7d5d8ac9cea4c567f6e5d47448068afe.ppt
- Количество слайдов: 38

Using verbal autopsy to assess to pass to death Infant Mortality in Talas oblast, Kyrgyzstan, Years 1997 -2001 A. Napoletano, D. Coclite, R. Ferrelli, А. Маzzaccara Istituto Supepriore di Sanita, ISS, Rome - Italy М. Аshiraliev, М. Мinbaev Center for Social and Economic Research, Bishkek -Кyrgyzstan
The Survey Aimed at: Identifying mother and infants that died in Talas oblast, Kyrgyz Repbulic between 1 January, 1997 and 31 December, 2001 Estimating levels of IMR in rural and urban population of Talas oblast Investigating biological and medical causes of infant and maternal deahts Describing the care seeking process that lead to death Identifying family risk factors which expose chilren to an excess of risk of dying compared to the children who lived more than one year
METHODS AND TOOLS The medical aspects of infant and maternal deaths were investigated by means of a modified version of the WHO standard verbal autopsy. The Tool consists of three components: • two structured sets of questions (verbal autopsy) addressed to the caretakers in the sampled households, meant to frame biological or medical causes of death; and • a set of semi- and unstructured questions to describe the care seeking process that led to death.
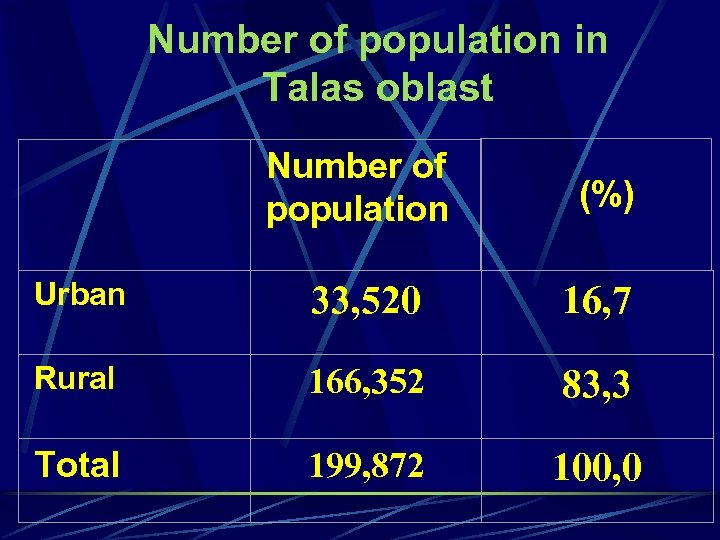
Number of population in Talas oblast Number of population (%) Urban 33, 520 16, 7 Rural 166, 352 83, 3 Total 199, 872 100, 0
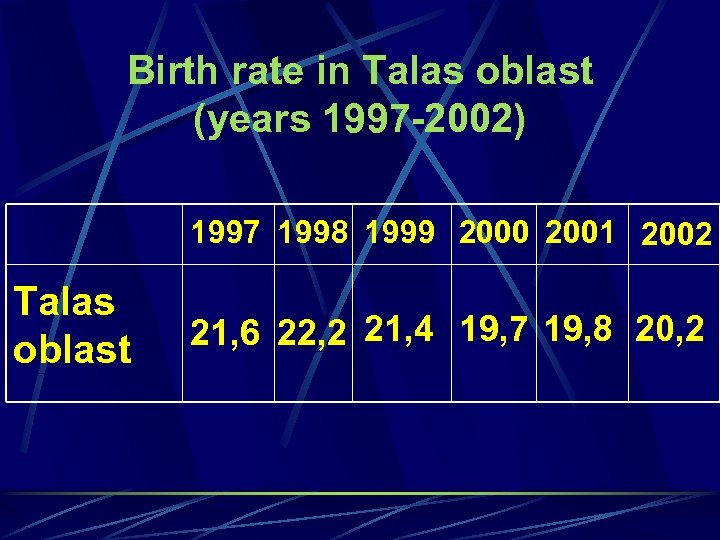
Birth rate in Talas oblast (years 1997 -2002) 1997 1998 1999 2000 2001 2002 Talas oblast 21, 6 22, 2 21, 4 19, 7 19, 8 20, 2
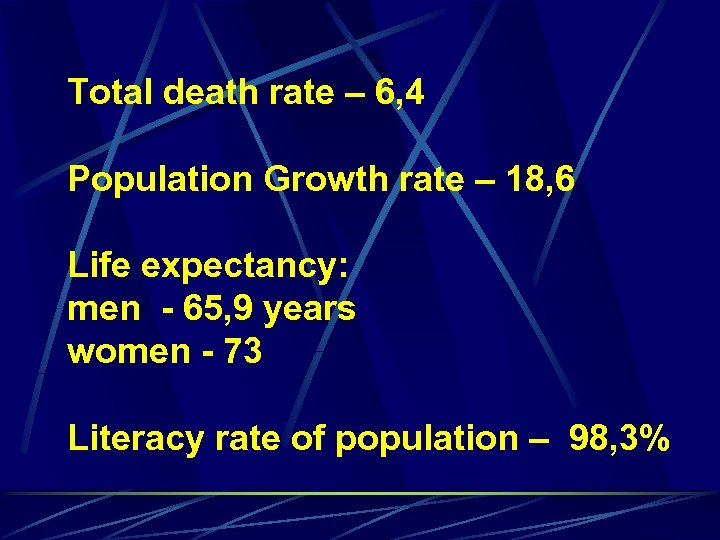
Total death rate – 6, 4 Population Growth rate – 18, 6 Life expectancy: men - 65, 9 years women - 73 Literacy rate of population – 98, 3%
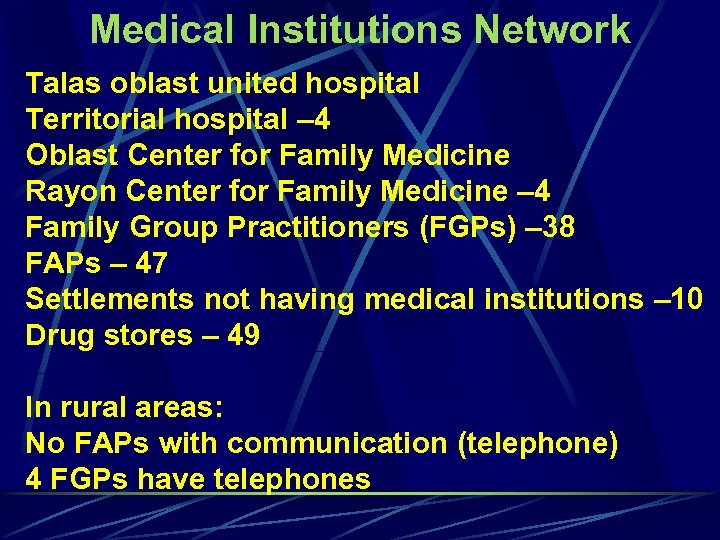
