0db154b2ce54c79cc7a73b5877fad528.ppt
- Количество слайдов: 54
Using the Medical Literature to Make Decisions About Preventive Health Services Kenny Lin, MD Associate Editor, Essential Evidence Plus Associate Editor, American Family Physician May 17, 2011
Disclosures Associate Editor, Essential Evidence Plus (Wiley) n Associate Editor, American Family Physician (AAFP) n Adjunct Faculty Positions n Georgetown University School of Medicine n Johns Hopkins Univ. School of Public Health n Uniformed Services Univ. of the Health Sciences n n Former Medical Officer, Agency for Healthcare Research and Quality (DHHS)
Learning Objectives n n Review the burden of chronic preventable diseases in the United States. Estimate the potential for improving health through effective clinical prevention. Understand the importance of using an evidencebased process to develop preventive health guidelines based on searches of the medical literature. Introduce multiple tools for accessing preventive health information at the point of care.
“An ounce of prevention is worth a pound of cure” Burden of Chronic Illness in the United States
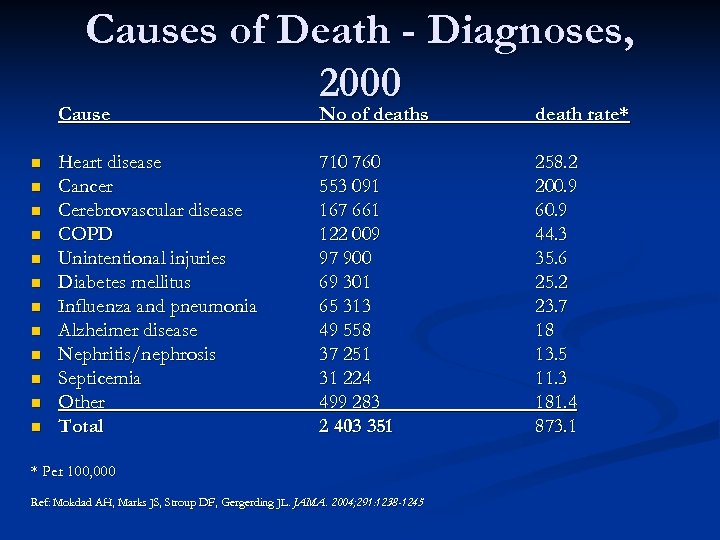
Causes of Death - Diagnoses, 2000 Cause n n n No of deaths death rate* Heart disease Cancer Cerebrovascular disease COPD Unintentional injuries Diabetes mellitus Influenza and pneumonia Alzheimer disease Nephritis/nephrosis Septicemia Other Total 710 760 553 091 167 661 122 009 97 900 69 301 65 313 49 558 37 251 31 224 499 283 2 403 351 258. 2 200. 9 60. 9 44. 3 35. 6 25. 2 23. 7 18 13. 5 11. 3 181. 4 873. 1 * Per 100, 000 Ref: Mokdad AH, Marks JS, Stroup DF, Gergerding JL. JAMA. 2004; 291: 1238 -1245
