beb11cf9448740bc0ccbf01b9fa32154.ppt
- Количество слайдов: 30
 Ventilator-Associated Pneumonia (VAP) An Overview for RC Students Special thanks to: Donald Dumford Beth Israel Deaconess Medical Center CDC
Ventilator-Associated Pneumonia (VAP) An Overview for RC Students Special thanks to: Donald Dumford Beth Israel Deaconess Medical Center CDC
 General Overview of Medical Protocols n n n Morbidity, mortality and cost associated with VAP Who gets VAP? Risk factors that increase likelihood of developing VAP Etiology: The bugs Treatment: The drugs How VAP develops (Pathogenesis) Measures to prevent VAP
General Overview of Medical Protocols n n n Morbidity, mortality and cost associated with VAP Who gets VAP? Risk factors that increase likelihood of developing VAP Etiology: The bugs Treatment: The drugs How VAP develops (Pathogenesis) Measures to prevent VAP
 General Care & Nursing Objectives n n Review policy and procedural practice changes for VAP prevention Discuss BIDMC practice changes related to: n n n Hand Hygiene Oral Care HOB elevation Suctioning Vent Circuits
General Care & Nursing Objectives n n Review policy and procedural practice changes for VAP prevention Discuss BIDMC practice changes related to: n n n Hand Hygiene Oral Care HOB elevation Suctioning Vent Circuits
 Who is at Greatest Risk? n n n Reintubation Supine position Impaired cough/depressed LOC Oropharyngeal colonization Presence of NG/OG tubes and enteral feeding Cross contamination by staff
Who is at Greatest Risk? n n n Reintubation Supine position Impaired cough/depressed LOC Oropharyngeal colonization Presence of NG/OG tubes and enteral feeding Cross contamination by staff
 Definition- “Know thy enemy” Pneumonia that develops in someone who has been intubated -Typically in studies, patients are only included if intubated greater than 48 hours -Early onset= less than 4 days -Late onset= greater than 4 days Endotracheal intubation increases risk of developing pneumonia by 6 to 21 fold Accounts for 90% of infections in mechanically ventilated patients American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia.
Definition- “Know thy enemy” Pneumonia that develops in someone who has been intubated -Typically in studies, patients are only included if intubated greater than 48 hours -Early onset= less than 4 days -Late onset= greater than 4 days Endotracheal intubation increases risk of developing pneumonia by 6 to 21 fold Accounts for 90% of infections in mechanically ventilated patients American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia.
 Why Do We Care? n n Hospital acquired pneumonia (HAP) is the second most common hospital infection VAP is the most common intensive care unit (ICU) infection VAP occurs in 10 - 65% of all ventilated patients Crit Care Clin (2002) VAP is one of critical care’s quality initiatives which can improve patient outcomes
Why Do We Care? n n Hospital acquired pneumonia (HAP) is the second most common hospital infection VAP is the most common intensive care unit (ICU) infection VAP occurs in 10 - 65% of all ventilated patients Crit Care Clin (2002) VAP is one of critical care’s quality initiatives which can improve patient outcomes
