1bbd7d8e9e548ed73802c1fc53af7c3e.ppt
- Количество слайдов: 33
Venous Thromboembolism in Pediatrics Shalu Narang, M. D. Pediatric Hematology Newark Beth Israel Medical Center
Objectives • Epidemiology and pathophysiology of pediatric thrombotic disorders • Signs, symptoms and diagnosis of deep venous thrombosis (DVT) • Acquired vs. inherited thrombophilia • Diagnostic screening tests for thrombotic disorders • Role of anticoagulation in children with thrombotic disorders • Long-term sequelae of thrombosis
Epidemiology
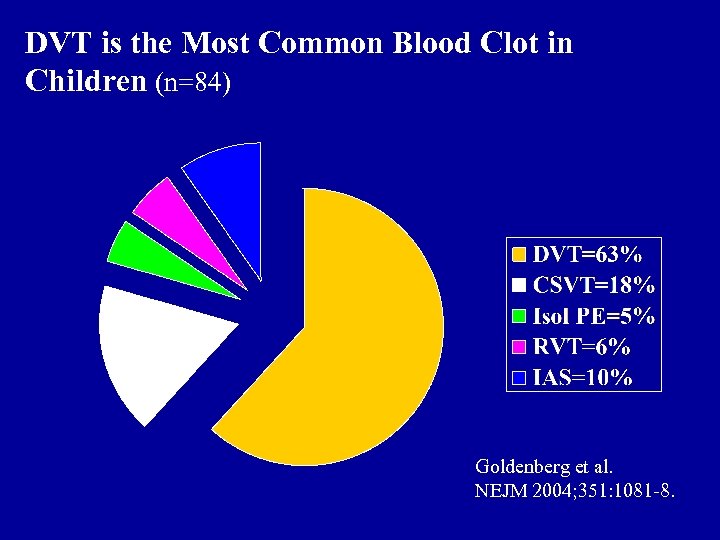
DVT is the Most Common Blood Clot in Children (n=84) Goldenberg et al. NEJM 2004; 351: 1081 -8.
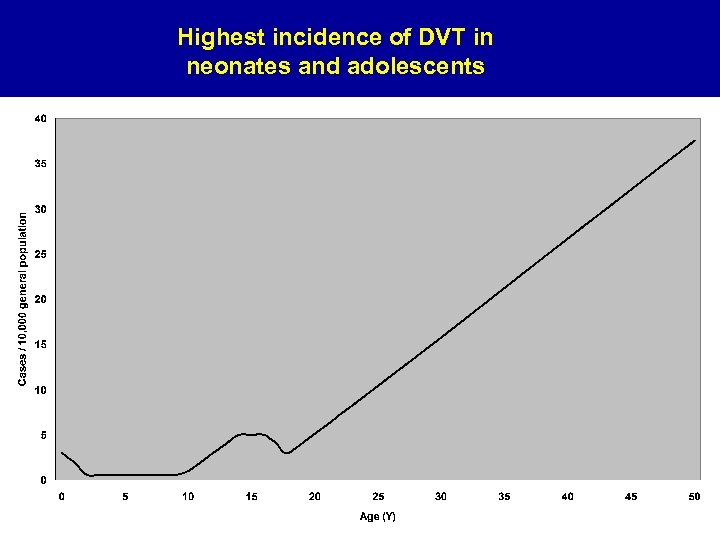
Highest incidence of DVT in neonates and adolescents
Pathophysiology
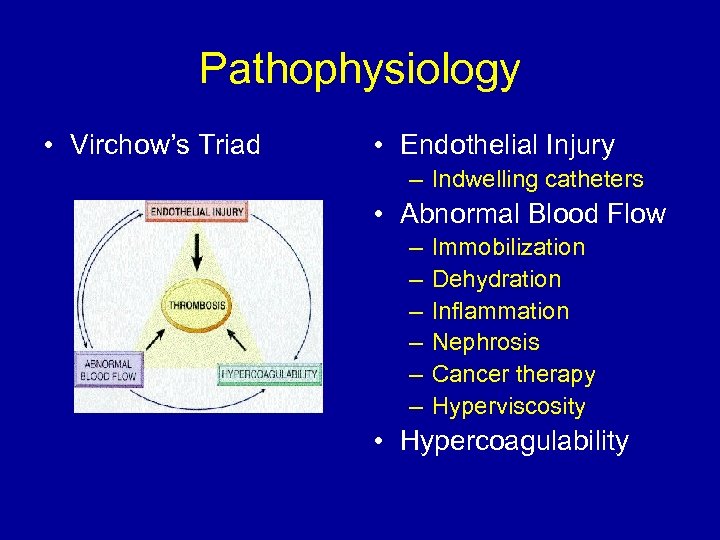
Pathophysiology • Virchow’s Triad • Endothelial Injury – Indwelling catheters • Abnormal Blood Flow – – – Immobilization Dehydration Inflammation Nephrosis Cancer therapy Hyperviscosity • Hypercoagulability
Conceptual Model of Hemostasis Reprinted with permission from Sidney Harris.
