24ac9a3129c22ffaa17c0edd43839b6c.ppt
- Количество слайдов: 115
 Welcome First National Stroke Audit Meeting RCP(Ed) 17 th Dec 02
Welcome First National Stroke Audit Meeting RCP(Ed) 17 th Dec 02
 Agenda • Who is here and who isn’t? • Background – relationship to national strategy – purpose • • Examples of output which will be available Overview of National Audit of Stroke How to run the system locally Tea/coffee Live demonstration of software system Questions Future Plans
Agenda • Who is here and who isn’t? • Background – relationship to national strategy – purpose • • Examples of output which will be available Overview of National Audit of Stroke How to run the system locally Tea/coffee Live demonstration of software system Questions Future Plans
 Establishing a National Audit of Stroke in Scotland Joint project: Intercollegiate committee on audit & standards Scottish Stroke Collaboration Information & Statistics Division funded so far by CHSS & RCP (Edin) now by the Scottish Executive
Establishing a National Audit of Stroke in Scotland Joint project: Intercollegiate committee on audit & standards Scottish Stroke Collaboration Information & Statistics Division funded so far by CHSS & RCP (Edin) now by the Scottish Executive
 Who’s Here • Members of the steering group – MSD – Gordon Lowe - SIGN & RCPE – David Stott - Intercollegiate Standards Committee – Campbell Chalmers - CHSS – Beatrice Cant - CRAG/CEPS – Apologies from Rod Muir - ISD
Who’s Here • Members of the steering group – MSD – Gordon Lowe - SIGN & RCPE – David Stott - Intercollegiate Standards Committee – Campbell Chalmers - CHSS – Beatrice Cant - CRAG/CEPS – Apologies from Rod Muir - ISD
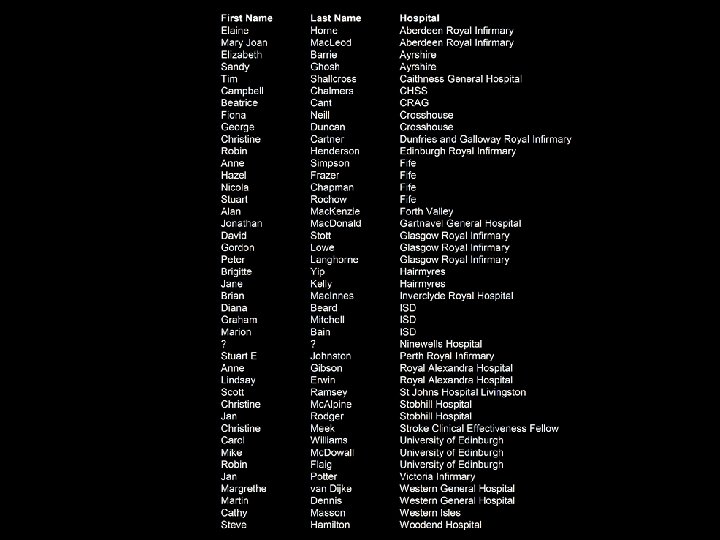
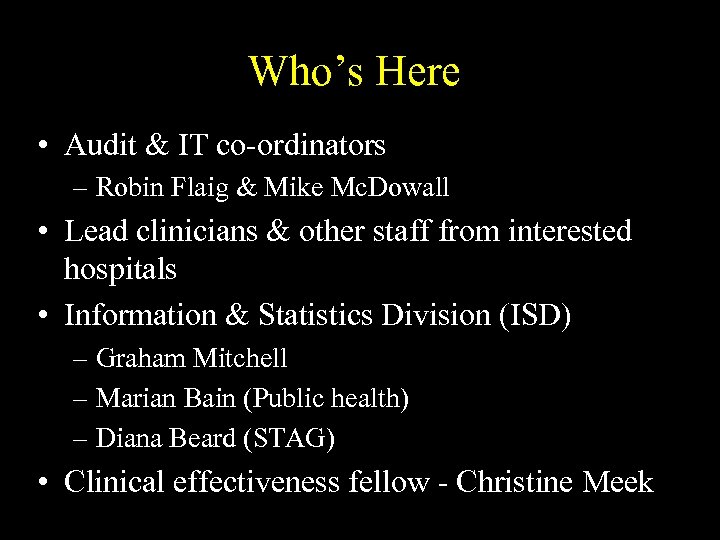 Who’s Here • Audit & IT co-ordinators – Robin Flaig & Mike Mc. Dowall • Lead clinicians & other staff from interested hospitals • Information & Statistics Division (ISD) – Graham Mitchell – Marian Bain (Public health) – Diana Beard (STAG) • Clinical effectiveness fellow - Christine Meek
Who’s Here • Audit & IT co-ordinators – Robin Flaig & Mike Mc. Dowall • Lead clinicians & other staff from interested hospitals • Information & Statistics Division (ISD) – Graham Mitchell – Marian Bain (Public health) – Diana Beard (STAG) • Clinical effectiveness fellow - Christine Meek
 Background
Background
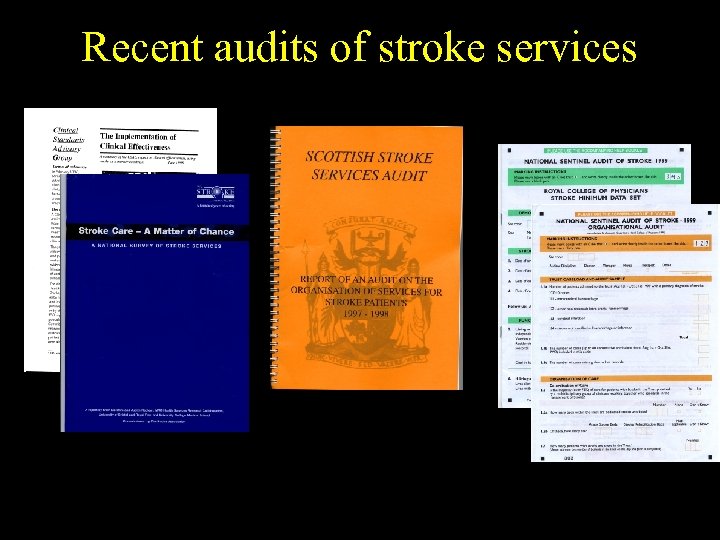 Recent audits of stroke services
Recent audits of stroke services
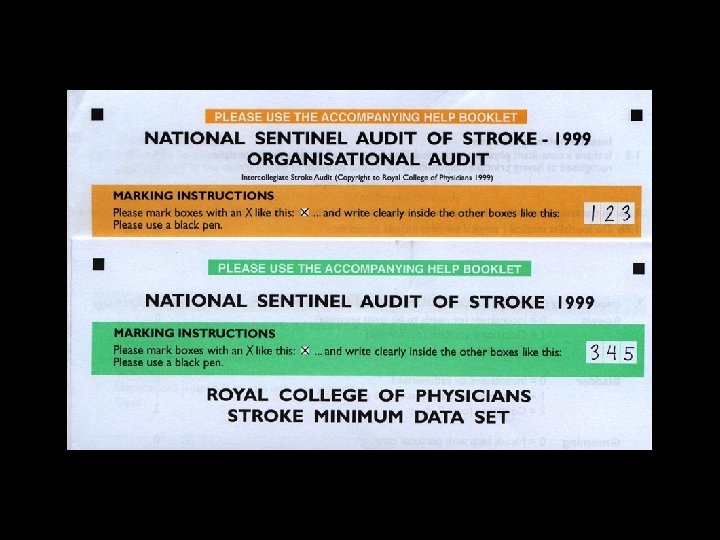
 National Sentinel Audit (England, Wales & N Ireland) • Co-ordinated by RCP (Lond) • Organisation, min dataset, case note review • Uses modified, extended and tested version of RCP stroke Audit Package • Inter-rater reliability tested • Completed for 40 consecutive patients in most Trusts • 6894 cases in first round • third round now completed
National Sentinel Audit (England, Wales & N Ireland) • Co-ordinated by RCP (Lond) • Organisation, min dataset, case note review • Uses modified, extended and tested version of RCP stroke Audit Package • Inter-rater reliability tested • Completed for 40 consecutive patients in most Trusts • 6894 cases in first round • third round now completed
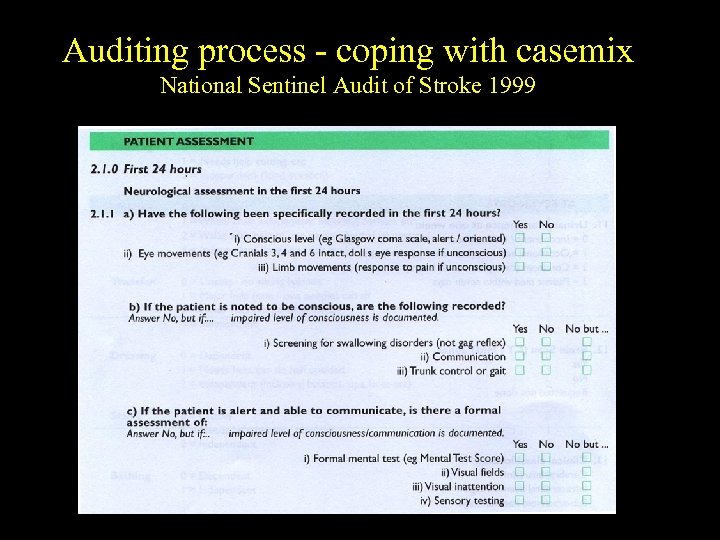 Auditing process - coping with casemix National Sentinel Audit of Stroke 1999
Auditing process - coping with casemix National Sentinel Audit of Stroke 1999
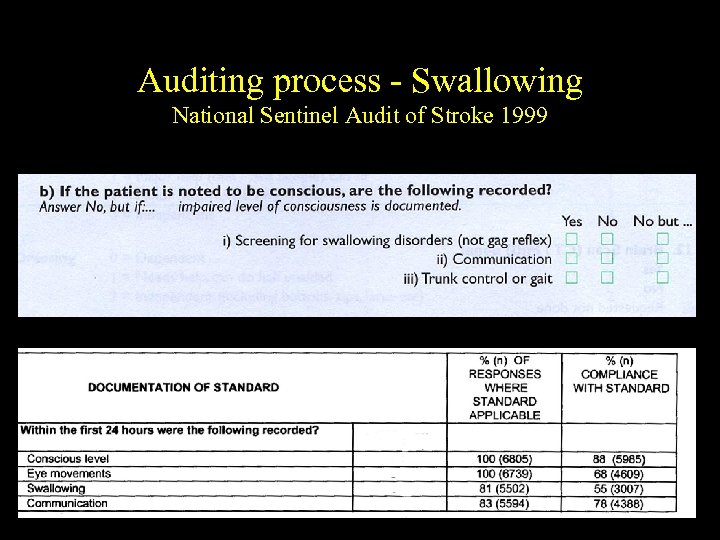 Auditing process - Swallowing National Sentinel Audit of Stroke 1999
Auditing process - Swallowing National Sentinel Audit of Stroke 1999
 Problems of Sentinel Audits • Only 40 sets of case notes per Trust therefore imprecise • Little control over sampling - therefore potentially biased • Data extraction not resourced • No independent data extraction - therefore potentially biased