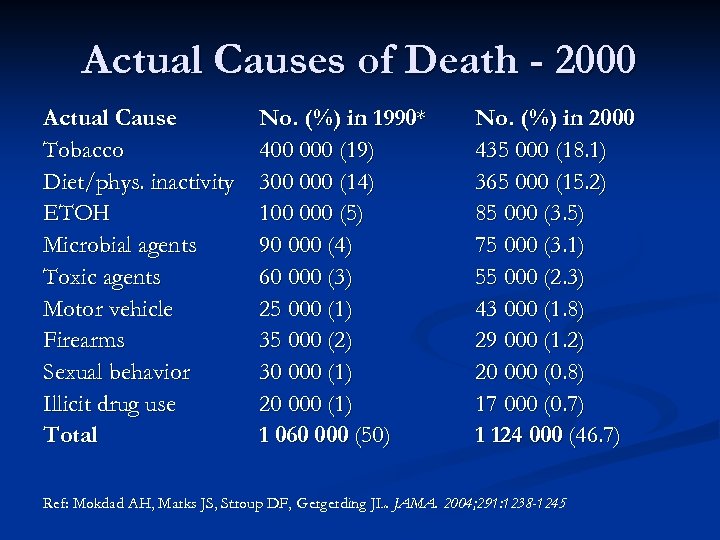
Actual Causes of Death - 2000 Actual Cause Tobacco Diet/phys. inactivity ETOH Microbial agents Toxic agents Motor vehicle Firearms Sexual behavior Illicit drug use Total No. (%) in 1990* 400 000 (19) 300 000 (14) 100 000 (5) 90 000 (4) 60 000 (3) 25 000 (1) 35 000 (2) 30 000 (1) 20 000 (1) 1 060 000 (50) No. (%) in 2000 435 000 (18. 1) 365 000 (15. 2) 85 000 (3. 5) 75 000 (3. 1) 55 000 (2. 3) 43 000 (1. 8) 29 000 (1. 2) 20 000 (0. 8) 17 000 (0. 7) 1 124 000 (46. 7) Ref: Mokdad AH, Marks JS, Stroup DF, Gergerding JL. JAMA. 2004; 291: 1238 -1245
Preventable Deaths in the U. S. ranks last among industrialized nations in preventable deaths Could prevent 100, 000 deaths annually if rates were similar to high-performing nations Health Affairs, Sept. 2006
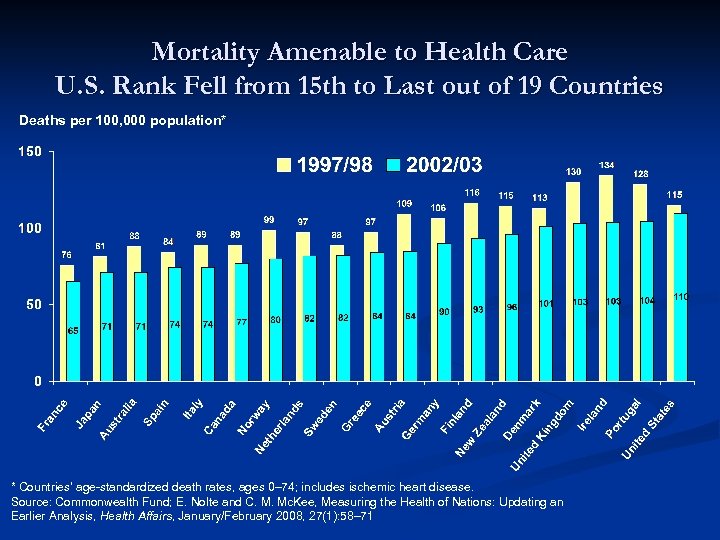
Mortality Amenable to Health Care U. S. Rank Fell from 15 th to Last out of 19 Countries Deaths per 100, 000 population* * Countries’ age-standardized death rates, ages 0– 74; includes ischemic heart disease. Source: Commonwealth Fund; E. Nolte and C. M. Mc. Kee, Measuring the Health of Nations: Updating an Earlier Analysis, Health Affairs, January/February 2008, 27(1): 58– 71
Costs of Preventable Diseases We cannot effectively address escalating health care costs without addressing the problem of chronic diseases and finding ways to delay or prevent their onset. q More than 90 million Americans live with chronic illness q Chronic diseases account for 70% of all deaths in the U. S. q The medical costs of people with chronic diseases account for more than 75% of the nation’s approximately $1. 5 trillion in annual medical care costs.
