e814787b03c0684ae9c9986f18cb401a.ppt
- Количество слайдов: 47
 Violence against Doctors in the English National Health Service: the undermining of trust? Jonathan Gabe Royal Holloway, University of London
Violence against Doctors in the English National Health Service: the undermining of trust? Jonathan Gabe Royal Holloway, University of London
 Introduction l l Claimed we live in insecure times Fear & risk said to dominate people’s thinking Working in health care often considered risky - violence from patients and others Surveys show doctors & nurses at risk of threats & assaults (British Crime Survey – Upson 2004))
Introduction l l Claimed we live in insecure times Fear & risk said to dominate people’s thinking Working in health care often considered risky - violence from patients and others Surveys show doctors & nurses at risk of threats & assaults (British Crime Survey – Upson 2004))
 Violence against General Practitioners Most research on violence in hospitals l What about those health care workers who are based in the community – GPs? l Use to throw light on Trust relations - Doctors/Patients l Do doctors feel trust being undermined? l
Violence against General Practitioners Most research on violence in hospitals l What about those health care workers who are based in the community – GPs? l Use to throw light on Trust relations - Doctors/Patients l Do doctors feel trust being undermined? l
 Sociological approaches to the medical profession (1) l 1970 s-80 s professional dominance & autonomy - doctors dominating division of labour - maintaining status & privilege – e. g in negotiations with state - expressing paternalistic/ patriarchal values with patients l 1980 s dominance challenged - de-professionalisation USA (Haug) declining knowledge gap increase in lay knowledge reduced cultural authority -
Sociological approaches to the medical profession (1) l 1970 s-80 s professional dominance & autonomy - doctors dominating division of labour - maintaining status & privilege – e. g in negotiations with state - expressing paternalistic/ patriarchal values with patients l 1980 s dominance challenged - de-professionalisation USA (Haug) declining knowledge gap increase in lay knowledge reduced cultural authority -
 Sociological approaches to the medical profession – increasing emphasis on Trust (2) l 1990 s-2000 s end of `golden age’ of doctoring USA (Mc. Kinlay & Marceau 2003) Macro level – bureaucratisation – globalisation of information - knowledgeable patients evaluate treatments afterwards Micro level – patients more in control – shop around – trust doctors less
Sociological approaches to the medical profession – increasing emphasis on Trust (2) l 1990 s-2000 s end of `golden age’ of doctoring USA (Mc. Kinlay & Marceau 2003) Macro level – bureaucratisation – globalisation of information - knowledgeable patients evaluate treatments afterwards Micro level – patients more in control – shop around – trust doctors less
 Decline in Trust part of challenge to Medicine’s Authority l l l Trust a major concern for medical profession in the UK Fuelled by Medical Scandals - patient safety – Shipman, Bristol Hospital Concern of the British state - attempts to raise standards - clinical governance, protocols, audit
Decline in Trust part of challenge to Medicine’s Authority l l l Trust a major concern for medical profession in the UK Fuelled by Medical Scandals - patient safety – Shipman, Bristol Hospital Concern of the British state - attempts to raise standards - clinical governance, protocols, audit
 What is Trust - Trust relations in health care (1) l Trust essential to smooth functioning of society - grease that helps wheels of society move l Public Trust - Trust in institution/system - Generalised attitude - influenced by contact with the system & media reports l Interpersonal Trust - Trust placed by one person in another - Ability to take for granted motives/behaviour of others - Give others benefit of doubt - Important in health care where risk and uncertainty key - Patients feel vulnerable due to illness & unequal relations (Calnan & Rowe 2008)
What is Trust - Trust relations in health care (1) l Trust essential to smooth functioning of society - grease that helps wheels of society move l Public Trust - Trust in institution/system - Generalised attitude - influenced by contact with the system & media reports l Interpersonal Trust - Trust placed by one person in another - Ability to take for granted motives/behaviour of others - Give others benefit of doubt - Important in health care where risk and uncertainty key - Patients feel vulnerable due to illness & unequal relations (Calnan & Rowe 2008)
 What is Trust - Trust relations in health care (2) Most literature on interpersonal trust - but from patient’s perspective l What about from practitioner perspective? l Meaning of trust to doctors - feel undermined by actions of patients? - not respected l OR is nature of trust changing – from blind/passive trust to Informed/active Trust? l
What is Trust - Trust relations in health care (2) Most literature on interpersonal trust - but from patient’s perspective l What about from practitioner perspective? l Meaning of trust to doctors - feel undermined by actions of patients? - not respected l OR is nature of trust changing – from blind/passive trust to Informed/active Trust? l
 Trust for General Practitioners l l l Focus on whether GPs see trust changing? Use study of violence against GPs as way to consider this What does it tell us about interpersonal trust between doctors & patients?
Trust for General Practitioners l l l Focus on whether GPs see trust changing? Use study of violence against GPs as way to consider this What does it tell us about interpersonal trust between doctors & patients?
 Working as a GP in the English NHS VISIBILITY OF GPs IN THE COMMUNITY - may still live locally - problem of separating professional/personal life - less home visits/COOPs l DECLINE IN RECRUITMENT & MORALE - recruitment problems – especially inner city/London - overworked/morale low? l
Working as a GP in the English NHS VISIBILITY OF GPs IN THE COMMUNITY - may still live locally - problem of separating professional/personal life - less home visits/COOPs l DECLINE IN RECRUITMENT & MORALE - recruitment problems – especially inner city/London - overworked/morale low? l
 Study Research Questions l How often do GPs experience violent/abusive behaviour? l To what extent is this violence a consequence of a loss of authority? l Are younger GPs less concerned about such a loss of authority/more in favour of an egalitarian relationship? l l What role do other factors play in violence experienced by GPs? - patient’s illness/addiction - patient’s socio-economic circumstances - over-stretched service delivery What are the implications for doctors’ trust in patients?
