148fece1641c391fdbf6df1dbfa961a1.ppt
- Количество слайдов: 105
Vector-borne Infections Allison Liddell, M. D. Infectious Diseases September 22 nd, 2003
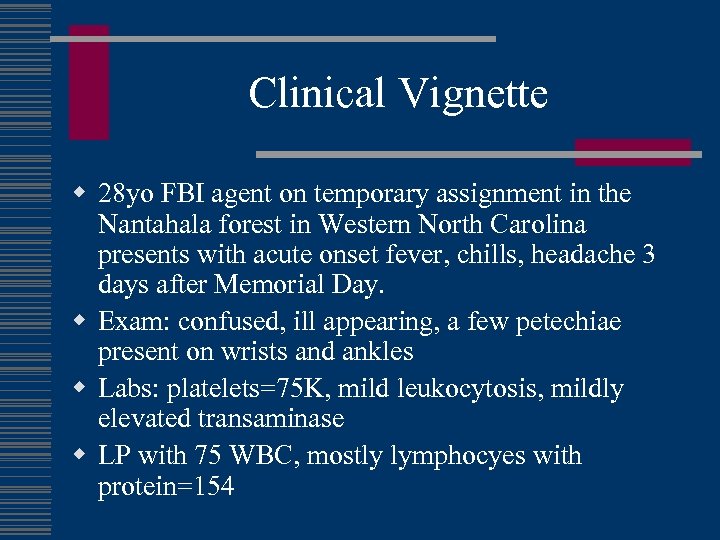
Clinical Vignette w 28 yo FBI agent on temporary assignment in the Nantahala forest in Western North Carolina presents with acute onset fever, chills, headache 3 days after Memorial Day. w Exam: confused, ill appearing, a few petechiae present on wrists and ankles w Labs: platelets=75 K, mild leukocytosis, mildly elevated transaminase w LP with 75 WBC, mostly lymphocyes with protein=154
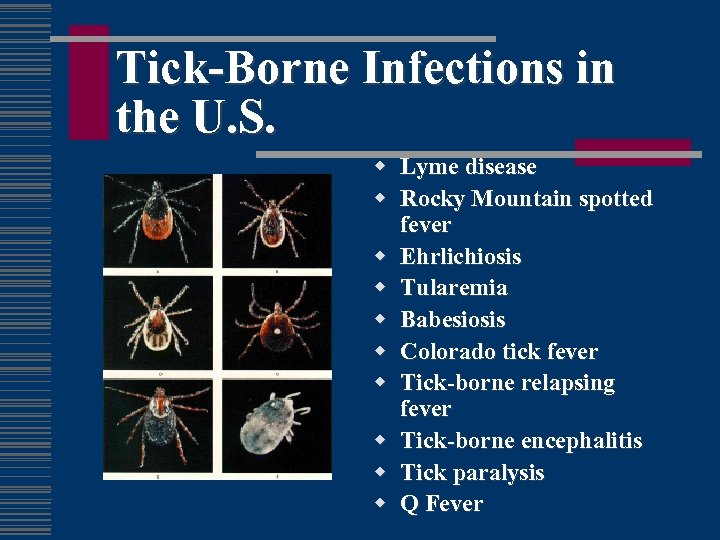
Tick-Borne Infections in the U. S. w Lyme disease w Rocky Mountain spotted fever w Ehrlichiosis w Tularemia w Babesiosis w Colorado tick fever w Tick-borne relapsing fever w Tick-borne encephalitis w Tick paralysis w Q Fever
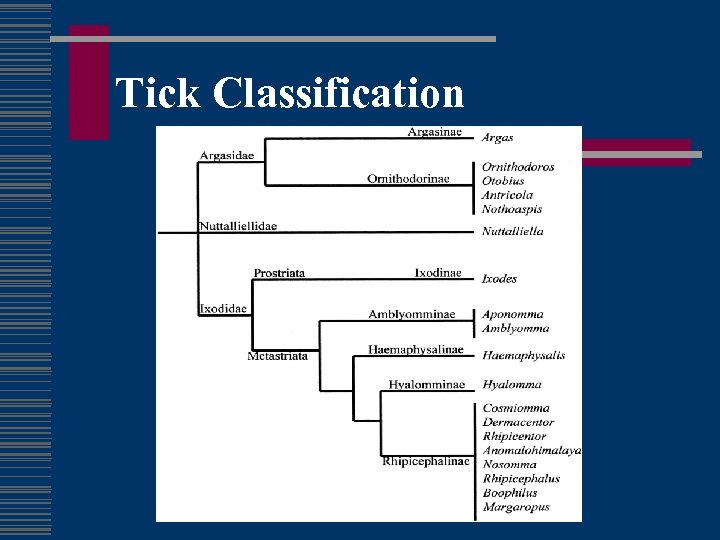
Tick Classification
Questing tick
Rocky Mountain Spotted Fever w Described in late 1900’s in Bitter Root Valley w Caused by infection with Rickettsia rickettsii w Obligate intracellular, requires cell culture to cultivate
RMSF transmission w Maintained transovarially in ticks w Tick vectors are hard ticks: n Dermacentor variabilis (eastern US) n D. andersoni (western US) n A. americanum (southwestern US)
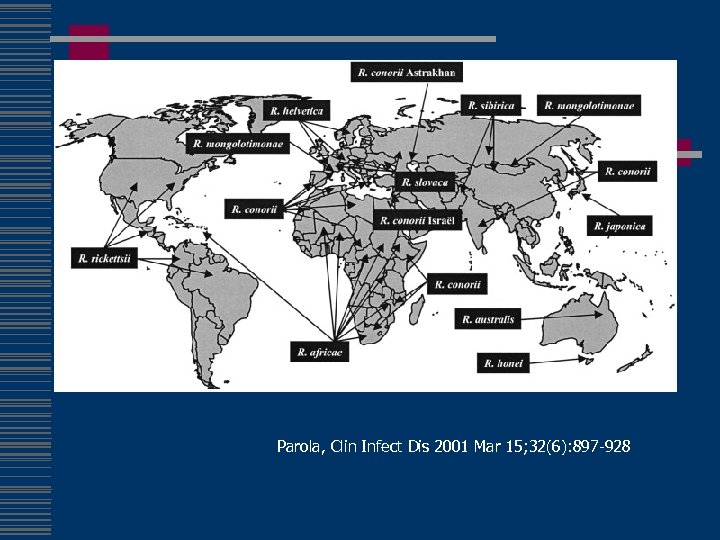
Parola, Clin Infect Dis 2001 Mar 15; 32(6): 897 -928
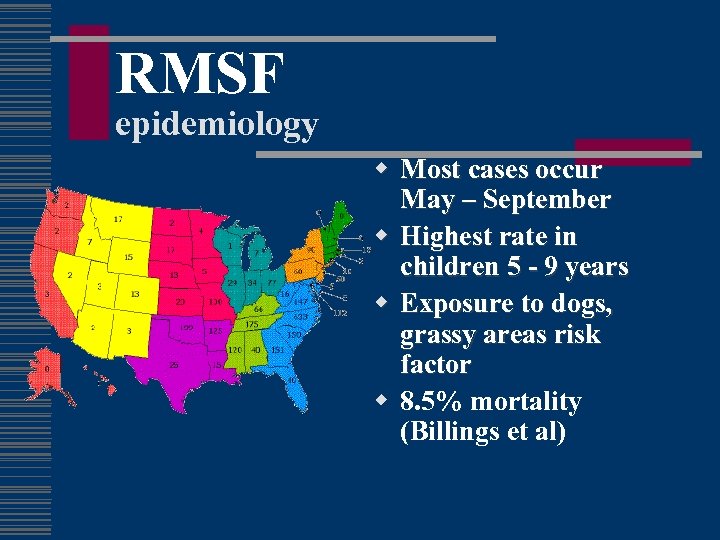
RMSF epidemiology w Most cases occur May – September w Highest rate in children 5 - 9 years w Exposure to dogs, grassy areas risk factor w 8. 5% mortality (Billings et al)
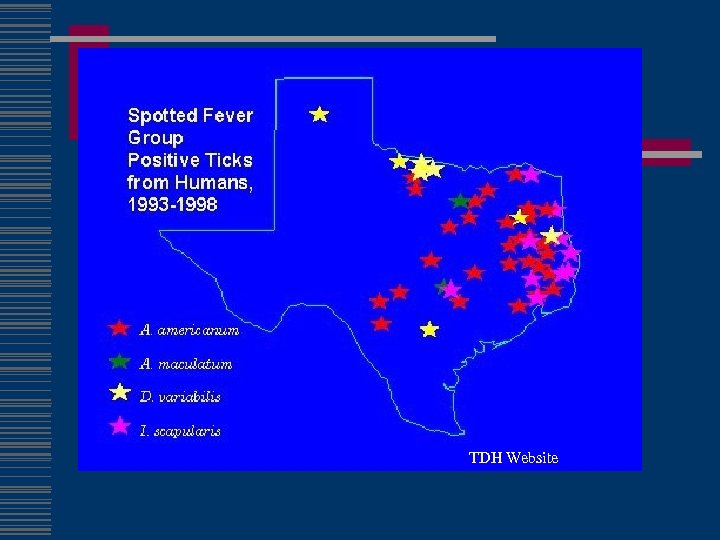
TDH Website
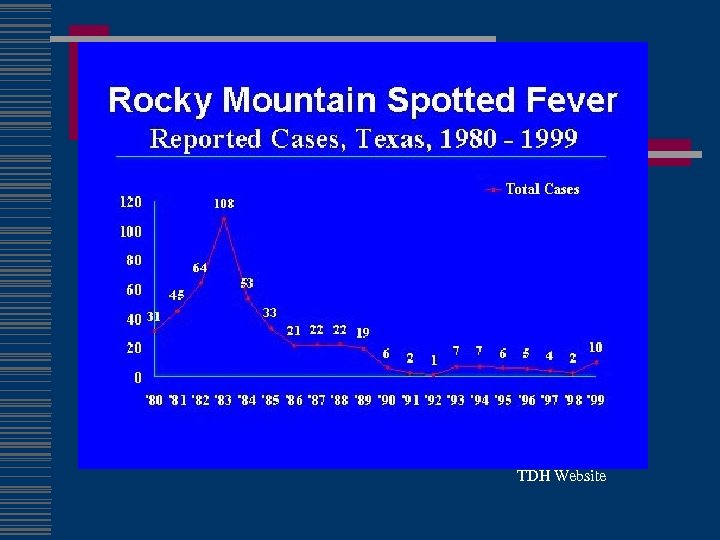
TDH Website
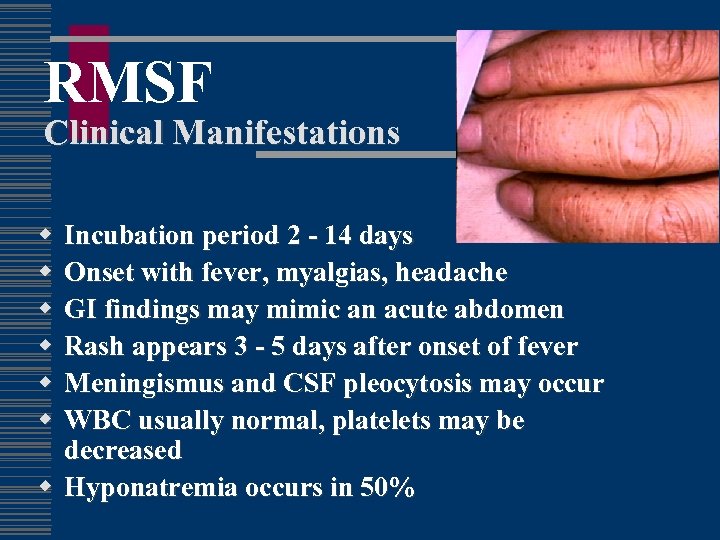
RMSF Clinical Manifestations w w w Incubation period 2 - 14 days Onset with fever, myalgias, headache GI findings may mimic an acute abdomen Rash appears 3 - 5 days after onset of fever Meningismus and CSF pleocytosis may occur WBC usually normal, platelets may be decreased w Hyponatremia occurs in 50%


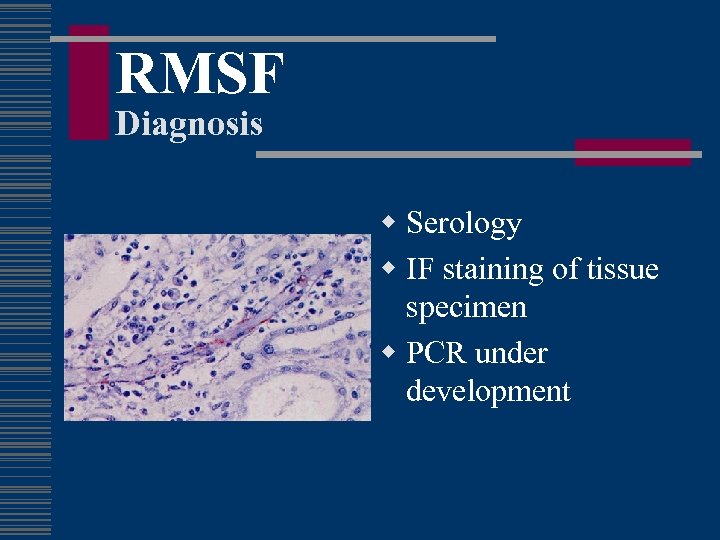
RMSF Diagnosis w Serology w IF staining of tissue specimen w PCR under development
RMSF Outcome w N=6388 over 1981 -1998 w Annual case-fatality rate 3. 3% w Risk factors for mortality: n n Old age Chloramphenicol only Tetracycline not primary therapy Treatment delayed > 5 days Holman et al JID 2001
