934ee051491f146e77b7a24890b4da2b.ppt
- Количество слайдов: 18
VTE Risk Assessment & Prophylaxis in OB Engaging the Entire Clinical Team to Achieve QI Success
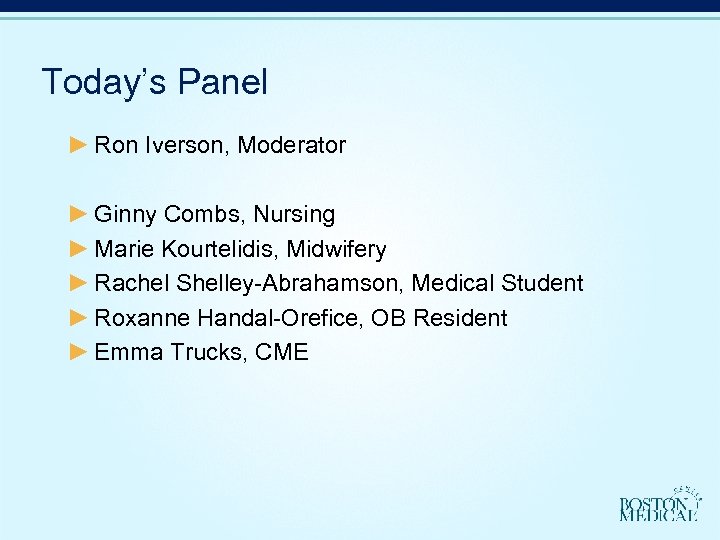
Today’s Panel ► Ron Iverson, Moderator ► Ginny Combs, Nursing ► Marie Kourtelidis, Midwifery ► Rachel Shelley-Abrahamson, Medical Student ► Roxanne Handal-Orefice, OB Resident ► Emma Trucks, CME
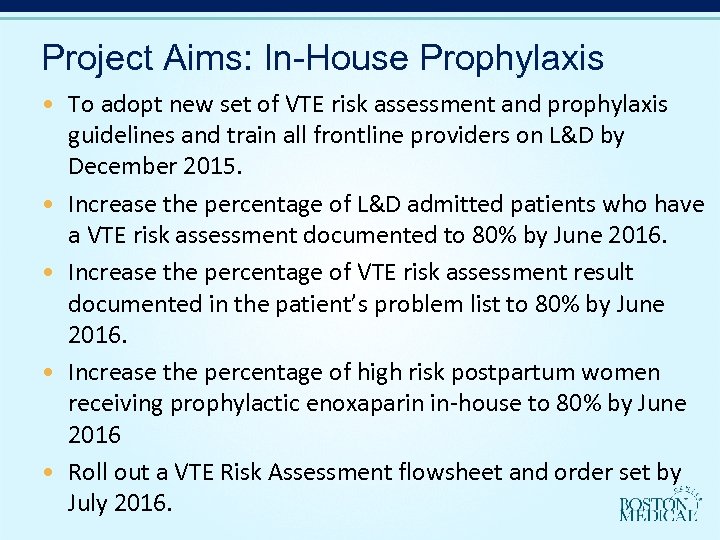
Project Aims: In-House Prophylaxis • To adopt new set of VTE risk assessment and prophylaxis guidelines and train all frontline providers on L&D by December 2015. • Increase the percentage of L&D admitted patients who have a VTE risk assessment documented to 80% by June 2016. • Increase the percentage of VTE risk assessment result documented in the patient’s problem list to 80% by June 2016. • Increase the percentage of high risk postpartum women receiving prophylactic enoxaparin in-house to 80% by June 2016 • Roll out a VTE Risk Assessment flowsheet and order set by July 2016.
