a45b7a4119d03057300228d111fdc86e.ppt
- Количество слайдов: 30
 Welcome Ask The Experts March 24 -27, 2007 New Orleans, LA
Welcome Ask The Experts March 24 -27, 2007 New Orleans, LA
 Incorporating Patient Risk into Decisions Regarding the Optimal Reperfusion Strategy for ST Elevation MI Duane S. Pinto, MD Assistant Professor of Medicine Harvard Medical School Director, Cardiology Fellowship Training Program Beth Israel Deaconess Medical Center Boston, MA
Incorporating Patient Risk into Decisions Regarding the Optimal Reperfusion Strategy for ST Elevation MI Duane S. Pinto, MD Assistant Professor of Medicine Harvard Medical School Director, Cardiology Fellowship Training Program Beth Israel Deaconess Medical Center Boston, MA
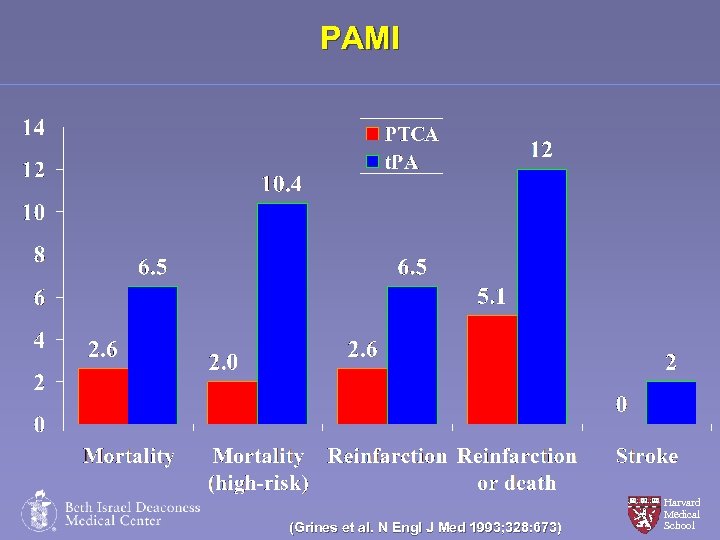 PAMI (Grines et al. N Engl J Med 1993; 328: 673) Harvard Medical School
PAMI (Grines et al. N Engl J Med 1993; 328: 673) Harvard Medical School
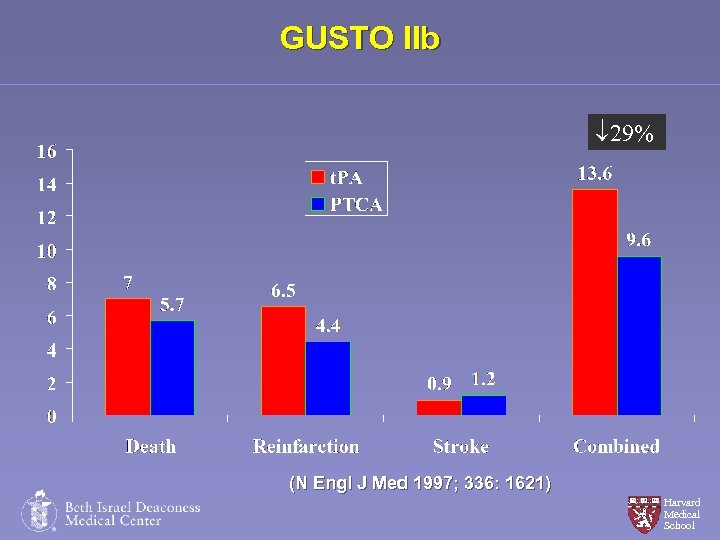 GUSTO IIb 29% (N Engl J Med 1997; 336: 1621) Harvard Medical School
GUSTO IIb 29% (N Engl J Med 1997; 336: 1621) Harvard Medical School
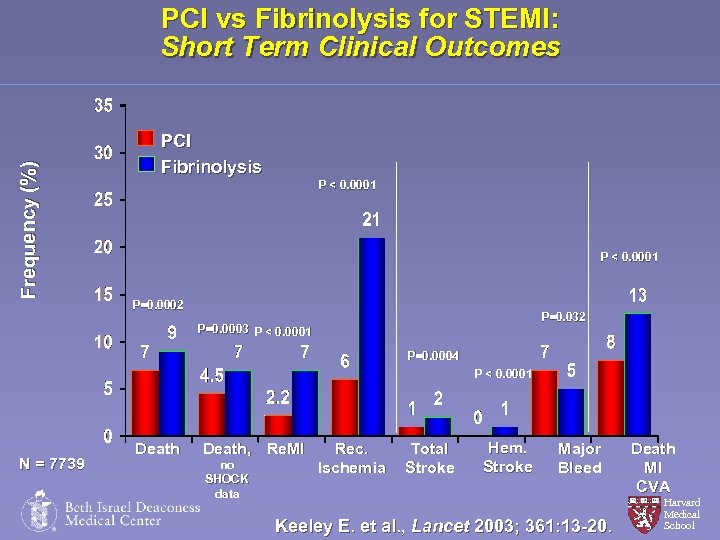 Frequency (%) PCI vs Fibrinolysis for STEMI: Short Term Clinical Outcomes PCI Fibrinolysis P < 0. 0001 P=0. 0002 P=0. 032 P=0. 0003 P < 0. 0001 P=0. 0004 P < 0. 0001 N = 7739 Death, Re. MI no SHOCK data Rec. Ischemia Total Stroke Hem. Stroke Major Bleed Keeley E. et al. , Lancet 2003; 361: 13 -20. Death MI CVA Harvard Medical School
Frequency (%) PCI vs Fibrinolysis for STEMI: Short Term Clinical Outcomes PCI Fibrinolysis P < 0. 0001 P=0. 0002 P=0. 032 P=0. 0003 P < 0. 0001 P=0. 0004 P < 0. 0001 N = 7739 Death, Re. MI no SHOCK data Rec. Ischemia Total Stroke Hem. Stroke Major Bleed Keeley E. et al. , Lancet 2003; 361: 13 -20. Death MI CVA Harvard Medical School
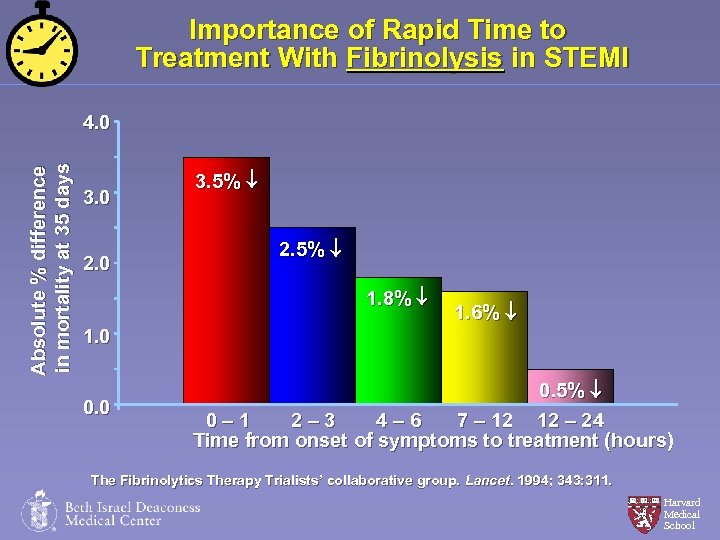 Importance of Rapid Time to Treatment With Fibrinolysis in STEMI Absolute % difference in mortality at 35 days 4. 0 3. 0 2. 0 3. 5% ¯ 2. 5% ¯ 1. 8% ¯ 1. 6% ¯ 1. 0 0. 5% ¯ 0– 1 2– 3 4– 6 7 – 12 12 – 24 Time from onset of symptoms to treatment (hours) The Fibrinolytics Therapy Trialists’ collaborative group. Lancet. 1994; 343: 311. Harvard Medical School
