3c0a3c388e987f36b08a7aa37f6215c5.ppt
- Количество слайдов: 48
VTE Prevention Roxie M. Albrecht, MD, FACS Associate Professor of Surgery University of Oklahoma
Rationale for Thromboprophylasis • • • High Prevalence of VTE Adverse Consequences of VTE Efficacy and effectiveness of thromboprophylaxis – Highly efficacious in prevention of DVT – Highly efficacious in prevention of symptomatic VTE and fatal PE – DVT prevention prevents PE – Cost effectiveness has been demonstrated
Incidence • 10 -40% in medical or general surgery patients • 40 -60% following major orthopaedic surgery • 10% hospital deaths attributed to PE
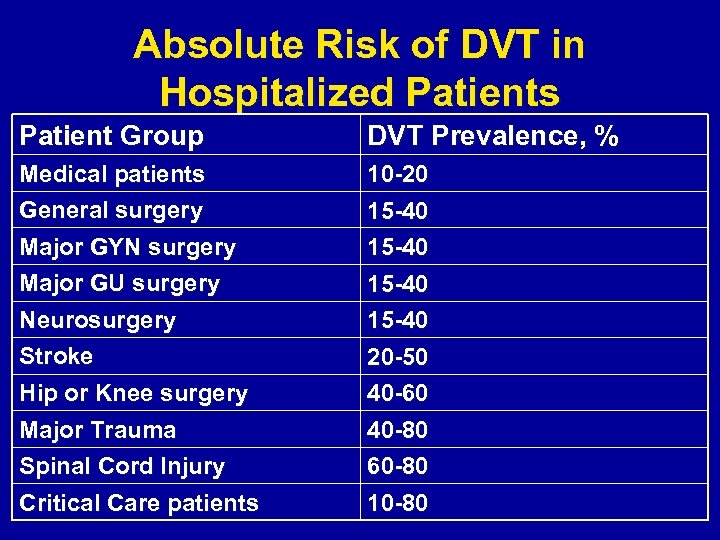
Absolute Risk of DVT in Hospitalized Patients Patient Group DVT Prevalence, % Medical patients General surgery 10 -20 15 -40 Major GYN surgery Major GU surgery 15 -40 Neurosurgery Stroke 15 -40 20 -50 Hip or Knee surgery Major Trauma 40 -60 40 -80 Spinal Cord Injury Critical Care patients 60 -80 10 -80
Consequences of Unprevented VTE • • • Symptomatic DVT and PE Fatal PE Costs of investigating symptomatic patients Risks and costs of treating unprevented VTE Increased future risk of recurrent VTE Chronic post-thrombotic syndrome
Thromboprophylaxis reduces VTE events • PE is the most common preventable cause of hospital death • Highest ranked safety practice – Appropriate use of VTE prophylaxis
Risk Factors for VTE • • • Surgery Trauma Immobility, paresis Malignancy Cancer therapy Previous VTE Increasing age Pregnancy and postpartum Estrogen-containing oral contraception or HRT • Selective estrogen receptor modulators • Acute medical illness • • • Heart or respiratory failure Inflammatory bowel disease Nephrotic syndrome Myeloproliferative disorders Paroxysmal nocturnal hemoglobinuria Obesity Smoking Varicose veins Central venous catheterization Inherited or acquired thrombophilia
Risk Factor Stratification • Individual Approach – Individual predisposing factors and risk associated with current illness or procedure • Group-specific prophylaxis
