0e21f3913c853418888b4834c78cbb34.ppt
- Количество слайдов: 81
 Voiding Dysfunction in Children Ø COL John Roscelli Ø Pediatric Nephrology Ø San Antonio Military Pediatric Center
Voiding Dysfunction in Children Ø COL John Roscelli Ø Pediatric Nephrology Ø San Antonio Military Pediatric Center
 Agenda Ø How the Lower Urinary Tract Works Ø Voiding Dysfunction in children with no organic pathology ØDefinition ØPresentation modes ØEvaluation ØTreatment
Agenda Ø How the Lower Urinary Tract Works Ø Voiding Dysfunction in children with no organic pathology ØDefinition ØPresentation modes ØEvaluation ØTreatment
 How the Lower Urinary Tract Works
How the Lower Urinary Tract Works
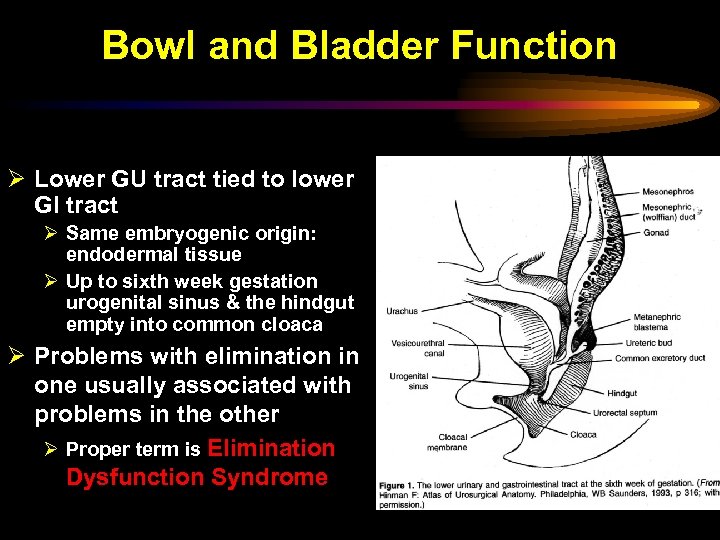 Bowl and Bladder Function Ø Lower GU tract tied to lower GI tract Ø Same embryogenic origin: endodermal tissue Ø Up to sixth week gestation urogenital sinus & the hindgut empty into common cloaca Ø Problems with elimination in one usually associated with problems in the other Ø Proper term is Elimination Dysfunction Syndrome
Bowl and Bladder Function Ø Lower GU tract tied to lower GI tract Ø Same embryogenic origin: endodermal tissue Ø Up to sixth week gestation urogenital sinus & the hindgut empty into common cloaca Ø Problems with elimination in one usually associated with problems in the other Ø Proper term is Elimination Dysfunction Syndrome
 Function of Lower Urinary Tract ØSTORAGE of adequate volumes of urine at low pressure & with no leakage ØEMPTYING that is ØVoluntary ØEfficient ØComplete ØLow pressure
Function of Lower Urinary Tract ØSTORAGE of adequate volumes of urine at low pressure & with no leakage ØEMPTYING that is ØVoluntary ØEfficient ØComplete ØLow pressure
 Lower Urinary Tract is a Functionally Integrated Unit ØUreteral Vesicle Junction ØBladder ØSphincter ØUrethra ØNeurologic control mechanisms
Lower Urinary Tract is a Functionally Integrated Unit ØUreteral Vesicle Junction ØBladder ØSphincter ØUrethra ØNeurologic control mechanisms
 Anatomy & Neurophysiology of the Lower Urinary Tract ØBladder (detrusor) ØStores urine at low pressure ØCompresses urine for voiding ØUrethra ØConveys urine from bladder to outside world ØSphincter(s) internal & external ØControls urine flow & maintain continence between voidings
Anatomy & Neurophysiology of the Lower Urinary Tract ØBladder (detrusor) ØStores urine at low pressure ØCompresses urine for voiding ØUrethra ØConveys urine from bladder to outside world ØSphincter(s) internal & external ØControls urine flow & maintain continence between voidings
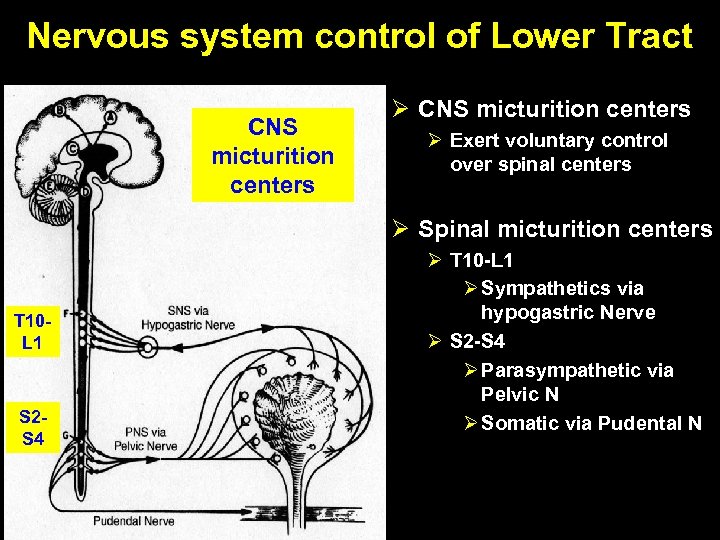 Nervous system control of Lower Tract CNS micturition centers Ø Exert voluntary control over spinal centers Ø Spinal micturition centers T 10 L 1 S 2 S 4 Ø T 10 -L 1 Ø Sympathetics via hypogastric Nerve Ø S 2 -S 4 Ø Parasympathetic via Pelvic N Ø Somatic via Pudental N
Nervous system control of Lower Tract CNS micturition centers Ø Exert voluntary control over spinal centers Ø Spinal micturition centers T 10 L 1 S 2 S 4 Ø T 10 -L 1 Ø Sympathetics via hypogastric Nerve Ø S 2 -S 4 Ø Parasympathetic via Pelvic N Ø Somatic via Pudental N
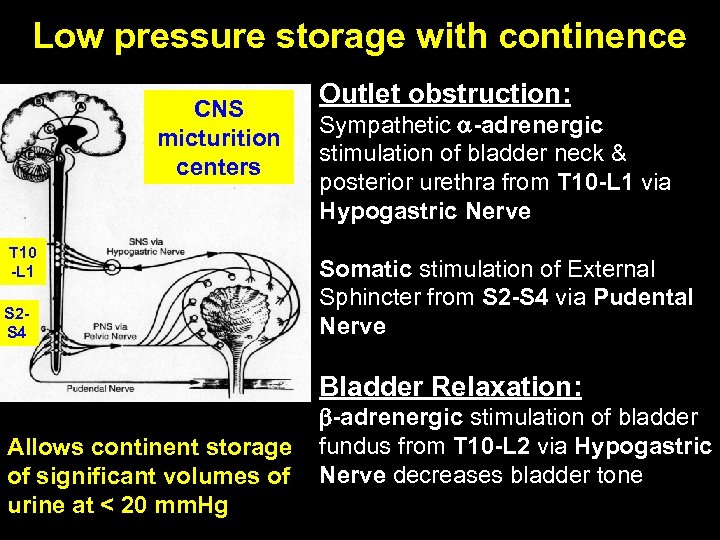 Low pressure storage with continence CNS micturition centers T 10 -L 1 S 2 S 4 Outlet obstruction: Sympathetic -adrenergic stimulation of bladder neck & posterior urethra from T 10 -L 1 via Hypogastric Nerve Somatic stimulation of External Sphincter from S 2 -S 4 via Pudental Nerve Bladder Relaxation: Allows continent storage of significant volumes of urine at < 20 mm. Hg -adrenergic stimulation of bladder fundus from T 10 -L 2 via Hypogastric Nerve decreases bladder tone
Low pressure storage with continence CNS micturition centers T 10 -L 1 S 2 S 4 Outlet obstruction: Sympathetic -adrenergic stimulation of bladder neck & posterior urethra from T 10 -L 1 via Hypogastric Nerve Somatic stimulation of External Sphincter from S 2 -S 4 via Pudental Nerve Bladder Relaxation: Allows continent storage of significant volumes of urine at < 20 mm. Hg -adrenergic stimulation of bladder fundus from T 10 -L 2 via Hypogastric Nerve decreases bladder tone
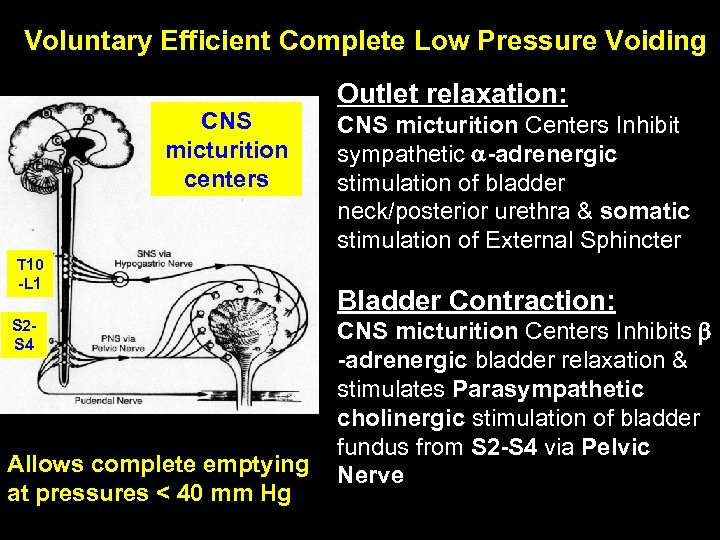 Voluntary Efficient Complete Low Pressure Voiding CNS micturition centers T 10 -L 1 S 2 S 4 Allows complete emptying at pressures < 40 mm Hg Outlet relaxation: CNS micturition Centers Inhibit sympathetic -adrenergic stimulation of bladder neck/posterior urethra & somatic stimulation of External Sphincter Bladder Contraction: CNS micturition Centers Inhibits -adrenergic bladder relaxation & stimulates Parasympathetic cholinergic stimulation of bladder fundus from S 2 -S 4 via Pelvic Nerve
Voluntary Efficient Complete Low Pressure Voiding CNS micturition centers T 10 -L 1 S 2 S 4 Allows complete emptying at pressures < 40 mm Hg Outlet relaxation: CNS micturition Centers Inhibit sympathetic -adrenergic stimulation of bladder neck/posterior urethra & somatic stimulation of External Sphincter Bladder Contraction: CNS micturition Centers Inhibits -adrenergic bladder relaxation & stimulates Parasympathetic cholinergic stimulation of bladder fundus from S 2 -S 4 via Pelvic Nerve
