b94423490367790dbf1179f6c7e1f620.ppt
- Количество слайдов: 37
 VTE Prophylaxis in the Hospitalized Patient: Importance and Strategies for Improved Compliance Andrew H. Dombro, M. D. Instructor of Medicine Division of General Internal Medicine, Hospital Medicine Section University of Colorado Health Sciences Center
VTE Prophylaxis in the Hospitalized Patient: Importance and Strategies for Improved Compliance Andrew H. Dombro, M. D. Instructor of Medicine Division of General Internal Medicine, Hospital Medicine Section University of Colorado Health Sciences Center
 Overview n n n n Background / Prevalence of VTE Benefits / Rationale for VTE prophylaxis Identification of hospitalized patients most at risk Methods of VTE prophylaxis National Consensus Standards for Prevention and Care of VTE (CMS as well? ) Factors related to under-use of established guidelines Strategies to improve compliance
Overview n n n n Background / Prevalence of VTE Benefits / Rationale for VTE prophylaxis Identification of hospitalized patients most at risk Methods of VTE prophylaxis National Consensus Standards for Prevention and Care of VTE (CMS as well? ) Factors related to under-use of established guidelines Strategies to improve compliance
 Background / Prevalence of VTE n n n PE is responsible for up to 200 K deaths per year in the United States¹ PE remains the most common preventable cause of hospital death, accounting for up to 10%² DVT/PE is much more common in the hospitalized patient -- medical and surgical³ 1. Horlander, KT, Mannino, DM, Leeper, KV. Arch Intern Med 2003; 163: 1711 2. Pendleton R et al. Am J Hemat. 2005; 79: 229 -237. 3. Edelsberg J et al. Am J Health Syst Pharm 2006; 63: 16 S-22 S
Background / Prevalence of VTE n n n PE is responsible for up to 200 K deaths per year in the United States¹ PE remains the most common preventable cause of hospital death, accounting for up to 10%² DVT/PE is much more common in the hospitalized patient -- medical and surgical³ 1. Horlander, KT, Mannino, DM, Leeper, KV. Arch Intern Med 2003; 163: 1711 2. Pendleton R et al. Am J Hemat. 2005; 79: 229 -237. 3. Edelsberg J et al. Am J Health Syst Pharm 2006; 63: 16 S-22 S
 Background / Prevalence n VTE is more than 130 times greater among hospitalized patients than community residents¹ half of community-based cases nursing home patients or within 90 days of hospital discharge n 60% of all cases occurred in either hospitalized, recently d/c’d, or NH patients! n n Hospitalization for acute medical illness is associated with up to an 8 -fold increase in relative risk for VTE 1. Heit, JA, Melton, LJ, Lohse, CM, et al. Mayo Clin Proc 2001; 76: 1102
Background / Prevalence n VTE is more than 130 times greater among hospitalized patients than community residents¹ half of community-based cases nursing home patients or within 90 days of hospital discharge n 60% of all cases occurred in either hospitalized, recently d/c’d, or NH patients! n n Hospitalization for acute medical illness is associated with up to an 8 -fold increase in relative risk for VTE 1. Heit, JA, Melton, LJ, Lohse, CM, et al. Mayo Clin Proc 2001; 76: 1102
 Background / Prevalence n n n Death occurs in about 6% of DVT cases within one month of diagnosis 1 Death occurs in about 12% of PE cases within one month of diagnosis 1 Up to 25% of distal DVT can propagate into proximal DVT² Pulmonary emboli are detected in approximately 50% of patients with proximal DVT² Recurrent DVT: n Can occur in 30% of DVT patients within 10 years after initial treatment³ 1. American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. 2. Anand, SA et al. JAMA. 1998; 279: 1094 -1099. 3. Prandoni P et al. Haemotologia 2007; 92: 199 -205
Background / Prevalence n n n Death occurs in about 6% of DVT cases within one month of diagnosis 1 Death occurs in about 12% of PE cases within one month of diagnosis 1 Up to 25% of distal DVT can propagate into proximal DVT² Pulmonary emboli are detected in approximately 50% of patients with proximal DVT² Recurrent DVT: n Can occur in 30% of DVT patients within 10 years after initial treatment³ 1. American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. 2. Anand, SA et al. JAMA. 1998; 279: 1094 -1099. 3. Prandoni P et al. Haemotologia 2007; 92: 199 -205
 Background / Prevalence¹ n Without prophylaxis, overall DVT incidence in hospitalized medical and general surgical patients is 10 -40% n n 40 -60% following major orthopedic surgery Without prophylaxis, fatal PE occurs with the following frequency in hospitalized patients: 0. 1 -0. 8% undergoing elective general surgery n 2 -3% undergoing elective hip replacement n 4 -7% undergoing surgery for fractured hip! n 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S
Background / Prevalence¹ n Without prophylaxis, overall DVT incidence in hospitalized medical and general surgical patients is 10 -40% n n 40 -60% following major orthopedic surgery Without prophylaxis, fatal PE occurs with the following frequency in hospitalized patients: 0. 1 -0. 8% undergoing elective general surgery n 2 -3% undergoing elective hip replacement n 4 -7% undergoing surgery for fractured hip! n 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S
 Background / Prevalence n Without prophylaxis, reported VTE occurrence in the ICU ranges between <10% to nearly 100%!! Virtually all critical care patients are at moderate to high risk Up to 10% to 15% of patients with cancer may develop a VTE 1 Malignancy independent factor for decreased early and late survival after VTE event² n n n 1. Viale PH, Schwartz RN. Clin J Onco Nurs. 2004; 8: 455 -461. 2. Heit JA et al. Arch Intern Med. 1999; 159: 445 -453
Background / Prevalence n Without prophylaxis, reported VTE occurrence in the ICU ranges between <10% to nearly 100%!! Virtually all critical care patients are at moderate to high risk Up to 10% to 15% of patients with cancer may develop a VTE 1 Malignancy independent factor for decreased early and late survival after VTE event² n n n 1. Viale PH, Schwartz RN. Clin J Onco Nurs. 2004; 8: 455 -461. 2. Heit JA et al. Arch Intern Med. 1999; 159: 445 -453