Clinical Vignette w 54 yo WM farmer in Missouri presents with 3 day h/o high fevers, chills, headache and marked malaise in June w Exam notes a confused, ill-appearing man but is otherwise unremarkable w Labs note transaminases 3 x normal, platelets 115 K, WBC 2. 1, CSF 32 WBC, protein 127
History of Ehrlichiosis w 1935 - E. canis-hemorrhagic illness in Algerian dogs w 1950 s – E. sennetsumononucleosis-like illness in Japan w 1986 – Ehrlichiosis-patient in Detroit after tick bites in Arkansas w 1991 - E. chaffeensis cultured from patient at Fort Chaffee in Arkansas
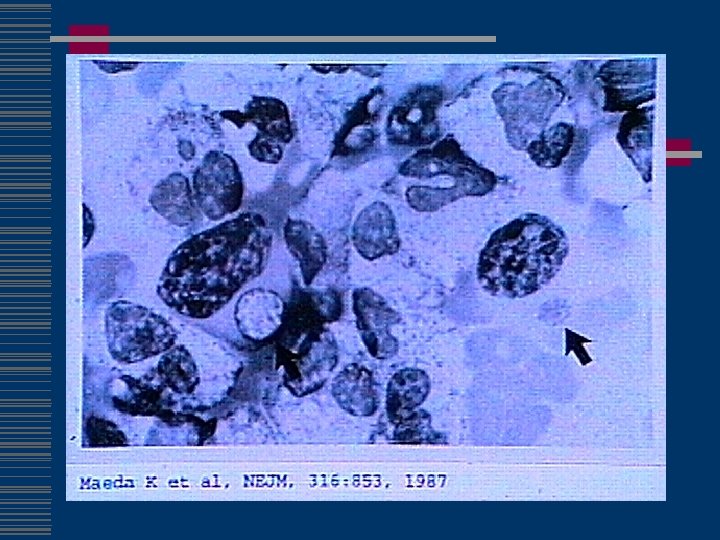
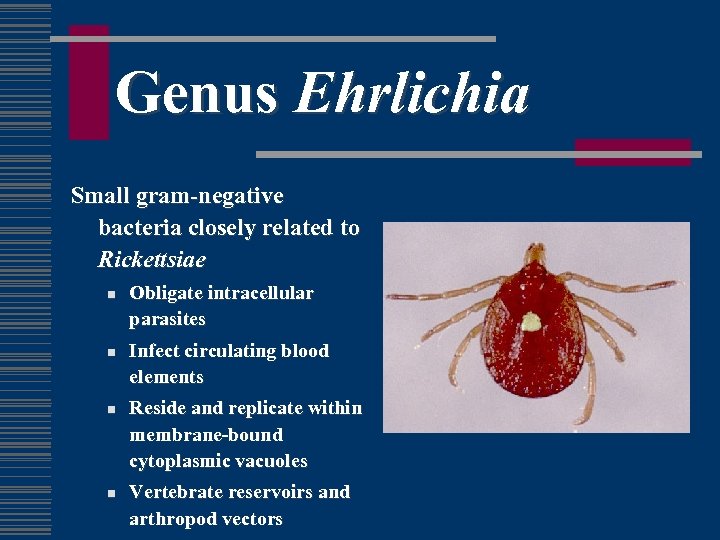
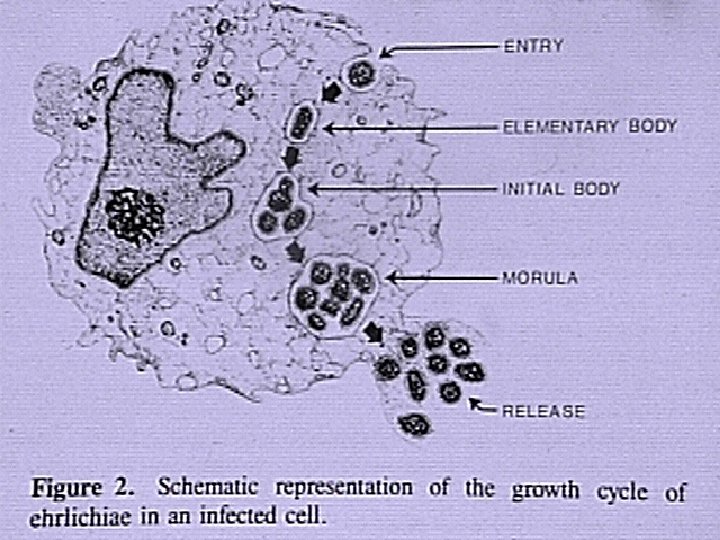
Genus Ehrlichia Small gram-negative bacteria closely related to Rickettsiae n n Obligate intracellular parasites Infect circulating blood elements Reside and replicate within membrane-bound cytoplasmic vacuoles Vertebrate reservoirs and arthropod vectors


Ehrlichia ewingii w First discovered in dogs with granulocytic ehrlichiosis, 1992 w Disease is milder than E. canis infection w Manifestations include fever, lethargy and polyarthritis w Found to date in dogs in Missouri, Arkansas, Oklahoma and N. Carolina w Member of E. canis genogroup (cross-reactivity) w Experimental transmission by A. americanum

Ehrlichiae Causing Human & Veterinary Disease
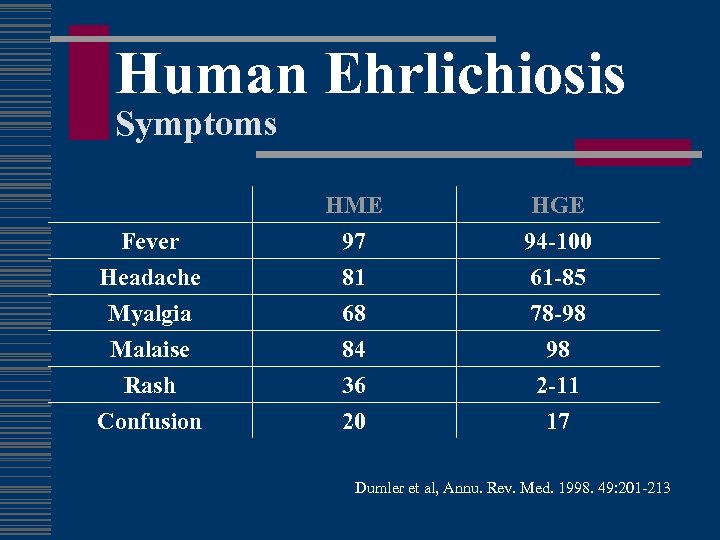
Human Ehrlichiosis Symptoms Fever Headache Myalgia HME 97 81 68 HGE 94 -100 61 -85 78 -98 Malaise Rash Confusion 84 36 20 98 2 -11 17 Dumler et al, Annu. Rev. Med. 1998. 49: 201 -213
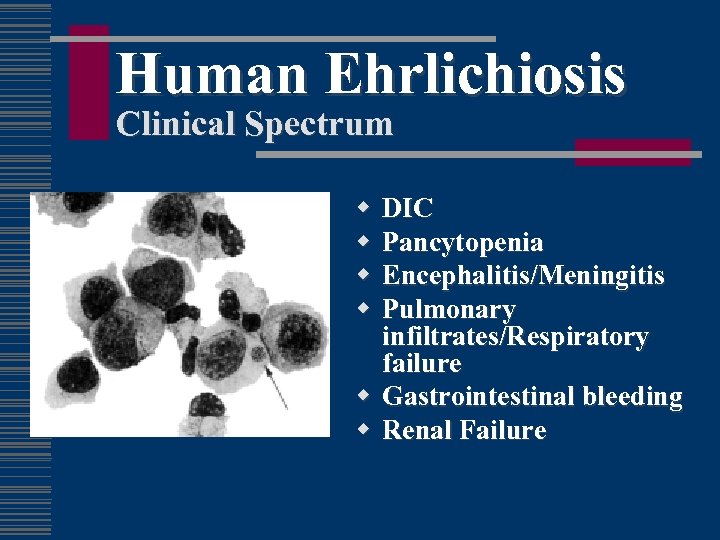
Human Ehrlichiosis Clinical Spectrum w w DIC Pancytopenia Encephalitis/Meningitis Pulmonary infiltrates/Respiratory failure w Gastrointestinal bleeding w Renal Failure
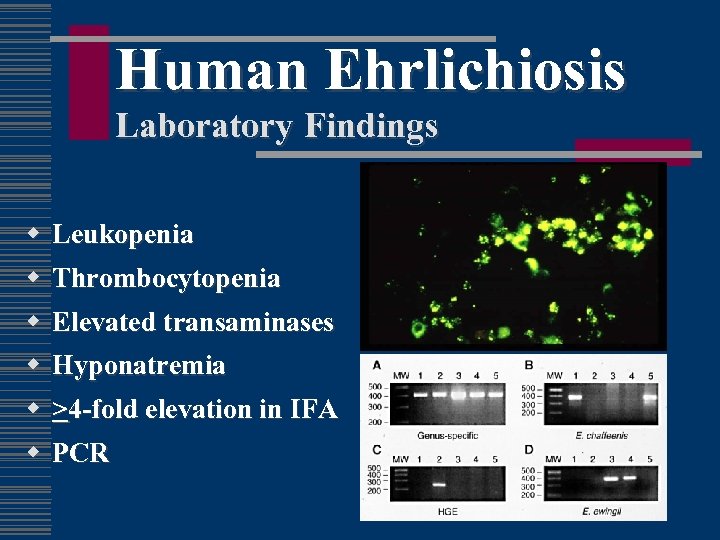
Human Ehrlichiosis Laboratory Findings w w Leukopenia Thrombocytopenia w Elevated transaminases w Hyponatremia w >4 -fold elevation in IFA w PCR
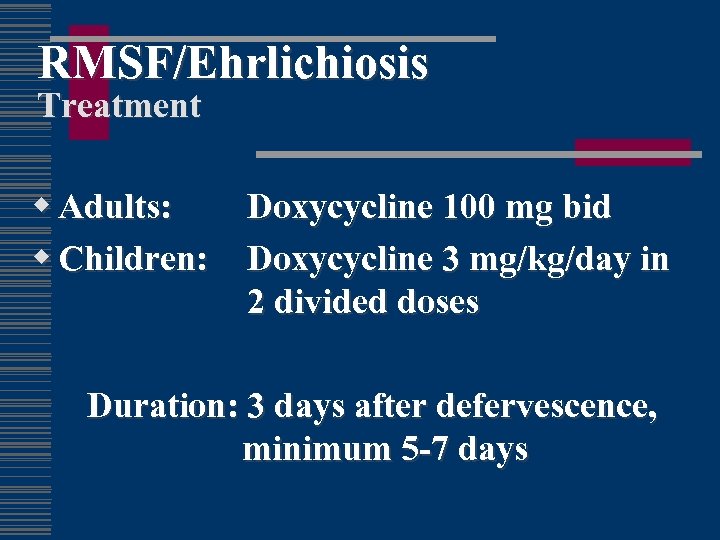
RMSF/Ehrlichiosis Treatment w Adults: w Children: Doxycycline 100 mg bid Doxycycline 3 mg/kg/day in 2 divided doses Duration: 3 days after defervescence, minimum 5 -7 days