Problems of Sentinel Audits • Only 40 sets of case notes per Trust therefore imprecise • Little control over sampling - therefore potentially biased • Data extraction not resourced • No independent data extraction - therefore potentially biased
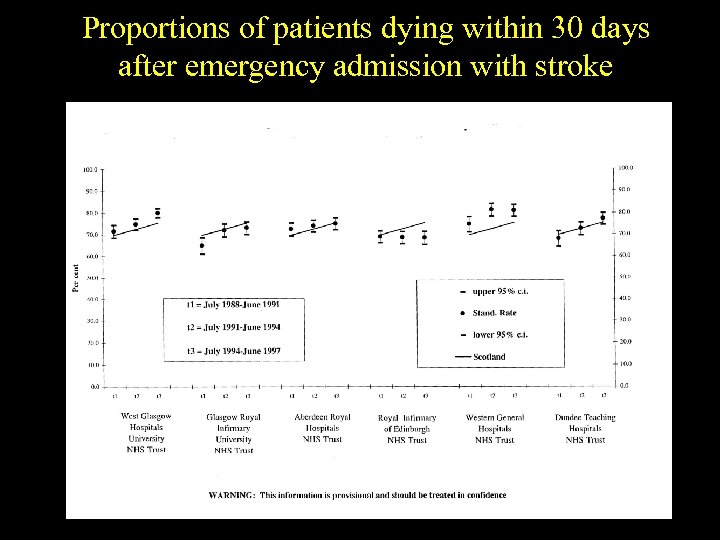 Proportions of patients dying within 30 days after emergency admission with stroke
Proportions of patients dying within 30 days after emergency admission with stroke
 Problem of Stroke Outcome Indicators • • • Diagnostic inaccuracies Lack of confidence in data Insufficient data on outcomes Virtually no data on process Inadequate casemix adjustment
Problem of Stroke Outcome Indicators • • • Diagnostic inaccuracies Lack of confidence in data Insufficient data on outcomes Virtually no data on process Inadequate casemix adjustment
 6 month Case Fatality Rate Crude Adjusted
6 month Case Fatality Rate Crude Adjusted
 Death or dependency at 6 month Crude Adjusted
Death or dependency at 6 month Crude Adjusted
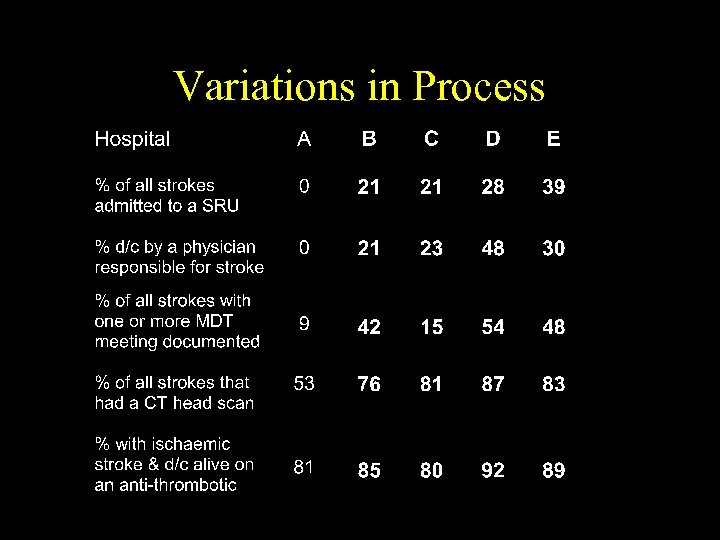 Variations in Process
Variations in Process
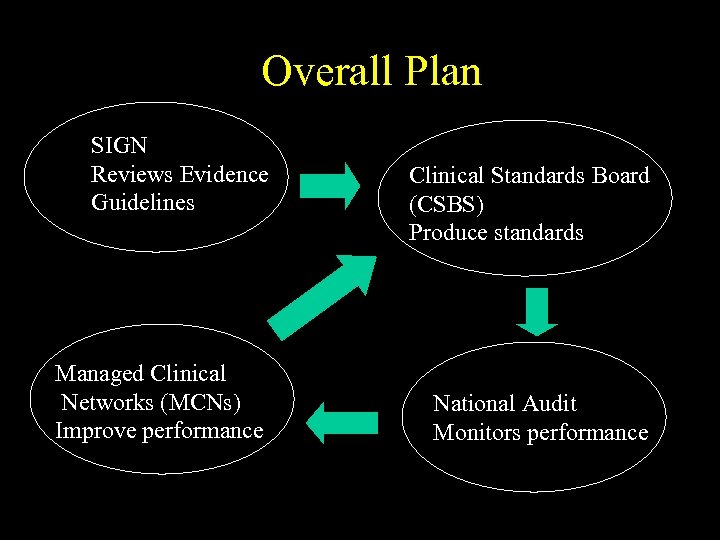 Overall Plan SIGN Reviews Evidence Guidelines Managed Clinical Networks (MCNs) Improve performance Clinical Standards Board (CSBS) Produce standards National Audit Monitors performance
Overall Plan SIGN Reviews Evidence Guidelines Managed Clinical Networks (MCNs) Improve performance Clinical Standards Board (CSBS) Produce standards National Audit Monitors performance
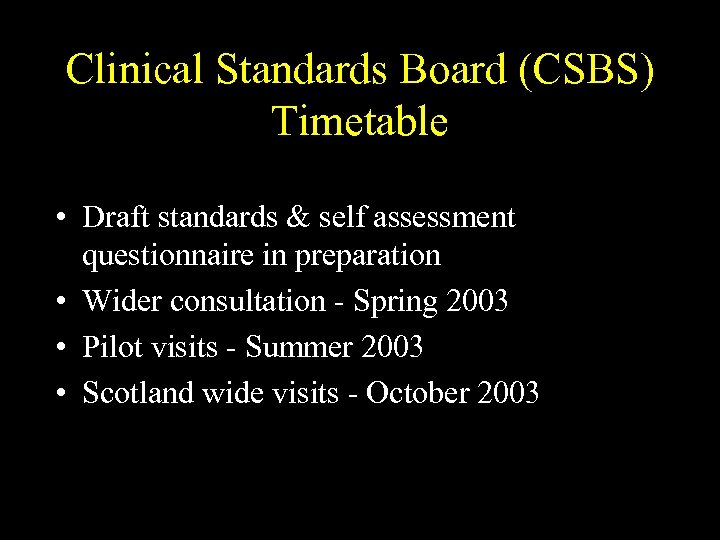 Clinical Standards Board (CSBS) Timetable • Draft standards & self assessment questionnaire in preparation • Wider consultation - Spring 2003 • Pilot visits - Summer 2003 • Scotland wide visits - October 2003
Clinical Standards Board (CSBS) Timetable • Draft standards & self assessment questionnaire in preparation • Wider consultation - Spring 2003 • Pilot visits - Summer 2003 • Scotland wide visits - October 2003
 Some current draft standards CSBS >70% admitted to a stroke unit within 24 hours >90% having a CT or MR scan (within 7 days of admission) >90% of ischaemic strokes given aspirin within 48 hours of admission >80% of patients seen in Neurovascular clinics within 14 days A system is in place to collect data specified in the Scottish Minimum Data Set for all patients
Some current draft standards CSBS >70% admitted to a stroke unit within 24 hours >90% having a CT or MR scan (within 7 days of admission) >90% of ischaemic strokes given aspirin within 48 hours of admission >80% of patients seen in Neurovascular clinics within 14 days A system is in place to collect data specified in the Scottish Minimum Data Set for all patients
 The CHD & Stroke Strategy • All hospitals which routinely admit patients with acute stroke should introduce systems to facilitate the collection of a nationallydefined minimum dataset for each patient admitted, in order to allow monitoring of performance against nationally agreed standards
The CHD & Stroke Strategy • All hospitals which routinely admit patients with acute stroke should introduce systems to facilitate the collection of a nationallydefined minimum dataset for each patient admitted, in order to allow monitoring of performance against nationally agreed standards
 The CHD & Stroke Strategy • All hospitals which routinely admit patients with stroke should join the pilot phase if the Scottish Executive project to establish a National Monitoring System for hospitalbased stroke services.
The CHD & Stroke Strategy • All hospitals which routinely admit patients with stroke should join the pilot phase if the Scottish Executive project to establish a National Monitoring System for hospitalbased stroke services.
 The CHD & Stroke Strategy • Hospitals will need to identify a lead clinician for this project as well as staff to ensure complete data collection. • Where an IT system already exists, resources should be identified to ensure its compatibility with nationally-agreed methods and datasets;