 Consequences of Unprevented VTE n n n n Fatal PE -- usually occurs without warning and often with no potential to resuscitate¹ Patient discomfort associated with VTE n Initial pain and discomfort n Post-thrombotic syndrome (PTS)² n Chronic Thromboembolic Pulmonary Hypertension (CTPH)³ $$ spent in the investigation of suspected and treatment of documented VTE Risk of treatment once VTE occurs Increased length of initialhospital stay More frequent hospital readmission Increased future risk of VTE (4) 1. Anderson FA et al. Arch Intern Med 1991; 151: 933 -8 2. Büller, HR et al. Chest. 2004; 126: 4018 -4288. 3. Pengo V et al. N Engl. J Med. 2004; 350: 2257 -2264. 4. Heit JA et al. Arch Intern Med 2000; 160: 761 -8
Consequences of Unprevented VTE n n n n Fatal PE -- usually occurs without warning and often with no potential to resuscitate¹ Patient discomfort associated with VTE n Initial pain and discomfort n Post-thrombotic syndrome (PTS)² n Chronic Thromboembolic Pulmonary Hypertension (CTPH)³ $$ spent in the investigation of suspected and treatment of documented VTE Risk of treatment once VTE occurs Increased length of initialhospital stay More frequent hospital readmission Increased future risk of VTE (4) 1. Anderson FA et al. Arch Intern Med 1991; 151: 933 -8 2. Büller, HR et al. Chest. 2004; 126: 4018 -4288. 3. Pengo V et al. N Engl. J Med. 2004; 350: 2257 -2264. 4. Heit JA et al. Arch Intern Med 2000; 160: 761 -8
 Benefits / Rationale of VTE Prophylaxis n n n DVT and PE are prevalent and serious complications 1 Difficult to predict with any certainty which patients will develop VTE² Patients can experience VTE weeks after surgery 2 Clinical consequences of VTE, including mortality, are common 3 Health burden associated with VTE is expected to grow dramatically during coming years, in part due to aging population (4) 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S. 2. White RH et al. Arch Intern Med. 1998; 158: 1525 -1531. 3. Pengo V et al. N Engl J Med. 2004; 350: 2257 -2264. 4. Stein PQ et al. Arch Intern Med 2004. 164: 2260 -65
Benefits / Rationale of VTE Prophylaxis n n n DVT and PE are prevalent and serious complications 1 Difficult to predict with any certainty which patients will develop VTE² Patients can experience VTE weeks after surgery 2 Clinical consequences of VTE, including mortality, are common 3 Health burden associated with VTE is expected to grow dramatically during coming years, in part due to aging population (4) 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S. 2. White RH et al. Arch Intern Med. 1998; 158: 1525 -1531. 3. Pengo V et al. N Engl J Med. 2004; 350: 2257 -2264. 4. Stein PQ et al. Arch Intern Med 2004. 164: 2260 -65
 Benefits / Rationale of VTE Prophylaxis¹ n n Hospital-acquired DVT/PE is usually clinically silent -only 1/3 present with classic symptoms² Overall incidence likely underestimated³ Screening, either by physical exam or noninvasive testing, is not clinically effective or cost effective Prophylaxis is far more effective for preventing death/morbidity from VTE than is treatment of established disease 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S 2. Turkstra F et al. Ann Intern Med 1997; 126: 775 -81 3. Kyrle PA et al. Lancet 2005; 365: 1163 -74
Benefits / Rationale of VTE Prophylaxis¹ n n Hospital-acquired DVT/PE is usually clinically silent -only 1/3 present with classic symptoms² Overall incidence likely underestimated³ Screening, either by physical exam or noninvasive testing, is not clinically effective or cost effective Prophylaxis is far more effective for preventing death/morbidity from VTE than is treatment of established disease 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S 2. Turkstra F et al. Ann Intern Med 1997; 126: 775 -81 3. Kyrle PA et al. Lancet 2005; 365: 1163 -74
 Benefits / Rationale of VTE prophylaxis n n n Effective and safe prophylactic measures are available for most high-risk patients (1, 2) n pharmacologic prophylaxis lowers the risk of symptomatic and asymptomatic VTE in medical patients by 50%-75%! n little or no increase in rates of clinically important bleeding complications Based on solid principles and scientific evidence from large numbers of randomized clinical trials³ Most hospitalized patients have one or more risk factor for VTE – and importantly, these are cumulative(4) 1. Gerotziafas, GT, Samama, MM. Curr Opin Pulm Med 2004; 10: 356 2. Clagett, GP, Reisch, JS. Ann Surg 1988; 208: 227 3. Patel R et al. J Crit Care 2005; 20: 34 -7 4. Dorfman, et al. J Clin Pharm Therap 2006; 31: 455 -9
Benefits / Rationale of VTE prophylaxis n n n Effective and safe prophylactic measures are available for most high-risk patients (1, 2) n pharmacologic prophylaxis lowers the risk of symptomatic and asymptomatic VTE in medical patients by 50%-75%! n little or no increase in rates of clinically important bleeding complications Based on solid principles and scientific evidence from large numbers of randomized clinical trials³ Most hospitalized patients have one or more risk factor for VTE – and importantly, these are cumulative(4) 1. Gerotziafas, GT, Samama, MM. Curr Opin Pulm Med 2004; 10: 356 2. Clagett, GP, Reisch, JS. Ann Surg 1988; 208: 227 3. Patel R et al. J Crit Care 2005; 20: 34 -7 4. Dorfman, et al. J Clin Pharm Therap 2006; 31: 455 -9
 Benefits of VTE Prophylaxis n Appropriate VTE prophylaxis achieves two very desirable results: n n Improved patient outcomes Reduced costs
Benefits of VTE Prophylaxis n Appropriate VTE prophylaxis achieves two very desirable results: n n Improved patient outcomes Reduced costs
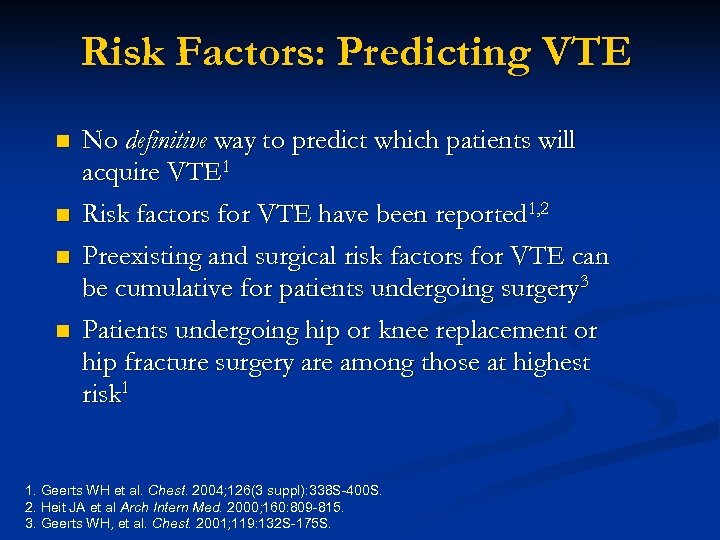 Risk Factors: Predicting VTE n n No definitive way to predict which patients will acquire VTE 1 Risk factors for VTE have been reported 1, 2 Preexisting and surgical risk factors for VTE can be cumulative for patients undergoing surgery 3 Patients undergoing hip or knee replacement or hip fracture surgery are among those at highest risk 1 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S. 2. Heit JA et al Arch Intern Med. 2000; 160: 809 -815. 3. Geerts WH, et al. Chest. 2001; 119: 132 S-175 S.
Risk Factors: Predicting VTE n n No definitive way to predict which patients will acquire VTE 1 Risk factors for VTE have been reported 1, 2 Preexisting and surgical risk factors for VTE can be cumulative for patients undergoing surgery 3 Patients undergoing hip or knee replacement or hip fracture surgery are among those at highest risk 1 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S. 2. Heit JA et al Arch Intern Med. 2000; 160: 809 -815. 3. Geerts WH, et al. Chest. 2001; 119: 132 S-175 S.
