VASCULITIS for russians 2003.ppt
- Количество слайдов: 55
VASCULITIS Alexandra Balbir-Gurman
Definition • Blood vessels inflammation and damage • Tissue ischemia Primary vasculitis Secondary vasculitis (infections, viruses, tumors, collagen diseases: RA, Sjögren’s syndrome, SLE, SSc, Myositis)
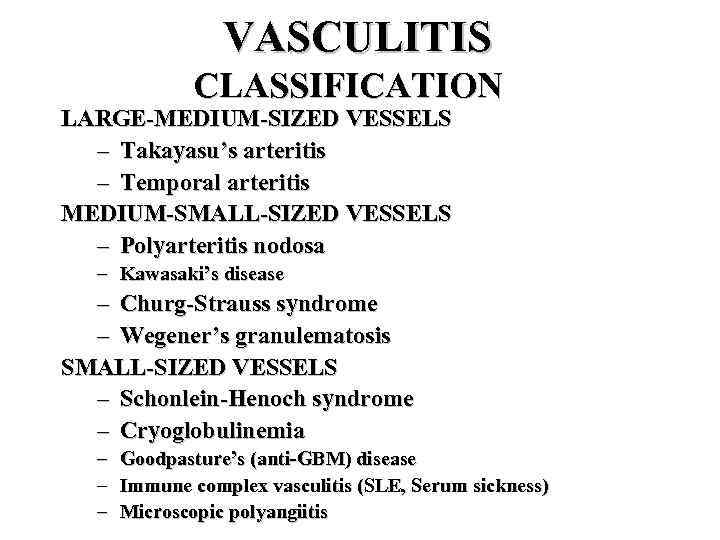
VASCULITIS CLASSIFICATION LARGE-MEDIUM-SIZED VESSELS – Takayasu’s arteritis – Temporal arteritis MEDIUM-SMALL-SIZED VESSELS – Polyarteritis nodosa – Kawasaki’s disease – Churg-Strauss syndrome – Wegener’s granulematosis SMALL-SIZED VESSELS – Schonlein-Henoch syndrome – Cryoglobulinemia – – – Goodpasture’s (anti-GBM) disease Immune complex vasculitis (SLE, Serum sickness) Microscopic polyangiitis
VASCULITIS CLASSIFICATION MISCELLANEOUS SYNDROMES – Behcet’s syndrome – Pyoderma gangrenosum
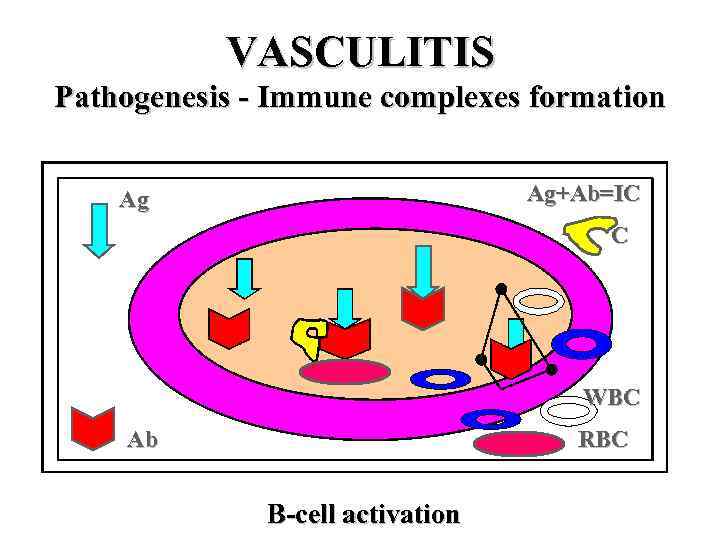
VASCULITIS Pathogenesis - Immune complexes formation Ag+Ab=IC Ag C WBC Ab RBC B-cell activation
Vasculitis with IC • Serum sickness • CTD – SLE • PAN – Virus hepatitis B in IC • Cryoglobulinemic vasculitis – Hepatitis C related IC in cryoprecipitates
Vasculitis with IC • Antigen excess • IC formation • Increased permeability of blood vessels – PLT & MC: histamine, bradykinin, leukotriens • Activation of complement – C 5 a – chemotaxis of PMNC – Degranulation of PMNC • Compromised blood flow – Tissue ischemia
Vasculitis with IC depositions • • • Henoch-Schonlein purpura CVD Serum sickness HCV related mixed cryoglobulinemia HBV related PAN
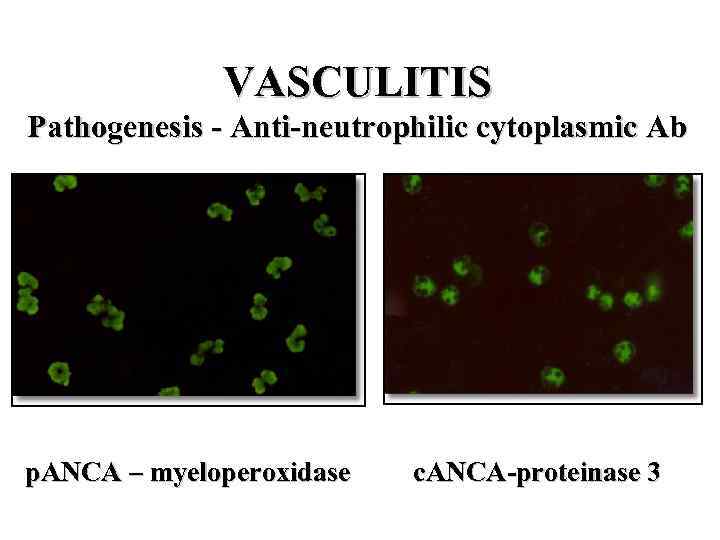
