72ad3ab648f28448ded8032949fc07bf.ppt
- Количество слайдов: 38
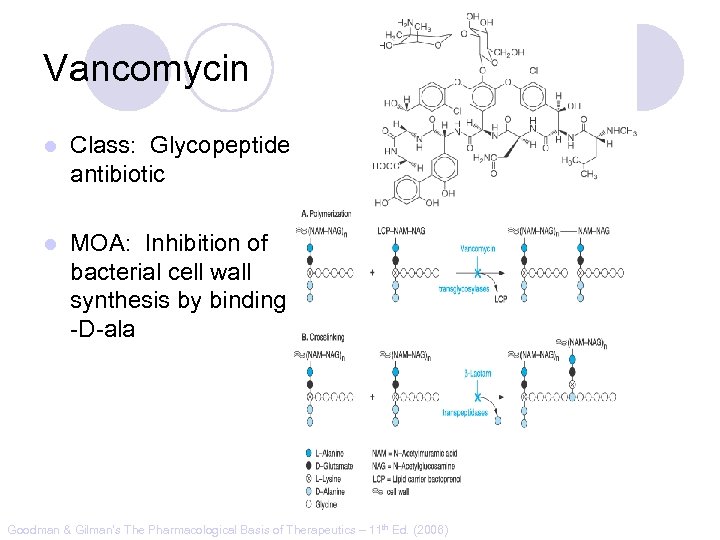
Vancomycin l Class: Glycopeptide antibiotic l MOA: Inhibition of bacterial cell wall synthesis by binding D-ala -D-ala Goodman & Gilman’s The Pharmacological Basis of Therapeutics – 11 th Ed. (2006)
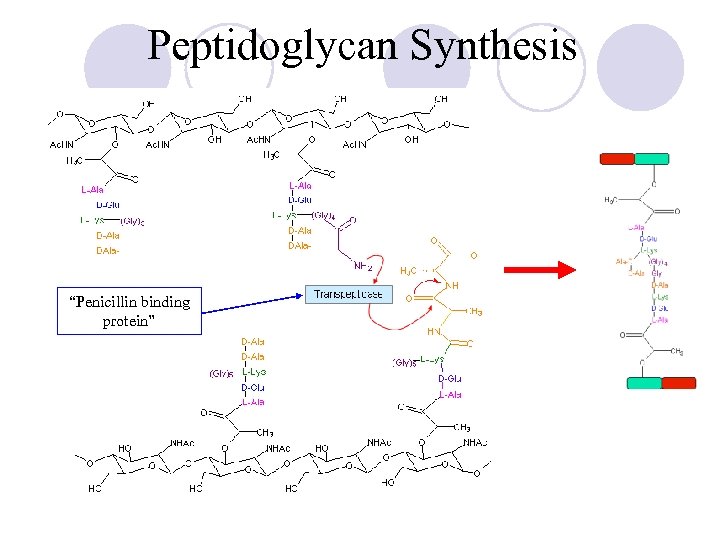
Peptidoglycan Synthesis “Penicillin binding protein”
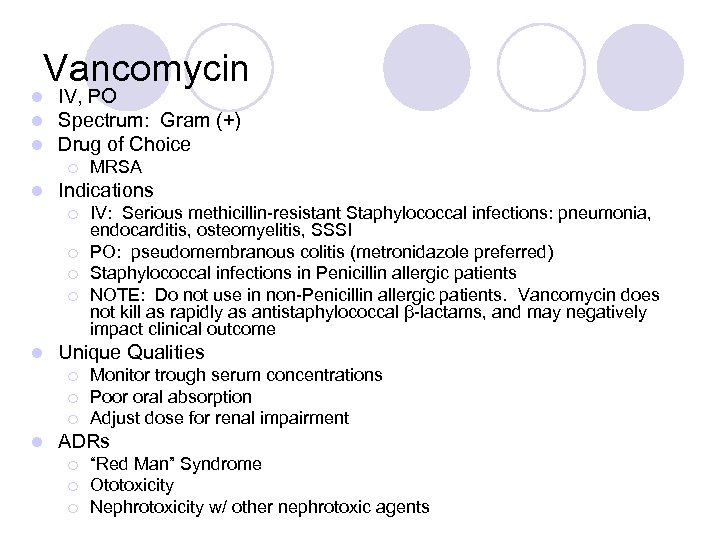
Vancomycin l l l IV, PO Spectrum: Gram (+) Drug of Choice ¡ l Indications ¡ ¡ l IV: Serious methicillin-resistant Staphylococcal infections: pneumonia, endocarditis, osteomyelitis, SSSI PO: pseudomembranous colitis (metronidazole preferred) Staphylococcal infections in Penicillin allergic patients NOTE: Do not use in non-Penicillin allergic patients. Vancomycin does not kill as rapidly as antistaphylococcal β-lactams, and may negatively impact clinical outcome Unique Qualities ¡ ¡ ¡ l MRSA Monitor trough serum concentrations Poor oral absorption Adjust dose for renal impairment ADRs ¡ ¡ ¡ “Red Man” Syndrome Ototoxicity Nephrotoxicity w/ other nephrotoxic agents
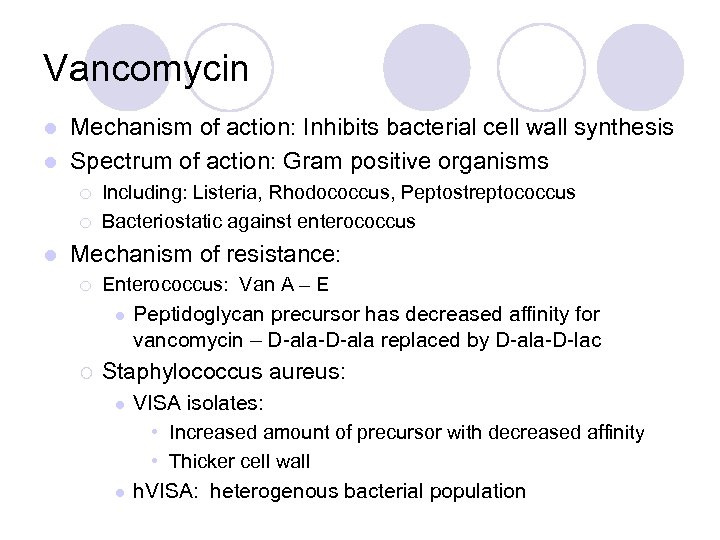
Vancomycin Mechanism of action: Inhibits bacterial cell wall synthesis l Spectrum of action: Gram positive organisms l ¡ ¡ l Including: Listeria, Rhodococcus, Peptostreptococcus Bacteriostatic against enterococcus Mechanism of resistance: ¡ Enterococcus: Van A – E l ¡ Peptidoglycan precursor has decreased affinity for vancomycin – D-ala-D-ala replaced by D-ala-D-lac Staphylococcus aureus: l l VISA isolates: • Increased amount of precursor with decreased affinity • Thicker cell wall h. VISA: heterogenous bacterial population