Challenges in Prevention n n Most important messages about prevention may not be getting through to clinicians and patients Not everything that might work does work Services should be supported by good evidence (but often aren’t) before they are widely recommended Necessity of providing individual preventive services often skewed by: n n Beliefs, anecdotal experiences of clinicians and patients Inaccurate media messages Advocacy groups Political considerations
Primary care: is there time enough for prevention? Yarnall KS et al. , Am J Public Health, 2003 n Used published and estimated times to determine the total physician time required to provide all recommended preventive services to a patient panel of 2500 with an age and sex distribution similar to that of the US population n 1773 hours annually, or 7. 4 hours per working day n
How much time do primary care clinicians actually spend on preventive care? n n Pollak KI et al. , BMJ Health Serv Res, 2008 Data on family and internal medicine visits from 200104 National Ambulatory Medical Care Survey Most time spent on: PSA (4. 9 minutes), cholesterol, Pap smear, mammograms, exercise counseling, and blood pressure Spent less time than recommended on tobacco cessation (0. 11 vs. 3 minutes) and nutrition counseling (1. 34 vs. 8. 2 minutes)
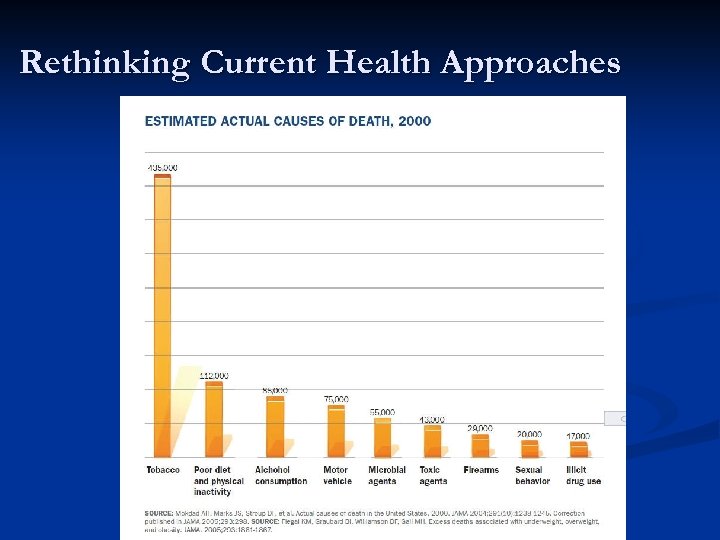
Rethinking Current Health Approaches
Problem of Underuse of Clinical Preventive Services n n n Insurance coverage makes a difference in whether people receive preventive services Approximately half (52%) of adults receive preventive care according to guidelines for their age and sex. 1 In 2004, NCQA identified 48, 600 cases of late-stage breast cancer and colorectal cancer and osteoporosisrelated fractures that could have been averted if individuals received appropriate and timely preventive care. 2 Sources: 1. The Commonwealth Fund Commission on a High Performance Healthcare System, Sept 2006; 2. National Committee for Quality Assurance. The State of Healthcare Quality 2005. Washington, DC; NCQA: 2006.