Study Research Questions l How often do GPs experience violent/abusive behaviour? l To what extent is this violence a consequence of a loss of authority? l Are younger GPs less concerned about such a loss of authority/more in favour of an egalitarian relationship? l l What role do other factors play in violence experienced by GPs? - patient’s illness/addiction - patient’s socio-economic circumstances - over-stretched service delivery What are the implications for doctors’ trust in patients?
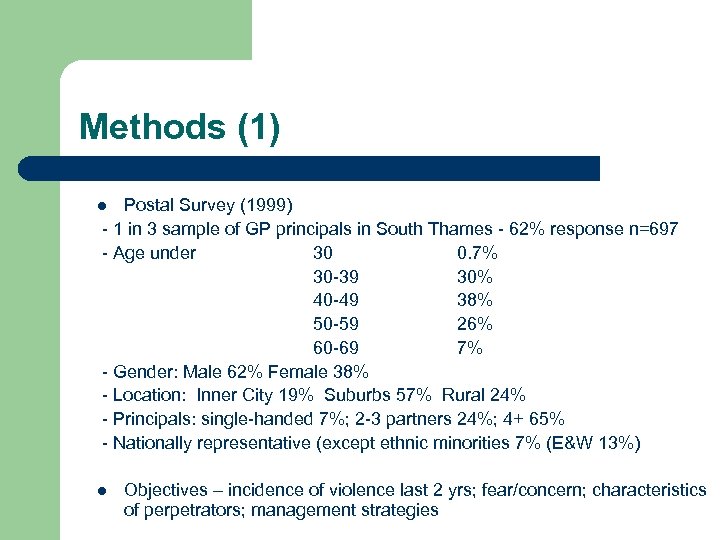 Methods (1) Postal Survey (1999) - 1 in 3 sample of GP principals in South Thames - 62% response n=697 - Age under 30 0. 7% 30 -39 30% 40 -49 38% 50 -59 26% 60 -69 7% - Gender: Male 62% Female 38% - Location: Inner City 19% Suburbs 57% Rural 24% - Principals: single-handed 7%; 2 -3 partners 24%; 4+ 65% - Nationally representative (except ethnic minorities 7% (E&W 13%) l l Objectives – incidence of violence last 2 yrs; fear/concern; characteristics of perpetrators; management strategies
Methods (1) Postal Survey (1999) - 1 in 3 sample of GP principals in South Thames - 62% response n=697 - Age under 30 0. 7% 30 -39 30% 40 -49 38% 50 -59 26% 60 -69 7% - Gender: Male 62% Female 38% - Location: Inner City 19% Suburbs 57% Rural 24% - Principals: single-handed 7%; 2 -3 partners 24%; 4+ 65% - Nationally representative (except ethnic minorities 7% (E&W 13%) l l Objectives – incidence of violence last 2 yrs; fear/concern; characteristics of perpetrators; management strategies
 Methods (2) Follow-up `in depth’ interviews (2000) - 26 doctors – assaulted or threatened - spread almost equally across 3 age groups (<40. 40 -9. >50) - more from inner city practices (16 inner city; 10 suburban/town) l Objectives: - explanations for violence - context for specific incidents - consequences for victim/relatives - impact on practice l
Methods (2) Follow-up `in depth’ interviews (2000) - 26 doctors – assaulted or threatened - spread almost equally across 3 age groups (<40. 40 -9. >50) - more from inner city practices (16 inner city; 10 suburban/town) l Objectives: - explanations for violence - context for specific incidents - consequences for victim/relatives - impact on practice l
 Defining Violence (1) l Critique of traditional definition for focusing on physical assaults l Ignores emotional consequences of verbal violence/stalking l STUDY DEFINITION INCLUSIVE: `any incident involving abuse, threats or assaults related to work, affecting safety, well-being or health’
Defining Violence (1) l Critique of traditional definition for focusing on physical assaults l Ignores emotional consequences of verbal violence/stalking l STUDY DEFINITION INCLUSIVE: `any incident involving abuse, threats or assaults related to work, affecting safety, well-being or health’
 Defining Violence (2) l l l Questionnaire based on assumptions about what counts as violence Disruptive behaviour – complaining loudly, rudeness, shouting, verbal abuse Threats - self / relative Violent behaviour - pushed, kicked, punched, hit with weapon, sexual assault. Incidence relates to last 2 years / most recent In interviews asked for respondents’ own definitions
Defining Violence (2) l l l Questionnaire based on assumptions about what counts as violence Disruptive behaviour – complaining loudly, rudeness, shouting, verbal abuse Threats - self / relative Violent behaviour - pushed, kicked, punched, hit with weapon, sexual assault. Incidence relates to last 2 years / most recent In interviews asked for respondents’ own definitions
 Presentation of data l Quantitative Data on extent of violence experienced – age differences l Qualitative data on meaning of violence
Presentation of data l Quantitative Data on extent of violence experienced – age differences l Qualitative data on meaning of violence
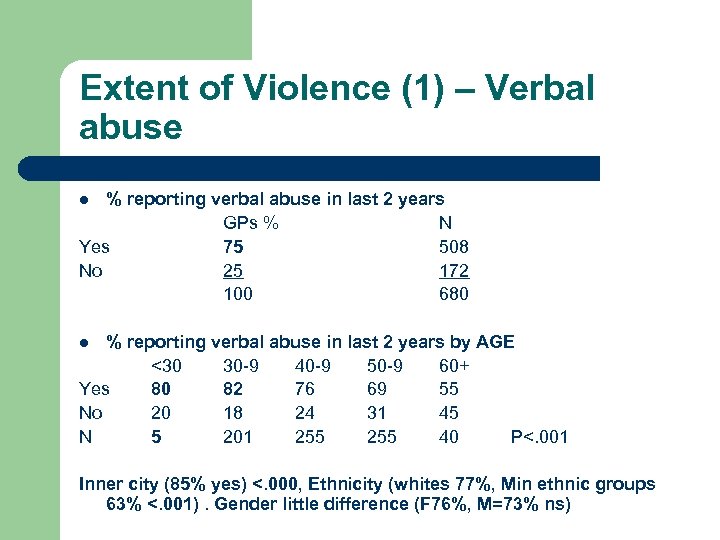 Extent of Violence (1) – Verbal abuse % reporting verbal abuse in last 2 years GPs % N Yes 75 508 No 25 172 100 680 l % reporting verbal abuse in last 2 years by AGE <30 30 -9 40 -9 50 -9 60+ Yes 80 82 76 69 55 No 20 18 24 31 45 N 5 201 255 40 P<. 001 l Inner city (85% yes) <. 000, Ethnicity (whites 77%, Min ethnic groups 63% <. 001). Gender little difference (F 76%, M=73% ns)
