ac11a763270bc3d41f896178535a8b61.ppt
- Количество слайдов: 28
Walk the Walk: A Public School Intervention for Worksite Wellness Sue Baldwin, Ph. D, CHES Assistant Professor & Internship Program Coordinator State University of New York – Buffalo State College Pete Renkas, MS Health and Physical Education Teacher Buffalo Public Schools, Buffalo, NY
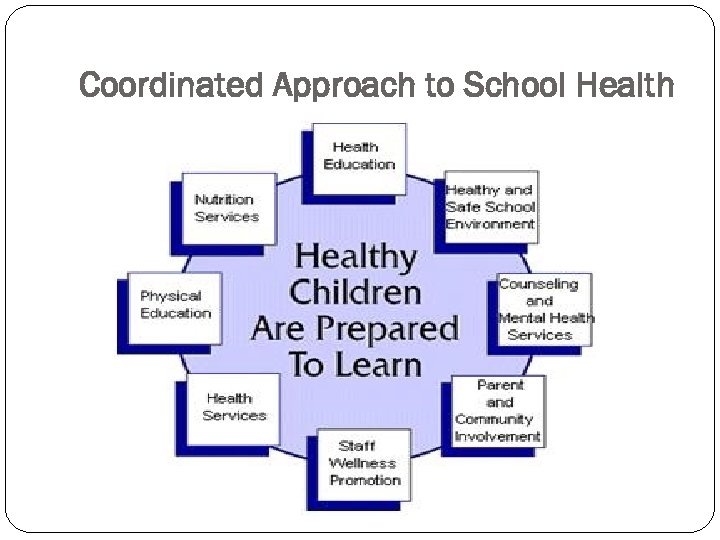
Coordinated Approach to School Health
Introduction Obesity - one of the 10 leading U. S. health indicators Associated with increased risk for hypertension, dyslipidemia, type II diabetes, coronary heart disease, stroke, and certain cancers A Healthy People 2010 objective was to reduce to 15% the prevalence of obesity among adults in the United States (objective 19 -2). In 2003, one study estimated that state-specific, obesityattributable medical expenditures ranged from $87 million in Wyoming to $7. 7 billion in California 23. 9% of U. S. adults were obese in 2005, and the prevalence of obesity increased during 1995 --2005 in all states Healthy People 2010, 2000; Finkelstein EA, Fiebelkorn IC, Wang G, 2004
Focus of this Research: Faculty and Staff Health Promotion 53% of polled companies (N=600, 350 of largest US employers) incorporate a disease management or health improvement program according to 2010 survey 145 million American adults are overweight and 74 million are obese, placing more than one-third of the working-age US population at risk for chronic disease Obesity-related diseases are nearly 10% of all medical spending or $147 billion/year – ½ financed through Medicare/Medicaid Asthma, diabetes and hypertension = 164 million lost work days/year amounting to $30 billion 74. 5 million people in US have hypertension – increased risk of heart disease and stroke In 2010, hypertension will cost US $76. 6 billion in health care services, medications and missed days at work Hewitt Associates, 2010; American Heart Association, 2010; Lloyd-James, Adams & Brown, 2010
Research Question: Research question: Will a 10 -week faculty/staff physical activity and blood pressure self-monitoring program improve participant physical activity and readiness to change regarding diet, body weight, physical activity, blood pressure self-monitoring and stress management behaviors? Program Purposes/Goals: 1. Advance participants’ behavior across the Transtheoretical Model 2. Increase participant physical activity 3. Encourage weekly blood pressure self-monitoring Increase the number of participants who know their BP Lower diastolic BP Lower systolic BP
Methods: Design & Tool Quantitative approach – pilot, pre/post-test research design; SPSS version 15 Physical Activity and Blood Pressure Questionnaire: four-part, pre/post-test tool: (49 items) Demographics: (8 items) 1. 2. 3. Gender, age, race/ethnicity, marital status, education, income, job status, job description General Health: (9 items) Overall health, BP known, actual BP, saw doctor for hypertension, on medications or under care for hypertension, family history of hypertension, diabetes, heart disease, hypercholesterolemia Transtheoretical Model: (5 items) 1 item on healthy diet 1 item on healthy body weight 1 item on physical activity 1 item on stress management 1 item on blood pressure