Medical Institutions Network Таlas oblast united hospital Territorial hospital – 4 Oblast Center for Family Medicine Rayon Center for Family Medicine – 4 Family Group Practitioners (FGPs) – 38 FAPs – 47 Settlements not having medical institutions – 10 Drug stores – 49 In rural areas: No FAPs with communication (telephone) 4 FGPs have telephones
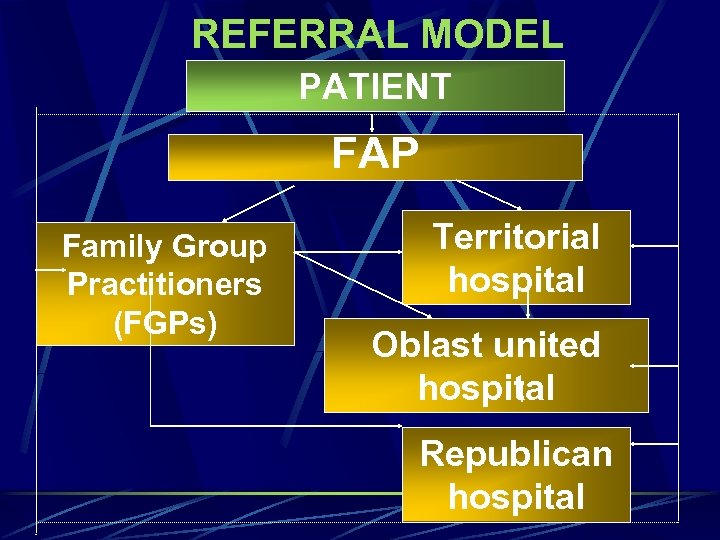
REFERRAL MODEL PATIENT FAP Family Group Practitioners (FGPs) Territorial hospital Oblast united hospital Republican hospital
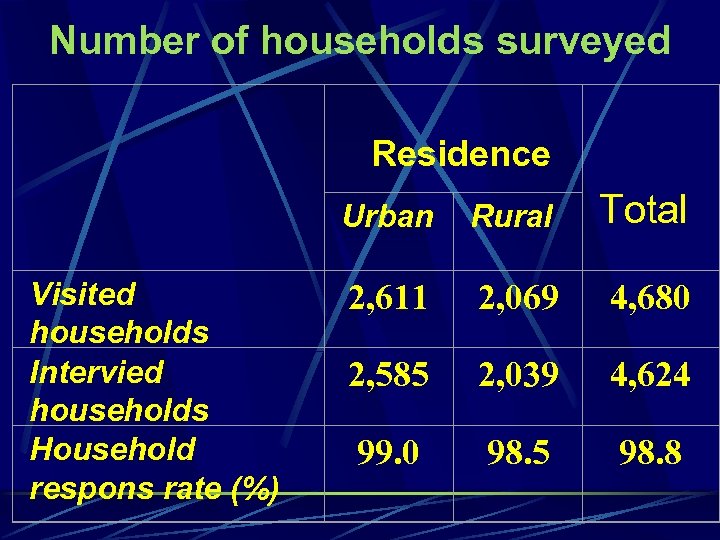
Number of households surveyed Residence Urban Visited households Intervied households Household respons rate (%) Rural Total 2, 611 2, 069 4, 680 2, 585 2, 039 4, 624 99. 0 98. 5 98. 8
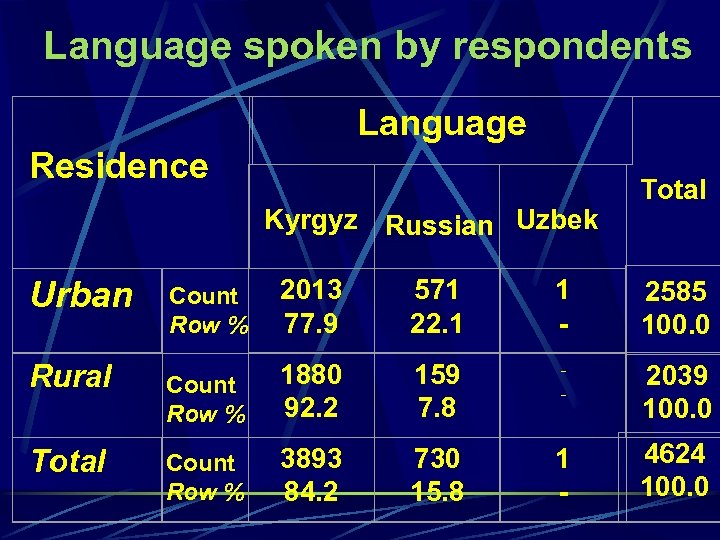
Language spoken by respondents Language Residence Kyrgyz Russian Uzbek Urban Rural Total Count Row % 2013 77. 9 571 22. 1 1 - 2585 100. 0 Count Row % 1880 92. 2 159 7. 8 - 2039 100. 0 Count Row % 3893 84. 2 730 15. 8 1 - 4624 100. 0
