27a0ec2a51c48c37f353d7305dc3f4d9.ppt
- Количество слайдов: 40
Using Predictive Modeling to Target Interventions Barry P. Chaiken, MD, MPH Chief Medical Officer ABQAURP - PSOS
Overview n Cost and Quality Trends n Disease Management and Modeling n Predictive Modeling Fundamentals n Accuracy of Models - Case Study 2
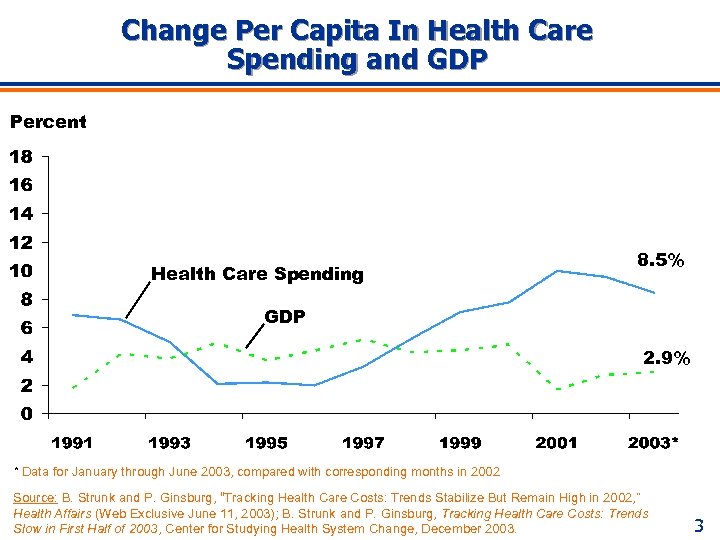
Change Per Capita In Health Care Spending and GDP Percent Health Care Spending 8. 5% GDP 2. 9% * Data for January through June 2003, compared with corresponding months in 2002 Source: B. Strunk and P. Ginsburg, “Tracking Health Care Costs: Trends Stabilize But Remain High in 2002, ” Health Affairs (Web Exclusive June 11, 2003); B. Strunk and P. Ginsburg, Tracking Health Care Costs: Trends Slow in First Half of 2003, Center for Studying Health System Change, December 2003. 3
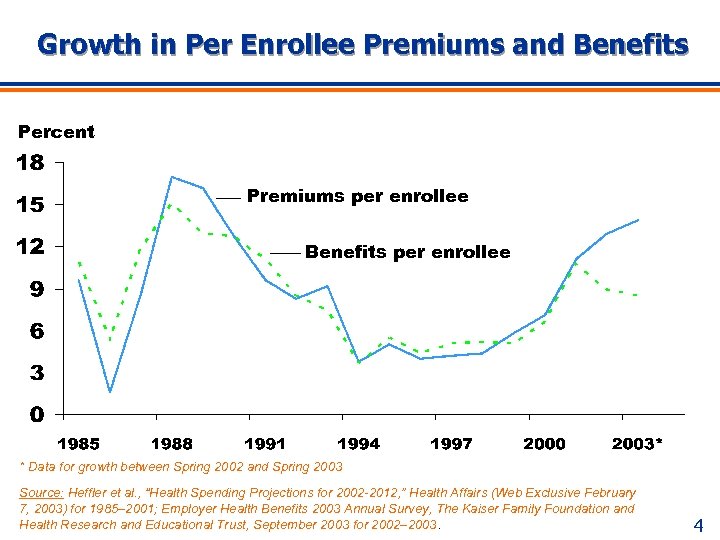
Growth in Per Enrollee Premiums and Benefits Percent Premiums per enrollee Benefits per enrollee * Data for growth between Spring 2002 and Spring 2003 Source: Heffler et al. , “Health Spending Projections for 2002 -2012, ” Health Affairs (Web Exclusive February 7, 2003) for 1985– 2001; Employer Health Benefits 2003 Annual Survey, The Kaiser Family Foundation and Health Research and Educational Trust, September 2003 for 2002– 2003. 4