Vancomycin l Dose: ¡ Based on total body weight and renal function ¡ 15 – 20 mg/kg ¡ Normal renal function: q 12 dosing l Goal trough concentrations: ¡ 10 – 15 mcg/m. L: bacteremia, skin and soft tissue infections ¡ 15 – 20 mcg/m. L: osteomyelitis, meningitis, pneumonia
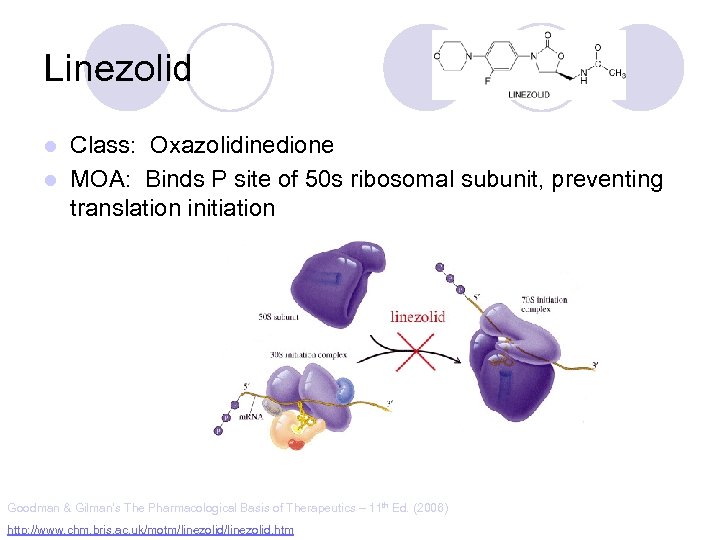
Linezolid Class: Oxazolidinedione l MOA: Binds P site of 50 s ribosomal subunit, preventing translation initiation l Goodman & Gilman’s The Pharmacological Basis of Therapeutics – 11 th Ed. (2006) http: //www. chm. bris. ac. uk/motm/linezolid. htm
Linezolid l l IV, PO Gram (+) Indications ¡ ¡ l Unique Qualities ¡ ¡ ¡ l VRE (E. faecium) Nosocomial pneumonia (S. aureus) Community-acquired pneumonia (S. pneumoniae) c. SSSI (S. aureus) F~100%, IV=PO Reserve use for treatment of multiple drug resistant strains No CYP interaction ADRs ¡ ¡ ¡ Generally well tolerated w/ minor SE in short term Rx Myelosuppression: anemia, leukopenia, pancytopenia, thrombocytopenia Peripheral and optic neuropathy
Linezolid l Penetration: ¡ ¡ ¡ Plasma Pulmonary lining Blister fluid > MIC 90 for Staphylococcus Dose (IV or PO): 600 mg Q 12 H l Drug-drug interactions: l ¡ ¡ Non-selective inhibitor of MAO Possible serotonergic or adrenergic interaction with antidepressant medications (incidence < 1%)
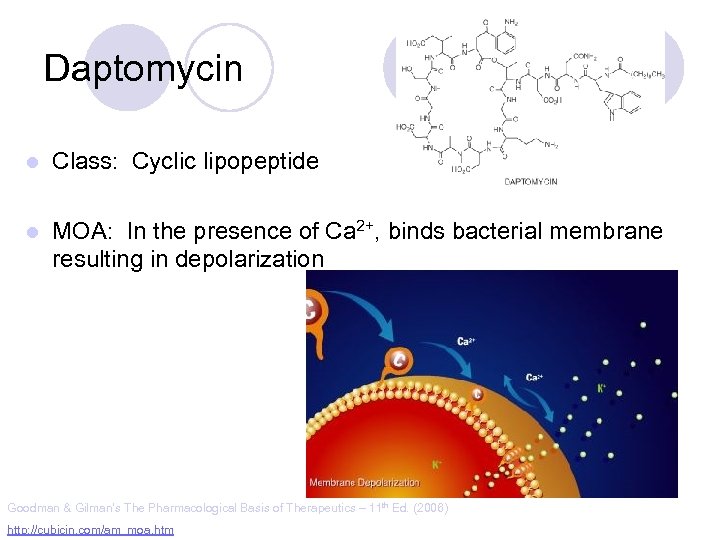
Daptomycin l Class: Cyclic lipopeptide l MOA: In the presence of Ca 2+, binds bacterial membrane resulting in depolarization Goodman & Gilman’s The Pharmacological Basis of Therapeutics – 11 th Ed. (2006) http: //cubicin. com/am_moa. htm
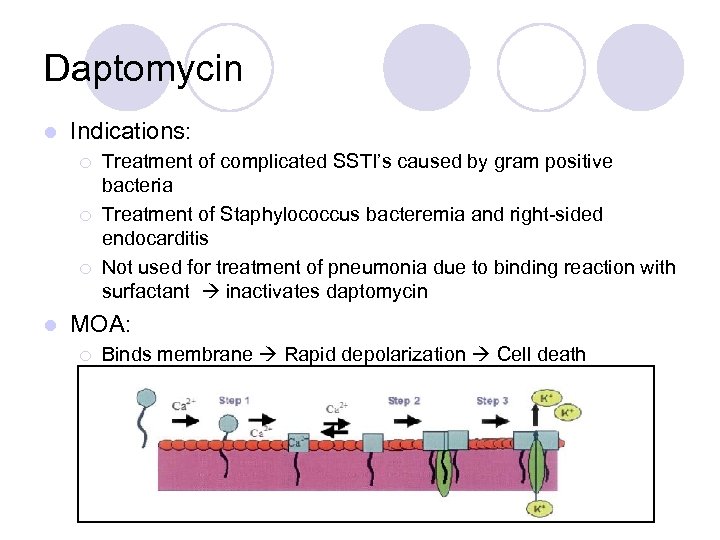