Extent of Violence (1) – Verbal abuse % reporting verbal abuse in last 2 years GPs % N Yes 75 508 No 25 172 100 680 l % reporting verbal abuse in last 2 years by AGE <30 30 -9 40 -9 50 -9 60+ Yes 80 82 76 69 55 No 20 18 24 31 45 N 5 201 255 40 P<. 001 l Inner city (85% yes) <. 000, Ethnicity (whites 77%, Min ethnic groups 63% <. 001). Gender little difference (F 76%, M=73% ns)
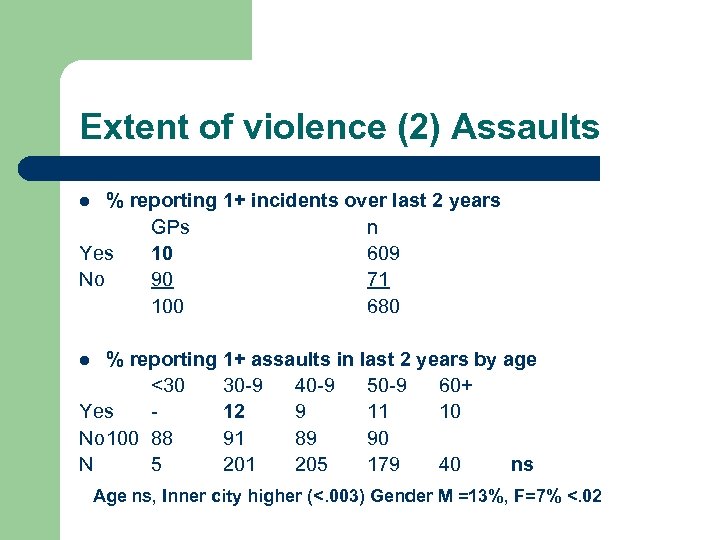 Extent of violence (2) Assaults % reporting 1+ incidents over last 2 years GPs n Yes 10 609 No 90 71 100 680 l % reporting 1+ assaults in last 2 years by age <30 30 -9 40 -9 50 -9 60+ Yes 12 9 11 10 No 100 88 91 89 90 N 5 201 205 179 40 ns l Age ns, Inner city higher (<. 003) Gender M =13%, F=7% <. 02
Extent of violence (2) Assaults % reporting 1+ incidents over last 2 years GPs n Yes 10 609 No 90 71 100 680 l % reporting 1+ assaults in last 2 years by age <30 30 -9 40 -9 50 -9 60+ Yes 12 9 11 10 No 100 88 91 89 90 N 5 201 205 179 40 ns l Age ns, Inner city higher (<. 003) Gender M =13%, F=7% <. 02
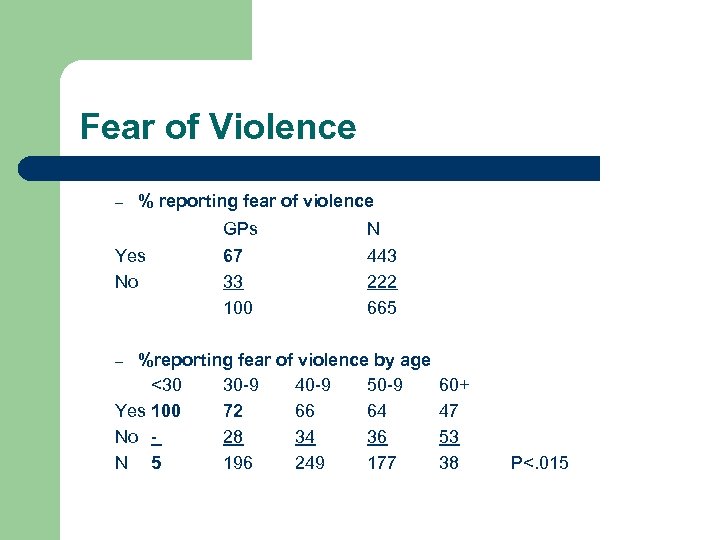 Fear of Violence – % reporting fear of violence Yes No GPs 67 33 100 N 443 222 665 %reporting fear of violence by age <30 30 -9 40 -9 50 -9 Yes 100 72 66 64 No 28 34 36 N 5 196 249 177 – 60+ 47 53 38 P<. 015
Fear of Violence – % reporting fear of violence Yes No GPs 67 33 100 N 443 222 665 %reporting fear of violence by age <30 30 -9 40 -9 50 -9 Yes 100 72 66 64 No 28 34 36 N 5 196 249 177 – 60+ 47 53 38 P<. 015
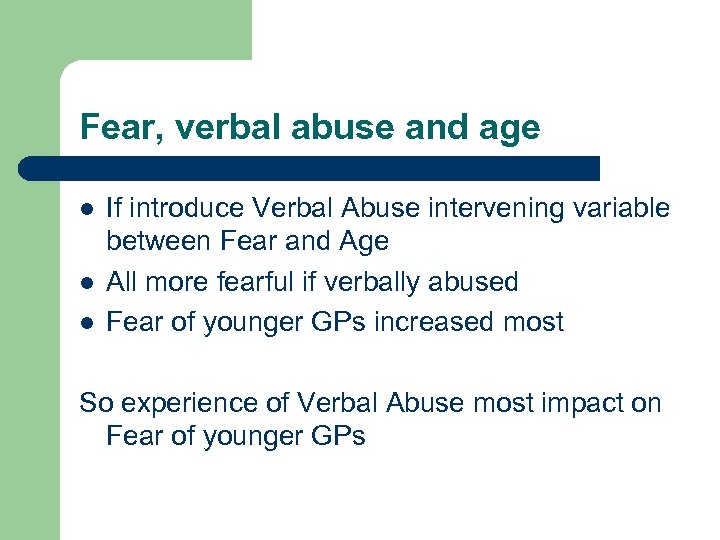 Fear, verbal abuse and age l l l If introduce Verbal Abuse intervening variable between Fear and Age All more fearful if verbally abused Fear of younger GPs increased most So experience of Verbal Abuse most impact on Fear of younger GPs
Fear, verbal abuse and age l l l If introduce Verbal Abuse intervening variable between Fear and Age All more fearful if verbally abused Fear of younger GPs increased most So experience of Verbal Abuse most impact on Fear of younger GPs
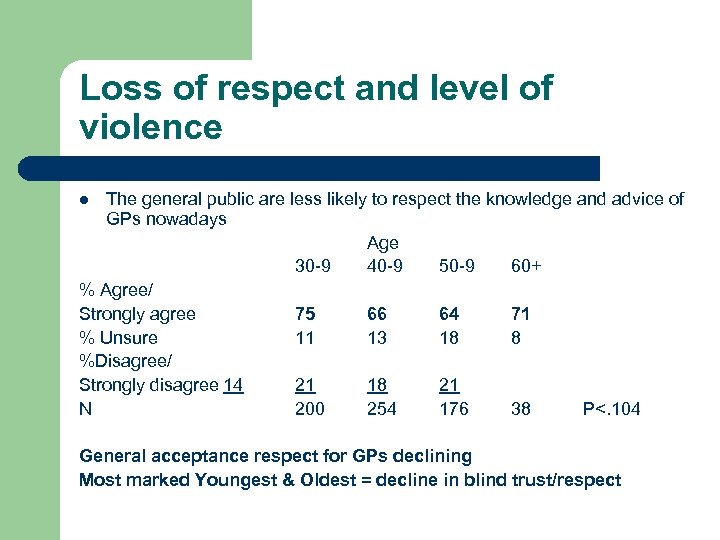 Loss of respect and level of violence The general public are less likely to respect the knowledge and advice of GPs nowadays Age 30 -9 40 -9 50 -9 60+ % Agree/ Strongly agree 75 66 64 71 % Unsure 11 13 18 8 %Disagree/ Strongly disagree 14 21 18 21 N 200 254 176 38 P<. 104 l General acceptance respect for GPs declining Most marked Youngest & Oldest = decline in blind trust/respect
Loss of respect and level of violence The general public are less likely to respect the knowledge and advice of GPs nowadays Age 30 -9 40 -9 50 -9 60+ % Agree/ Strongly agree 75 66 64 71 % Unsure 11 13 18 8 %Disagree/ Strongly disagree 14 21 18 21 N 200 254 176 38 P<. 104 l General acceptance respect for GPs declining Most marked Youngest & Oldest = decline in blind trust/respect
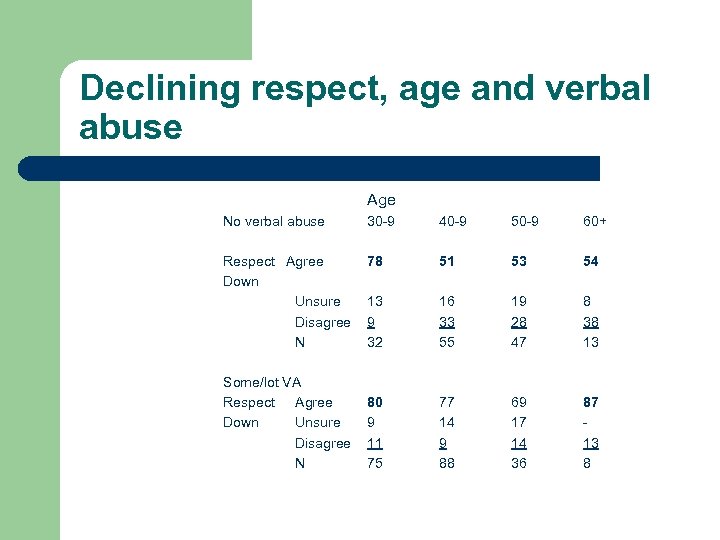 Declining respect, age and verbal abuse Age No verbal abuse 30 -9 40 -9 50 -9 60+ Respect Agree Down Unsure Disagree N 78 51 53 54 13 9 32 16 33 55 19 28 47 8 38 13 80 9 11 75 77 14 9 88 69 17 14 36 87 13 8 Some/lot VA Respect Agree Down Unsure Disagree N
Declining respect, age and verbal abuse Age No verbal abuse 30 -9 40 -9 50 -9 60+ Respect Agree Down Unsure Disagree N 78 51 53 54 13 9 32 16 33 55 19 28 47 8 38 13 80 9 11 75 77 14 9 88 69 17 14 36 87 13 8 Some/lot VA Respect Agree Down Unsure Disagree N
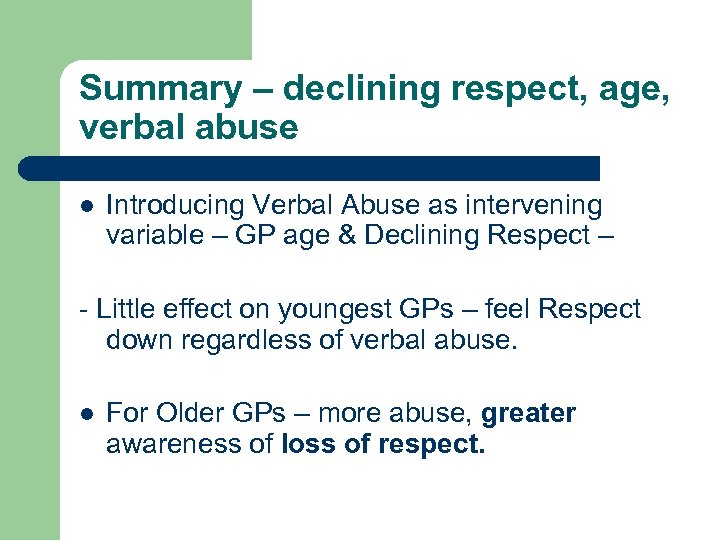 Summary – declining respect, age, verbal abuse l Introducing Verbal Abuse as intervening variable – GP age & Declining Respect – - Little effect on youngest GPs – feel Respect down regardless of verbal abuse. l For Older GPs – more abuse, greater awareness of loss of respect.
Summary – declining respect, age, verbal abuse l Introducing Verbal Abuse as intervening variable – GP age & Declining Respect – - Little effect on youngest GPs – feel Respect down regardless of verbal abuse. l For Older GPs – more abuse, greater awareness of loss of respect.