Guidelines for Prophylaxis • American College of Chest Physicians – Chest 2004 • Grade I – Recommendations are strong and indicate that the benefits do or do not out weigh risks, burden and costs • Grade 2 – Recommendations are less certain. Suggest feasibility, acceptability and cost related to implementation strategies. • Grade A – RCT’s with consistent results • Grade B – RCT’s with inconsistent results or method weaknesses • Grade C – Observational studies or generalizations from one group of patients in a RCT. A + is given if the generalizations are secure or overwhelming.
Methods of Prophylaxis • Mechanical Methods – Graduated Compression Stockings – Intermittent pneumatic compression device – Venous foot pump • Studies – – – Not blinded High rate of false negative scans Compliance in true practice – poor • Acceptable option – High risk for bleeding (Grade 1 C+) – Adjunct to anticoagulant prophylaxis (Grade 2 A) • Improves efficacy when used in combination with anticoagulant prophylaxis
Methods of Prophylaxis • Aspirin – Poor study methods • Acceptable DVT screening – 38% • ASA alone in only 1/3 of trials – No significant benefit – Small increased risk of major bleeding – Poor results v. LMWH – Not recommended alone for VTE in any patient group (Group 1 A)
Unfractionated Heparin & Low Molecular Weight Heparin • Most widely used and studied prophylaxis • Low molecular weight heparin have more predictable pharmacokinetic and pharmacodynamic properties due to consistent binding sites • Dosing LMWH more cumbersome – Anti – Xa monitoring • UFH – needs site specific validation of a. PTT therapeutic range due to variability of reagents • LMWH – ? Limited uses in renal failure and obesity – dose adjustments possible
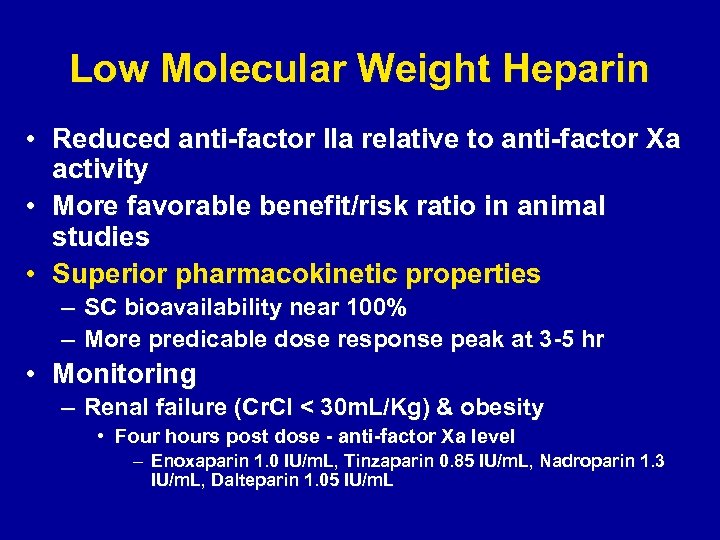
Low Molecular Weight Heparin • Reduced anti-factor IIa relative to anti-factor Xa activity • More favorable benefit/risk ratio in animal studies • Superior pharmacokinetic properties – SC bioavailability near 100% – More predicable dose response peak at 3 -5 hr • Monitoring – Renal failure (Cr. Cl < 30 m. L/Kg) & obesity • Four hours post dose - anti-factor Xa level – Enoxaparin 1. 0 IU/m. L, Tinzaparin 0. 85 IU/m. L, Nadroparin 1. 3 IU/m. L, Dalteparin 1. 05 IU/m. L
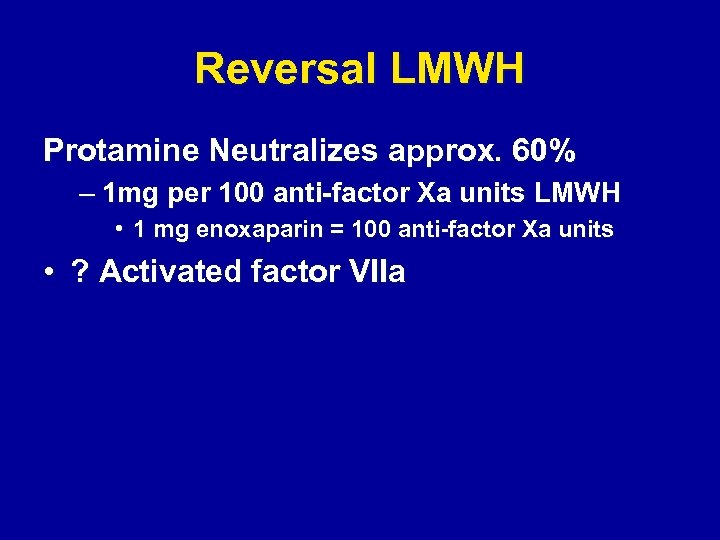