VASCULITIS Pathogenesis - Anti-neutrophilic cytoplasmic Ab p. ANCA – myeloperoxidase c. ANCA-proteinase 3
ANCA related • • • Wegener’s granulomatosis Churg-Strauss syndrome Microscopic polyangiitis Necrotizing & crescentic GN Goodpasture’s syndrome Crohn’s disease , others IBD
ANCA associated vasculitis • TNF , IL-1 induce translocation of azurophilic granules to membrane of monocytes and PMNC • Myeloperoxidase or proteinase 3 interact with extracellular ANCA • Monocytes and PMNC degranulate and release ROS, IL-1, IL-8 • Tissue damage • No correlation between c. ANCA and WG activity
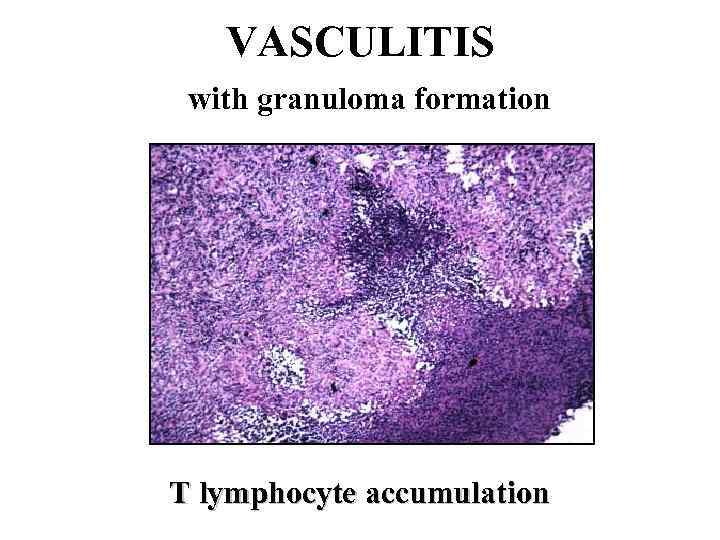
VASCULITIS with granuloma formation T lymphocyte accumulation
VASCULITIS with granuloma formation • Ag or IC induce delayed hypersensitivity and cell mediated injury • EC activation – INF, IL-1 – T-ly activation • TNF • IL-1 – Adhesion molecules formation » ELAM-1 » VCAM-1
T-ly response and granuloma formation • • GCA Takayasu-s Wegener’s granulomatosis Churg-Strauss syndrome
Suspicion of vasculitis • • Systemic ilness Purpura Pulmonary infiltrates Microhematuria Chronic sinusitis Mononeuritis multiplex Unexplaned ischemia GN
DD vasculitis • • • Infection Neoplasia Lymphoma Coagulopathy Drugs/toxins Others
Takayasu’s Arteritis Pulse-less disease Incidence: 1 -3/1 000/year. Epidemiology: girls+young women Japan, India, Africa, Asia, South America, Europe, US. F: M=7: 1. Age 10 -50 years (90% <30 y) Pathology: Involves aortic arch, descending aorta and its branches + AV involvement, coronary and pulmonary arteries Panarteritis with granuloma (mononuclears) narrowed vessels and thrombus formation
