6ca97d8f829eeb9bf409329ad31efdaf.ppt
- Количество слайдов: 13
 USING THE AERONAUTICAL MODEL TO DECREASE MEDICAL ERROR IN FAMILY MEDICINE RESIDENTS A Pilot Study Stephen Stripe MD, FAAFP Shirley Cole-Harding Ph. D Vicki Michels Ph. D
USING THE AERONAUTICAL MODEL TO DECREASE MEDICAL ERROR IN FAMILY MEDICINE RESIDENTS A Pilot Study Stephen Stripe MD, FAAFP Shirley Cole-Harding Ph. D Vicki Michels Ph. D
 The Problem • IOM in 1999 showed that 44, 000 to 98, 000 people die/year due to medical error. • $17 to $29 Billion dollars are spent due to medical error per year. Not including the legal fees. • An article in the Journal of Medical Practice Management 2004 stated that as much as $97. 5 Billion in hospital and physician service costs per year is due to malpractice litigation.
The Problem • IOM in 1999 showed that 44, 000 to 98, 000 people die/year due to medical error. • $17 to $29 Billion dollars are spent due to medical error per year. Not including the legal fees. • An article in the Journal of Medical Practice Management 2004 stated that as much as $97. 5 Billion in hospital and physician service costs per year is due to malpractice litigation.
 Aeronautical Model • 85% of all accidents and 52% of all general aviation accidents are due to pilot error, i. e. poor decision making or risk management. • FAA instituted 12 years of research. – Most errors were cognitive in nature; the result of attitudes, behavioral traps, stresses and other influences. – Since 1987 pilots have been teaching risk management techniques.
Aeronautical Model • 85% of all accidents and 52% of all general aviation accidents are due to pilot error, i. e. poor decision making or risk management. • FAA instituted 12 years of research. – Most errors were cognitive in nature; the result of attitudes, behavioral traps, stresses and other influences. – Since 1987 pilots have been teaching risk management techniques.
 Aeronautical Model • 10 -50% decrease in accident rate since the introduction of the curriculum to pilots. • The largest general aviation insurance company in the U. S. has seen a 50% decline in claims of those pilots who have taken the course versus those who have not.
Aeronautical Model • 10 -50% decrease in accident rate since the introduction of the curriculum to pilots. • The largest general aviation insurance company in the U. S. has seen a 50% decline in claims of those pilots who have taken the course versus those who have not.
 Medicine • A recent study (Stripe et al. , 2006) showed that up to 59% of the same type of factors identified in aviation accidents can be identified in medical malpractice cases that go to trial in a legal data base.
Medicine • A recent study (Stripe et al. , 2006) showed that up to 59% of the same type of factors identified in aviation accidents can be identified in medical malpractice cases that go to trial in a legal data base.
 Method - Participants • Family Medicine Residents; PGY 1, 2, and 3 from FM program were enrolled. • The last 4 months of the academic year. • Paid $5/day that they reported errors. • 14/15 residents entered study. • 8/14 completed the entire study period reporting every day.
Method - Participants • Family Medicine Residents; PGY 1, 2, and 3 from FM program were enrolled. • The last 4 months of the academic year. • Paid $5/day that they reported errors. • 14/15 residents entered study. • 8/14 completed the entire study period reporting every day.
 Method - Procedure • Self reporting errors on a form placed in a lock box that the primary investigator could not access. Each resident had a code name. The errors reports were collected twice a week by personnel not directly involved with the residents. • A certificate of confidentiality was obtained. • Type of errors were reported; procedural, orders, assessment, prescription, miscommunication, other and none. • They also reported the following items: illness, medication, stress, psychoactive subst. , fatigue, hunger/thirst, need to relieve oneself, strong emotion and other. • Reported errors for one month. • Had two sessions of training during a two week period. • Reported errors for one month following.
Method - Procedure • Self reporting errors on a form placed in a lock box that the primary investigator could not access. Each resident had a code name. The errors reports were collected twice a week by personnel not directly involved with the residents. • A certificate of confidentiality was obtained. • Type of errors were reported; procedural, orders, assessment, prescription, miscommunication, other and none. • They also reported the following items: illness, medication, stress, psychoactive subst. , fatigue, hunger/thirst, need to relieve oneself, strong emotion and other. • Reported errors for one month. • Had two sessions of training during a two week period. • Reported errors for one month following.