Daptomycin l Indications: ¡ ¡ ¡ l Treatment of complicated SSTI’s caused by gram positive bacteria Treatment of Staphylococcus bacteremia and right-sided endocarditis Not used for treatment of pneumonia due to binding reaction with surfactant inactivates daptomycin MOA: ¡ Binds membrane Rapid depolarization Cell death
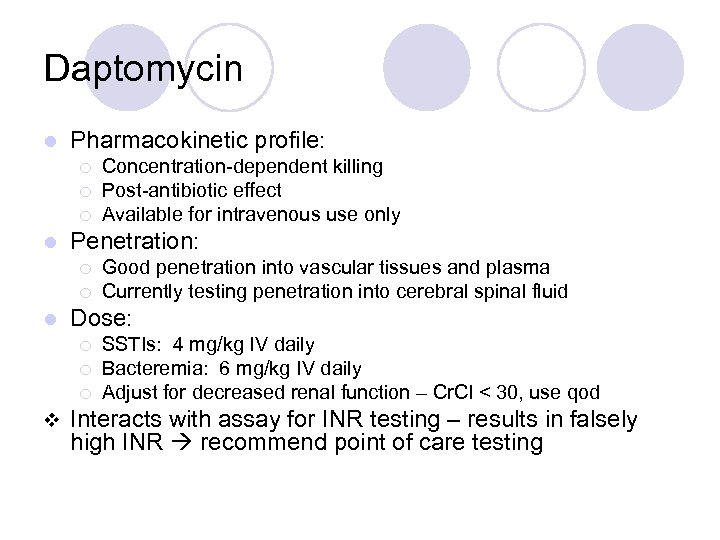
Daptomycin l Pharmacokinetic profile: ¡ ¡ ¡ l Penetration: ¡ ¡ l Good penetration into vascular tissues and plasma Currently testing penetration into cerebral spinal fluid Dose: ¡ ¡ ¡ v Concentration-dependent killing Post-antibiotic effect Available for intravenous use only SSTIs: 4 mg/kg IV daily Bacteremia: 6 mg/kg IV daily Adjust for decreased renal function – Cr. Cl < 30, use qod Interacts with assay for INR testing – results in falsely high INR recommend point of care testing
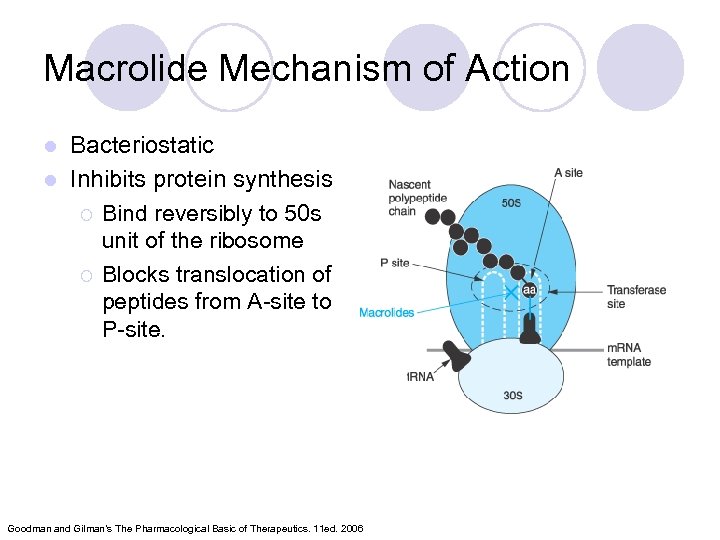
Macrolide Mechanism of Action Bacteriostatic l Inhibits protein synthesis ¡ Bind reversibly to 50 s unit of the ribosome ¡ Blocks translocation of peptides from A-site to P-site. l Goodman and Gilman’s The Pharmacological Basic of Therapeutics. 11 ed. 2006
Macrolides l Achieve higher tissue than plasma concentrations ¡ Penetrate into respiratory, tonsillar, and prostate tissues ¡ Also l l penetrate into PMN leukocytes Important for Atypicals like: Chlamydia and Legionella species PD: Time the bacteria is exposed to therapeutic concentrations above the MIC best predicts efficacy – time dependent killing
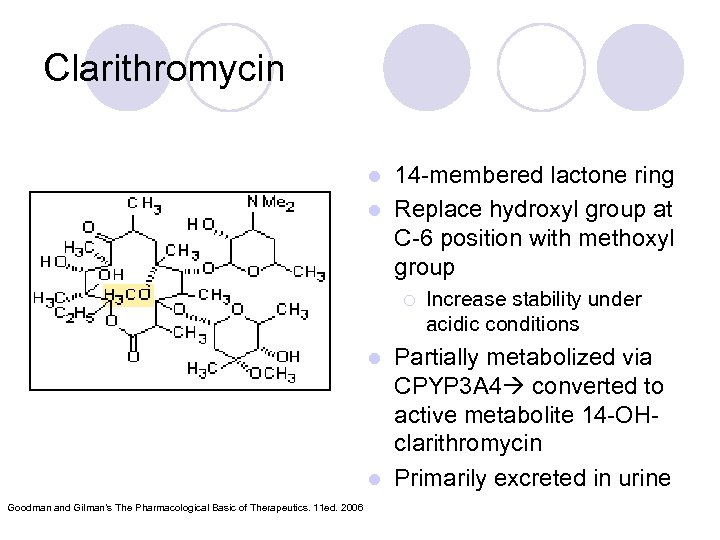
Clarithromycin 14 -membered lactone ring l Replace hydroxyl group at C-6 position with methoxyl group l ¡ Increase stability under acidic conditions Partially metabolized via CPYP 3 A 4 converted to active metabolite 14 -OHclarithromycin l Primarily excreted in urine l Goodman and Gilman’s The Pharmacological Basic of Therapeutics. 11 ed. 2006