Takayasu’s Arteritis General: malaise, fever, night sweats, weight loss, arthralgia/arthritis Vascular: – Arm claudication/numbness – Pulses changes/discrepancy – Hypertension – Renal failure – Aortic regurgitation (AR) – Pulmonary hypertension Laboratory: anemia, ESR/CRP elevation Diagnosis: angiography, MRI angiography Treatment: steroids, cytotoxic drugs, control of hypertension, arterial reconstruction, AVR Prognosis: 15 year survival 90%
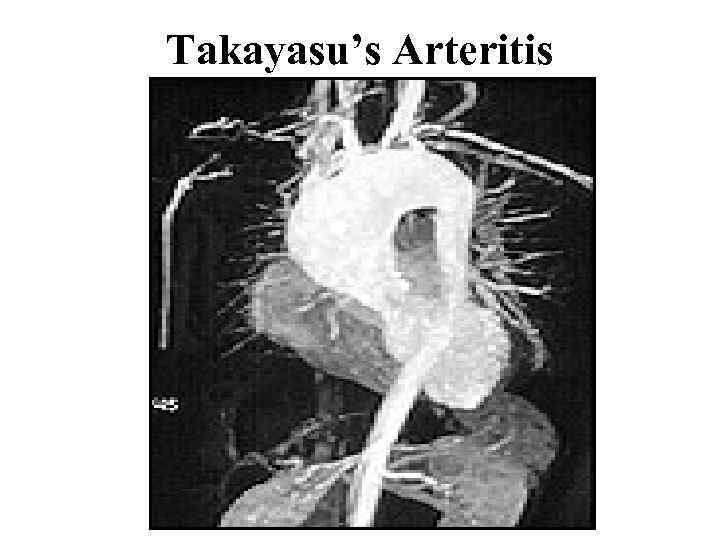
Takayasu’s Arteritis
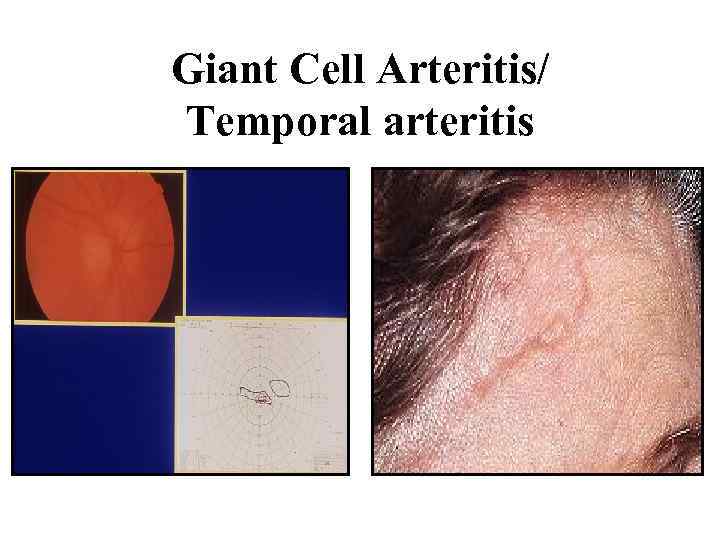
Giant Cell Arteritis/ Temporal arteritis
GCA • Medial and large vessels vasculitis – Branches of carotid artery – Temporal arteries • Strong association with PMR (50%) – Morning stiffness – Shoulder’s and pelvic pain • Isolated PMR is associated with GCA in 20%
GCA/PMR • • Age >50 F>>M Rare in blacks 6 -30/100000 HLA DR 4, HLA DRB 1 IL-2, INF CD 4+ Panarteritis with mononuclear cells accumulation and giant cells, intimal proliferation • Ischemia of tissues
GCA • • • Fever Headache General signs PMR Scalp tenderness Jaw claudication Ischemic optic neuropathy, visual loss Visceral ischemia, strokes Aortic aneurisms, dissection Anemia High ESR Liver enzymes elevation
GCA • Diagnosis – US Doppler – TA biopsy • 14 days • Treatment – Cs (40 -60 mg/d ~1 months) – Aspirin – MTX • Follow up: ESR
PMR • Diagnosis – Shoulder and hip pain – Stiffness – High ESR – Absence of signs GCA • Treatment – Cs (20 mg/d)