Methods: Tool (continued) International Physical Activity Questionnaire (IPAQ) – perceived levels of physical activity placed into low, moderate or vigorous category (27 items) 4. 7 items on job-related physical activity 6 items on transportation-related physical activity 6 items on housework, house maintenance, and caring for family physical activity 6 items on recreation, sport and leisure-time physical activity 2 items on time spent sitting IPAQ created repeatable data (Spearman’s clustered around 0. 8) and criterion validity as a median of about 0. 3, which is similar to other self-report validation studies (Vandelanotte, Bourdeaudhuij, Pilippaerts, Sjostrom & Sallis, 2005)
Setting/Participants: Large, urban school district in Western New York 46 Elementary Schools 13 High Schools 2 Adult Education Schools This pilot intervention was in the Hospitality High School Convenience sample of 55 employees 25 usable pre/post test surveys and program completion 45% response rate District looking to implement full-scale faculty/staff wellness program
Methods Walking 10, 000 steps per day for 10 -weeks with pedometer Blood pressure “how-to” tri-fold stations with automatic sphygmomanometer and blood pressure recommendations
Methods 30 -minute, interactive education sessions Exercise and blood pressure Exercise and heat/sun-related conditions Exercise and weight management Exercise and heart disease Incentive: blood pressure 10 readings for 10 weeks: Walk the Walk t-shirt Incentives: physical activity Weeks 1 -2: 12 -14 days at 5, 000 steps/day: stress ball or salad clip Weeks 3 -4: 12 -14 days at 8, 000 steps/day: backpack or calculator Weeks 5 -6: 12 -14 days at 10, 000 steps/day: lunch bag or water bottle Weeks 7 -8: 12 -14 days at 10, 000 steps/day: Delta Sonic basic car wash GC Weeks 9 -10: 12 -14 days at 10, 000 steps/day: Cinema/movie passes for two
Results: Demographics 80% (n=20) were females and 20%(n=5) were males 63% of employees were White (Non. Hispanic) (n=13), 30% were Black (Non -Hispanic) (n=6) and 5% were Hispanic (n=1) 87% (n=18) were 40 -59 years old and 13% (n=7) were age 18 -39 80% (n=15) were married, 22% (n=4) were single, and 17% (n=3) were divorced Income level reflected that 52% (n=8) made $50, 000 -$74, 000 or more per year, 21% (n=4) made $100, 000 or more, 14% (n=5) made $75, 000$99, 000, 8% (n=3) made $35, 000$49, 000 and 1% (n=2) made less than $35, 000 per year Education level reflected that 79% (n=18) held post graduate/professional degrees, 18% (n=4) were college graduates and 3% (n=1) were high school graduates 97% (n=24) worked full-time and 3% (n=1) worked part-time in the school district 63% (n=12) had professional job titles, 