Clarithromycin l l l PO: Biaxin® 250 -500 mg q 12 hours; Biaxin XL® 1000 mg qday Spectrum of Activity: Gram (+) and Gram (-) Indications: otitis media, CAP, pharyngitis/tonsillitis, sinusitis, l Drug Interactions: Substrate of CYP 3 A 4 and Inhibits CPY 3 A 4(major) CYP 1 A 2 (weak) uncomplicated skin infections, prevention of MAC, duodenal ulcer disease ¡ S. aures, S. pyogenes, S. pneumoniae, Mycobacterium avium complex ¡ C. pneumoniae, C. trachomatis, L. pneumoniae ¡ H. influenzae, H. pylori ¡ l Renal Adjustments: ¡ l Cr. Cl < 30 ml/min: ½ the normal dose or double the dosing interval ADR: ¡ ¡ l Theophylline, statins, digoxin, warfarin, cyclosporine Prolongs the QT interval – use with caution in CAD N/V, diarrhea, headache Counseling Points: ¡ Take XL formulation with food; do not chew or crush
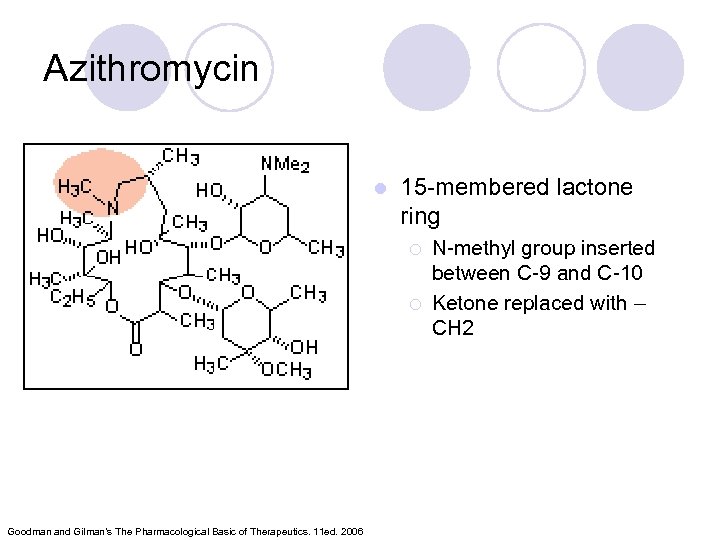
Azithromycin l 15 -membered lactone ring ¡ ¡ Goodman and Gilman’s The Pharmacological Basic of Therapeutics. 11 ed. 2006 N-methyl group inserted between C-9 and C-10 Ketone replaced with – CH 2
Azithromycin l PO, IV Azithromyicn: 500 mg x day 1 then 250 mg x day 2 -5 ¡ STDs: C. trachomatis: 1 g x 1; N. gonorrheae: 2 g x 1 l Spectrum of Activity: Less Gram (+), increased Gram (-) l Indications: otitis media, pharyngitis/tonsillitis, upper and lower respiratory tract infections, skin and skin structure, CAP, PID, STDs ¡ S. aures, S. pneumoniae, H. influenzae, Mycobacterium avium complex ¡ C. trachomatis, M. catarrhalis, M. pneumonia, N. gonorrheae, Chlamydia pneumoniae l Drug Interactions: not as significant as other macrolides ¡ Most documented with cyclosporine and tacrolimus ¡ l Unique Characteristics: ¡ ¡ l T ½ of immediate release: 68 -72 hours; extended release: 59 hours Caution in patients with Cr. Cl < 10 ml/min ADRs: ¡ Generally well-tolerated, may cause GI upset