Reversal LMWH Protamine Neutralizes approx. 60% – 1 mg per 100 anti-factor Xa units LMWH • 1 mg enoxaparin = 100 anti-factor Xa units • ? Activated factor VIIa
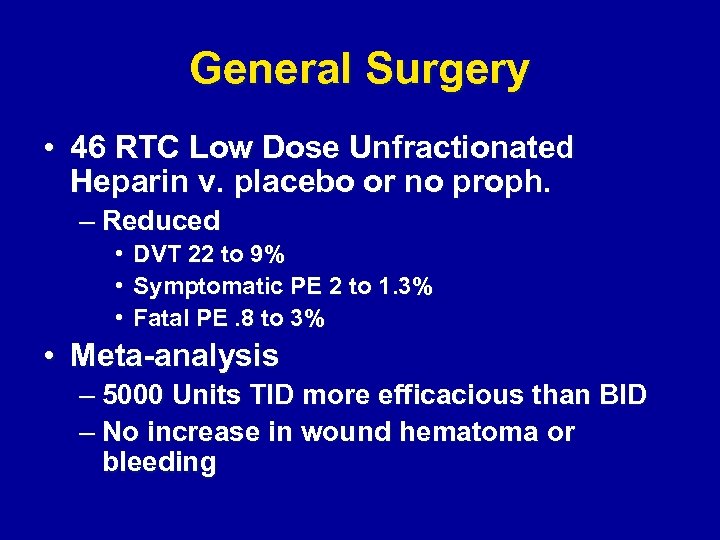
General Surgery • 46 RTC Low Dose Unfractionated Heparin v. placebo or no proph. – Reduced • DVT 22 to 9% • Symptomatic PE 2 to 1. 3% • Fatal PE. 8 to 3% • Meta-analysis – 5000 Units TID more efficacious than BID – No increase in wound hematoma or bleeding
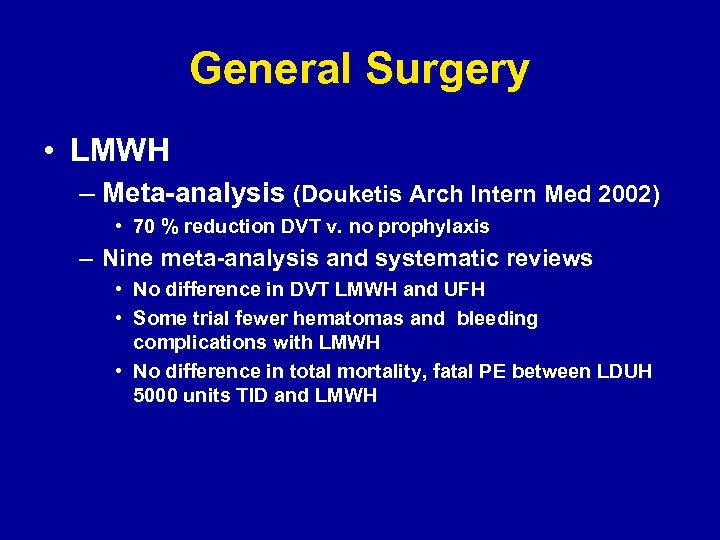
General Surgery • LMWH – Meta-analysis (Douketis Arch Intern Med 2002) • 70 % reduction DVT v. no prophylaxis – Nine meta-analysis and systematic reviews • No difference in DVT LMWH and UFH • Some trial fewer hematomas and bleeding complications with LMWH • No difference in total mortality, fatal PE between LDUH 5000 units TID and LMWH
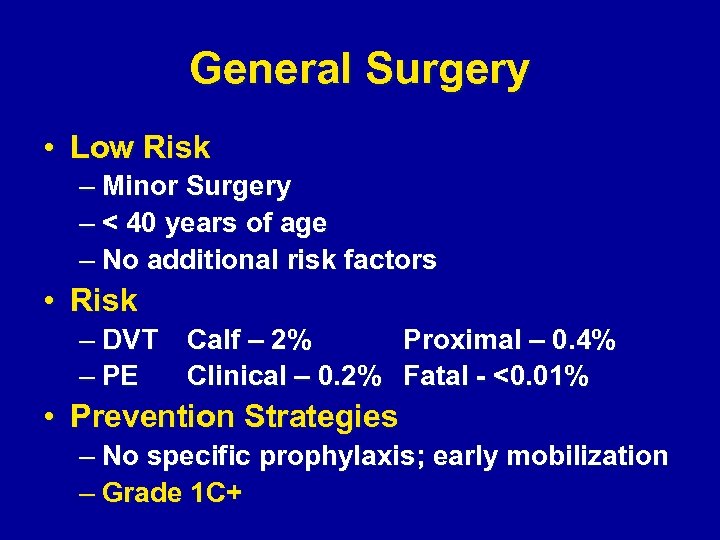
General Surgery • Low Risk – Minor Surgery – < 40 years of age – No additional risk factors • Risk – DVT Calf – 2% Proximal – 0. 4% – PE Clinical – 0. 2% Fatal - <0. 01% • Prevention Strategies – No specific prophylaxis; early mobilization – Grade 1 C+
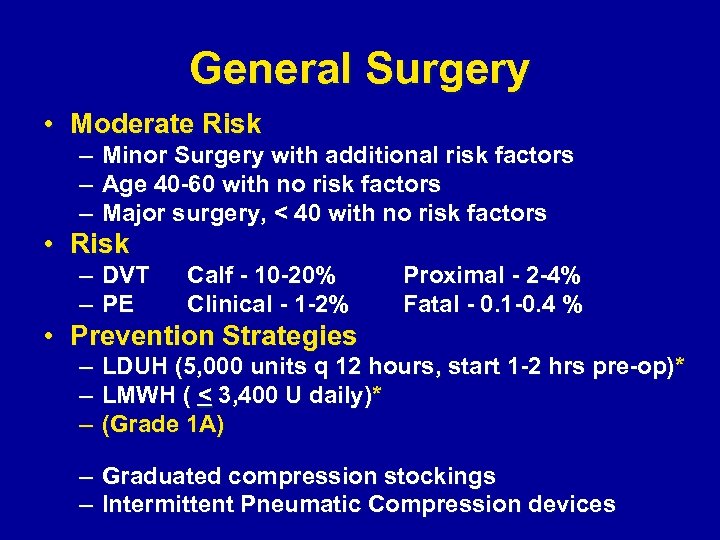
General Surgery • Moderate Risk – – – Minor Surgery with additional risk factors Age 40 -60 with no risk factors Major surgery, < 40 with no risk factors • Risk – DVT – PE Calf - 10 -20% Clinical - 1 -2% Proximal - 2 -4% Fatal - 0. 1 -0. 4 % • Prevention Strategies – – – LDUH (5, 000 units q 12 hours, start 1 -2 hrs pre-op)* LMWH ( < 3, 400 U daily)* (Grade 1 A) – Graduated compression stockings – Intermittent Pneumatic Compression devices
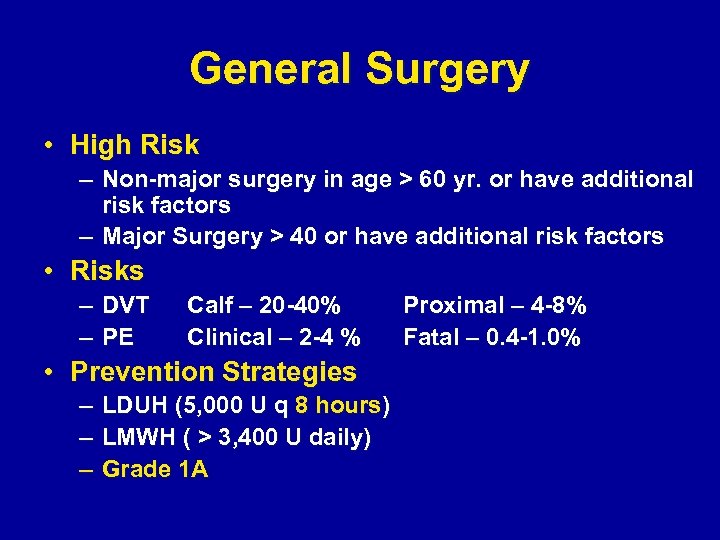
General Surgery • High Risk – Non-major surgery in age > 60 yr. or have additional risk factors – Major Surgery > 40 or have additional risk factors • Risks – DVT – PE Calf – 20 -40% Clinical – 2 -4 % • Prevention Strategies – LDUH (5, 000 U q 8 hours) – LMWH ( > 3, 400 U daily) – Grade 1 A Proximal – 4 -8% Fatal – 0. 4 -1. 0%
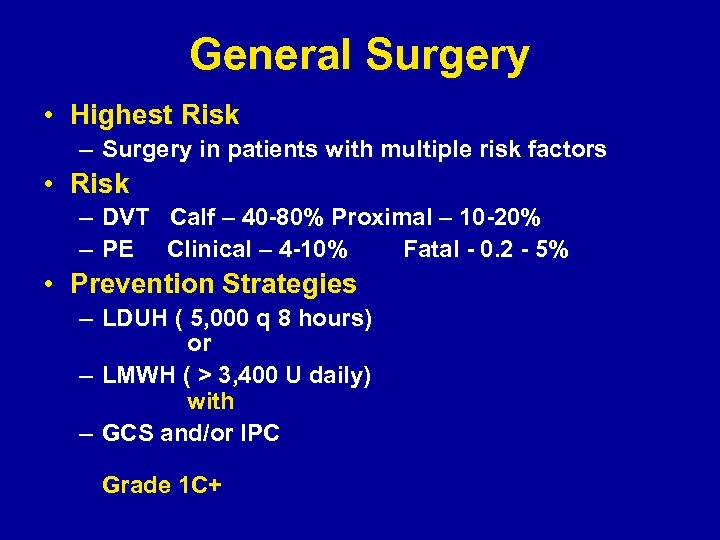
General Surgery • Highest Risk – Surgery in patients with multiple risk factors • Risk – DVT Calf – 40 -80% Proximal – 10 -20% – PE Clinical – 4 -10% Fatal - 0. 2 - 5% • Prevention Strategies – LDUH ( 5, 000 q 8 hours) or – LMWH ( > 3, 400 U daily) with – GCS and/or IPC Grade 1 C+
