vaccine for students.pptx
- Количество слайдов: 33
Vaccine (Passive immunization Active immunization) Abdulina G. A.
Protection of individuals from disease by vaccination can take two forms, passive and active immunization. Passive immunization is achieved by injecting a recipient with immunoglobulins directed against an already present infection. Active immunization involves injection of modified or purified pathogens, or their products.
A vaccine is a biological preparation that improves immunity to a particular disease. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins or one of its surface protein The term vaccine derives from Edward Jenner's 1796 use of cow pox (Latin variola vaccinia, adapted from the Latin vaccīn-us, from vacca, cow), to inoculate humans, providing them protection against smallpox.
Vaccines for active immunization 1) live, attenuated microorganisms; 2) killed microorganisms; 3) Subunit 4) vaccine conjugates; 5) inactivated toxins (toxoids). DDD, the value of vaccines: • Reduce Disease, • Reduce Disability, • Reduce Death.
1. Live attenuated (weakened) vaccine : • Attenuated pathogen multiplies inside human host and provides continuous antigenic stimulation. • Vaccine provides prolonged immunity (years to life), usually after a single dose. • Vaccine often provides cell- mediated immunity. Back side effect: there is a possibility that the attenuated vaccine strain will revert to an active pathogen after administration to the patient. For example, vaccineassociated poliomyelitis occurs following administration of approximately one out of every 2. 4 million doses of live polio vaccine. All recent cases of polio in the United States are vaccineassociated. Also, live, attenuated vaccines should not be given to immunocompromised individuals.
Live attenuated (weakened) vaccine Attenuated pathogen : 1. Typhoid fever 2. Rubeola 3. Mumps 4. Polio (Sabin) 5. Varicella-zoster 6. Adenovirus infections 7. Yellow fever 8. Rubella 9. Variola
2. Killed vaccines have the advantage over attenuated microorganisms in that they pose no risk of vaccineassociated infection. • Killed pathogen does not multiply in the human host; often provide a weak or short-lived immune response. • Multiple doses of vaccine are required, with subsequent booster doses. • Vaccine provides little cell-mediated immunity. • Vaccine is administered by injection Killed vaccines: Pertussis , Cholera, Plague, Typhoid fever, Q Fever, Polio (Salk), Hepatitis A, Influenza (whole virus), Rabies, Japanese encephalitis
Subunit Examples include the subunit vaccine against Hepatitis B virus that is composed of only the surface proteins of the virus (previously extracted from the blood serum of chronically infected patients, but