f62ddf6c2ed2a4963331dba2ee65e721.ppt
- Количество слайдов: 29

 Value Over Volume: Paying for Quality March 28, 2012 Ellen Andrews, Ph. D CT Health Policy Project CSG/ERC
Value Over Volume: Paying for Quality March 28, 2012 Ellen Andrews, Ph. D CT Health Policy Project CSG/ERC
 Health care spending health costs vs. state budgets, US National health exp. 20 state budgets nominal increase 10 5 2009 2007 2005 2003 2001 1999 1997 1995 1993 1991 1989 1987 1985 1983 1981 0 1979 annual % change 15 -5 Sources: National Health Accounts, CMS, accessed 3/20/11, Fiscal Survey of States, NASBO, Fall 2010
Health care spending health costs vs. state budgets, US National health exp. 20 state budgets nominal increase 10 5 2009 2007 2005 2003 2001 1999 1997 1995 1993 1991 1989 1987 1985 1983 1981 0 1979 annual % change 15 -5 Sources: National Health Accounts, CMS, accessed 3/20/11, Fiscal Survey of States, NASBO, Fall 2010
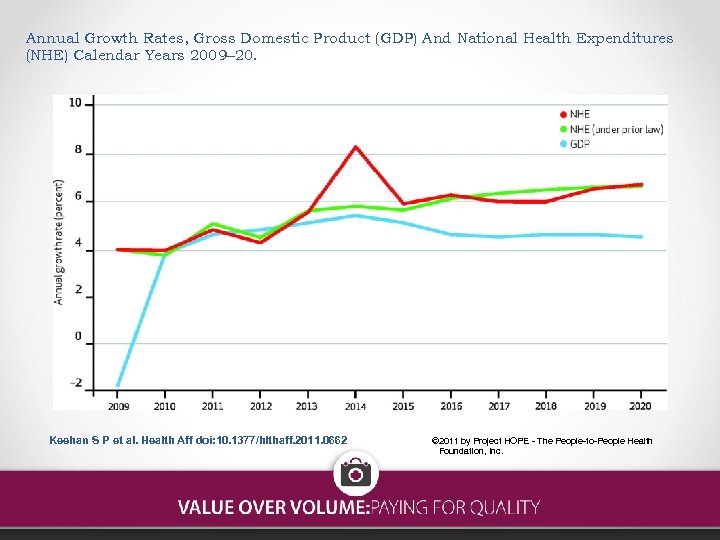 Annual Growth Rates, Gross Domestic Product (GDP) And National Health Expenditures (NHE) Calendar Years 2009– 20. Keehan S P et al. Health Aff doi: 10. 1377/hlthaff. 2011. 0662 © 2011 by Project HOPE - The People-to-People Health Foundation, Inc.
Annual Growth Rates, Gross Domestic Product (GDP) And National Health Expenditures (NHE) Calendar Years 2009– 20. Keehan S P et al. Health Aff doi: 10. 1377/hlthaff. 2011. 0662 © 2011 by Project HOPE - The People-to-People Health Foundation, Inc.
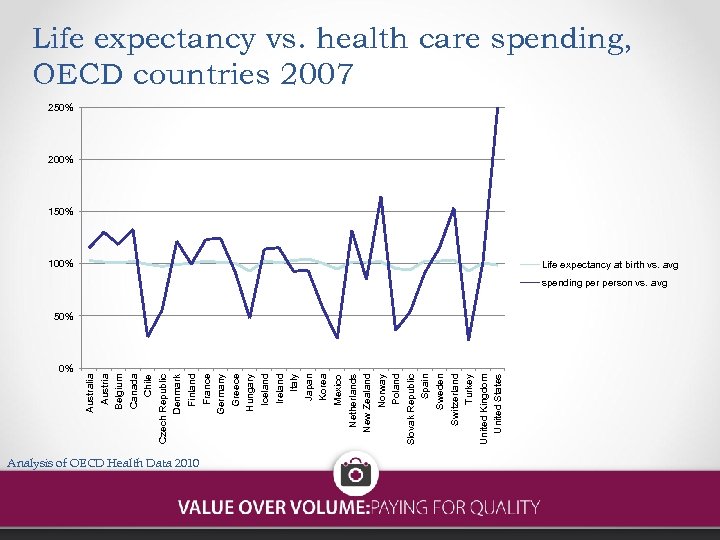 0% Australia Austria Belgium Canada Chile Czech Republic Denmark Finland France Germany Greece Hungary Iceland Ireland Italy Japan Korea Mexico Netherlands New Zealand Norway Poland Slovak Republic Spain Sweden Switzerland Turkey United Kingdom United States Life expectancy vs. health care spending, OECD countries 2007 250% 200% 150% 100% Life expectancy at birth vs. avg spending person vs. avg 50% Analysis of OECD Health Data 2010
0% Australia Austria Belgium Canada Chile Czech Republic Denmark Finland France Germany Greece Hungary Iceland Ireland Italy Japan Korea Mexico Netherlands New Zealand Norway Poland Slovak Republic Spain Sweden Switzerland Turkey United Kingdom United States Life expectancy vs. health care spending, OECD countries 2007 250% 200% 150% 100% Life expectancy at birth vs. avg spending person vs. avg 50% Analysis of OECD Health Data 2010
 We are all getting less recommended care than we should Source: RAND Compare
We are all getting less recommended care than we should Source: RAND Compare
 Quality question • Only 39% of American adults are confident that they can get safe, effective care when needed • Americans get only 55% of recommended care on average • One in three Americans reports getting unnecessary care or duplicate tests. • Almost one in five Medicare patients discharged from the hospital are readmitted within 30 days
Quality question • Only 39% of American adults are confident that they can get safe, effective care when needed • Americans get only 55% of recommended care on average • One in three Americans reports getting unnecessary care or duplicate tests. • Almost one in five Medicare patients discharged from the hospital are readmitted within 30 days
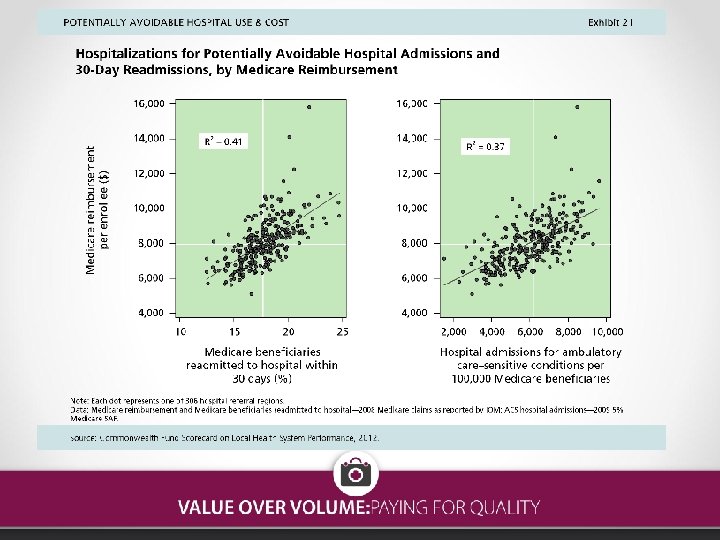
 Current incentives • Pay the same for high and low quality services • Consumers have no information and no incentive to choose higher quality/higher efficiency services or providers • Encourages overuse, misuse of services • Higher spending not correlated with higher quality • Higher spending not correlated with better patient satisfaction
Current incentives • Pay the same for high and low quality services • Consumers have no information and no incentive to choose higher quality/higher efficiency services or providers • Encourages overuse, misuse of services • Higher spending not correlated with higher quality • Higher spending not correlated with better patient satisfaction
 Fee-for-service misaligned incentives Fee for service encourages: More services Less coordination Incentives for duplication Few incentives for prevention Stifles innovation Only pays for selected services - not email, group visits, phone calls • No link to quality • Incentives to increase high profit services/patients and avoid low profit • • •
