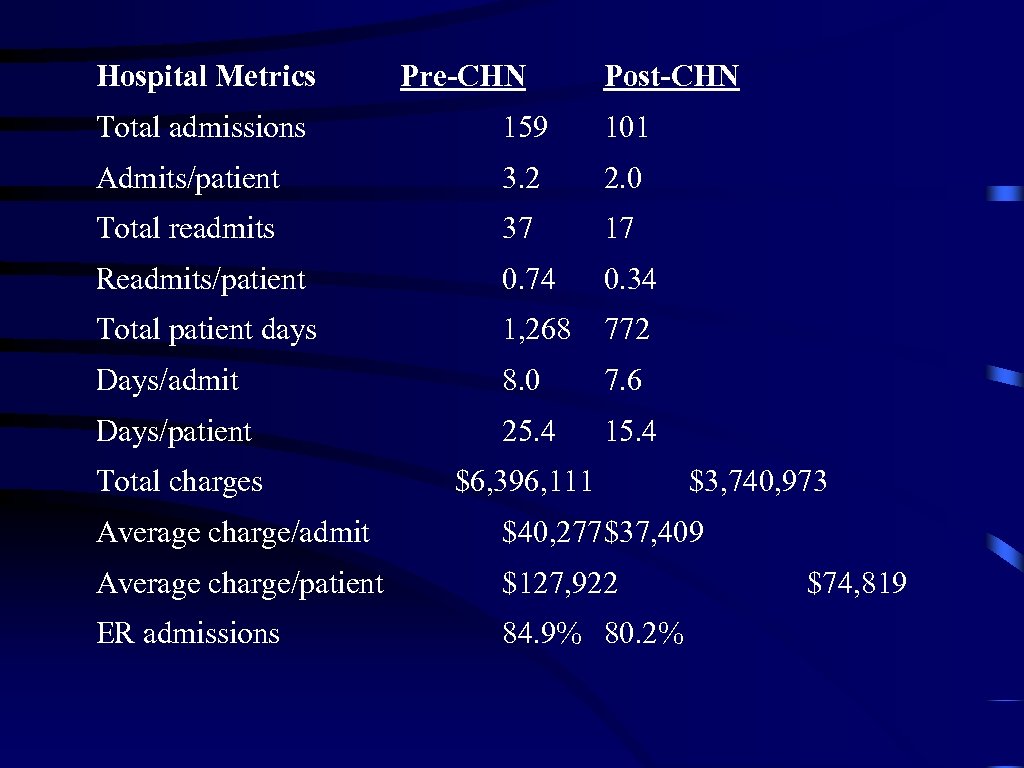
Hospital Metrics Pre-CHN Post-CHN Total admissions 159 101 Admits/patient 3. 2 2. 0 Total readmits 37 17 Readmits/patient 0. 74 0. 34 Total patient days 1, 268 772 Days/admit 8. 0 7. 6 Days/patient 25. 4 15. 4 Total charges $6, 396, 111 $3, 740, 973 Average charge/admit $40, 277$37, 409 Average charge/patient $127, 922 ER admissions 84. 9% 80. 2% $74, 819
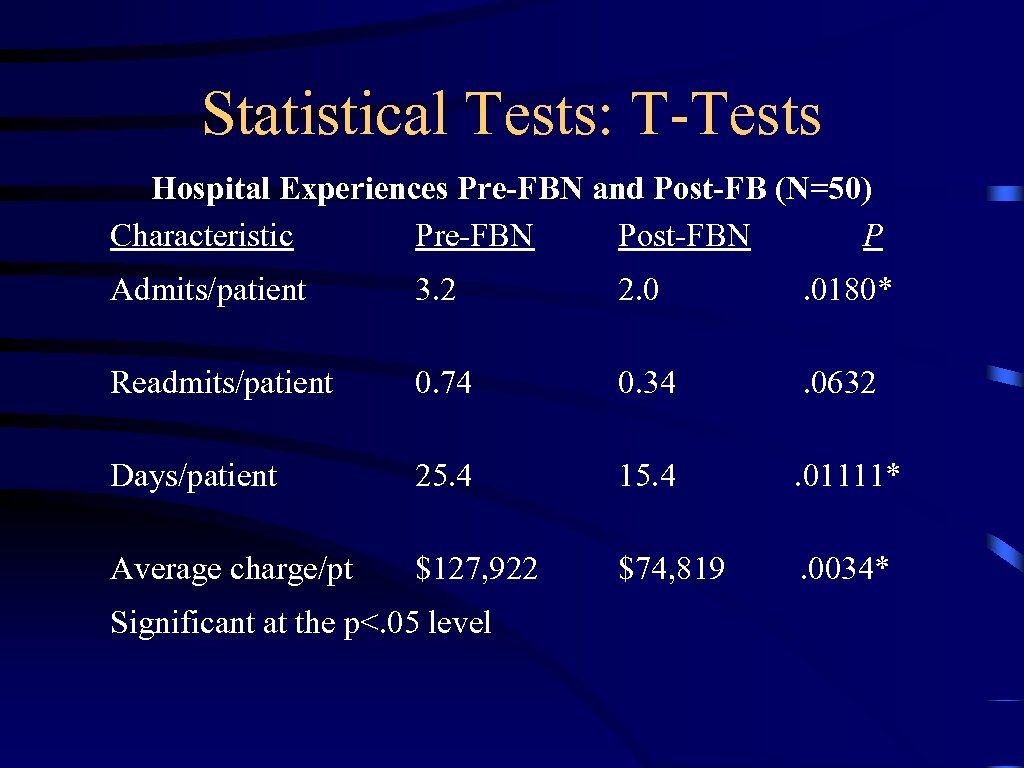
Statistical Tests: T-Tests Hospital Experiences Pre-FBN and Post-FB (N=50) Characteristic Pre-FBN Post-FBN P Admits/patient 3. 2 2. 0 . 0180* Readmits/patient 0. 74 0. 34 . 0632 Days/patient 25. 4 15. 4 . 01111* Average charge/pt $127, 922 $74, 819 . 0034* Significant at the p<. 05 level
CHN Pre-Post Data • Significant utilization differences existed for patients served before and after the CHN existed – Fewer Admits, Hospital Days, Lower Average Charge/Patient; Decrease in mean # admissions – Readmits/Patient Approached Significance – Charge data were not adjusted for inflation over the full 54 month period – Cohort aged over the timeframe – Not due to inpatient clinical management differences (no change in average charge/admission) – Which Leads Us Outside of Hospital….
What’s moving the data? –Blended intelligence • What the hospital knows about disease • What the clergy and liaisons know about life –Aligned assets leveraging raw Trust • Faith-driven treatment system (reimbursed) • Faith-driven healing system (non-reimbursed)
CHN Outcome Data Preliminary data is promising, but needs more systematic review, more rigorous scrutiny and deeper dive. • Data sets archive at no cost • Need funds/resources to analyze data • Developing best practice models for analyzing these data via interdisciplinary models/lens