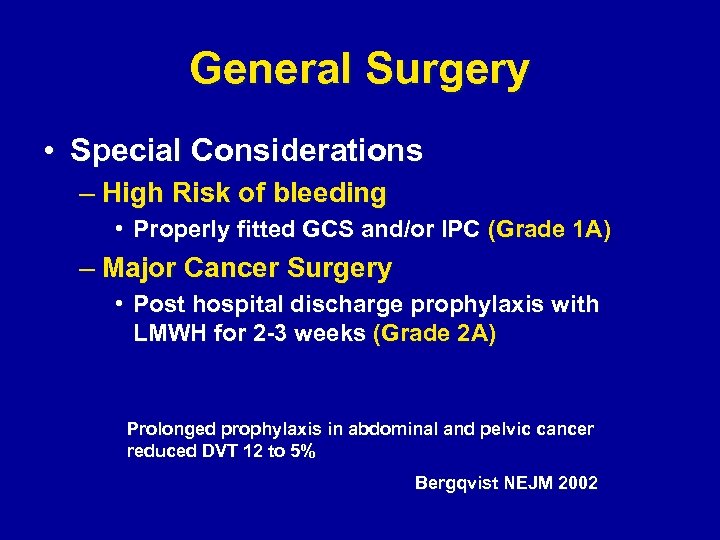
General Surgery • Special Considerations – High Risk of bleeding • Properly fitted GCS and/or IPC (Grade 1 A) – Major Cancer Surgery • Post hospital discharge prophylaxis with LMWH for 2 -3 weeks (Grade 2 A) Prolonged prophylaxis in abdominal and pelvic cancer reduced DVT 12 to 5% Bergqvist NEJM 2002
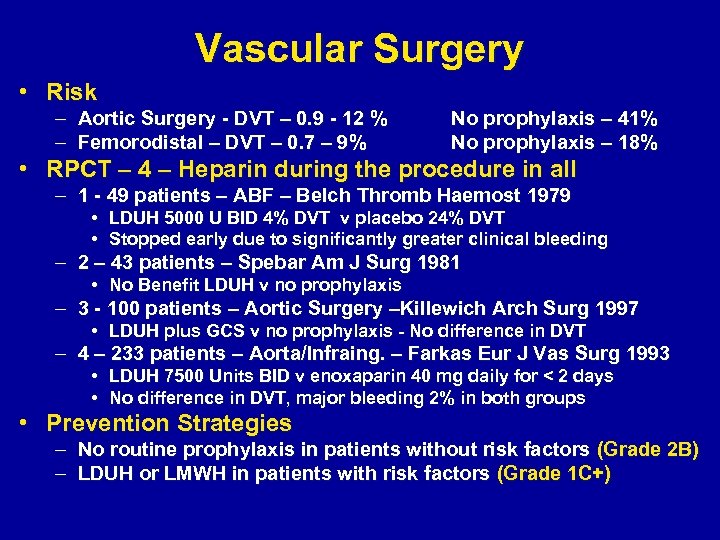
Vascular Surgery • Risk – Aortic Surgery - DVT – 0. 9 - 12 % – Femorodistal – DVT – 0. 7 – 9% No prophylaxis – 41% No prophylaxis – 18% • RPCT – 4 – Heparin during the procedure in all – 1 - 49 patients – ABF – Belch Thromb Haemost 1979 • LDUH 5000 U BID 4% DVT v placebo 24% DVT • Stopped early due to significantly greater clinical bleeding – 2 – 43 patients – Spebar Am J Surg 1981 • No Benefit LDUH v no prophylaxis – 3 - 100 patients – Aortic Surgery –Killewich Arch Surg 1997 • LDUH plus GCS v no prophylaxis - No difference in DVT – 4 – 233 patients – Aorta/Infraing. – Farkas Eur J Vas Surg 1993 • LDUH 7500 Units BID v enoxaparin 40 mg daily for < 2 days • No difference in DVT, major bleeding 2% in both groups • Prevention Strategies – No routine prophylaxis in patients without risk factors (Grade 2 B) – LDUH or LMWH in patients with risk factors (Grade 1 C+)
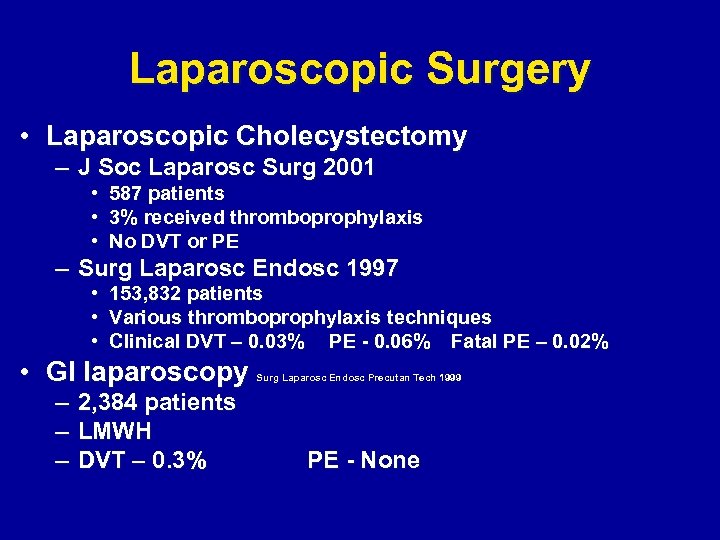
Laparoscopic Surgery • Laparoscopic Cholecystectomy – J Soc Laparosc Surg 2001 • • • 587 patients 3% received thromboprophylaxis No DVT or PE – Surg Laparosc Endosc 1997 • 153, 832 patients • Various thromboprophylaxis techniques • Clinical DVT – 0. 03% PE - 0. 06% Fatal PE – 0. 02% • GI laparoscopy – – – 2, 384 patients LMWH DVT – 0. 3% Surg Laparosc Endosc Precutan Tech 1999 PE - None
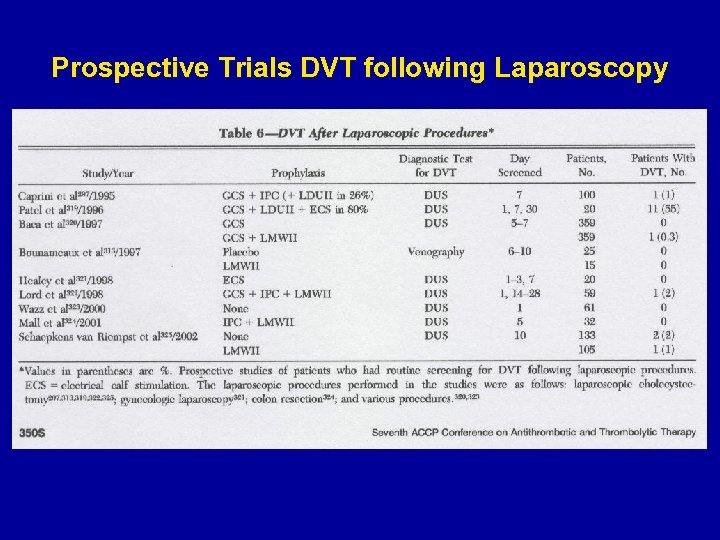
Prospective Trials DVT following Laparoscopy
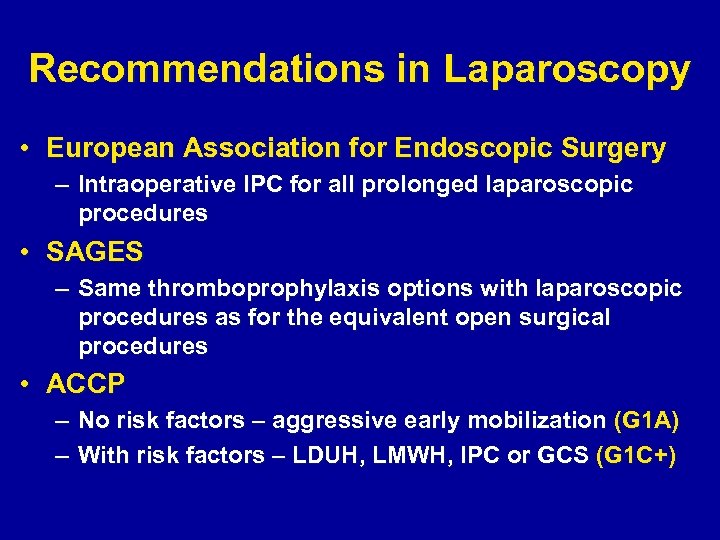
Recommendations in Laparoscopy • European Association for Endoscopic Surgery – Intraoperative IPC for all prolonged laparoscopic procedures • SAGES – Same thromboprophylaxis options with laparoscopic procedures as for the equivalent open surgical procedures • ACCP – No risk factors – aggressive early mobilization (G 1 A) – With risk factors – LDUH, LMWH, IPC or GCS (G 1 C+)
