6c2ea23b3460d11f5b81e64bde6f0c44.ppt
- Количество слайдов: 16
Using the BCSC Research Infrastructure as a Junior Investigator BCSC Meeting: Celebrating 15 Years of Accomplishment Bethesda, MD April 27, 2010 E. Shelley Hwang MD, MPH Chief, Division of Breast Surgery UCSF Helen Diller Family Comprehensive Cancer Center
Personal Background §Training: • Surgical oncology • Joined UCSF faculty at UCSF after completing fellowship • Little prior background in epidemiology/research methods §Research interest: • DCIS and preinvasive breast cancer • Obtained training grant 2004 • Interested in working with large datasets as part of master’s thesis for MPH
BCSC and me §Advantages to a junior investigator • Limited funding • Large existing datasets • Research mentorship • Statistical support • High likelihood of a completing a successful product §Junior researcher responsibilities: • Define research question • Identify time, resources • Bring energy, enthusiasm, focus to project
BCSC and me §Introduction to BCSC • Research infrastructure: UCSF Women’s Health Research Center (PI: Grady) • BCSC primary mentor (Kerlikowske): • Identify opportunities; bring together junior researchers and data • Navigate process of data request, analysis, interpretation • BCSC senior staff (Miglioretti, Ballard-Barbash): • Guide the analysis and presentation of data • Facilitate access to data dictionary, dataset • Establish team of BCSC researchers with like interests • Create opportunities to present research
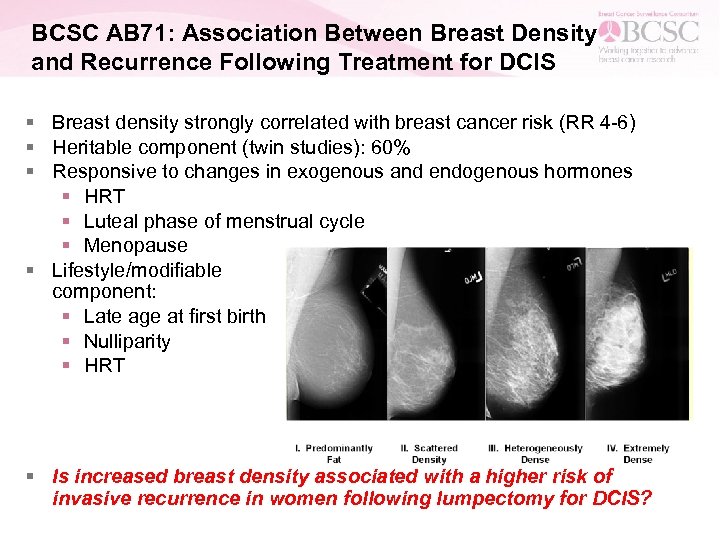
BCSC AB 71: Association Between Breast Density and Recurrence Following Treatment for DCIS § Breast density strongly correlated with breast cancer risk (RR 4 -6) § Heritable component (twin studies): 60% § Responsive to changes in exogenous and endogenous hormones § HRT § Luteal phase of menstrual cycle § Menopause § Lifestyle/modifiable component: § Late age at first birth § Nulliparity § HRT § Is increased breast density associated with a higher risk of invasive recurrence in women following lumpectomy for DCIS?