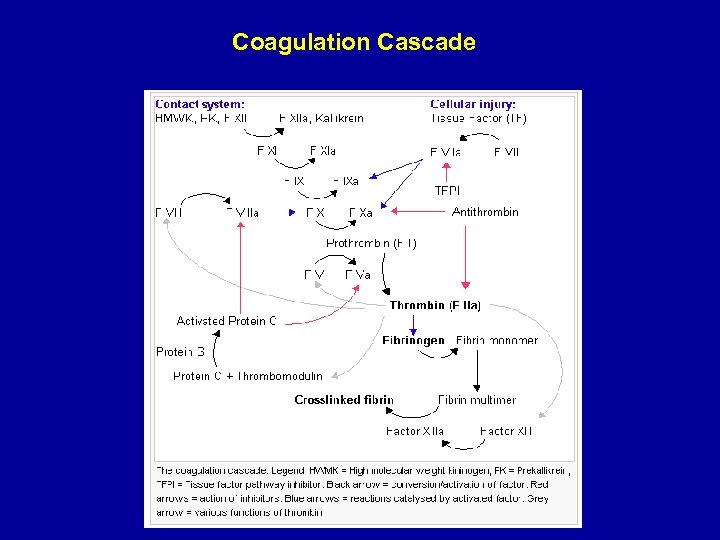
Coagulation Cascade
Pathophysiology Fibrinolysis Coagulation Hemostasis
Pathophysiology Coagulation ↓ Thrombosis Hemostasis Fibrinolysis
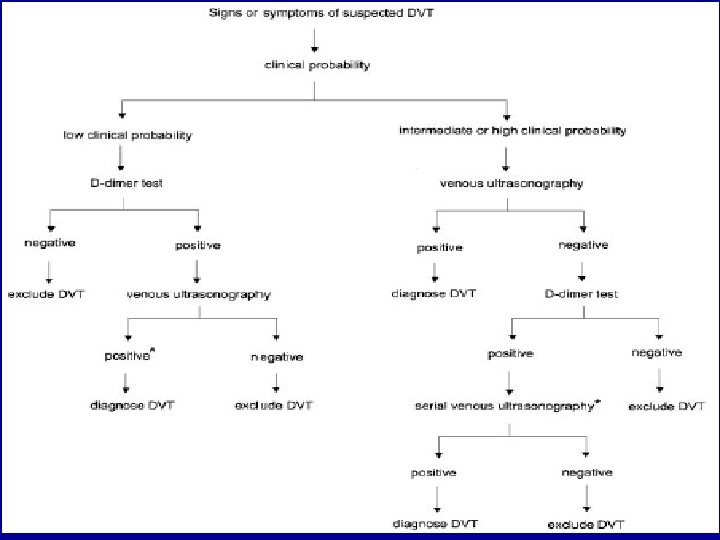
Signs, Symptoms and Diagnosis

Signs & Symptoms • DVT: – Poorly Functioning Catheters – Edematous extremity – Plethoric extremity – Warm extremity – Painful extremity • PE: – Cough, SOB, Hemoptysis – Tachycardia

Risk Factors • • • Indwelling catheters Thrombophilia Malignancy Chemotherapy Prosthetic cardiac valves Diabetes mellitus Sickle cell anemia Infection Surgery
Thrombophilia
Thrombophilia • Inherited: – – – Protein C deficiency Protein S deficiency Antithrombin deficiency Factor V