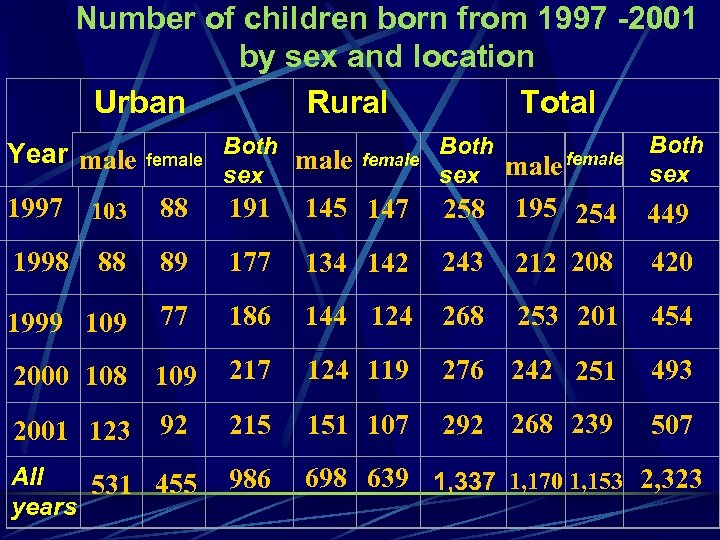
Number of children born from 1997 -2001 by sex and location Urban Rural Total Both male sex Both male female sex Both sex Year male female 1997 103 88 191 145 147 258 195 254 449 1998 88 89 177 134 142 243 212 208 420 1999 109 77 186 144 124 268 253 201 454 2000 108 109 217 124 119 276 242 251 493 92 215 151 107 292 268 239 507 986 698 639 1, 337 1, 170 1, 153 2, 323 2001 123 All 531 455 years female
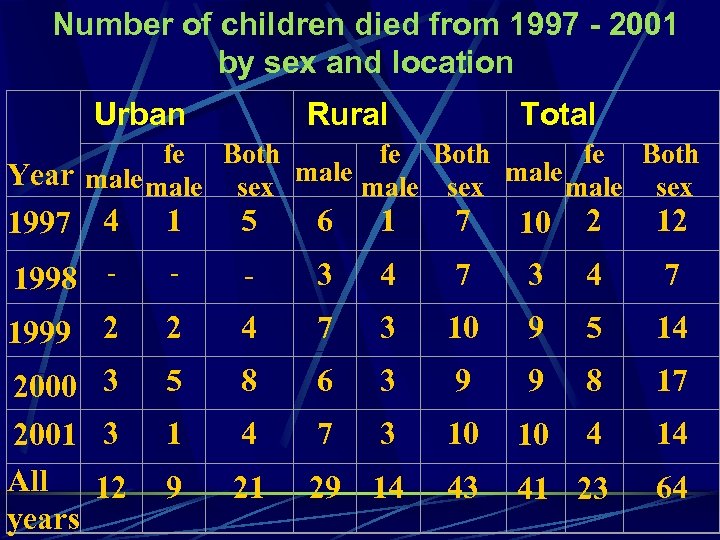
Number of children died from 1997 - 2001 by sex and location Urban Rural Total fe Both Year male sex male sex 4 1 5 6 1 7 10 2 12 1998 - - - 3 4 7 2 2 4 7 3 10 9 5 14 2000 3 2001 3 All 12 years 5 8 6 3 9 9 8 17 1 4 7 3 10 10 4 14 9 21 29 14 43 41 23 64 1997 1999
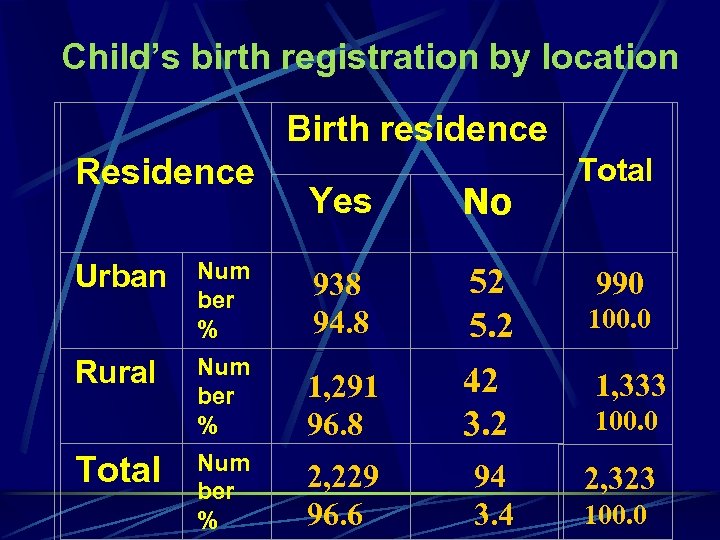