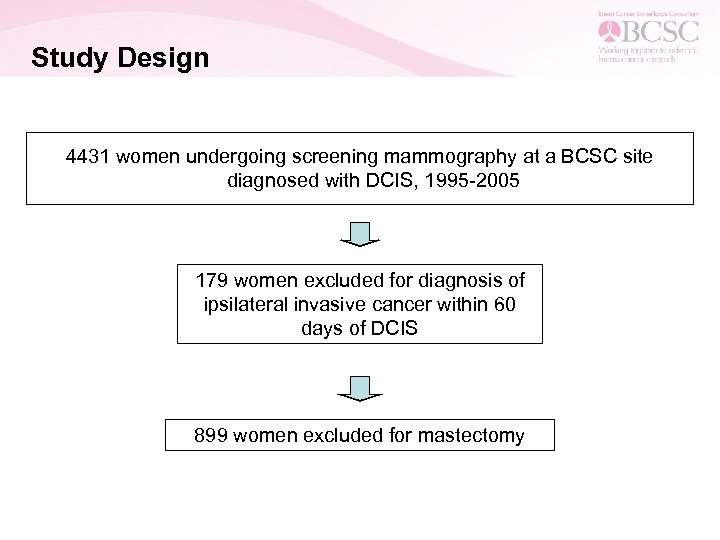
Study Design 4431 women undergoing screening mammography at a BCSC site diagnosed with DCIS, 1995 -2005 179 women excluded for diagnosis of ipsilateral invasive cancer within 60 days of DCIS 899 women excluded for mastectomy
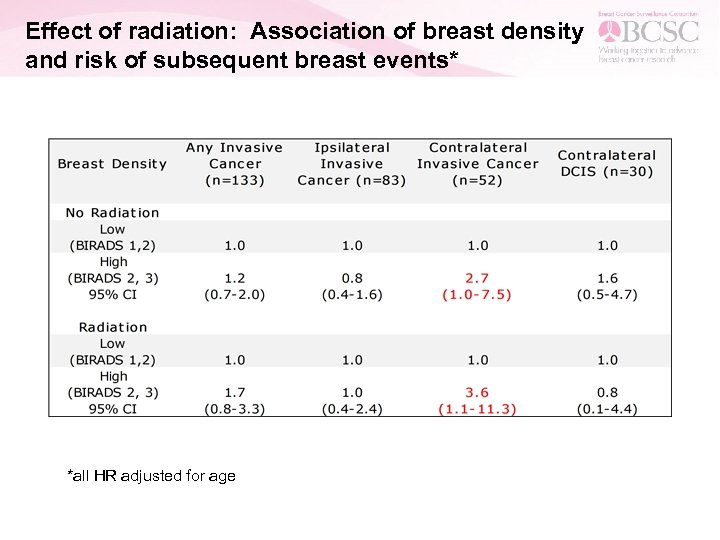
Effect of radiation: Association of breast density and risk of subsequent breast events* *all HR adjusted for age
Conclusions § Women with higher breast density are not more likely to develop invasive cancer in the ipsilateral breast following treatment for DCIS § High breast density is associated with a 3 -fold higher risk of contralateral invasive cancer compared to women with low density § Women undergoing treatment for DCIS with increased breast density may benefit most from strategies aimed towards contralateral risk reduction
I had such a great experience that I’m working with the BCSC again! § AB 81: The Association of Breast Density and Contralateral Breast Events in Women Undergoing Lumpectomy and Radiation § --Do women undergoing radiation as part of treatment for index cancer have increased risk of CBC compared to women who did not receive radiation? § --Are young age or breast density associated with this risk?
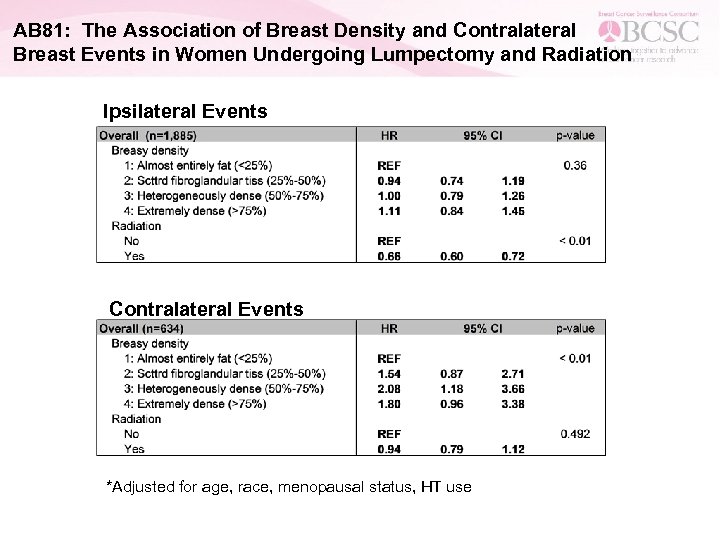
AB 81: The Association of Breast Density and Contralateral Breast Events in Women Undergoing Lumpectomy and Radiation Ipsilateral Events Contralateral Events *Adjusted for age, race, menopausal status, HT use
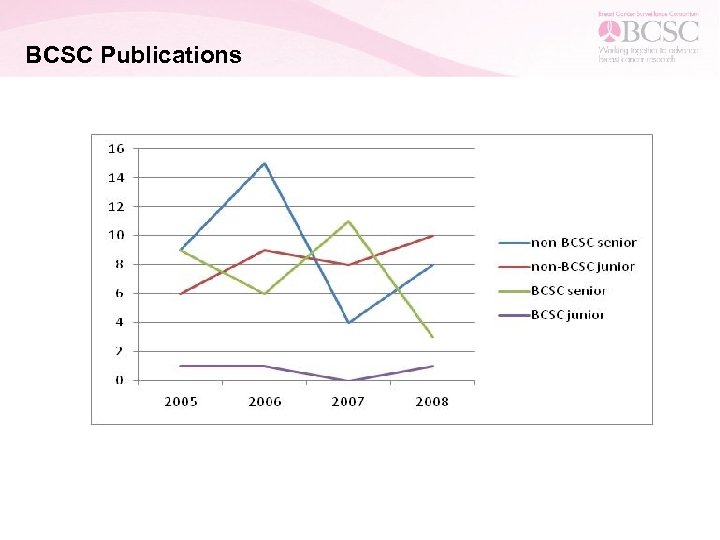
BCSC Publications
Recent High Impact BCSC publications by Junior Investigators (success is not the exception!) § Are there racial/ethnic disparities among women younger than 40 undergoing mammography? Kapp JM, Walker R, Haneuse S, Buist DS, Yankaskas BC. Breast Cancer Res Treat. 