leiden Prothrombin gene mutation Elevated Lipoprotein a, homocysteine • Acuired: – Antiphospholipid Syndrome – Nephrotic syndrome
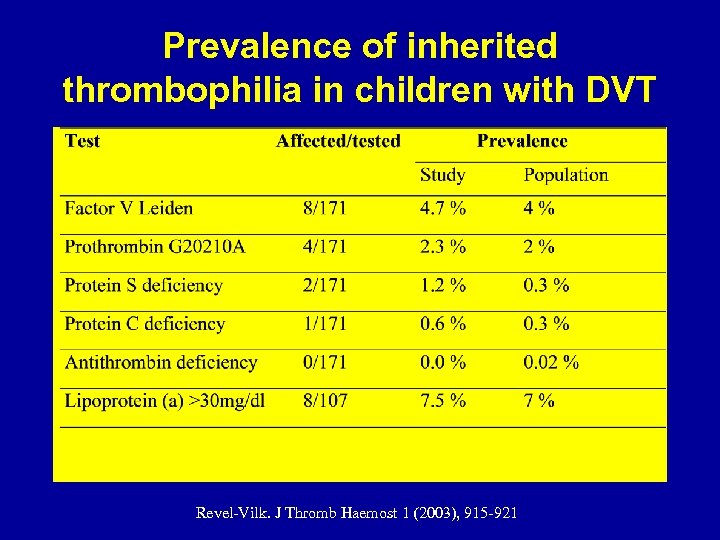
Prevalence of inherited thrombophilia in children with DVT Revel-Vilk. J Thromb Haemost 1 (2003), 915 -921
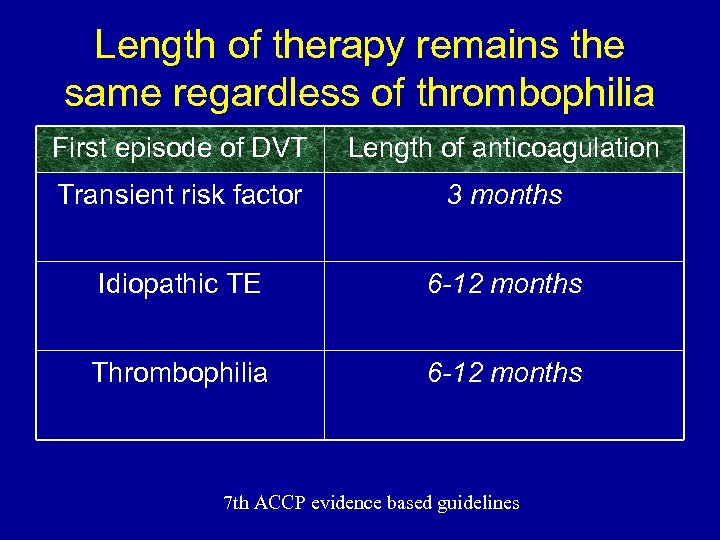
Length of therapy remains the same regardless of thrombophilia First episode of DVT Length of anticoagulation Transient risk factor 3 months Idiopathic TE 6 -12 months Thrombophilia 6 -12 months 7 th ACCP evidence based guidelines
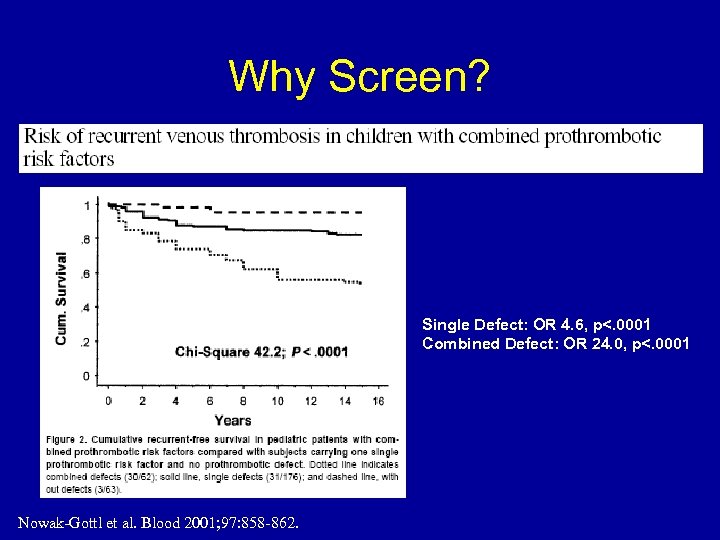
Why Screen? Single Defect: OR 4. 6, p<. 0001 Combined Defect: OR 24. 0, p<. 0001 Nowak-Gottl et al. Blood 2001; 97: 858 -862.