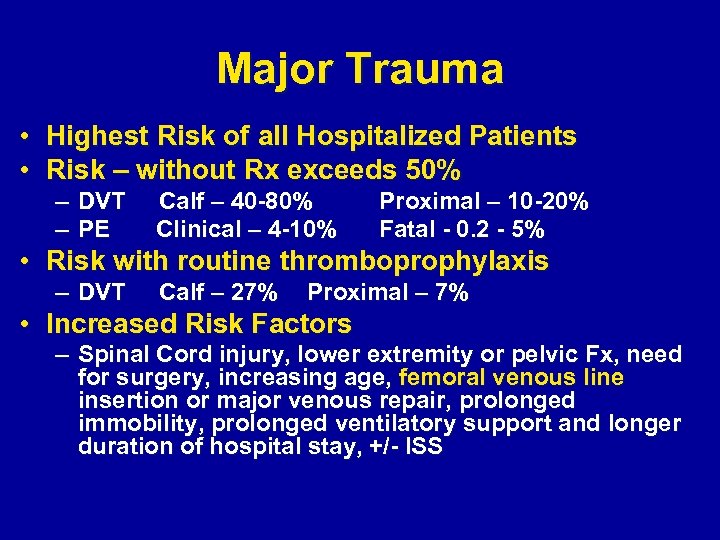
Major Trauma • Highest Risk of all Hospitalized Patients • Risk – without Rx exceeds 50% – DVT – PE Calf – 40 -80% Clinical – 4 -10% Proximal – 10 -20% Fatal - 0. 2 - 5% • Risk with routine thromboprophylaxis – DVT Calf – 27% Proximal – 7% • Increased Risk Factors – Spinal Cord injury, lower extremity or pelvic Fx, need for surgery, increasing age, femoral venous line insertion or major venous repair, prolonged immobility, prolonged ventilatory support and longer duration of hospital stay, +/- ISS
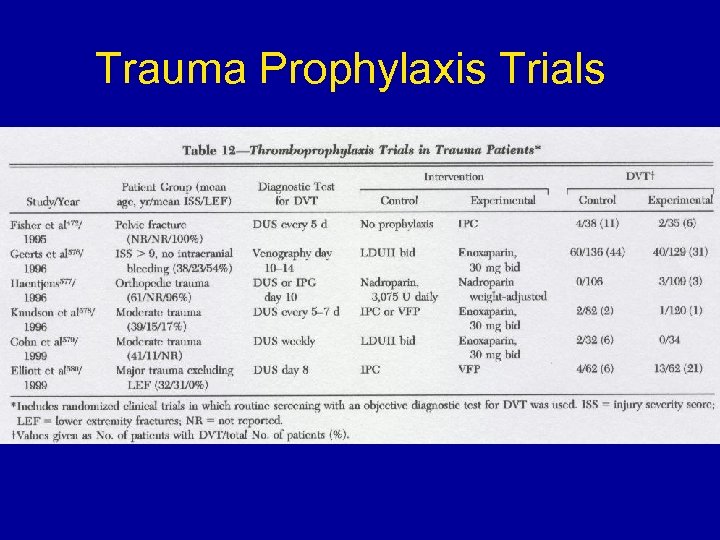
Trauma Prophylaxis Trials
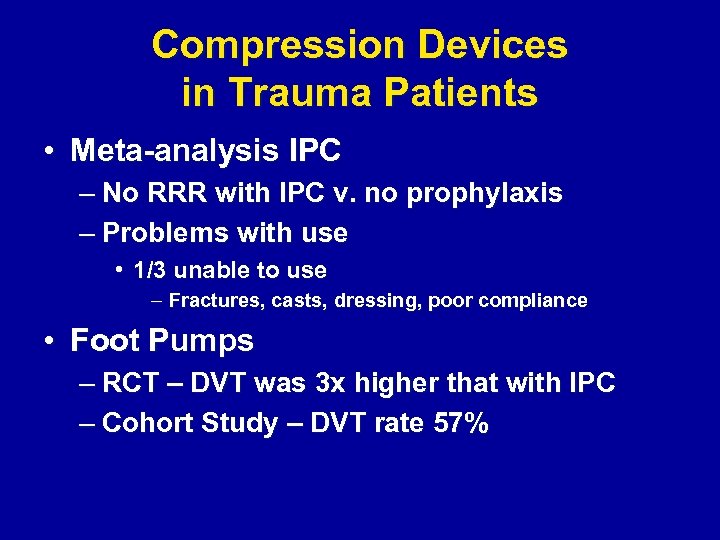
Compression Devices in Trauma Patients • Meta-analysis IPC – No RRR with IPC v. no prophylaxis – Problems with use • 1/3 unable to use – Fractures, casts, dressing, poor compliance • Foot Pumps – RCT – DVT was 3 x higher that with IPC – Cohort Study – DVT rate 57%
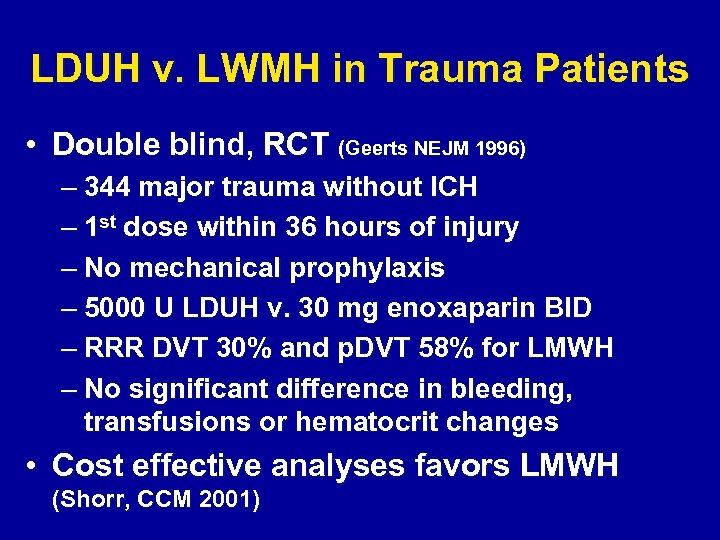
LDUH v. LWMH in Trauma Patients • Double blind, RCT (Geerts NEJM 1996) – 344 major trauma without ICH – 1 st dose within 36 hours of injury – No mechanical prophylaxis – 5000 U LDUH v. 30 mg enoxaparin BID – RRR DVT 30% and p. DVT 58% for LMWH – No significant difference in bleeding, transfusions or hematocrit changes • Cost effective analyses favors LMWH (Shorr, CCM 2001)
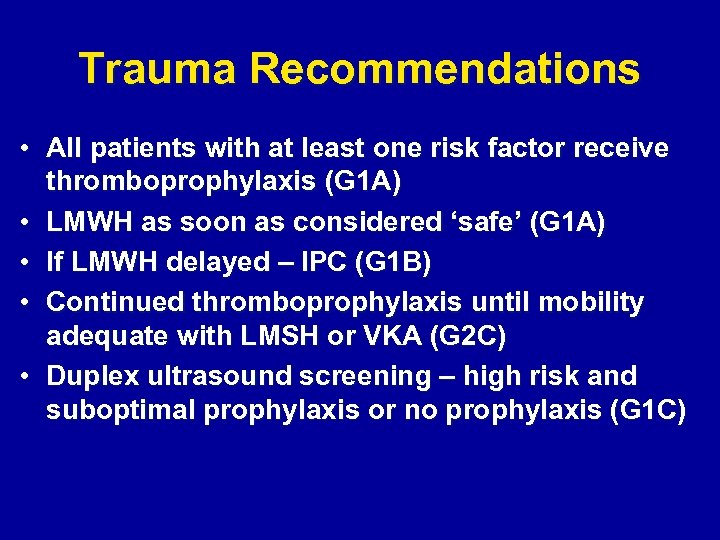
Trauma Recommendations • All patients with at least one risk factor receive thromboprophylaxis (G 1 A) • LMWH as soon as considered ‘safe’ (G 1 A) • If LMWH delayed – IPC (G 1 B) • Continued thromboprophylaxis until mobility adequate with LMSH or VKA (G 2 C) • Duplex ultrasound screening – high risk and suboptimal prophylaxis or no prophylaxis (G 1 C)
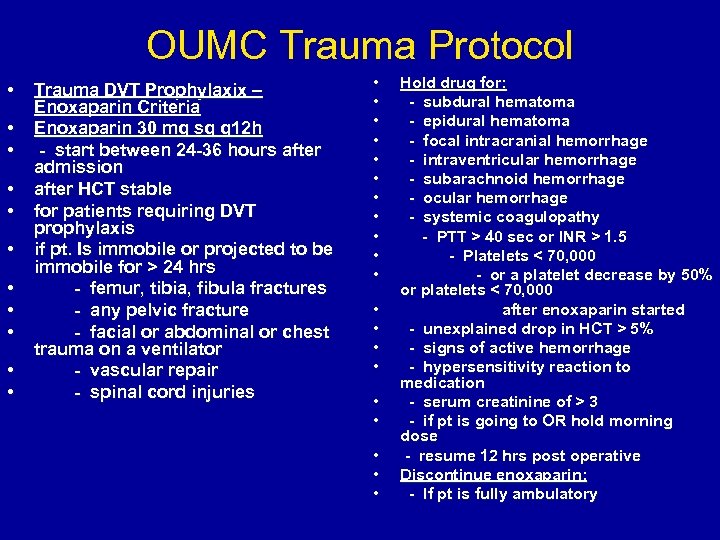