Polyarteritis Nodosa (PAN) Incidence: 5 -9 to 80/1 000 Epidemiology: M: F=2 -3: 1, young patients Pathology: fibrinoid necrosis medium/small arteries, aneurysms formation, mononuclear cells and PMNC infiltration, lumen thrombosis, obliteration of the lumen, sparing of pulmonary arteries. Segmental lesions In kidney – arteritis without GN Primary or secondary (RA, Sjogren’s syndrome, SLE, Hepatitis B, Hepatitis C, HIV, FMF, hairy cell leukemia)
Polyarteritis Nodosa Clinical features: General: severe disease, weight loss, mild to high fever, malaise Musculo-skeletal (64%): arthralgia, asymmetric polyarthritis, myalgia Skin (43|%): palpable purpura, ulceration, ischemic necrosis Neural (50%): peripheral neuropathy, mononeuritis multiplex, CVA
Polyarteritis Nodosa GIT: abdominal pain, mesenteric thrombosis, peritonitis, bleeding Kidney (60%): hypertension, renal failure, proteinuria, hematuria – not glomerulonephritis, hemorrhage from microaneurisms Cardiac (36%): CHF, MI Eyes: retinal detachment, scleritis Genito-urinary (25%): testicular, ovarian pain
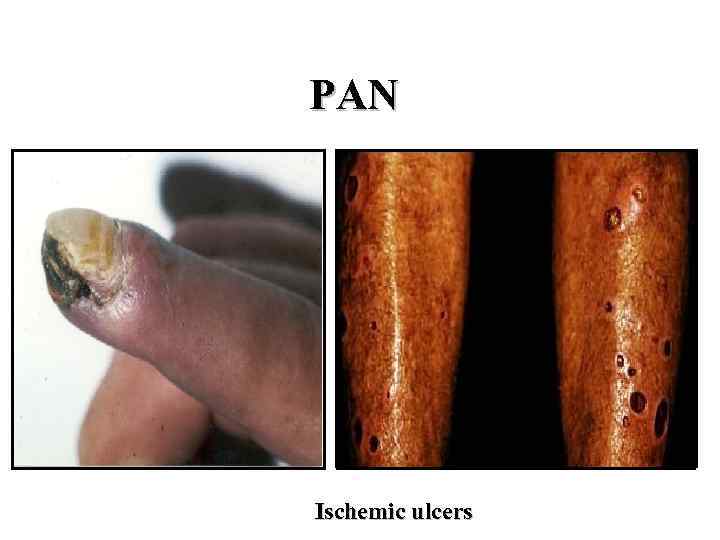
PAN Ischemic ulcers
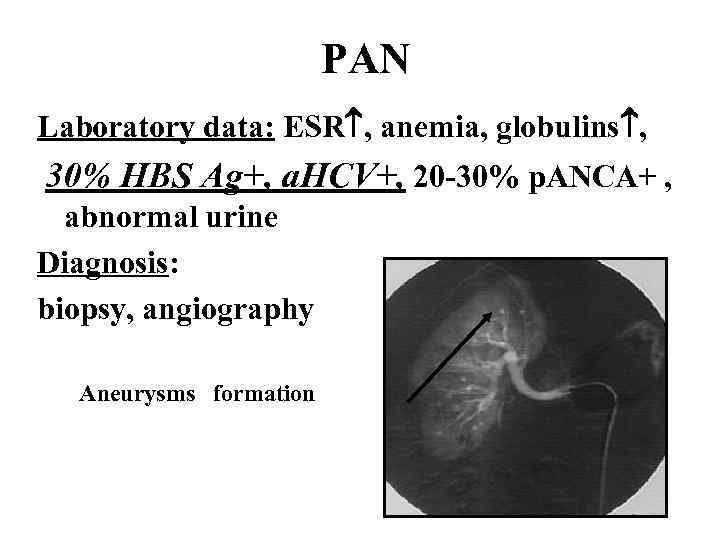
PAN Laboratory data: ESR , anemia, globulins , 30% HBS Ag+, a. HCV+, 20 -30% p. ANCA+ , abnormal urine Diagnosis: biopsy, angiography Aneurysms formation
PAN Prognosis: 5 year survival 15%-80% Treatment: Hepatitis neg: Steroids, Cyclophosphamide, Imuran, Methotrexate Hepatitis pos: Antiviral treatment (Interferon, plasmapheresis, Ribaverin), Cs, plasma exchange Relapse in 10%