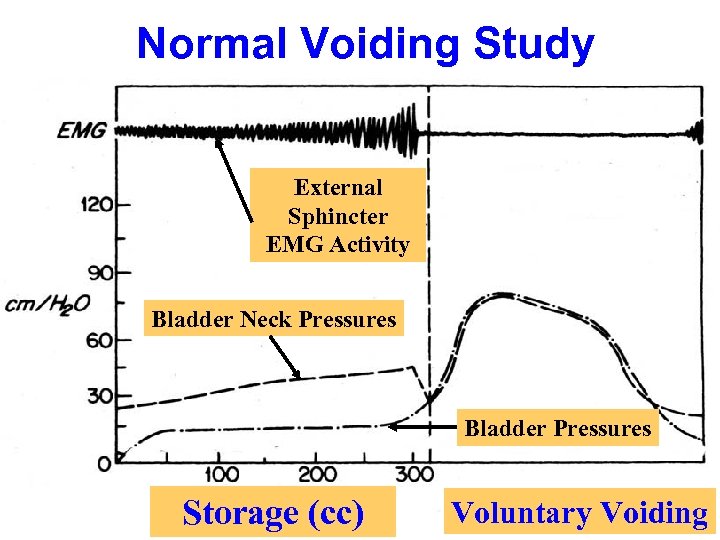 Normal Voiding Study External Sphincter EMG Activity Bladder Neck Pressures Bladder Pressures Storage (cc) Voluntary Voiding
Normal Voiding Study External Sphincter EMG Activity Bladder Neck Pressures Bladder Pressures Storage (cc) Voluntary Voiding
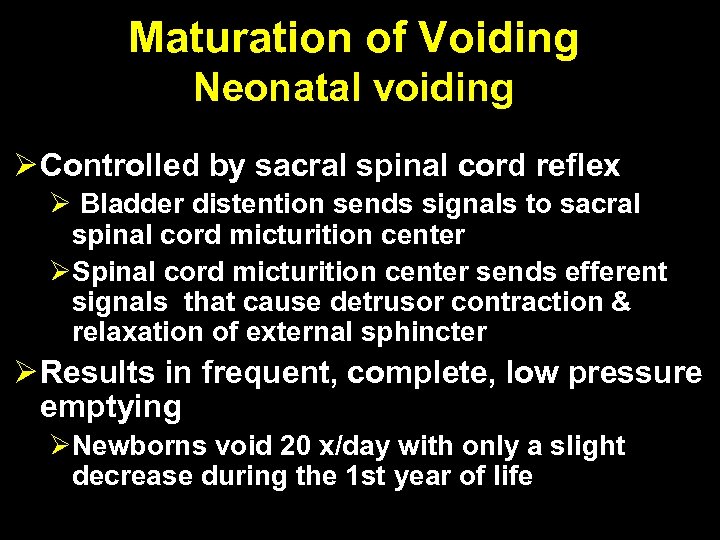 Maturation of Voiding Neonatal voiding Ø Controlled by sacral spinal cord reflex Ø Bladder distention sends signals to sacral spinal cord micturition center ØSpinal cord micturition center sends efferent signals that cause detrusor contraction & relaxation of external sphincter Ø Results in frequent, complete, low pressure emptying ØNewborns void 20 x/day with only a slight decrease during the 1 st year of life
Maturation of Voiding Neonatal voiding Ø Controlled by sacral spinal cord reflex Ø Bladder distention sends signals to sacral spinal cord micturition center ØSpinal cord micturition center sends efferent signals that cause detrusor contraction & relaxation of external sphincter Ø Results in frequent, complete, low pressure emptying ØNewborns void 20 x/day with only a slight decrease during the 1 st year of life
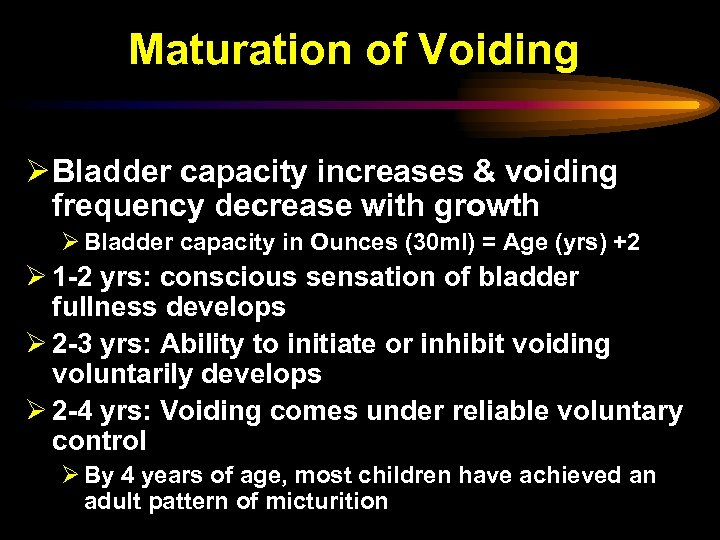 Maturation of Voiding Ø Bladder capacity increases & voiding frequency decrease with growth Ø Bladder capacity in Ounces (30 ml) = Age (yrs) +2 Ø 1 -2 yrs: conscious sensation of bladder fullness develops Ø 2 -3 yrs: Ability to initiate or inhibit voiding voluntarily develops Ø 2 -4 yrs: Voiding comes under reliable voluntary control Ø By 4 years of age, most children have achieved an adult pattern of micturition
Maturation of Voiding Ø Bladder capacity increases & voiding frequency decrease with growth Ø Bladder capacity in Ounces (30 ml) = Age (yrs) +2 Ø 1 -2 yrs: conscious sensation of bladder fullness develops Ø 2 -3 yrs: Ability to initiate or inhibit voiding voluntarily develops Ø 2 -4 yrs: Voiding comes under reliable voluntary control Ø By 4 years of age, most children have achieved an adult pattern of micturition
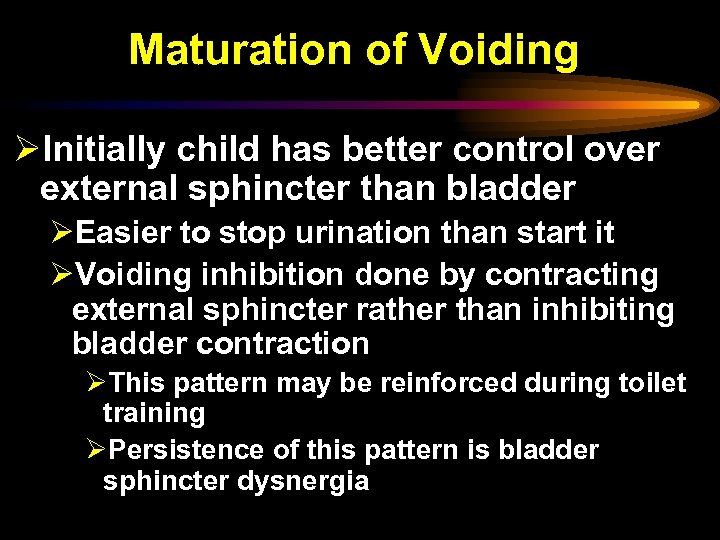 Maturation of Voiding ØInitially child has better control over external sphincter than bladder ØEasier to stop urination than start it ØVoiding inhibition done by contracting external sphincter rather than inhibiting bladder contraction ØThis pattern may be reinforced during toilet training ØPersistence of this pattern is bladder sphincter dysnergia
Maturation of Voiding ØInitially child has better control over external sphincter than bladder ØEasier to stop urination than start it ØVoiding inhibition done by contracting external sphincter rather than inhibiting bladder contraction ØThis pattern may be reinforced during toilet training ØPersistence of this pattern is bladder sphincter dysnergia

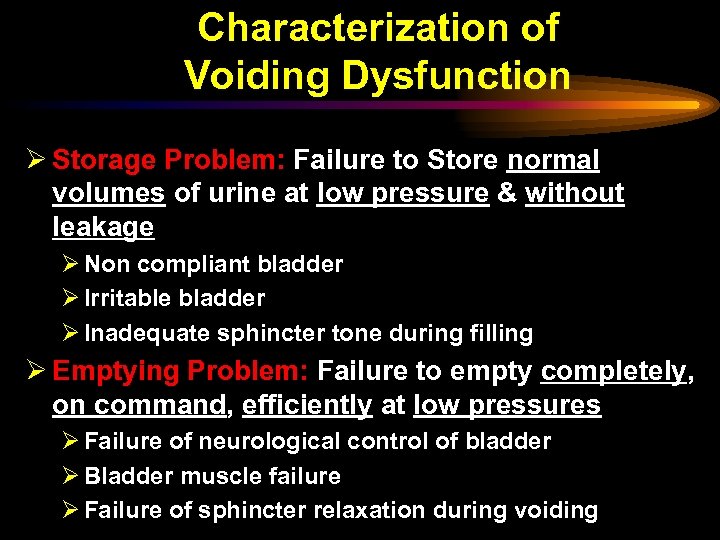 Characterization of Voiding Dysfunction Ø Storage Problem: Failure to Store normal volumes of urine at low pressure & without leakage Ø Non compliant bladder Ø Irritable bladder Ø Inadequate sphincter tone during filling Ø Emptying Problem: Failure to empty completely, on command, efficiently at low pressures Ø Failure of neurological control of bladder Ø Bladder muscle failure Ø Failure of sphincter relaxation during voiding
Characterization of Voiding Dysfunction Ø Storage Problem: Failure to Store normal volumes of urine at low pressure & without leakage Ø Non compliant bladder Ø Irritable bladder Ø Inadequate sphincter tone during filling Ø Emptying Problem: Failure to empty completely, on command, efficiently at low pressures Ø Failure of neurological control of bladder Ø Bladder muscle failure Ø Failure of sphincter relaxation during voiding
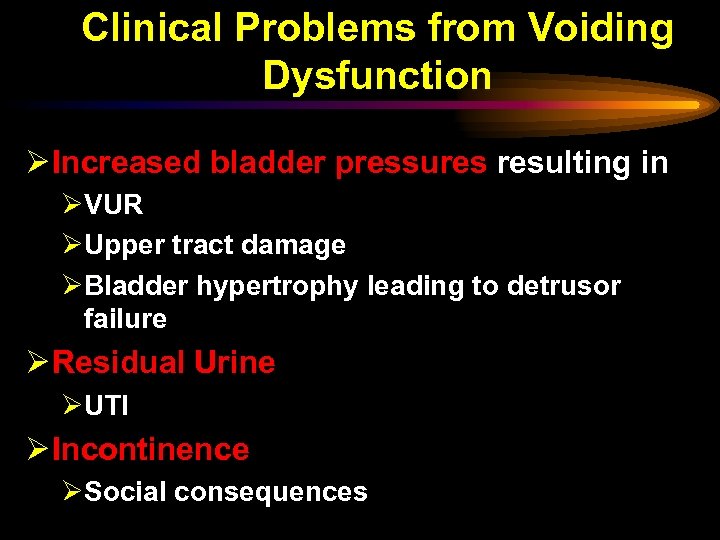 Clinical Problems from Voiding Dysfunction Ø Increased bladder pressures resulting in ØVUR ØUpper tract damage ØBladder hypertrophy leading to detrusor failure Ø Residual Urine ØUTI Ø Incontinence ØSocial consequences
Clinical Problems from Voiding Dysfunction Ø Increased bladder pressures resulting in ØVUR ØUpper tract damage ØBladder hypertrophy leading to detrusor failure Ø Residual Urine ØUTI Ø Incontinence ØSocial consequences
 Voiding Dysfunction in Children with no organic pathology
Voiding Dysfunction in Children with no organic pathology
 Voiding Dysfunction in “Normal Children”- 3 Issues Ø Clinician must 1 st suspect voiding dysfunction in certain clinical circumstances in normal children Ø Clinician must then rule out Neurologic, Urologic & other organic (diabetes, concentrating defects) problems Ø Clinician must then characterize & Rx the functional voiding dysfunction
Voiding Dysfunction in “Normal Children”- 3 Issues Ø Clinician must 1 st suspect voiding dysfunction in certain clinical circumstances in normal children Ø Clinician must then rule out Neurologic, Urologic & other organic (diabetes, concentrating defects) problems Ø Clinician must then characterize & Rx the functional voiding dysfunction
 Presentations of Voiding Dysfunction in “Normal” Children ØUrologic Presentation ØGI Presentation ØOccult Neurologic presentation