Clinical Vignette w 34 yo WF owner of a campground presents with a nonhealing lesion on the right index finger for 2 weeks, adjacent to the nail bed. w Failed Augmentin and acyclovir by PCP for “infected paronychia” w Exam notes an ulcerated lesion and regional adenopathy
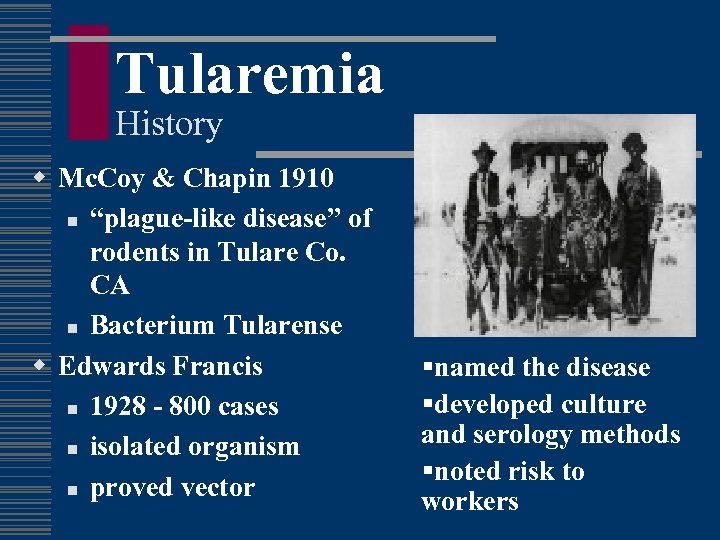
Tularemia History w Mc. Coy & Chapin 1910 n “plague-like disease” of rodents in Tulare Co. CA n Bacterium Tularense w Edwards Francis n 1928 - 800 cases n isolated organism n proved vector §named the disease §developed culture and serology methods §noted risk to workers
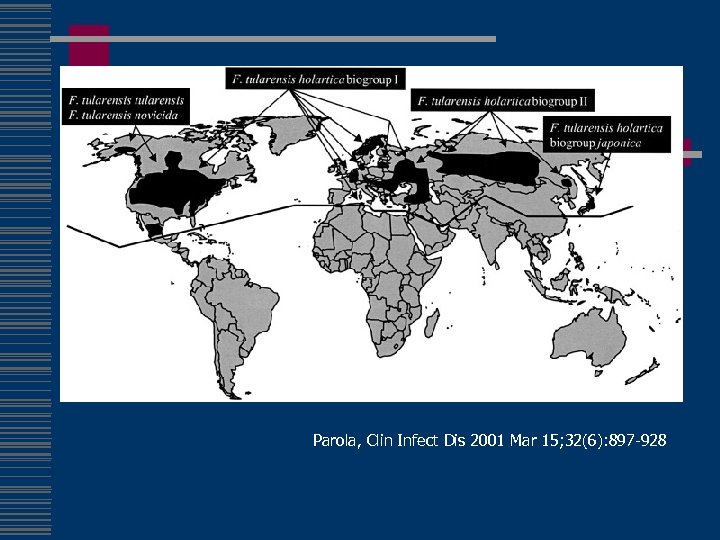
Parola, Clin Infect Dis 2001 Mar 15; 32(6): 897 -928
Tularemia Epidemiology w 1368 cases 1990 -2000 w All states except Hawaii, but predominately MO, AK, OK & SD w Reinstated on nationally notifiable list 2000 (n=142) w Type A (biogroup tularensis) w Multiple vectors (tick, deerfly) w >250 animal species n n n rabbits hares muskrats w Other transmission n carnivores direct contact inhalation/ingestion w Peak incidence 1939
Outbreak 2001 Pneumonic Tularemia w 15 patients in Martha’s Vineyard w 11 primary pulmonary w 1 death Feldman et al, N Engl J Med 2001 Nov 29; 345(22): 1601 -6
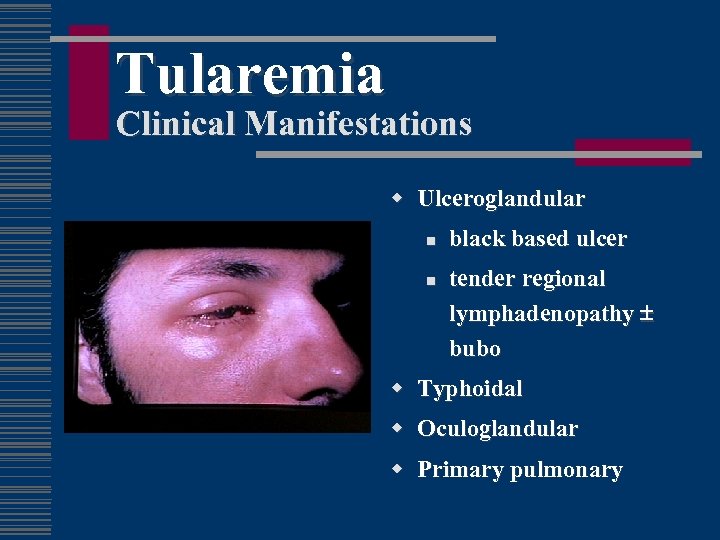
Tularemia Clinical Manifestations w Ulceroglandular n n black based ulcer tender regional lymphadenopathy bubo w Typhoidal w Oculoglandular w Primary pulmonary

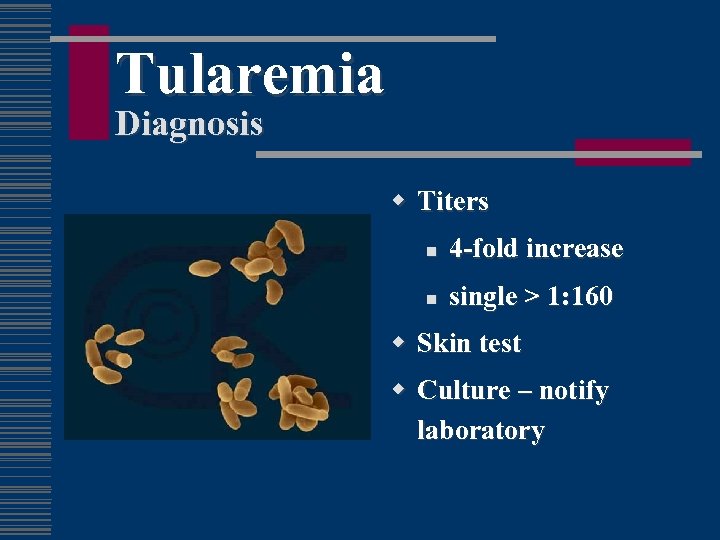
Tularemia Diagnosis w Titers n 4 -fold increase n single > 1: 160 w Skin test w Culture – notify laboratory
Tularemia Treatment w w Streptomycin 1 gm iv q 12 h for 10 days Gentamicin 5 mg/kg/d for 10 days w Tetracycline/chloramphenicol n associated with 15 -20% relapse w Quinolones n Excellent in vitro activity n Limited data, anecdotal experience suggests efficacy w Live attenuated vaccine for high risk groups
Tularemia Complications w Pneumonia abscess, effusion w Rhabdomyolysis w Acute renal failure w Meningitis w Pericarditis
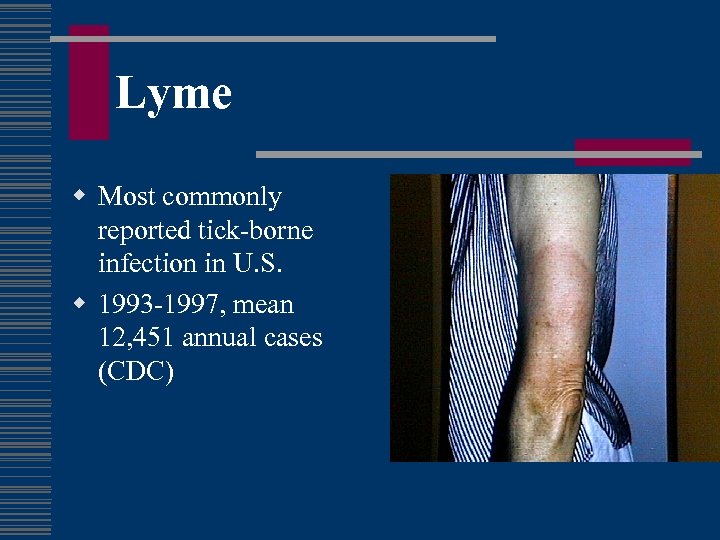
Lyme w Most commonly reported tick-borne infection in U. S. w 1993 -1997, mean 12, 451 annual cases (CDC)

Lyme History w Cluster of cases near Lyme, CT 1975 w Johnson RC, Schmid GP, Hyde FW, Steigerwalt AG, Brenner DJ. Borrelia burgdorferi sp. nov. : etiological agent of Lyme disease. Int J Syst Bacteriol 1984; 34: 496 7.