Fee-for-service misaligned incentives Fee for service encourages: More services Less coordination Incentives for duplication Few incentives for prevention Stifles innovation Only pays for selected services - not email, group visits, phone calls • No link to quality • Incentives to increase high profit services/patients and avoid low profit • • •
 Quality-based purchasing • Rewards better outcomes • Payments based on value -- quality balanced with cost • Data driven • Remove incentives for more services • Reward providing the right services to the right patient at the right time in the most effective setting • • Flexibility for providers to customize care Reward patient satisfaction Remove fragmentation and conflicting incentives Align provider, payer and consumer incentives to reward quality, effectiveness and efficiency
Quality-based purchasing • Rewards better outcomes • Payments based on value -- quality balanced with cost • Data driven • Remove incentives for more services • Reward providing the right services to the right patient at the right time in the most effective setting • • Flexibility for providers to customize care Reward patient satisfaction Remove fragmentation and conflicting incentives Align provider, payer and consumer incentives to reward quality, effectiveness and efficiency
 Consumers support quality-based purchasing • 96% of Americans feel it is important to have information about the quality of care provided by different doctors and hospitals • 89% feel it is important that they have information about the costs of care to them before they actually get care • 85% want public and private payers to reward high quality doctors and hospitals
Consumers support quality-based purchasing • 96% of Americans feel it is important to have information about the quality of care provided by different doctors and hospitals • 89% feel it is important that they have information about the costs of care to them before they actually get care • 85% want public and private payers to reward high quality doctors and hospitals
 Why should states implement VBP? • State employee groups usually one of largest groups in state – 42 states self-insure • Medicaid programs – covers one in five Americans • States regulate insurers, license providers, CON • Trusted source for consumer education, data collection, research • Public health collaborations • Innovators – medical home, HIT, coverage programs • Provider training – promote primary care, emphasis on accountability, transparency • Convener – can get people to the table, anti-trust protections
Why should states implement VBP? • State employee groups usually one of largest groups in state – 42 states self-insure • Medicaid programs – covers one in five Americans • States regulate insurers, license providers, CON • Trusted source for consumer education, data collection, research • Public health collaborations • Innovators – medical home, HIT, coverage programs • Provider training – promote primary care, emphasis on accountability, transparency • Convener – can get people to the table, anti-trust protections
 Options: Payment system overhaul • • Never events Transparency Pay for performance (P 4 P) Market share – tier and steer Shared savings Episodes of care, bundled payments Global capitation
Options: Payment system overhaul • • Never events Transparency Pay for performance (P 4 P) Market share – tier and steer Shared savings Episodes of care, bundled payments Global capitation
 Options: Transparency • Data reporting, definitions are a challenge • Report cards evolving, mixed results o Improving science of how to effectively convey information • Coalitions with other payers, providers for joint reporting o All payer data aggregation • State employee, Medicaid use in contracting • Moves providers to improve quality and/or reconsider pricing
Options: Transparency • Data reporting, definitions are a challenge • Report cards evolving, mixed results o Improving science of how to effectively convey information • Coalitions with other payers, providers for joint reporting o All payer data aggregation • State employee, Medicaid use in contracting • Moves providers to improve quality and/or reconsider pricing
 Options: P 4 P • • • Widespread, but mixed results Process vs. outcome measures Benchmarks vs. improvement Medicaid P 4 P in 28 states Federal Medicaid limits on incentive payments in risk -based systems Target health plans and/or providers Outcomes vs. process and teaching to the test/cookbooks Provider resistance, low Medicaid participation rates Coordinate and join with other payers to make payments salient to providers