 $$$$ n VAP increases: Medical costs n Ventilator days n ICU and hospital LOS n n Estimated direct cost of excess hospital stay due to VAP is $40, 000 per patient Chest (2002)
$$$$ n VAP increases: Medical costs n Ventilator days n ICU and hospital LOS n n Estimated direct cost of excess hospital stay due to VAP is $40, 000 per patient Chest (2002)
 Length of stay and cost n n n Remember that Medicare is no longer reimbursing for nosocomial infections VAP increased length of stay in the ICU by 5 -7 days (mean of 6. 1 days)1, 2 Increase in cost n Increase of $10, 000 -$40, 000 per patient 1, 2 Safdar N et al. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review 2 Rello et al. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database 1
Length of stay and cost n n n Remember that Medicare is no longer reimbursing for nosocomial infections VAP increased length of stay in the ICU by 5 -7 days (mean of 6. 1 days)1, 2 Increase in cost n Increase of $10, 000 -$40, 000 per patient 1, 2 Safdar N et al. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review 2 Rello et al. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database 1
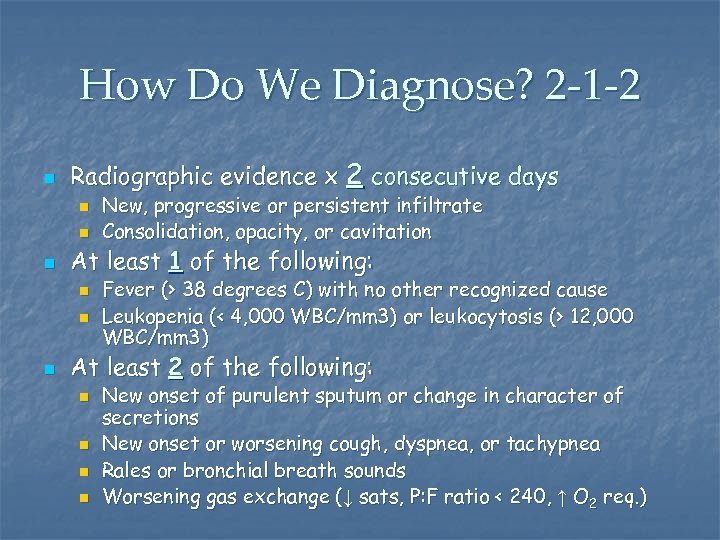 How Do We Diagnose? 2 -1 -2 n Radiographic evidence x 2 consecutive days n n n At least 1 of the following: n n n New, progressive or persistent infiltrate Consolidation, opacity, or cavitation Fever (> 38 degrees C) with no other recognized cause Leukopenia (< 4, 000 WBC/mm 3) or leukocytosis (> 12, 000 WBC/mm 3) At least 2 of the following: n n New onset of purulent sputum or change in character of secretions New onset or worsening cough, dyspnea, or tachypnea Rales or bronchial breath sounds Worsening gas exchange (↓ sats, P: F ratio < 240, ↑ O 2 req. )
How Do We Diagnose? 2 -1 -2 n Radiographic evidence x 2 consecutive days n n n At least 1 of the following: n n n New, progressive or persistent infiltrate Consolidation, opacity, or cavitation Fever (> 38 degrees C) with no other recognized cause Leukopenia (< 4, 000 WBC/mm 3) or leukocytosis (> 12, 000 WBC/mm 3) At least 2 of the following: n n New onset of purulent sputum or change in character of secretions New onset or worsening cough, dyspnea, or tachypnea Rales or bronchial breath sounds Worsening gas exchange (↓ sats, P: F ratio < 240, ↑ O 2 req. )
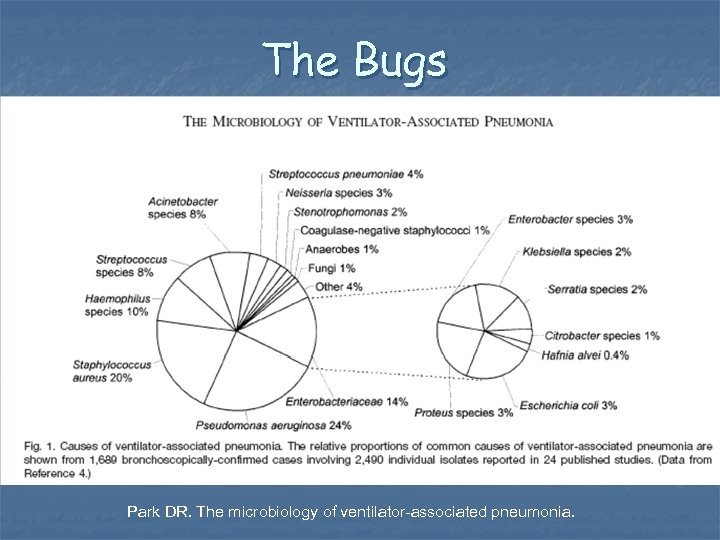 The Bugs n Figure 1 from Park DR. The microbiology of ventilator-associated pneumonia.
The Bugs n Figure 1 from Park DR. The microbiology of ventilator-associated pneumonia.
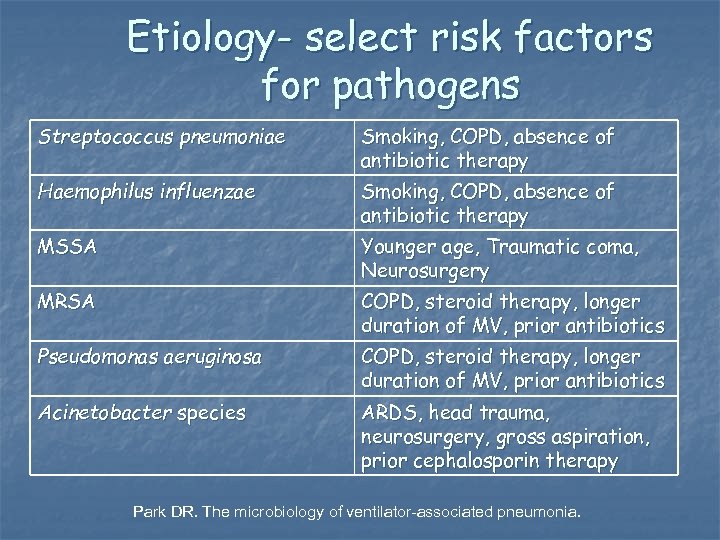 Etiology- select risk factors for pathogens Streptococcus pneumoniae Smoking, COPD, absence of antibiotic therapy Haemophilus influenzae Smoking, COPD, absence of antibiotic therapy MSSA Younger age, Traumatic coma, Neurosurgery MRSA COPD, steroid therapy, longer duration of MV, prior antibiotics Pseudomonas aeruginosa COPD, steroid therapy, longer duration of MV, prior antibiotics Acinetobacter species ARDS, head trauma, neurosurgery, gross aspiration, prior cephalosporin therapy Park DR. The microbiology of ventilator-associated pneumonia.