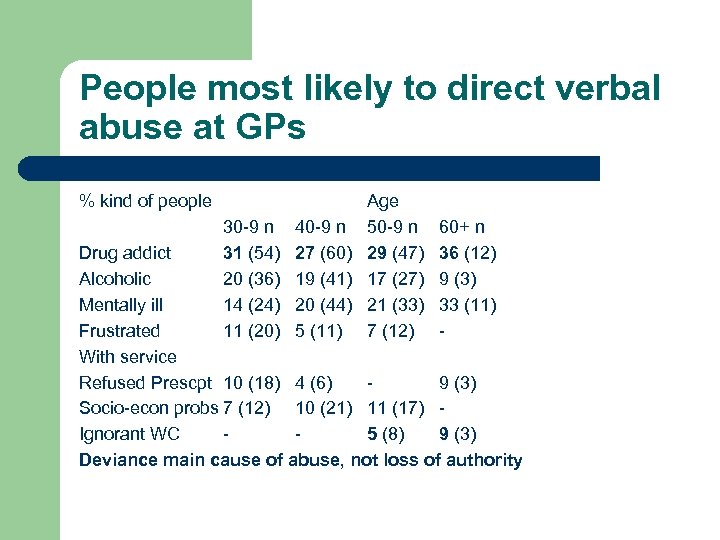 People most likely to direct verbal abuse at GPs % kind of people Age 30 -9 n 40 -9 n 50 -9 n 31 (54) 27 (60) 29 (47) 20 (36) 19 (41) 17 (27) 14 (24) 20 (44) 21 (33) 11 (20) 5 (11) 7 (12) 60+ n 36 (12) 9 (3) 33 (11) - Drug addict Alcoholic Mentally ill Frustrated With service Refused Prescpt 10 (18) 4 (6) 9 (3) Socio-econ probs 7 (12) 10 (21) 11 (17) Ignorant WC 5 (8) 9 (3) Deviance main cause of abuse, not loss of authority
People most likely to direct verbal abuse at GPs % kind of people Age 30 -9 n 40 -9 n 50 -9 n 31 (54) 27 (60) 29 (47) 20 (36) 19 (41) 17 (27) 14 (24) 20 (44) 21 (33) 11 (20) 5 (11) 7 (12) 60+ n 36 (12) 9 (3) 33 (11) - Drug addict Alcoholic Mentally ill Frustrated With service Refused Prescpt 10 (18) 4 (6) 9 (3) Socio-econ probs 7 (12) 10 (21) 11 (17) Ignorant WC 5 (8) 9 (3) Deviance main cause of abuse, not loss of authority
 Summary – Quantitative Data l l Overall Violence a problem for Young/Inner City GPs feel lost Authority – esp Young & Old Young feel loss of status regardless of verbal abuse, Older feel this if experienced Violence Deviance main cause of verbal abuse – all GPs
Summary – Quantitative Data l l Overall Violence a problem for Young/Inner City GPs feel lost Authority – esp Young & Old Young feel loss of status regardless of verbal abuse, Older feel this if experienced Violence Deviance main cause of verbal abuse – all GPs
 Qualitative Data l l l Interviews with 26 GPs – assaulted/threatened Use to test quantitative findings When asked if patients becoming less deferential – most agreed Young patients seen as least respectful Older patients most respectful Younger GPs most likely to say this // survey
Qualitative Data l l l Interviews with 26 GPs – assaulted/threatened Use to test quantitative findings When asked if patients becoming less deferential – most agreed Young patients seen as least respectful Older patients most respectful Younger GPs most likely to say this // survey
 Age differences in patient deference `There are different attitudes from different groups. There’s one group who have been with this practice for 20, 30 years with us. . And wouldn’t say anything (disrespectful). And there is another group of patients who don’t have that sort of respect or attitude at all, especially the young age group. . There is a difference in attitude among some of the youngsters belonging to the low socioeconomic classes where they can be very demanding and can lose their patience or control or respect. . They can explode on any trigger. . So we tend to get both. Like an elderly patient. . Would say “you decide doctor, you know best” and another would say “I want this and I want it now” sort of attitude. ’ (170, female GP, aged 38)
Age differences in patient deference `There are different attitudes from different groups. There’s one group who have been with this practice for 20, 30 years with us. . And wouldn’t say anything (disrespectful). And there is another group of patients who don’t have that sort of respect or attitude at all, especially the young age group. . There is a difference in attitude among some of the youngsters belonging to the low socioeconomic classes where they can be very demanding and can lose their patience or control or respect. . They can explode on any trigger. . So we tend to get both. Like an elderly patient. . Would say “you decide doctor, you know best” and another would say “I want this and I want it now” sort of attitude. ’ (170, female GP, aged 38)
 Role of Consumerism l Many GPs linked decline in deference to Consumerism l Role of government policy – Patients’ Charter l Role of Mass Media
Role of Consumerism l Many GPs linked decline in deference to Consumerism l Role of government policy – Patients’ Charter l Role of Mass Media
 Consumerism and the Patient’s Charter `There’s been a big change in the last few years in terms of patient anger and demand, a huge change, particularly in the last 5 years. . We get a lot more complaints than we used to do. Complaints were incredibly rare 30 years ago and now we get a complaint once a fortnight probably. You know a proper complaint. . I think they are angry people who’ve got to offload some frustration and anger somewhere. I don’t think it has been helped by the Patient’s Charter and encouragement to complain about everything in every walk of life. There’s no Doctor’s Charter!’ (3094), female GP, aged 56)