Microscopic polyangiitis • • • Necrotizing vasculitis of small vessels M>F, >55 y GN (80%) Pulmonary capillaritis (12%) – hemorrhage Cardiac and GIT involvement Vascular lesions are similar to PAN, but in kidney – typical GN ESR, anemia, leukocytosis, thrombocytosis, abnormal urine, p. ANCA pos+++ Diagnosis: kidney biopsy (pauci-immune GN) Treatment: Cs, CYC Relapse in 34%
Churg-Strauss Syndrome Incidence: 1 -2/1 000 Epidemiology: M: F=2: 1 Pathology: • allergic necrotizing angiitis, eosinophils infiltration, extra-vascular granuloma formation • Small and medium sized vessels
Churg-Strauss Syndrome Prodromal period: bronchial asthma Second phase: • eosinophilia • Lóffler s-me - eosinophilic pneumonia • eosinophilic gastroenteritis Third phase: systemic vasculitis
Churg-Strauss Syndrome Clinical features: • General signs: fever, malaise, weight loss • Lung involvement: asthma, lung infiltrates, allergic rhinitis and sinusitis • GIT involvement: abdominal pain, diarrhea, bleeding • NS involvement: mononeuritis multiplex • Heart disease • Kidney involvement: GN • Skin: purpura • Arthritis
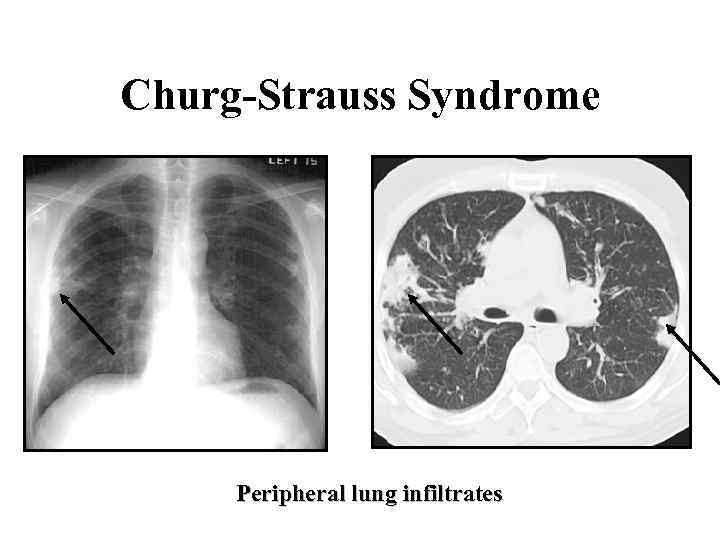
Churg-Strauss Syndrome Peripheral lung infiltrates
Churg-Strauss Syndrome Laboratory data: anemia, ESR , 5 000 -10 000 eosinophils/mm 3, Ig. E , p. ANCA + (70%) Diagnosis: biopsy Prognosis: 5 years survival-65% Treatment: Steroids, Cyclophosphamide, Imuran