Child’s birth registration by location Birth residence Residence Urban Rural Total Yes No Num ber % 938 94. 8 52 5. 2 Num ber % 1, 291 96. 8 42 3. 2 Num ber % 2, 229 96. 6 94 3. 4 Total 990 100. 0 1, 333 100. 0 2, 323 100. 0
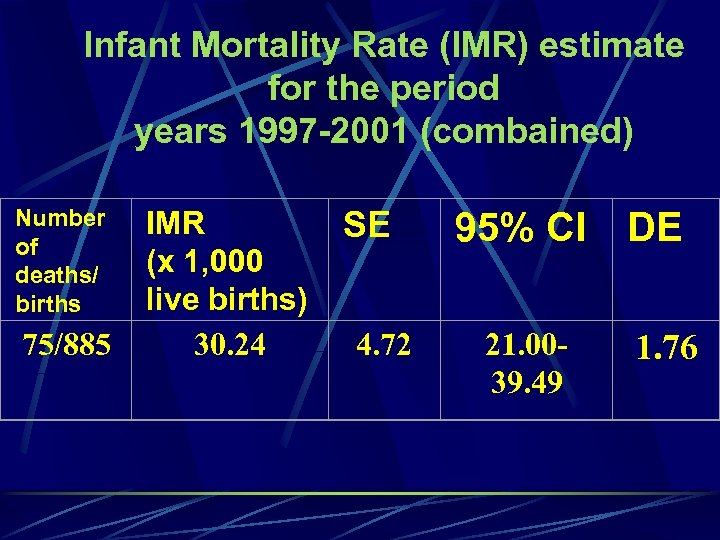
Infant Mortality Rate (IMR) estimate for the period years 1997 -2001 (combained) Number of deaths/ births 75/885 IMR (x 1, 000 live births) 30. 24 SE 4. 72 95% CI 21. 0039. 49 DE 1. 76
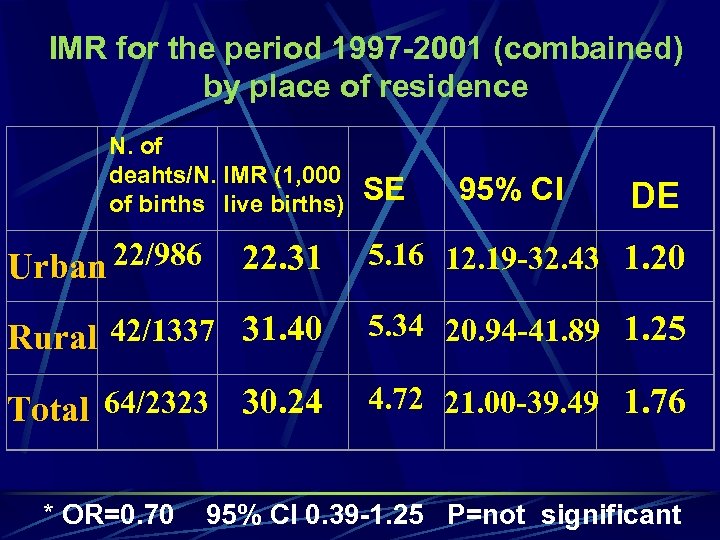
IMR for the period 1997 -2001 (combained) by place of residence N. of deahts/N. IMR (1, 000 of births live births) Urban 22/986 SE 95% CI DE 22. 31 5. 16 12. 19 -32. 43 1. 20 Rural 42/1337 31. 40 5. 34 20. 94 -41. 89 1. 25 Total 64/2323 30. 24 4. 72 21. 00 -39. 49 1. 76 * OR=0. 70 95% CI 0. 39 -1. 25 P=not significant
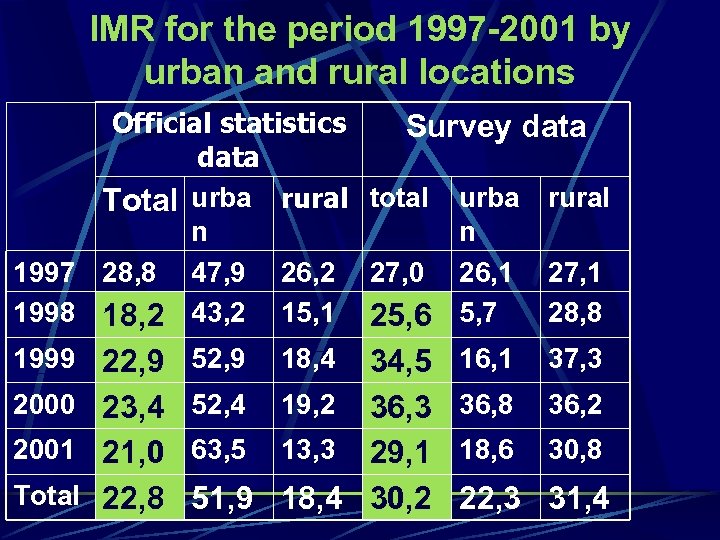