Etiology- select risk factors for pathogens Streptococcus pneumoniae Smoking, COPD, absence of antibiotic therapy Haemophilus influenzae Smoking, COPD, absence of antibiotic therapy MSSA Younger age, Traumatic coma, Neurosurgery MRSA COPD, steroid therapy, longer duration of MV, prior antibiotics Pseudomonas aeruginosa COPD, steroid therapy, longer duration of MV, prior antibiotics Acinetobacter species ARDS, head trauma, neurosurgery, gross aspiration, prior cephalosporin therapy Park DR. The microbiology of ventilator-associated pneumonia.
 What Are Our Practice Goals? n n n Hand Hygiene Mouth care Q 2 -4 hours HOB > 30 degrees unless contraindicated Closed inline suction – saline only when needed Change vent circuits only when needed
What Are Our Practice Goals? n n n Hand Hygiene Mouth care Q 2 -4 hours HOB > 30 degrees unless contraindicated Closed inline suction – saline only when needed Change vent circuits only when needed
 Hand Hygiene n n Hand hygiene is the single most important (and easiest!!!) method for reducing the transmission of pathogens. Waterless antiseptic preparations are more effective than soap and water and may increase compliance.
Hand Hygiene n n Hand hygiene is the single most important (and easiest!!!) method for reducing the transmission of pathogens. Waterless antiseptic preparations are more effective than soap and water and may increase compliance.
 Oral Care n n Daily inspection and assessment of oral cavity Brush teeth q 12 hours Swab mouth with antiseptic agent q 2 -4 hours between brushing Moisturize mouth prn
Oral Care n n Daily inspection and assessment of oral cavity Brush teeth q 12 hours Swab mouth with antiseptic agent q 2 -4 hours between brushing Moisturize mouth prn
 HOB > 30 Degrees n n HOB > 30 degrees at all times including transport unless contraindicated. Aspiration of oral secretions is a presumed step in the development of VAP Pulmonary aspiration is increased by supine positioning Positioning the HOB to 30 degrees or higher significantly reduces gastric reflux and VAP
HOB > 30 Degrees n n HOB > 30 degrees at all times including transport unless contraindicated. Aspiration of oral secretions is a presumed step in the development of VAP Pulmonary aspiration is increased by supine positioning Positioning the HOB to 30 degrees or higher significantly reduces gastric reflux and VAP
 Stryker beds display Fowler angle at foot of bed Keep patient at 30 -45 degrees while intubated
Stryker beds display Fowler angle at foot of bed Keep patient at 30 -45 degrees while intubated
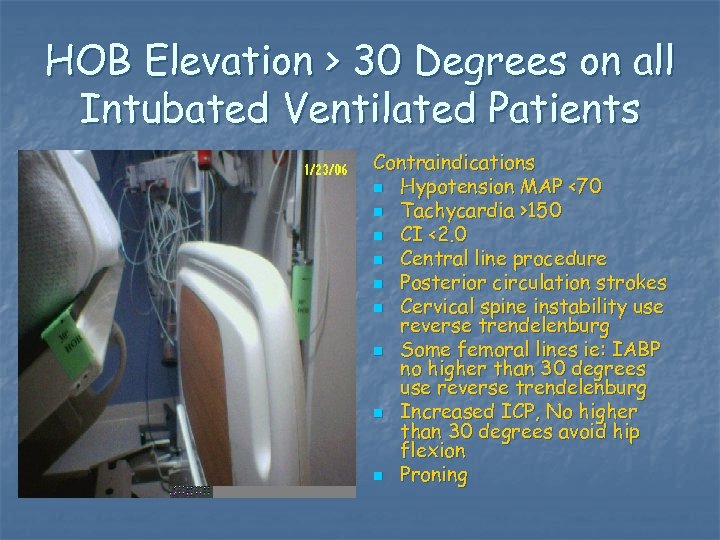 HOB Elevation > 30 Degrees on all Intubated Ventilated Patients Contraindications n Hypotension MAP <70 n Tachycardia >150 n CI <2. 0 n Central line procedure n Posterior circulation strokes n Cervical spine instability use reverse trendelenburg n Some femoral lines ie: IABP no higher than 30 degrees use reverse trendelenburg n Increased ICP, No higher than 30 degrees avoid hip flexion n Proning
HOB Elevation > 30 Degrees on all Intubated Ventilated Patients Contraindications n Hypotension MAP <70 n Tachycardia >150 n CI <2. 0 n Central line procedure n Posterior circulation strokes n Cervical spine instability use reverse trendelenburg n Some femoral lines ie: IABP no higher than 30 degrees use reverse trendelenburg n Increased ICP, No higher than 30 degrees avoid hip flexion n Proning
 Reverse Trendelenburg n n n In full reverse Trendelenburg the foot of bed will read -12 degrees. Angle of head elevation is approximately 20 degrees not 30 degrees when at -12. Evaluate the individual clinical situation to assess if the patient can tolerate the addition of a small amount of Fowlers angle which may flex the hip.