Wegener’s Granulomatosis Incidence: 3/1 000 Epidemiology: M: F=1, 2: 1 Rare in blacks Age >40 y Pathology: necrotizing vasculitis of small arteies and veins, neutrophils accumulation and granuloma: upper airways (sinuses and nasopharyngs), lungs, kidney (pauci-immune GN no granuloma) INF, TNF, CD 4+ (Th 1 type) c. ANCA
Wegener’s Granulomatosis • General signs: fever, malaise, weight loss • Upper Respiratory Tract (95%): sinusitis, otitis media, nasal ulceration, septal perforation, subglottic stenosis Often Staph aureus • Low Respiratory Tract (80%): Pulmonary infiltrates, nodules, cavities (cough, dyspnea, hemopthysis), bronchiectasia • Kidney (75%): Glomerulonephritis, hypertension, renal failure
Wegener’s Granulomatosis • • • Purpura (45%) Necrotic ulcers Arthritis (50 -70%) Eyes (52%): orbital/periorbital mass and damage, scleritis, vasculitis, NS: peripheral neuropathy, central (33%) Heart (8%): pericarditis, CHF, MI, arrhythmias DVT and PE more then in healthy
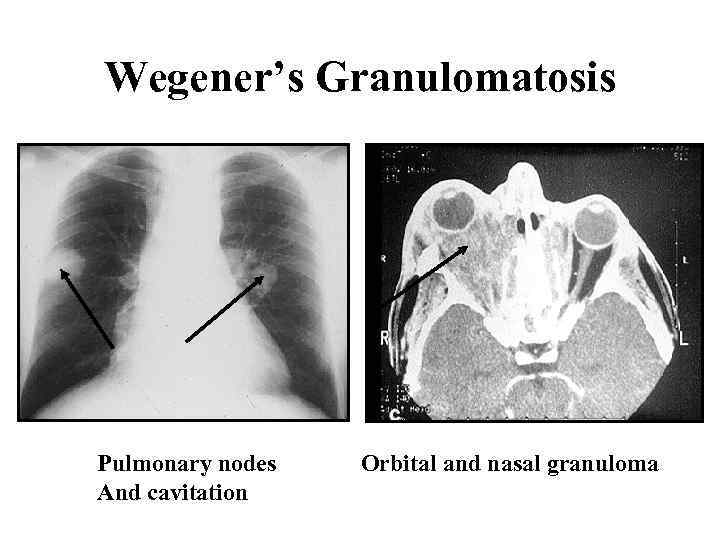
Wegener’s Granulomatosis Pulmonary nodes And cavitation Orbital and nasal granuloma
Wegener’s Granulomatosis Laboratory data: leukocytosis, anemia, ESR , c. ANCA + (90%), abnormal urine, RF+, thrombocytosis Diagnosis: nasal biopsy (granuloma), open lung biopsy (granuloma and vasculitis) Renal biopsy is not specific
Wegener’s Granulomatosis Prognosis: 5 years survival - 50 -75% Progressive renal failure Late organ damage Co-morbidities Cancer (bladder) Follow up: clinically, ANCA? ? ? Treatment: CYC (oral/IV) and Cs, Imuran, MTX, MMF, Trimethoprim Sulfamethoxazole (Resprim) Biological (RTX+, ETN-)