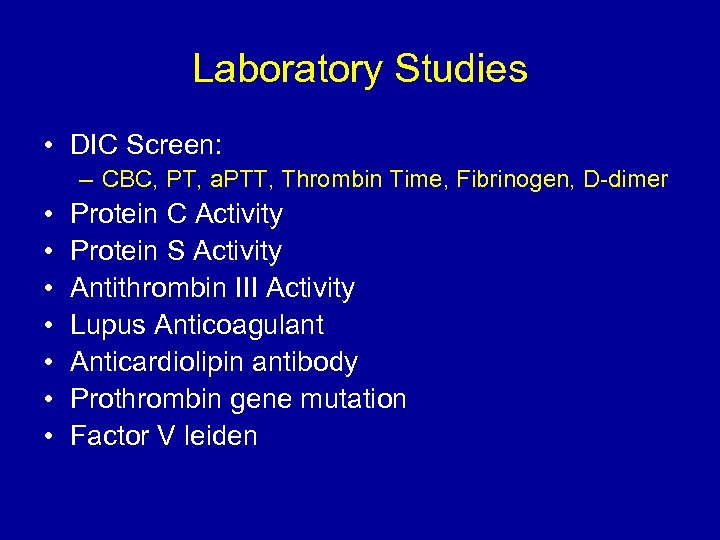
Laboratory Studies • DIC Screen: – CBC, PT, a. PTT, Thrombin Time, Fibrinogen, D-dimer • • Protein C Activity Protein S Activity Antithrombin III Activity Lupus Anticoagulant Anticardiolipin antibody Prothrombin gene mutation Factor V leiden
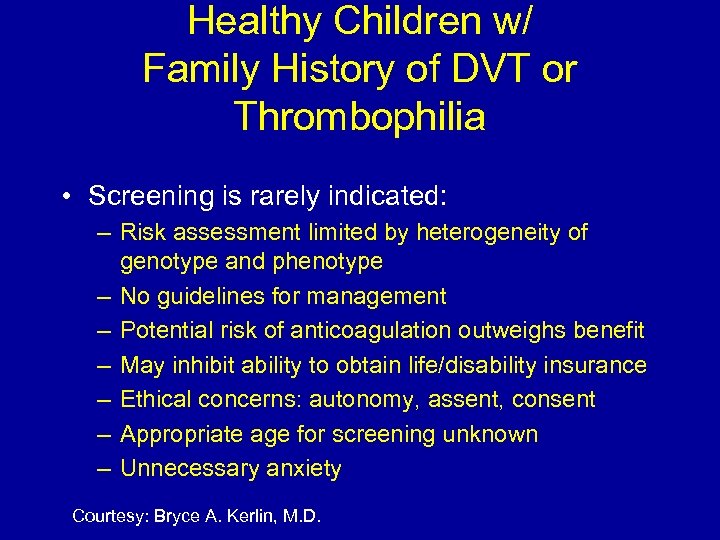
Healthy Children w/ Family History of DVT or Thrombophilia • Screening is rarely indicated: – Risk assessment limited by heterogeneity of genotype and phenotype – No guidelines for management – Potential risk of anticoagulation outweighs benefit – May inhibit ability to obtain life/disability insurance – Ethical concerns: autonomy, assent, consent – Appropriate age for screening unknown – Unnecessary anxiety Courtesy: Bryce A. Kerlin, M. D.