IMR for the period 1997 -2001 by urban and rural locations Official statistics Survey data Total urba rural total urba rural n n 1997 28, 8 47, 9 26, 2 27, 0 26, 1 27, 1 1998 18, 2 43, 2 15, 1 25, 6 5, 7 28, 8 1999 22, 9 52, 9 2000 23, 4 52, 4 18, 4 34, 5 19, 2 36, 3 2001 21, 0 63, 5 13, 3 29, 1 Total 22, 8 51, 9 18, 4 30, 2 16, 1 37, 3 36, 8 36, 2 18, 6 30, 8 22, 3 31, 4
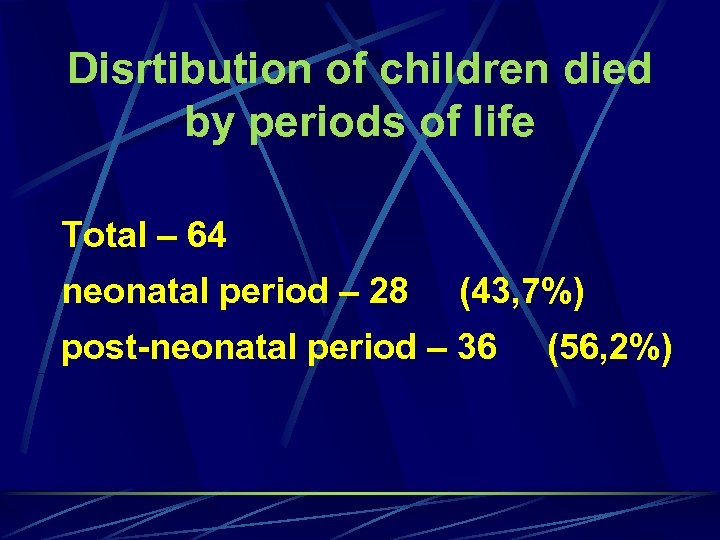
Disrtibution of children died by periods of life Total – 64 neonatal period – 28 (43, 7%) post-neonatal period – 36 (56, 2%)
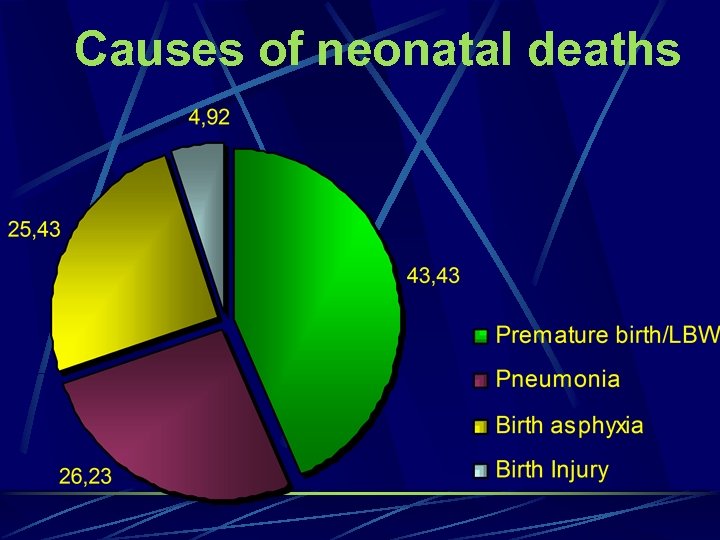
Causes of neonatal deaths
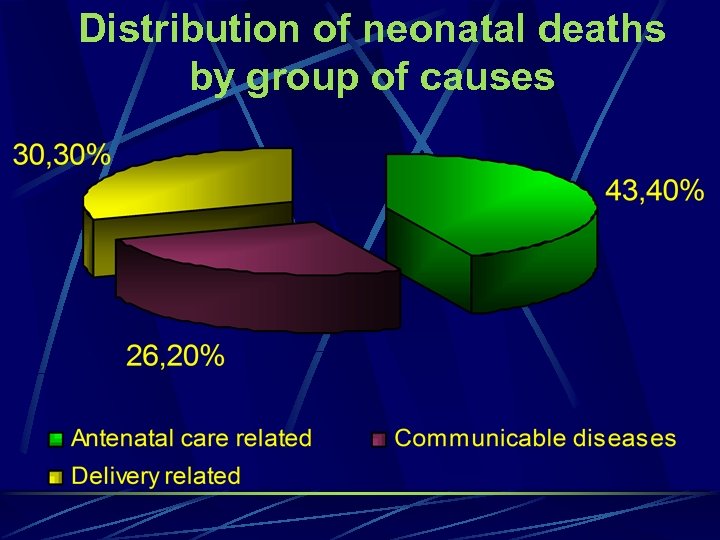
Distribution of neonatal deaths by group of causes
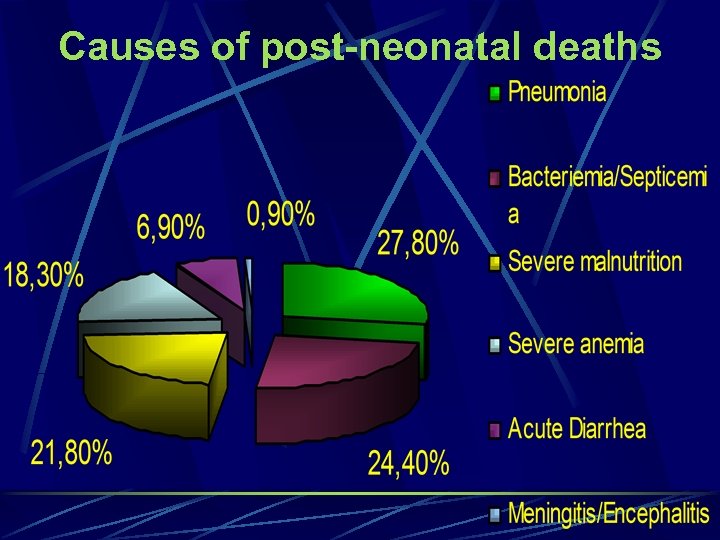
Causes of post-neonatal deaths
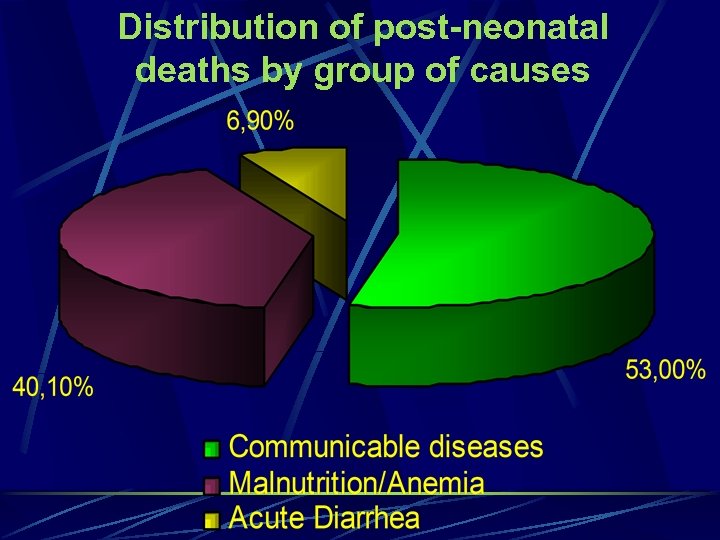
Distribution of post-neonatal deaths by group of causes
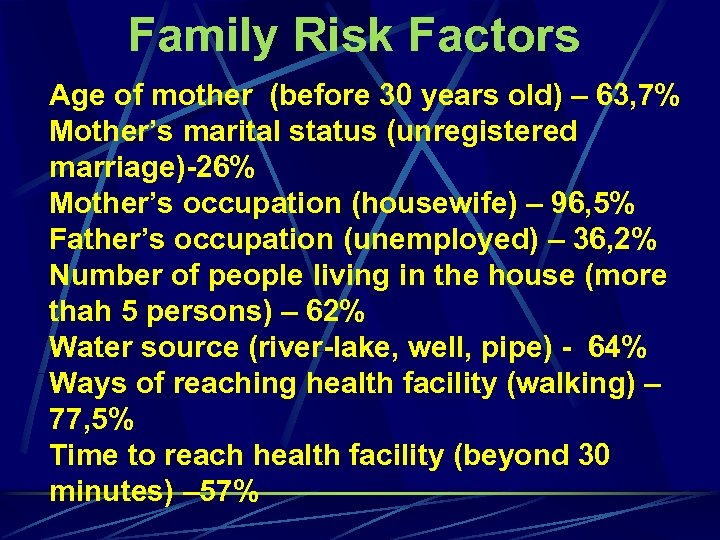