now produced by recombination of the viral genes into yeast), the virus-like particle (VLP) vaccine against human papillomavirus (HPV) that is composed of the viral major capsid protein, and the hemagglutinin and neuraminidase subunits of the influenza virus. Subunit vaccine is being used for plague immunization.
Conjugated polysaccharide vaccines • Covalent binding (conjugation) of an antigenic polysaccharide to a protein enhances the immune response to these vaccines, particularly in children less than 2 years of age. (Haemophilus influenzae type B vaccine) • Toxoids: These are derivatives of bacterial exotoxins that can be produced by chemically altering the natural toxin, or by engineering bacteria to produce harmless variants of the toxin. Tetanus and Diphtheria (toxoid)
Adverse reactions to active vaccination Among the most common and mildest consequences of immunization are tenderness and swelling at the site of injection, and a mild fever (these complaints are occasionally more severe in neonates and young children). Symptoms vary with the nature of the vaccination. (Diphtheria and tetanus toxoids • Anaphylaxis (Measles-mumps-rubella vaccine = Thrombocytopenia and Anaphylaxis ( Oral poliovirus vaccine • Poliomyelitis in recipient or contact ( Hepatitis B vaccine • Anaphylaxis
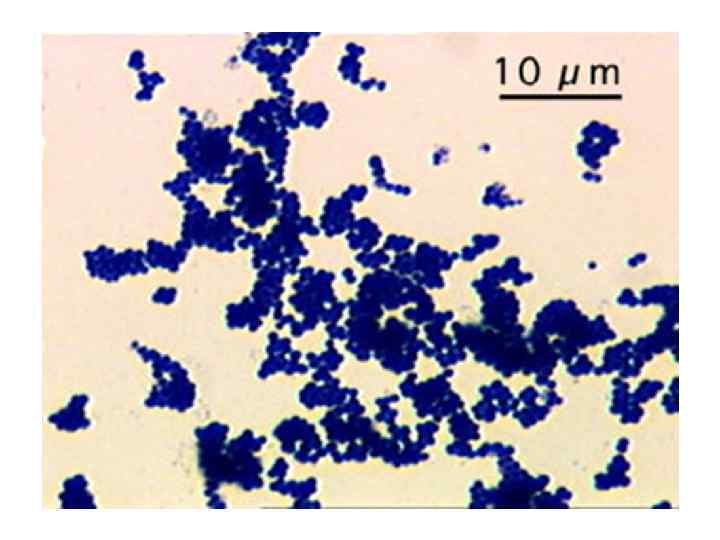
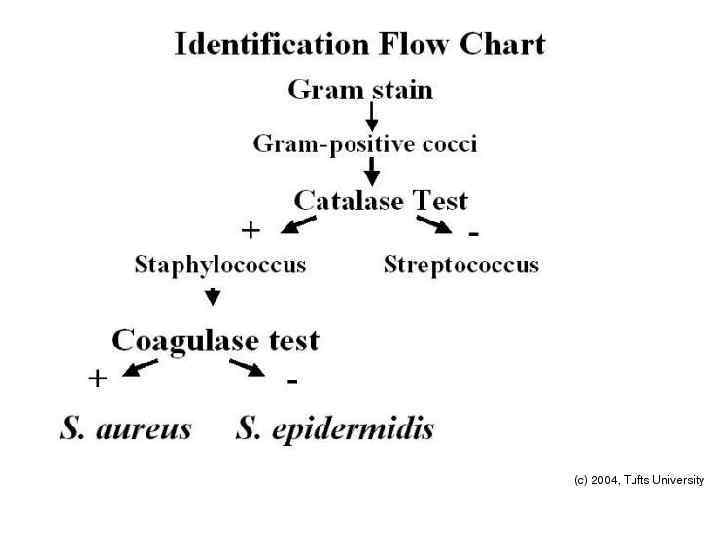