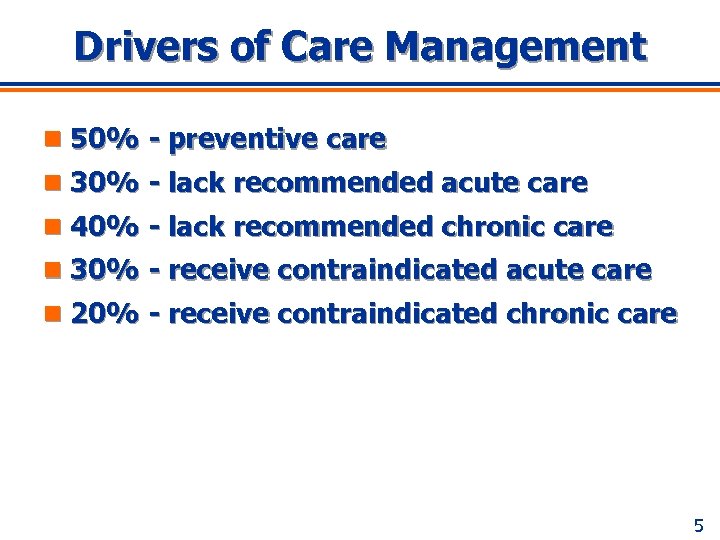
Drivers of Care Management n 50% - preventive care n 30% - lack recommended acute care n 40% - lack recommended chronic care n 30% - receive contraindicated acute care n 20% - receive contraindicated chronic care 5
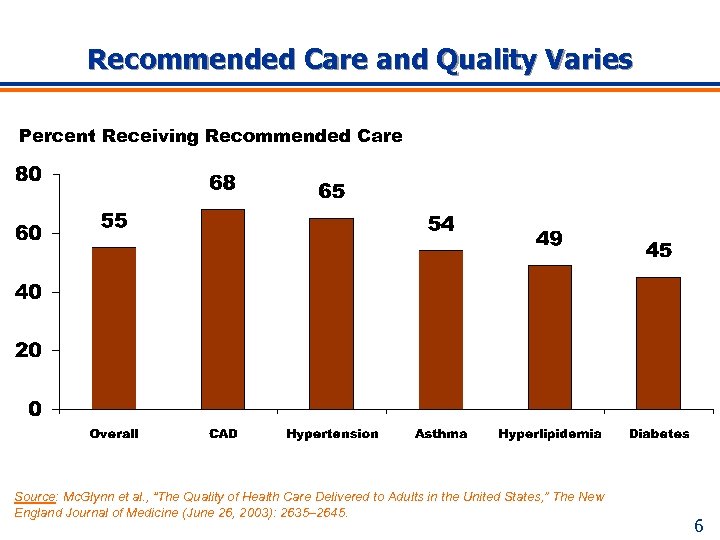
Recommended Care and Quality Varies Percent Receiving Recommended Care Source: Mc. Glynn et al. , “The Quality of Health Care Delivered to Adults in the United States, ” The New England Journal of Medicine (June 26, 2003): 2635– 2645. 6
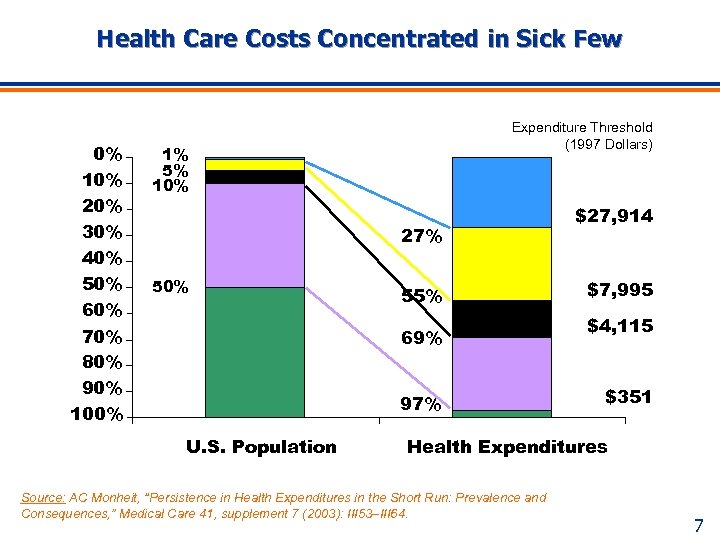
Health Care Costs Concentrated in Sick Few 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Expenditure Threshold (1997 Dollars) 1% 5% 10% 27% 50% 55% 69% 97% U. S. Population $27, 914 $7, 995 $4, 115 $351 Health Expenditures Source: AC Monheit, “Persistence in Health Expenditures in the Short Run: Prevalence and Consequences, ” Medical Care 41, supplement 7 (2003): III 53–III 64. 7
Overview n Cost and Quality Trends n Disease Management and Modeling n Predictive Modeling Fundamentals n Accuracy of Models - Case Study 8
DM Defined “Knowledge-based process intended to improve continuously the value of health care delivery from the perspectives of those who receive, purchase, provide, supply and evaluate it. ” --James B. Couch, MD 9