The CHD & Stroke Strategy • Hospitals will need to identify a lead clinician for this project as well as staff to ensure complete data collection. • Where an IT system already exists, resources should be identified to ensure its compatibility with nationally-agreed methods and datasets;
 The CHD & Stroke Strategy • Further development work should be resourced to establish the feasibility and methods of linking the hospital-based systems with those in primary care, to allow capture of information relating to longerterm management of stroke patients and outcome.
The CHD & Stroke Strategy • Further development work should be resourced to establish the feasibility and methods of linking the hospital-based systems with those in primary care, to allow capture of information relating to longerterm management of stroke patients and outcome.
 Why should your hospital participate? • To identify deficiencies of service which can be addressed • To inform development of Managed Clinical Network • To meet data needs of CSBS • To help monitor progress of CHD & Stroke strategy • To meet requirements for appraisal & revalidation
Why should your hospital participate? • To identify deficiencies of service which can be addressed • To inform development of Managed Clinical Network • To meet data needs of CSBS • To help monitor progress of CHD & Stroke strategy • To meet requirements for appraisal & revalidation
 Any Comments or Questions?
Any Comments or Questions?
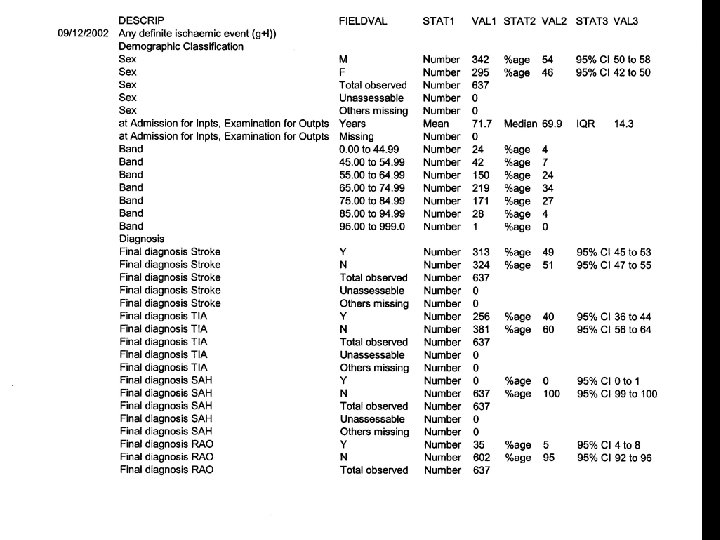
 Examples of Output from SSCAS Based on data collection in Lothian
Examples of Output from SSCAS Based on data collection in Lothian
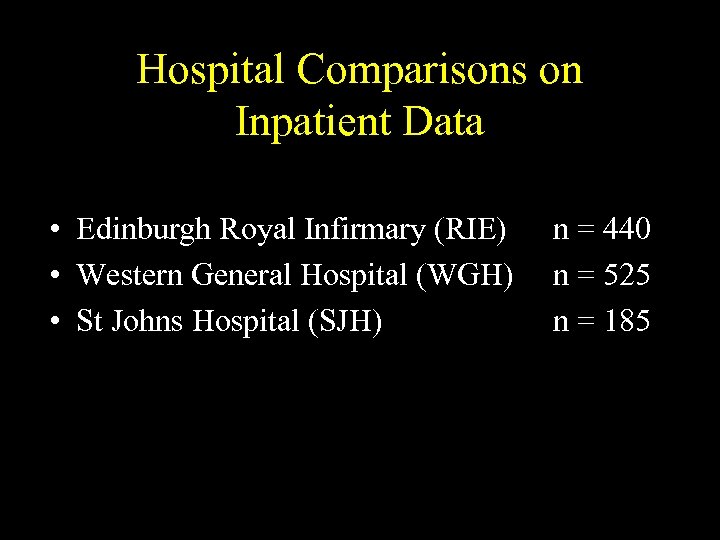 Hospital Comparisons on Inpatient Data • Edinburgh Royal Infirmary (RIE) • Western General Hospital (WGH) • St Johns Hospital (SJH) n = 440 n = 525 n = 185
Hospital Comparisons on Inpatient Data • Edinburgh Royal Infirmary (RIE) • Western General Hospital (WGH) • St Johns Hospital (SJH) n = 440 n = 525 n = 185
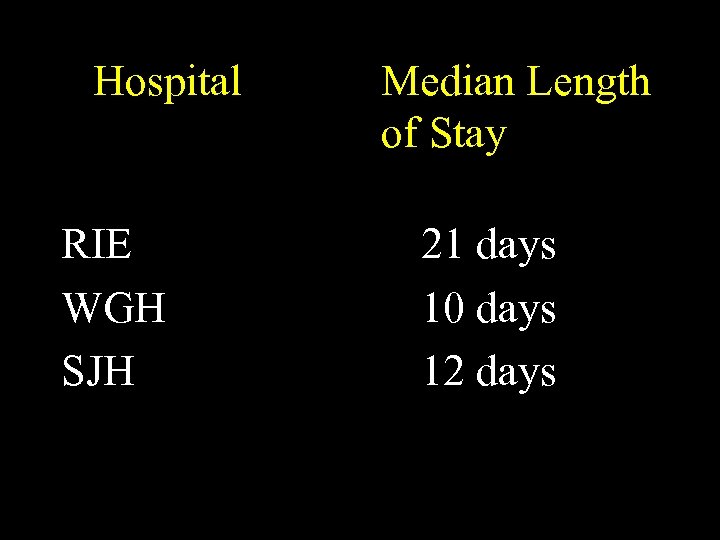 Hospital RIE WGH SJH Median Length of Stay 21 days 10 days 12 days
Hospital RIE WGH SJH Median Length of Stay 21 days 10 days 12 days
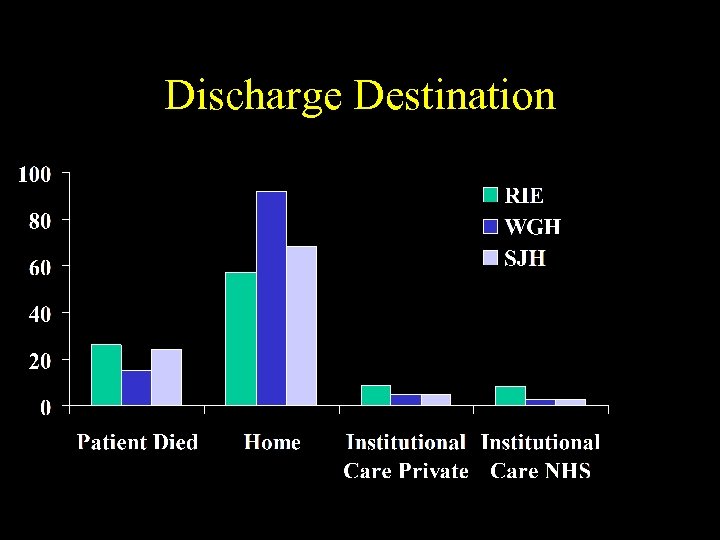 Discharge Destination
Discharge Destination
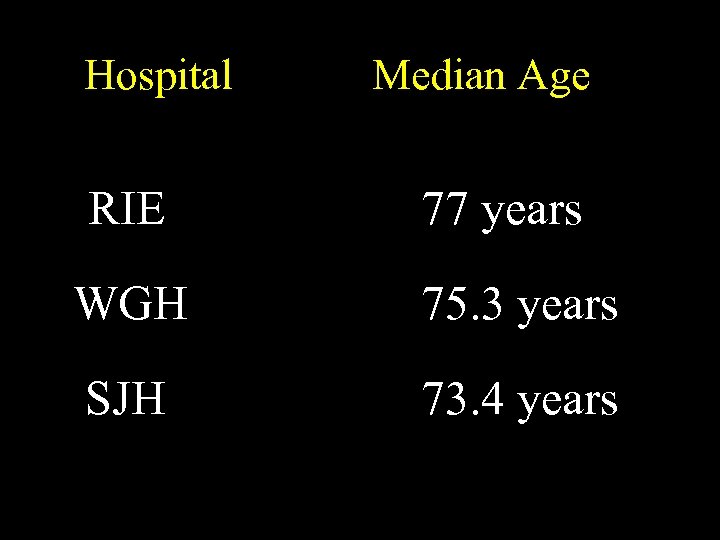 Hospital RIE Median Age 77 years WGH 75. 3 years SJH 73. 4 years
Hospital RIE Median Age 77 years WGH 75. 3 years SJH 73. 4 years
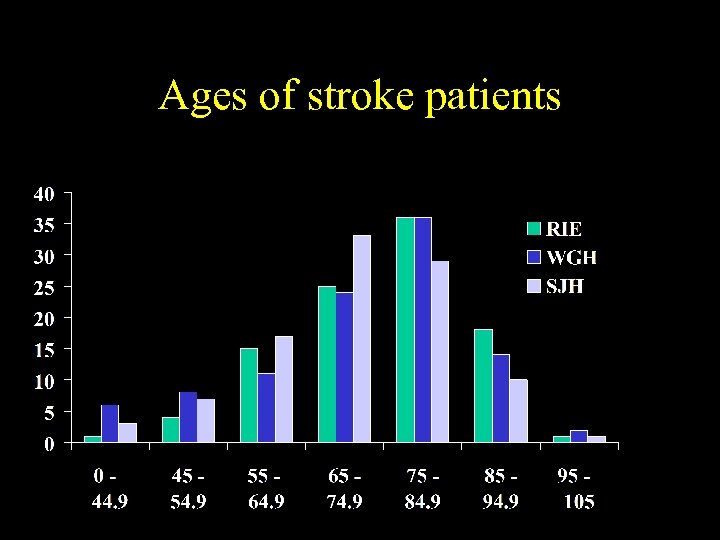 Ages of stroke patients
Ages of stroke patients
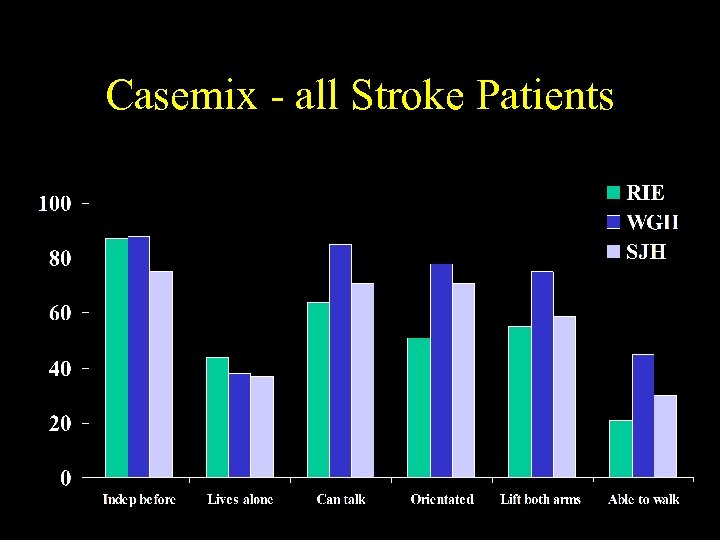 Casemix - all Stroke Patients
Casemix - all Stroke Patients
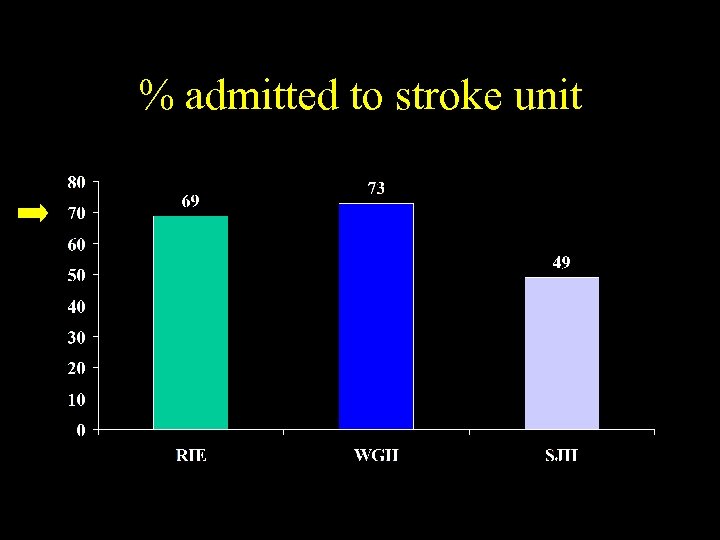 % admitted to stroke unit
% admitted to stroke unit
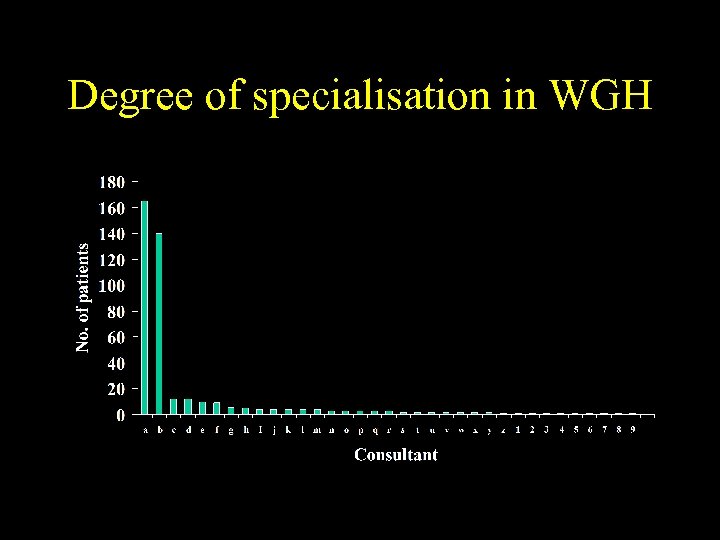 Degree of specialisation in WGH
Degree of specialisation in WGH
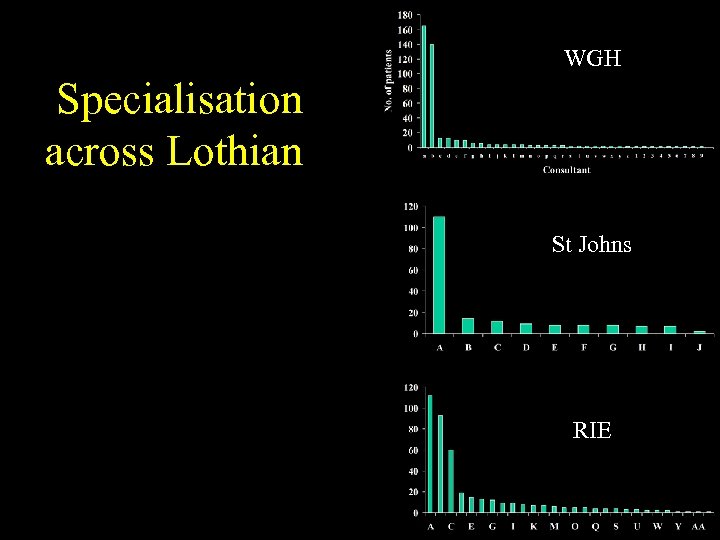 WGH Specialisation across Lothian St Johns RIE
WGH Specialisation across Lothian St Johns RIE
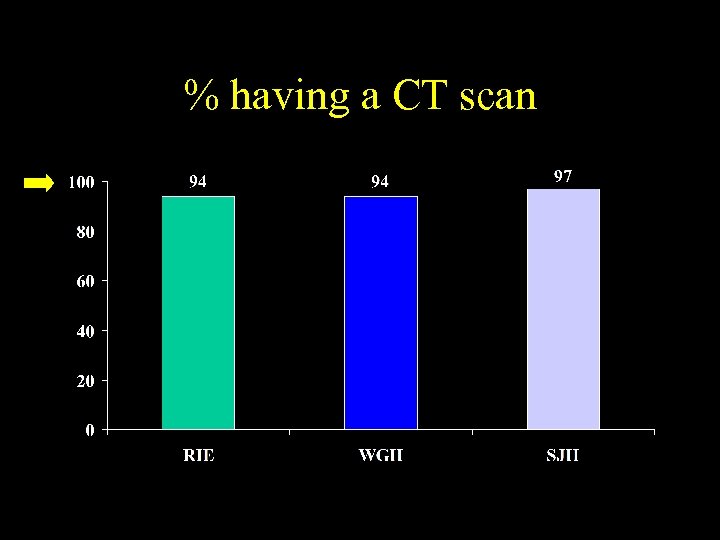 % having a CT scan
% having a CT scan
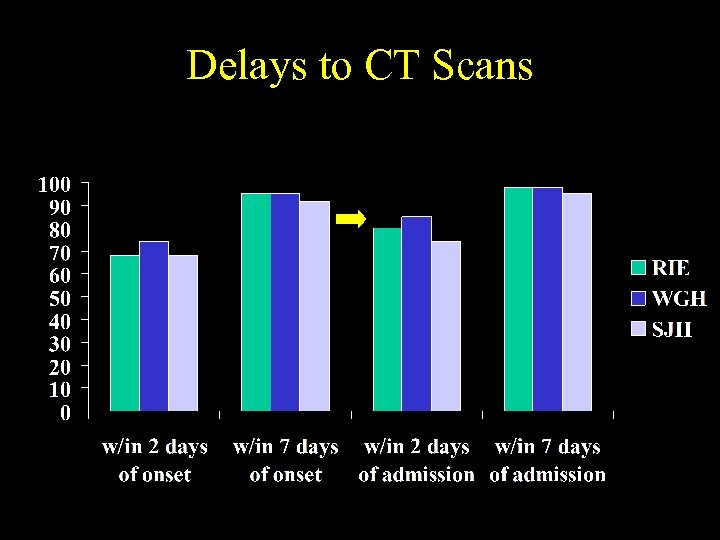 Delays to CT Scans
Delays to CT Scans
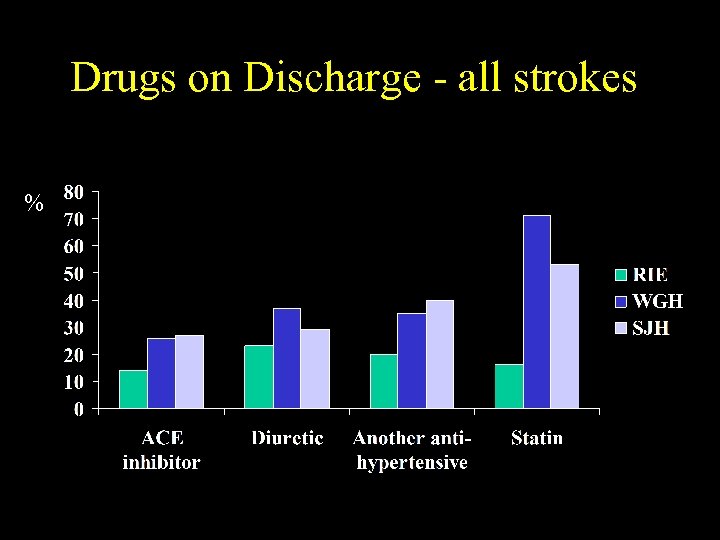 Drugs on Discharge - all strokes %
Drugs on Discharge - all strokes %
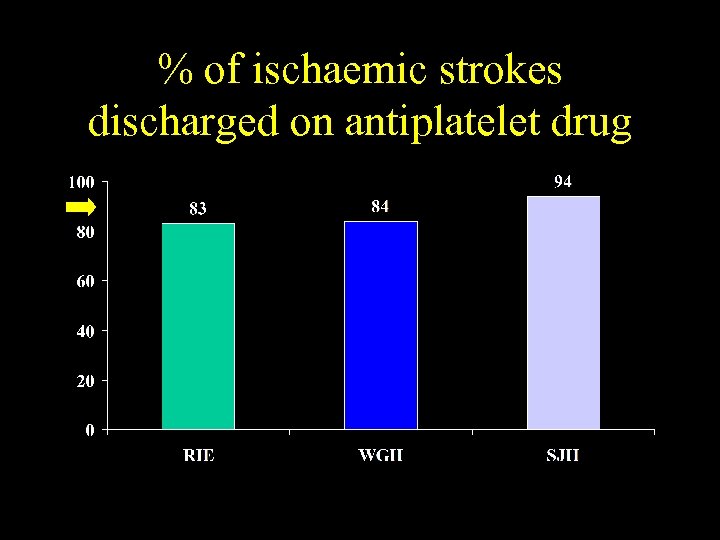 % of ischaemic strokes discharged on antiplatelet drug
% of ischaemic strokes discharged on antiplatelet drug
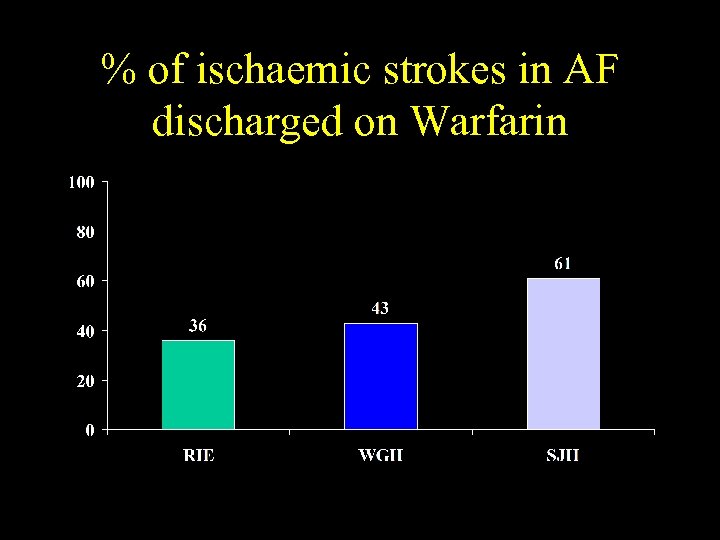 % of ischaemic strokes in AF discharged on Warfarin
% of ischaemic strokes in AF discharged on Warfarin
 Performance of WGH Neurovascular Clinic
Performance of WGH Neurovascular Clinic
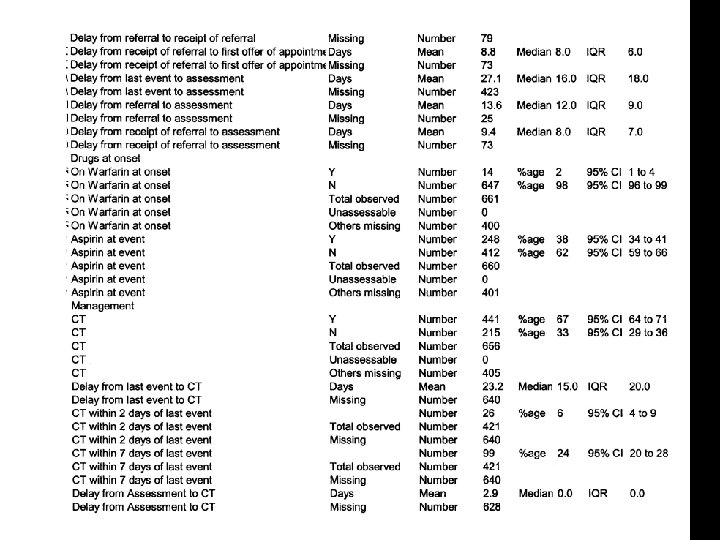
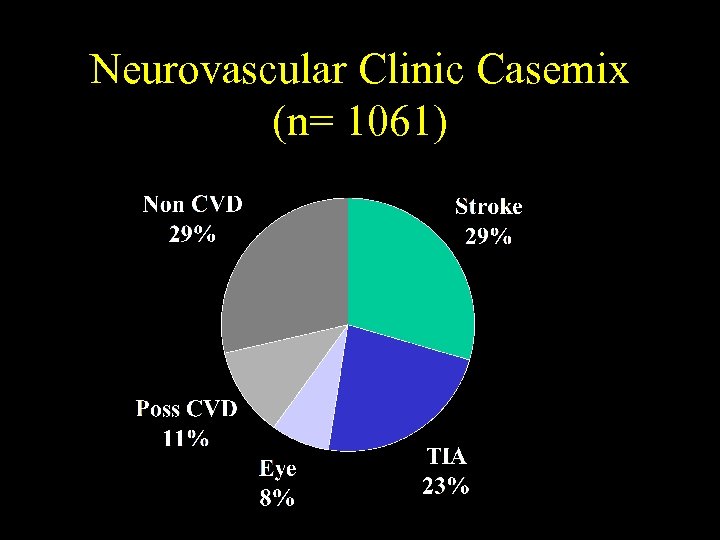 Neurovascular Clinic Casemix (n= 1061)
Neurovascular Clinic Casemix (n= 1061)
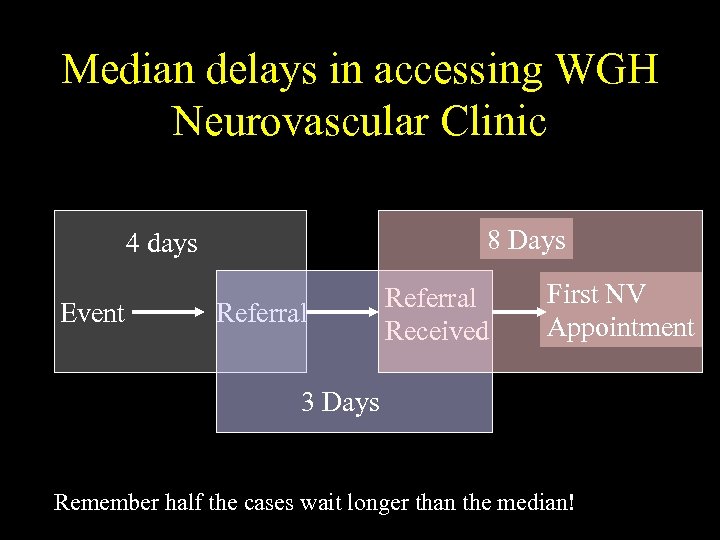 Median delays in accessing WGH Neurovascular Clinic 8 Days 4 days Event Referral Received First NV Appointment 3 Days Remember half the cases wait longer than the median!