OUMC Trauma Protocol • • • Trauma DVT Prophylaxix – Enoxaparin Criteria Enoxaparin 30 mg sq q 12 h - start between 24 -36 hours after admission after HCT stable for patients requiring DVT prophylaxis if pt. Is immobile or projected to be immobile for > 24 hrs - femur, tibia, fibula fractures - any pelvic fracture - facial or abdominal or chest trauma on a ventilator - vascular repair - spinal cord injuries • • • • • Hold drug for: - subdural hematoma - epidural hematoma - focal intracranial hemorrhage - intraventricular hemorrhage - subarachnoid hemorrhage - ocular hemorrhage - systemic coagulopathy - PTT > 40 sec or INR > 1. 5 - Platelets < 70, 000 - or a platelet decrease by 50% or platelets < 70, 000 after enoxaparin started - unexplained drop in HCT > 5% - signs of active hemorrhage - hypersensitivity reaction to medication - serum creatinine of > 3 - if pt is going to OR hold morning dose - resume 12 hrs post operative Discontinue enoxaparin: - If pt is fully ambulatory
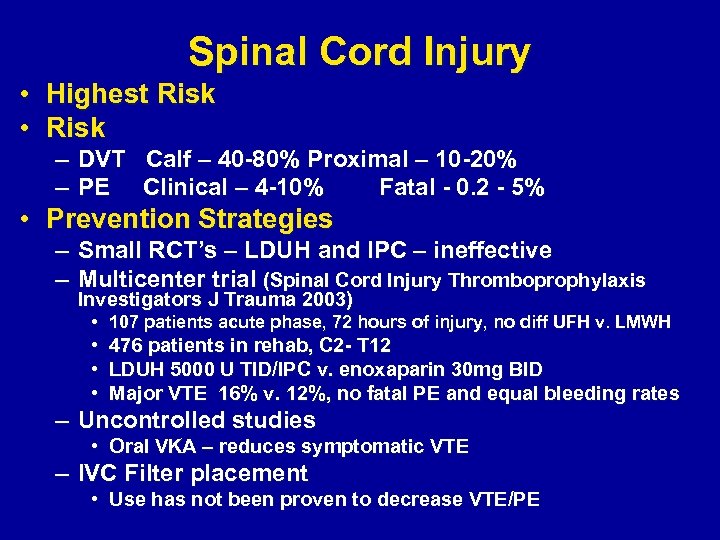
Spinal Cord Injury • Highest Risk • Risk – DVT Calf – 40 -80% Proximal – 10 -20% – PE Clinical – 4 -10% Fatal - 0. 2 - 5% • Prevention Strategies – Small RCT’s – LDUH and IPC – ineffective – Multicenter trial (Spinal Cord Injury Thromboprophylaxis Investigators J Trauma 2003) • 107 patients acute phase, 72 hours of injury, no diff UFH v. LMWH • 476 patients in rehab, C 2 - T 12 • LDUH 5000 U TID/IPC v. enoxaparin 30 mg BID • Major VTE 16% v. 12%, no fatal PE and equal bleeding rates – Uncontrolled studies • Oral VKA – reduces symptomatic VTE – IVC Filter placement • Use has not been proven to decrease VTE/PE
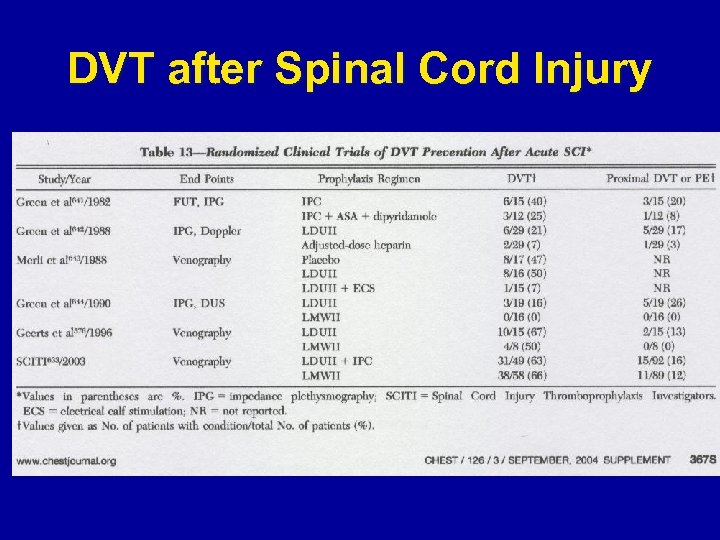
DVT after Spinal Cord Injury
Acute Spinal Cord Injury VTE prophylaxis recommendations • Recommend against the use of LDUH, GCS or IPC as single agents (G 1 A) • GCS and/or IPC when anticoagulation is contraindicated early after injury (G 1 C+) • Prophylaxis with LMWH once primary hemostasis is evident (G 1 B) • Combined use of IPC and LDUH (G 2 B) or LMWH (G 2 C) as alternative to above • Continuation of LMWH or oral VKA during rehabilitation phase (G 1 C)
Neurosurgery • Risk Factors – Intracranial surgery, active malignancy, length of procedure, presence of leg weakness and advance age. – Highest risk - Malignant Brain Tumors • 31% symptomatic DVT • IPC with or without GCS - Most common • Concern for intracranial/spinal bleeding • 68% relative risk reduction – lowering DVT from 22 to 7% • Heparin – One RCT - LDUH v. no Rx – RRR of 82% – 2 Studies – GCS v. GCS/LMWH postop • Control DVT/p. DVT – 26/12% • Control DVT/p. DVT – 33/13% Rx 19/7% Rx 17/5%