Importance of Rapid Time to Treatment With Fibrinolysis in STEMI Absolute % difference in mortality at 35 days 4. 0 3. 0 2. 0 3. 5% ¯ 2. 5% ¯ 1. 8% ¯ 1. 6% ¯ 1. 0 0. 5% ¯ 0– 1 2– 3 4– 6 7 – 12 12 – 24 Time from onset of symptoms to treatment (hours) The Fibrinolytics Therapy Trialists’ collaborative group. Lancet. 1994; 343: 311. Harvard Medical School
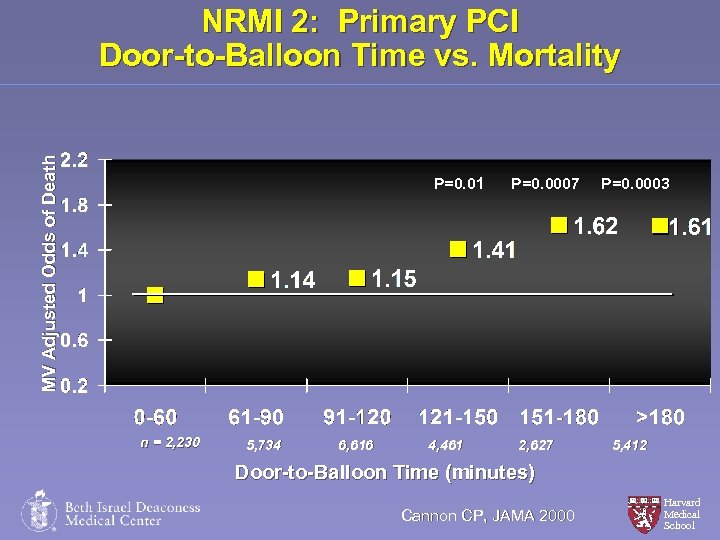 MV Adjusted Odds of Death NRMI 2: Primary PCI Door-to-Balloon Time vs. Mortality P=0. 01 n = 2, 230 5, 734 6, 616 4, 461 P=0. 0007 2, 627 P=0. 0003 5, 412 Door-to-Balloon Time (minutes) Cannon CP, JAMA 2000 Harvard Medical School
MV Adjusted Odds of Death NRMI 2: Primary PCI Door-to-Balloon Time vs. Mortality P=0. 01 n = 2, 230 5, 734 6, 616 4, 461 P=0. 0007 2, 627 P=0. 0003 5, 412 Door-to-Balloon Time (minutes) Cannon CP, JAMA 2000 Harvard Medical School
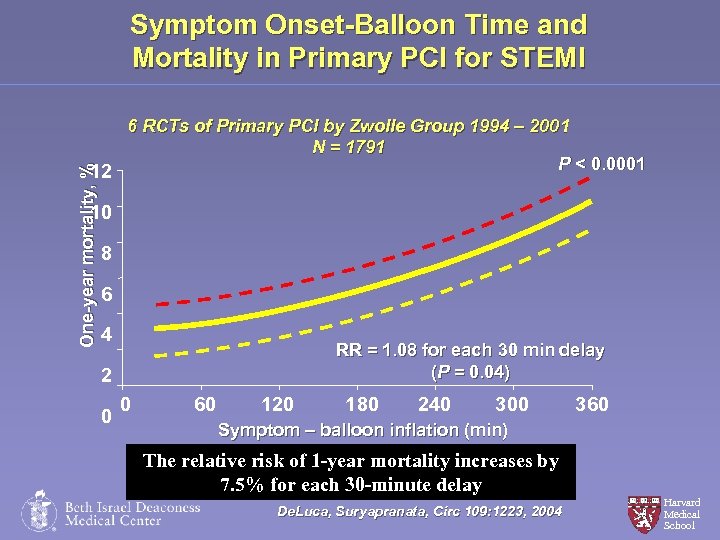 Symptom Onset-Balloon Time and Mortality in Primary PCI for STEMI One-year mortality, % 6 RCTs of Primary PCI by Zwolle Group 1994 – 2001 N = 1791 P < 0. 0001 12 10 8 6 4 RR = 1. 08 for each 30 min delay (P = 0. 04) 2 0 0 60 120 180 240 300 360 Symptom – balloon inflation (min) The relative risk of 1 -year mortality increases by 7. 5% for each 30 -minute delay De. Luca, Suryapranata, Circ 109: 1223, 2004 Harvard Medical School
Symptom Onset-Balloon Time and Mortality in Primary PCI for STEMI One-year mortality, % 6 RCTs of Primary PCI by Zwolle Group 1994 – 2001 N = 1791 P < 0. 0001 12 10 8 6 4 RR = 1. 08 for each 30 min delay (P = 0. 04) 2 0 0 60 120 180 240 300 360 Symptom – balloon inflation (min) The relative risk of 1 -year mortality increases by 7. 5% for each 30 -minute delay De. Luca, Suryapranata, Circ 109: 1223, 2004 Harvard Medical School