Anticoagulation Therapy
Therapeutic Goals • Prevent thrombus propagation and/or embolization • Restore blood flow (rapidly, when necessary) • Minimize long-term sequelae
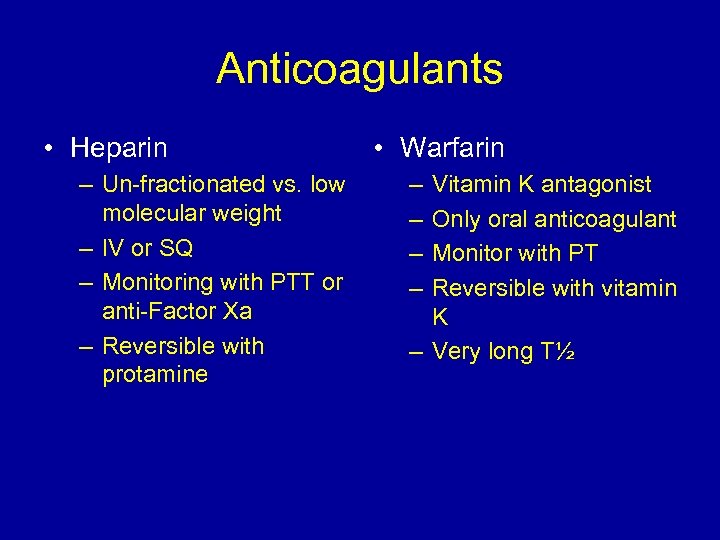
Anticoagulants • Heparin – Un-fractionated vs. low molecular weight – IV or SQ – Monitoring with PTT or anti-Factor Xa – Reversible with protamine • Warfarin – – Vitamin K antagonist Only oral anticoagulant Monitor with PT Reversible with vitamin K – Very long T½
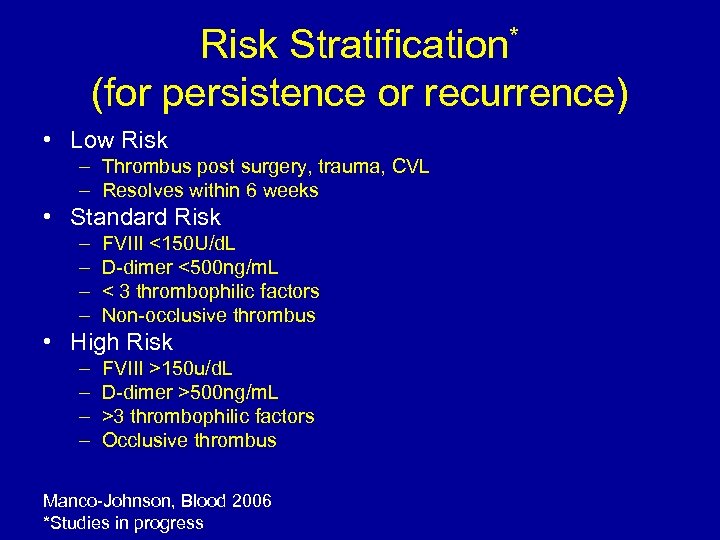
Risk Stratification* (for persistence or recurrence) • Low Risk – Thrombus post surgery, trauma, CVL – Resolves within 6 weeks • Standard Risk – – FVIII <150 U/d. L D-dimer <500 ng/m. L < 3 thrombophilic factors Non-occlusive thrombus • High Risk – – FVIII >150 u/d. L D-dimer >500 ng/m. L >3 thrombophilic factors Occlusive thrombus Manco-Johnson, Blood 2006 *Studies in progress
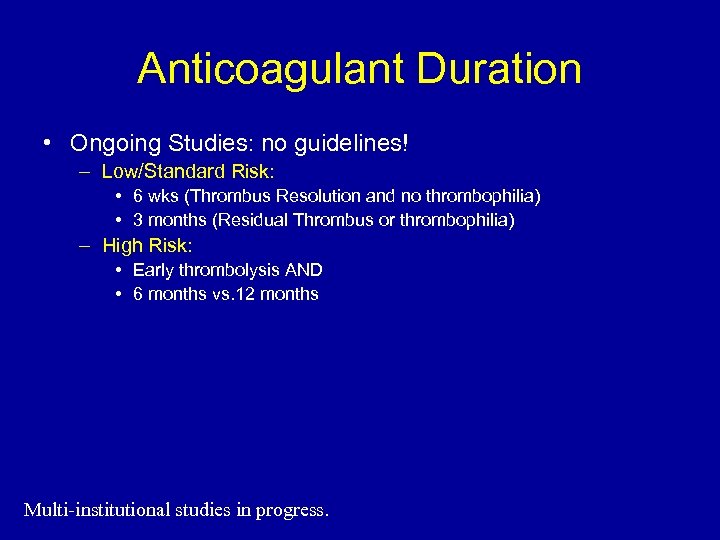
Anticoagulant Duration • Ongoing Studies: no guidelines! – Low/Standard Risk: • 6 wks (Thrombus Resolution and no thrombophilia) • 3 months (Residual Thrombus or thrombophilia) – High Risk: • Early thrombolysis AND • 6 months vs. 12 months Multi-institutional studies in progress.