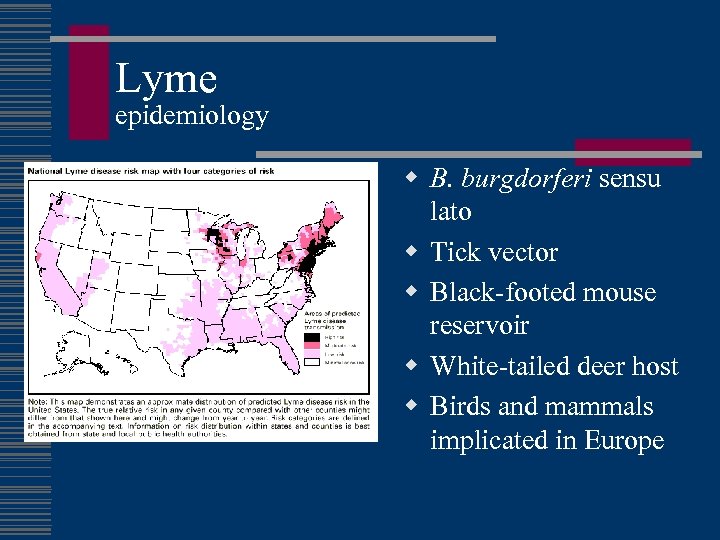
Lyme epidemiology w B. burgdorferi sensu lato w Tick vector w Black-footed mouse reservoir w White-tailed deer host w Birds and mammals implicated in Europe
Lyme Disease Early Manifestations w Erythema migrans (90%) n n Occurs 8 -14 days after bite Single lesion, average size 15 cm Systemic symptoms may be present Secondary lesions may occur w Carditis w Aseptic meningitis w Bell’s palsy
Lyme Disease Late Manifestations w Arthritis n Knees involved in 90% n Usually resolves, 1 -2 weeks n May recur w CNS disease (rare in children)
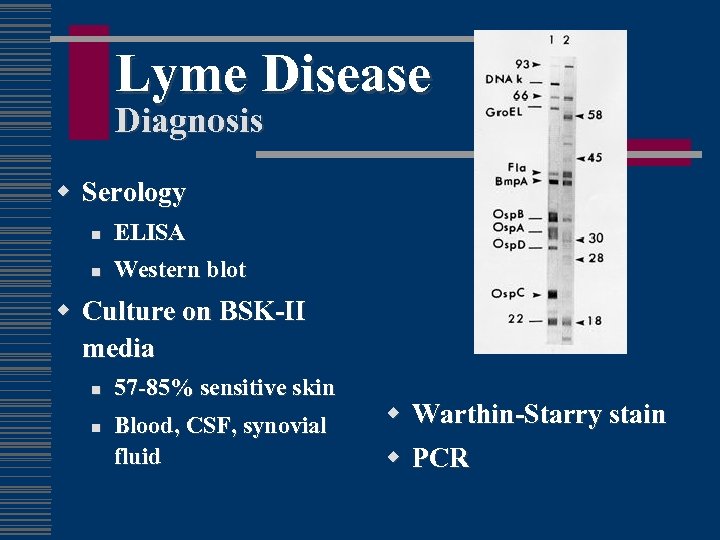
Lyme Disease Diagnosis w Serology n ELISA n Western blot w Culture on BSK-II media n n 57 -85% sensitive skin Blood, CSF, synovial fluid w w Warthin-Starry stain PCR
Lyme Disease Treatment of Early Disease w Doxycycline ( 8 years of age) w Ampicillin n Penicillin allergic: cefuroxime axetil or erythromycin w Duration 14 - 21 days

Lyme Disease Treatment-Disseminated & Late Disease w Multiple skin lesions Oral, 21 days w Isolated facial palsy Oral, 21 -28 days w Arthritis Oral, 28 days w Persistent arthritis Parenteral, 14 - 21 days w Carditis Parenteral, 14 - 21 days w CNS Parenteral, 14 - 21 days
Lyme Disease Vaccine w recombinant B. burgdorferi lipidated outer-surface protein A (r. Osp. A) w Antigen not expressed in host w Antibody is taken up into tick and bacteria destroyed in vector w 0, 1 and 12 months w As of February 25, 2002 LYMErix™ off the market
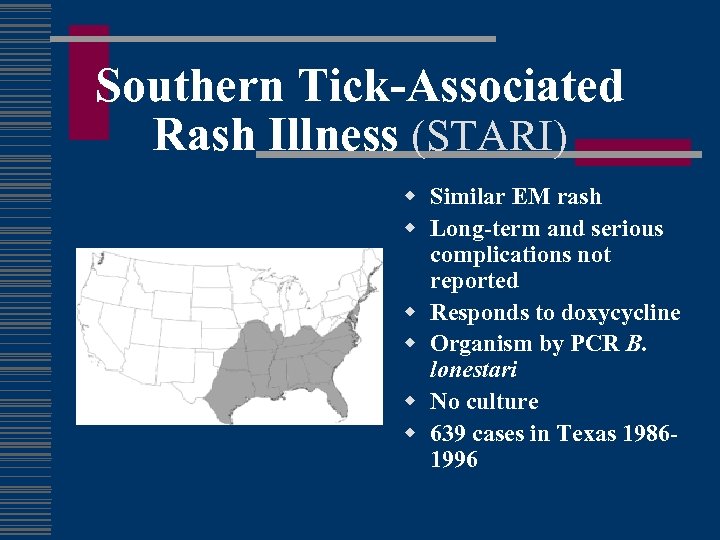
Southern Tick-Associated Rash Illness (STARI) w Similar EM rash w Long-term and serious complications not reported w Responds to doxycycline w Organism by PCR B. lonestari w No culture w 639 cases in Texas 19861996
Clinical Vignette w 25 yo male camper in Montana presents with a 2 week history of intermittent fevers. Initially he had a high fever with headache, red eyes, jaundice, severe body aches, and after about 3 days a diffuse red rash on his trunk. The fever resolved, then about a week later recurred without the other symptoms.
Tick-borne Relapsing Fever w Dutton JE, Todd JL. The nature of tick fever in the eastern part of the Congo Free State, with notes on the distribution and bionomics of the tick. Br Med J 1905; 2: 1259 60. n n n Described tick relapsing fever Borrelia duttonii transmitted by Ornithodoros moubata in W. Africa w 13 species of Borrelia w genus Ornithodoros n Noctural feeder n Short attachment w worldwide
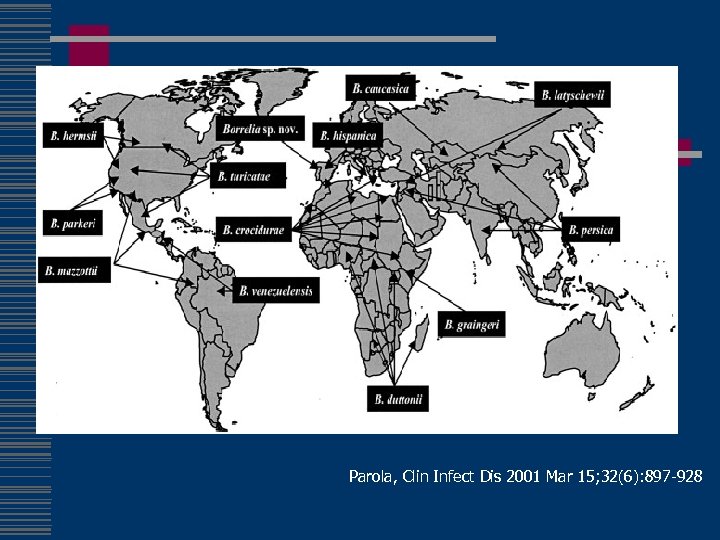
Parola, Clin Infect Dis 2001 Mar 15; 32(6): 897 -928
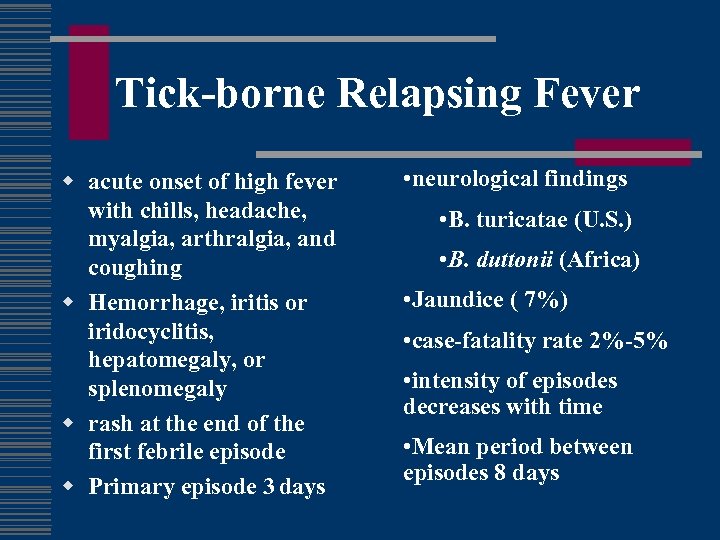
Tick-borne Relapsing Fever w acute onset of high fever with chills, headache, myalgia, arthralgia, and coughing w Hemorrhage, iritis or iridocyclitis, hepatomegaly, or splenomegaly w rash at the end of the first febrile episode w Primary episode 3 days • neurological findings • B. turicatae (U. S. ) • B. duttonii (Africa) • Jaundice ( 7%) • case-fatality rate 2%-5% • intensity of episodes decreases with time • Mean period between episodes 8 days
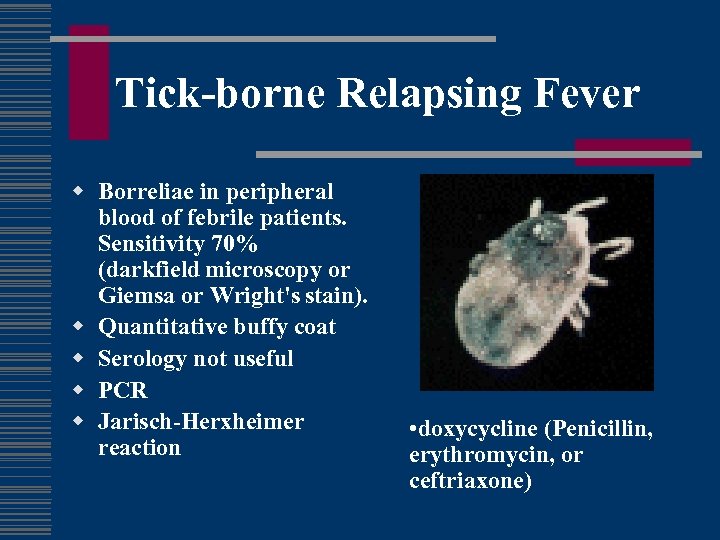
Tick-borne Relapsing Fever w Borreliae in peripheral blood of febrile patients. Sensitivity 70% (darkfield microscopy or Giemsa or Wright's stain). w Quantitative buffy coat w Serology not useful w PCR w Jarisch-Herxheimer reaction • doxycycline (Penicillin, erythromycin, or ceftriaxone)
Tick-Transmitted Diseases Prevention w Avoid tick-infested areas w Wear protective clothing that covers exposed areas w Use DEET - containing insect repellants w Spray permethrin on clothes w Remove attached ticks promptly Do not squeeze
Clinical Vignette w 45 yo BM with h/o Hodgkin’s in remission 5 years after chemo/XRT for Stage 4 disease, presents with acute fever, fatigue, abdominal pain, SOB/DOE, in June in New Jersey. w Exam: hepatosplenomegaly, hyperdynamic precordium, pale.