DM Criteria Specific n High dollar and volume n Preventable complications n Short time frame for results n Treatment variability n Extensive patient non-compliance n Practical guidelines n Measurable quality metrics 10
DM Processes n Identify patients n Develop therapeutic programs n Improve outcomes n Achieve acceptable cost levels n Provide evidence based care 11
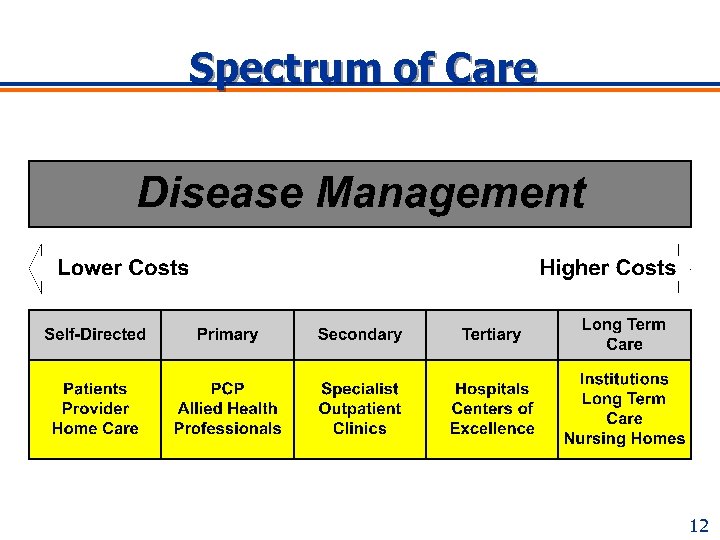
Spectrum of Care 12
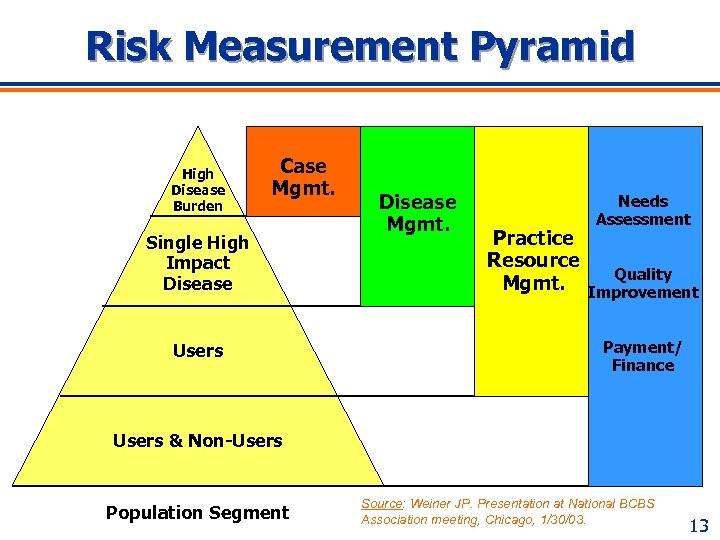
Risk Measurement Pyramid High Disease Burden Case Mgmt. Single High Impact Disease Users Disease Mgmt. Practice Resource Mgmt. Needs Assessment Quality Improvement Payment/ Finance Users & Non-Users Population Segment Source: Weiner JP. Presentation at National BCBS Association meeting, Chicago, 1/30/03. 13
Overview n Cost and Quality Trends n Disease Management and Modeling n Predictive Modeling Fundamentals n Accuracy of Models - Case Study 14
Predictive Modeling Defined Use of clinical information available for all members of a population to predict future healthcare needs, overall or for specific types of services. Source: CB Forrest, “Population-based Predictive Modeling Using ACGs: Application to Disease and Case Management”, International ACG User’s Conference, November 11, 2003 15