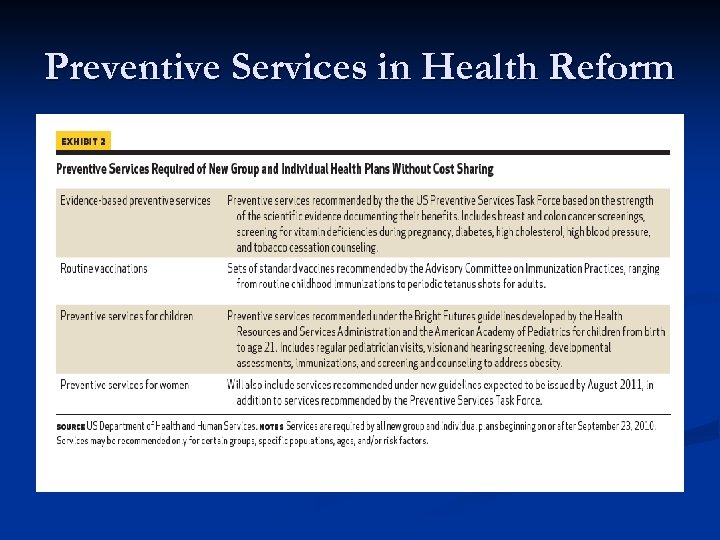
Preventive Services in Health Reform
Why Evidence-Based? n Need transparent, systematic process to obtain and distill best available evidence to support clinical decision making n n Identifying, evaluating and summarizing scientific evidence about outcomes or interventions or policies Translating research evidence into clinical practice recommendations
General Attributes of Good Clinical Practice Guidelines n n n n Comprehensive, systematic evidence search Evidence linked directly to recommendations via strength of recommendation grading system Recommendations based on patient-oriented rather than disease-oriented outcomes Development process is transparent Potential conflicts of interest identified and addressed Prospective validation Clinical flexibility
U. S. Preventive Services Task Force: Prevention in the Clinical Setting
What is the US Preventive Services Task Force? n Congressionally mandated, independent panel of non. Federal experts in prevention and evidence-based medicine, established in 1984 n 16 primary care clinicians (internists, pediatricians, family physicians, ob/gyns, nurses and health behavior specialists) appointed to rotating 4 -year terms http: //www. uspreventiveservicestaskforce. org/about. htm
![What is the USPSTF Mission? “to evaluate the benefits of individual [preventive] services based What is the USPSTF Mission? “to evaluate the benefits of individual [preventive] services based](https://present5.com/presentation/0db154b2ce54c79cc7a73b5877fad528/image-21.jpg)