Babesiosis w Hemoprotozoan Babesia microti and Babesia divergens w similar vector, animal reservoir and geographic distribution as Lyme w Multiplication of the blood stage parasites is responsible for the clinical manifestations of the disease
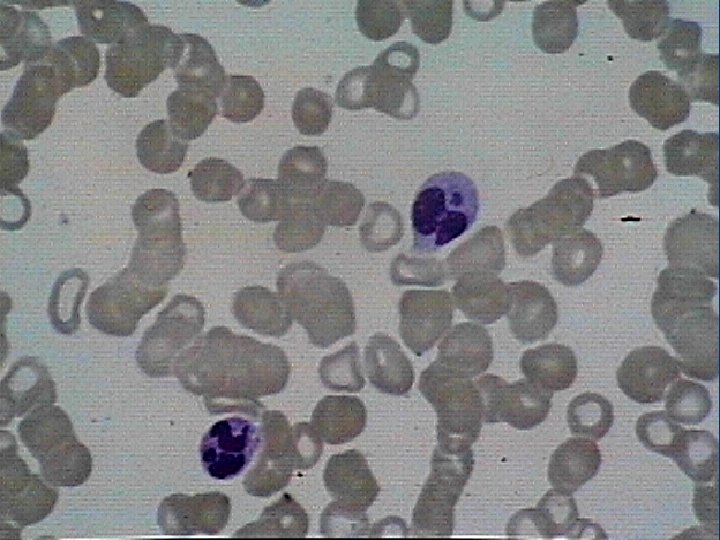
Babesiosis w more severe in patients who are immunosuppressed, splenectomized, and/or elderly w diagnosis by thick and thin smear w Treatment with clindamycin + quinine or atovaquone + azithromycin w exchange transfusion has been used in severely ill patients with high parasitemias
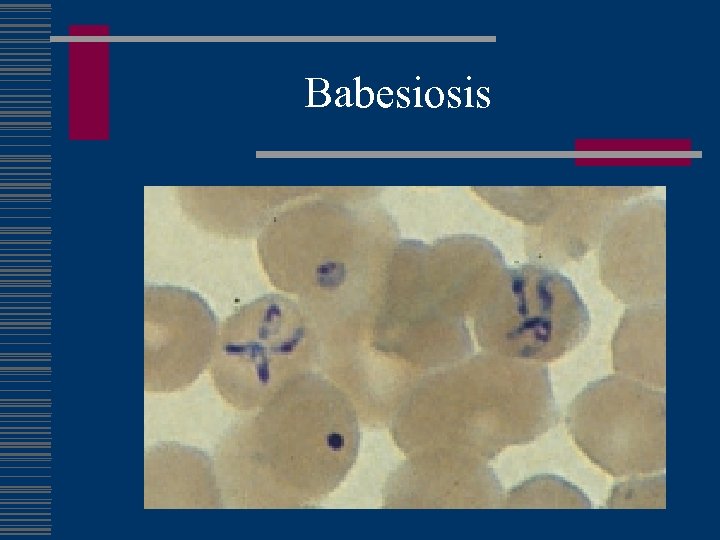
Babesiosis
Clinical Vignette w 48 yo male presents with acute onset episodic fever abdominal pain, headache, myalgias and nausea/vomiting, then profuse sweats. w Recent trip to Thailand looking for exotic bird species. w Exam notes tender right and left upper quadrant and splenomegaly w Labs note pancytopenia
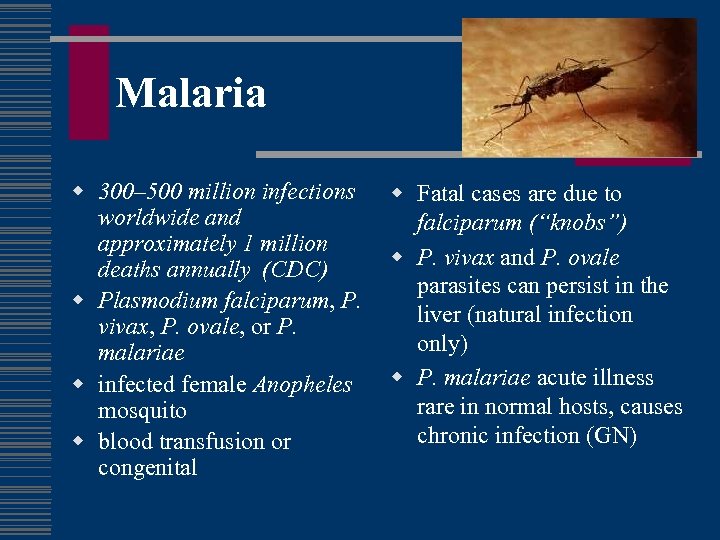
Malaria w 300– 500 million infections worldwide and approximately 1 million deaths annually (CDC) w Plasmodium falciparum, P. vivax, P. ovale, or P. malariae w infected female Anopheles mosquito w blood transfusion or congenital w Fatal cases are due to falciparum (“knobs”) w P. vivax and P. ovale parasites can persist in the liver (natural infection only) w P. malariae acute illness rare in normal hosts, causes chronic infection (GN)
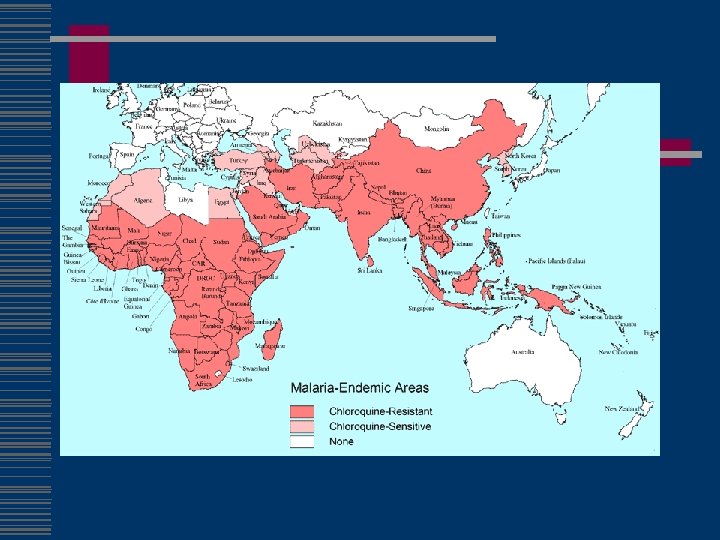

Malaria w Chloroquine-susc n n Dominican Republic, Haiti Central America west of the former Panama Canal Zone Egypt some countries in the Middle East w mefloquine resistance n n n borders of Thailand with Burma (Myanmar) and Cambodia western provinces of Cambodia eastern states of Burma (Myanmar) w Fansidar resistance n n Amazon River Basin area of South America, Southeast Asia other parts of Asia large parts of Africa
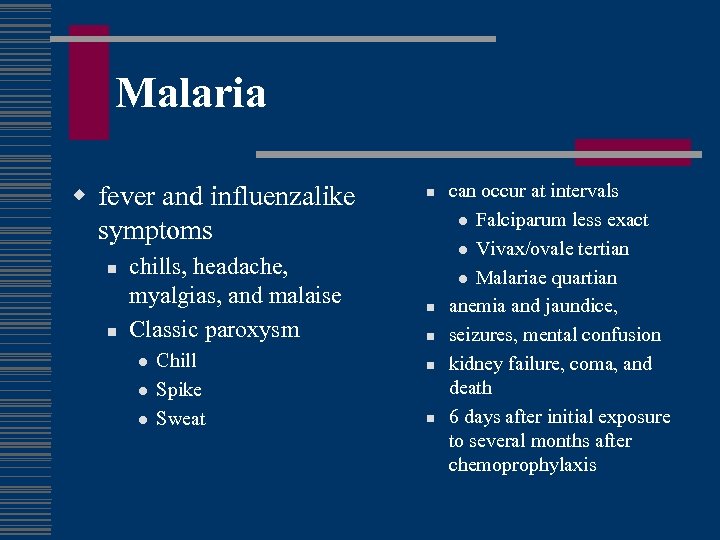
Malaria w fever and influenzalike symptoms n n chills, headache, myalgias, and malaise Classic paroxysm l l l Chill Spike Sweat n n n can occur at intervals l Falciparum less exact l Vivax/ovale tertian l Malariae quartian anemia and jaundice, seizures, mental confusion kidney failure, coma, and death 6 days after initial exposure to several months after chemoprophylaxis
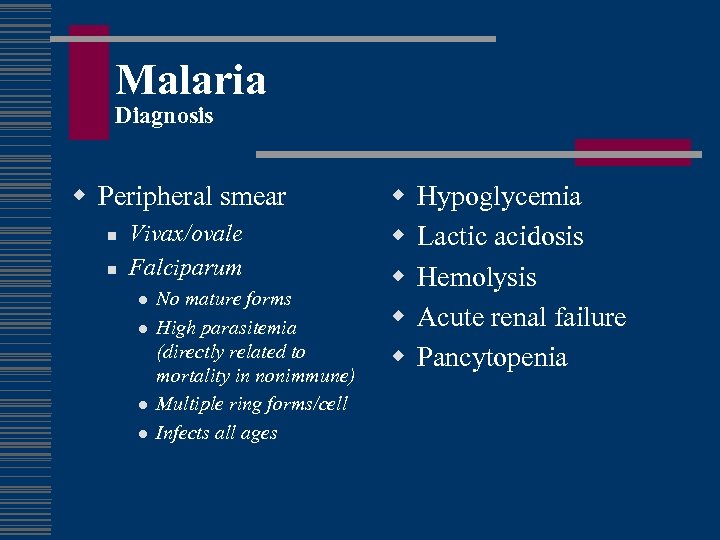
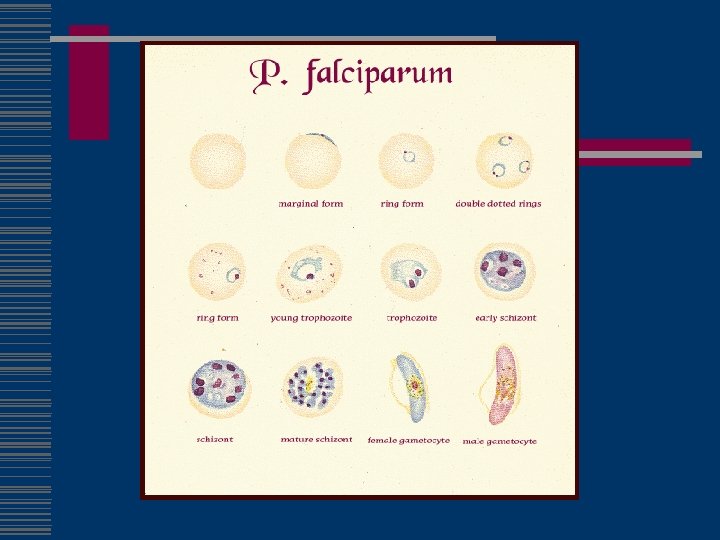
Malaria Diagnosis w Peripheral smear n n Vivax/ovale Falciparum l l No mature forms High parasitemia (directly related to mortality in nonimmune) Multiple ring forms/cell Infects all ages w w w Hypoglycemia Lactic acidosis Hemolysis Acute renal failure Pancytopenia
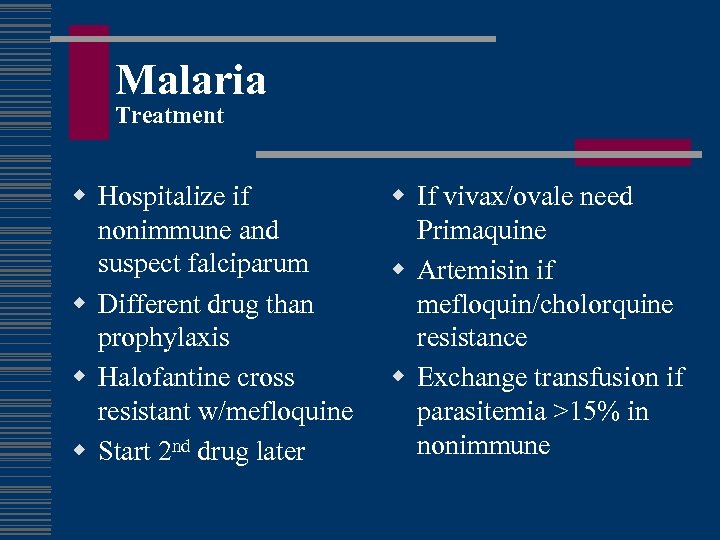
Malaria Treatment w Hospitalize if nonimmune and suspect falciparum w Different drug than prophylaxis w Halofantine cross resistant w/mefloquine w Start 2 nd drug later w If vivax/ovale need Primaquine w Artemisin if mefloquin/cholorquine resistance w Exchange transfusion if parasitemia >15% in nonimmune
Malaria Prevention w transmission occurs w pyrethroid-containing primarily between dusk flying-insect spray in and dawn living and sleeping areas w well-screened areas, mosquito nets, clothes that cover w DEET (N, Ndiethylmetatoluamide)