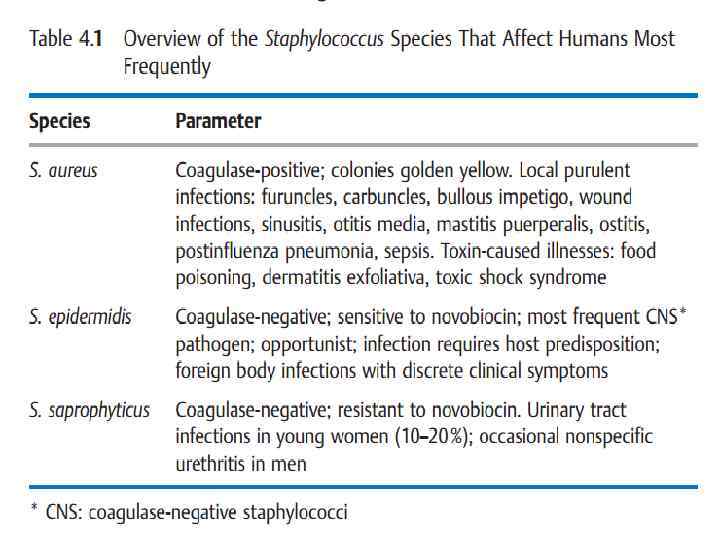
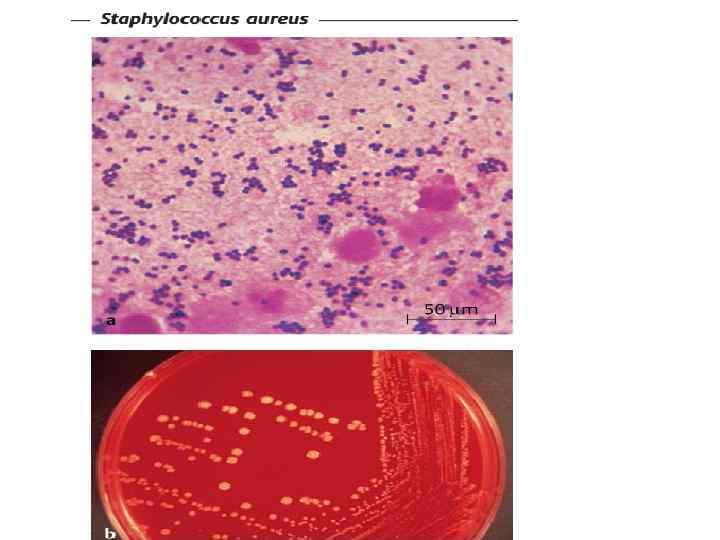
Family Micrococcaceae, the genus Staphylococcus. Staphylococci are pathogens of man and other mammals. Traditionally they were divided into two groups on the basis of their ability to clot blood plasma (the coagulase reaction). S aureus is coagulase-positive and the most pathogenic species. Coagulase-negative staphylococci (CNS) are now known to comprise over 30 other species Staphylococci are Gram+, Catalase-positive, facultative anaerobs. Shape is small clusters (staphylo = cluster). Staphylococcus is usually either beta hemolytic or not hemolytic at all (called gamma hemolysis)
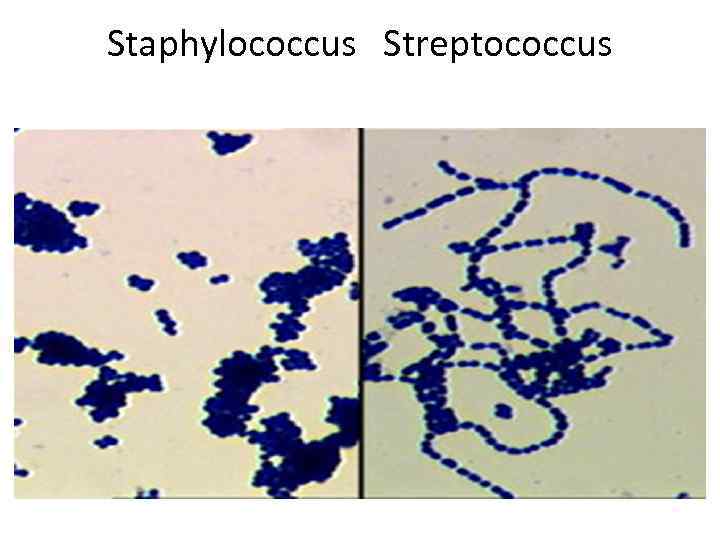
Staphylococcus Streptococcus
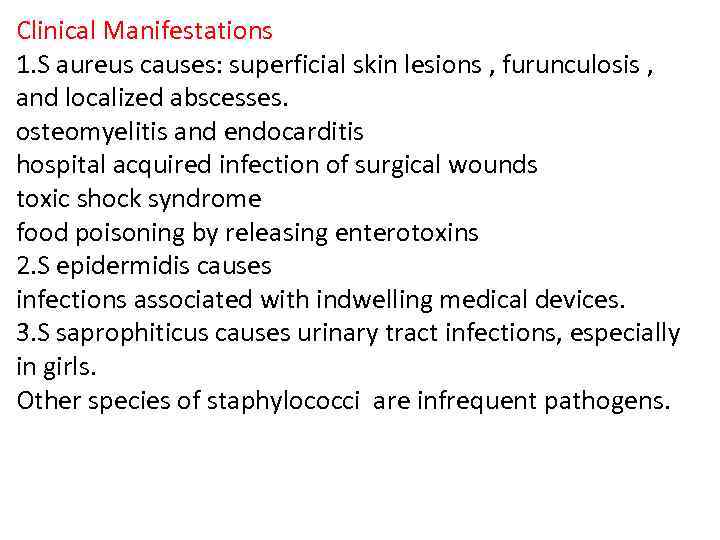
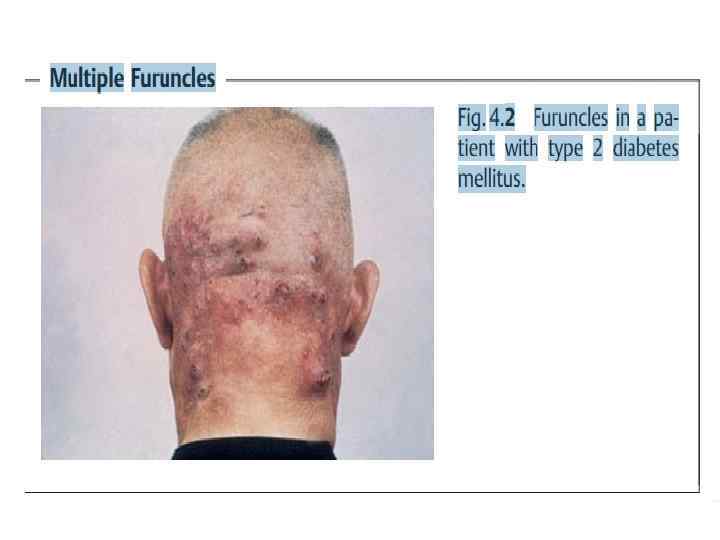
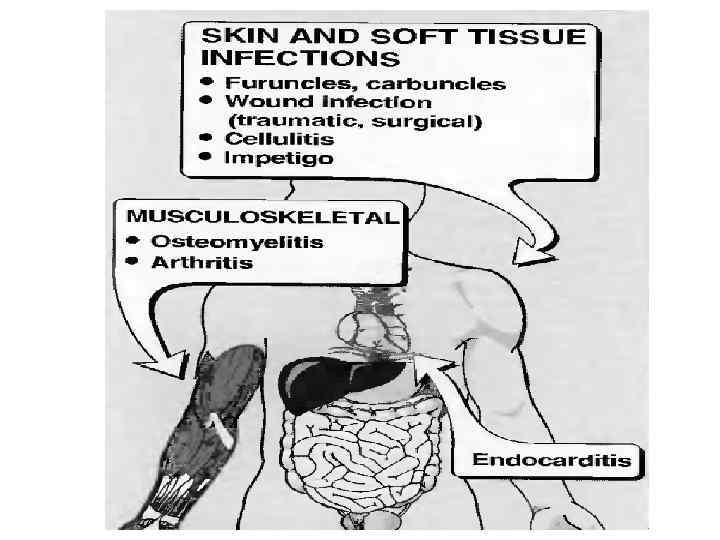
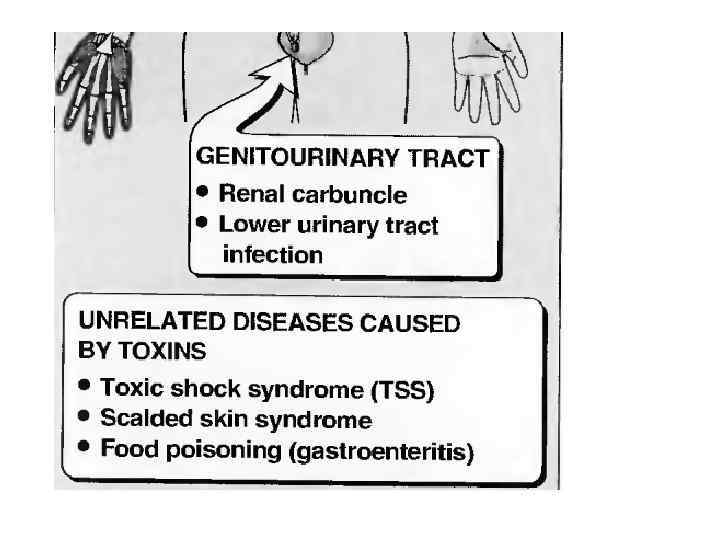
Clinical Manifestations 1. S aureus causes: superficial skin lesions , furunculosis , and localized abscesses. osteomyelitis and endocarditis hospital acquired infection of surgical wounds toxic shock syndrome food poisoning by releasing enterotoxins 2. S epidermidis causes infections associated with indwelling medical devices. 3. S saprophiticus causes urinary tract infections, especially in girls. Other species of staphylococci are infrequent pathogens.