Presentations of Voiding Dysfunction in “Normal” Children ØUrologic Presentation ØGI Presentation ØOccult Neurologic presentation
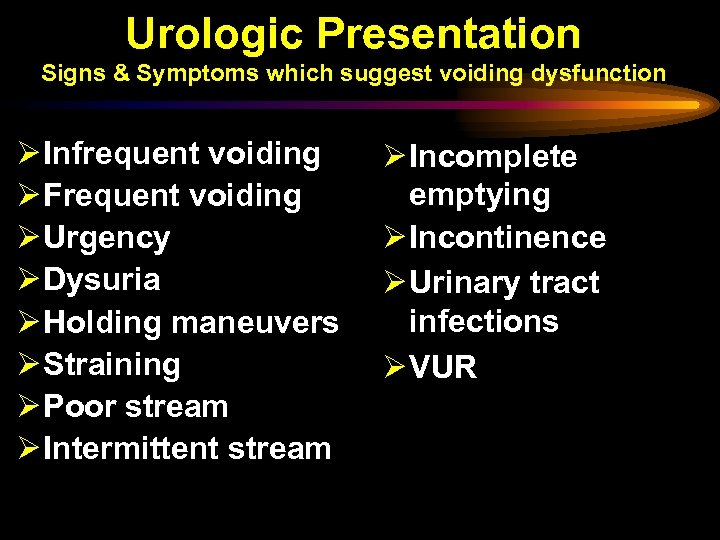 Urologic Presentation Signs & Symptoms which suggest voiding dysfunction Ø Infrequent voiding Ø Frequent voiding Ø Urgency Ø Dysuria Ø Holding maneuvers Ø Straining Ø Poor stream Ø Intermittent stream Ø Incomplete emptying Ø Incontinence Ø Urinary tract infections Ø VUR
Urologic Presentation Signs & Symptoms which suggest voiding dysfunction Ø Infrequent voiding Ø Frequent voiding Ø Urgency Ø Dysuria Ø Holding maneuvers Ø Straining Ø Poor stream Ø Intermittent stream Ø Incomplete emptying Ø Incontinence Ø Urinary tract infections Ø VUR
 Urologic Presentation It can not be overemphasized to the general pediatrician how important it is that they rule out voiding dysfunction in all their children with recurrent UTIs, VUR or incontinence
Urologic Presentation It can not be overemphasized to the general pediatrician how important it is that they rule out voiding dysfunction in all their children with recurrent UTIs, VUR or incontinence
 GI Presentation Signs & Symptoms which suggest voiding dysfunction Ø Fecal staining of undergarments Ø Fecal incontinence Ø Constipation Ø Encopresis Ø Obstipation (i. e. , severe constipation causing obstruction) Ø Abdominal pains
GI Presentation Signs & Symptoms which suggest voiding dysfunction Ø Fecal staining of undergarments Ø Fecal incontinence Ø Constipation Ø Encopresis Ø Obstipation (i. e. , severe constipation causing obstruction) Ø Abdominal pains
 Ocult Neurologic Presentation Spinal cord tethering suggested by Ø Lower back abnormalities such as nevus, dermal sinus, or dimple Ø Pain in the lower back during stretching of the lower extremities Ø Gait abnormalities Ø Worsening symptoms during growth spurts Ø Severe stool incontinence Ø Complex enuresis refractory to routine Rx
Ocult Neurologic Presentation Spinal cord tethering suggested by Ø Lower back abnormalities such as nevus, dermal sinus, or dimple Ø Pain in the lower back during stretching of the lower extremities Ø Gait abnormalities Ø Worsening symptoms during growth spurts Ø Severe stool incontinence Ø Complex enuresis refractory to routine Rx
 Types of Voiding Dysfunction Disorders in “normal” Children
Types of Voiding Dysfunction Disorders in “normal” Children
 Minor Voiding Dysfunctional Disorders Ø Extraordinary daytime urinary frequency syndrome Ø Giggle incontinence Ø Stress incontinence Ø Post void dribbling Ø Vaginal voiding Ø Primary monosymptomatic nocturnal enuresis
Minor Voiding Dysfunctional Disorders Ø Extraordinary daytime urinary frequency syndrome Ø Giggle incontinence Ø Stress incontinence Ø Post void dribbling Ø Vaginal voiding Ø Primary monosymptomatic nocturnal enuresis
 Major Voiding Dysfunctional Disorders ØHinman syndromenon neruogenic neurogenic bladder ØOchoa (urofacial) syndrome ØHinman syndrome with Autosomal dominant inheritance & facial grimace when smiling ØMyogenic detrusor failure
Major Voiding Dysfunctional Disorders ØHinman syndromenon neruogenic neurogenic bladder ØOchoa (urofacial) syndrome ØHinman syndrome with Autosomal dominant inheritance & facial grimace when smiling ØMyogenic detrusor failure
 Moderate Voiding Dysfunctional Disorders ØOveractive bladder/Urge Syndrome ØBladder Sphincter Dysnergia ØLazy bladder syndrome
Moderate Voiding Dysfunctional Disorders ØOveractive bladder/Urge Syndrome ØBladder Sphincter Dysnergia ØLazy bladder syndrome
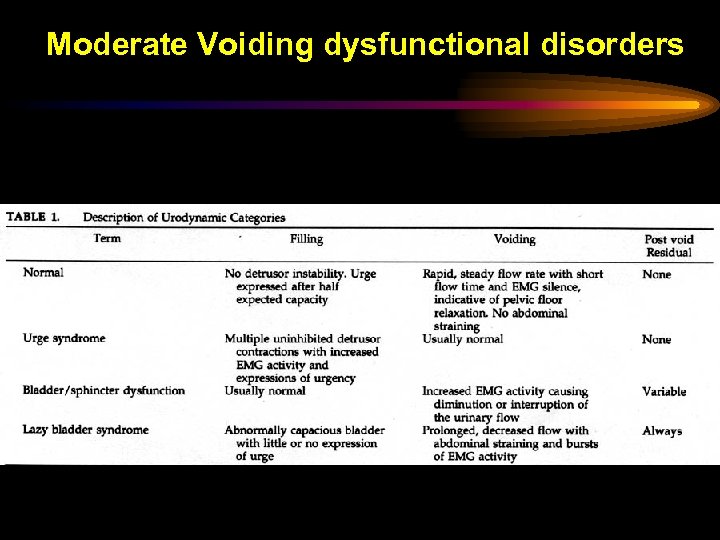 Moderate Voiding dysfunctional disorders
Moderate Voiding dysfunctional disorders
 Evaluation of Voiding Dysfunction
Evaluation of Voiding Dysfunction
 Purpose of evaluation ØCharacterize the Elimination problems to direct treatment ØStorage problem ØEmptying problem ØContinence problem ØRule out Neurolgic, Urologic or other organic causes
Purpose of evaluation ØCharacterize the Elimination problems to direct treatment ØStorage problem ØEmptying problem ØContinence problem ØRule out Neurolgic, Urologic or other organic causes
 Evaluation of Dysfunctional Voiding Ø Index of suspicion Ø History Ø Physical Exam Ø Simple Lab Tests Ø Imaging Ø Urodynamics
Evaluation of Dysfunctional Voiding Ø Index of suspicion Ø History Ø Physical Exam Ø Simple Lab Tests Ø Imaging Ø Urodynamics
 History To characterize the Problem Ø Evaluation of dysfunctional voiding begins with a detailed elimination history ØHistory of current elimination problems ØDetailed voiding history ØDetailed Stooling history ØPast elimination/urologic History ØUTIs ØConstipation ØAge of toilet training ØIntake history- fluids and diet ØFamily history of urologic problems
History To characterize the Problem Ø Evaluation of dysfunctional voiding begins with a detailed elimination history ØHistory of current elimination problems ØDetailed voiding history ØDetailed Stooling history ØPast elimination/urologic History ØUTIs ØConstipation ØAge of toilet training ØIntake history- fluids and diet ØFamily history of urologic problems