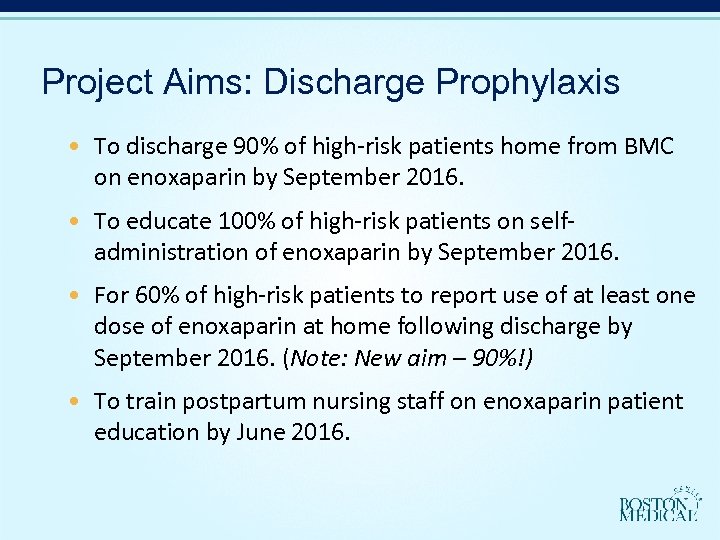
Project Aims: Discharge Prophylaxis • To discharge 90% of high-risk patients home from BMC on enoxaparin by September 2016. • To educate 100% of high-risk patients on selfadministration of enoxaparin by September 2016. • For 60% of high-risk patients to report use of at least one dose of enoxaparin at home following discharge by September 2016. (Note: New aim – 90%!) • To train postpartum nursing staff on enoxaparin patient education by June 2016.
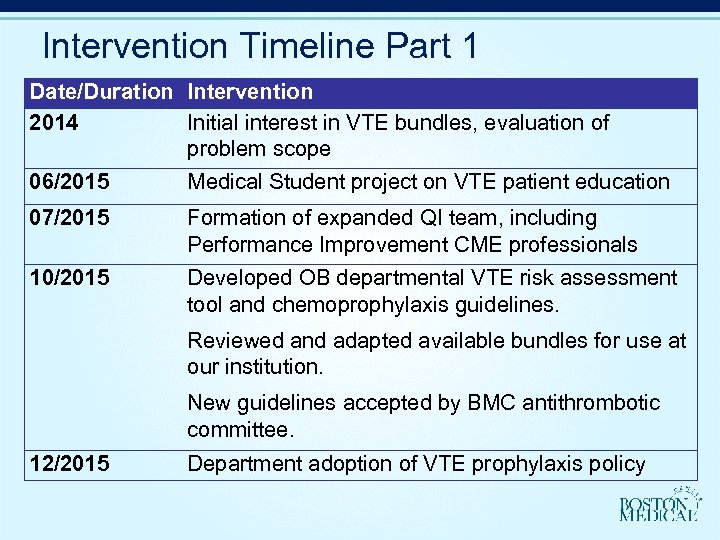
Intervention Timeline Part 1 Date/Duration Intervention 2014 Initial interest in VTE bundles, evaluation of problem scope 06/2015 Medical Student project on VTE patient education 07/2015 Formation of expanded QI team, including Performance Improvement CME professionals 10/2015 Developed OB departmental VTE risk assessment tool and chemoprophylaxis guidelines. Reviewed and adapted available bundles for use at our institution. New guidelines accepted by BMC antithrombotic committee. 