Consumerism and the Patient’s Charter `There’s been a big change in the last few years in terms of patient anger and demand, a huge change, particularly in the last 5 years. . We get a lot more complaints than we used to do. Complaints were incredibly rare 30 years ago and now we get a complaint once a fortnight probably. You know a proper complaint. . I think they are angry people who’ve got to offload some frustration and anger somewhere. I don’t think it has been helped by the Patient’s Charter and encouragement to complain about everything in every walk of life. There’s no Doctor’s Charter!’ (3094), female GP, aged 56)
 Factors minimising loss of deference (1) Not all GPs saw decline in deference as inevitable l Countervailing factors - small size of practice - length of time worked in practice - living locally l
Factors minimising loss of deference (1) Not all GPs saw decline in deference as inevitable l Countervailing factors - small size of practice - length of time worked in practice - living locally l
 Factor minimising loss of deference (2) `I think it is nearly thirty years I’ve worked in this area and twenty years as a full partner. I have got to know the practice, the patients extremely well. And I think that fosters a degree of … you have a different relationship with your patients if you are a pillar of the community I suppose, a well known member of the community which I am, I live locally’. (3360, female GP, aged 56)
Factor minimising loss of deference (2) `I think it is nearly thirty years I’ve worked in this area and twenty years as a full partner. I have got to know the practice, the patients extremely well. And I think that fosters a degree of … you have a different relationship with your patients if you are a pillar of the community I suppose, a well known member of the community which I am, I live locally’. (3360, female GP, aged 56)
 Different views of Declining Deference For some a Good Thing - end subservience - suggests more equal relationship - importance of Mutual Respect = EGALITARIAN WORLD VIEW l For others a matter of Regret - no longer looked up to/pillar of community - now them and us - feel used by patients = TRADITIONALIST WORLD VIEW l
Different views of Declining Deference For some a Good Thing - end subservience - suggests more equal relationship - importance of Mutual Respect = EGALITARIAN WORLD VIEW l For others a matter of Regret - no longer looked up to/pillar of community - now them and us - feel used by patients = TRADITIONALIST WORLD VIEW l
 Making sense of loss of deference – Egalitarian World View (1) `My Dad worked in a rural practice. He was the centre of the community, you know. They all thought he was wonderful and he’d get Christmas presents flooding through the door. And that’s not nearly the same. . I think that sort of deference and subservience that the people adopted, it’s a certain respect, people have lost that a lot, which I think is good. But it doesn’t mean they’re rude or bossy all the time. They just have a different kind of respect. It’s like they respect me like I respect them. She continued:
Making sense of loss of deference – Egalitarian World View (1) `My Dad worked in a rural practice. He was the centre of the community, you know. They all thought he was wonderful and he’d get Christmas presents flooding through the door. And that’s not nearly the same. . I think that sort of deference and subservience that the people adopted, it’s a certain respect, people have lost that a lot, which I think is good. But it doesn’t mean they’re rude or bossy all the time. They just have a different kind of respect. It’s like they respect me like I respect them. She continued:
 Making sense of loss of deference – a preference for mutual respect (2) `We don’t have the same power that doctors used to have. So I think if people have respect for me as a GP it’s partly as a person and partly for my knowledge, but much less for my authority… People aren’t afraid of me. . Of their doctors any more. They might respect them but it’s not fear, whereas I think they used to be a lot of that. It was like the priest, the policeman and the doctor, and you were going to be caught by any of them doing anything. ’ (2562, female GP, aged 34)