 History To characterize the Problem ØVoiding symptoms & pattern of incontinence must be quantified ØUrgency, frequency, straining, dysuria etc ØHolding maneuvers such as leg crossing, squatting, or "Vincent's curtsey" ØContinuous incontinence in a girl suggests ectopic ureter that inserts distal to urethral sphincter or into the vagina
History To characterize the Problem ØVoiding symptoms & pattern of incontinence must be quantified ØUrgency, frequency, straining, dysuria etc ØHolding maneuvers such as leg crossing, squatting, or "Vincent's curtsey" ØContinuous incontinence in a girl suggests ectopic ureter that inserts distal to urethral sphincter or into the vagina
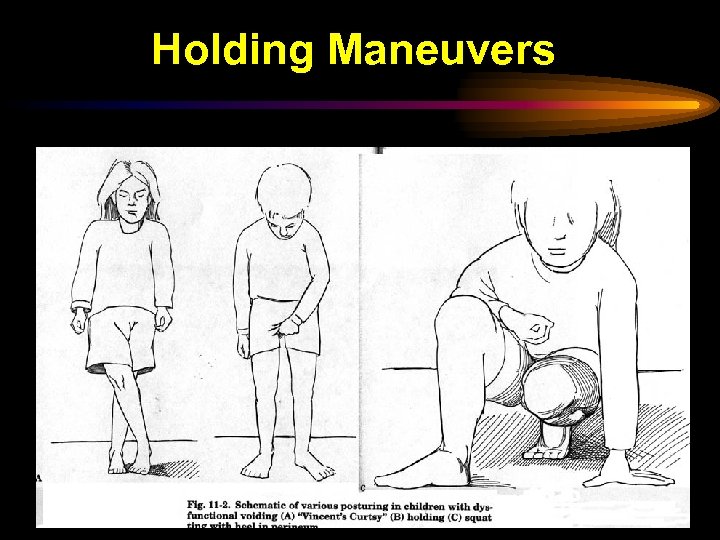 Holding Maneuvers
Holding Maneuvers
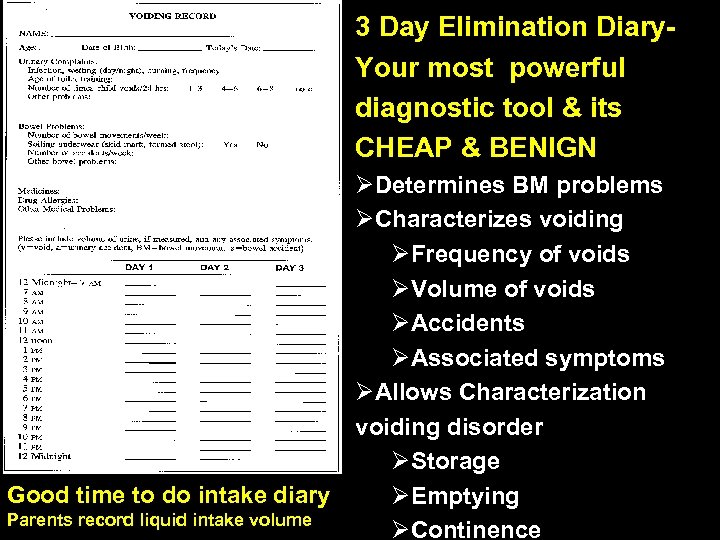 3 Day Elimination Diary. Your most powerful diagnostic tool & its CHEAP & BENIGN ØDetermines BM problems ØCharacterizes voiding ØFrequency of voids ØVolume of voids ØAccidents ØAssociated symptoms ØAllows Characterization voiding disorder ØStorage Good time to do intake diary ØEmptying Parents record liquid intake volume ØContinence
3 Day Elimination Diary. Your most powerful diagnostic tool & its CHEAP & BENIGN ØDetermines BM problems ØCharacterizes voiding ØFrequency of voids ØVolume of voids ØAccidents ØAssociated symptoms ØAllows Characterization voiding disorder ØStorage Good time to do intake diary ØEmptying Parents record liquid intake volume ØContinence
 History Irritable Bladder Ø Urgency & frequency as Cerebral cortex unable to inhibit reflex bladder contractions triggered during filling Ø Parents need to know where every bathroom is at mall etc Ø When they void, void normally although usually have a small bladder capacity Ø Exhibit behaviors to avoid leakage: Dancing, squatting, holding & posturing Ø Classic sign of bladder instability is "Vincent's curtsy“- squatting posture in girls in which the heel compresses the perineum and thereby obstructs the urethra to prevent urinary leakage Ø If unsuccessful get urge incontinence of small amount of urine Ø These behaviors can lead to bladder sphincter dysnergia
History Irritable Bladder Ø Urgency & frequency as Cerebral cortex unable to inhibit reflex bladder contractions triggered during filling Ø Parents need to know where every bathroom is at mall etc Ø When they void, void normally although usually have a small bladder capacity Ø Exhibit behaviors to avoid leakage: Dancing, squatting, holding & posturing Ø Classic sign of bladder instability is "Vincent's curtsy“- squatting posture in girls in which the heel compresses the perineum and thereby obstructs the urethra to prevent urinary leakage Ø If unsuccessful get urge incontinence of small amount of urine Ø These behaviors can lead to bladder sphincter dysnergia
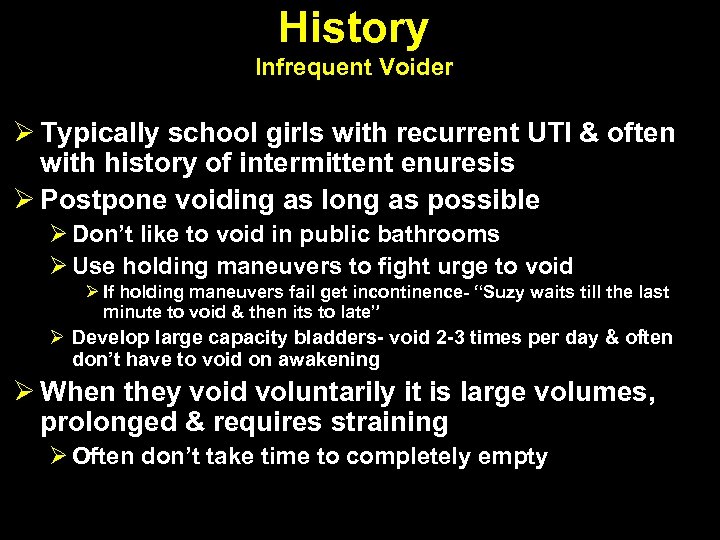 History Infrequent Voider Ø Typically school girls with recurrent UTI & often with history of intermittent enuresis Ø Postpone voiding as long as possible Ø Don’t like to void in public bathrooms Ø Use holding maneuvers to fight urge to void Ø If holding maneuvers fail get incontinence- “Suzy waits till the last minute to void & then its to late” Ø Develop large capacity bladders- void 2 -3 times per day & often don’t have to void on awakening Ø When they void voluntarily it is large volumes, prolonged & requires straining Ø Often don’t take time to completely empty
History Infrequent Voider Ø Typically school girls with recurrent UTI & often with history of intermittent enuresis Ø Postpone voiding as long as possible Ø Don’t like to void in public bathrooms Ø Use holding maneuvers to fight urge to void Ø If holding maneuvers fail get incontinence- “Suzy waits till the last minute to void & then its to late” Ø Develop large capacity bladders- void 2 -3 times per day & often don’t have to void on awakening Ø When they void voluntarily it is large volumes, prolonged & requires straining Ø Often don’t take time to completely empty
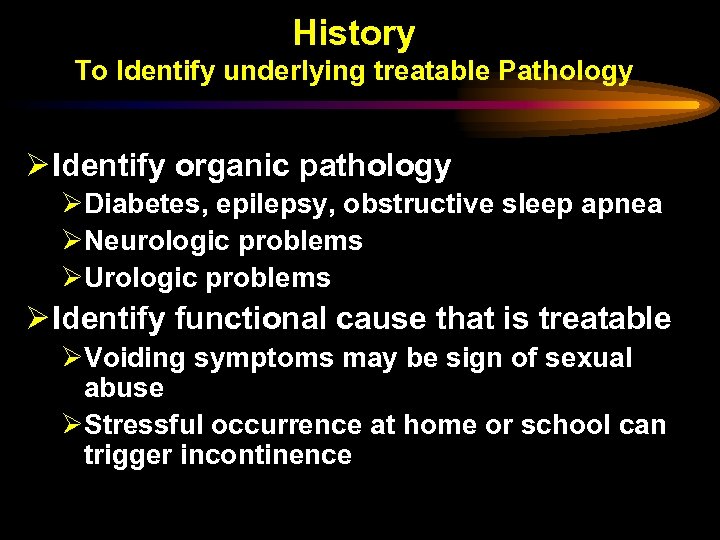 History To Identify underlying treatable Pathology Ø Identify organic pathology ØDiabetes, epilepsy, obstructive sleep apnea ØNeurologic problems ØUrologic problems Ø Identify functional cause that is treatable ØVoiding symptoms may be sign of sexual abuse ØStressful occurrence at home or school can trigger incontinence
History To Identify underlying treatable Pathology Ø Identify organic pathology ØDiabetes, epilepsy, obstructive sleep apnea ØNeurologic problems ØUrologic problems Ø Identify functional cause that is treatable ØVoiding symptoms may be sign of sexual abuse ØStressful occurrence at home or school can trigger incontinence
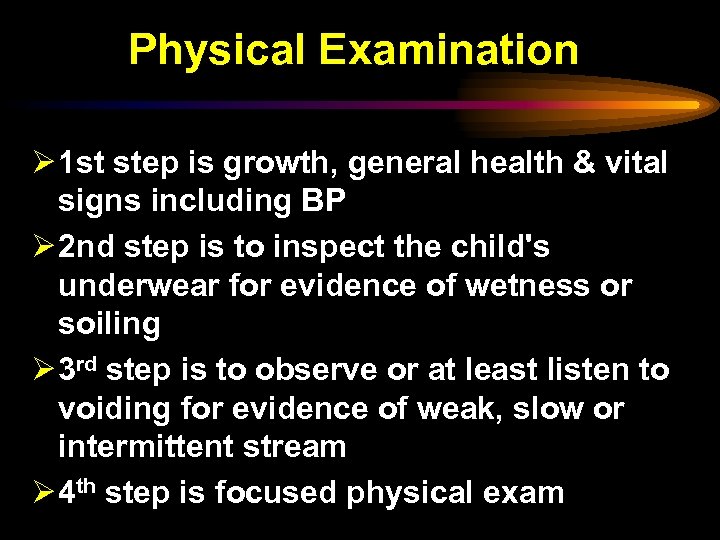 Physical Examination Ø 1 st step is growth, general health & vital signs including BP Ø 2 nd step is to inspect the child's underwear for evidence of wetness or soiling Ø 3 rd step is to observe or at least listen to voiding for evidence of weak, slow or intermittent stream Ø 4 th step is focused physical exam
Physical Examination Ø 1 st step is growth, general health & vital signs including BP Ø 2 nd step is to inspect the child's underwear for evidence of wetness or soiling Ø 3 rd step is to observe or at least listen to voiding for evidence of weak, slow or intermittent stream Ø 4 th step is focused physical exam