Options: P 4 P • • • Widespread, but mixed results Process vs. outcome measures Benchmarks vs. improvement Medicaid P 4 P in 28 states Federal Medicaid limits on incentive payments in risk -based systems Target health plans and/or providers Outcomes vs. process and teaching to the test/cookbooks Provider resistance, low Medicaid participation rates Coordinate and join with other payers to make payments salient to providers
 Options: bundled payments • Also called episodes or buckets of care • One payment for full range of services associated with a specific event, e. g. knee replacement • Common now for physicians in general surgery and obstetrics, DRGs in Medicare • Similar to DRGs in Medicare • Places providers at some financial risk • Incentives to coordinate care, nontraditional supports, reduce duplicate services • No incentive to prevent illness in the first place • ACA pilots for Medicare and Medicaid
Options: bundled payments • Also called episodes or buckets of care • One payment for full range of services associated with a specific event, e. g. knee replacement • Common now for physicians in general surgery and obstetrics, DRGs in Medicare • Similar to DRGs in Medicare • Places providers at some financial risk • Incentives to coordinate care, nontraditional supports, reduce duplicate services • No incentive to prevent illness in the first place • ACA pilots for Medicare and Medicaid
 Options: shared savings • Allow providers to “share” some part of reductions in cost per patient • To avoid incentives to deny care, tied to quality standards • Medicare demonstration had mixed results o Took five years to implement, with ten sophisticated groups o Quality improvements good o Did not reach expected savings targets • ACA includes more opportunities for Medicare and Medicaid • Medicare ASOs
Options: shared savings • Allow providers to “share” some part of reductions in cost per patient • To avoid incentives to deny care, tied to quality standards • Medicare demonstration had mixed results o Took five years to implement, with ten sophisticated groups o Quality improvements good o Did not reach expected savings targets • ACA includes more opportunities for Medicare and Medicaid • Medicare ASOs
 Options: Global payment rates • Massachusetts a leader, 20% of commercial payments • Pay one risk-adjusted rate for each patient to cover all their care – in and outpatient, LTC, rehab, drugs • Linked to Pay for Performance to ensure quality of care maintained, up to 10% of budget • Year One mixed results o Quality up for some measures, not others o All groups met savings targets and received rewards o Savings from reducing prices, shift to outpatient care, not reduced utilization o But total savings did not equal total bonuses
Options: Global payment rates • Massachusetts a leader, 20% of commercial payments • Pay one risk-adjusted rate for each patient to cover all their care – in and outpatient, LTC, rehab, drugs • Linked to Pay for Performance to ensure quality of care maintained, up to 10% of budget • Year One mixed results o Quality up for some measures, not others o All groups met savings targets and received rewards o Savings from reducing prices, shift to outpatient care, not reduced utilization o But total savings did not equal total bonuses
 Supportive options Patient-Centered Medical Homes Accountable care organizations EMRs, health information exchange Wellness programs with employee supports and rewards • Workforce development, esp primary care • Comparative effectiveness research • •
Supportive options Patient-Centered Medical Homes Accountable care organizations EMRs, health information exchange Wellness programs with employee supports and rewards • Workforce development, esp primary care • Comparative effectiveness research • •
 Patient-Centered Medical Homes • About half of Americans report poor coordination of care • 93% believe it is important to have one place or doctor responsible for primary care and coordinating care • 86% support providers working in teams to improve patient care • Patients linked to a team of providers that are responsible for their primary care, coordination, prevention, and supports for self-management • Evidence that the model improves care, reduces overall costs • Preferred by primary care providers • More efficient use of scarce primary care resources • Accreditation by national organizations • Support for Medicaid PCMHs in ACA