Making sense of loss of deference – a preference for mutual respect (2) `We don’t have the same power that doctors used to have. So I think if people have respect for me as a GP it’s partly as a person and partly for my knowledge, but much less for my authority… People aren’t afraid of me. . Of their doctors any more. They might respect them but it’s not fear, whereas I think they used to be a lot of that. It was like the priest, the policeman and the doctor, and you were going to be caught by any of them doing anything. ’ (2562, female GP, aged 34)
 Making sense of a loss of deference – regret for a lost past Traditionalist World View `when I first came into practice a doctor was a respected member of society, and people sort of looked up to you, you had some degree of respect and people would accept what you say. Now you’re actually a civil servant, it’s an `us’ and `them’ situation. You’re seen as part of the establishment and they don’t believe what you say. And obviously a lot of conflict arises from what people read in the newspapers and see on television, and if they come and talk to you about it umm. . They are less likely to accept any reasoned argument or look at the thing in perspective. People don’t respect you, they see you as a means to an end. . ’ (2470, male GP, aged 58)
Making sense of a loss of deference – regret for a lost past Traditionalist World View `when I first came into practice a doctor was a respected member of society, and people sort of looked up to you, you had some degree of respect and people would accept what you say. Now you’re actually a civil servant, it’s an `us’ and `them’ situation. You’re seen as part of the establishment and they don’t believe what you say. And obviously a lot of conflict arises from what people read in the newspapers and see on television, and if they come and talk to you about it umm. . They are less likely to accept any reasoned argument or look at the thing in perspective. People don’t respect you, they see you as a means to an end. . ’ (2470, male GP, aged 58)
 The role of Time l GPs feelings about declining deference linked to length of time as a GP l Traditionalists all been GPs for 20+ years - in late 40 s/50 s l Egalitarians been GPs for less than 10 yrs - all in 30 s
The role of Time l GPs feelings about declining deference linked to length of time as a GP l Traditionalists all been GPs for 20+ years - in late 40 s/50 s l Egalitarians been GPs for less than 10 yrs - all in 30 s
 Pragmatist GPs l l l Combined elements of Traditionalism & Egalitarianism Uncomfortable if patients totally trusting Don’t want to be `put on a pedestal’ BUT Aware of more complaints/more demanding patients
Pragmatist GPs l l l Combined elements of Traditionalism & Egalitarianism Uncomfortable if patients totally trusting Don’t want to be `put on a pedestal’ BUT Aware of more complaints/more demanding patients
 World Views and perception of violence l l l Majority talked about deviant patients as most violent, whatever world view Same as survey Traditionalists also identified Social Background
World Views and perception of violence l l l Majority talked about deviant patients as most violent, whatever world view Same as survey Traditionalists also identified Social Background
 Problem patients – drugs and alcohol (regardless of world view) `Drug addiction and the constant nuisance, I would say, when they demand (drugs cause the most problems). We have to be very strict. Drugs like temazepam, which is a huge drug of abuse. . Oh (and) alcoholics. . They come and demand something and the girls (receptionists) can’t cope and they won’t leave the premises, they’re drunk. It’s usually the case of the local winos. They want to be seen now, and they have got a bad toe or a bad foot. . ’ (252, female GP, aged 55)
Problem patients – drugs and alcohol (regardless of world view) `Drug addiction and the constant nuisance, I would say, when they demand (drugs cause the most problems). We have to be very strict. Drugs like temazepam, which is a huge drug of abuse. . Oh (and) alcoholics. . They come and demand something and the girls (receptionists) can’t cope and they won’t leave the premises, they’re drunk. It’s usually the case of the local winos. They want to be seen now, and they have got a bad toe or a bad foot. . ’ (252, female GP, aged 55)