Macrolide Resistance Decrease of permeation of drug through the cell membrane, or drug efflux pumps l Methylase modifies the ribosomal target l Hydrolysis of macrolides by endogenous esterase l
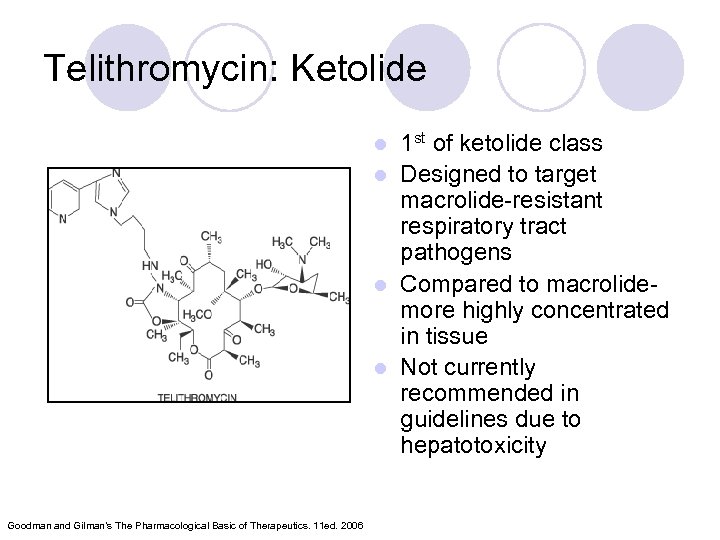
Telithromycin: Ketolide 1 st of ketolide class l Designed to target macrolide-resistant respiratory tract pathogens l Compared to macrolidemore highly concentrated in tissue l Not currently recommended in guidelines due to hepatotoxicity l Goodman and Gilman’s The Pharmacological Basic of Therapeutics. 11 ed. 2006
Telithromycin (Ketek ®) PO: CAP-800 mg qday x 7 -10 days Spectrum of activity: Gram (+) and Gram (-) Indications: acute exacerbations of chronic bronchitis, acute sinusitis, CAP ¡ Staphylococci, S. pneumoniae (DRSP), H. influenzae, Moraxella catarrhalis, mycoplasma, chlamydia, Legionella l Drug Interactions: Inhibits CYP 2 D 69(weak) 3 A 4(strong): ¡ Multiple Drug Interactions l ADRs ¡ Hepatotoxicity: Monitor LFTs, sxs of liver failure ¡ QT prolongation ¡ N/V: take with or without food ¡ Dose adjust for renal insufficiency l l l Goodman and Gilman’s The Pharmacological Basic of Therapeutics. 11 ed. 2006
Clindamycin l Class: Lincosamide l Mechanism of Action: Binds exclusively to the 50 S subunit of bacterial ribosomes and suppress protein synthesis