What is the USPSTF Mission? “to evaluate the benefits of individual [preventive] services based on age, gender, and risk factors for disease; make recommendations about which preventive services should be incorporated routinely into primary medical care and for which populations; and identify a research agenda for clinical preventive care. ” www. uspreventiveservicestaskforce. org/about. htm
Who Supports the USPSTF? n n Administrative, research, technical and dissemination support provided by the Agency for Healthcare Research and Quality (AHRQ), a division of the Department of Health and Human Services (DHHS) Scientific support from AHRQ-funded Evidence-Based Practice Centers (EPCs) Ø EPCs conduct systematic evidence reviews on topics in clinical prevention that serve as the scientific basis for USPSTF recommendations www. uspreventiveservicestaskforce. org/about. htm
What are US Preventive Services Task Force Activities? n n n Guidelines published in the form of “recommendation statements” 2010 Affordable Care Act singles out positive recommendations by the USPSTF ( “A” or “B”) for coverage without cost-sharing Recommendations are graded to convey two major elements: certainty and magnitude of net benefit of the preventive service http: //www. uspreventiveservicestaskforce. org/about. htm
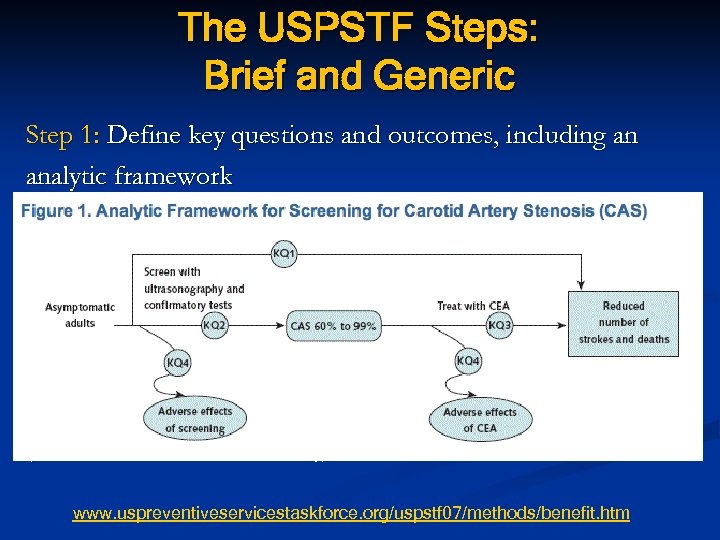
The USPSTF Steps: Brief and Generic Step 1: Define key questions and outcomes, including an analytic framework (Note: CEA = carotid endarterectomy) www. uspreventiveservicestaskforce. org/uspstf 07/methods/benefit. htm
The USPSTF Steps: Brief and Generic Step 2: Define, retrieve and summarize relevant evidence from the medical literature Step 3: Judge quality of individual studies: good, fair, poor Step 4: Synthesize and judge the adequacy of the evidence about benefits and harms: convincing, adequate, inadequate www. uspreventiveservicestaskforce. org/uspstf 07/methods/benefit. htm