2010 Mar 4. [Epub ahead of print] § Rates of atypical ductal hyperplasia have declined with less use of postmenopausal hormone treatment: findings from the Breast Cancer Surveillance Consortium. Menes TS, Kerlikowske K, Jaffer S, Seger D, Miglioretti DL. Cancer Epidemiol Biomarkers Prev. 2009 Nov; 18(11): 2822 -8. § Using clinical factors and mammographic breast density to estimate breast cancer risk: development and validation of a new predictive model. Tice JA, Cummings SR, Smith. Bindman R, Ichikawa L, Barlow WE, Kerlikowske K. Ann Intern Med. 2008 Mar 4; 148(5): 337 -47. § Influence of computer-aided detection on performance of screening mammography. Fenton JJ, Taplin SH, Carney PA, Abraham L, Sickles EA, D'Orsi C, Berns EA, Cutter G, Hendrick RE, Barlow WE, Elmore JG. N Engl J Med. 2007 Apr 5; 356(14): 1399 -409.
Working with the BCSC § Outstanding resource for investigators, particularly junior researchers § Access to BCSC mentoring, large datasets, analytical support (Statistical Coordinating Center); ease of application process for data requests § Important to have clear research question, clear definitions and parameters for variables (years of diagnosis, definition of “recurrence”) § Potential resource to gather preliminary data for grant submissions • Specific Data Requests • Risk Estimation Data Set • Cancer Incidence Data
Summary § BCSC has made key contributions in breast screening and breast cancer outcomes research; this is expected to continue well into the future as new questions emerge • cost-effectiveness • resource allocation • quality metrics § Excellent ROI as many projects attain funding apart from BCSC; BCSC essential to providing the resources and data to secure such funding § The resource and infrastructure have made important contributions to academic training and career advancement; this resource is vital in institutions with strong BCSC mentorship § Need to continue outreach efforts to non-BCSC investigators
Acknowledgements § Karla Kerlikowske § Diana Miglioretti § Rachel Ballard-Barbash § Donald Weaver § Ed Sickles § Steve Taplin § Staff and Researchers of the Statistical Coordinating Center § Sebastian Haneuse § Ina Gylys-Colwell § Patients who continue to contribute their valuable time and data to support the BCSC
Thank you!
6c2ea23b3460d11f5b81e64bde6f0c44.ppt