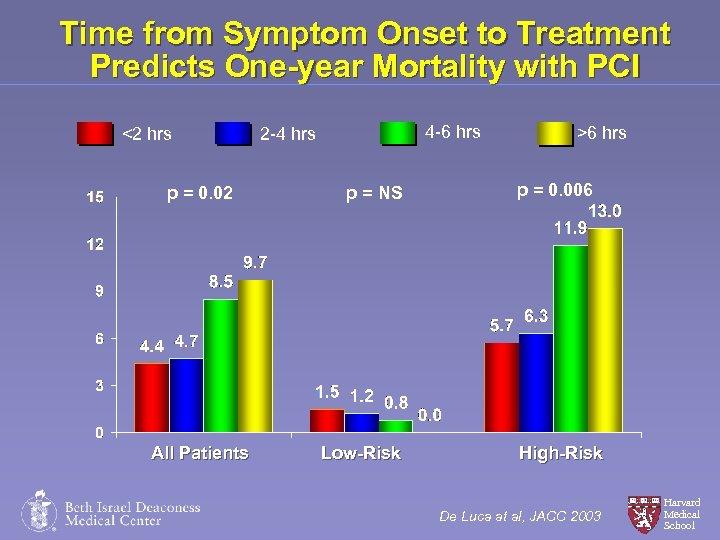 Time from Symptom Onset to Treatment Predicts One-year Mortality with PCI <2 hrs p = 0. 02 All Patients 4 -6 hrs 2 -4 hrs p = NS Low-Risk >6 hrs p = 0. 006 High-Risk De Luca at al, JACC 2003 Harvard Medical School
Time from Symptom Onset to Treatment Predicts One-year Mortality with PCI <2 hrs p = 0. 02 All Patients 4 -6 hrs 2 -4 hrs p = NS Low-Risk >6 hrs p = 0. 006 High-Risk De Luca at al, JACC 2003 Harvard Medical School
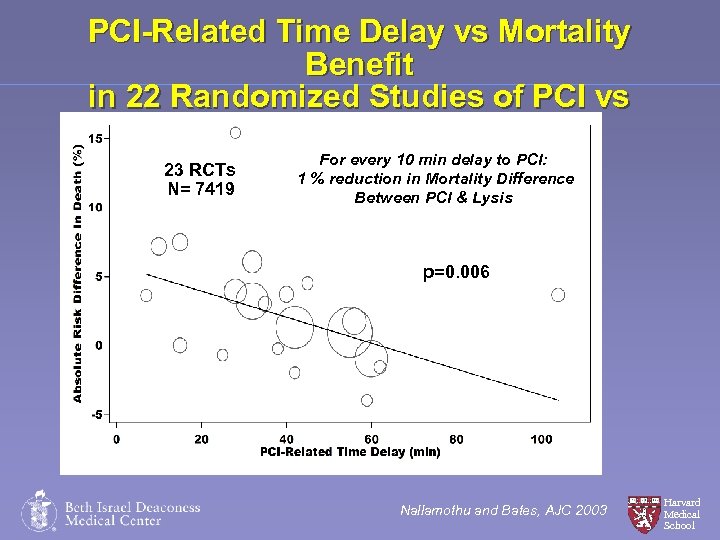 PCI-Related Time Delay vs Mortality Benefit in 22 Randomized Studies of PCI vs Fibrinolytic Therapy 23 RCTs N= 7419 For every 10 min delay to PCI: 1 % reduction in Mortality Difference Between PCI & Lysis p=0. 006 Nallamothu and Bates, AJC 2003 Harvard Medical School
PCI-Related Time Delay vs Mortality Benefit in 22 Randomized Studies of PCI vs Fibrinolytic Therapy 23 RCTs N= 7419 For every 10 min delay to PCI: 1 % reduction in Mortality Difference Between PCI & Lysis p=0. 006 Nallamothu and Bates, AJC 2003 Harvard Medical School
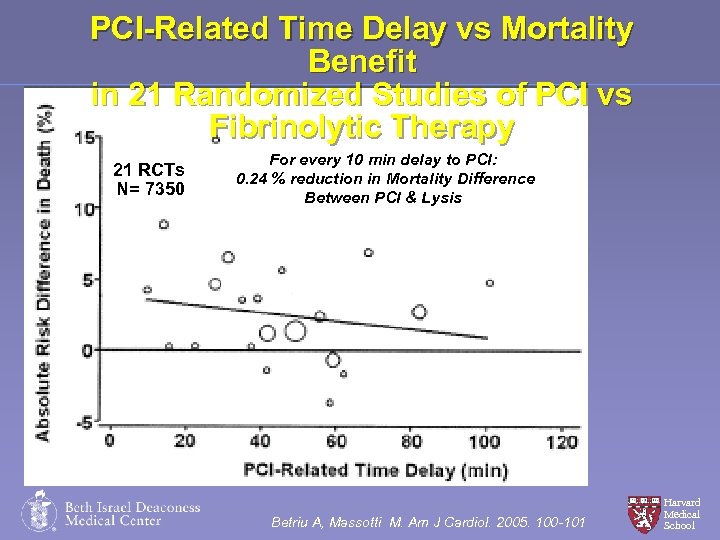 PCI-Related Time Delay vs Mortality Benefit in 21 Randomized Studies of PCI vs Fibrinolytic Therapy 21 RCTs N= 7350 For every 10 min delay to PCI: 0. 24 % reduction in Mortality Difference Between PCI & Lysis Betriu A, Massotti M. Am J Cardiol. 2005. 100 -101 Harvard Medical School
PCI-Related Time Delay vs Mortality Benefit in 21 Randomized Studies of PCI vs Fibrinolytic Therapy 21 RCTs N= 7350 For every 10 min delay to PCI: 0. 24 % reduction in Mortality Difference Between PCI & Lysis Betriu A, Massotti M. Am J Cardiol. 2005. 100 -101 Harvard Medical School
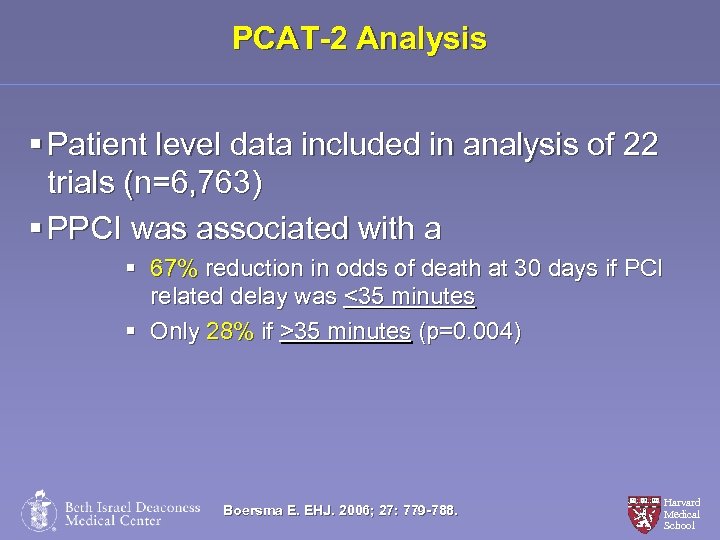 PCAT-2 Analysis § Patient level data included in analysis of 22 trials (n=6, 763) § PPCI was associated with a § 67% reduction in odds of death at 30 days if PCI related delay was <35 minutes § Only 28% if >35 minutes (p=0. 004) Boersma E. EHJ. 2006; 27: 779 -788. Harvard Medical School