Clindamycin l Trade names: Cleocin ®, Clindesse®, Clindagel ®, l Delivery forms: ¡ ¡ ¡ capsules: 75, 150, 300 mg; granules for oral solution 75 mg/5 ml; injection 150 mg/ml; vaginal cream 2%; vaginal suppositories 100 mg; Clindamax ®, Evoclin ® ¡ ¡ topical gel 1%; topical lotion 1%; topical solution 1%; foam 1%
Clindamycin l Indications: Serious infections caused by susceptible anaerobic bacteria l Dosing: ¡ ¡ l Off-label indications: CNS toxoplasmosis in AIDS patients in addition to pyrimethamine; chlamydia infections in women; bacterial vaginosis due to Gardnerella vaginalis l Instructions: ¡ l Adults: 150 -450 mg Q 6 hrs Children: 8 -20 mg/kg/day divided TID-QID Take with full glass of water Warning: ¡ Pseudomembranous colitis
Clindamycin l Precautions: ¡ ¡ ¡ Renal impairment/liver disease Elderly Meningitis GI disease Superinfections Pregnancy Category B l Drug Interactions: ¡ ¡ l Erythromycin Neuromuscular blocking agents ADRs: ¡ Dermatologic, GI, Hypersenstivity
Aminoglycosides • Bactericidal inhibitors of protein synthesis • Concentration dependent bacteria killing • Postantibiotic effect • Major limitation of use is the serious toxicity • • Nephrotoxicity Ototoxicity
Aminoglycosides: Indications • Primarily against aerobic, gram negative bacilli • Activity against gram positive bacteria limited • Synergistic effect against “sensitive” (highlevel) streptococci and enterococci when used with a cell wall active agent
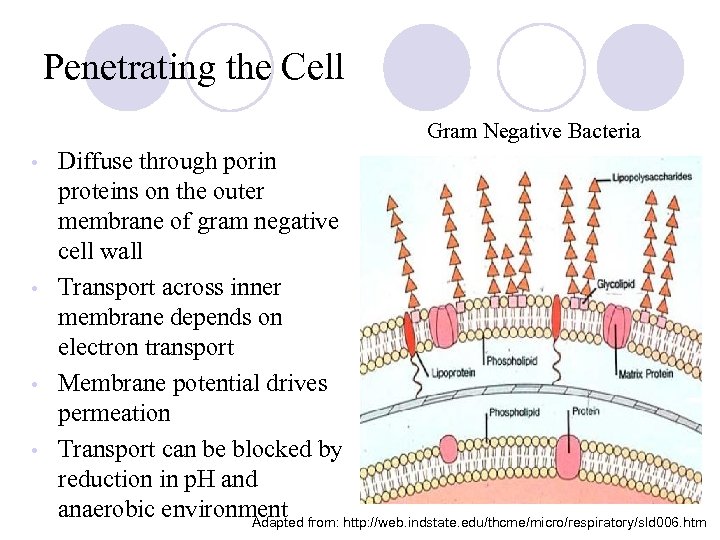
Penetrating the Cell Gram Negative Bacteria Diffuse through porin proteins on the outer membrane of gram negative cell wall • Transport across inner membrane depends on electron transport • Membrane potential drives permeation • Transport can be blocked by reduction in p. H and anaerobic environment from: http: //web. indstate. edu/thcme/micro/respiratory/sld 006. htm Adapted •