Henoch-Schőnlein Purpura Incidence: 4 -10/100 000 Epidemiology: M: F=1, 2: 1, age 4 -14 years Pathogenesis: IC vasculitis (Drugs? Infections? ) Pathology: small vessels necrotizing leukocytoclastic vasculitis, fibrinoid necrosis, IC, Ig. A and C 3 deposition (skin, gut, kidney [glomerrular& tubular]), MNC infiltration
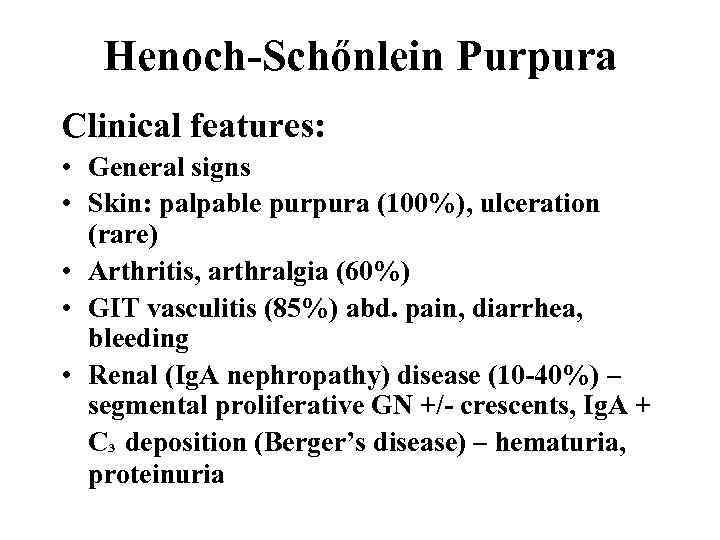
Henoch-Schőnlein Purpura Clinical features: • General signs • Skin: palpable purpura (100%), ulceration (rare) • Arthritis, arthralgia (60%) • GIT vasculitis (85%) abd. pain, diarrhea, bleeding • Renal (Ig. A nephropathy) disease (10 -40%) – segmental proliferative GN +/- crescents, Ig. A + C³ deposition (Berger’s disease) – hematuria, proteinuria
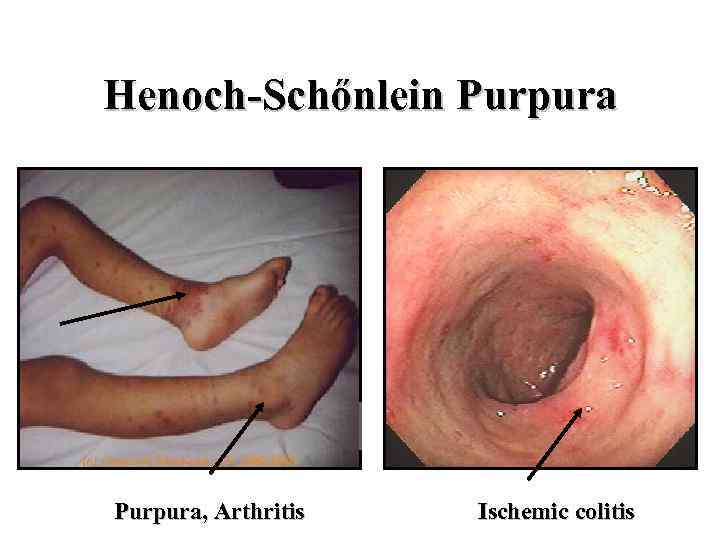
Henoch-Schőnlein Purpura, Arthritis Ischemic colitis
Henoch-Schőnlein Purpura Laboratory data: elevated ESR/CRP, leukocytosis, mild anemia, hematuria, high Ig. A Diagnosis: clinical +/- biopsy Prognosis: good (except severe GIT vasculitis and Ig. A nephropathy) Treatment: rest, tratement of underlying disease, NSAID, Cs, CYC – only in severe internal organ involvement
Essential Mixed Cryoglobulinemia • • Cryo – cold-precipitable Ig (mono/polyclonal) Systemic signs Primary - rare Secondary in most cases
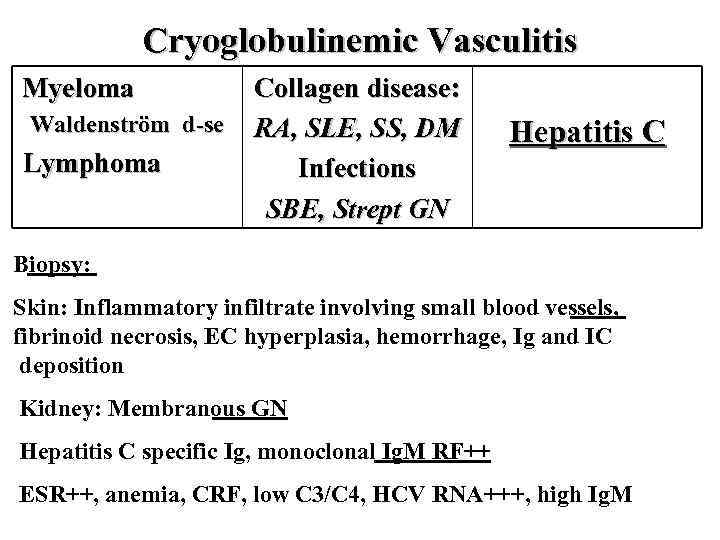
Cryoglobulinemic Vasculitis Myeloma Waldenström d-se Lymphoma Collagen disease: RA, SLE, SS, DM Infections SBE, Strept GN Hepatitis C Biopsy: Skin: Inflammatory infiltrate involving small blood vessels, fibrinoid necrosis, EC hyperplasia, hemorrhage, Ig and IC deposition Kidney: Membranous GN Hepatitis C specific Ig, monoclonal Ig. M RF++ ESR++, anemia, CRF, low C 3/C 4, HCV RNA+++, high Ig. M