Chemoprophylaxis w mefloquine or chloroquine 1– 2 weeks before w doxycycline and atovaquone/proguanil 1– 2 days before w continuously while in malaria-endemic areas w 4 weeks (chloroquine, doxycycline, or mefloquine) after w 7 days (atovaquone/proguanil) after w Terminal prophylaxis with Primaquine final 14 days n fatal hemolysis in those who are G 6 PD deficient
Chemoprophylaxis pregnancy w Long history of chloroquine and quinine use w Data supports safety of mefloquine in 2 nd an 3 rd trimester w Data in first trimester sketchy, patient must weigh risks w No Doxycycline or Primaquine w No data for Malarone
Malaria Information w http: //www. cdc. gov/travel w Voice information service 1 -877 -FYI-TRIP w CDC Malaria Hotline (770 -488 -7788) from 8: 00 a. m. to 4: 30 p. m. Eastern time w CDC Emergency Operation Center at 770 -488 -7100 n page person on call for the Malaria Epidemiology Branch.
Clinical Vignette w 72 yo WM alcoholic with CAD presents with 3 day h/o fever, myalgias, headache followed by acute onset confusion and tremulousness w Works as a nursery sales rep and travels frequently to East Texas w No improvement on levaquin w EKG afib w CSF notes elevated protein and lymphocytic pleiocytosis
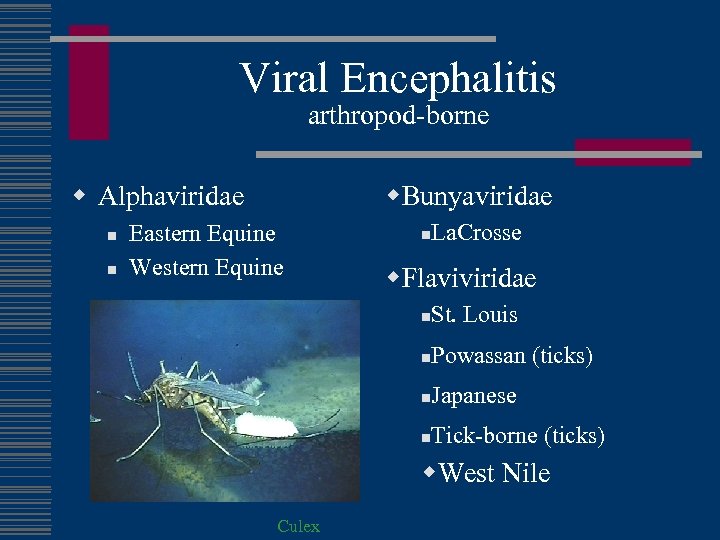
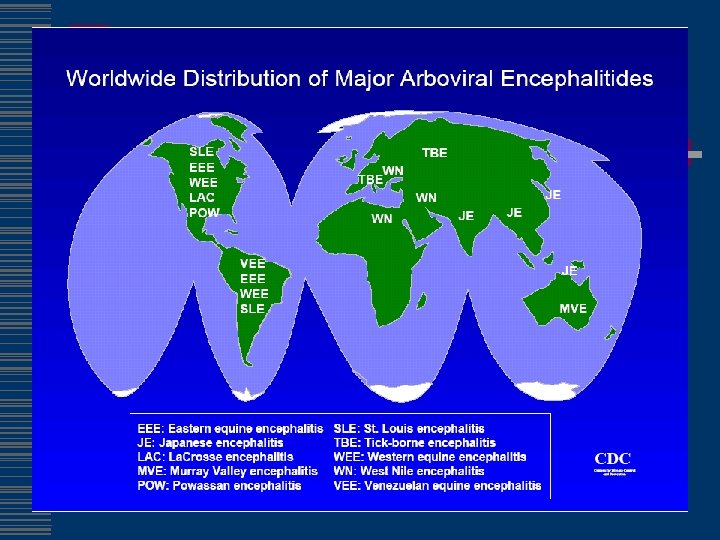
Viral Encephalitis arthropod-borne w. Bunyaviridae w Alphaviridae n n Eastern Equine Western Equine n La. Crosse w. Flaviviridae n St. Louis n Powassan (ticks) n Japanese n Tick-borne (ticks) w. West Nile Culex
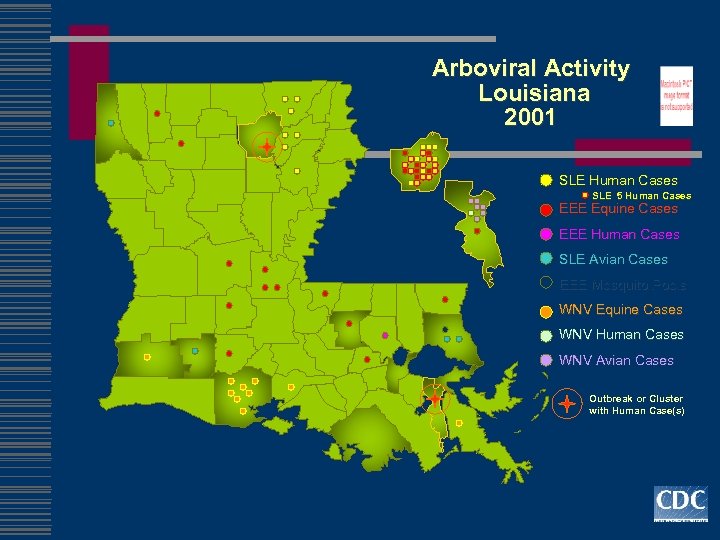
Arboviral Activity Louisiana 2001 SLE Human Cases SLE 5 Human Cases EEE Equine Cases EEE Human Cases SLE Avian Cases EEE Mosquito Pools WNV Equine Cases WNV Human Cases WNV Avian Cases Outbreak or Cluster with Human Case(s)
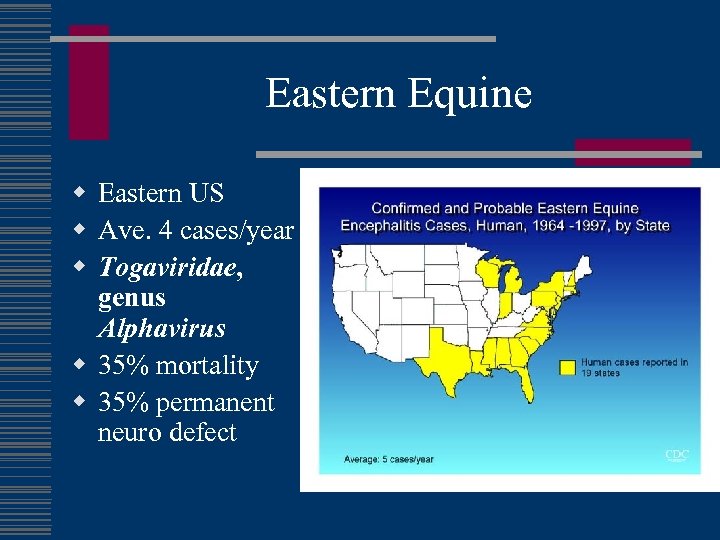
Eastern Equine w Eastern US w Ave. 4 cases/year w Togaviridae, genus Alphavirus w 35% mortality w 35% permanent neuro defect
St. Louis Encephalitis w Aseptic meningitis or encephalitis w Majority subclinical or mild illness w Intermittent epidemic transmission - up to 3, 000 cases per year (1975) w Culex mosquitoes w Elderly - biological risk factor w Low SES areas - environmental risk factor w Outdoor occupation - exposure risk factor
St. Louis Encephalitis w Largest outbreaks in 15 years occurred in 1990 w Urban transmission in west first recognized in 1987 w Deterioration of inner cities, global warming may increase vector abundance and transmission w Unpredictable and intermittent occurrences of outbreaks w Multiple environmental, biological and social factors contributing to disease occurrence w Virus maintenance and overwintering cycle
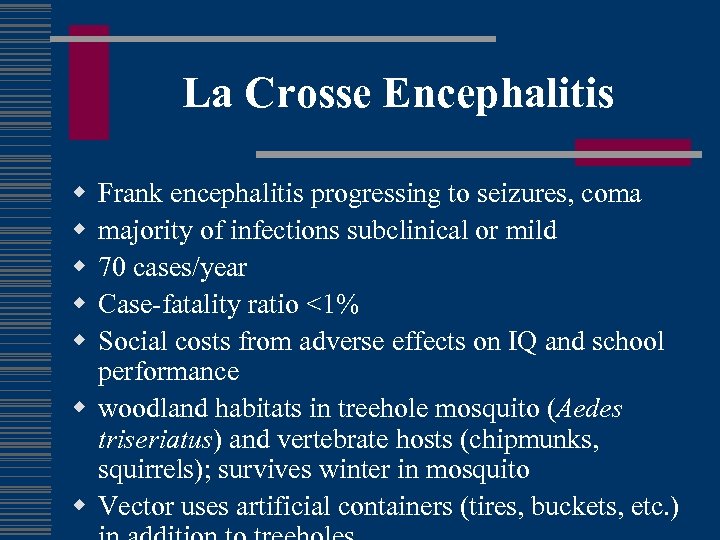
La Crosse Encephalitis w w w Frank encephalitis progressing to seizures, coma majority of infections subclinical or mild 70 cases/year Case-fatality ratio <1% Social costs from adverse effects on IQ and school performance w woodland habitats in treehole mosquito (Aedes triseriatus) and vertebrate hosts (chipmunks, squirrels); survives winter in mosquito w Vector uses artificial containers (tires, buckets, etc. )