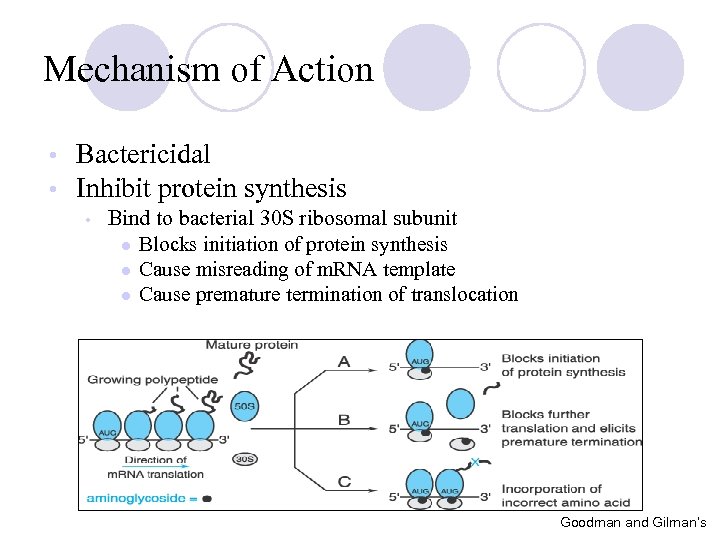
Mechanism of Action • • Bactericidal Inhibit protein synthesis • Bind to bacterial 30 S ribosomal subunit l Blocks initiation of protein synthesis l Cause misreading of m. RNA template l Cause premature termination of translocation Goodman and Gilman’s
Aminoglycosides: Resistance Modes of resistance • Decreased permeation of aminoglycosides • Low affinity for bacterial ribosome • Drug inactivation by microbial enzymes • • Important clinically Amikacin is less vulnerable
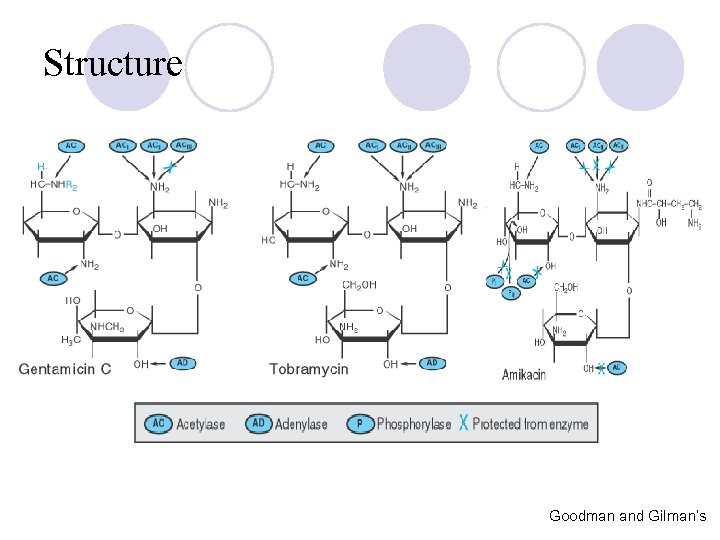
Structure Goodman and Gilman’s
Aminoglycosides l Resistance: Intrinsic vs. Acquired ¡ Intrinsic: Anaerobes: lack active electron transport chain to cross membrane l Mutation at 16 s r. RNA (ie TB) l ¡ Acquired: Efflux: seen in Pseudomonas l Decreased transmembrane potential: seen in Enterococcus l
Aminoglycosides Distribution: ¡ Freely into the vascular space ¡ Interstitial spaces of most tissues ¡ Volume of distribution increases in edematous states and decreases in obese patients (on L/kg basis) l Decreased concentrations: ¡ Bronchial secretions, CSF, biliary tract, synovial fluid, and in the eye l Excreted by the kidneys l Half-life: 1. 5 to 3. 5 hours l
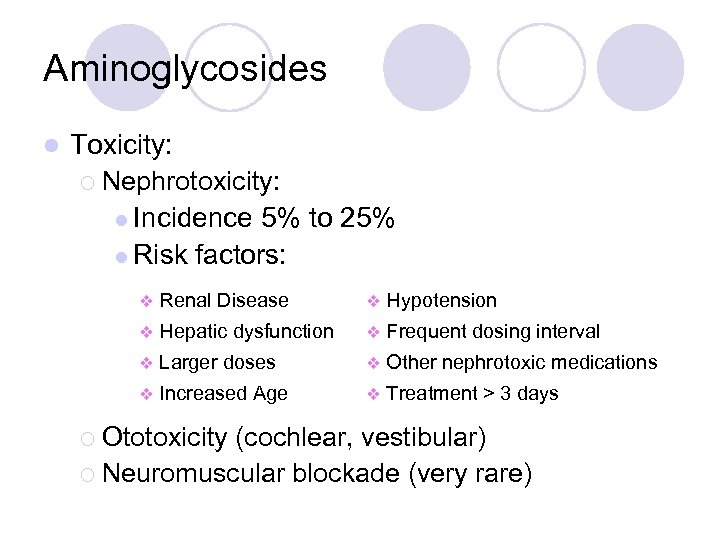
Aminoglycosides l Toxicity: ¡ Nephrotoxicity: l Incidence 5% to 25% l Risk factors: v Renal Disease v Hypotension v Hepatic dysfunction v Frequent dosing interval v Larger doses v Other nephrotoxic medications v Increased Age v Treatment > 3 days ¡ Ototoxicity (cochlear, vestibular) ¡ Neuromuscular blockade (very rare)
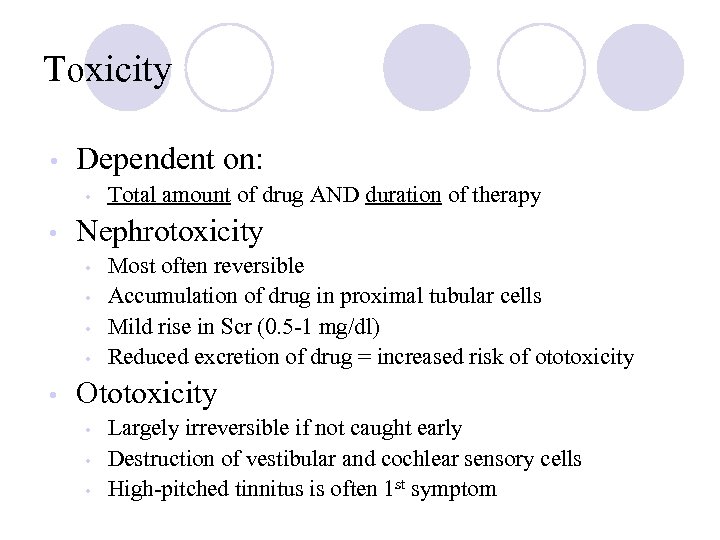