Patient-Centered Medical Homes • About half of Americans report poor coordination of care • 93% believe it is important to have one place or doctor responsible for primary care and coordinating care • 86% support providers working in teams to improve patient care • Patients linked to a team of providers that are responsible for their primary care, coordination, prevention, and supports for self-management • Evidence that the model improves care, reduces overall costs • Preferred by primary care providers • More efficient use of scarce primary care resources • Accreditation by national organizations • Support for Medicaid PCMHs in ACA
 Accountable Care Organizations • Networks of providers collectively rewarded to slow cost growth for their patients while improving quality of care • Patients can get care outside the network if they choose • Quality standards must be met to get share of savings • Some in one corporate entity, some are contractual networks • Medicare and private payers, some Medicaid programs considering them • Patients cannot be in Medicare ACO and any other state shared savings program o Providers may have incentives to guide patients based on their bottom line • For dual eligibles, how will Medicare ensure that providers are not shifting costs onto Medicaid
Accountable Care Organizations • Networks of providers collectively rewarded to slow cost growth for their patients while improving quality of care • Patients can get care outside the network if they choose • Quality standards must be met to get share of savings • Some in one corporate entity, some are contractual networks • Medicare and private payers, some Medicaid programs considering them • Patients cannot be in Medicare ACO and any other state shared savings program o Providers may have incentives to guide patients based on their bottom line • For dual eligibles, how will Medicare ensure that providers are not shifting costs onto Medicaid
 Comparative Effectiveness Research • New treatments, drugs, devices, procedures largest driver of rising health costs • Little information on which are worth the expense over current care • Even the research that is available takes years to enter practice patterns • Large federal investments in research • CEPAC – New England collaborative of clinicians, researchers and patient advocates deep dive into CER, votes on whether evidence is sufficient to recommend treatments o Medicare in our region changed authorization policy on treatment resistant depression vote
Comparative Effectiveness Research • New treatments, drugs, devices, procedures largest driver of rising health costs • Little information on which are worth the expense over current care • Even the research that is available takes years to enter practice patterns • Large federal investments in research • CEPAC – New England collaborative of clinicians, researchers and patient advocates deep dive into CER, votes on whether evidence is sufficient to recommend treatments o Medicare in our region changed authorization policy on treatment resistant depression vote
 Federal payment reform • Strong feature in national reform o o Innovation Center, waivers ACOs Comparative effectiveness research Medicare and Medicaid bundled payment pilots • Medicare o 23 programs – P 4 P, pay for reporting, never events, medical home, gain sharing, removing regulatory barriers, eprescribing, data aggregation o Premiere Demonstration – hospital P 4 P o Physician Group Demonstration o Implementing differential payments based on readmission rates
Federal payment reform • Strong feature in national reform o o Innovation Center, waivers ACOs Comparative effectiveness research Medicare and Medicaid bundled payment pilots • Medicare o 23 programs – P 4 P, pay for reporting, never events, medical home, gain sharing, removing regulatory barriers, eprescribing, data aggregation o Premiere Demonstration – hospital P 4 P o Physician Group Demonstration o Implementing differential payments based on readmission rates
 Medicaid payment reform • Most states risk adjust managed care plan capitation rates o 22 adjust for health status • 19 states include pay for performance in health plan payments o Withholds, bonuses, enhanced rates, shared savings, auto assignment, data reporting incentives, performance pools • 8 of 31 states with PCCM programs include P 4 P • Three-fourths of states with managed care plans publicly report on their quality o Some report on provider quality • 16 states assess quality in their fee-for-service programs