 Physical Examination Abdomen ØRenal masses ØDistended bladder ØLarge stool mass suggestive of constipation
Physical Examination Abdomen ØRenal masses ØDistended bladder ØLarge stool mass suggestive of constipation
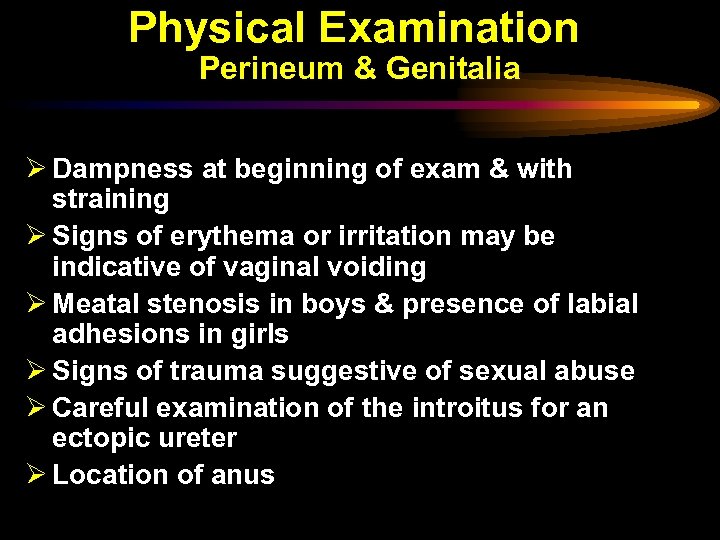 Physical Examination Perineum & Genitalia Ø Dampness at beginning of exam & with straining Ø Signs of erythema or irritation may be indicative of vaginal voiding Ø Meatal stenosis in boys & presence of labial adhesions in girls Ø Signs of trauma suggestive of sexual abuse Ø Careful examination of the introitus for an ectopic ureter Ø Location of anus
Physical Examination Perineum & Genitalia Ø Dampness at beginning of exam & with straining Ø Signs of erythema or irritation may be indicative of vaginal voiding Ø Meatal stenosis in boys & presence of labial adhesions in girls Ø Signs of trauma suggestive of sexual abuse Ø Careful examination of the introitus for an ectopic ureter Ø Location of anus
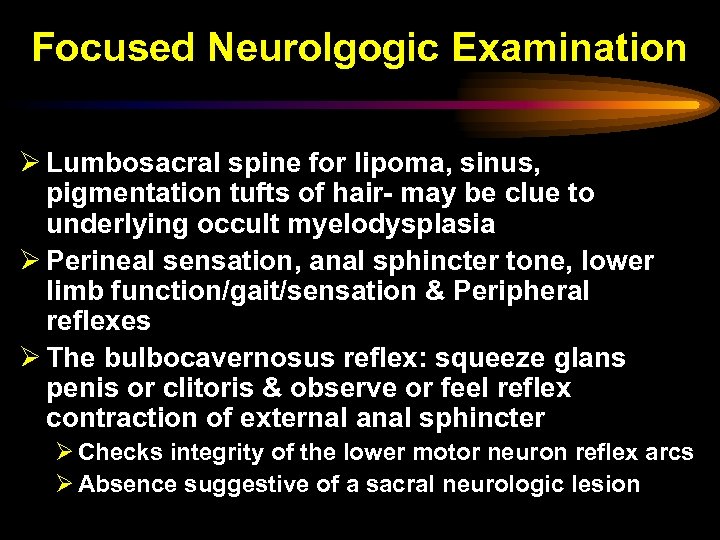 Focused Neurolgogic Examination Ø Lumbosacral spine for lipoma, sinus, pigmentation tufts of hair- may be clue to underlying occult myelodysplasia Ø Perineal sensation, anal sphincter tone, lower limb function/gait/sensation & Peripheral reflexes Ø The bulbocavernosus reflex: squeeze glans penis or clitoris & observe or feel reflex contraction of external anal sphincter Ø Checks integrity of the lower motor neuron reflex arcs Ø Absence suggestive of a sacral neurologic lesion
Focused Neurolgogic Examination Ø Lumbosacral spine for lipoma, sinus, pigmentation tufts of hair- may be clue to underlying occult myelodysplasia Ø Perineal sensation, anal sphincter tone, lower limb function/gait/sensation & Peripheral reflexes Ø The bulbocavernosus reflex: squeeze glans penis or clitoris & observe or feel reflex contraction of external anal sphincter Ø Checks integrity of the lower motor neuron reflex arcs Ø Absence suggestive of a sacral neurologic lesion

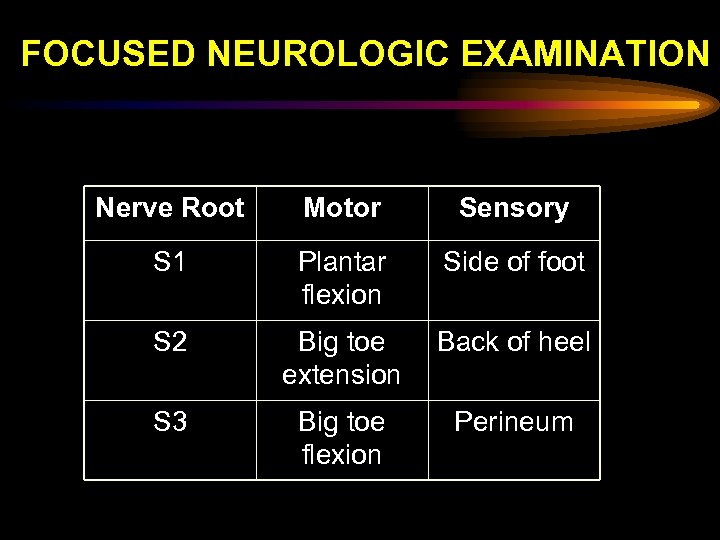 FOCUSED NEUROLOGIC EXAMINATION Nerve Root Motor Sensory S 1 Plantar flexion Side of foot S 2 Big toe extension Back of heel S 3 Big toe flexion Perineum
FOCUSED NEUROLOGIC EXAMINATION Nerve Root Motor Sensory S 1 Plantar flexion Side of foot S 2 Big toe extension Back of heel S 3 Big toe flexion Perineum
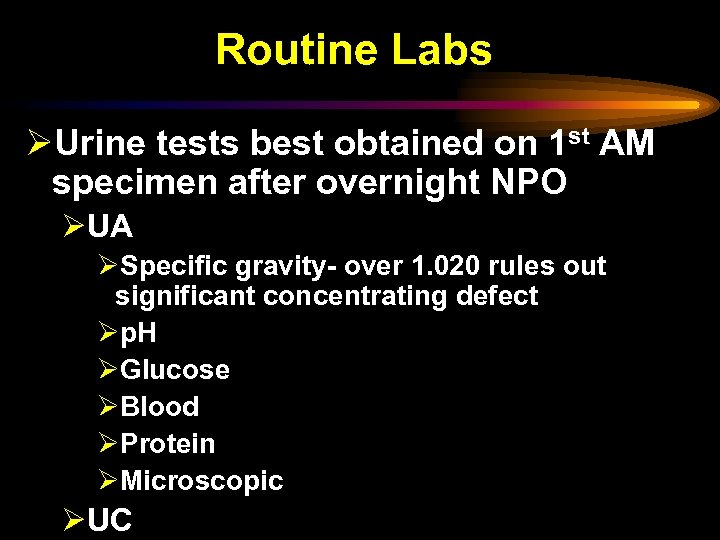 Routine Labs ØUrine tests best obtained on 1 st AM specimen after overnight NPO ØUA ØSpecific gravity- over 1. 020 rules out significant concentrating defect Øp. H ØGlucose ØBlood ØProtein ØMicroscopic ØUC
Routine Labs ØUrine tests best obtained on 1 st AM specimen after overnight NPO ØUA ØSpecific gravity- over 1. 020 rules out significant concentrating defect Øp. H ØGlucose ØBlood ØProtein ØMicroscopic ØUC
 Other Studies that can be obtained prior to referral ØPost void residual urine by catheter ØAbdominal radiograph (KUB) ØIdentifies lumbar-sacral anomalies, bowel gas patterns & amount of stool ØRenal and bladder ultrasound
Other Studies that can be obtained prior to referral ØPost void residual urine by catheter ØAbdominal radiograph (KUB) ØIdentifies lumbar-sacral anomalies, bowel gas patterns & amount of stool ØRenal and bladder ultrasound
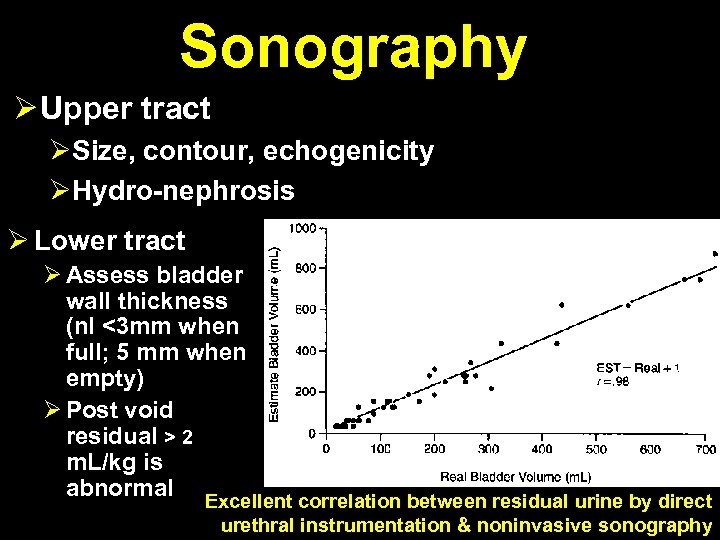 Sonography Ø Upper tract ØSize, contour, echogenicity ØHydro-nephrosis Ø Lower tract Ø Assess bladder wall thickness (nl <3 mm when full; 5 mm when empty) Ø Post void residual > 2 m. L/kg is abnormal Excellent correlation between residual urine by direct urethral instrumentation & noninvasive sonography
Sonography Ø Upper tract ØSize, contour, echogenicity ØHydro-nephrosis Ø Lower tract Ø Assess bladder wall thickness (nl <3 mm when full; 5 mm when empty) Ø Post void residual > 2 m. L/kg is abnormal Excellent correlation between residual urine by direct urethral instrumentation & noninvasive sonography
 Other Studies that can be obtained prior to referral ØNuclear Medicine renal scan ØCortical scan to RO scars or difference in function ØFunctional SCAN with/without lasix to RO obstruction ØVoiding cystourethrography ØHistory of UTIs ØFamily history of VUR
Other Studies that can be obtained prior to referral ØNuclear Medicine renal scan ØCortical scan to RO scars or difference in function ØFunctional SCAN with/without lasix to RO obstruction ØVoiding cystourethrography ØHistory of UTIs ØFamily history of VUR
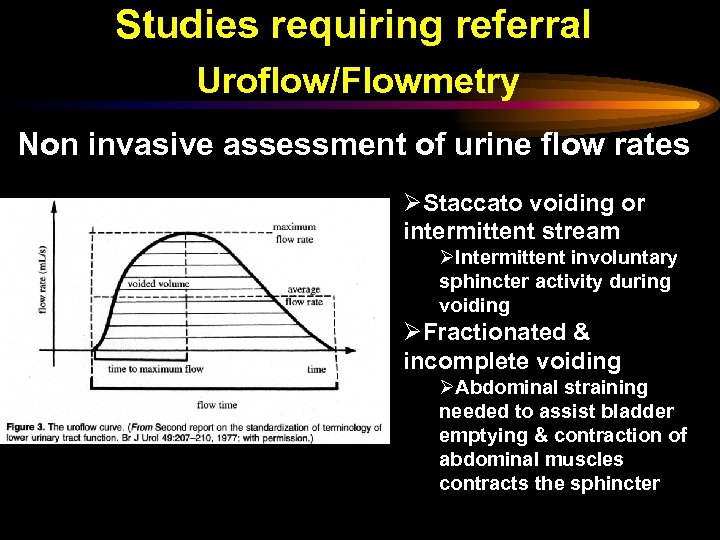 Studies requiring referral Uroflow/Flowmetry Non invasive assessment of urine flow rates ØStaccato voiding or intermittent stream ØIntermittent involuntary sphincter activity during voiding ØFractionated & incomplete voiding ØAbdominal straining needed to assist bladder emptying & contraction of abdominal muscles contracts the sphincter
Studies requiring referral Uroflow/Flowmetry Non invasive assessment of urine flow rates ØStaccato voiding or intermittent stream ØIntermittent involuntary sphincter activity during voiding ØFractionated & incomplete voiding ØAbdominal straining needed to assist bladder emptying & contraction of abdominal muscles contracts the sphincter