Toxicity • Dependent on: • • Nephrotoxicity • • • Total amount of drug AND duration of therapy Most often reversible Accumulation of drug in proximal tubular cells Mild rise in Scr (0. 5 -1 mg/dl) Reduced excretion of drug = increased risk of ototoxicity Ototoxicity • • • Largely irreversible if not caught early Destruction of vestibular and cochlear sensory cells High-pitched tinnitus is often 1 st symptom
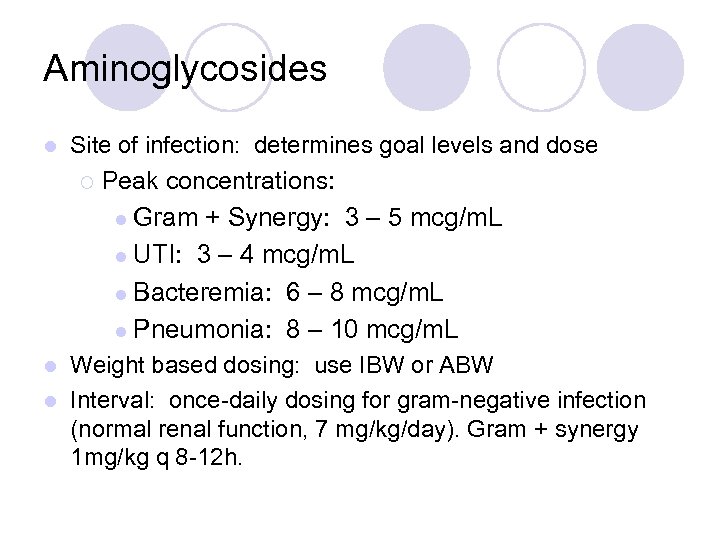
Aminoglycosides l Site of infection: determines goal levels and dose ¡ Peak concentrations: l Gram + Synergy: 3 – 5 mcg/m. L l UTI: 3 – 4 mcg/m. L l Bacteremia: 6 – 8 mcg/m. L l Pneumonia: 8 – 10 mcg/m. L Weight based dosing: use IBW or ABW l Interval: once-daily dosing for gram-negative infection (normal renal function, 7 mg/kg/day). Gram + synergy 1 mg/kg q 8 -12 h. l
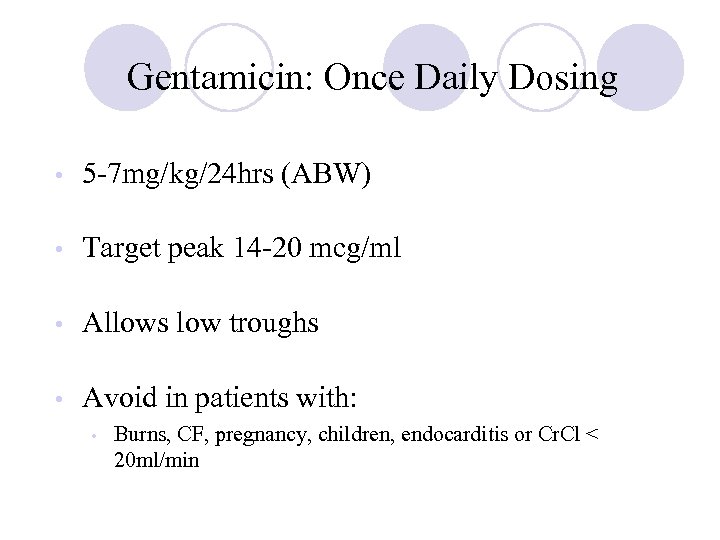
Gentamicin: Once Daily Dosing • 5 -7 mg/kg/24 hrs (ABW) • Target peak 14 -20 mcg/ml • Allows low troughs • Avoid in patients with: • Burns, CF, pregnancy, children, endocarditis or Cr. Cl < 20 ml/min
Tobramycin • Antimicrobial activity and PK properties very similar to gentamicin • • Superior activity against P. aeruginosa Less active than gentamicin against enterococci • Can be given IV or IM • Dosage and serum levels are same as gentamicin
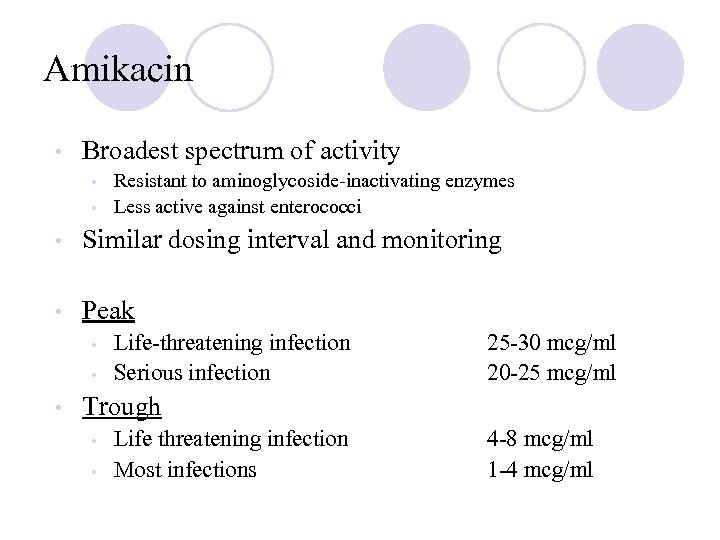
Amikacin • Broadest spectrum of activity • • Resistant to aminoglycoside-inactivating enzymes Less active against enterococci • Similar dosing interval and monitoring • Peak • • • Life-threatening infection Serious infection 25 -30 mcg/ml 20 -25 mcg/ml Trough • • Life threatening infection Most infections 4 -8 mcg/ml 1 -4 mcg/ml
72ad3ab648f28448ded8032949fc07bf.ppt