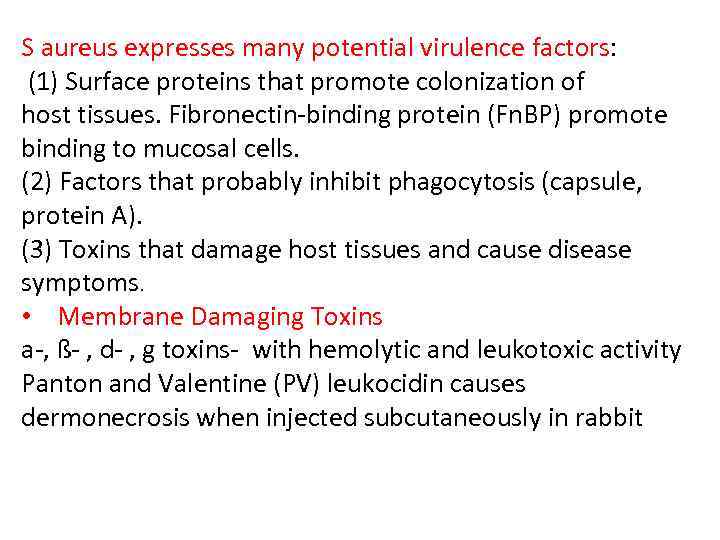
S aureus expresses many potential virulence factors: (1) Surface proteins that promote colonization of host tissues. Fibronectin-binding protein (Fn. BP) promote binding to mucosal cells. (2) Factors that probably inhibit phagocytosis (capsule, protein A). (3) Toxins that damage host tissues and cause disease symptoms. • Membrane Damaging Toxins a-, ß- , d- , g toxins- with hemolytic and leukotoxic activity Panton and Valentine (PV) leukocidin causes dermonecrosis when injected subcutaneously in rabbit
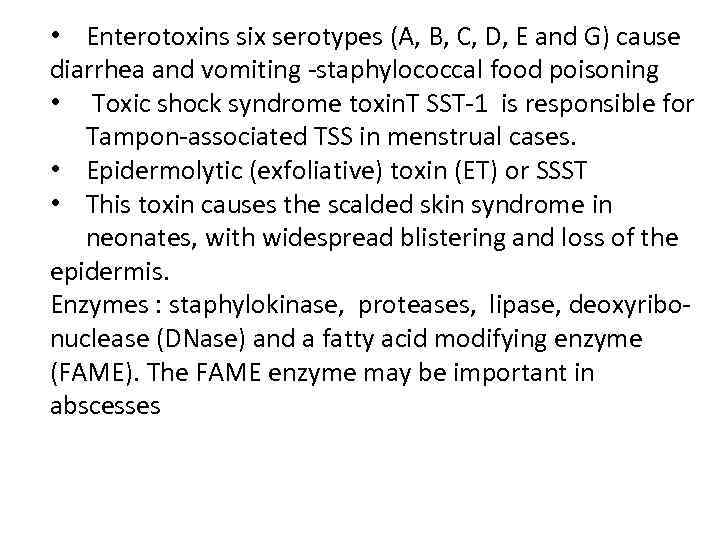
• Enterotoxins six serotypes (A, B, C, D, E and G) cause diarrhea and vomiting -staphylococcal food poisoning • Toxic shock syndrome toxin. T SST-1 is responsible for Tampon-associated TSS in menstrual cases. • Epidermolytic (exfoliative) toxin (ET) or SSST • This toxin causes the scalded skin syndrome in neonates, with widespread blistering and loss of the epidermis. Enzymes : staphylokinase, proteases, lipase, deoxyribonuclease (DNase) and a fatty acid modifying enzyme (FAME). The FAME enzyme may be important in abscesses
Antibiotic Resistance Multiple antibiotic resistance is increasingly common in S aureus and S epidermidis. Methicillin resistance is indicative of multiple resistance. Methicillin-resistant S aureus (MRSA) causes outbreaks in hospitals and can be epidemic.