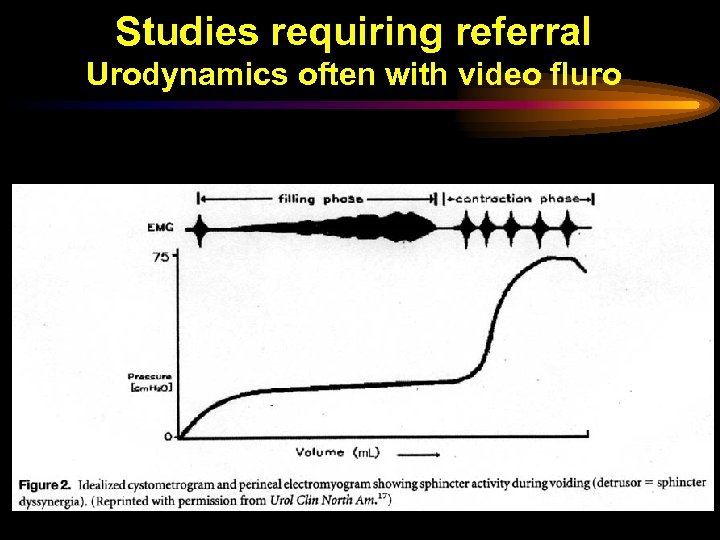 Studies requiring referral Urodynamics often with video fluro
Studies requiring referral Urodynamics often with video fluro
 Studies that should never be done ØCystoscopy with or without urethral dilation or meatotomy ØThese are rarely if ever useful and are expensive & potentially dangerous
Studies that should never be done ØCystoscopy with or without urethral dilation or meatotomy ØThese are rarely if ever useful and are expensive & potentially dangerous
 Management of Voiding Dysfunction in Children with no treatable Neruologic, Urologic or other organic etiology
Management of Voiding Dysfunction in Children with no treatable Neruologic, Urologic or other organic etiology
 Treatment of Voiding Dysfunction Non Pharmacological ØTimed voiding is the easiest & most effective Rx & it works for irritable bladder & infrequent voider ØRegular by the clock voids q 2 -3 hours during day ØBiofeedback ØKegel exercises
Treatment of Voiding Dysfunction Non Pharmacological ØTimed voiding is the easiest & most effective Rx & it works for irritable bladder & infrequent voider ØRegular by the clock voids q 2 -3 hours during day ØBiofeedback ØKegel exercises
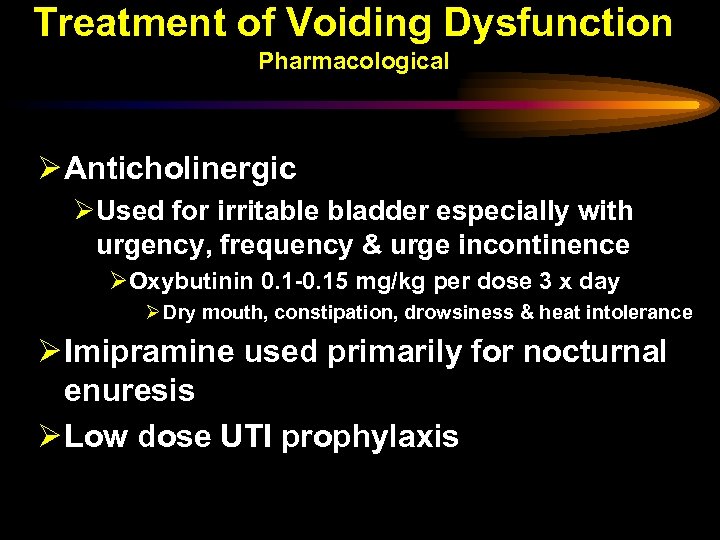 Treatment of Voiding Dysfunction Pharmacological Ø Anticholinergic ØUsed for irritable bladder especially with urgency, frequency & urge incontinence ØOxybutinin 0. 1 -0. 15 mg/kg per dose 3 x day Ø Dry mouth, constipation, drowsiness & heat intolerance Ø Imipramine used primarily for nocturnal enuresis Ø Low dose UTI prophylaxis
Treatment of Voiding Dysfunction Pharmacological Ø Anticholinergic ØUsed for irritable bladder especially with urgency, frequency & urge incontinence ØOxybutinin 0. 1 -0. 15 mg/kg per dose 3 x day Ø Dry mouth, constipation, drowsiness & heat intolerance Ø Imipramine used primarily for nocturnal enuresis Ø Low dose UTI prophylaxis
 Treatment of Voiding Dysfunction TREAT STOOLING DYSFUNCTION
Treatment of Voiding Dysfunction TREAT STOOLING DYSFUNCTION
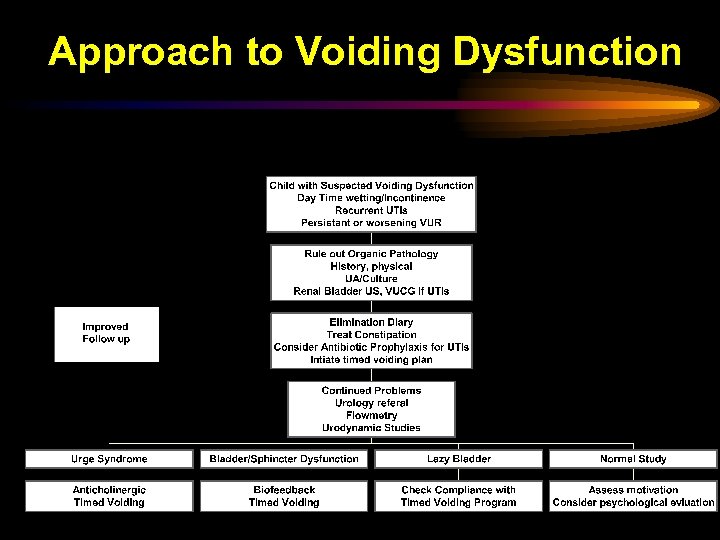 Approach to Voiding Dysfunction
Approach to Voiding Dysfunction
 Summary We have reviewed Ø Function (continent storage & voluntary emptying at low pressures) & how the lower GU tract works & how it matures Ø Relationship with lower GI tract Ø Voiding dysfunction syndromes in normal children Ø When to suspect it- UTIs, VUR, incontinence Ø How to evaluate (history, voiding diary) Ø How to RX voiding dysfunction Ø Timed urination, Ø Treat stooling dysfunction
Summary We have reviewed Ø Function (continent storage & voluntary emptying at low pressures) & how the lower GU tract works & how it matures Ø Relationship with lower GI tract Ø Voiding dysfunction syndromes in normal children Ø When to suspect it- UTIs, VUR, incontinence Ø How to evaluate (history, voiding diary) Ø How to RX voiding dysfunction Ø Timed urination, Ø Treat stooling dysfunction
 Voiding Dysfunction in Children with Neurogenic Bladder
Voiding Dysfunction in Children with Neurogenic Bladder
 Spinal cord injury (SCI) produces profound alterations in lower urinary tract function ØIncontinence ØNeurological obstruction ØElevated intravesical pressure ØVUR ØIncreased risk of UTIs ØStones
Spinal cord injury (SCI) produces profound alterations in lower urinary tract function ØIncontinence ØNeurological obstruction ØElevated intravesical pressure ØVUR ØIncreased risk of UTIs ØStones
 Neurogenic Bladder Made Simple Lack of higher CNS control results in Ø Inability to sense fullness & voluntarily void Ø Detrusor controlled by un modulated spinal reflex Ø Sphincter with fixed passive resistance- Leak Point Pressure (LPP) Ø Varies between patients may change in same patient Ø At bladder pressures < LPP no leakage Ø At bladder pressures > LPP leakage or urination Ø Sphincter may not relax when bladder contractsbladder sphincter dysnergia Ø Results in high voiding pressures
Neurogenic Bladder Made Simple Lack of higher CNS control results in Ø Inability to sense fullness & voluntarily void Ø Detrusor controlled by un modulated spinal reflex Ø Sphincter with fixed passive resistance- Leak Point Pressure (LPP) Ø Varies between patients may change in same patient Ø At bladder pressures < LPP no leakage Ø At bladder pressures > LPP leakage or urination Ø Sphincter may not relax when bladder contractsbladder sphincter dysnergia Ø Results in high voiding pressures
 Neurogenic Bladder Made Simple Ø High LPP pressure is good for continence but bad for the kidney ØProlonged LPP > than 40 cm H 2 O have been associated with ØVUR ØUpper tract deterioration ØDecreasing bladder compliance
Neurogenic Bladder Made Simple Ø High LPP pressure is good for continence but bad for the kidney ØProlonged LPP > than 40 cm H 2 O have been associated with ØVUR ØUpper tract deterioration ØDecreasing bladder compliance
 Neurogenic Bladder Made Simple ØBladder compliance is another key variable & may change over time ØDetermined by neurologic reflex activity & LPP ØPoor bladder compliance associated with ØIncontinence ØUTIs ØUpper Tract Damage