Median delays in accessing WGH Neurovascular Clinic 8 Days 4 days Event Referral Received First NV Appointment 3 Days Remember half the cases wait longer than the median!
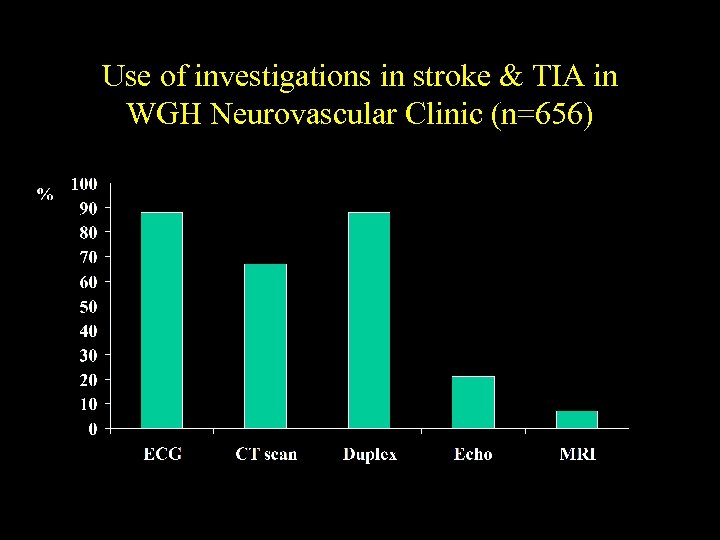 Use of investigations in stroke & TIA in WGH Neurovascular Clinic (n=656)
Use of investigations in stroke & TIA in WGH Neurovascular Clinic (n=656)
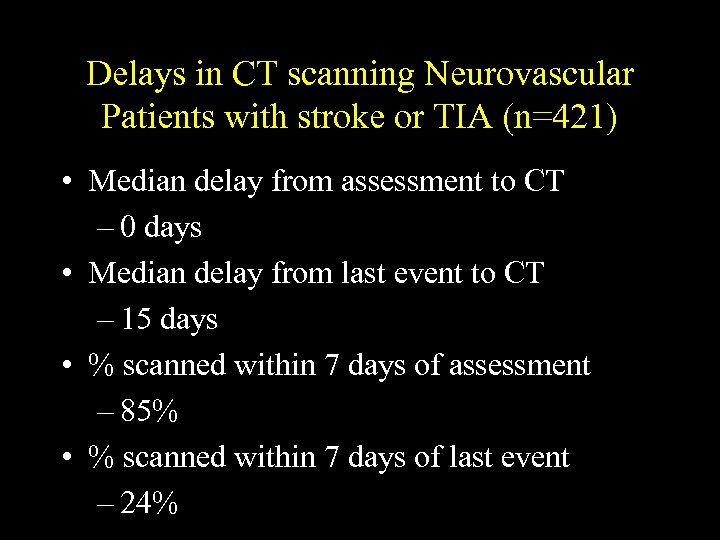 Delays in CT scanning Neurovascular Patients with stroke or TIA (n=421) • Median delay from assessment to CT – 0 days • Median delay from last event to CT – 15 days • % scanned within 7 days of assessment – 85% • % scanned within 7 days of last event – 24%
Delays in CT scanning Neurovascular Patients with stroke or TIA (n=421) • Median delay from assessment to CT – 0 days • Median delay from last event to CT – 15 days • % scanned within 7 days of assessment – 85% • % scanned within 7 days of last event – 24%
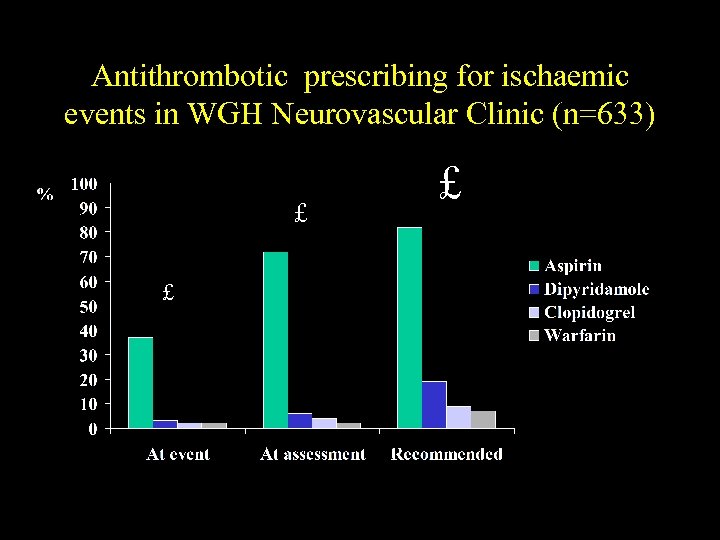 Antithrombotic prescribing for ischaemic events in WGH Neurovascular Clinic (n=633) £ £ £
Antithrombotic prescribing for ischaemic events in WGH Neurovascular Clinic (n=633) £ £ £
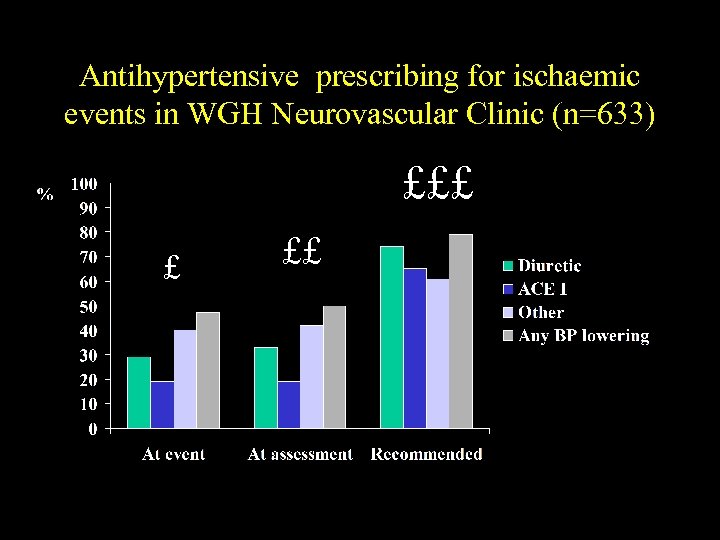 Antihypertensive prescribing for ischaemic events in WGH Neurovascular Clinic (n=633) £££ £ ££
Antihypertensive prescribing for ischaemic events in WGH Neurovascular Clinic (n=633) £££ £ ££
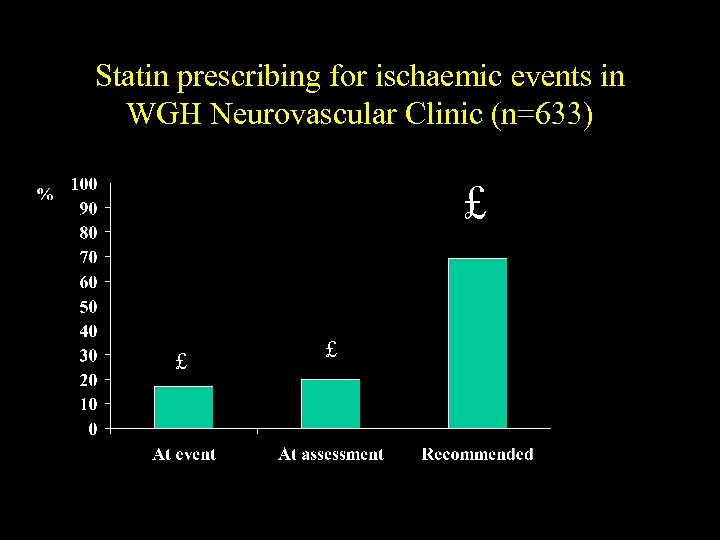 Statin prescribing for ischaemic events in WGH Neurovascular Clinic (n=633) £ £ £
Statin prescribing for ischaemic events in WGH Neurovascular Clinic (n=633) £ £ £
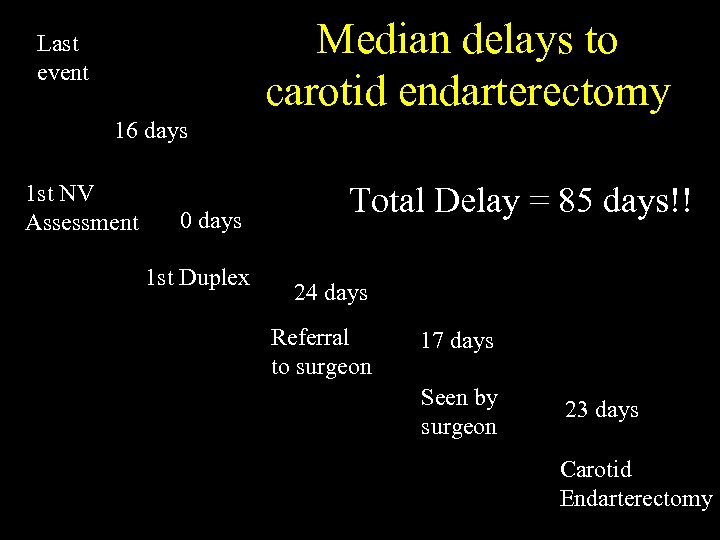 Median delays to carotid endarterectomy Last event 16 days 1 st NV Assessment 0 days 1 st Duplex Total Delay = 85 days!! 24 days Referral to surgeon 17 days Seen by surgeon 23 days Carotid Endarterectomy
Median delays to carotid endarterectomy Last event 16 days 1 st NV Assessment 0 days 1 st Duplex Total Delay = 85 days!! 24 days Referral to surgeon 17 days Seen by surgeon 23 days Carotid Endarterectomy
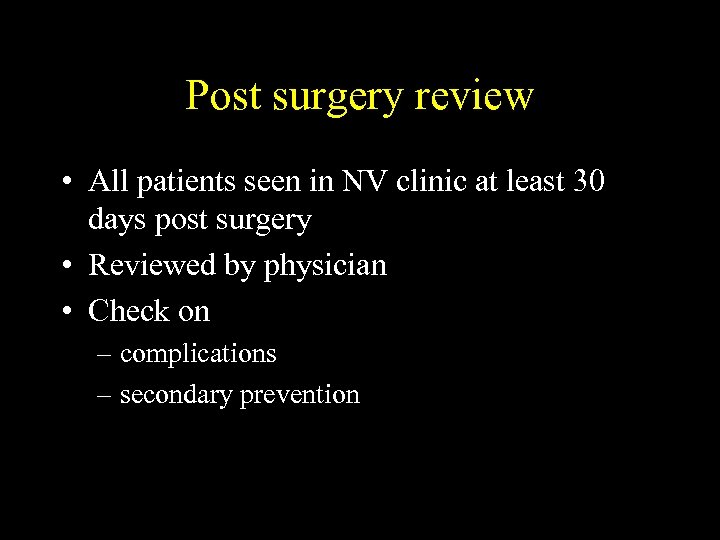 Post surgery review • All patients seen in NV clinic at least 30 days post surgery • Reviewed by physician • Check on – complications – secondary prevention
Post surgery review • All patients seen in NV clinic at least 30 days post surgery • Reviewed by physician • Check on – complications – secondary prevention
 Outpatient performance at WGH • Description of patients • Delays in – assessment – investigations – surgical assessment – operation • use of secondary prevention drugs • surgical complications
Outpatient performance at WGH • Description of patients • Delays in – assessment – investigations – surgical assessment – operation • use of secondary prevention drugs • surgical complications
 Any Comments or Questions?
Any Comments or Questions?