Reverse Trendelenburg n n n In full reverse Trendelenburg the foot of bed will read -12 degrees. Angle of head elevation is approximately 20 degrees not 30 degrees when at -12. Evaluate the individual clinical situation to assess if the patient can tolerate the addition of a small amount of Fowlers angle which may flex the hip.
 Suctioning n In line suction: n n n Maintain closed system Use separate suction tubing for inline & yankauer Normal saline: n n n Should not be routinely used to suction pts Causes desaturation Does not increase removal of secretions Can potentially dislodge bacteria Should be used to rinse the suction catheter after suctioning
Suctioning n In line suction: n n n Maintain closed system Use separate suction tubing for inline & yankauer Normal saline: n n n Should not be routinely used to suction pts Causes desaturation Does not increase removal of secretions Can potentially dislodge bacteria Should be used to rinse the suction catheter after suctioning
 Subglottal Suctioning n Should be done using a 14 Fr sterile suction catheter: Prior to ETT rotation n Prior to lying patient supine n Prior to extubation n
Subglottal Suctioning n Should be done using a 14 Fr sterile suction catheter: Prior to ETT rotation n Prior to lying patient supine n Prior to extubation n
 Suctioning n Yankauer: § Use separate suction tubing § Change q 24 hours – unless visibly soiled date and time when changed § Clean after each use with NS or sterile H 2 O § Wipe with clean 4 X 4 gauze, place in package § Store in original package, taped to vent
Suctioning n Yankauer: § Use separate suction tubing § Change q 24 hours – unless visibly soiled date and time when changed § Clean after each use with NS or sterile H 2 O § Wipe with clean 4 X 4 gauze, place in package § Store in original package, taped to vent
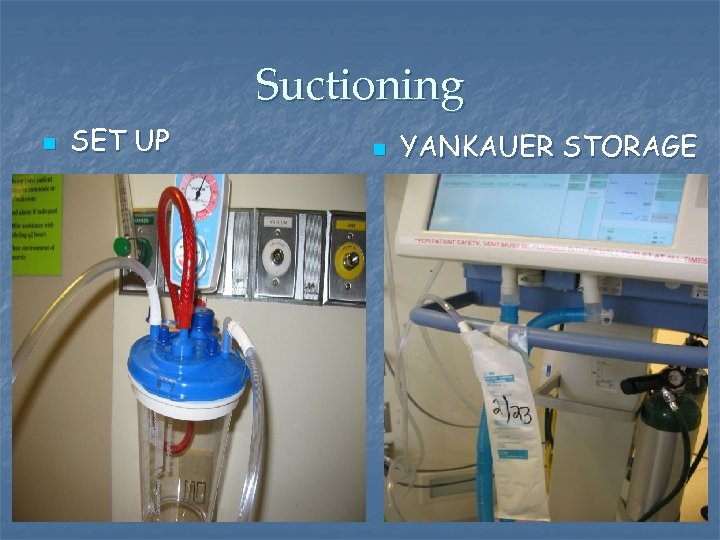 Suctioning n SET UP n YANKAUER STORAGE
Suctioning n SET UP n YANKAUER STORAGE
 Pathogenesis- Through the tube 1) 2) Condensate in tubing Development of ETT biofilm
Pathogenesis- Through the tube 1) 2) Condensate in tubing Development of ETT biofilm
 Condensate n n Condensate in ventilator tubing becomes rapidly contaminated with bacteria from patient’s oropharynx Craven et al showed that 33% of inspiratory circuits were colonized within 2 hours and 80% within 24 hours
Condensate n n Condensate in ventilator tubing becomes rapidly contaminated with bacteria from patient’s oropharynx Craven et al showed that 33% of inspiratory circuits were colonized within 2 hours and 80% within 24 hours
 ET tube biofilm (RT’s should know this…) n Exopolysaccharide outer layer with quiescent bacteria within n n Difficult for bacteria to penetrate outer layer and bacteria within resistant to bactericidal effects of bacteria Adair et al study n “Microorganisms of high pathogenic potential were isolated from all ETs collected from patients with VAP compared with 30% of ETs from the control group. ”