Craniotomy • RCT – 100 patients - preop – IPC + LDUH 5000 BID or IPC + dalteparin 2500 daily – Intracranial bleed equal 1/49 v 2/51 – DVT rate equal – 0/49 v. 2 asymptomatic/51 • Pooled Data – Intracranial hemorrhage in RCT’s • 2. 1% for postoperative LMWH • 1. 1% for mechanical or no prophylaxis – Intracranial hemorrhage in meta-analysis • Bleeding with post operative LMWH – 6. 1% • Bleeding with mechanical prophylaxis – 3. 0%
Traumatic Brain Injury • Norwood Arch Surg 2002 – 150 patients with Blunt TBI – LMWH 24 hours after admission – Marshall CT grade progression of ICH – 23% had CT progression – 19% before LMWH and 6% after – All with progression survived, none to OR – DVT rate 2%
Neurosurgery Recommendations • Major Elective Neurosurgery/Intracranial Surgery – IPC, with or without GCS (Grade 1 A) – IPC, w or w/o GCS + LDUH (Grade 2 B) – IPC, w or w/o GCS + postoperative LMWH (G 2 A) • High Risk Neurosurgery Patients – Mechanical + LDUH or LMWH (G 2 B)
Critical Care • Critical Ill patients have multiple risk factors for VTE, some predate admission • ICU entry – 990 patients with DUS at admit – DVT rate 5. 5%
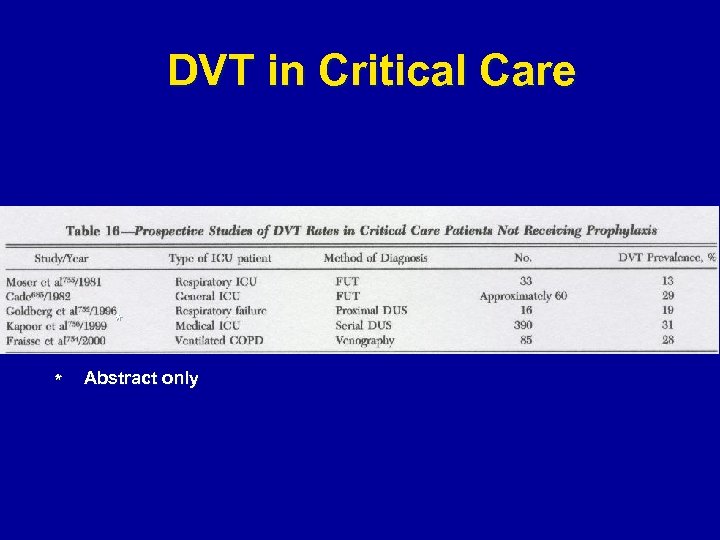
DVT in Critical Care * * Abstract only
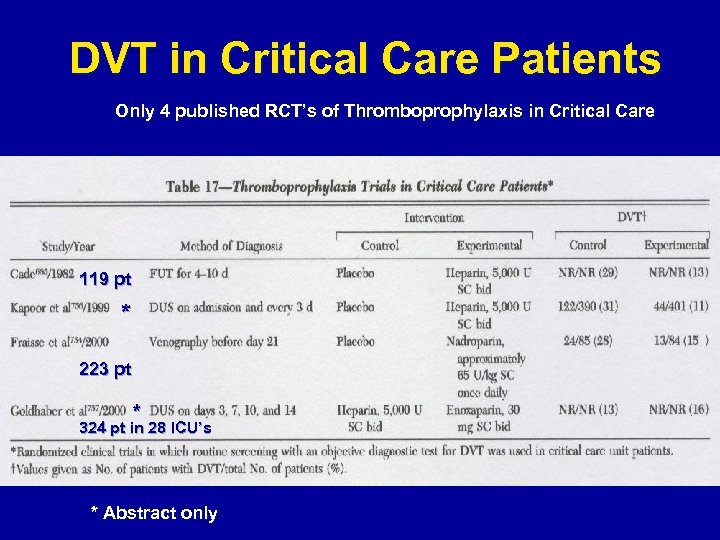
DVT in Critical Care Patients Only 4 published RCT’s of Thromboprophylaxis in Critical Care 119 pt * 223 pt * 324 pt in 28 ICU’s * Abstract only
Recommendations: Critical Care • Assess all patients risk for VTE at admit (G 1 A) – Moderate VTE risk – LDUH or LMWH (G 1 A) • Medically ill or postoperative – High VTE risk – LMWH (G 1 A) • Major trauma, orthopaedic surgery • High bleeding risk patients – Mechanical Prophylaxis (G 1 C+)