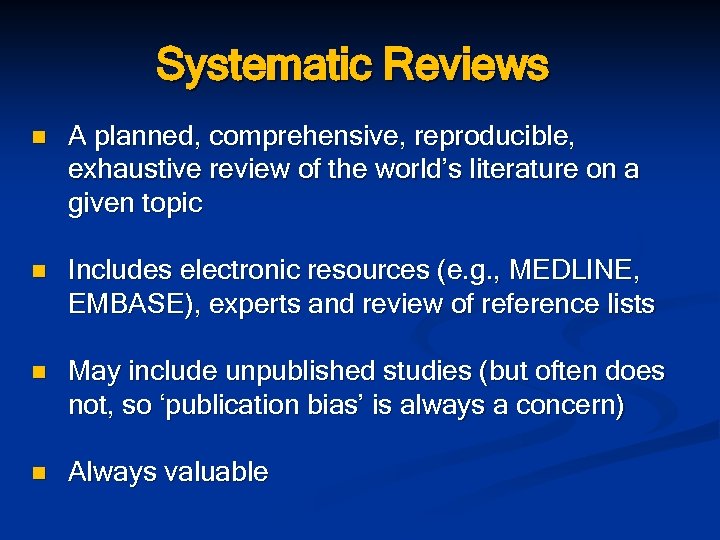
Systematic Reviews n A planned, comprehensive, reproducible, exhaustive review of the world’s literature on a given topic n Includes electronic resources (e. g. , MEDLINE, EMBASE), experts and review of reference lists n May include unpublished studies (but often does not, so ‘publication bias’ is always a concern) n Always valuable
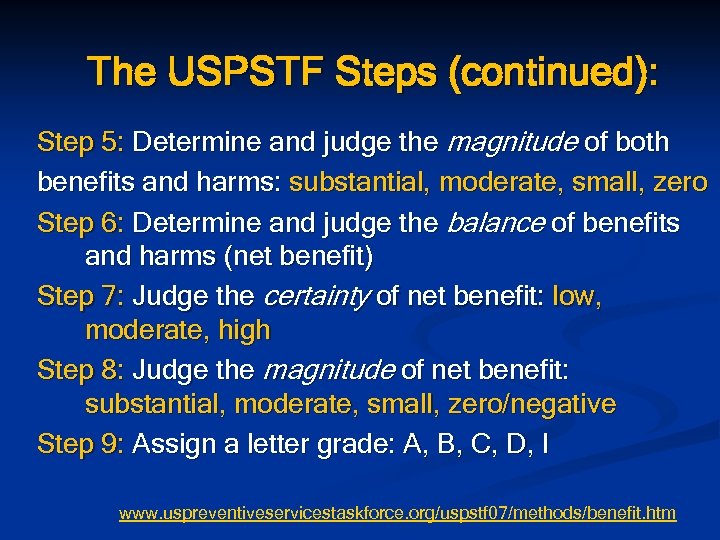
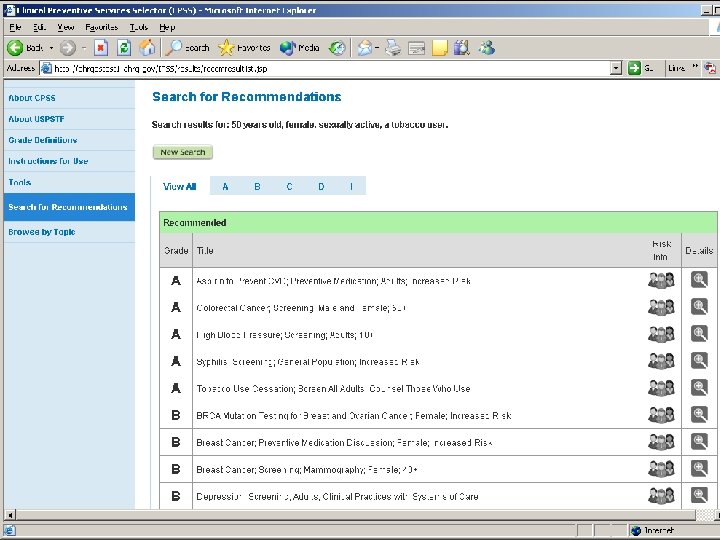
The USPSTF Steps (continued): Step 5: Determine and judge the magnitude of both benefits and harms: substantial, moderate, small, zero Step 6: Determine and judge the balance of benefits and harms (net benefit) Step 7: Judge the certainty of net benefit: low, moderate, high Step 8: Judge the magnitude of net benefit: substantial, moderate, small, zero/negative Step 9: Assign a letter grade: A, B, C, D, I www. uspreventiveservicestaskforce. org/uspstf 07/methods/benefit. htm
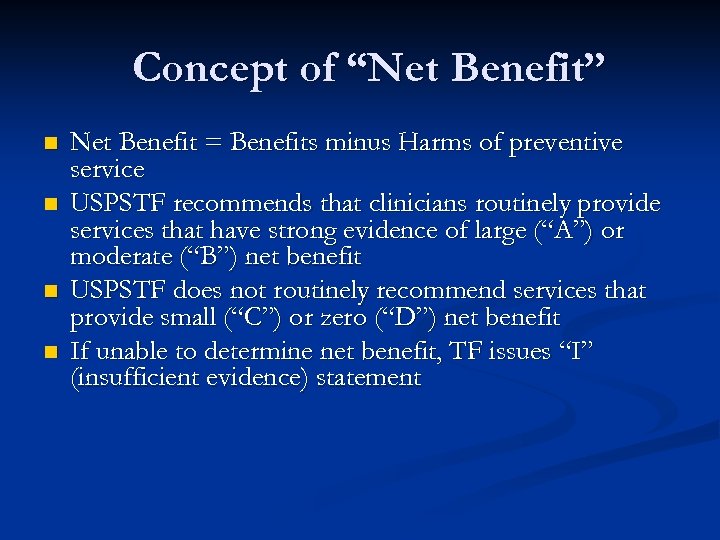
Concept of “Net Benefit” n n Net Benefit = Benefits minus Harms of preventive service USPSTF recommends that clinicians routinely provide services that have strong evidence of large (“A”) or moderate (“B”) net benefit USPSTF does not routinely recommend services that provide small (“C”) or zero (“D”) net benefit If unable to determine net benefit, TF issues “I” (insufficient evidence) statement
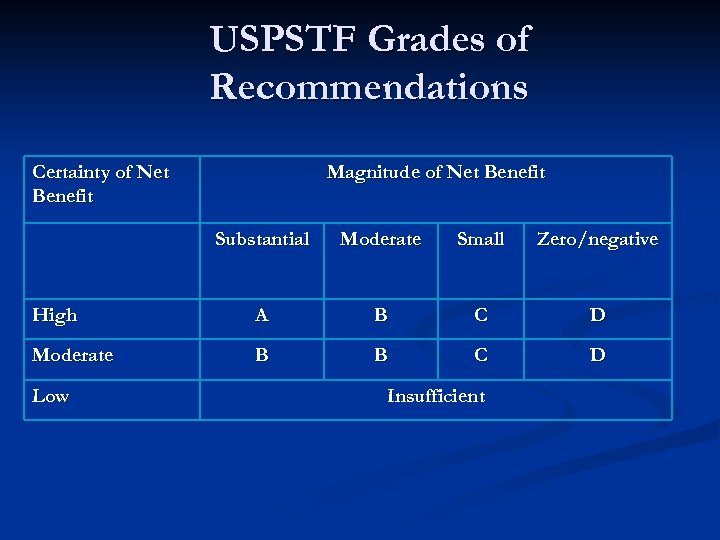
USPSTF Grades of Recommendations Certainty of Net Benefit Magnitude of Net Benefit Substantial Moderate Small Zero/negative High A B C D Moderate B B C D Low Insufficient
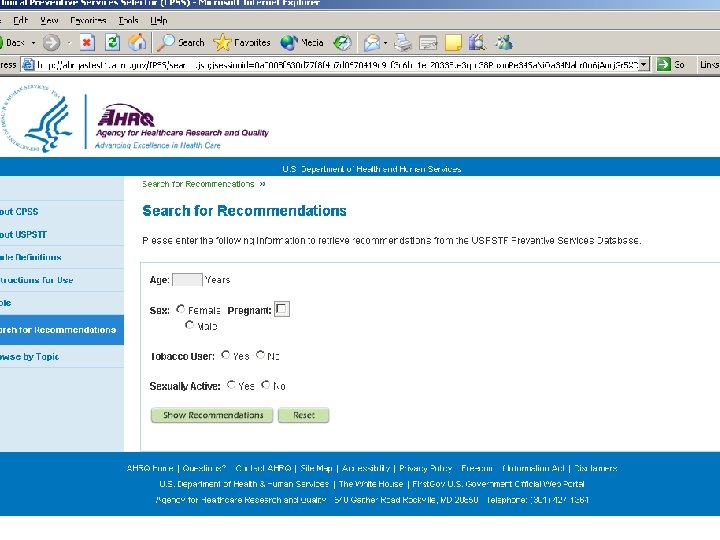
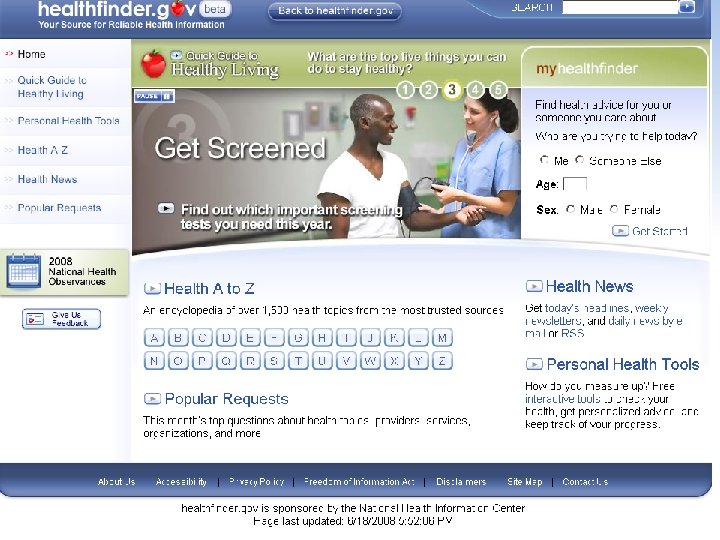
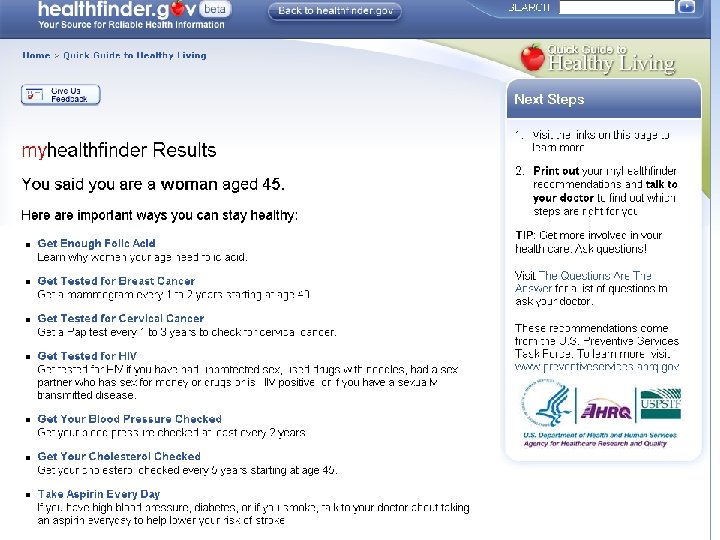
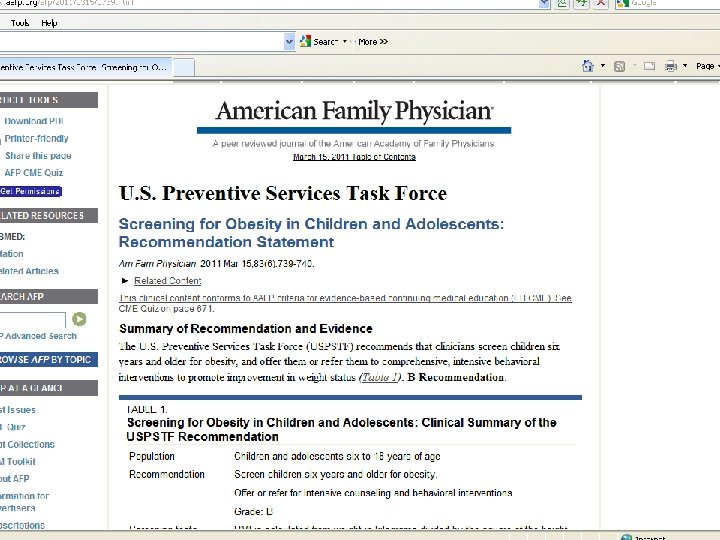