Family Risk Factors Age of mother (before 30 years old) – 63, 7% Mother’s marital status (unregistered marriage)-26% Mother’s occupation (housewife) – 96, 5% Father’s occupation (unemployed) – 36, 2% Number of people living in the house (more thah 5 persons) – 62% Water source (river-lake, well, pipe) - 64% Ways of reaching health facility (walking) – 77, 5% Time to reach health facility (beyond 30 minutes) – 57%
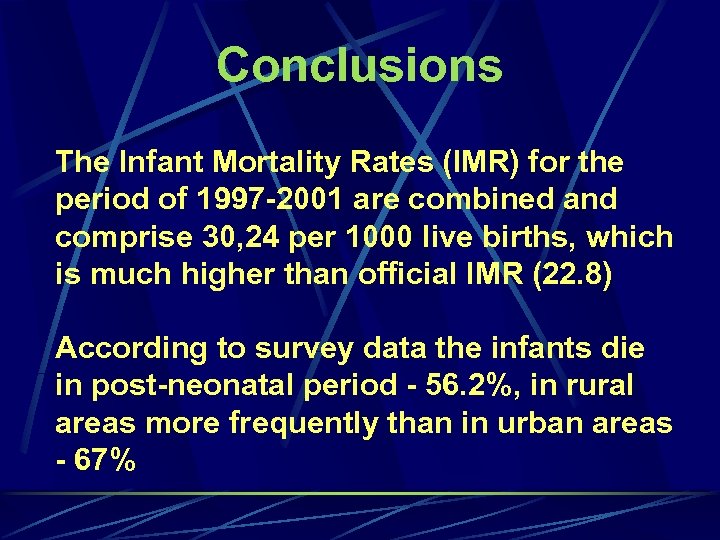
Conclusions The Infant Mortality Rates (IMR) for the period of 1997 -2001 are combined and comprise 30, 24 per 1000 live births, which is much higher than official IMR (22. 8) According to survey data the infants die in post-neonatal period - 56. 2%, in rural areas more frequently than in urban areas - 67%
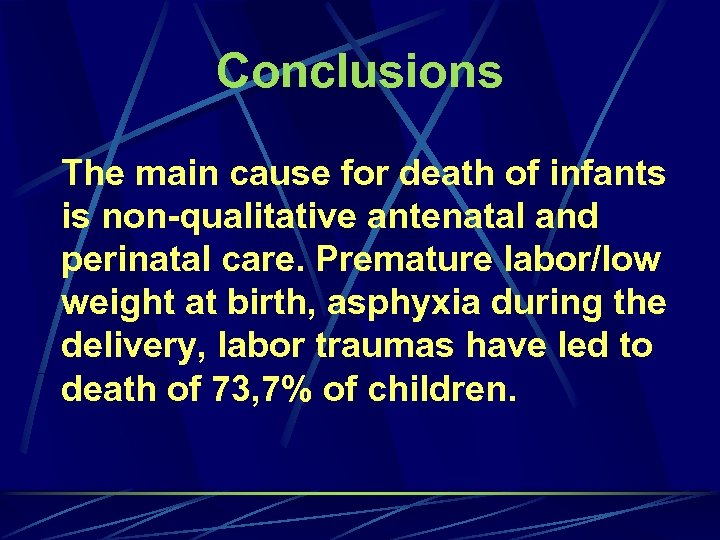
Conclusions The main cause for death of infants is non-qualitative antenatal and perinatal care. Premature labor/low weight at birth, asphyxia during the delivery, labor traumas have led to death of 73, 7% of children.