New Antithrombotic Agents • Ximelagatran – Oral direct thrombin inhibitor – Rapid absorption and conversion to melagatran – predictable pharmacokinetics, no food interactions • • Hip and knee replacement (Lancet 2002, phase II trial) Melagatran 3 mg BID/ximelagatran 24 mg/d v dalteparin 5000 IU BID • DVT 15. 1 v 28. 2% • Fondaparinux – synthetic pentasaccharides with selective inhibitor of activated factor X (NEJM 2001, Lancet 2002) • • • RRR 56. 4%/59. 5% v. enoxaparin q day hip surgery RRR 22. 6% v enoxaparin BID RRR 12. 5% in Knee sugery higher bleeding Both have better efficacy that LMWH for prophylaxis however cost effectiveness has not yet been proven
Conclusion • Most strategies include LMWH • Exception – – high bleeding risk – GCS and IPS best option Renal failure – monitor Obesity - monitor • Further research – – Laparoscopy Vascular Duration Safety of LMWH • Neurosurgery – New antithrombotic agents in nonorthopedic groups

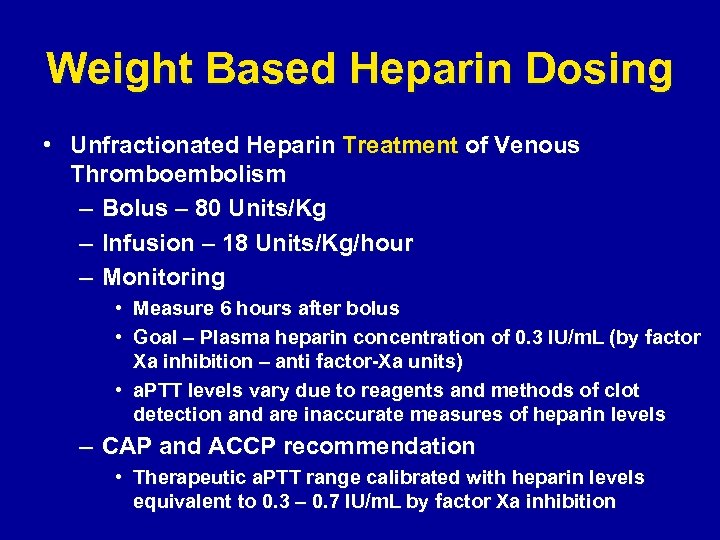
Weight Based Heparin Dosing • Unfractionated Heparin Treatment of Venous Thromboembolism – Bolus – 80 Units/Kg – Infusion – 18 Units/Kg/hour – Monitoring • Measure 6 hours after bolus • Goal – Plasma heparin concentration of 0. 3 IU/m. L (by factor Xa inhibition – anti factor-Xa units) • a. PTT levels vary due to reagents and methods of clot detection and are inaccurate measures of heparin levels – CAP and ACCP recommendation • Therapeutic a. PTT range calibrated with heparin levels equivalent to 0. 3 – 0. 7 IU/m. L by factor Xa inhibition
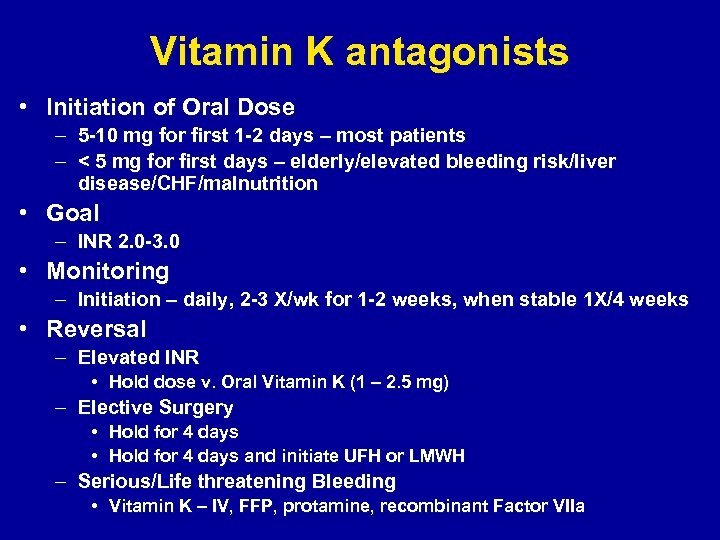
Vitamin K antagonists • Initiation of Oral Dose – 5 -10 mg for first 1 -2 days – most patients – < 5 mg for first days – elderly/elevated bleeding risk/liver disease/CHF/malnutrition • Goal – INR 2. 0 -3. 0 • Monitoring – Initiation – daily, 2 -3 X/wk for 1 -2 weeks, when stable 1 X/4 weeks • Reversal – Elevated INR • Hold dose v. Oral Vitamin K (1 – 2. 5 mg) – Elective Surgery • Hold for 4 days and initiate UFH or LMWH – Serious/Life threatening Bleeding • Vitamin K – IV, FFP, protamine, recombinant Factor VIIa
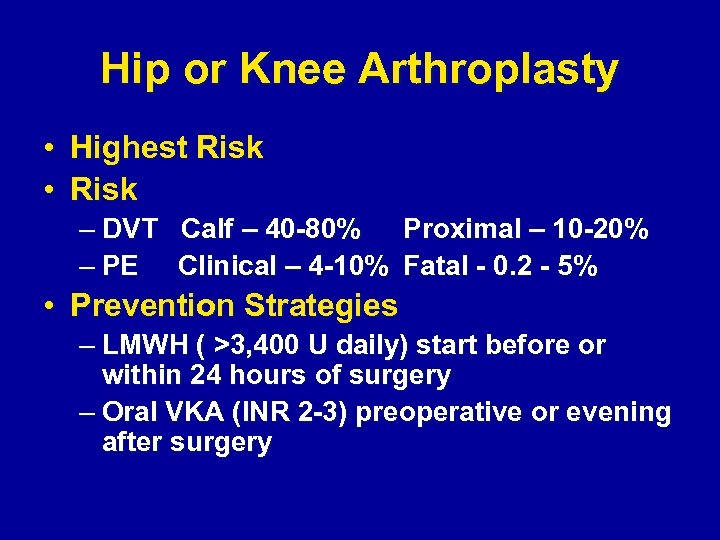
Hip or Knee Arthroplasty • Highest Risk • Risk – DVT Calf – 40 -80% Proximal – 10 -20% – PE Clinical – 4 -10% Fatal - 0. 2 - 5% • Prevention Strategies – LMWH ( >3, 400 U daily) start before or within 24 hours of surgery – Oral VKA (INR 2 -3) preoperative or evening after surgery
3c0a3c388e987f36b08a7aa37f6215c5.ppt