PCAT-2 Analysis § Patient level data included in analysis of 22 trials (n=6, 763) § PPCI was associated with a § 67% reduction in odds of death at 30 days if PCI related delay was <35 minutes § Only 28% if >35 minutes (p=0. 004) Boersma E. EHJ. 2006; 27: 779 -788. Harvard Medical School
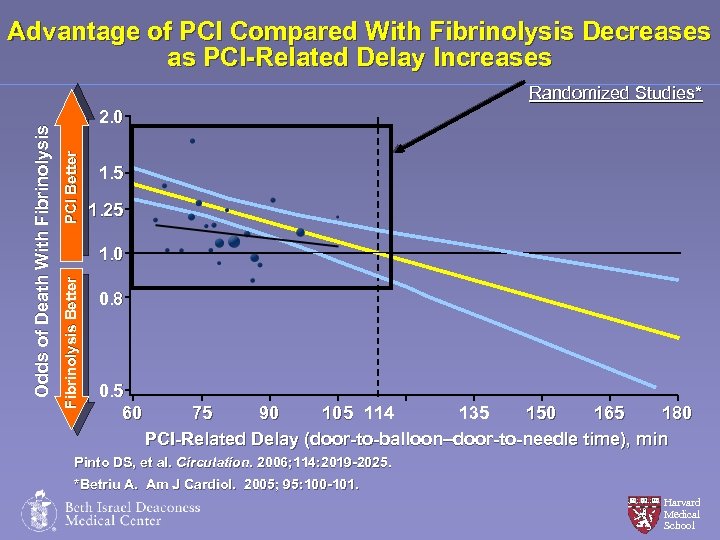 Advantage of PCI Compared With Fibrinolysis Decreases as PCI-Related Delay Increases PCI Better 2. 0 1. 5 1. 25 1. 0 Fibrinolysis Better O d d s o f D e a th W i th F i b r i n o l y s i s Randomized Studies* 0. 8 0. 5 60 135 75 90 150 165 180 105 114 PCI-Related Delay (door-to-balloon–door-to-needle time), min Pinto DS, et al. Circulation. 2006; 114: 2019 -2025. *Betriu A. Am J Cardiol. 2005; 95: 100 -101. Harvard Medical School
Advantage of PCI Compared With Fibrinolysis Decreases as PCI-Related Delay Increases PCI Better 2. 0 1. 5 1. 25 1. 0 Fibrinolysis Better O d d s o f D e a th W i th F i b r i n o l y s i s Randomized Studies* 0. 8 0. 5 60 135 75 90 150 165 180 105 114 PCI-Related Delay (door-to-balloon–door-to-needle time), min Pinto DS, et al. Circulation. 2006; 114: 2019 -2025. *Betriu A. Am J Cardiol. 2005; 95: 100 -101. Harvard Medical School
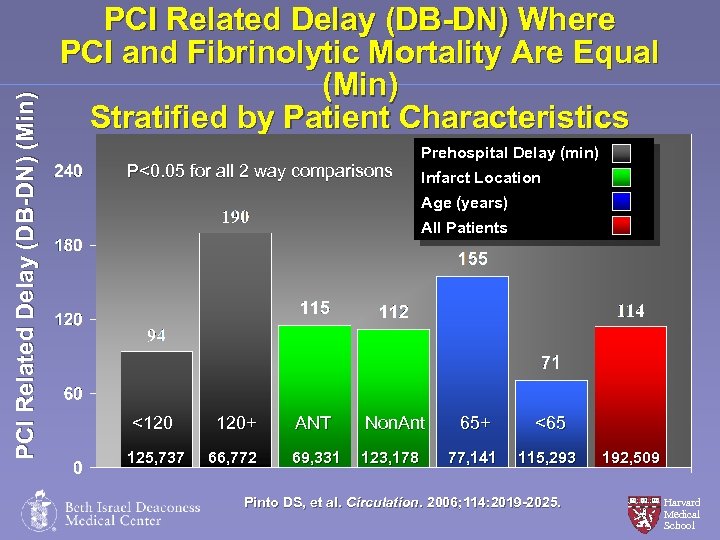 PCI Related Delay (DB-DN) (Min) PCI Related Delay (DB-DN) Where PCI and Fibrinolytic Mortality Are Equal (Min) Stratified by Patient Characteristics P<0. 05 for all 2 way comparisons Prehospital Delay (min) Infarct Location Age (years) All Patients <120 120+ ANT Non. Ant 125, 737 66, 772 69, 331 123, 178 65+ <65 77, 141 68, 716 123, 793 115, 293 192, 509 Pinto DS, et al. Circulation. 2006; 114: 2019 -2025. Harvard Medical School
PCI Related Delay (DB-DN) (Min) PCI Related Delay (DB-DN) Where PCI and Fibrinolytic Mortality Are Equal (Min) Stratified by Patient Characteristics P<0. 05 for all 2 way comparisons Prehospital Delay (min) Infarct Location Age (years) All Patients <120 120+ ANT Non. Ant 125, 737 66, 772 69, 331 123, 178 65+ <65 77, 141 68, 716 123, 793 115, 293 192, 509 Pinto DS, et al. Circulation. 2006; 114: 2019 -2025. Harvard Medical School