 Scottish Stroke Care Audit System
Scottish Stroke Care Audit System
 Progress • £ 512, 000 grant from the Scottish Executive over 3 years • Agreement in principal to involve STAG local co-ordinators • Co-ordinator - Robin Flaig • IT co-ordinator - Mike Mc. Dowall • £ 180, 000 for local support over 3 years
Progress • £ 512, 000 grant from the Scottish Executive over 3 years • Agreement in principal to involve STAG local co-ordinators • Co-ordinator - Robin Flaig • IT co-ordinator - Mike Mc. Dowall • £ 180, 000 for local support over 3 years
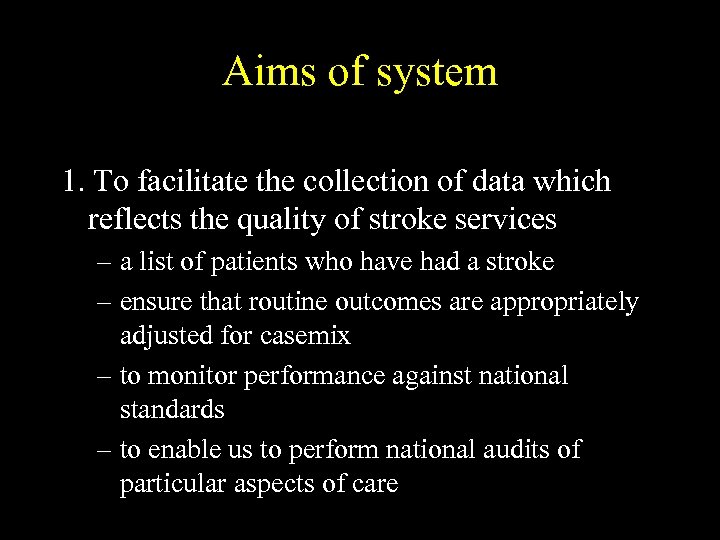 Aims of system 1. To facilitate the collection of data which reflects the quality of stroke services – a list of patients who have had a stroke – ensure that routine outcomes are appropriately adjusted for casemix – to monitor performance against national standards – to enable us to perform national audits of particular aspects of care
Aims of system 1. To facilitate the collection of data which reflects the quality of stroke services – a list of patients who have had a stroke – ensure that routine outcomes are appropriately adjusted for casemix – to monitor performance against national standards – to enable us to perform national audits of particular aspects of care
 Aims of system 2. To provide a tool to allow those running stroke service to collect data relevant to their service development and planning 3. To provide a database which can be expanded to meet the research needs of users
Aims of system 2. To provide a tool to allow those running stroke service to collect data relevant to their service development and planning 3. To provide a database which can be expanded to meet the research needs of users
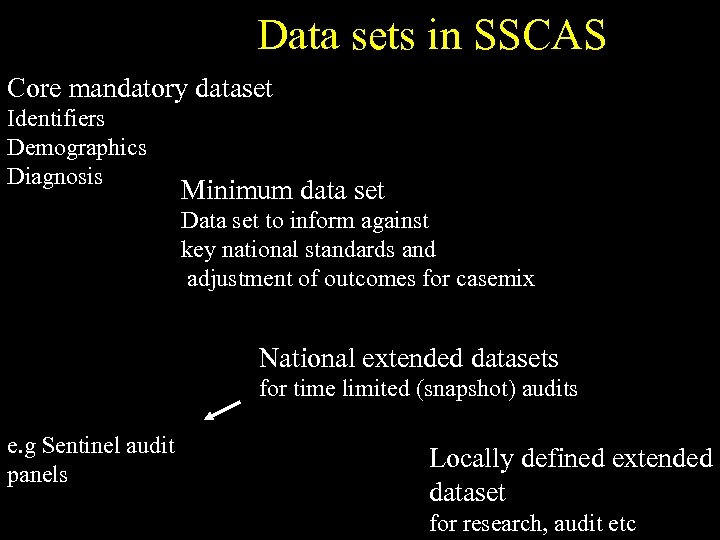 Data sets in SSCAS Core mandatory dataset Identifiers Demographics Diagnosis Minimum data set Data set to inform against key national standards and adjustment of outcomes for casemix National extended datasets for time limited (snapshot) audits e. g Sentinel audit panels Locally defined extended dataset for research, audit etc
Data sets in SSCAS Core mandatory dataset Identifiers Demographics Diagnosis Minimum data set Data set to inform against key national standards and adjustment of outcomes for casemix National extended datasets for time limited (snapshot) audits e. g Sentinel audit panels Locally defined extended dataset for research, audit etc
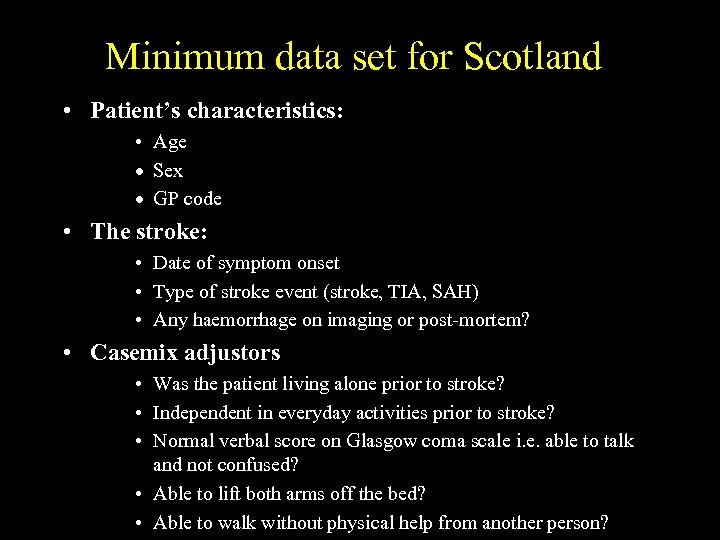 Minimum data set for Scotland • Patient’s characteristics: • Age · Sex · GP code • The stroke: • Date of symptom onset • Type of stroke event (stroke, TIA, SAH) • Any haemorrhage on imaging or post-mortem? • Casemix adjustors • Was the patient living alone prior to stroke? • Independent in everyday activities prior to stroke? • Normal verbal score on Glasgow coma scale i. e. able to talk and not confused? • Able to lift both arms off the bed? • Able to walk without physical help from another person?
Minimum data set for Scotland • Patient’s characteristics: • Age · Sex · GP code • The stroke: • Date of symptom onset • Type of stroke event (stroke, TIA, SAH) • Any haemorrhage on imaging or post-mortem? • Casemix adjustors • Was the patient living alone prior to stroke? • Independent in everyday activities prior to stroke? • Normal verbal score on Glasgow coma scale i. e. able to talk and not confused? • Able to lift both arms off the bed? • Able to walk without physical help from another person?
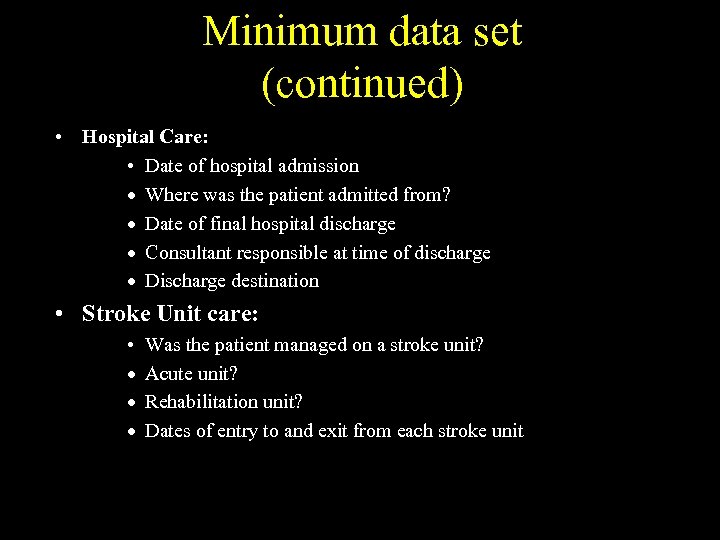 Minimum data set (continued) • Hospital Care: • Date of hospital admission · Where was the patient admitted from? · Date of final hospital discharge · Consultant responsible at time of discharge · Discharge destination • Stroke Unit care: • · · · Was the patient managed on a stroke unit? Acute unit? Rehabilitation unit? Dates of entry to and exit from each stroke unit
Minimum data set (continued) • Hospital Care: • Date of hospital admission · Where was the patient admitted from? · Date of final hospital discharge · Consultant responsible at time of discharge · Discharge destination • Stroke Unit care: • · · · Was the patient managed on a stroke unit? Acute unit? Rehabilitation unit? Dates of entry to and exit from each stroke unit
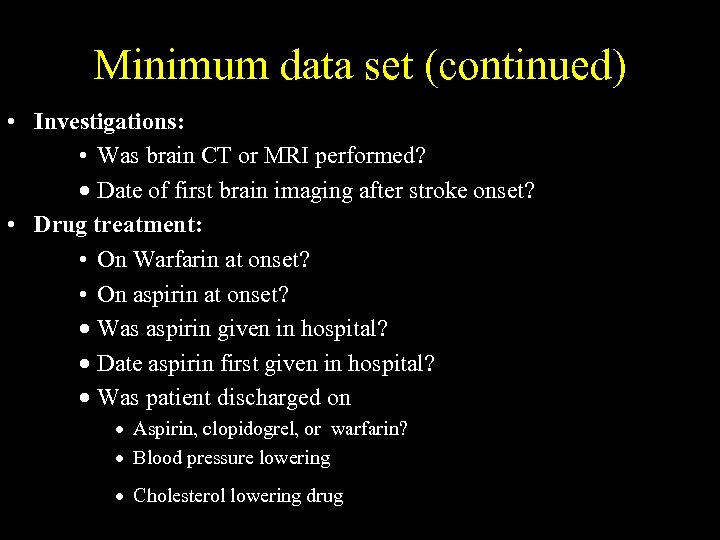 Minimum data set (continued) • Investigations: • Was brain CT or MRI performed? · Date of first brain imaging after stroke onset? • Drug treatment: • On Warfarin at onset? • On aspirin at onset? · Was aspirin given in hospital? · Date aspirin first given in hospital? · Was patient discharged on · Aspirin, clopidogrel, or warfarin? · Blood pressure lowering · Cholesterol lowering drug
Minimum data set (continued) • Investigations: • Was brain CT or MRI performed? · Date of first brain imaging after stroke onset? • Drug treatment: • On Warfarin at onset? • On aspirin at onset? · Was aspirin given in hospital? · Date aspirin first given in hospital? · Was patient discharged on · Aspirin, clopidogrel, or warfarin? · Blood pressure lowering · Cholesterol lowering drug
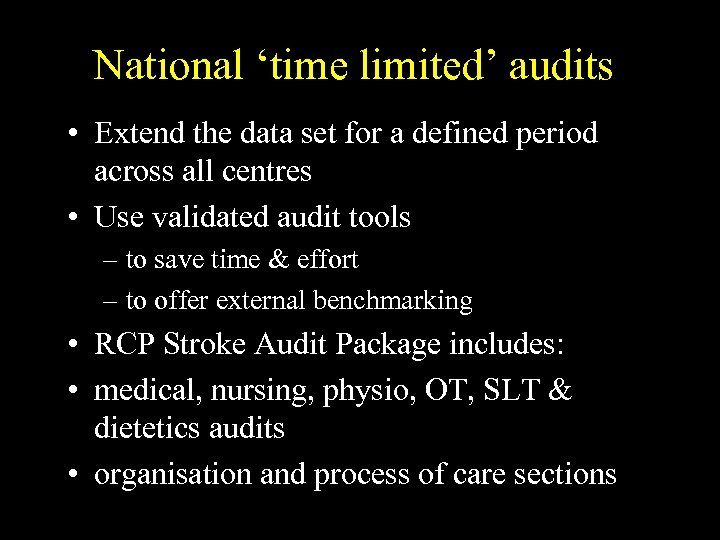 National ‘time limited’ audits • Extend the data set for a defined period across all centres • Use validated audit tools – to save time & effort – to offer external benchmarking • RCP Stroke Audit Package includes: • medical, nursing, physio, OT, SLT & dietetics audits • organisation and process of care sections
National ‘time limited’ audits • Extend the data set for a defined period across all centres • Use validated audit tools – to save time & effort – to offer external benchmarking • RCP Stroke Audit Package includes: • medical, nursing, physio, OT, SLT & dietetics audits • organisation and process of care sections
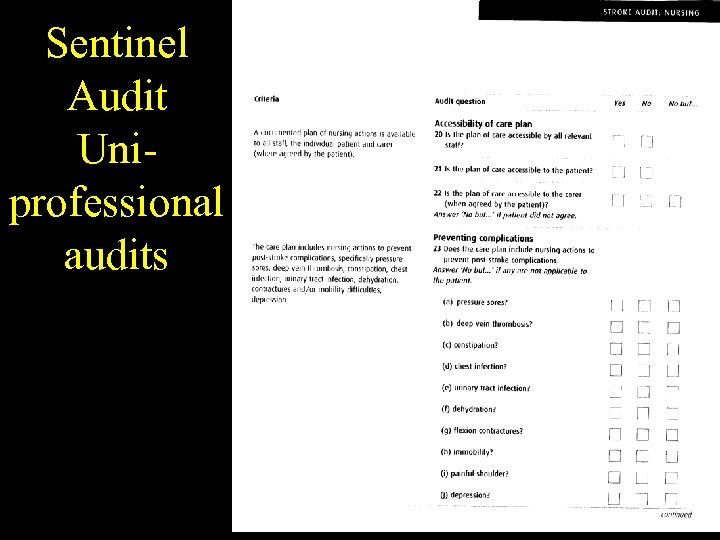 Sentinel Audit Uniprofessional audits
Sentinel Audit Uniprofessional audits
 Methods of capturing these data? • Extraction from – unstructured casenotes – clerking proforma – integrated care pathway – structured discharge summary – hospital information system – stroke register
Methods of capturing these data? • Extraction from – unstructured casenotes – clerking proforma – integrated care pathway – structured discharge summary – hospital information system – stroke register
 Other methods of data capture • Real time entry - but need to make data work • Possible to link discharge summary to database electronically?
Other methods of data capture • Real time entry - but need to make data work • Possible to link discharge summary to database electronically?