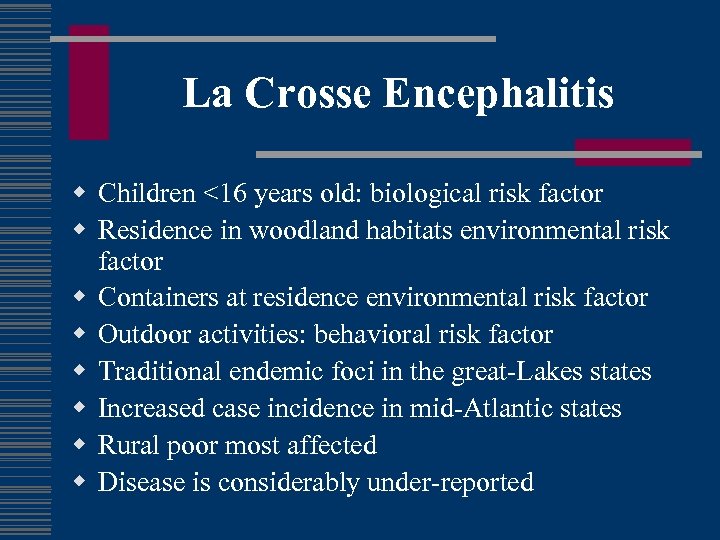
La Crosse Encephalitis w Children <16 years old: biological risk factor w Residence in woodland habitats environmental risk factor w Containers at residence environmental risk factor w Outdoor activities: behavioral risk factor w Traditional endemic foci in the great-Lakes states w Increased case incidence in mid-Atlantic states w Rural poor most affected w Disease is considerably under-reported
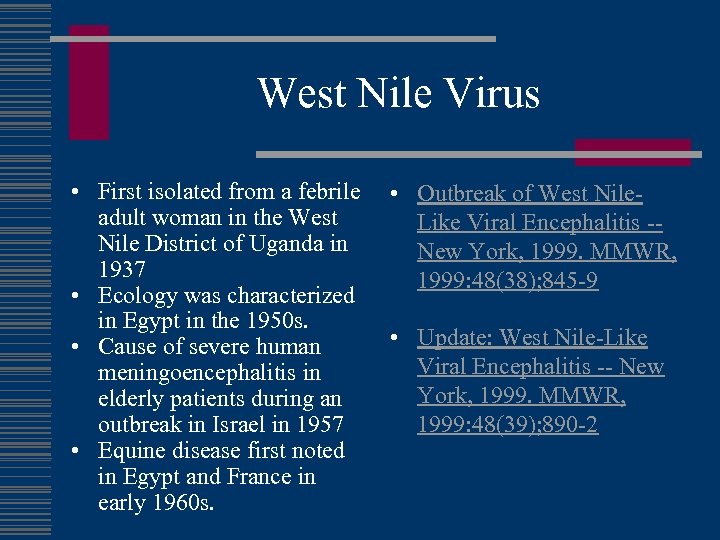
West Nile Virus • First isolated from a febrile adult woman in the West Nile District of Uganda in 1937 • Ecology was characterized in Egypt in the 1950 s. • Cause of severe human meningoencephalitis in elderly patients during an outbreak in Israel in 1957 • Equine disease first noted in Egypt and France in early 1960 s. • Outbreak of West Nile. Like Viral Encephalitis -New York, 1999. MMWR, 1999: 48(38); 845 -9 • Update: West Nile-Like Viral Encephalitis -- New York, 1999. MMWR, 1999: 48(39); 890 -2
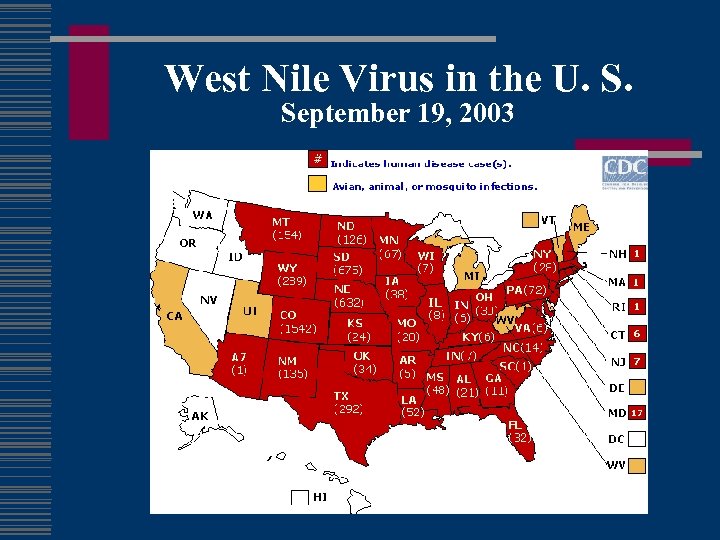
West Nile Virus in the U. S. September 19, 2003
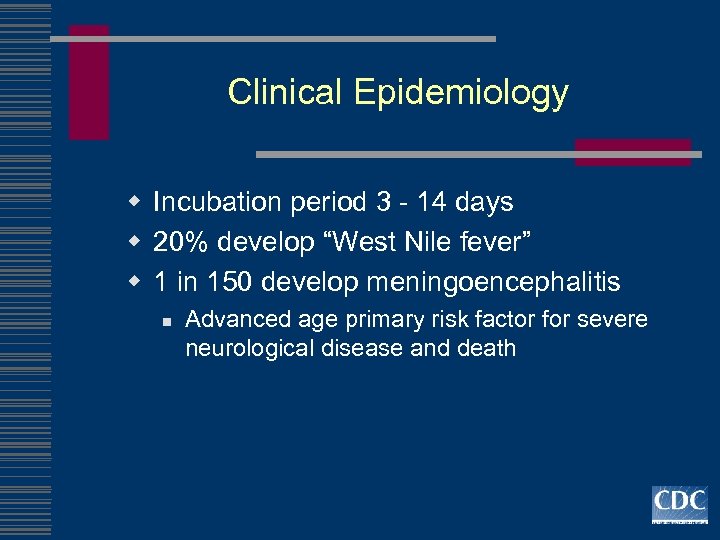
Clinical Epidemiology w Incubation period 3 - 14 days w 20% develop “West Nile fever” w 1 in 150 develop meningoencephalitis n Advanced age primary risk factor for severe neurological disease and death
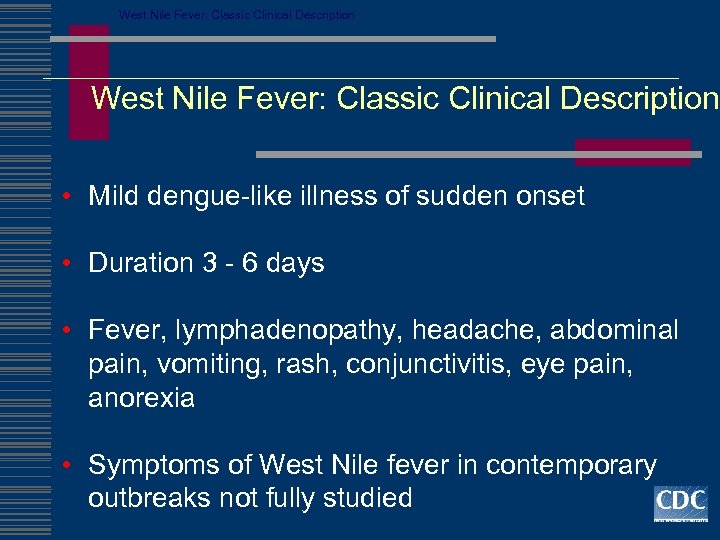
West Nile Fever: Classic Clinical Description • Mild dengue-like illness of sudden onset • Duration 3 - 6 days • Fever, lymphadenopathy, headache, abdominal pain, vomiting, rash, conjunctivitis, eye pain, anorexia • Symptoms of West Nile fever in contemporary outbreaks not fully studied
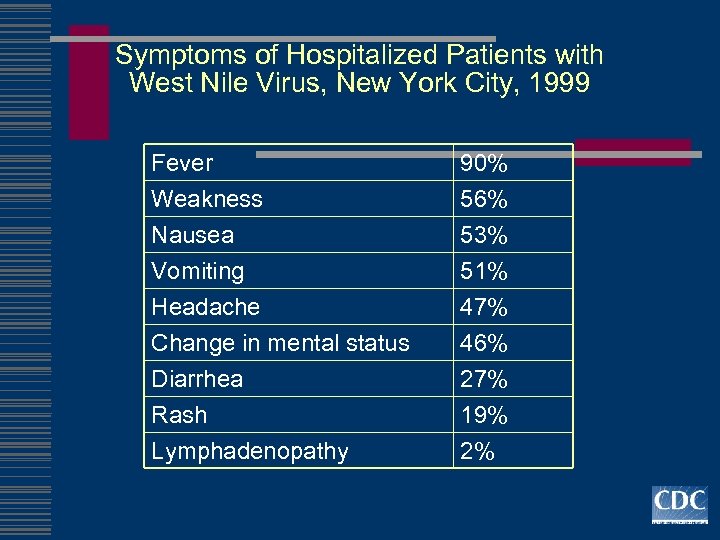
Symptoms of Hospitalized Patients with West Nile Virus, New York City, 1999 Fever Weakness Nausea Vomiting Headache Change in mental status Diarrhea Rash Lymphadenopathy 90% 56% 53% 51% 47% 46% 27% 19% 2%
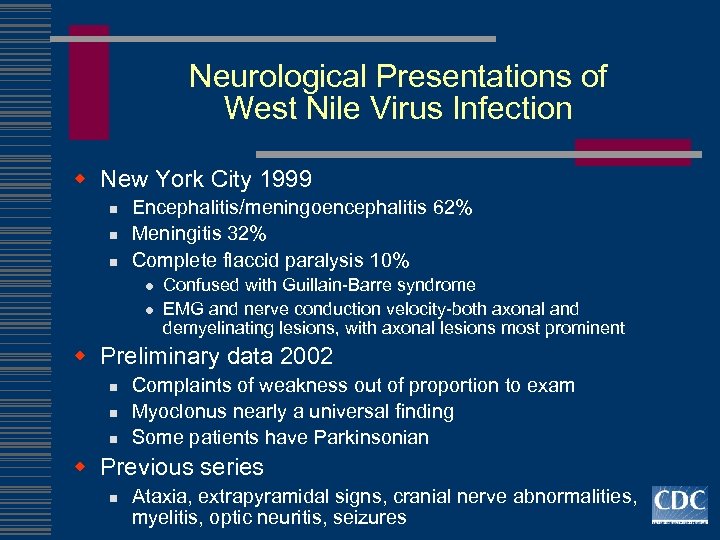
Neurological Presentations of West Nile Virus Infection w New York City 1999 n n n Encephalitis/meningoencephalitis 62% Meningitis 32% Complete flaccid paralysis 10% l l Confused with Guillain-Barre syndrome EMG and nerve conduction velocity-both axonal and demyelinating lesions, with axonal lesions most prominent w Preliminary data 2002 n n n Complaints of weakness out of proportion to exam Myoclonus nearly a universal finding Some patients have Parkinsonian w Previous series n Ataxia, extrapyramidal signs, cranial nerve abnormalities, myelitis, optic neuritis, seizures
West Nile Virus w 489 WNV-viremic donors as of 9/16/03 w two cases of blood transfusion-associated WNV in 2003, (TX and Nebraska). Both encephalitis and are recovering. w In 2003, all blood banks screening for West Nile virus and will not take donations from people w/fever and headache in the week prior
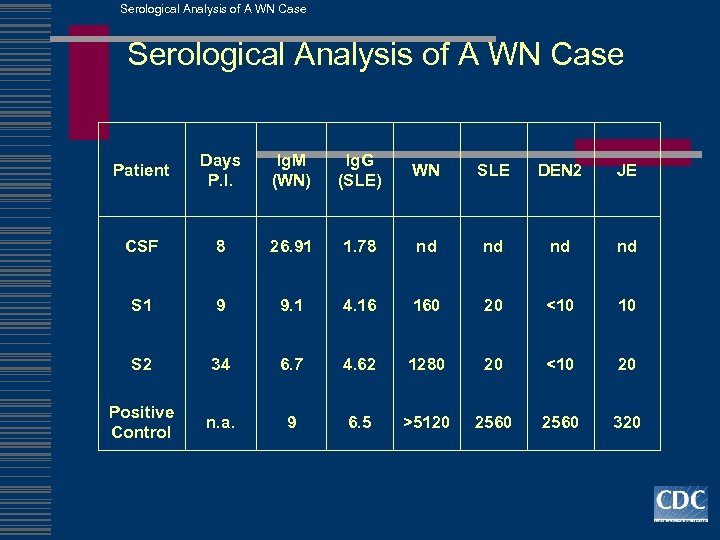
Serological Analysis of A WN Case Patient Days P. I. Ig. M (WN) Ig. G (SLE) WN SLE DEN 2 JE CSF 8 26. 91 1. 78 nd nd S 1 9 9. 1 4. 16 160 20 <10 10 S 2 34 6. 7 4. 62 1280 20 <10 20 Positive Control n. a. 9 6. 5 >5120 2560 320
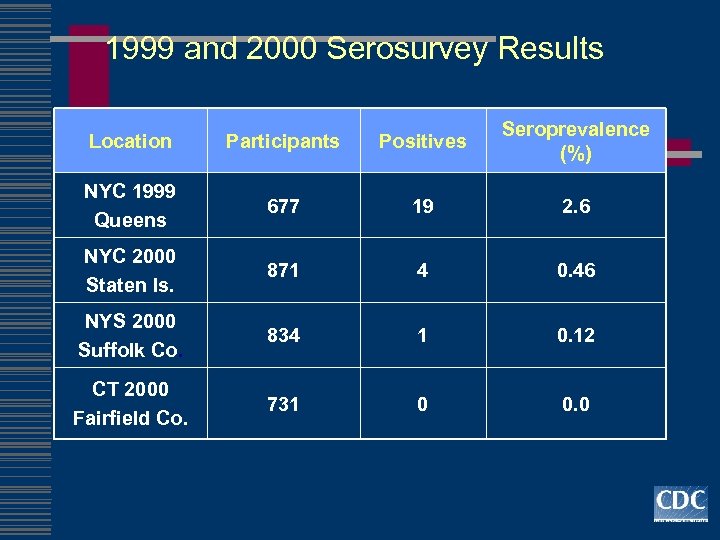