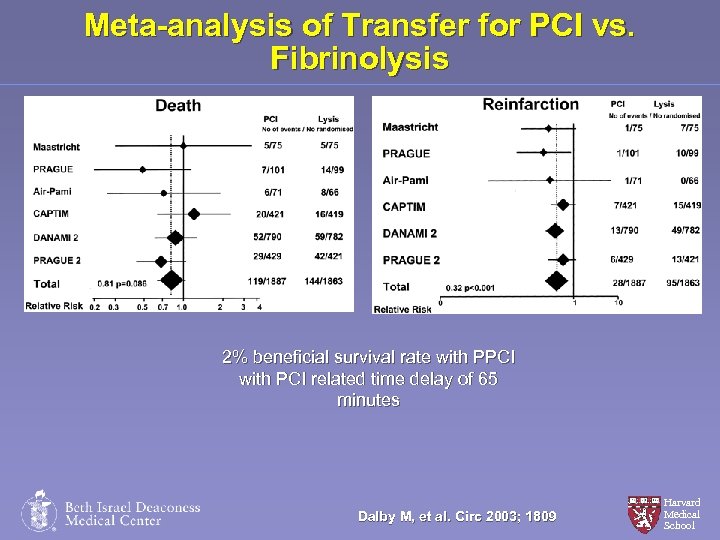 Meta-analysis of Transfer for PCI vs. Fibrinolysis 2% beneficial survival rate with PPCI with PCI related time delay of 65 minutes Dalby M, et al. Circ 2003; 1809 Harvard Medical School
Meta-analysis of Transfer for PCI vs. Fibrinolysis 2% beneficial survival rate with PPCI with PCI related time delay of 65 minutes Dalby M, et al. Circ 2003; 1809 Harvard Medical School
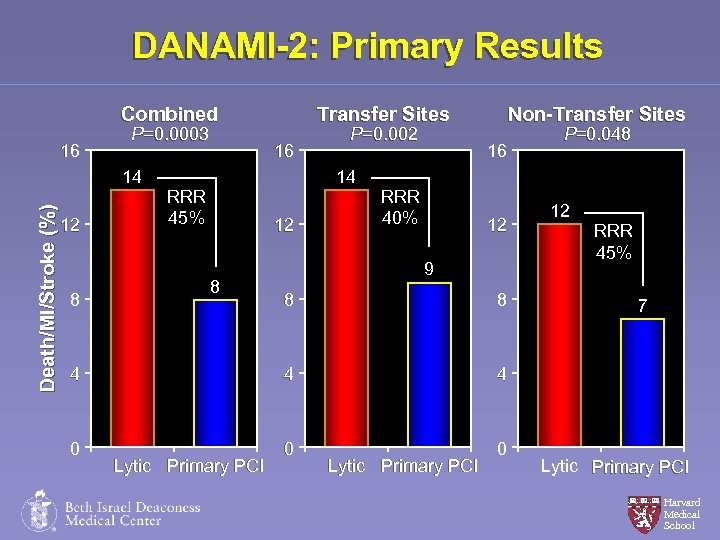 DANAMI-2: Primary Results Combined 16 P=0. 0003 Death/MI/Stroke (%) 14 12 8 Transfer Sites 16 P=0. 002 14 RRR 45% 12 8 Non-Transfer Sites 16 RRR 40% 12 9 8 8 4 4 0 0 12 RRR 45% 4 0 P=0. 048 Lytic Primary PCI 7 Lytic Primary PCI Harvard Medical School
DANAMI-2: Primary Results Combined 16 P=0. 0003 Death/MI/Stroke (%) 14 12 8 Transfer Sites 16 P=0. 002 14 RRR 45% 12 8 Non-Transfer Sites 16 RRR 40% 12 9 8 8 4 4 0 0 12 RRR 45% 4 0 P=0. 048 Lytic Primary PCI 7 Lytic Primary PCI Harvard Medical School
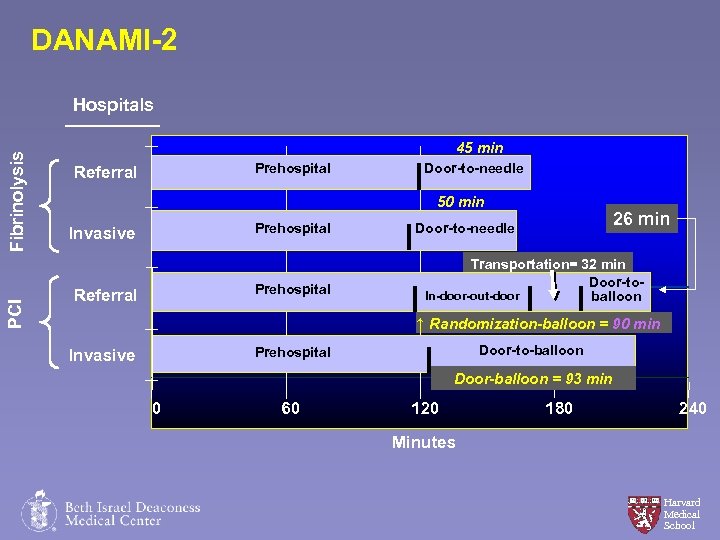 DANAMI-2 PCI Fibrinolysis Hospitals 45 min Prehospital Referral Door-to-needle 50 min Prehospital Invasive Prehospital Referral 26 min Door-to-needle Transportation= 32 min Door-to. In-door-out-door balloon ↑ Randomization-balloon = 90 min Door-to-balloon Prehospital Invasive Door-balloon = 93 min 0 60 120 180 240 Minutes Harvard Medical School
DANAMI-2 PCI Fibrinolysis Hospitals 45 min Prehospital Referral Door-to-needle 50 min Prehospital Invasive Prehospital Referral 26 min Door-to-needle Transportation= 32 min Door-to. In-door-out-door balloon ↑ Randomization-balloon = 90 min Door-to-balloon Prehospital Invasive Door-balloon = 93 min 0 60 120 180 240 Minutes Harvard Medical School
 Maybe Our Systems Are Not Completely Optimized in the US! Harvard Medical School
Maybe Our Systems Are Not Completely Optimized in the US! Harvard Medical School
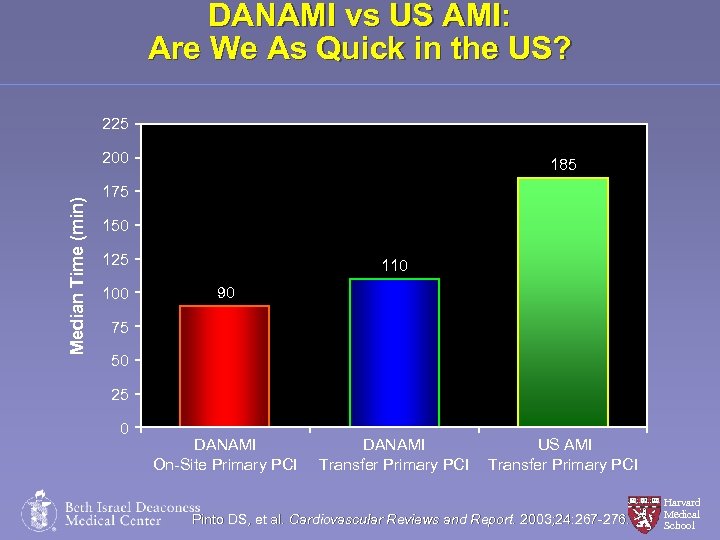 DANAMI vs US AMI: Are We As Quick in the US? 225 Median Time (min) 200 185 175 150 125 100 110 90 75 50 25 0 DANAMI On-Site Primary PCI DANAMI Transfer Primary PCI US AMI Transfer Primary PCI Pinto DS, et al. Cardiovascular Reviews and Report. 2003; 24: 267 -276. Harvard Medical School