 How precise does ones measure of performance need to be? • To detect small differences – over time – between units • for example: – to confirm an increase in % given aspirin (50% to 80%) - 80 pts – to confirm an increase in % admitted to stroke unit (50% to 60%) -800 pts – to confirm a 4% absolute difference in mortality (24% to 20%) - 3400 pts
How precise does ones measure of performance need to be? • To detect small differences – over time – between units • for example: – to confirm an increase in % given aspirin (50% to 80%) - 80 pts – to confirm an increase in % admitted to stroke unit (50% to 60%) -800 pts – to confirm a 4% absolute difference in mortality (24% to 20%) - 3400 pts
 Consequences • Need continuous monitoring of some aspects of care to achieve sufficient numbers – e. g. % in stroke unit • Extended data collection for a few months where precision is less crucial
Consequences • Need continuous monitoring of some aspects of care to achieve sufficient numbers – e. g. % in stroke unit • Extended data collection for a few months where precision is less crucial
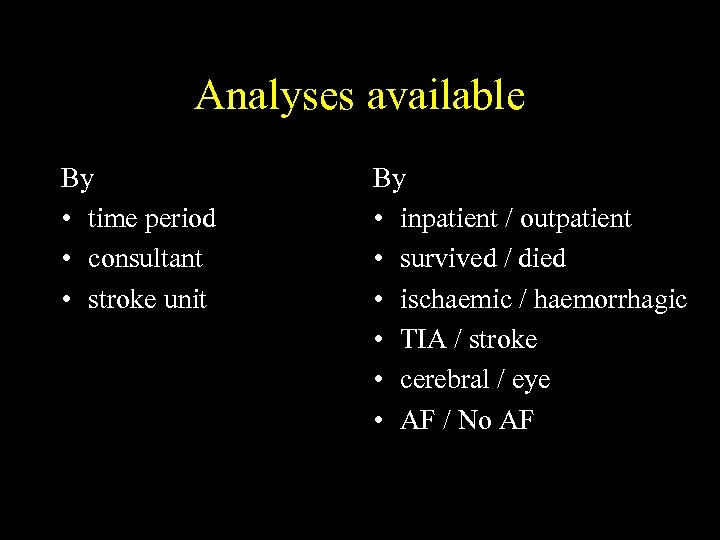 Analyses available By • time period • consultant • stroke unit By • inpatient / outpatient • survived / died • ischaemic / haemorrhagic • TIA / stroke • cerebral / eye • AF / No AF
Analyses available By • time period • consultant • stroke unit By • inpatient / outpatient • survived / died • ischaemic / haemorrhagic • TIA / stroke • cerebral / eye • AF / No AF
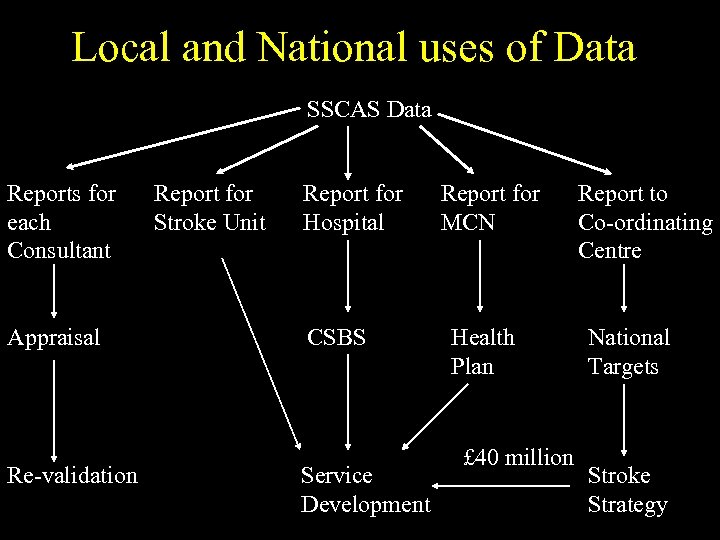 Local and National uses of Data SSCAS Data Reports for each Consultant Appraisal Re-validation Report for Stroke Unit Report for Hospital CSBS Service Development Report for MCN Health Plan £ 40 million Report to Co-ordinating Centre National Targets Stroke Strategy
Local and National uses of Data SSCAS Data Reports for each Consultant Appraisal Re-validation Report for Stroke Unit Report for Hospital CSBS Service Development Report for MCN Health Plan £ 40 million Report to Co-ordinating Centre National Targets Stroke Strategy
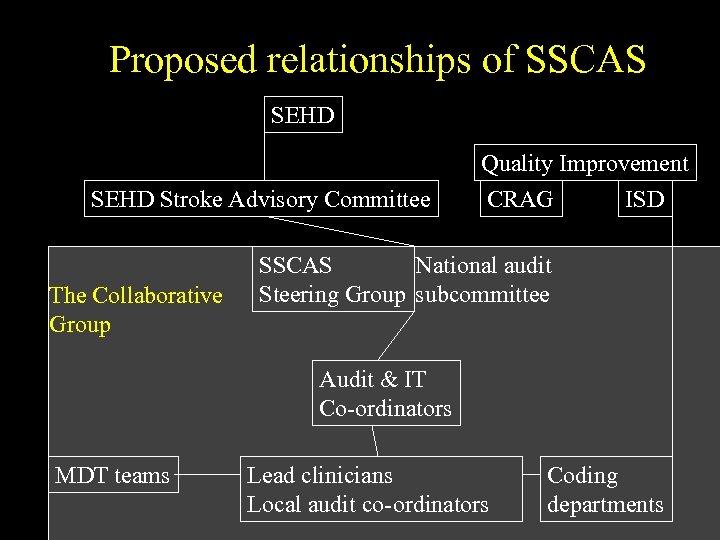 Proposed relationships of SSCAS SEHD Stroke Advisory Committee The Collaborative Group Quality Improvement CRAG ISD SSCAS National audit Steering Group subcommittee Audit & IT Co-ordinators MDT teams Lead clinicians Local audit co-ordinators Coding departments
Proposed relationships of SSCAS SEHD Stroke Advisory Committee The Collaborative Group Quality Improvement CRAG ISD SSCAS National audit Steering Group subcommittee Audit & IT Co-ordinators MDT teams Lead clinicians Local audit co-ordinators Coding departments
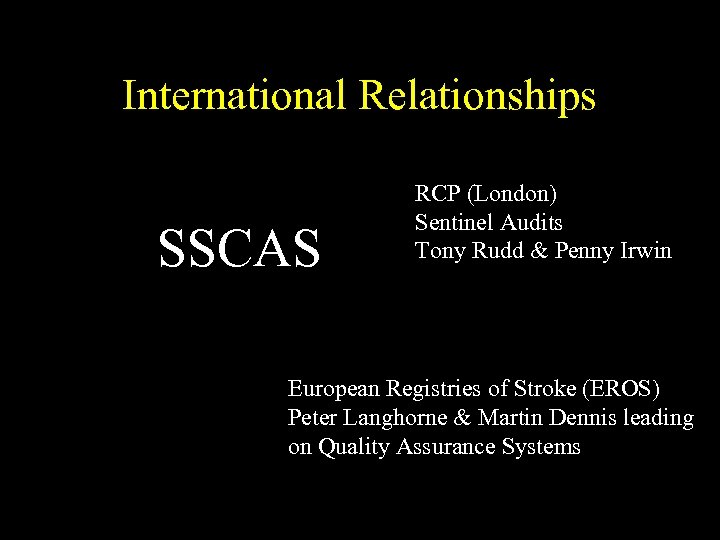 International Relationships SSCAS RCP (London) Sentinel Audits Tony Rudd & Penny Irwin European Registries of Stroke (EROS) Peter Langhorne & Martin Dennis leading on Quality Assurance Systems
International Relationships SSCAS RCP (London) Sentinel Audits Tony Rudd & Penny Irwin European Registries of Stroke (EROS) Peter Langhorne & Martin Dennis leading on Quality Assurance Systems
 Any Comments or Questions?
Any Comments or Questions?
 Who does what?
Who does what?
 Role of Steering group • Monitor progress of National Audit • Report back to Stroke Advisory Committee & funders • Set timetable for focused time limited audits involving an extended data set • Plan exit strategy
Role of Steering group • Monitor progress of National Audit • Report back to Stroke Advisory Committee & funders • Set timetable for focused time limited audits involving an extended data set • Plan exit strategy
 Role of Audit Co-ordinator Robin Flaig • Central Administration, including budget and organising meetings • Training people how to collect data, fill out forms and using SSCAS • Helpline for the centres • Generally there to help the centres with the audit • Produce National reports
Role of Audit Co-ordinator Robin Flaig • Central Administration, including budget and organising meetings • Training people how to collect data, fill out forms and using SSCAS • Helpline for the centres • Generally there to help the centres with the audit • Produce National reports
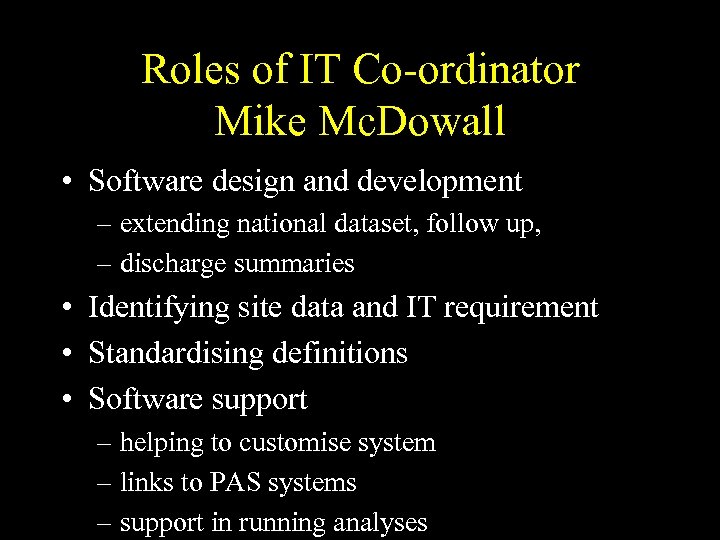 Roles of IT Co-ordinator Mike Mc. Dowall • Software design and development – extending national dataset, follow up, – discharge summaries • Identifying site data and IT requirement • Standardising definitions • Software support – helping to customise system – links to PAS systems – support in running analyses
Roles of IT Co-ordinator Mike Mc. Dowall • Software design and development – extending national dataset, follow up, – discharge summaries • Identifying site data and IT requirement • Standardising definitions • Software support – helping to customise system – links to PAS systems – support in running analyses
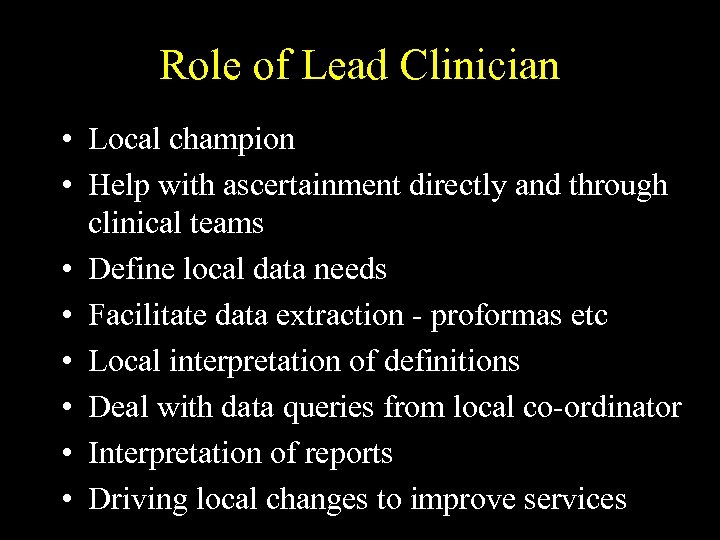 Role of Lead Clinician • Local champion • Help with ascertainment directly and through clinical teams • Define local data needs • Facilitate data extraction - proformas etc • Local interpretation of definitions • Deal with data queries from local co-ordinator • Interpretation of reports • Driving local changes to improve services
Role of Lead Clinician • Local champion • Help with ascertainment directly and through clinical teams • Define local data needs • Facilitate data extraction - proformas etc • Local interpretation of definitions • Deal with data queries from local co-ordinator • Interpretation of reports • Driving local changes to improve services
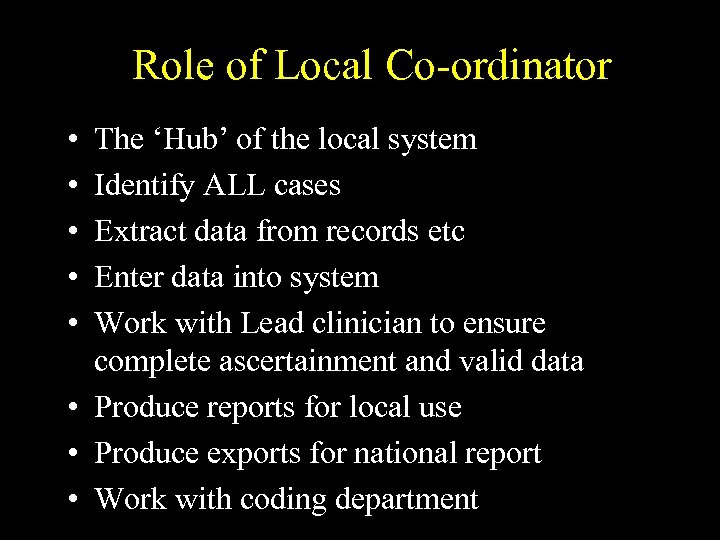 Role of Local Co-ordinator • • • The ‘Hub’ of the local system Identify ALL cases Extract data from records etc Enter data into system Work with Lead clinician to ensure complete ascertainment and valid data • Produce reports for local use • Produce exports for national report • Work with coding department
Role of Local Co-ordinator • • • The ‘Hub’ of the local system Identify ALL cases Extract data from records etc Enter data into system Work with Lead clinician to ensure complete ascertainment and valid data • Produce reports for local use • Produce exports for national report • Work with coding department
 Any Comments or Questions?
Any Comments or Questions?