 Problem patients – working class patients (Traditionalists) `There’s no doubt that patients who live in what you might loosely call council estates, the less well off patients or disadvantaged patients, whatever you want to call them, social class four, five, they often. . They seem to have a lower threshold for becoming violent somehow. I don’t know whether it is lack of education, whether they don’t understand the system. I don’t know but they would be the first ones to fly off the handle and get agitated with you. Not always, tends to be. They are often unemployed, unmarried mothers or unmarried mothers’ boyfriends. . (3382, male GP, aged 47)
Problem patients – working class patients (Traditionalists) `There’s no doubt that patients who live in what you might loosely call council estates, the less well off patients or disadvantaged patients, whatever you want to call them, social class four, five, they often. . They seem to have a lower threshold for becoming violent somehow. I don’t know whether it is lack of education, whether they don’t understand the system. I don’t know but they would be the first ones to fly off the handle and get agitated with you. Not always, tends to be. They are often unemployed, unmarried mothers or unmarried mothers’ boyfriends. . (3382, male GP, aged 47)
 Problem patients – negotiate with them (Egalitarian World View) l l Only egalitarians said need to understand WHY patients violent See it from patient’s standpoint Put aside own ego as doctor Negotiate with them
Problem patients – negotiate with them (Egalitarian World View) l l Only egalitarians said need to understand WHY patients violent See it from patient’s standpoint Put aside own ego as doctor Negotiate with them
 Understanding violence – the egalitarian ethos `(I’ve had) people saying they will do certain things if you don’t do certain things for them. And basically people will say “Well, if you don’t do this I am going to sue you, and I’ve got problems”. But again it’s a case of negotiating with them I think. You know I’m sure a lot of threats are made because they are afraid of something. They have something they want to get out of it and they’re afraid they’re not going to get it. And it’s very difficult to get out of them what the problem is. . I think the reason why you get violence is because there are two egos. If there’s only one ego there’s never any violence. . ’ (1430, male GP, aged 40)
Understanding violence – the egalitarian ethos `(I’ve had) people saying they will do certain things if you don’t do certain things for them. And basically people will say “Well, if you don’t do this I am going to sue you, and I’ve got problems”. But again it’s a case of negotiating with them I think. You know I’m sure a lot of threats are made because they are afraid of something. They have something they want to get out of it and they’re afraid they’re not going to get it. And it’s very difficult to get out of them what the problem is. . I think the reason why you get violence is because there are two egos. If there’s only one ego there’s never any violence. . ’ (1430, male GP, aged 40)
 Conclusion (1) – Quantitative Data l l l Violence a problem for Young/Inner City GPs Young GPs also more fearful, especially if experienced violence GPs – young & old – feel loss of authority Young GPs feel loss of status, regardless of whether experienced violence Older GPs more aware of loss of status if witnessed violence Deviant patients rather than demanding patients seen as most dangerous
Conclusion (1) – Quantitative Data l l l Violence a problem for Young/Inner City GPs Young GPs also more fearful, especially if experienced violence GPs – young & old – feel loss of authority Young GPs feel loss of status, regardless of whether experienced violence Older GPs more aware of loss of status if witnessed violence Deviant patients rather than demanding patients seen as most dangerous