DANAMI vs US AMI: Are We As Quick in the US? 225 Median Time (min) 200 185 175 150 125 100 110 90 75 50 25 0 DANAMI On-Site Primary PCI DANAMI Transfer Primary PCI US AMI Transfer Primary PCI Pinto DS, et al. Cardiovascular Reviews and Report. 2003; 24: 267 -276. Harvard Medical School
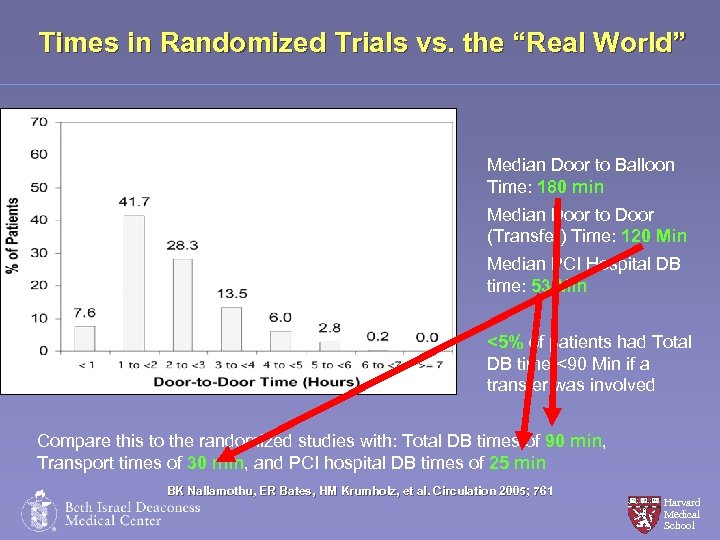 Times in Randomized Trials vs. the “Real World” Median Door to Balloon Time: 180 min Median Door to Door (Transfer) Time: 120 Min Median PCI Hospital DB time: 53 Min <5% of patients had Total DB time <90 Min if a transfer was involved Compare this to the randomized studies with: Total DB times of 90 min, Transport times of 30 min, and PCI hospital DB times of 25 min BK Nallamothu, ER Bates, HM Krumholz, et al. Circulation 2005; 761 Nallamothu, Krumholz, Harvard Medical School
Times in Randomized Trials vs. the “Real World” Median Door to Balloon Time: 180 min Median Door to Door (Transfer) Time: 120 Min Median PCI Hospital DB time: 53 Min <5% of patients had Total DB time <90 Min if a transfer was involved Compare this to the randomized studies with: Total DB times of 90 min, Transport times of 30 min, and PCI hospital DB times of 25 min BK Nallamothu, ER Bates, HM Krumholz, et al. Circulation 2005; 761 Nallamothu, Krumholz, Harvard Medical School
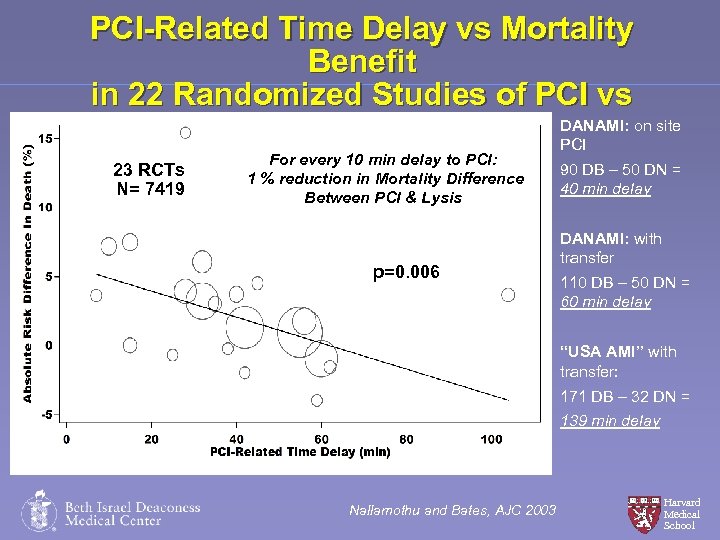 PCI-Related Time Delay vs Mortality Benefit in 22 Randomized Studies of PCI vs Fibrinolytic Therapy DANAMI: on site PCI 23 RCTs N= 7419 For every 10 min delay to PCI: 1 % reduction in Mortality Difference Between PCI & Lysis p=0. 006 90 DB – 50 DN = 40 min delay DANAMI: with transfer 110 DB – 50 DN = 60 min delay “USA AMI” with transfer: 171 DB – 32 DN = 139 min delay Nallamothu and Bates, AJC 2003 Harvard Medical School