Accessing Prevention Guidelines at the Point of Care n Annual pocket-sized Guide to Clinical Preventive Services n www. uspreventiveservicestaskforce. org n Web-based and PDA Electronic Preventive Services Selector (e. PSS) n www. healthfinder. gov (for patients) Essential Evidence Plus online and mobile resource American Family Physician journal n n
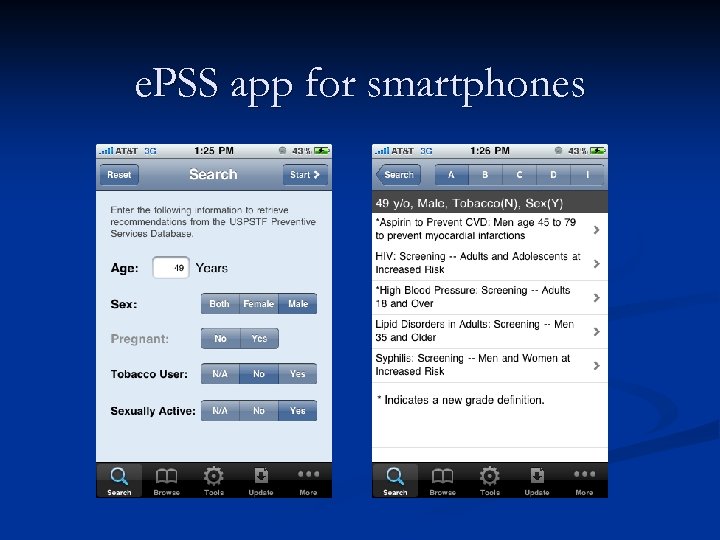
e. PSS app for smartphones
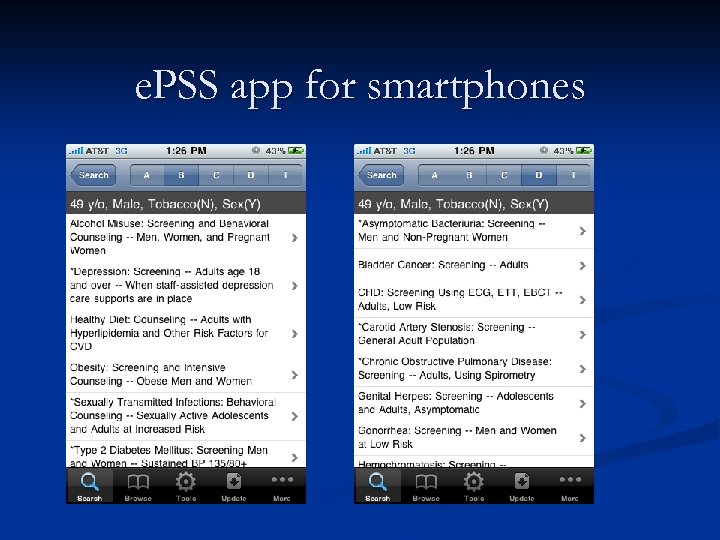
e. PSS app for smartphones

Contending with “prevention for profit” Not everything that might work does work – that’s why guidelines require evidence!
An advertisement in my church’s bulletin earlier this year n n n Life Line Screening, the nation's leading provider of preventive health screenings, will offer their affordable, non-invasive, painless health screenings. Five screenings will be offered that scan for potential health problems related to: blocked arteries, which is a leading cause of stroke; abdominal aortic aneurysms, which can lead to a ruptured aorta; hardening of the arteries in the legs, which is a strong predictor of heart disease; atrial fibrillation or irregular heart beat, which is closely tied to stroke risk; and a bone density screening, for men and women, used to assess the risk of osteoporosis. Register for a Wellness Package with Heart Rhythm for $149. Add Disease Risk Assessment with blood testing & biometrics for $79 more.

Sounds good … but what does the evidence say? USPSTF Systematic Reviews, 2005 through 2010
Stroke screenings? Just say no n "Blocked arteries" / stroke screening is most likely a carotid ultrasound scan, which doesn't help because most patients with asymptomatic carotid artery blockages will not suffer strokes. Although the screening test is "non-invasive and painless, " the confirmatory test, angiography, is not (it actually causes a stroke in a small number of patients) and unnecessary carotid endarterectomy can lead to death.