Neurogenic Bladder Made Simple ØBladder compliance is another key variable & may change over time ØDetermined by neurologic reflex activity & LPP ØPoor bladder compliance associated with ØIncontinence ØUTIs ØUpper Tract Damage
 Focus is on 2 issues ØPreservation of Renal function ØMaintaining normal bladder pressures during filling & voiding ØMinimizing UTIs ØContinence ØNot an issue in first couple of years of life
Focus is on 2 issues ØPreservation of Renal function ØMaintaining normal bladder pressures during filling & voiding ØMinimizing UTIs ØContinence ØNot an issue in first couple of years of life
 Evaluation of Newborn with Neurogenic Bladder Ø Assess upper tract for damage or evidence of high pressure (hydronephrosis) ØCreatinine, lytes ØUA & Cultures ØRenal US ØCT urography can give more detail if US abnormal ØCan do non contrast MRI if there is renal failure ØSome use nuclear studies
Evaluation of Newborn with Neurogenic Bladder Ø Assess upper tract for damage or evidence of high pressure (hydronephrosis) ØCreatinine, lytes ØUA & Cultures ØRenal US ØCT urography can give more detail if US abnormal ØCan do non contrast MRI if there is renal failure ØSome use nuclear studies
 Evaluation of Newborn with Neurogenic Bladder ØAssess lower tract for evidence of increased voiding pressure ØBladder US for bladder hypertrophy & post void residual- obtain in newborn period ØVCUG for VUR & bladder hypertrophy ØUrodynamics for LPP & compliance
Evaluation of Newborn with Neurogenic Bladder ØAssess lower tract for evidence of increased voiding pressure ØBladder US for bladder hypertrophy & post void residual- obtain in newborn period ØVCUG for VUR & bladder hypertrophy ØUrodynamics for LPP & compliance
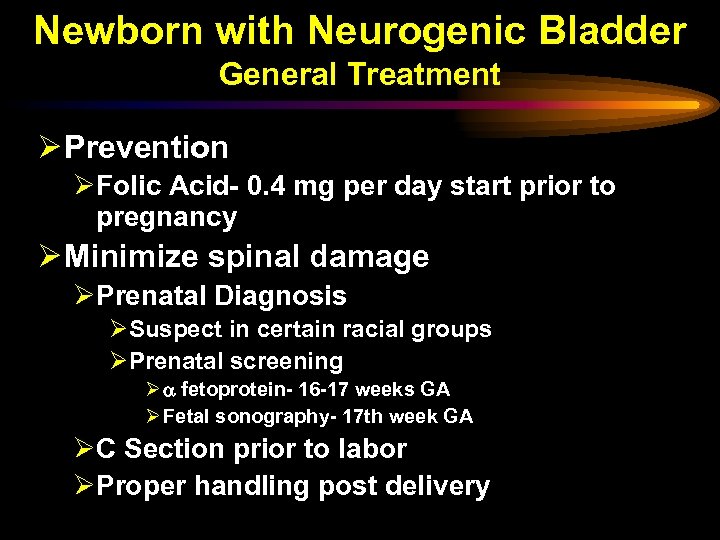 Newborn with Neurogenic Bladder General Treatment Ø Prevention ØFolic Acid- 0. 4 mg per day start prior to pregnancy Ø Minimize spinal damage ØPrenatal Diagnosis ØSuspect in certain racial groups ØPrenatal screening Ø fetoprotein- 16 -17 weeks GA Ø Fetal sonography- 17 th week GA ØC Section prior to labor ØProper handling post delivery
Newborn with Neurogenic Bladder General Treatment Ø Prevention ØFolic Acid- 0. 4 mg per day start prior to pregnancy Ø Minimize spinal damage ØPrenatal Diagnosis ØSuspect in certain racial groups ØPrenatal screening Ø fetoprotein- 16 -17 weeks GA Ø Fetal sonography- 17 th week GA ØC Section prior to labor ØProper handling post delivery
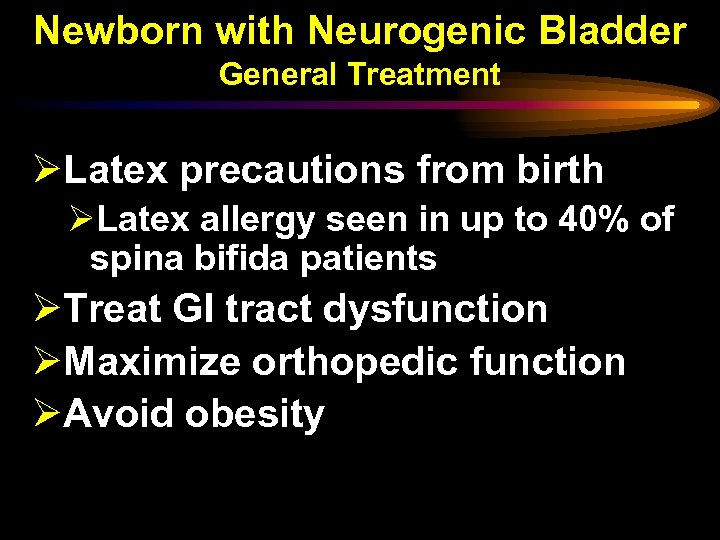 Newborn with Neurogenic Bladder General Treatment ØLatex precautions from birth ØLatex allergy seen in up to 40% of spina bifida patients ØTreat GI tract dysfunction ØMaximize orthopedic function ØAvoid obesity
Newborn with Neurogenic Bladder General Treatment ØLatex precautions from birth ØLatex allergy seen in up to 40% of spina bifida patients ØTreat GI tract dysfunction ØMaximize orthopedic function ØAvoid obesity
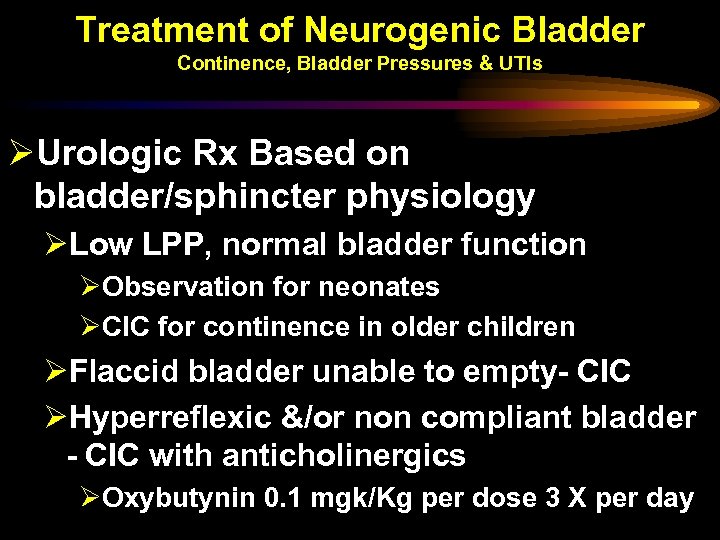 Treatment of Neurogenic Bladder Continence, Bladder Pressures & UTIs ØUrologic Rx Based on bladder/sphincter physiology ØLow LPP, normal bladder function ØObservation for neonates ØCIC for continence in older children ØFlaccid bladder unable to empty- CIC ØHyperreflexic &/or non compliant bladder - CIC with anticholinergics ØOxybutynin 0. 1 mgk/Kg per dose 3 X per day
Treatment of Neurogenic Bladder Continence, Bladder Pressures & UTIs ØUrologic Rx Based on bladder/sphincter physiology ØLow LPP, normal bladder function ØObservation for neonates ØCIC for continence in older children ØFlaccid bladder unable to empty- CIC ØHyperreflexic &/or non compliant bladder - CIC with anticholinergics ØOxybutynin 0. 1 mgk/Kg per dose 3 X per day
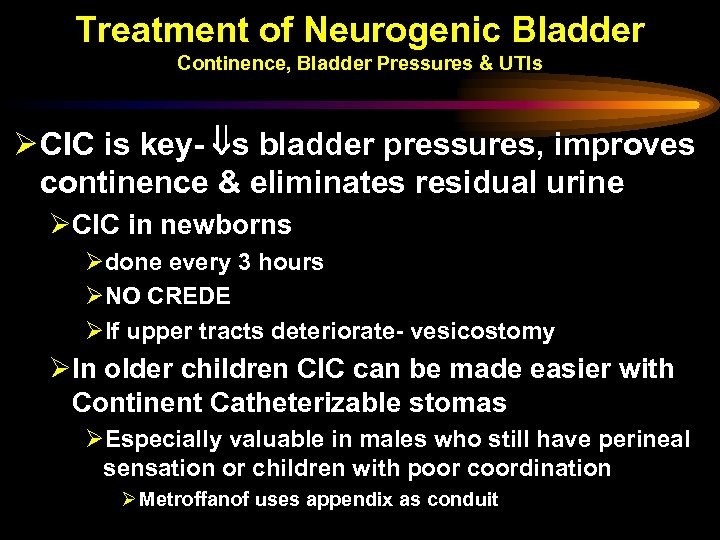 Treatment of Neurogenic Bladder Continence, Bladder Pressures & UTIs Ø CIC is key- s bladder pressures, improves continence & eliminates residual urine ØCIC in newborns Ødone every 3 hours ØNO CREDE ØIf upper tracts deteriorate- vesicostomy ØIn older children CIC can be made easier with Continent Catheterizable stomas ØEspecially valuable in males who still have perineal sensation or children with poor coordination Ø Metroffanof uses appendix as conduit
Treatment of Neurogenic Bladder Continence, Bladder Pressures & UTIs Ø CIC is key- s bladder pressures, improves continence & eliminates residual urine ØCIC in newborns Ødone every 3 hours ØNO CREDE ØIf upper tracts deteriorate- vesicostomy ØIn older children CIC can be made easier with Continent Catheterizable stomas ØEspecially valuable in males who still have perineal sensation or children with poor coordination Ø Metroffanof uses appendix as conduit
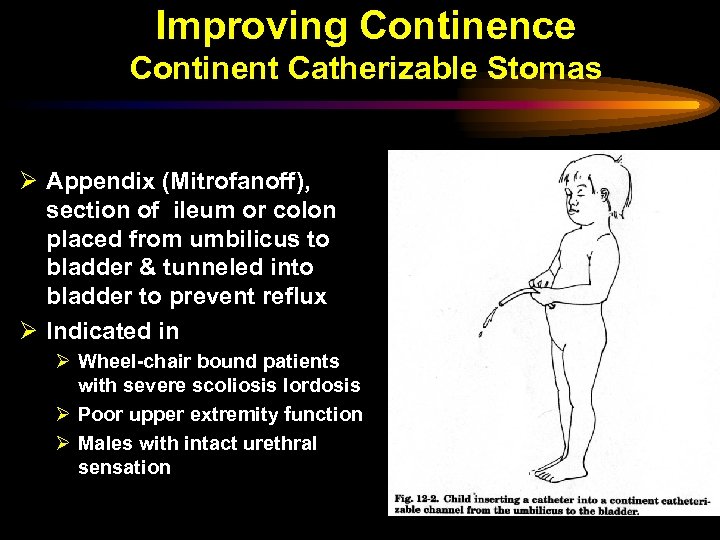 Improving Continence Continent Catherizable Stomas Ø Appendix (Mitrofanoff), section of ileum or colon placed from umbilicus to bladder & tunneled into bladder to prevent reflux Ø Indicated in Ø Wheel-chair bound patients with severe scoliosis lordosis Ø Poor upper extremity function Ø Males with intact urethral sensation