PCI-Related Time Delay vs Mortality Benefit in 22 Randomized Studies of PCI vs Fibrinolytic Therapy DANAMI: on site PCI 23 RCTs N= 7419 For every 10 min delay to PCI: 1 % reduction in Mortality Difference Between PCI & Lysis p=0. 006 90 DB – 50 DN = 40 min delay DANAMI: with transfer 110 DB – 50 DN = 60 min delay “USA AMI” with transfer: 171 DB – 32 DN = 139 min delay Nallamothu and Bates, AJC 2003 Harvard Medical School
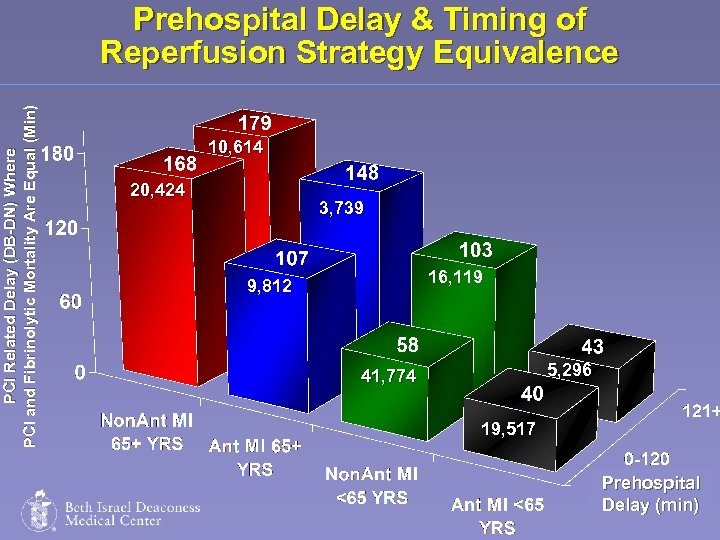 PCI Related Delay (DB-DN) Where PCI and Fibrinolytic Mortality Are Equal (Min) Prehospital Delay & Timing of Reperfusion Strategy Equivalence 10, 614 20, 424 3, 739 16, 119 9, 812 5, 296 41, 774 19, 517 Prehospital Harvard Delay (min) Medical School
PCI Related Delay (DB-DN) Where PCI and Fibrinolytic Mortality Are Equal (Min) Prehospital Delay & Timing of Reperfusion Strategy Equivalence 10, 614 20, 424 3, 739 16, 119 9, 812 5, 296 41, 774 19, 517 Prehospital Harvard Delay (min) Medical School
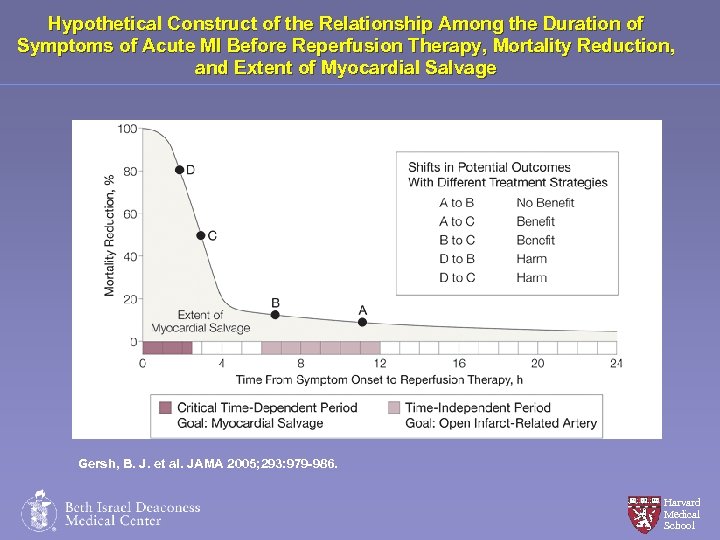 Hypothetical Construct of the Relationship Among the Duration of Symptoms of Acute MI Before Reperfusion Therapy, Mortality Reduction, and Extent of Myocardial Salvage Gersh, B. J. et al. JAMA 2005; 293: 979 -986. Harvard Medical School
Hypothetical Construct of the Relationship Among the Duration of Symptoms of Acute MI Before Reperfusion Therapy, Mortality Reduction, and Extent of Myocardial Salvage Gersh, B. J. et al. JAMA 2005; 293: 979 -986. Harvard Medical School
 Harvard Medical School One Size Does Not Fit All!
Harvard Medical School One Size Does Not Fit All!
 Summary Simple rules: § DB<90 min § DB-DN <60 min § DN <30 min § Transfer all for PCI, etc are not enough to determine the optimal reperfusion strategy for all patients in all situations Harvard Medical School
Summary Simple rules: § DB<90 min § DB-DN <60 min § DN <30 min § Transfer all for PCI, etc are not enough to determine the optimal reperfusion strategy for all patients in all situations Harvard Medical School
 Summary § The clinician must integrate: § Prehospital Delay § Anticipated STEMI Risk (age, anterior, inferior, shock) § Anticipated Risk for ICH § Anticipated Transfer time/PCI related delay Harvard Medical School