ET tube biofilm (RT’s should know this…) n Exopolysaccharide outer layer with quiescent bacteria within n n Difficult for bacteria to penetrate outer layer and bacteria within resistant to bactericidal effects of bacteria Adair et al study n “Microorganisms of high pathogenic potential were isolated from all ETs collected from patients with VAP compared with 30% of ETs from the control group. ”
 Around the tube 1) 2) 3) 4) Oral decontamination and selective decontamination of the digestive tract Aspiraton of subglottic secretions including continuous aspiration of subglottic secretions Semi-recumbent positioning Sucralfate for stress ulcer prophylaxis
Around the tube 1) 2) 3) 4) Oral decontamination and selective decontamination of the digestive tract Aspiraton of subglottic secretions including continuous aspiration of subglottic secretions Semi-recumbent positioning Sucralfate for stress ulcer prophylaxis
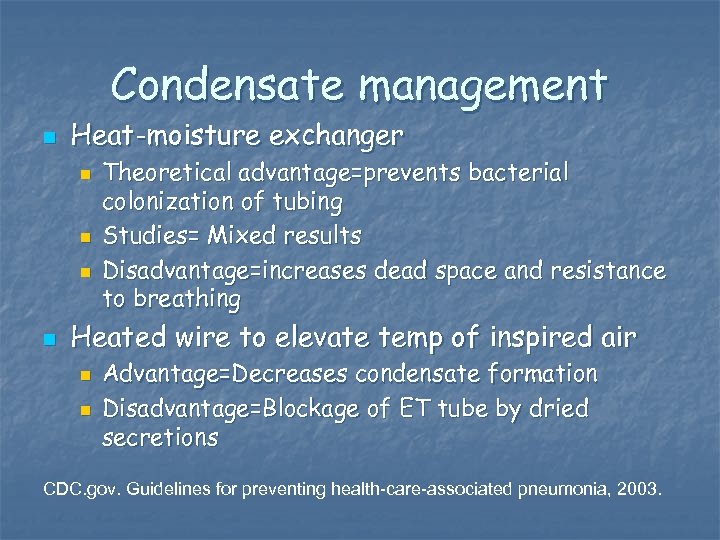 Condensate management n Heat-moisture exchanger n n Theoretical advantage=prevents bacterial colonization of tubing Studies= Mixed results Disadvantage=increases dead space and resistance to breathing Heated wire to elevate temp of inspired air n n Advantage=Decreases condensate formation Disadvantage=Blockage of ET tube by dried secretions CDC. gov. Guidelines for preventing health-care-associated pneumonia, 2003.
Condensate management n Heat-moisture exchanger n n Theoretical advantage=prevents bacterial colonization of tubing Studies= Mixed results Disadvantage=increases dead space and resistance to breathing Heated wire to elevate temp of inspired air n n Advantage=Decreases condensate formation Disadvantage=Blockage of ET tube by dried secretions CDC. gov. Guidelines for preventing health-care-associated pneumonia, 2003.
 Ventilator Circuits n Vent circuits (including inline suction systems) will be in place for the duration of ventilation unless: Defective n Damaged n Visibly soiled n The humidification system requires changing n
Ventilator Circuits n Vent circuits (including inline suction systems) will be in place for the duration of ventilation unless: Defective n Damaged n Visibly soiled n The humidification system requires changing n
 What Is Next? n Standardization of oral care n n Sedation n n Products being trialed Improve practice regarding weaning sedation and daily wake up Vent weaning n Improve practice around weaning and extubation
What Is Next? n Standardization of oral care n n Sedation n n Products being trialed Improve practice regarding weaning sedation and daily wake up Vent weaning n Improve practice around weaning and extubation
 Stay Tuned… n More to come!
Stay Tuned… n More to come!