Reasons for Predictive Modeling n Existing high utilization by the few n Uses available data to identify high-risk n Allows intervention early in disease cycle n Enhances case and disease management 16
Predictive Modeling Focus n Case management targeting l Identify persons for care programs n Disease management risk stratification l Intensity tiers n Financial forecasting l Actuarial risk Source: CB Forrest, “Population-based Predictive Modeling Using ACGs: Application to Disease and Case Management”, International ACG User’s Conference, November 11, 2003 17
What Predictive Modeling Does n Stratify members l Enhance impact of interventions n Probabilistic identification of high utilizers l n n Assign risk scores – Describe comparative severity of illness Identify members not receiving proper care Highlight inconsistency of care Prospectively identify adverse events Allow focused interventions l Maximize benefits of disease management n Discover inefficient care 18
Additional Uses of Modeling n Influence adoption of best practices n Track effectiveness of interventions n Establish pay for performance n Set more accurate premiums n Develop contracts with providers l Actuarial n Help plan network composition l Based on member needs 19
Target Populations n Risk stratify l Subpopulation l Risk factors l Identify most likely to benefit n Develop specific, targeted interventions l Probabilities for certain outcomes l Practice guidelines l Practice standardization – Decrease variation 20
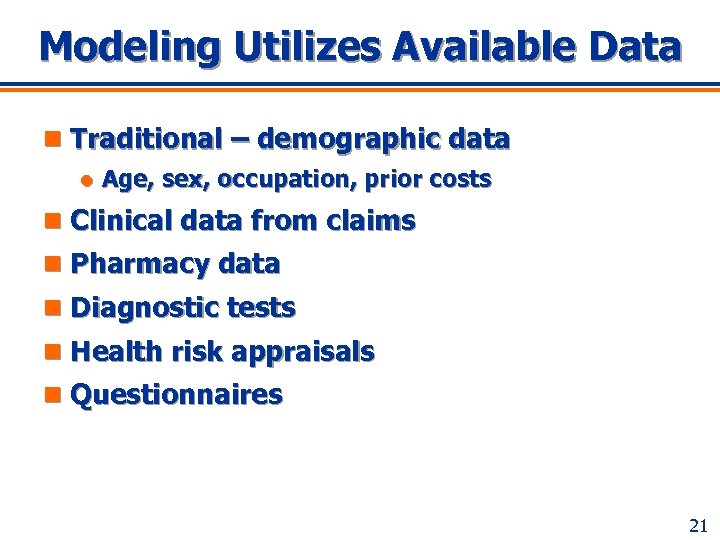
Modeling Utilizes Available Data n Traditional – demographic data l Age, sex, occupation, prior costs n Clinical data from claims n Pharmacy data n Diagnostic tests n Health risk appraisals n Questionnaires 21
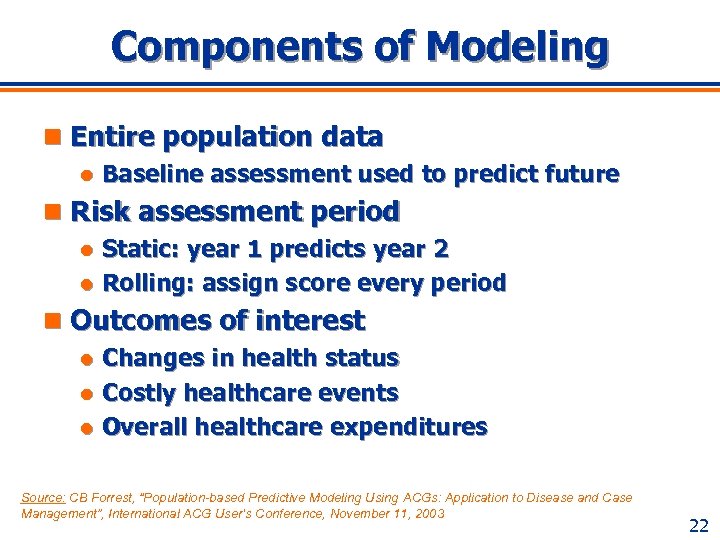
Components of Modeling n Entire population data l Baseline assessment used to predict future n Risk assessment period Static: year 1 predicts year 2 l Rolling: assign score every period l n Outcomes of interest Changes in health status l Costly healthcare events l Overall healthcare expenditures l Source: CB Forrest, “Population-based Predictive Modeling Using ACGs: Application to Disease and Case Management”, International ACG User’s Conference, November 11, 2003 22
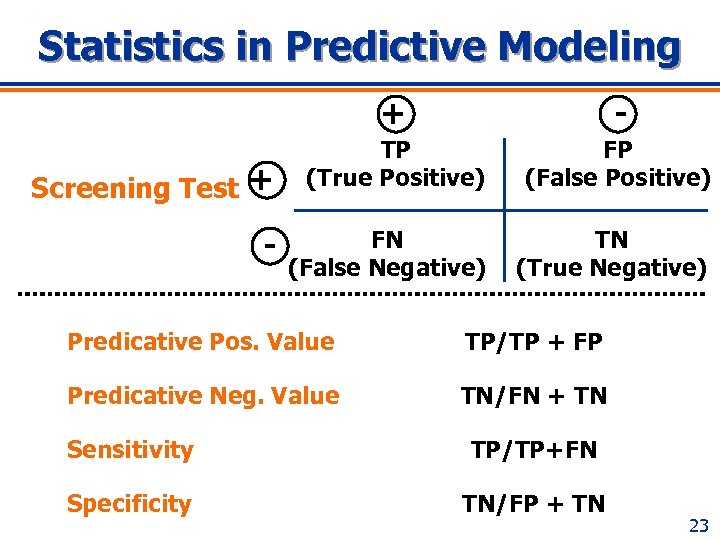
Statistics in Predictive Modeling + Screening Test + - - TP (True Positive) FP (False Positive) FN (False Negative) TN (True Negative) Predicative Pos. Value TP/TP + FP Predicative Neg. Value TN/FN + TN Sensitivity TP/TP+FN Specificity TN/FP + TN 23