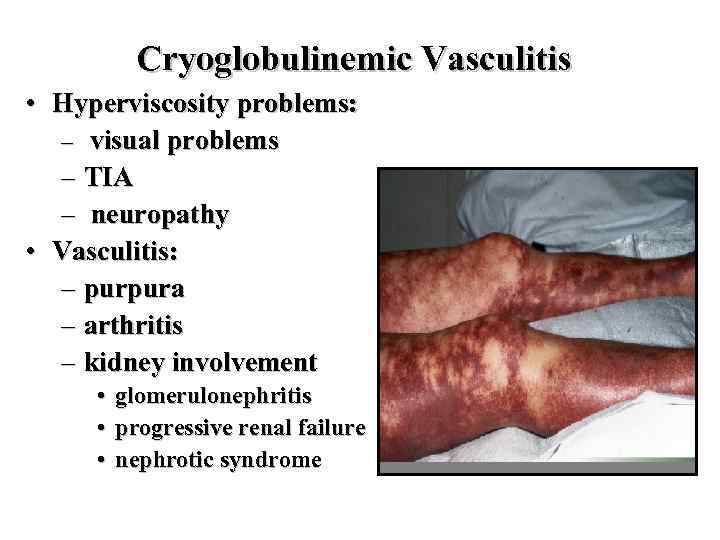
Cryoglobulinemic Vasculitis • Hyperviscosity problems: – visual problems – TIA – neuropathy • Vasculitis: – purpura – arthritis – kidney involvement • • • glomerulonephritis progressive renal failure nephrotic syndrome
Cryoglobulinemic Vasculitis Prognosis: poor, depends on viremia Treatment: plasmapheresis, antiviral therapy (Ribaverin + Interferon ) Cs = CYC
Behcet’s Disease Epidemiology: Japan, Meddle East (Silk rood) Family penetration Clinical feature: • Oral aphthous ulcers (100%) – 3/year • Genital ulcerations (80%) • Eye inflammation (65%)-anterior/posterior uveitis, retinal vasculitis • Skin inflammation (70%)-(folliculitis-like, acnelike, erythema nodosum-like) • Vasculitis (arterial-CNS, venous – thrombosis superficial and deep)
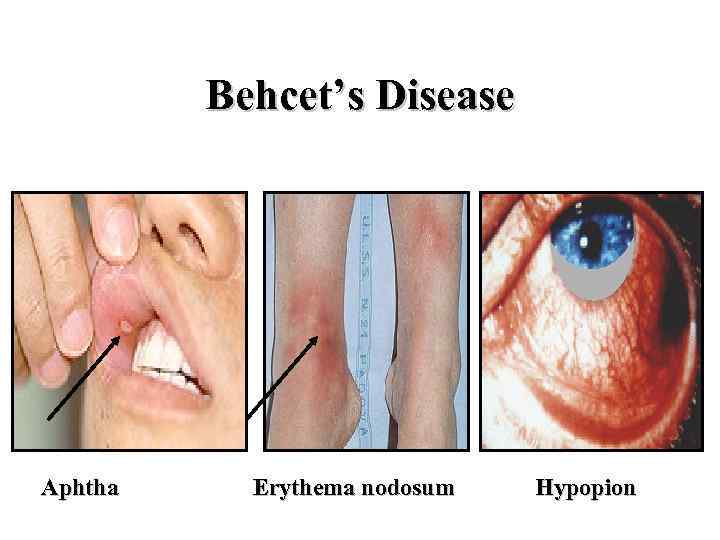
Behcet’s Disease Aphtha Erythema nodosum Hypopion
Behcet’s Disease Laboratory data: HLA B 51 pos. Pathergy skin test Prognosis: serious in uveitis - blindness, CNS vasculitis, thrombosis Treatment: Colchicine CS +/- MTX, Imuran, Salazopyrine CS +Neoral Thalidomide Anticoagulants
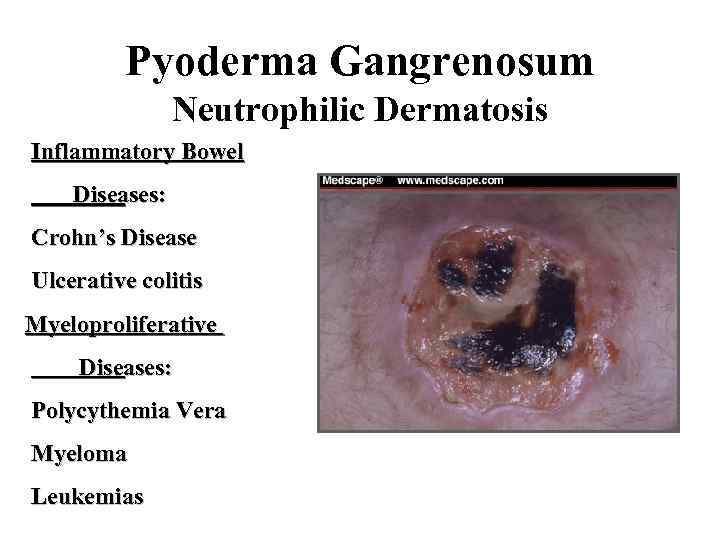
Pyoderma Gangrenosum Neutrophilic Dermatosis Inflammatory Bowel Diseases: Crohn’s Disease Ulcerative colitis Myeloproliferative Diseases: Polycythemia Vera Myeloma Leukemias
VASCULITIS for russians 2003.ppt