Isolation and Identification The presence of staphylococci in a lesion might first be suspected after examination of a direct Gram stain. However, in blood require culturing first. Culture media: 1. Blood agar (BAP) is a common medium used to culture bacteria because • it is a great enriched medium for fastidious bacteria • hemolysis of blood cells can be very useful as an identification test 2. Chistovich agar containing 7. 5% sodium chloride – selective vtdium 3. MPA – pigment production
Vaccines No vaccine is currently available to combat staphylococcal infections. There may now be a case for considering methods to prevent disease, particularly in hospitalized patients. Hyperimmune serum from human volunteer donors. which could be given to patients in hospital before surgery A vaccine based on fibronectin binding protein induces protective immunity against mastitis in cattle and might also be used as a vaccine in humans.
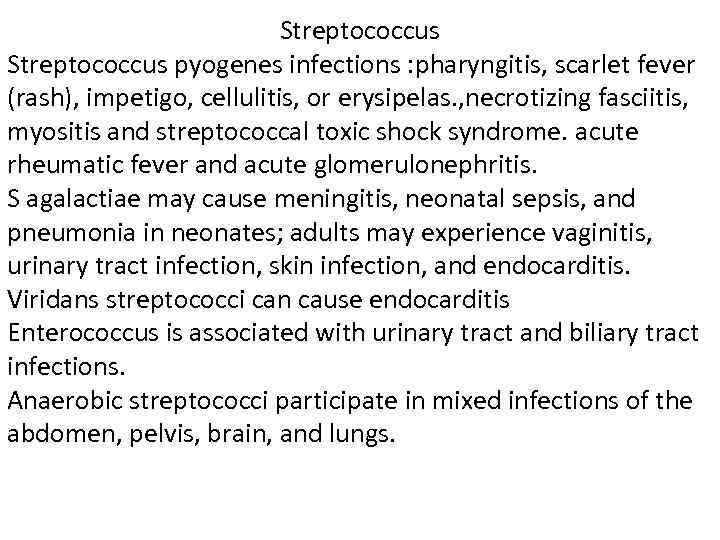
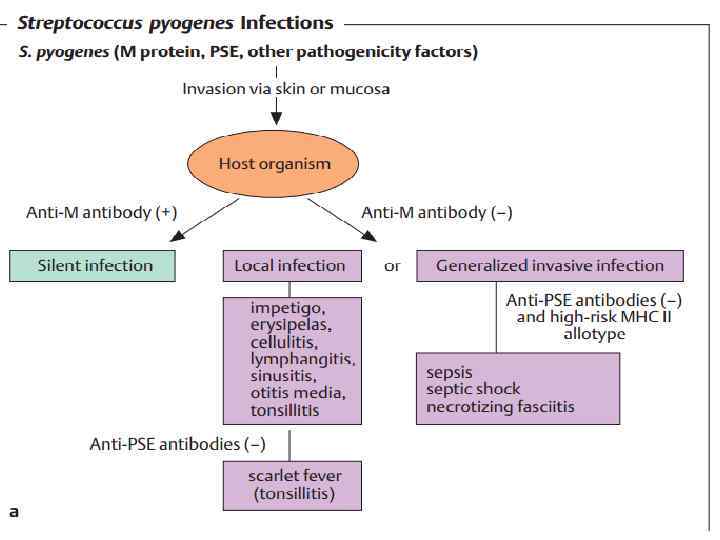
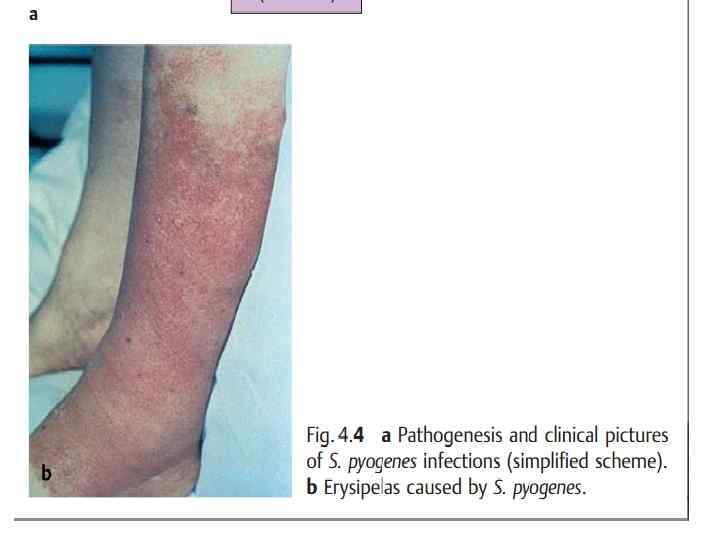
Streptococcus pyogenes infections : pharyngitis, scarlet fever (rash), impetigo, cellulitis, or erysipelas. , necrotizing fasciitis, myositis and streptococcal toxic shock syndrome. acute rheumatic fever and acute glomerulonephritis. S agalactiae may cause meningitis, neonatal sepsis, and pneumonia in neonates; adults may experience vaginitis, urinary tract infection, skin infection, and endocarditis. Viridans streptococci can cause endocarditis Enterococcus is associated with urinary tract and biliary tract infections. Anaerobic streptococci participate in mixed infections of the abdomen, pelvis, brain, and lungs.