 How to run SSCAS in your hospital
How to run SSCAS in your hospital
 Local Requirements • • lead clinician local co-ordinator with desk and chair PC, Windows 95 or higher printer Iomega ZIP drive external email (preferred) customised data collection forms
Local Requirements • • lead clinician local co-ordinator with desk and chair PC, Windows 95 or higher printer Iomega ZIP drive external email (preferred) customised data collection forms
 Ethics & consent • SSCAS has MREC approval • No need to LREC applications unless adding on research studies • No need for explicit consent for in-hospital data collection • Consent for follow up obtained at time of follow up • Trusts have a responsibility to make patients aware of uses data are put to • We can provide examples of patient information leaflets approved by MREC
Ethics & consent • SSCAS has MREC approval • No need to LREC applications unless adding on research studies • No need for explicit consent for in-hospital data collection • Consent for follow up obtained at time of follow up • Trusts have a responsibility to make patients aware of uses data are put to • We can provide examples of patient information leaflets approved by MREC
 Confidentiality • Data forms should be stored in locked filing cabinet • Computers should be password protected • Staff should have signed confidentiality agreements • Data should not be passed to others who are not involved with the project without agreement • Never leave unsecured data unattended
Confidentiality • Data forms should be stored in locked filing cabinet • Computers should be password protected • Staff should have signed confidentiality agreements • Data should not be passed to others who are not involved with the project without agreement • Never leave unsecured data unattended
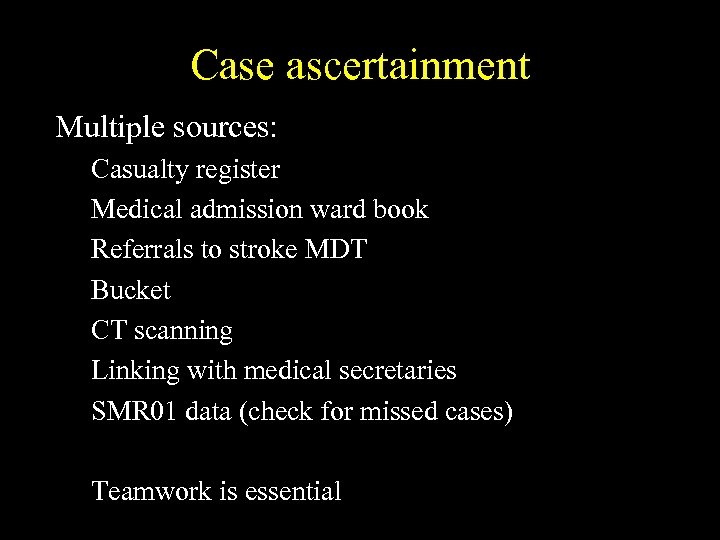 Case ascertainment Multiple sources: Casualty register Medical admission ward book Referrals to stroke MDT Bucket CT scanning Linking with medical secretaries SMR 01 data (check for missed cases) Teamwork is essential
Case ascertainment Multiple sources: Casualty register Medical admission ward book Referrals to stroke MDT Bucket CT scanning Linking with medical secretaries SMR 01 data (check for missed cases) Teamwork is essential
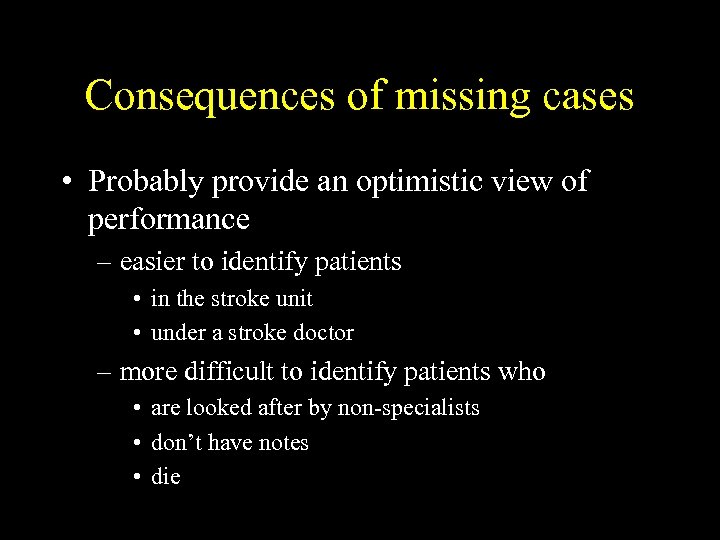 Consequences of missing cases • Probably provide an optimistic view of performance – easier to identify patients • in the stroke unit • under a stroke doctor – more difficult to identify patients who • are looked after by non-specialists • don’t have notes • die
Consequences of missing cases • Probably provide an optimistic view of performance – easier to identify patients • in the stroke unit • under a stroke doctor – more difficult to identify patients who • are looked after by non-specialists • don’t have notes • die
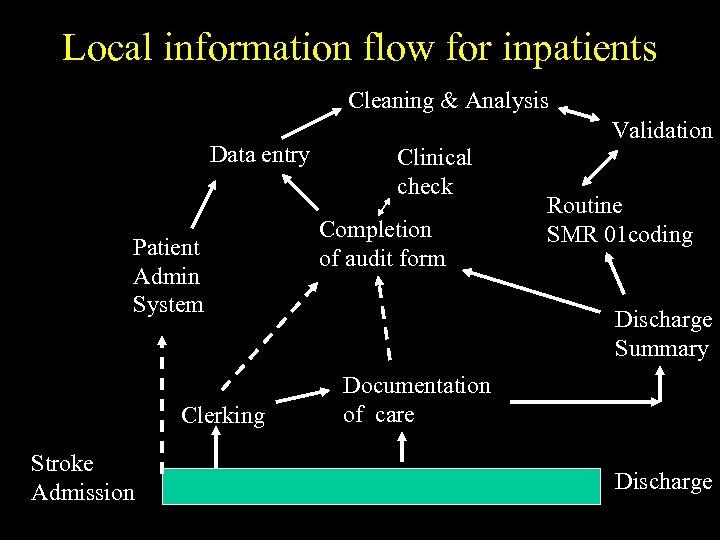 Local information flow for inpatients Cleaning & Analysis Data entry Patient Admin System Clerking Stroke Admission Validation Clinical check Completion of audit form Routine SMR 01 coding Discharge Summary Documentation of care Discharge
Local information flow for inpatients Cleaning & Analysis Data entry Patient Admin System Clerking Stroke Admission Validation Clinical check Completion of audit form Routine SMR 01 coding Discharge Summary Documentation of care Discharge
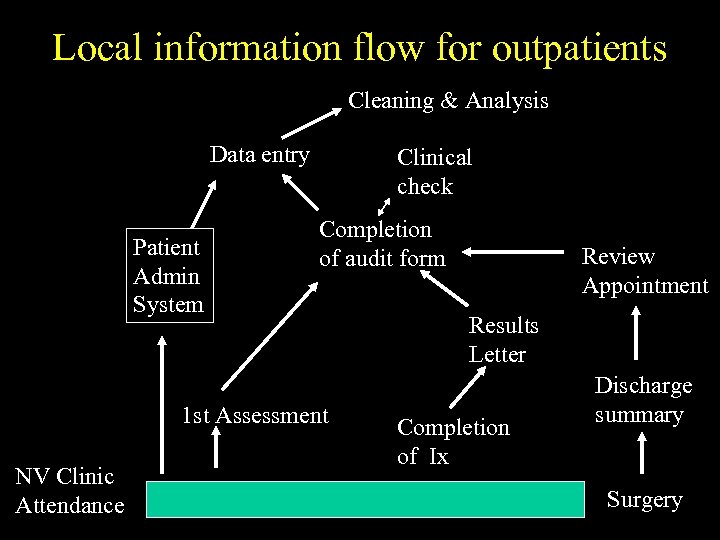 Local information flow for outpatients Cleaning & Analysis Data entry Patient Admin System Clinical check Completion of audit form 1 st Assessment NV Clinic Attendance Review Appointment Results Letter Completion of Ix Discharge summary Surgery
Local information flow for outpatients Cleaning & Analysis Data entry Patient Admin System Clinical check Completion of audit form 1 st Assessment NV Clinic Attendance Review Appointment Results Letter Completion of Ix Discharge summary Surgery
 Data Capture Facilitated by: Single point of admission Clerking proforma Single point for stroke referral Structured records Structured discharge summary Link to PAS
Data Capture Facilitated by: Single point of admission Clerking proforma Single point for stroke referral Structured records Structured discharge summary Link to PAS