Memphis Model: What’s Adaptable/Replicable? • Anchor organization with strong community commitment • Federally qualified Community Health Clinic • Strong Faith Leader(s) and grassroots organization • Use of Memphis Model logic to build webs of trust: invitation, transparency, sharing resources, leadership holds open space for emergence, building and nurturing trust, honoring blended intelligence
The Center of Excellence: Blending Faith & Health Relevant Science should: – Be evidence based – Result in improvement in quality of life for all – Eliminate disparity But also be: – Participatory and teachable by blended intelligence – Innovative – or grounded in life; – Disruptively useful for promoting justice… – Comparative across sites
Fundamental Systems Challenges • Health assets under multiple ownership and control and perversely incentivised to compete or run in parallel • History of class and race fuel fear, friction and disconnection and appropriate distrust • Even within our 7 hospitals, irrational deployment of assets because that's what you get with humans and the institutions they create over time
Need More Mature Science. . • . . . understanding of turbulent human systems as they adapt to changing context of science, demographics, global drivers and multi-layered policy • . . . understanding of what spirit, faith, vision and religion have to do with the above as both liability and asset • . . . especially in the minds of those in a position to influence the development of those systems • . . . so they might bend toward justice and health QUESTION & ANSWERS?
Catholic Health Strategy Webinar: Integrating Services for Seniors – Parish-based Programs Q&A © 2011 by the Catholic Health Association of the United States May 31, 2011 70
97432138145b6866be90b21dc60ce6a3.ppt