1999 and 2000 Serosurvey Results Location Participants Positives Seroprevalence (%) NYC 1999 Queens 677 19 2. 6 NYC 2000 Staten Is. 871 4 0. 46 NYS 2000 Suffolk Co. 834 1 0. 12 CT 2000 Fairfield Co. 731 0 0. 0
Clinical Vignette w 59 yo Mexican immigrant admit with 3 month history of progressive shortness of breath, PND, orthopnea, LE edema.
Chagas’ Disease w American trypanosomiasis (Trypanosoma cruzi) w 16 -18 million people are infected w 50, 000 will die each year. w poorly constructed houses found in the rural areas of the above-mentioned countries are at elevated risk of infection. Houses constructed from mud, adobe, or thatch present the greatest risk.
Chagas’ Disease w Reduviid bugs, or "kissing w Uncooked food bugs" in South and Central contaminated with infective America feces of "kissing bugs. " w deposits feces on a person's w one-third chronic symptoms skin at night develop after 10 -20 years. w rubs the feces into the bite w average life expectancy wound, an open cut, the decreases by an average of 9 eyes, or mouth. years. w Transplacental, congenital or breastfeeding. w By blood transfusion
Chagas’ Disease w Acute: n n n 1% of cases. Romaña's sign fatigue, fever, enlarged liver or spleen, and swollen lymph glands. rash, loss of appetite, diarrhea, and vomiting occur. infants and in very young children cerebral edema symptoms last for 4 -8 weeks. w Indeterminate (asymptomatic: ) w Chronic: n n n CHF megaesophagus, megacolon in immune compromised, including persons with HIV/AIDS, Chagas disease can be severe.
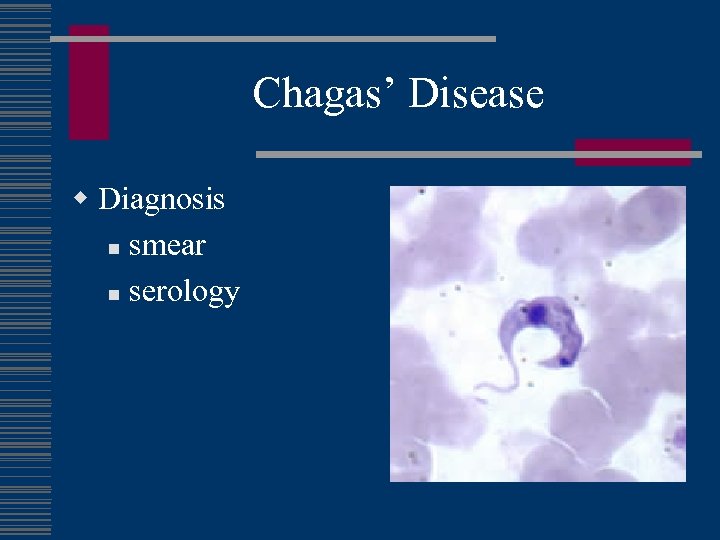
Chagas’ Disease w Diagnosis n smear n serology
Clinical Vignette w September 9, 1981, a 72 -year-old male from Edinburg, Texas, developed fever and weakness 16 days after being bitten by tsetse flies during a hunting trip in northwest Tanzania. Several days after onset of fever, he noticed a raised, tender, erythematous nodule (6 -8 cm in diameter) on the posterior aspect of his right arm.
East African Trypanosomiasis w six patients have shared several characteristics: n n n exposure to infected tsetse flies while visiting game parks in eastern or southern Africa, development of acute, febrile illness consistent with Trypanosoma brucei rhodesiense infection 1 -21 days after visiting detectable typanosomes on peripheral blood smears, and recovery after appropriate therapy. Only 2/5 showed clear evidence of central nervous system (CNS) involvement; both patients had elevated CSF protein, increased CSF cell count, and trypanosomes in the CSF.
East African Trypanosomiasis w Suramin is recommended for hemolymphatic stage n n does not cross the blood-brain barrier, Melarsoprol, (relatively toxic) +/- suramin when infection involves the CNS w trypanosomes are observed in the CSF w morula cells of Mott or an elevated CSF Ig. M is strongly suggest CNS involvement w elevated CSF cell count usually w should be monitored for CNS involvement during treatment and at regular intervals for 1 -2 years thereafter
Don’t forget w w w Dengue Plague Yellow fever Onchocerciasis Loaiasis West African Trypanosomiasis w Typhus w Q fever w Louse-borne relapsing fever w Leischmaniasis
148fece1641c391fdbf6df1dbfa961a1.ppt