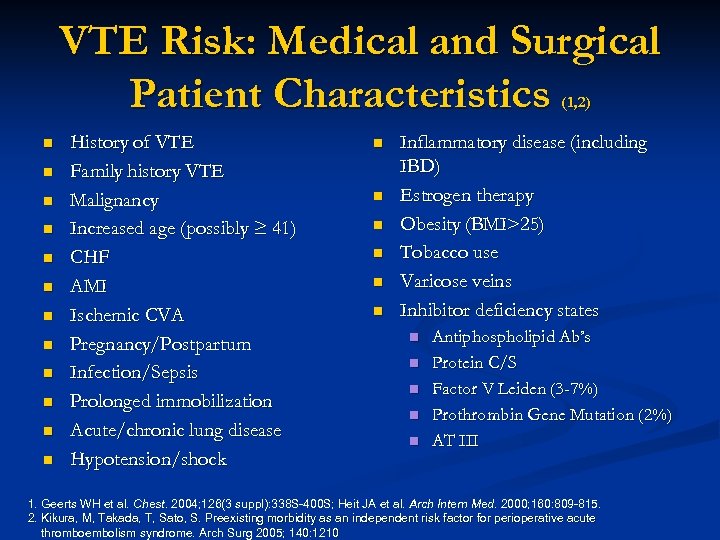 VTE Risk: Medical and Surgical Patient Characteristics (1, 2) n n n History of VTE Family history VTE Malignancy Increased age (possibly ≥ 41) CHF AMI Ischemic CVA Pregnancy/Postpartum Infection/Sepsis Prolonged immobilization Acute/chronic lung disease Hypotension/shock n n n Inflammatory disease (including IBD) Estrogen therapy Obesity (BMI>25) Tobacco use Varicose veins Inhibitor deficiency states n n n Antiphospholipid Ab’s Protein C/S Factor V Leiden (3 -7%) Prothrombin Gene Mutation (2%) AT III 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S; Heit JA et al. Arch Intern Med. 2000; 160: 809 -815. 2. Kikura, M, Takada, T, Sato, S. Preexisting morbidity as an independent risk factor for perioperative acute thromboembolism syndrome. Arch Surg 2005; 140: 1210
VTE Risk: Medical and Surgical Patient Characteristics (1, 2) n n n History of VTE Family history VTE Malignancy Increased age (possibly ≥ 41) CHF AMI Ischemic CVA Pregnancy/Postpartum Infection/Sepsis Prolonged immobilization Acute/chronic lung disease Hypotension/shock n n n Inflammatory disease (including IBD) Estrogen therapy Obesity (BMI>25) Tobacco use Varicose veins Inhibitor deficiency states n n n Antiphospholipid Ab’s Protein C/S Factor V Leiden (3 -7%) Prothrombin Gene Mutation (2%) AT III 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S; Heit JA et al. Arch Intern Med. 2000; 160: 809 -815. 2. Kikura, M, Takada, T, Sato, S. Preexisting morbidity as an independent risk factor for perioperative acute thromboembolism syndrome. Arch Surg 2005; 140: 1210
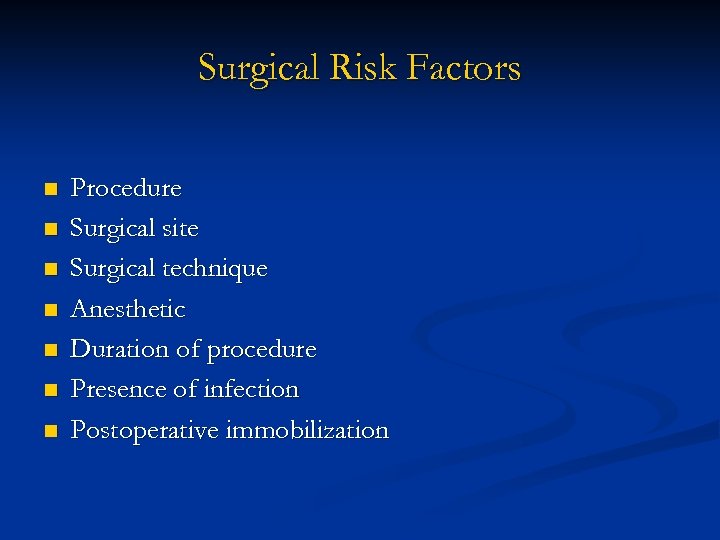 Surgical Risk Factors n n n n Procedure Surgical site Surgical technique Anesthetic Duration of procedure Presence of infection Postoperative immobilization
Surgical Risk Factors n n n n Procedure Surgical site Surgical technique Anesthetic Duration of procedure Presence of infection Postoperative immobilization
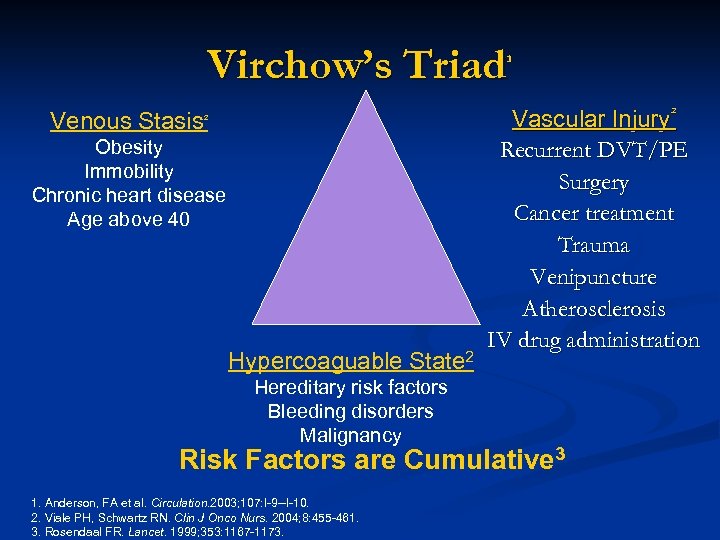 Virchow’s Triad¹ Venous Stasis² Obesity Immobility Chronic heart disease Age above 40 Hypercoaguable State 2 Hereditary risk factors Bleeding disorders Malignancy Vascular Injury² Recurrent DVT/PE Surgery Cancer treatment Trauma Venipuncture Atherosclerosis IV drug administration Risk Factors are Cumulative 3 1. Anderson, FA et al. Circulation. 2003; 107: I-9 --I-10. 2. Viale PH, Schwartz RN. Clin J Onco Nurs. 2004; 8: 455 -461. 3. Rosendaal FR. Lancet. 1999; 353: 1167 -1173.
Virchow’s Triad¹ Venous Stasis² Obesity Immobility Chronic heart disease Age above 40 Hypercoaguable State 2 Hereditary risk factors Bleeding disorders Malignancy Vascular Injury² Recurrent DVT/PE Surgery Cancer treatment Trauma Venipuncture Atherosclerosis IV drug administration Risk Factors are Cumulative 3 1. Anderson, FA et al. Circulation. 2003; 107: I-9 --I-10. 2. Viale PH, Schwartz RN. Clin J Onco Nurs. 2004; 8: 455 -461. 3. Rosendaal FR. Lancet. 1999; 353: 1167 -1173.