12/2015 Department adoption of VTE prophylaxis policy
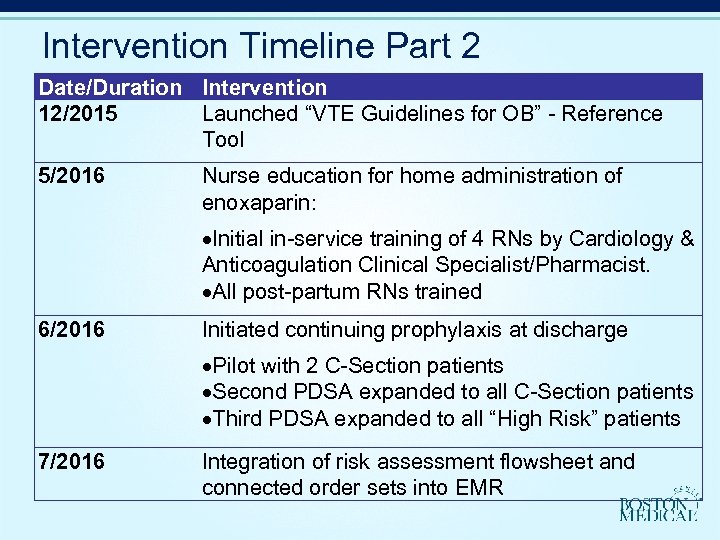
Intervention Timeline Part 2 Date/Duration Intervention 12/2015 Launched “VTE Guidelines for OB” - Reference Tool 5/2016 Nurse education for home administration of enoxaparin: Initial in-service training of 4 RNs by Cardiology & Anticoagulation Clinical Specialist/Pharmacist. All post-partum RNs trained 6/2016 Initiated continuing prophylaxis at discharge Pilot with 2 C-Section patients Second PDSA expanded to all C-Section patients Third PDSA expanded to all “High Risk” patients 7/2016 Integration of risk assessment flowsheet and connected order sets into EMR
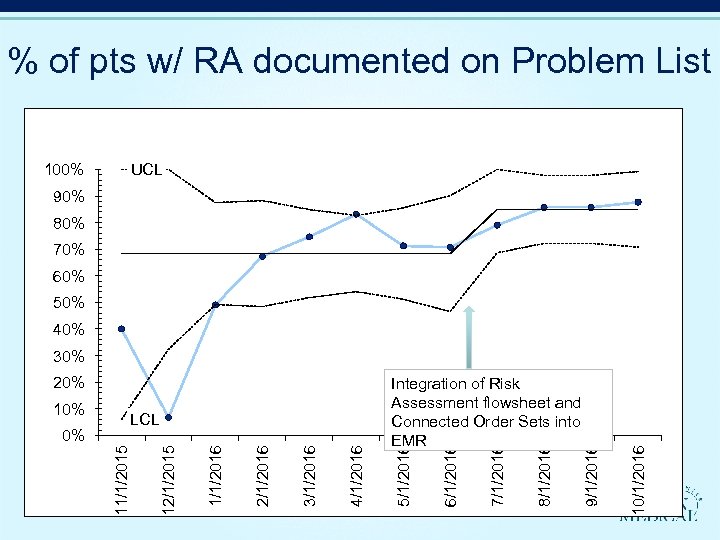