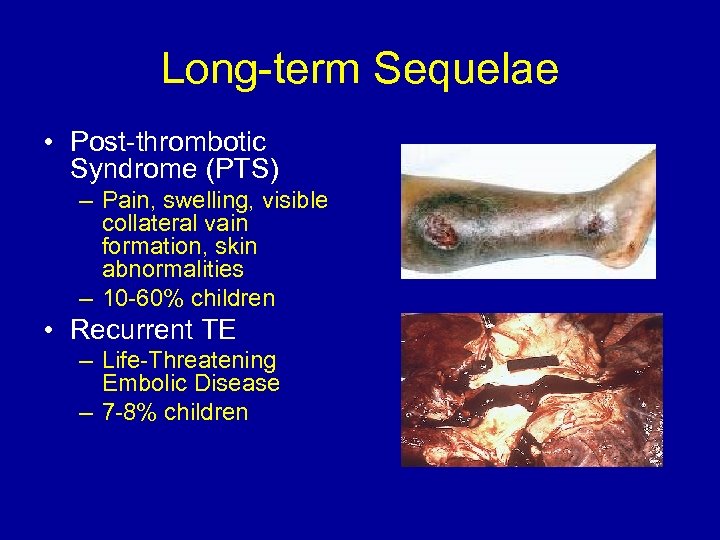
Long-term Sequelae • Post-thrombotic Syndrome (PTS) – Pain, swelling, visible collateral vain formation, skin abnormalities – 10 -60% children • Recurrent TE – Life-Threatening Embolic Disease – 7 -8% children
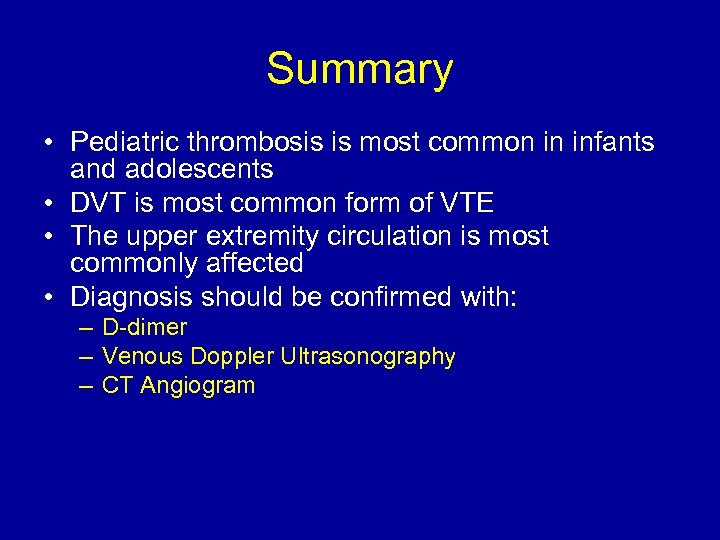
Summary • Pediatric thrombosis is most common in infants and adolescents • DVT is most common form of VTE • The upper extremity circulation is most commonly affected • Diagnosis should be confirmed with: – D-dimer – Venous Doppler Ultrasonography – CT Angiogram
Summary • Initial treatment should be standard or low molecular weight heparinization • Short courses may be completed with heparin, longer courses may benefit from transition to Warfarin • Duration of anticoagulant therapy is individualized based on underlying comorbidities • Patients should be followed closely for recurrent disease and/or post-phlebitic syndrome
Summary • All thrombosis patients should be screened for treatable molecular thrombophilias • Some patients may benefit from additional screening • Asymptomatic patients and family members not at increased risk for thrombosis should not routinely be screened
Thanks!
1bbd7d8e9e548ed73802c1fc53af7c3e.ppt