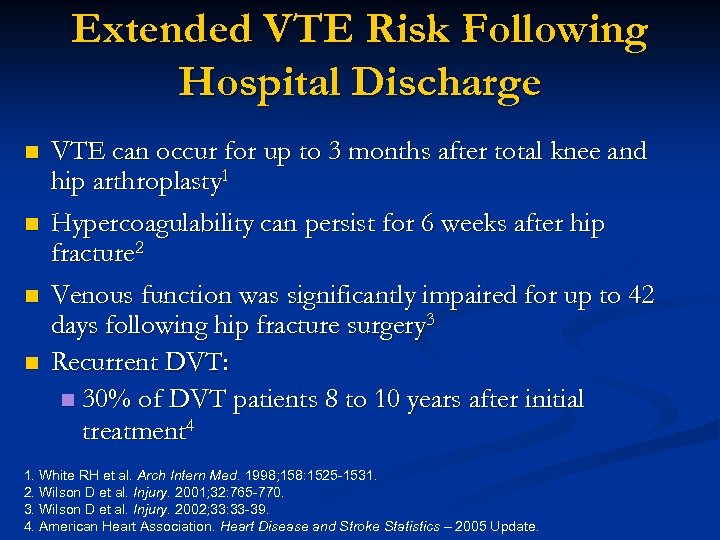 Extended VTE Risk Following Hospital Discharge n n VTE can occur for up to 3 months after total knee and hip arthroplasty 1 Hypercoagulability can persist for 6 weeks after hip fracture 2 Venous function was significantly impaired for up to 42 days following hip fracture surgery 3 Recurrent DVT: n 30% of DVT patients 8 to 10 years after initial treatment 4 1. White RH et al. Arch Intern Med. 1998; 158: 1525 -1531. 2. Wilson D et al. Injury. 2001; 32: 765 -770. 3. Wilson D et al. Injury. 2002; 33: 33 -39. 4. American Heart Association. Heart Disease and Stroke Statistics – 2005 Update.
Extended VTE Risk Following Hospital Discharge n n VTE can occur for up to 3 months after total knee and hip arthroplasty 1 Hypercoagulability can persist for 6 weeks after hip fracture 2 Venous function was significantly impaired for up to 42 days following hip fracture surgery 3 Recurrent DVT: n 30% of DVT patients 8 to 10 years after initial treatment 4 1. White RH et al. Arch Intern Med. 1998; 158: 1525 -1531. 2. Wilson D et al. Injury. 2001; 32: 765 -770. 3. Wilson D et al. Injury. 2002; 33: 33 -39. 4. American Heart Association. Heart Disease and Stroke Statistics – 2005 Update.
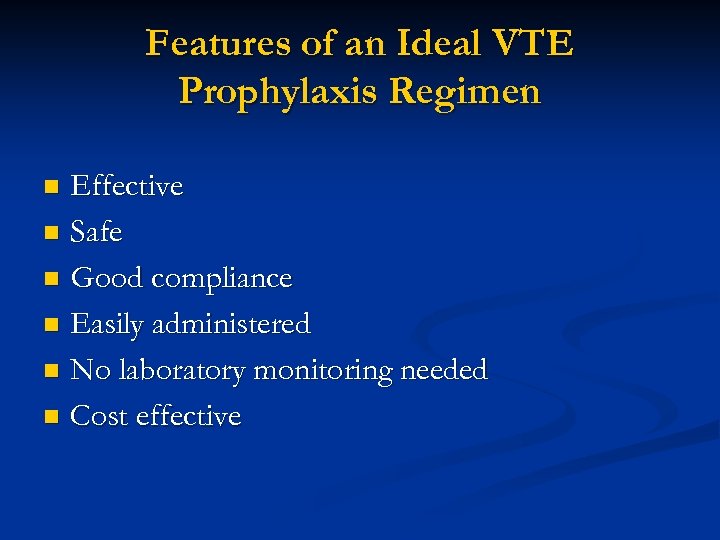 Features of an Ideal VTE Prophylaxis Regimen Effective n Safe n Good compliance n Easily administered n No laboratory monitoring needed n Cost effective n
Features of an Ideal VTE Prophylaxis Regimen Effective n Safe n Good compliance n Easily administered n No laboratory monitoring needed n Cost effective n
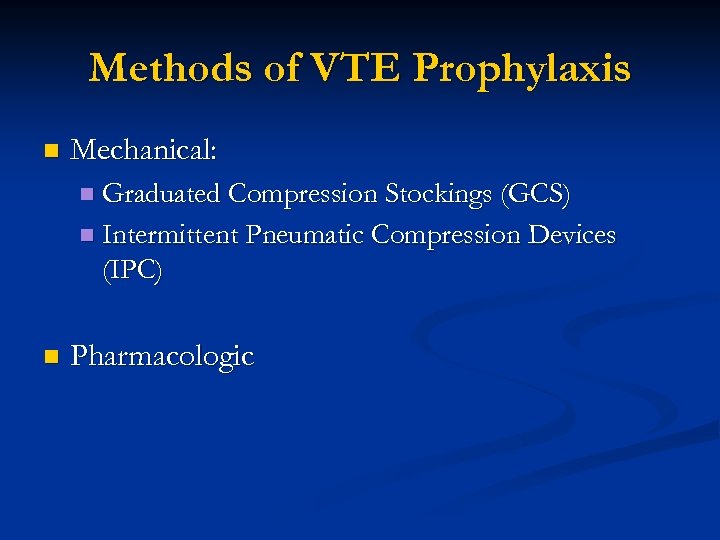 Methods of VTE Prophylaxis n Mechanical: n Graduated Compression Stockings (GCS) n Intermittent Pneumatic Compression Devices (IPC) n Pharmacologic
Methods of VTE Prophylaxis n Mechanical: n Graduated Compression Stockings (GCS) n Intermittent Pneumatic Compression Devices (IPC) n Pharmacologic
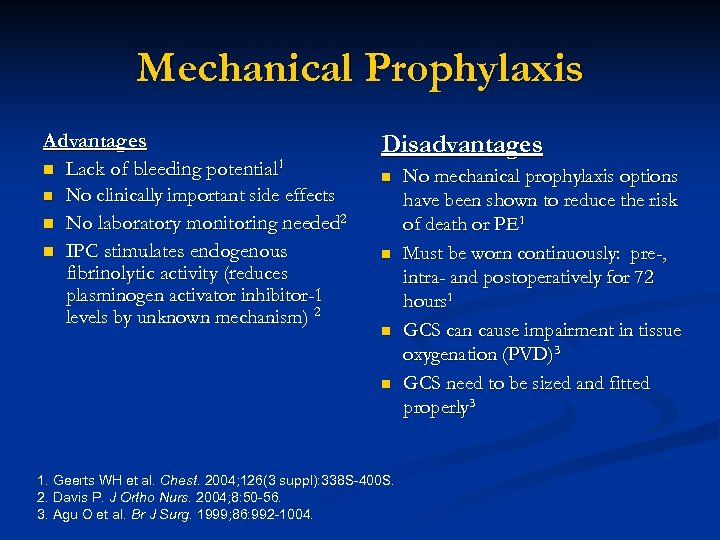 Mechanical Prophylaxis Advantages n Lack of bleeding potential 1 n No clinically important side effects n No laboratory monitoring needed 2 n IPC stimulates endogenous fibrinolytic activity (reduces plasminogen activator inhibitor-1 levels by unknown mechanism) 2 Disadvantages n n 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S. 2. Davis P. J Ortho Nurs. 2004; 8: 50 -56. 3. Agu O et al. Br J Surg. 1999; 86: 992 -1004. No mechanical prophylaxis options have been shown to reduce the risk of death or PE 1 Must be worn continuously: pre-, intra- and postoperatively for 72 hours 1 GCS can cause impairment in tissue oxygenation (PVD)3 GCS need to be sized and fitted properly 3