AAA screening? Not for most people n Abdominal aortic aneurysm screening is only recommended in men ages 65 to 75 who have ever smoked, because aneurysms are much less common in younger, female, and non-smoking populations. Even in men who are eligible for the test, it's important to weigh the potential benefits against the potential harms of corrective surgery, which has a not insignificant mortality rate itself.
Pass on screening for PVD n "Hardening of the arteries in the legs, " or screening for peripheral vascular disease with an arterial-brachial index, hasn't been proven to prevent heart attacks but will certainly lead to many false positive results.
Screening for atrial fibrillation? Are you kidding me? n I've never even heard of atrial fibrillation (irregular heart beat) screening, which I presume is doing a screening EKG, which is also totally unproven. Absolutely no organizations recommend this.
Even “good” screening tests should be cleared by clinicians n Screening for osteoporosis with bone density testing is the only test on the list that's actually worthwhile for a large number of adults, especially women over 65. But it's not appropriate to do this test without a prior consultation with a clinician who can discuss the risks and benefits of undergoing this type of screening. And there are still questions about whether men benefit to the same degree as women, or at all.
The Bottom Line Preventive services have great potential to improve national health outcomes n An evidence-based process is critical to select services of value and discourage ineffective and/or harmful tests n That process is based upon a careful, systematic search of the medical literature on a topic n Clinicians have many options for accessing prevention guidelines at the point of care n
Thank you! Questions?
0db154b2ce54c79cc7a73b5877fad528.ppt