17% (n=6) held manager or supervisor job titles, 13% (n=2) were technicians and 6% (n=2) were clerical/office support staff 73% (n=17) thought their overall general health was “good, ” 20% (n=5) reported “very good” and 8% (n=3) reported their health as “excellent” 76% of participants indicated that they had a family history of hypertension, 56% had history of heart disease, 60% had history of familial diabetes, and 52% indicated history of high cholesterol
Results: Blood Pressure 35% of participants did not currently know their blood pressure at pre-test - at post-test 83 % of participants indicated they knew their current blood pressure; reflecting a 48% change On average, systolic blood pressure was 128. 38 mm. Hg at pretest and dropped 4. 82 mm. Hg at post-test for all participants Diastolic pressure was 81. 38 mm. Hg at pre-test and dropped 7. 49 mm. Hg at post-test 31% of employees at pre-test reported having high blood pressure this decreased to 11% at post-test or a 20% change 32% were taking medications to control high blood pressure at pre-test there was an 8% increase at post-test 36% of participants at pre-test indicated they were under medical care for high blood pressure there was an 8% increase at posttest
Results: TTM & Behavioral Intention Participant mean change scores from the TTM (Prochaska & Di. Clemente) exhibited by participants over the 10 -week intervention were analyzed All of the areas assessed in participants increased as a result of this program Healthy diet=0. 56 (over ½ of a stage) Healthy body weight= 0. 48 (almost ½ of a stage) Physical activity=0. 64 (just over half of a stage) Stress management=0. 72 (nearly a full stage) Blood pressure=1. 36 (largest change; over a full stage)
Results: Physical Activity International Physical Activity Questionnaire (IPAQ) (long form) - to assess low, moderate and vigorous-intensity: Job-related physical activity Transportation physical activity Housework/house maintenance/caring for family physical activity Recreation/sport/leisure time physical activity Time spent sitting over the past 7 days at pre- and post-test
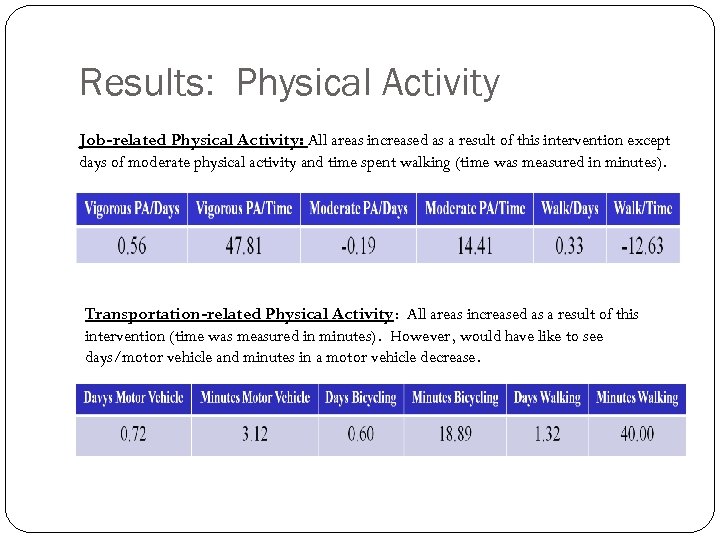
Results: Physical Activity Job-related Physical Activity: All areas increased as a result of this intervention except days of moderate physical activity and time spent walking (time was measured in minutes). Transportation-related Physical Activity: All areas increased as a result of this intervention (time was measured in minutes). However, would have like to see days/motor vehicle and minutes in a motor vehicle decrease.
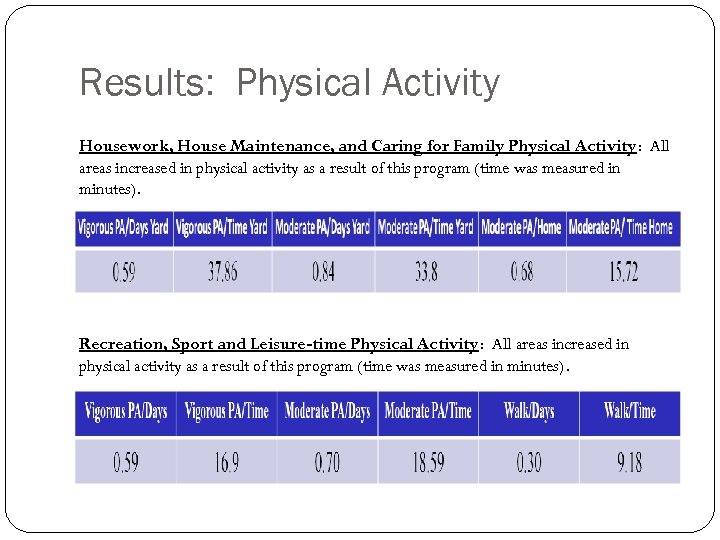
Results: Physical Activity Housework, House Maintenance, and Caring for Family Physical Activity: All areas increased in physical activity as a result of this program (time was measured in minutes). Recreation, Sport and Leisure-time Physical Activity: All areas increased in physical activity as a result of this program (time was measured in minutes).