Mechanical Prophylaxis Advantages n Lack of bleeding potential 1 n No clinically important side effects n No laboratory monitoring needed 2 n IPC stimulates endogenous fibrinolytic activity (reduces plasminogen activator inhibitor-1 levels by unknown mechanism) 2 Disadvantages n n 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S. 2. Davis P. J Ortho Nurs. 2004; 8: 50 -56. 3. Agu O et al. Br J Surg. 1999; 86: 992 -1004. No mechanical prophylaxis options have been shown to reduce the risk of death or PE 1 Must be worn continuously: pre-, intra- and postoperatively for 72 hours 1 GCS can cause impairment in tissue oxygenation (PVD)3 GCS need to be sized and fitted properly 3
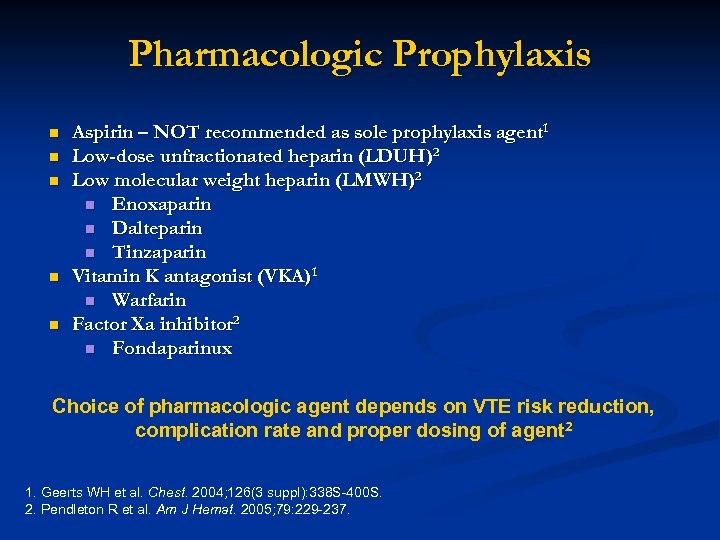 Pharmacologic Prophylaxis n n n Aspirin – NOT recommended as sole prophylaxis agent 1 Low-dose unfractionated heparin (LDUH)2 Low molecular weight heparin (LMWH)2 n Enoxaparin n Dalteparin n Tinzaparin Vitamin K antagonist (VKA)1 n Warfarin Factor Xa inhibitor 2 n Fondaparinux Choice of pharmacologic agent depends on VTE risk reduction, complication rate and proper dosing of agent 2 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S. 2. Pendleton R et al. Am J Hemat. 2005; 79: 229 -237.
Pharmacologic Prophylaxis n n n Aspirin – NOT recommended as sole prophylaxis agent 1 Low-dose unfractionated heparin (LDUH)2 Low molecular weight heparin (LMWH)2 n Enoxaparin n Dalteparin n Tinzaparin Vitamin K antagonist (VKA)1 n Warfarin Factor Xa inhibitor 2 n Fondaparinux Choice of pharmacologic agent depends on VTE risk reduction, complication rate and proper dosing of agent 2 1. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S. 2. Pendleton R et al. Am J Hemat. 2005; 79: 229 -237.
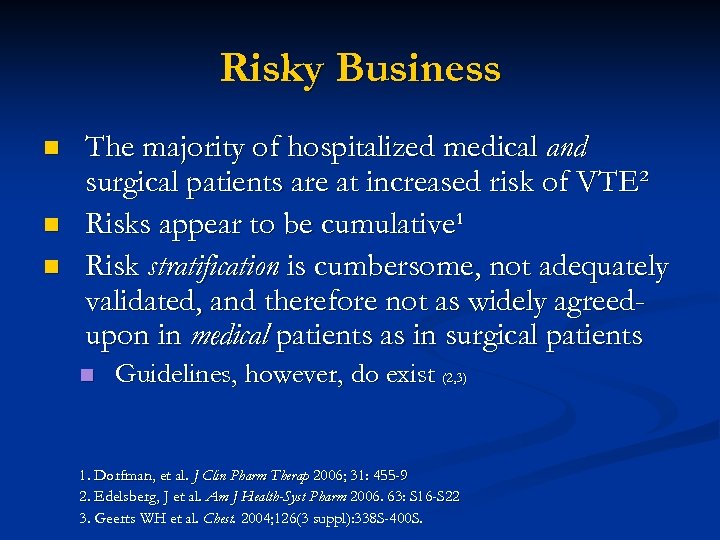 Risky Business n n n The majority of hospitalized medical and surgical patients are at increased risk of VTE² Risks appear to be cumulative¹ Risk stratification is cumbersome, not adequately validated, and therefore not as widely agreedupon in medical patients as in surgical patients n Guidelines, however, do exist (2, 3) 1. Dorfman, et al. J Clin Pharm Therap 2006; 31: 455 -9 2. Edelsberg, J et al. Am J Health-Syst Pharm 2006. 63: S 16 -S 22 3. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S.
Risky Business n n n The majority of hospitalized medical and surgical patients are at increased risk of VTE² Risks appear to be cumulative¹ Risk stratification is cumbersome, not adequately validated, and therefore not as widely agreedupon in medical patients as in surgical patients n Guidelines, however, do exist (2, 3) 1. Dorfman, et al. J Clin Pharm Therap 2006; 31: 455 -9 2. Edelsberg, J et al. Am J Health-Syst Pharm 2006. 63: S 16 -S 22 3. Geerts WH et al. Chest. 2004; 126(3 suppl): 338 S-400 S.