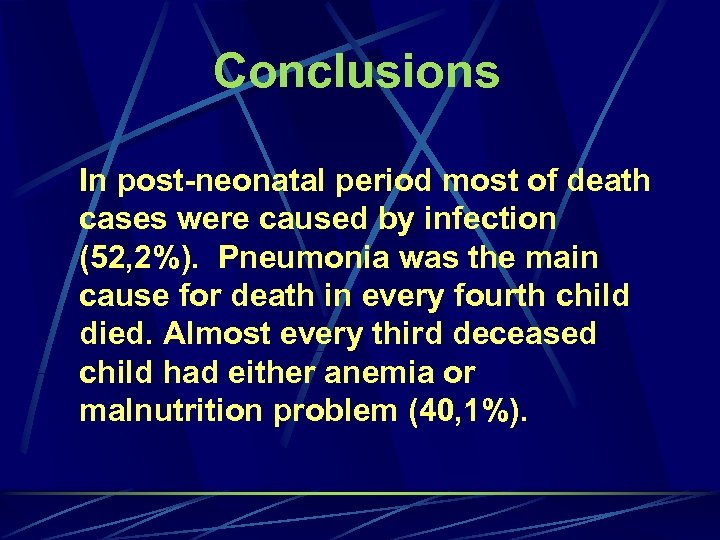
Conclusions In post-neonatal period most of death cases were caused by infection (52, 2%). Pneumonia was the main cause for death in every fourth child died. Almost every third deceased child had either anemia or malnutrition problem (40, 1%).
Conclusions The survival of children under 1 is influenced by several factors, including territorial location of the health care facility, mother’s age (young mothers), whether the child is first, lack of skills for child care, lack of support from family and community to be provided to mothers during pregnancy, labor, as well as breastfeeding periods.
Conclusions The Maternal Mortality Rate (MMR) in the oblast depends on qualified, safe provision of health care and aid by health facilities and awareness of population.
Recommendations for action • To develop and approve the National Program on Perinatolgy. • To introduce and use nation-wide the criteria of live birth – to train health staff, to approve normative documents and acts for registration and reporting.
Recommendations for action • To eliminate faulty practice of concealment of cases of infant mortality at health facilities. • To improve the work of services of registration of newborns at maternity (obstetric) facilities, to increase the quality of registration of maternal and children’s mortality.

Recommendations for action • To guarantee population’s rights to qualitative and adequate medical care, first of all medical - sanitary care (aid) at primary health care level, including delivery of services, related to antenatal and perinatal care.
Recommendations for action To provide an adequate qualified medical care (quality, accessibility, guarantee) for all population groups, both in urban and rural areas, regardless of the level of social status.
Recommendations for action To improve access (logistic aspects, territorial location) to health care facilities, to increase the role of a midwife, family and communities.
Recommendations for action To increase efficiency of health care (safe, based on evidence medicine).
Recommendations for action To increase the quality of perinatal care (premature labor, pre-eclampsia, obstetric bleeding) and qualitative training of health staff (cadre) for different levels of health care system, as well as to upgrade knowledge and skills of health staff on a continuous basis.

Recommendations for action To improve intensive care of newborns and children of young ages.
Recommendations for action To increase the awareness of all population layers, youth in particular, of health protection issues, on pregnancy, care of newborns and unwanted pregnancy.
Recommendations for action To promote and expand principles and methodology of IMCI.
Recommendations for action To increase advocacy in the area of women’s and children’s rights, to provide comprehensive services information, to improve efficiency of counseling services, to identify strategies from the point of view of cost efficiency, to expand successfully implemented projects in the area of perinatology.
7d5d8ac9cea4c567f6e5d47448068afe.ppt