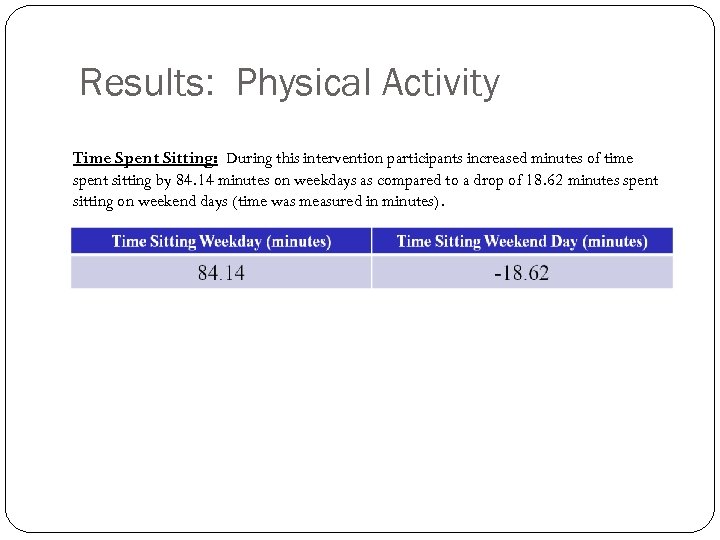
Results: Physical Activity Time Spent Sitting: During this intervention participants increased minutes of time spent sitting by 84. 14 minutes on weekdays as compared to a drop of 18. 62 minutes spent sitting on weekend days (time was measured in minutes).
Conclusions: Blood Pressure Program Goal: Encourage weekly blood pressure self-monitoring Increase the number of participants who know their BP Lower diastolic BP & systolic BP Nearly 50% more participants now know their BP Systolic BP (4. 82 mm. Hg) and diastolic BP readings decreased (7. 49 mm. Hg) at post-test There was a 20% decrease in participant report of having high BP at post-test 8% more employees found out they had high BP during the intervention and were placed on medications
Conclusions: Stages of Change TTM postulates that behavior change is a dynamic process involving movement through a sequence of discrete, qualitative distinct stages - change scores were analyzed One program goal was to move participants along these phases of change toward behavioral action All of the areas of change improved as a result of this program: Healthy diet Healthy body weight Physical activity Stress management Blood pressure
Conclusions: Physical Activity Another program goal was to improve physical activity IPAQ assessed various types of physical activity: 1. Job-related 2. Transportation-related 3. Housework, house maintenance, and caring for family 4. Recreation, sport and leisure-time 5. Time spent sitting Almost all of the areas of physical activity evaluated increased during the intervention except: Job-related physical activity days of moderate physical activity and days spent walking Would like days/motor vehicle and minutes in a motor vehicle decrease Time spent sitting on weekdays
Discussion: Worksite wellness initiatives over past 20 years: Large businesses, various industries and in public settings to improve overall health of employees and increase productivity More emphasis should be placed on schools as worksites Wellness activities to the school/worksite eliminates barriers to information and program accessibility for employees Program evaluation is critical - schools/worksites typically implement “feel good” programs - not typically evaluated for effectiveness Program planning models and health behavior theories not followed – schools lack training to do evaluation and personnel
Discussion: Self-report physical activity data collection, despite its popularity and advantages, has several negative aspects: 1. 2. 3. 4. 5. Difficult to calculate the intensity (i. e. light, moderate or vigorous physical activity) of activities (Montoye, Kemper, Saris & Washburn, 1996) Inaccurate perception and recalling errors (Freedson & Miller, 2000) Bias based on socially desirable responses (Sallis & Saelens, 2000) can lead to over-reporting of physical activity (Sallis & Saelens, 2000; Freedson & Miller, 2000) Light to moderate activities could be less accurate compared to high intensity activities (Bassett, Ainsworth, Swartz, Strath, O’Brien & King, 2000; Bassett, 2000) Physical activity is a multi-faceted behavior with significant daily variation, which self-assessment questionnaires cannot reveal (Freedson & Miller, 2000)