 ACCP Recommendations (since 1986) n Geerts, WH, et al. CHEST 2004; 126: 338 s-400 s
ACCP Recommendations (since 1986) n Geerts, WH, et al. CHEST 2004; 126: 338 s-400 s
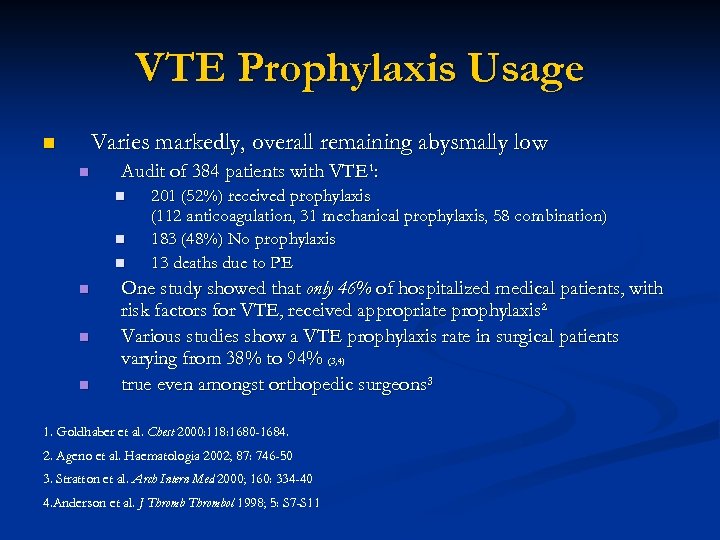 VTE Prophylaxis Usage Varies markedly, overall remaining abysmally low n n Audit of 384 patients with VTE¹: n n n 201 (52%) received prophylaxis (112 anticoagulation, 31 mechanical prophylaxis, 58 combination) 183 (48%) No prophylaxis 13 deaths due to PE One study showed that only 46% of hospitalized medical patients, with risk factors for VTE, received appropriate prophylaxis² Various studies show a VTE prophylaxis rate in surgical patients varying from 38% to 94% (3, 4) true even amongst orthopedic surgeons³ 1. Goldhaber et al. Chest 2000: 118: 1680 -1684. 2. Ageno et al. Haematologia 2002; 87: 746 -50 3. Stratton et al. Arch Intern Med 2000; 160: 334 -40 4. Anderson et al. J Thrombol 1998; 5: S 7 -S 11
VTE Prophylaxis Usage Varies markedly, overall remaining abysmally low n n Audit of 384 patients with VTE¹: n n n 201 (52%) received prophylaxis (112 anticoagulation, 31 mechanical prophylaxis, 58 combination) 183 (48%) No prophylaxis 13 deaths due to PE One study showed that only 46% of hospitalized medical patients, with risk factors for VTE, received appropriate prophylaxis² Various studies show a VTE prophylaxis rate in surgical patients varying from 38% to 94% (3, 4) true even amongst orthopedic surgeons³ 1. Goldhaber et al. Chest 2000: 118: 1680 -1684. 2. Ageno et al. Haematologia 2002; 87: 746 -50 3. Stratton et al. Arch Intern Med 2000; 160: 334 -40 4. Anderson et al. J Thrombol 1998; 5: S 7 -S 11
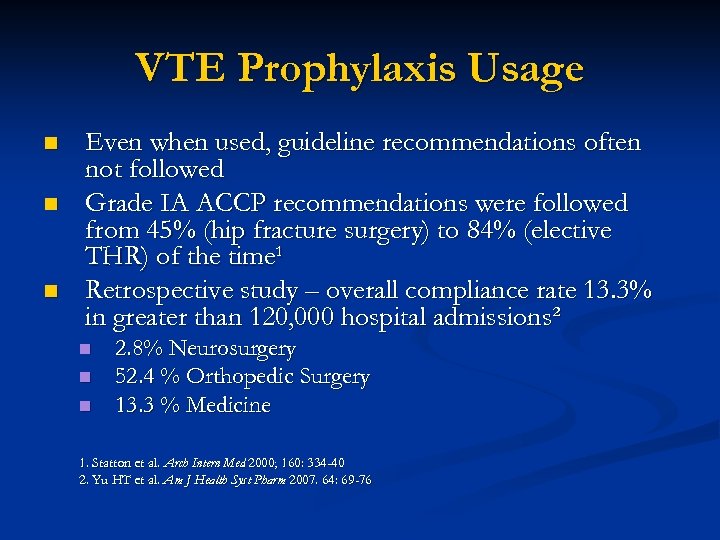 VTE Prophylaxis Usage n n n Even when used, guideline recommendations often not followed Grade IA ACCP recommendations were followed from 45% (hip fracture surgery) to 84% (elective THR) of the time¹ Retrospective study – overall compliance rate 13. 3% in greater than 120, 000 hospital admissions² n n n 2. 8% Neurosurgery 52. 4 % Orthopedic Surgery 13. 3 % Medicine 1. Statton et al. Arch Intern Med 2000; 160: 334 -40 2. Yu HT et al. Am J Health Syst Pharm 2007. 64: 69 -76
VTE Prophylaxis Usage n n n Even when used, guideline recommendations often not followed Grade IA ACCP recommendations were followed from 45% (hip fracture surgery) to 84% (elective THR) of the time¹ Retrospective study – overall compliance rate 13. 3% in greater than 120, 000 hospital admissions² n n n 2. 8% Neurosurgery 52. 4 % Orthopedic Surgery 13. 3 % Medicine 1. Statton et al. Arch Intern Med 2000; 160: 334 -40 2. Yu HT et al. Am J Health Syst Pharm 2007. 64: 69 -76
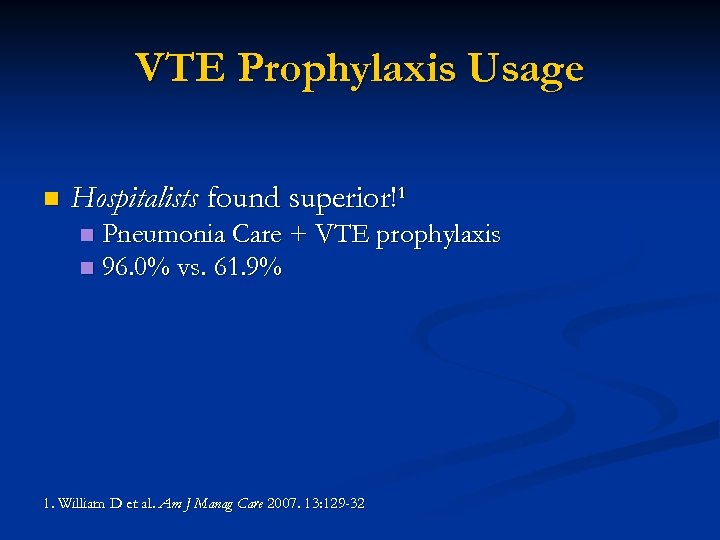 VTE Prophylaxis Usage n Hospitalists found superior!¹ Pneumonia Care + VTE prophylaxis n 96. 0% vs. 61. 9% n 1. William D et al. Am J Manag Care 2007. 13: 129 -32
VTE Prophylaxis Usage n Hospitalists found superior!¹ Pneumonia Care + VTE prophylaxis n 96. 0% vs. 61. 9% n 1. William D et al. Am J Manag Care 2007. 13: 129 -32
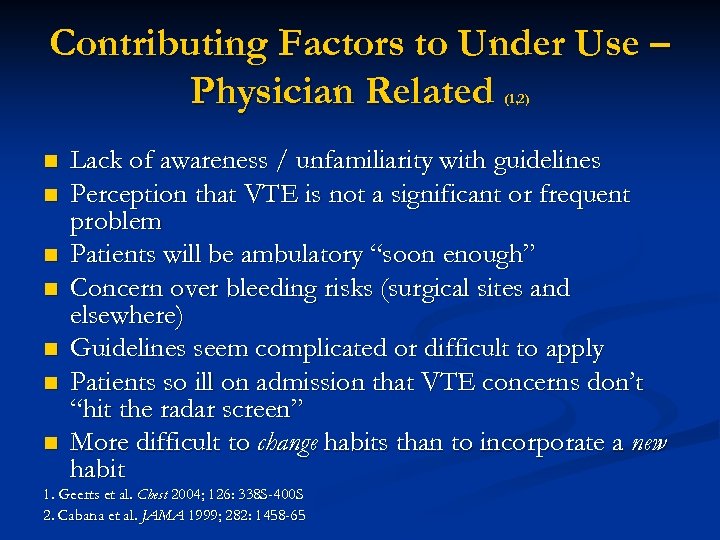 Contributing Factors to Under Use – Physician Related (1, 2) n n n n Lack of awareness / unfamiliarity with guidelines Perception that VTE is not a significant or frequent problem Patients will be ambulatory “soon enough” Concern over bleeding risks (surgical sites and elsewhere) Guidelines seem complicated or difficult to apply Patients so ill on admission that VTE concerns don’t “hit the radar screen” More difficult to change habits than to incorporate a new habit 1. Geerts et al. Chest 2004; 126: 338 S-400 S 2. Cabana et al. JAMA 1999; 282: 1458 -65
Contributing Factors to Under Use – Physician Related (1, 2) n n n n Lack of awareness / unfamiliarity with guidelines Perception that VTE is not a significant or frequent problem Patients will be ambulatory “soon enough” Concern over bleeding risks (surgical sites and elsewhere) Guidelines seem complicated or difficult to apply Patients so ill on admission that VTE concerns don’t “hit the radar screen” More difficult to change habits than to incorporate a new habit 1. Geerts et al. Chest 2004; 126: 338 S-400 S 2. Cabana et al. JAMA 1999; 282: 1458 -65