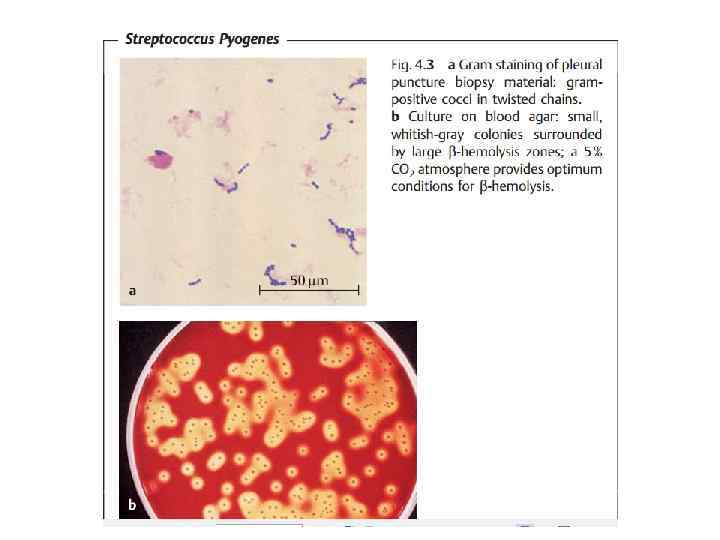
Structure Streptococci are Gram-positive, nonmotile, nonsporeforming, catalase-negative cocci that occur in pairs or chains. Most streptococci are facultative anaerobes, and some are obligate (strict) anaerobes. Most require enriched media (blood agar). Group A streptococci have a hyaluronic acid capsule
Classification and Antigenic Types Streptococci are classified on the basis of colony morphology, hemolysis, biochemical reactions, and (most definitively) serologic specificity. They are divided into three groups by the type of hemolysis on blood agar: • b-hemolytic (clear, complete lysis of red cells) • a- hemolytic (incomplete, green hemolysis) • g -hemolytic (no hemolysis). . Lancefield Serologic grouping is based on antigenic differences in cell wall carbohydrates (groups A to V)
Pathogenesis Streptococci are members of the normal flora. Virulence factors of group A streptococci include (1)M protein and lipoteichoic acid for attachment; (2) a hyaluronic acid capsule that inhibits phagocytosis; (3) other extracellular products, such as pyrogenic (erythrogenic) toxin. Three pyrogenic exotoxins of S pyogenes (SPEs) are recognized: types A, B, C which causes the rash of scarlet fever; (4) streptokinase, streptodornase (DNase B), and streptolysins. Some strains are nephritogenic. Nongroup A strains have no defined virulence factors

vaccine for students.pptx