Summary § The clinician must integrate: § Prehospital Delay § Anticipated STEMI Risk (age, anterior, inferior, shock) § Anticipated Risk for ICH § Anticipated Transfer time/PCI related delay Harvard Medical School
 Summary § Fibrinolysis is not unreasonable when § PCI associated with unacceptable delay (Class I) § Short time from symptom onset (<1 hr) (Class I) § Primary PCI is superior to Fibrinolysis in several clinical situations, particularly if: § Competent personnel involved § DB times are <90 Min, PCI related Delay Acceptable § High Risk for Bleeding or Complication from MI § Late Presentation Harvard Medical School
Summary § Fibrinolysis is not unreasonable when § PCI associated with unacceptable delay (Class I) § Short time from symptom onset (<1 hr) (Class I) § Primary PCI is superior to Fibrinolysis in several clinical situations, particularly if: § Competent personnel involved § DB times are <90 Min, PCI related Delay Acceptable § High Risk for Bleeding or Complication from MI § Late Presentation Harvard Medical School
 Summary § The benefits and limitations of Primary PCI should be considered when developing regionalized transfer and community based PCI systems § Continued work is needed to develop pharmacologic strategies to rapidly, effectively, and safely open closed arteries thereby extending the benefit of PCI to a larger group of patients Harvard Medical School
Summary § The benefits and limitations of Primary PCI should be considered when developing regionalized transfer and community based PCI systems § Continued work is needed to develop pharmacologic strategies to rapidly, effectively, and safely open closed arteries thereby extending the benefit of PCI to a larger group of patients Harvard Medical School
 Question & Answer
Question & Answer
 Thank You! Please make sure to hand in your evaluation and pick up a Clinical. Trial. Results. org flash drive
Thank You! Please make sure to hand in your evaluation and pick up a Clinical. Trial. Results. org flash drive