 Aims of linking with coding departments • Ensure fuller case ascertainment in SSCAS • Improve accuracy of SMR 01 data • Explore possibilities of collecting data for audit in extended COPPISH dataset
Aims of linking with coding departments • Ensure fuller case ascertainment in SSCAS • Improve accuracy of SMR 01 data • Explore possibilities of collecting data for audit in extended COPPISH dataset
 Any Comments or Questions?
Any Comments or Questions?
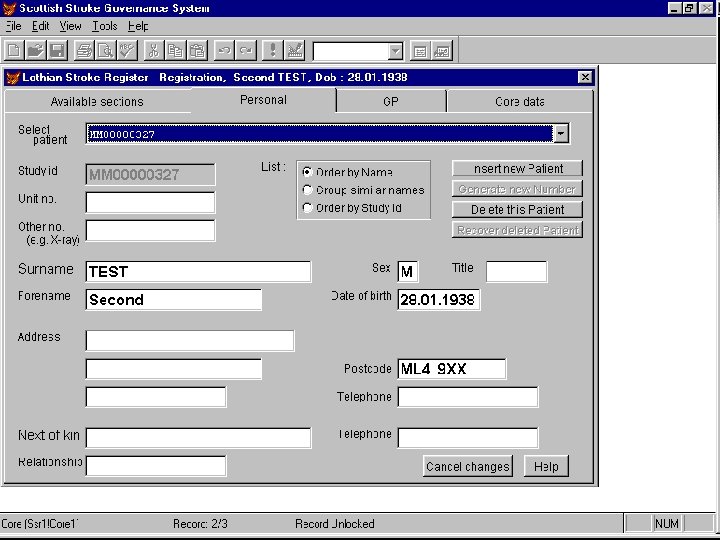
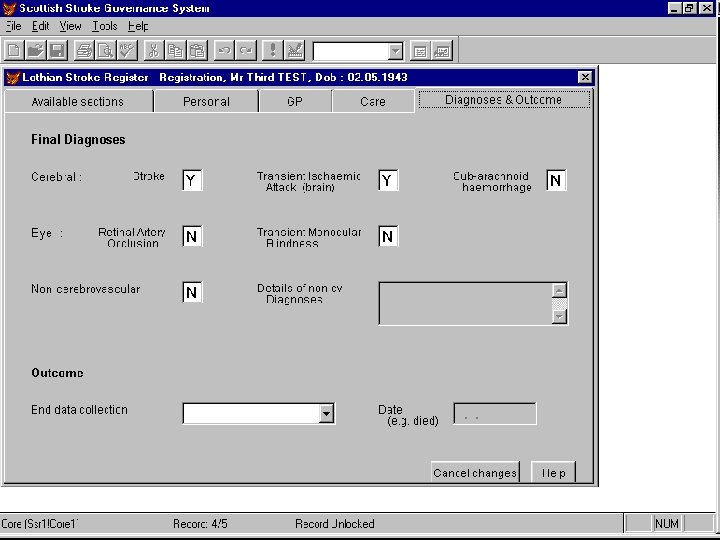
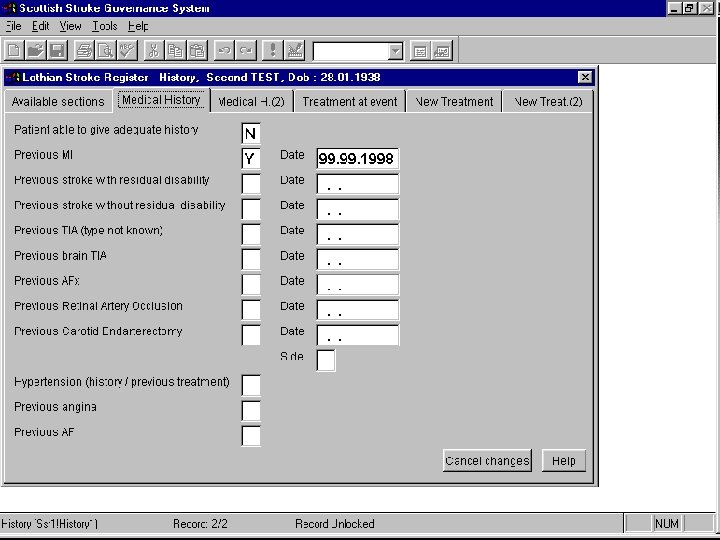
 Live demonstration of data entry and report generation Mike Mc. Dowall
Live demonstration of data entry and report generation Mike Mc. Dowall
 Any Comments or Questions?
Any Comments or Questions?
 For those with existing register Options • switch to using SSCAS software – possible to transfer old data into SSCAS • modify own software and data sets but vital to use common – definitions – methods of calculating performance
For those with existing register Options • switch to using SSCAS software – possible to transfer old data into SSCAS • modify own software and data sets but vital to use common – definitions – methods of calculating performance
 Exports from SSCAS • • Can be anonymised Produce standard reports Planning to produce Summary reports Data formatted to be imported into – Microsoft Access or Excel – Standard statistical packages
Exports from SSCAS • • Can be anonymised Produce standard reports Planning to produce Summary reports Data formatted to be imported into – Microsoft Access or Excel – Standard statistical packages
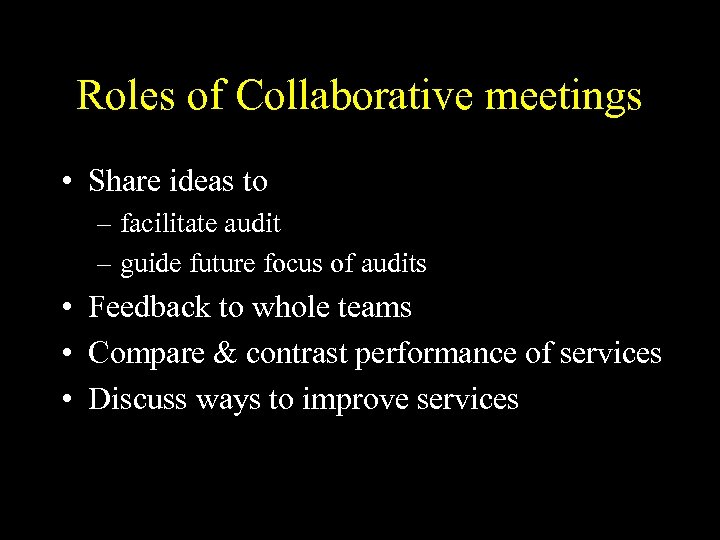 Roles of Collaborative meetings • Share ideas to – facilitate audit – guide future focus of audits • Feedback to whole teams • Compare & contrast performance of services • Discuss ways to improve services
Roles of Collaborative meetings • Share ideas to – facilitate audit – guide future focus of audits • Feedback to whole teams • Compare & contrast performance of services • Discuss ways to improve services
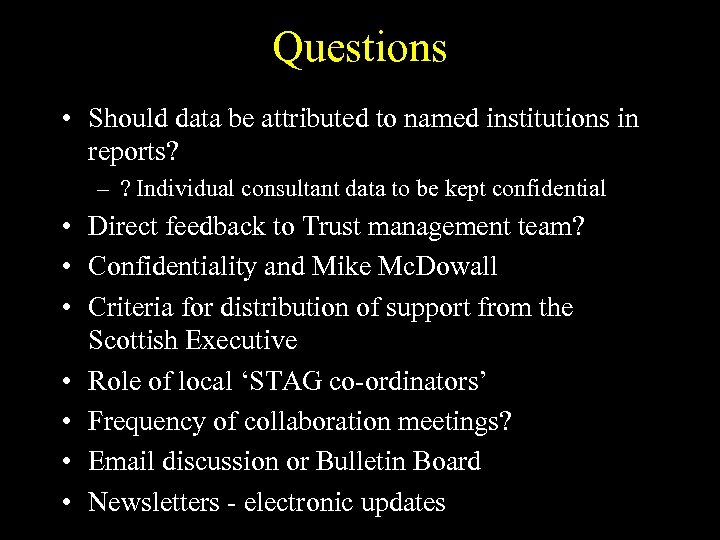 Questions • Should data be attributed to named institutions in reports? – ? Individual consultant data to be kept confidential • Direct feedback to Trust management team? • Confidentiality and Mike Mc. Dowall • Criteria for distribution of support from the Scottish Executive • Role of local ‘STAG co-ordinators’ • Frequency of collaboration meetings? • Email discussion or Bulletin Board • Newsletters - electronic updates
Questions • Should data be attributed to named institutions in reports? – ? Individual consultant data to be kept confidential • Direct feedback to Trust management team? • Confidentiality and Mike Mc. Dowall • Criteria for distribution of support from the Scottish Executive • Role of local ‘STAG co-ordinators’ • Frequency of collaboration meetings? • Email discussion or Bulletin Board • Newsletters - electronic updates
 Plan • Lead clinicians need to pull together resources needed • Let Robin know what you need from us
Plan • Lead clinicians need to pull together resources needed • Let Robin know what you need from us
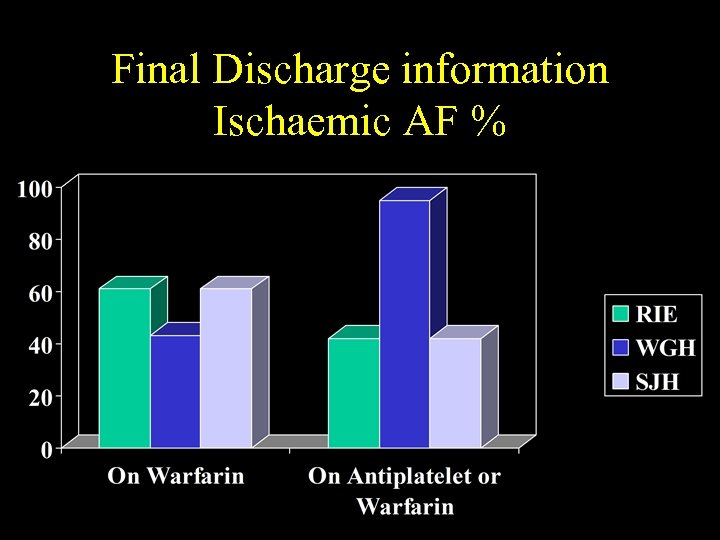 Final Discharge information Ischaemic AF %
Final Discharge information Ischaemic AF %
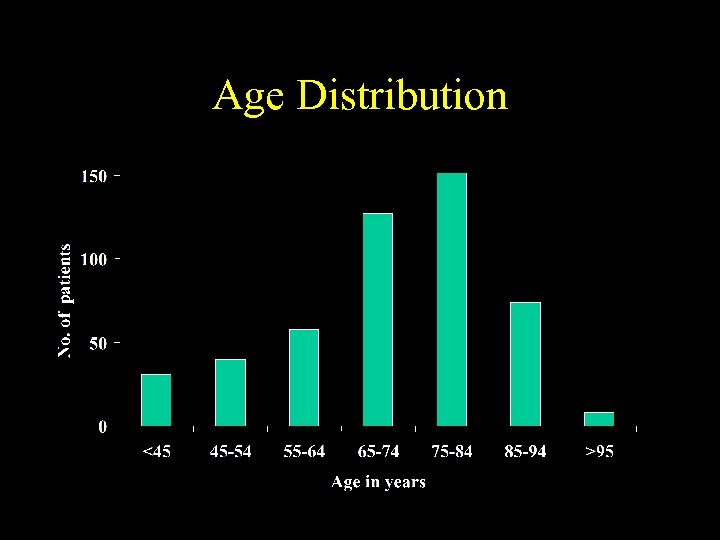 Age Distribution
Age Distribution
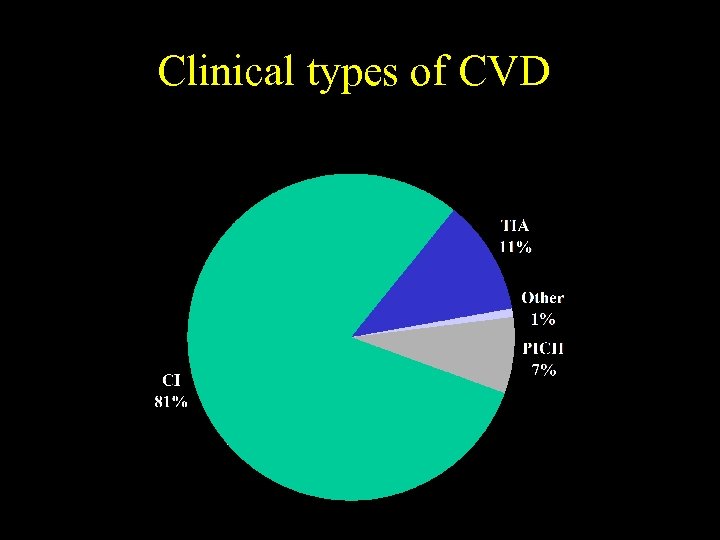 Clinical types of CVD
Clinical types of CVD
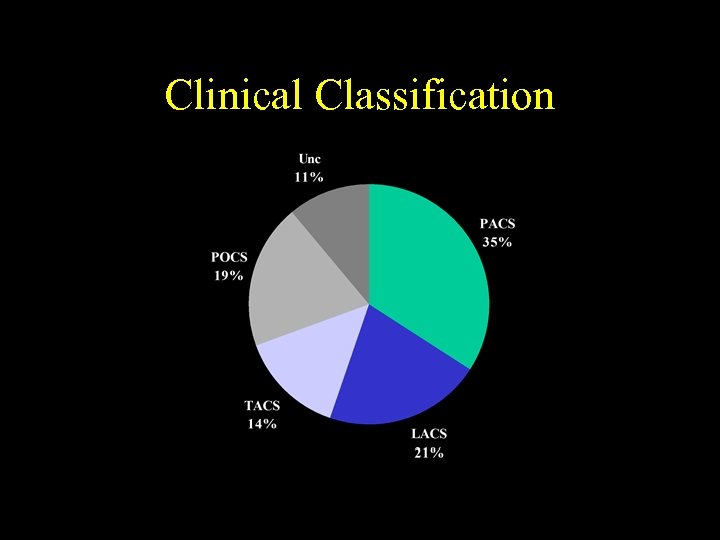 Clinical Classification
Clinical Classification
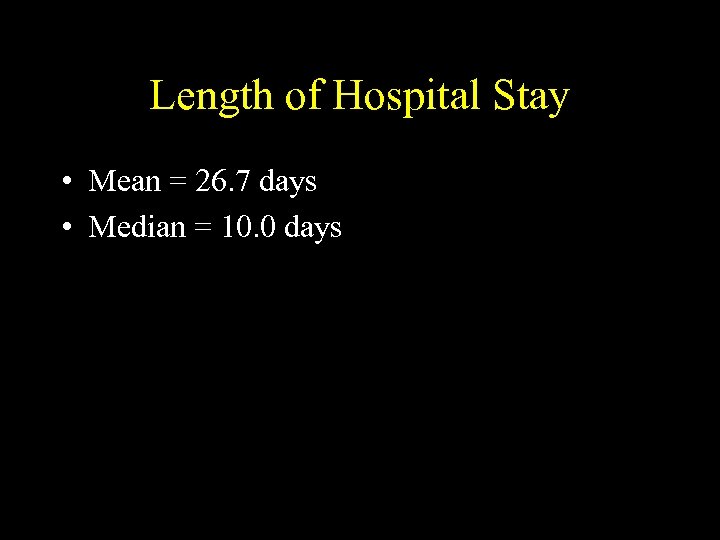 Length of Hospital Stay • Mean = 26. 7 days • Median = 10. 0 days
Length of Hospital Stay • Mean = 26. 7 days • Median = 10. 0 days
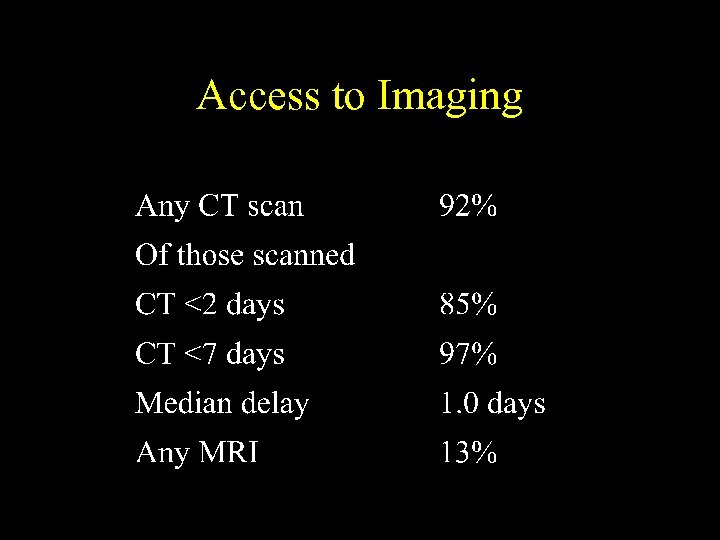 Access to Imaging
Access to Imaging
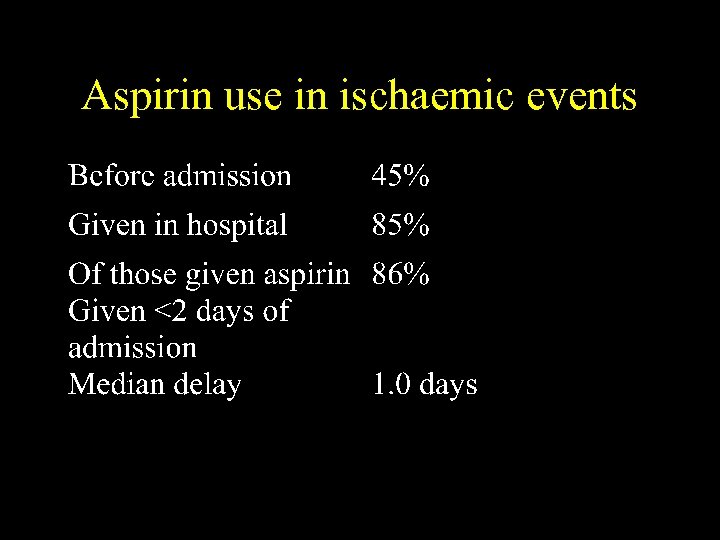 Aspirin use in ischaemic events
Aspirin use in ischaemic events
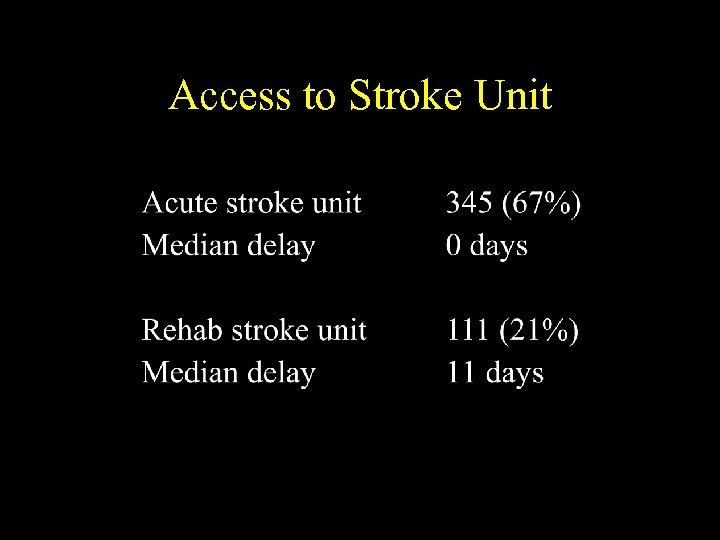 Access to Stroke Unit
Access to Stroke Unit
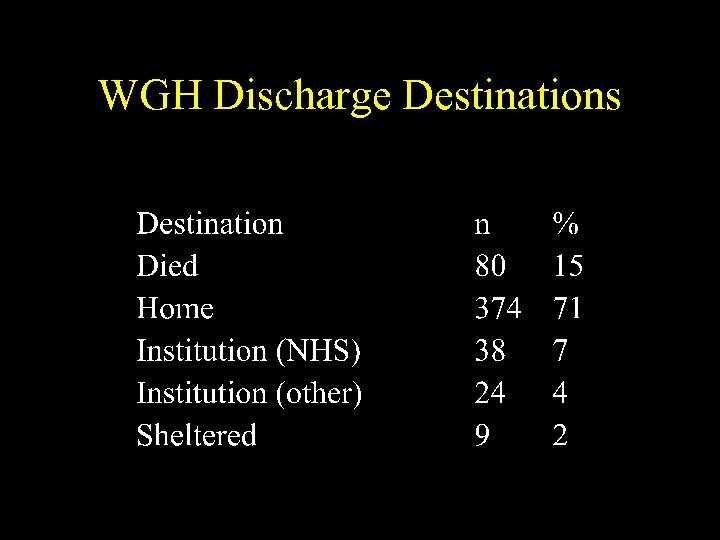 WGH Discharge Destinations
WGH Discharge Destinations
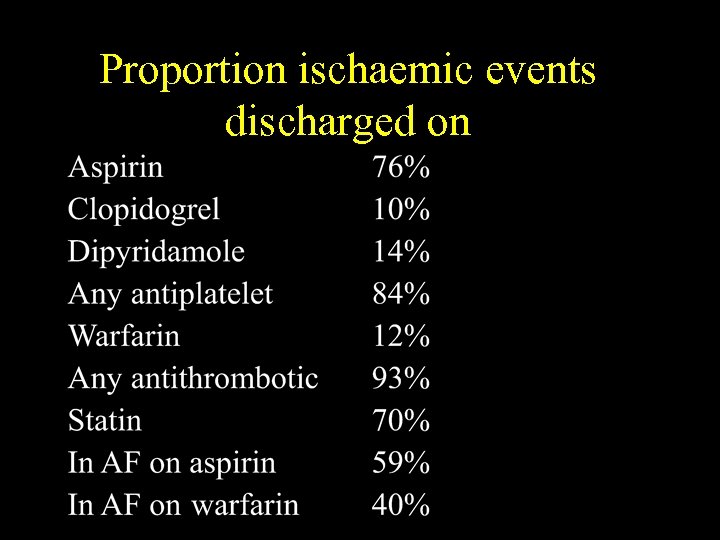 Proportion ischaemic events discharged on
Proportion ischaemic events discharged on
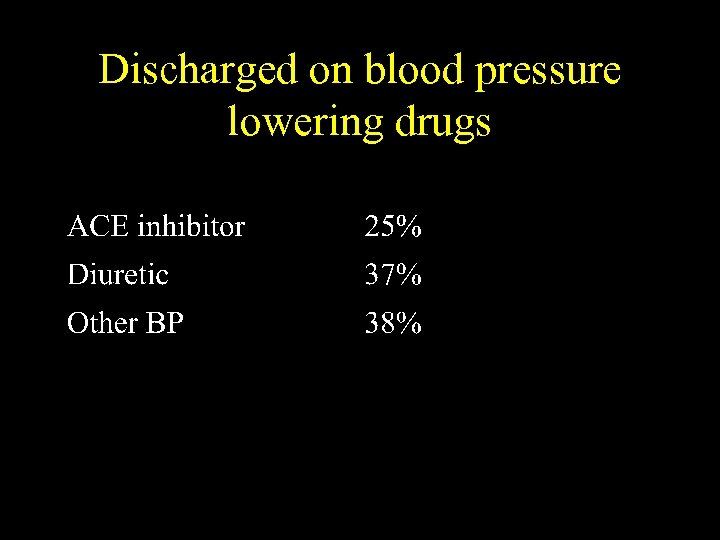 Discharged on blood pressure lowering drugs
Discharged on blood pressure lowering drugs