% of pts w/ RA documented on Problem List 100% UCL 90% 80% 70% 60% 50% 40% 10/1/2016 8/1/2016 7/1/2016 6/1/2016 4/1/2016 3/1/2016 2/1/2016 12/1/2015 0% LCL 11/1/2015 10% Integration of Risk Assessment flowsheet and Connected Order Sets into EMR 5/1/2016 20% 9/1/2016 30%
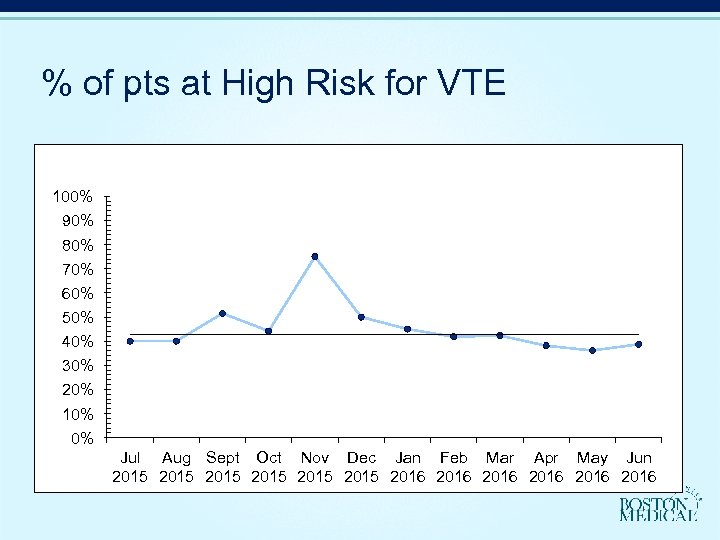
% of pts at High Risk for VTE 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Jul Aug Sept Oct Nov Dec Jan Feb Mar Apr May Jun 2015 2015 2016 2016
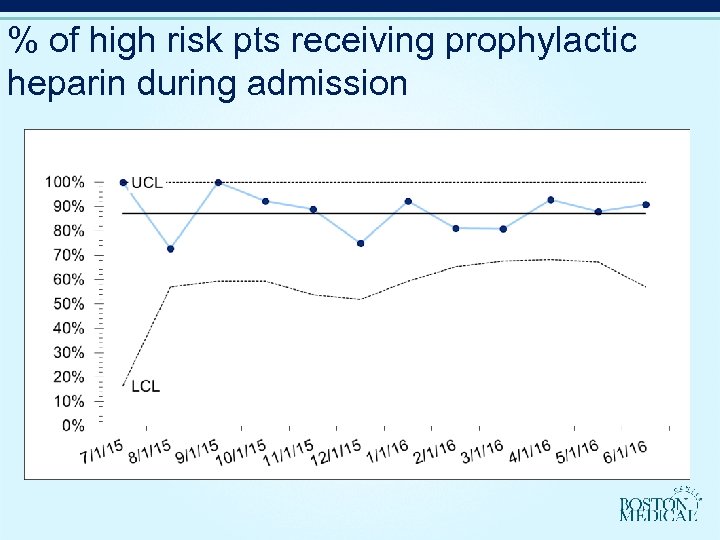
% of high risk pts receiving prophylactic heparin during admission
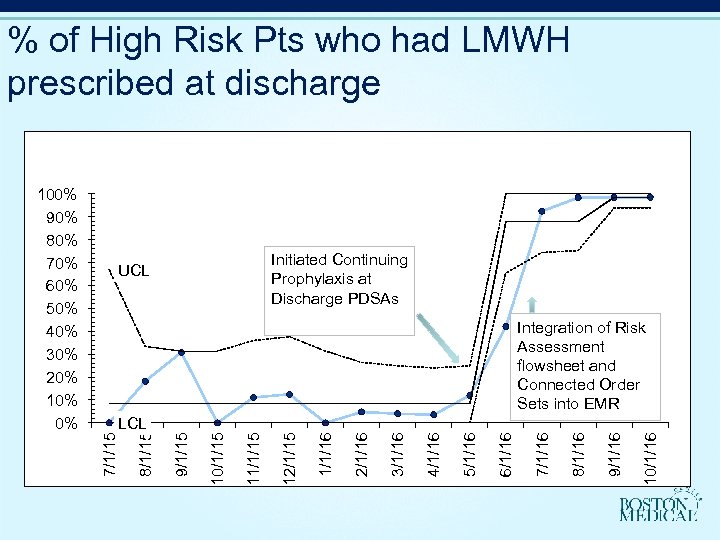
% of High Risk Pts who had LMWH prescribed at discharge Initiated Continuing Prophylaxis at Discharge PDSAs UCL Integration of Risk Assessment flowsheet and Connected Order Sets into EMR 10/1/16 9/1/16 8/1/16 7/1/16 6/1/16 5/1/16 4/1/16 3/1/16 2/1/16 12/1/15 11/1/15 10/1/15 9/1/15 8/1/15 LCL 7/1/15 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0%
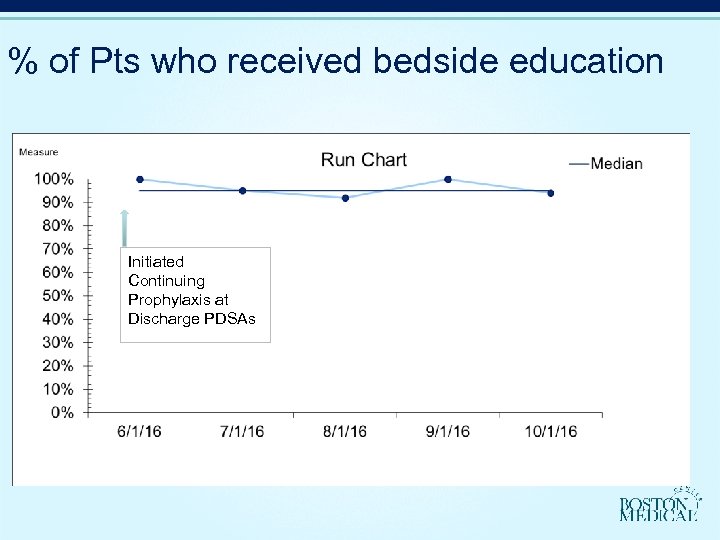