 Conclusion (2) – Qualitative Data l l Confirm much of picture of Survey data BUT refines it. CONFIRMS – general sense of Loss of Authority + Deviant patients most problematic REFINES - Age/length of time in practice NOT related to views about Deference/Violence in Simple Way Need to take account of GP WORLD VIEW - influences HOW see decline in authority/violence Egalitarians’ views quite different to Traditionalists - Egalitarians – younger/in practice less time/inner city Traditionalists – older/practice longer/suburbs - Pragmatists – welcome less deference but see the problems that follow – mixed re Age/Experience/Location l
Conclusion (2) – Qualitative Data l l Confirm much of picture of Survey data BUT refines it. CONFIRMS – general sense of Loss of Authority + Deviant patients most problematic REFINES - Age/length of time in practice NOT related to views about Deference/Violence in Simple Way Need to take account of GP WORLD VIEW - influences HOW see decline in authority/violence Egalitarians’ views quite different to Traditionalists - Egalitarians – younger/in practice less time/inner city Traditionalists – older/practice longer/suburbs - Pragmatists – welcome less deference but see the problems that follow – mixed re Age/Experience/Location l
 Conclusion (3) Implications for Decline in Trust l l l Survey data – trust declining – esp Young & Old GPs Interview data – many GPs questioned passive trust as desirable – pro active trust/informed trust. Some support for deference from Traditionalists – trained when Doctor’s authority unchallenged. Violence – significant for younger GPs – not because of less deference BUT from Deviant Patients General Practice changing - less deference/more violence but NO clear cut association between them
Conclusion (3) Implications for Decline in Trust l l l Survey data – trust declining – esp Young & Old GPs Interview data – many GPs questioned passive trust as desirable – pro active trust/informed trust. Some support for deference from Traditionalists – trained when Doctor’s authority unchallenged. Violence – significant for younger GPs – not because of less deference BUT from Deviant Patients General Practice changing - less deference/more violence but NO clear cut association between them
 A Caveat l l Danger of focusing on - ONE form of Trust – Interpersonal - Micro Level – Doctor/Patient Macro Level – Trust in Institution/System – also crucial - Relations between Doctors & state GPs/other Professionals GPs/patients collectively
A Caveat l l Danger of focusing on - ONE form of Trust – Interpersonal - Micro Level – Doctor/Patient Macro Level – Trust in Institution/System – also crucial - Relations between Doctors & state GPs/other Professionals GPs/patients collectively
 References l l l Calnan, M. and Rowe, R. (2008) Trust Matters in Health Care. Open University Press, Maidenhead. Gabe, J. and Elston, M. (2008) We don’t have to take this’: Zero tolerance of violence against health care workers in a time of insecurity. Social Policy & Administration 42: 691 -709. Elston, M. Gabe J. et al (2002) Violence against doctors: a medicalised problem? Sociology of Health & Illness 24: 575 -98. Haug, M. (1988) A re-examination of the hypothesis of deprofessionalisation. The Milbank Quarterly, 66, Supplement 2: 4856. Mc. Kinlay, J. and Marceau, L. (2003) The end of the golden age of doctoring. International Journal of Health Services 32: 379 -416. Upson, A. (2004) Violence at Work: Findings from the 2002/3 British Crime Survey. Home Office, London.
References l l l Calnan, M. and Rowe, R. (2008) Trust Matters in Health Care. Open University Press, Maidenhead. Gabe, J. and Elston, M. (2008) We don’t have to take this’: Zero tolerance of violence against health care workers in a time of insecurity. Social Policy & Administration 42: 691 -709. Elston, M. Gabe J. et al (2002) Violence against doctors: a medicalised problem? Sociology of Health & Illness 24: 575 -98. Haug, M. (1988) A re-examination of the hypothesis of deprofessionalisation. The Milbank Quarterly, 66, Supplement 2: 4856. Mc. Kinlay, J. and Marceau, L. (2003) The end of the golden age of doctoring. International Journal of Health Services 32: 379 -416. Upson, A. (2004) Violence at Work: Findings from the 2002/3 British Crime Survey. Home Office, London.