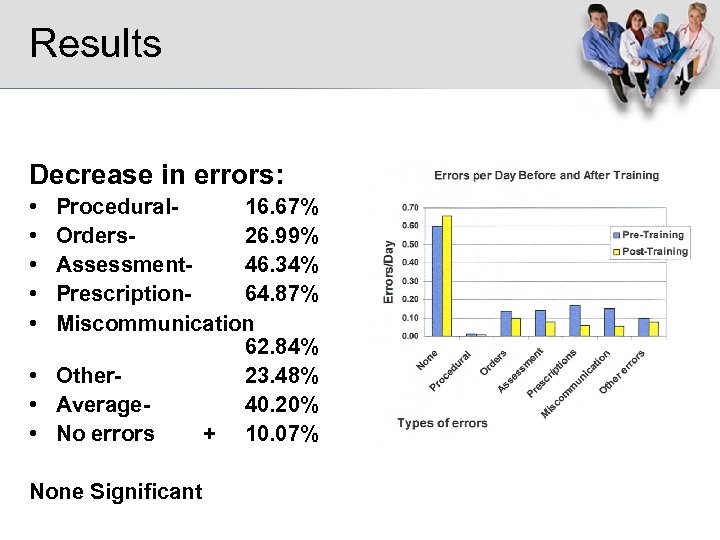 Results Decrease in errors: • • • Procedural 16. 67% Orders 26. 99% Assessment 46. 34% Prescription 64. 87% Miscommunication 62. 84% • Other 23. 48% • Average 40. 20% • No errors + 10. 07% None Significant
Results Decrease in errors: • • • Procedural 16. 67% Orders 26. 99% Assessment 46. 34% Prescription 64. 87% Miscommunication 62. 84% • Other 23. 48% • Average 40. 20% • No errors + 10. 07% None Significant
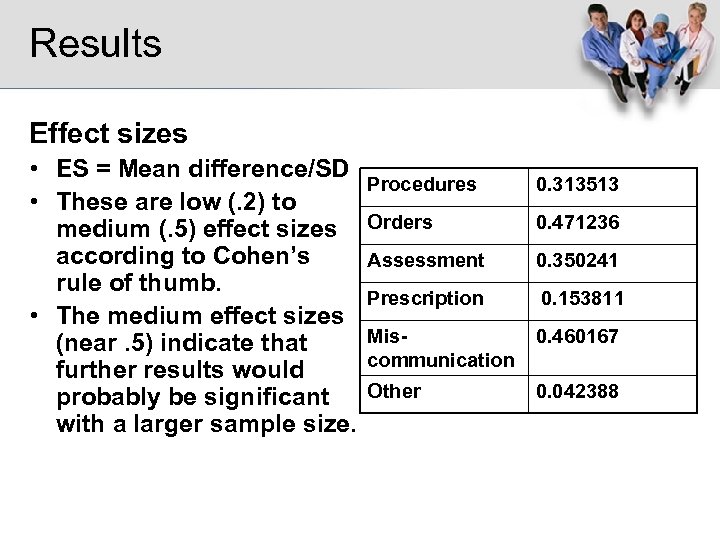 Results Effect sizes • ES = Mean difference/SD • These are low (. 2) to medium (. 5) effect sizes according to Cohen’s rule of thumb. • The medium effect sizes (near. 5) indicate that further results would probably be significant with a larger sample size. Procedures 0. 313513 Orders 0. 471236 Assessment 0. 350241 Prescription 0. 153811 Miscommunication 0. 460167 Other 0. 042388
Results Effect sizes • ES = Mean difference/SD • These are low (. 2) to medium (. 5) effect sizes according to Cohen’s rule of thumb. • The medium effect sizes (near. 5) indicate that further results would probably be significant with a larger sample size. Procedures 0. 313513 Orders 0. 471236 Assessment 0. 350241 Prescription 0. 153811 Miscommunication 0. 460167 Other 0. 042388
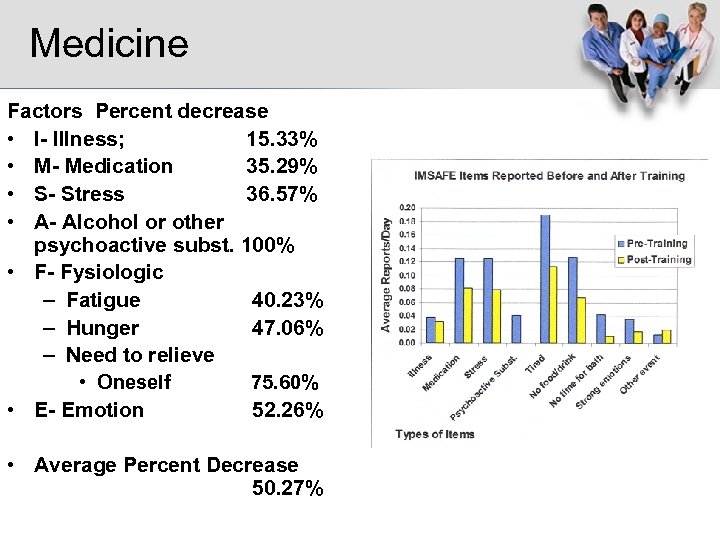 Medicine Factors Percent decrease • I- Illness; 15. 33% • M- Medication 35. 29% • S- Stress 36. 57% • A- Alcohol or other psychoactive subst. 100% • F- Fysiologic – Fatigue 40. 23% – Hunger 47. 06% – Need to relieve • Oneself 75. 60% • E- Emotion 52. 26% • Average Percent Decrease 50. 27%
Medicine Factors Percent decrease • I- Illness; 15. 33% • M- Medication 35. 29% • S- Stress 36. 57% • A- Alcohol or other psychoactive subst. 100% • F- Fysiologic – Fatigue 40. 23% – Hunger 47. 06% – Need to relieve • Oneself 75. 60% • E- Emotion 52. 26% • Average Percent Decrease 50. 27%
 Medicine • Problems – Not statistically significant – Small sample size – No control group. – Didn’t separate out differences between PGY. – Change over time. – Self Reporting
Medicine • Problems – Not statistically significant – Small sample size – No control group. – Didn’t separate out differences between PGY. – Change over time. – Self Reporting
 Proposal • Get grant for a larger study – Effect sizes indicate this is a potentially significant project • Need 200 subjects for a statistical significant number of 100 considering 50% drop out rate. • Control group would receive training at the end. • Two experimental groups with cross over.
Proposal • Get grant for a larger study – Effect sizes indicate this is a potentially significant project • Need 200 subjects for a statistical significant number of 100 considering 50% drop out rate. • Control group would receive training at the end. • Two experimental groups with cross over.
 Conclusion • This is not meant to replace the systems approach. Both cognitive and systems is needed. • 40. 2% decrease in error translates into possibly 17, 688 to 39, 396 lives saved per year and $6. 8 to $11. 7 Billion saved per year.
Conclusion • This is not meant to replace the systems approach. Both cognitive and systems is needed. • 40. 2% decrease in error translates into possibly 17, 688 to 39, 396 lives saved per year and $6. 8 to $11. 7 Billion saved per year.