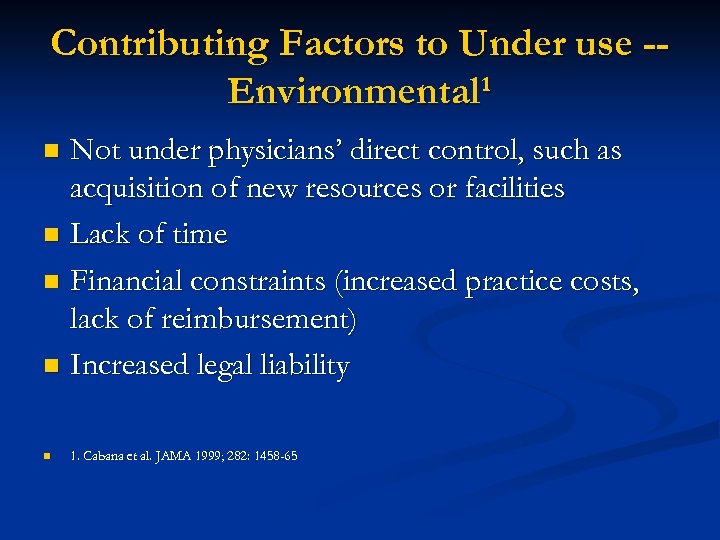 Contributing Factors to Under use -Environmental¹ Not under physicians’ direct control, such as acquisition of new resources or facilities n Lack of time n Financial constraints (increased practice costs, lack of reimbursement) n Increased legal liability n n 1. Cabana et al. JAMA 1999; 282: 1458 -65
Contributing Factors to Under use -Environmental¹ Not under physicians’ direct control, such as acquisition of new resources or facilities n Lack of time n Financial constraints (increased practice costs, lack of reimbursement) n Increased legal liability n n 1. Cabana et al. JAMA 1999; 282: 1458 -65
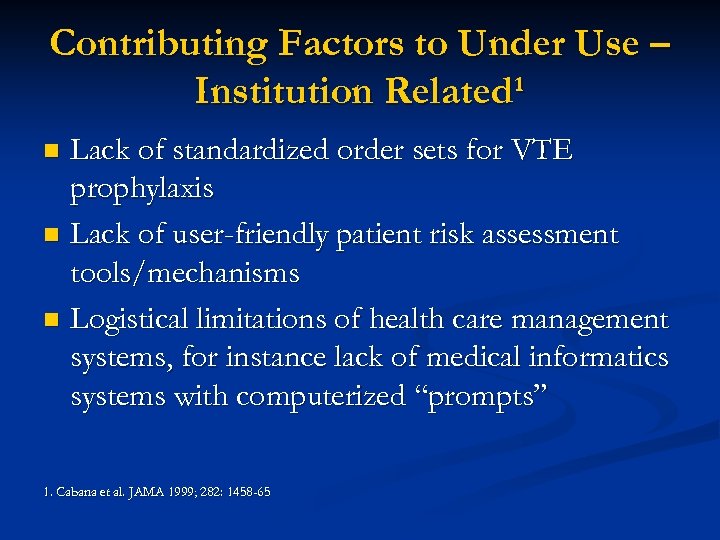 Contributing Factors to Under Use – Institution Related¹ Lack of standardized order sets for VTE prophylaxis n Lack of user-friendly patient risk assessment tools/mechanisms n Logistical limitations of health care management systems, for instance lack of medical informatics systems with computerized “prompts” n 1. Cabana et al. JAMA 1999; 282: 1458 -65
Contributing Factors to Under Use – Institution Related¹ Lack of standardized order sets for VTE prophylaxis n Lack of user-friendly patient risk assessment tools/mechanisms n Logistical limitations of health care management systems, for instance lack of medical informatics systems with computerized “prompts” n 1. Cabana et al. JAMA 1999; 282: 1458 -65
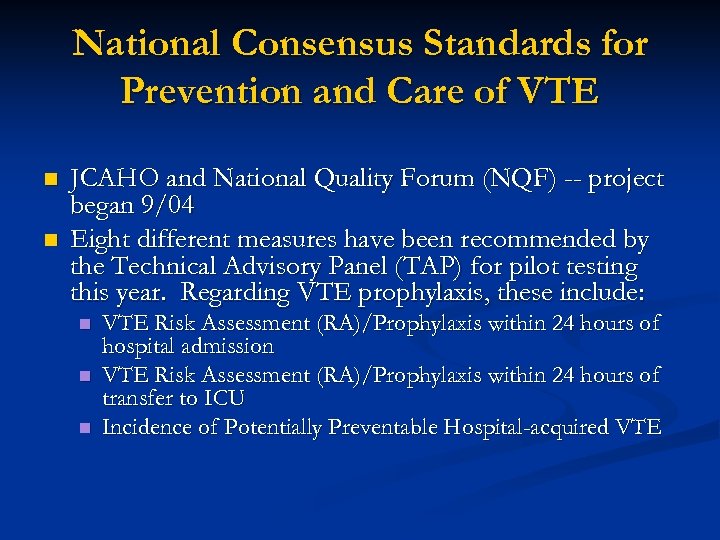 National Consensus Standards for Prevention and Care of VTE n n JCAHO and National Quality Forum (NQF) -- project began 9/04 Eight different measures have been recommended by the Technical Advisory Panel (TAP) for pilot testing this year. Regarding VTE prophylaxis, these include: n n n VTE Risk Assessment (RA)/Prophylaxis within 24 hours of hospital admission VTE Risk Assessment (RA)/Prophylaxis within 24 hours of transfer to ICU Incidence of Potentially Preventable Hospital-acquired VTE
National Consensus Standards for Prevention and Care of VTE n n JCAHO and National Quality Forum (NQF) -- project began 9/04 Eight different measures have been recommended by the Technical Advisory Panel (TAP) for pilot testing this year. Regarding VTE prophylaxis, these include: n n n VTE Risk Assessment (RA)/Prophylaxis within 24 hours of hospital admission VTE Risk Assessment (RA)/Prophylaxis within 24 hours of transfer to ICU Incidence of Potentially Preventable Hospital-acquired VTE
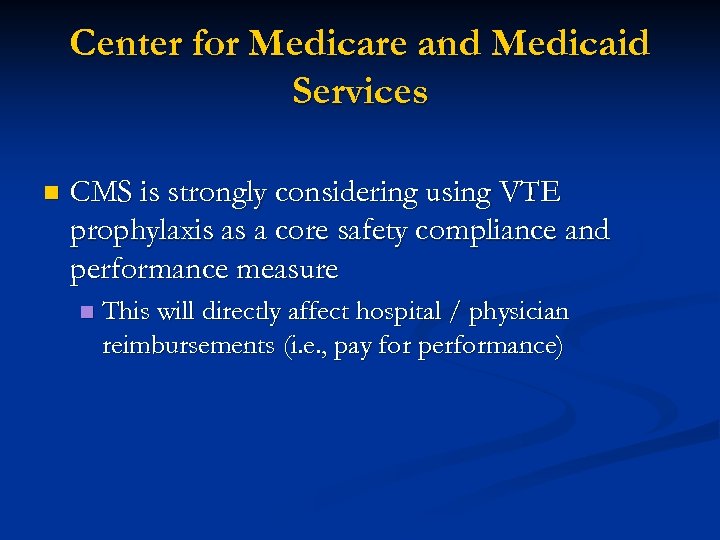 Center for Medicare and Medicaid Services n CMS is strongly considering using VTE prophylaxis as a core safety compliance and performance measure n This will directly affect hospital / physician reimbursements (i. e. , pay for performance)
Center for Medicare and Medicaid Services n CMS is strongly considering using VTE prophylaxis as a core safety compliance and performance measure n This will directly affect hospital / physician reimbursements (i. e. , pay for performance)
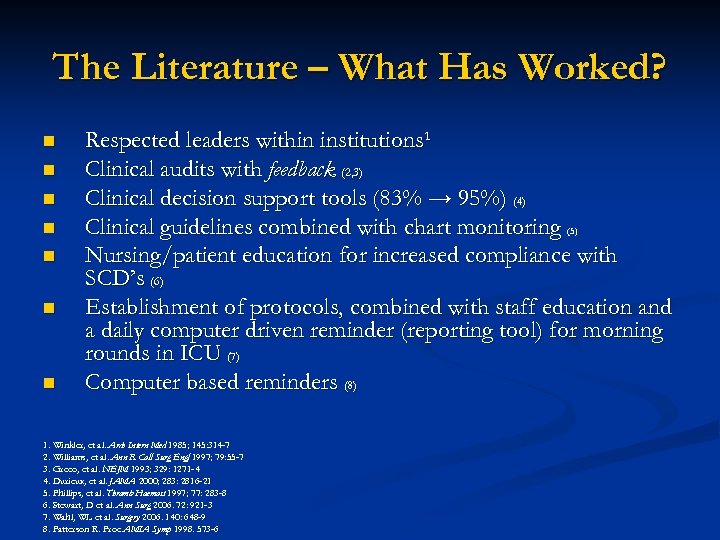 The Literature – What Has Worked? n n n n Respected leaders within institutions¹ Clinical audits with feedback (2, 3) Clinical decision support tools (83% → 95%) (4) Clinical guidelines combined with chart monitoring (5) Nursing/patient education for increased compliance with SCD’s (6) Establishment of protocols, combined with staff education and a daily computer driven reminder (reporting tool) for morning rounds in ICU (7) Computer based reminders (8) 1. Winkler, et al. Arch Intern Med 1985; 145: 314 -7 2. Williams, et al. Ann R Coll Surg Engl 1997; 79: 55 -7 3. Greco, et al. NEJM 1993; 329: 1271 -4 4. Durieux, et al. JAMA 2000; 283: 2816 -21 5. Phillips, et al. Thromb Haemost 1997; 77: 283 -8 6. Stewart, D et al. Ann Surg 2006. 72: 921 -3 7. Wahl, WL et al. Surgery 2006. 140: 648 -9 8. Patterson R. Proc AMIA Symp 1998. 573 -6