Discussion: Low population (N=55 employees) - due to a very low post- test return rate (N=25) our results may reflect bias. Low participation and post-test response rate due to first time the worksite implemented any health promotion program Participant skepticism of the program was elevated – WHO suddenly wants to know my BP and level of fitness and WHY
Implementation Barriers 1. 2. 3. 4. 5. Lack of program funding to purchase proper pedometers/accelerometers and incentive prizes appropriate to target audience (not a priority in school budgets). Lack of time in the teaching day to provide education interventions – took place after school hours. Participant buy-in/skepticism…why are we being asked to do this, who wants to know results, how will it affect me at my job, etc… first time program ever offered in district or building. Conduct a needs assessment and base-line screenings prior to program implementation to increase awareness of health and health-related issues. Person running program lacks designated time to run comprehensive, multifaceted health promotion program and wears many “other hats. ”
Recommendations: A study conducted in Washoe County School District in Nevada found a cost savings of $15. 60 for every dollar spent on a school faculty/staff wellness program as a result of reduced faculty absenteeism (Aldana, Merrill, Price, Hardy & Hagar, 2005) – create research that forecasts dollar savings along with this intervention A revised survey tool (IPAQ and Stages of Change Model) was created for use in this study as a previous study used a 5 -page tool reflecting a large participant drop-out rate this study utilized a one-page, double-sided Scantron form (increased efficiency and accuracy of research results)
Recommendations: Future Research Controlled study using a larger population (numerous school buildings) Utilize a pedometer that is of high-quality, durability and accuracy. If it is cost effective, accelerometers should be utilized to enhance research results Market and promote the program (email blasts, posters, mail-box stuffers, pay check stuffers, program flyers, PSA’s and public address system announcements) Incentive prizes based on participant wants and needs (items that will motive them to participate) Central location and time for participants to meet for education sessions is critical
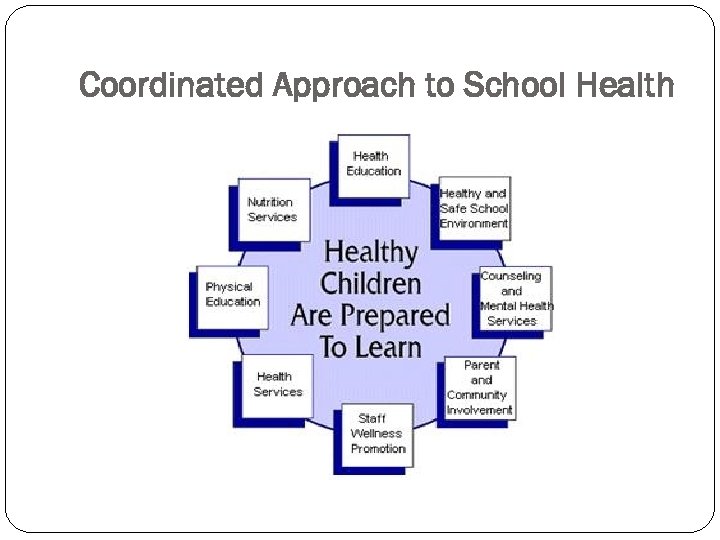
Coordinated Approach to School Health
For More Information Contact: Sue Baldwin, Ph. D, CHES Assistant Professor and Internship Program Coordinator SUNY – Buffalo State College Department of Health and Wellness baldwism@buffalostate. edu 716 -878 -6503 Peter Renkas, MS Health and Physical Education Teacher Buffalo Public Schools, Buffalo, NY Prenkas@buffaloschools. org 716 -984 -7305
ac11a763270bc3d41f896178535a8b61.ppt