Improving Continence Continent Catherizable Stomas Ø Appendix (Mitrofanoff), section of ileum or colon placed from umbilicus to bladder & tunneled into bladder to prevent reflux Ø Indicated in Ø Wheel-chair bound patients with severe scoliosis lordosis Ø Poor upper extremity function Ø Males with intact urethral sensation
 Bladder Augmentation Ø Indicated when medical therapy fails to achieve adequate low-pressure capacity with continence Ø Variety of substances and surgical techniques used each with problems ØUse of intestinal tract allows absorption or secretion of electrolytes from or into urine Ø All require religious CIC to avoid rupture
Bladder Augmentation Ø Indicated when medical therapy fails to achieve adequate low-pressure capacity with continence Ø Variety of substances and surgical techniques used each with problems ØUse of intestinal tract allows absorption or secretion of electrolytes from or into urine Ø All require religious CIC to avoid rupture
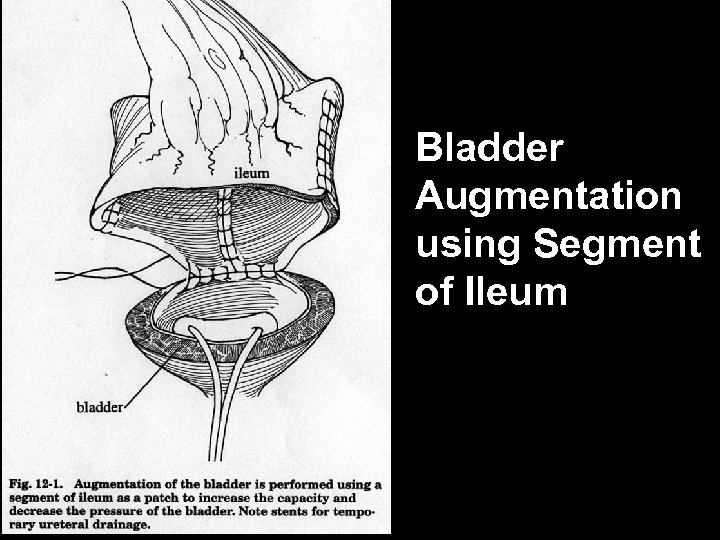 Bladder Augmentation using Segment of Ileum
Bladder Augmentation using Segment of Ileum
 Improving Continence by Increasing Sphincter Resistance Ø Adrenergic drugs (phenylpropanolamine, pseudoephedrine) increase sphincter tone ØUsually only marginally effective Ø Surgical techniques ØPeriurethral injections ØBladder neck suspension & Sling procedures ØArtificial urinary sphincter
Improving Continence by Increasing Sphincter Resistance Ø Adrenergic drugs (phenylpropanolamine, pseudoephedrine) increase sphincter tone ØUsually only marginally effective Ø Surgical techniques ØPeriurethral injections ØBladder neck suspension & Sling procedures ØArtificial urinary sphincter
 Vesicoureteral Reflux (VUR) Ø 40 -65% of neurogenic bladder patients have VUR Ø Rx aimed at reducing bladder pressures rather than fixing the VUR ØCIC ØBladder Augmentation Ø Prophylactic antibiotics controversial Ø Surgical correction of VUR indicated for ØDeterioration of upper tracts ØRecurrent pyelonephritis
Vesicoureteral Reflux (VUR) Ø 40 -65% of neurogenic bladder patients have VUR Ø Rx aimed at reducing bladder pressures rather than fixing the VUR ØCIC ØBladder Augmentation Ø Prophylactic antibiotics controversial Ø Surgical correction of VUR indicated for ØDeterioration of upper tracts ØRecurrent pyelonephritis
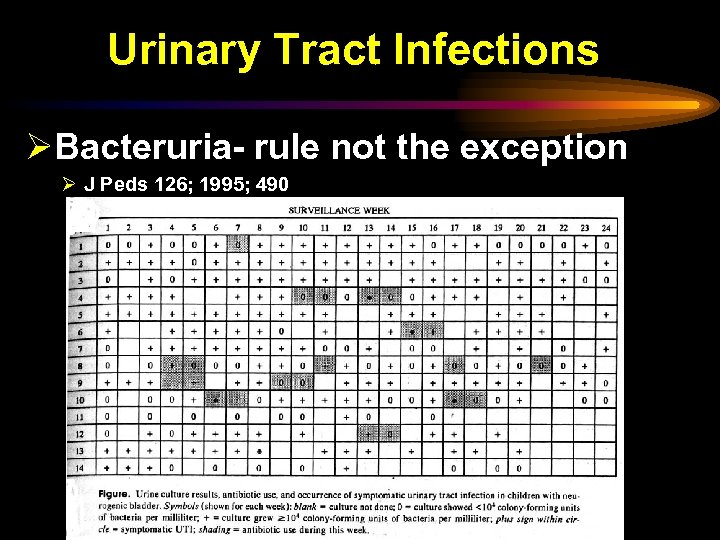 Urinary Tract Infections ØBacteruria- rule not the exception Ø J Peds 126; 1995; 490
Urinary Tract Infections ØBacteruria- rule not the exception Ø J Peds 126; 1995; 490
 Urinary Tract Infections ØTreatment of asymptomatic bacteriuria in SCI patients of no proven benefit ØDo not treat cultures treat patients ØWorking definition of true UTI in these patients is fever with + UC
Urinary Tract Infections ØTreatment of asymptomatic bacteriuria in SCI patients of no proven benefit ØDo not treat cultures treat patients ØWorking definition of true UTI in these patients is fever with + UC
 Rx of Urinary Tract Infections ØSymptomatic UTIs treated with narrowest spectrum antibiotics for the shortest possible time ØSame antibiotics as used for Rx of complicated UTIs in general population
Rx of Urinary Tract Infections ØSymptomatic UTIs treated with narrowest spectrum antibiotics for the shortest possible time ØSame antibiotics as used for Rx of complicated UTIs in general population
 Rx of Urinary Tract Infections ØProphylaxis does not decrease UTIs or asymptomatic bacteruria- (J Peds 132; 1998; 704) ØSome still use if there is VUR Ø Other methods also unsuccessful ØCranberry juice- J Peds 135; 1999; 698 ØSingle use sterile catheter Peds 108; 2001
Rx of Urinary Tract Infections ØProphylaxis does not decrease UTIs or asymptomatic bacteruria- (J Peds 132; 1998; 704) ØSome still use if there is VUR Ø Other methods also unsuccessful ØCranberry juice- J Peds 135; 1999; 698 ØSingle use sterile catheter Peds 108; 2001
 Summary We have reviewed Ø Function (storage & voluntary emptying at low pressures) & how the lower GU tract works & how it matures Ø Relationship with lower GI tract Ø Voiding dysfunction in normal children Ø When to suspect it- UTIs, VUR, incontinence Ø How to evaluate (voiding diary) & Rx it (timed urination) Ø Evaluation & Rx of children with neurogenic bladder- focus on preserving upper tract & continence
Summary We have reviewed Ø Function (storage & voluntary emptying at low pressures) & how the lower GU tract works & how it matures Ø Relationship with lower GI tract Ø Voiding dysfunction in normal children Ø When to suspect it- UTIs, VUR, incontinence Ø How to evaluate (voiding diary) & Rx it (timed urination) Ø Evaluation & Rx of children with neurogenic bladder- focus on preserving upper tract & continence
 References Ø Pediatric Clinics N America 48; Dec 01 1489 -1503 & 1505 -1518 Ø Fernandes; The Unstable Bladder in children; Journal Peds; 118; 1991; 831 Ø Pediatrics in Review; Volume 21 Number 10 October 2000; 336 -341
References Ø Pediatric Clinics N America 48; Dec 01 1489 -1503 & 1505 -1518 Ø Fernandes; The Unstable Bladder in children; Journal Peds; 118; 1991; 831 Ø Pediatrics in Review; Volume 21 Number 10 October 2000; 336 -341