% of Pts who received bedside education Initiated Continuing Prophylaxis at Discharge PDSAs
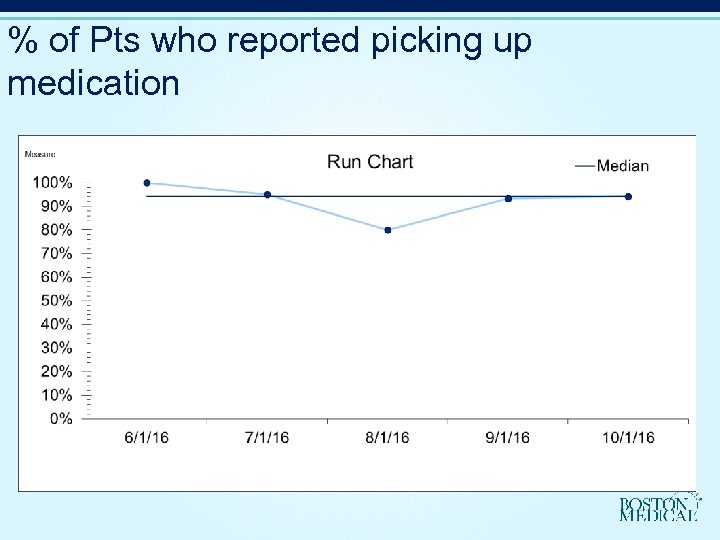
% of Pts who reported picking up medication
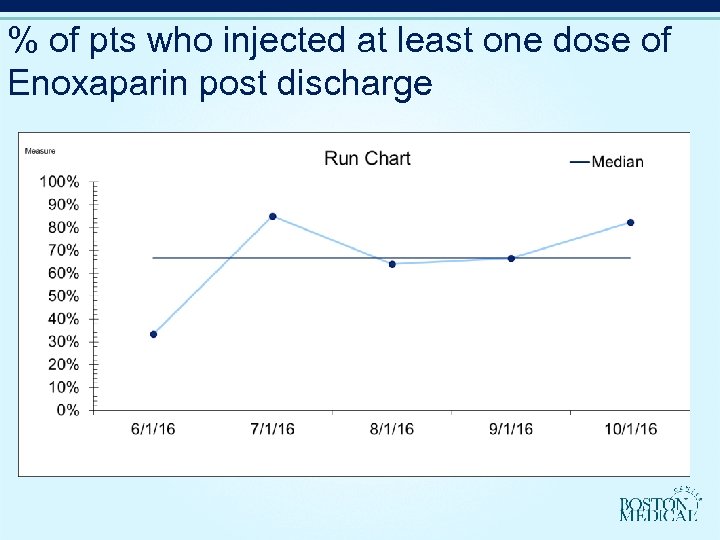
% of pts who injected at least one dose of Enoxaparin post discharge
![Breakdown of who administered injection at home [VALUE]% Self injection [VALUE]% Family/Friend VNA Breakdown of who administered injection at home [VALUE]% Self injection [VALUE]% Family/Friend VNA](https://present5.com/presentation/934ee051491f146e77b7a24890b4da2b/image-16.jpg)
Breakdown of who administered injection at home [VALUE]% Self injection [VALUE]% Family/Friend VNA
Today’s Panel ► Ron Iverson, Moderator ► Ginny Combs, Nursing ► Marie Kourtelidis, Midwifery ► Rachel Shelley-Abrahamson, Medical Student ► Roxanne Handal-Orefice, OB Resident ► Emma Trucks, CME
Questions? Ron Iverson, MD Ronald. Iverson@bmc. org
934ee051491f146e77b7a24890b4da2b.ppt