Medicaid payment reform • Most states risk adjust managed care plan capitation rates o 22 adjust for health status • 19 states include pay for performance in health plan payments o Withholds, bonuses, enhanced rates, shared savings, auto assignment, data reporting incentives, performance pools • 8 of 31 states with PCCM programs include P 4 P • Three-fourths of states with managed care plans publicly report on their quality o Some report on provider quality • 16 states assess quality in their fee-for-service programs
 Maine value-based purchasing • State employee plan leadership in larger multi-payer collaborative – Maine Health Management Coalition • 2005 adopted strategy to encourage consumers to make informed choices, incentives to access higher quality care, reward high quality providers, wellness programs with employee supports • Hospital and physician tiering by quality, expanded program in steps over the years o www. getbettermaine. org • Messaging to members, web-based, became a trusted source of information • Engaged providers in development of standards, QI plans • First year diabetes disease management participants averaged $1300 less in health care costs • Transitioning from FFS to bundled payments
Maine value-based purchasing • State employee plan leadership in larger multi-payer collaborative – Maine Health Management Coalition • 2005 adopted strategy to encourage consumers to make informed choices, incentives to access higher quality care, reward high quality providers, wellness programs with employee supports • Hospital and physician tiering by quality, expanded program in steps over the years o www. getbettermaine. org • Messaging to members, web-based, became a trusted source of information • Engaged providers in development of standards, QI plans • First year diabetes disease management participants averaged $1300 less in health care costs • Transitioning from FFS to bundled payments
 Vermont single payer reform • Global budget for health care costs, new payment models • Guaranteed coverage not linked to employment • Single system of provider payments and administrative rules • Health care system will remain privately owned • Payment reform to link payment to quality • Delivery reforms, workforce development • Expect to save $500 million/year and operating in 2017 • Planning through Green Mountain Care Board o Can set rates, CON controls, review insurance rates, hospital budgets
Vermont single payer reform • Global budget for health care costs, new payment models • Guaranteed coverage not linked to employment • Single system of provider payments and administrative rules • Health care system will remain privately owned • Payment reform to link payment to quality • Delivery reforms, workforce development • Expect to save $500 million/year and operating in 2017 • Planning through Green Mountain Care Board o Can set rates, CON controls, review insurance rates, hospital budgets
 Lessons from others Collaborate first Go slowly Start small and with strongest partners Coordinate across payers -- standardize Fair and open process Everyone on same page, all have same understanding Be clear on goals, single-minded dedication Strong consumer education piece necessary Plan for transitions Don’t underestimate the power of disclosure and transparency, often stronger motivator than $$$ • Be brave • The time is right for transforming delivery and payment systems – the status quo is not sustainable • • •
Lessons from others Collaborate first Go slowly Start small and with strongest partners Coordinate across payers -- standardize Fair and open process Everyone on same page, all have same understanding Be clear on goals, single-minded dedication Strong consumer education piece necessary Plan for transitions Don’t underestimate the power of disclosure and transparency, often stronger motivator than $$$ • Be brave • The time is right for transforming delivery and payment systems – the status quo is not sustainable • • •
 For more information: • • • www. valueovervolume. org www. csgeast. org www. cthealthpolicy. org eandrews@csg. org andrews@cthealthpolicy. org
For more information: • • • www. valueovervolume. org www. csgeast. org www. cthealthpolicy. org eandrews@csg. org andrews@cthealthpolicy. org