The Literature – What Has Worked? n n n n Respected leaders within institutions¹ Clinical audits with feedback (2, 3) Clinical decision support tools (83% → 95%) (4) Clinical guidelines combined with chart monitoring (5) Nursing/patient education for increased compliance with SCD’s (6) Establishment of protocols, combined with staff education and a daily computer driven reminder (reporting tool) for morning rounds in ICU (7) Computer based reminders (8) 1. Winkler, et al. Arch Intern Med 1985; 145: 314 -7 2. Williams, et al. Ann R Coll Surg Engl 1997; 79: 55 -7 3. Greco, et al. NEJM 1993; 329: 1271 -4 4. Durieux, et al. JAMA 2000; 283: 2816 -21 5. Phillips, et al. Thromb Haemost 1997; 77: 283 -8 6. Stewart, D et al. Ann Surg 2006. 72: 921 -3 7. Wahl, WL et al. Surgery 2006. 140: 648 -9 8. Patterson R. Proc AMIA Symp 1998. 573 -6
 Future Directions -- UCHSC Increase overall VTE prophylaxis compliance n Improved methods of risk stratification n Increased adherence to established guidelines n Proposed results: n Improved patient safety and outcomes n Improved adherence to JHACO / CMS standards and institutionally established compliance targets/goals n
Future Directions -- UCHSC Increase overall VTE prophylaxis compliance n Improved methods of risk stratification n Increased adherence to established guidelines n Proposed results: n Improved patient safety and outcomes n Improved adherence to JHACO / CMS standards and institutionally established compliance targets/goals n
 Proposed Study - UCHSC n Prospective historical controlled trial Develop simple, useable method of VTE risk stratification n Utilize prompts – written and eventually electronic n Measure compliance rates compared to historic rates n
Proposed Study - UCHSC n Prospective historical controlled trial Develop simple, useable method of VTE risk stratification n Utilize prompts – written and eventually electronic n Measure compliance rates compared to historic rates n
 Methods n n n Using established risk factors, develop simple, useable method of risk stratifications for clinicians, using methods that have proved effective¹ n Initially paper admission/transfer orders n With CPOE, add as “pop-up”² n Include current ACCP guidelines Use medication reconciliation sheets/orders as reminder n Forms would be mandatory for all admissions/transfers n Again, with CPOE, would be contained therein Measure rates of physician compliance and choice of method on high-risk patients (2 or more risk factors) pre and post implementation 1. Mc. Caffrey R et al. Worldviews Evid Based Nurs 2007; 4: 14 -20 2. Paterno MD et al. AMIA Annu Symp Proc 2006; 1058
Methods n n n Using established risk factors, develop simple, useable method of risk stratifications for clinicians, using methods that have proved effective¹ n Initially paper admission/transfer orders n With CPOE, add as “pop-up”² n Include current ACCP guidelines Use medication reconciliation sheets/orders as reminder n Forms would be mandatory for all admissions/transfers n Again, with CPOE, would be contained therein Measure rates of physician compliance and choice of method on high-risk patients (2 or more risk factors) pre and post implementation 1. Mc. Caffrey R et al. Worldviews Evid Based Nurs 2007; 4: 14 -20 2. Paterno MD et al. AMIA Annu Symp Proc 2006; 1058
 General Conclusions n VTE prophylaxis is justified, low-risk, and indicated in most hospitalized patients n n n Good for patients Good for hospitals Overall, VTE prophylaxis is under-utilized Hospitals and physicians will soon be judged on compliance Each hospital needs a standardized approach for VTE prophylaxis to improve compliance n n n protocols, pre-printed orders, risk stratification, etc. Multi-disciplinary approach auditing
General Conclusions n VTE prophylaxis is justified, low-risk, and indicated in most hospitalized patients n n n Good for patients Good for hospitals Overall, VTE prophylaxis is under-utilized Hospitals and physicians will soon be judged on compliance Each hospital needs a standardized approach for VTE prophylaxis to improve compliance n n n protocols, pre-printed orders, risk stratification, etc. Multi-disciplinary approach auditing
 Thanks …
Thanks …