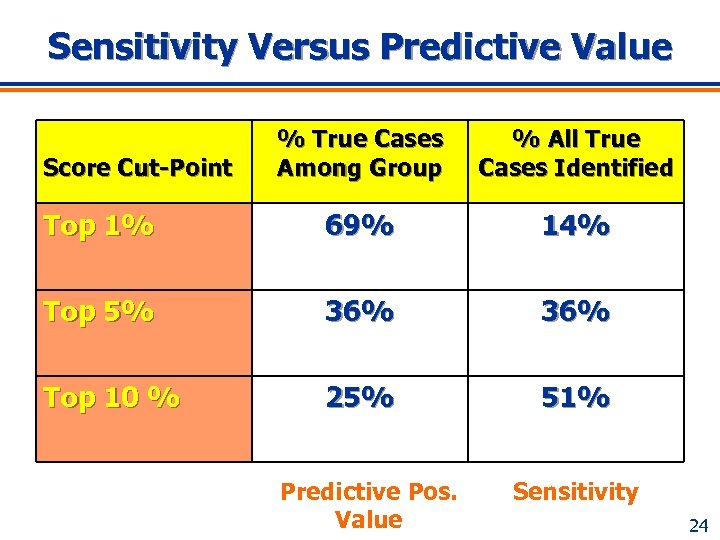
Sensitivity Versus Predictive Value % True Cases Among Group % All True Cases Identified Top 1% 69% 14% Top 5% 36% Top 10 % 25% 51% Score Cut-Point Predictive Pos. Value Sensitivity 24
First Generation Modeling n Utilize demographic data l Age, sex, diagnoses n Rely upon historical financial data n Predict risk 25
Second Generation Modeling n Utilize first generation data sources n Incorporate second generation sources l Pharmacy data l Lab data l Test data n Predictions based on risk adjustment l DCGs, ACGs, ETGs 26
Third Generation Modeling n Utilize first and second generation sources n Incorporate other sources and models Health risk appraisals, questionnaires l Surveys l Regional variability l ACGs, DCGs, ETGs l n Model the models Choose the best modeling of models for results l Learn from previous data modeling l 27
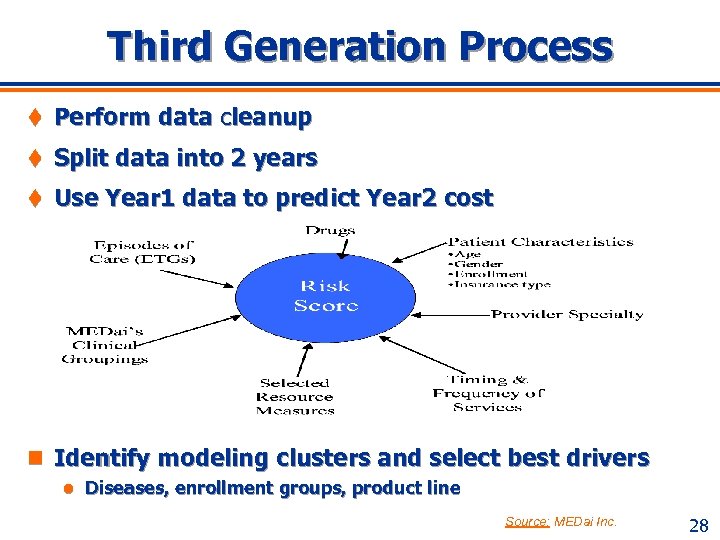
Third Generation Process t Perform data cleanup t Split data into 2 years t Use Year 1 data to predict Year 2 cost n Identify modeling clusters and select best drivers l Diseases, enrollment groups, product line Source: MEDai Inc. 28
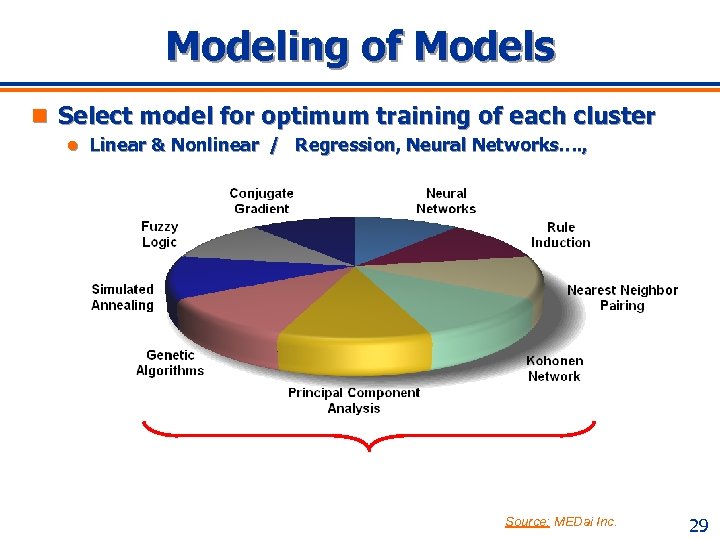
Modeling of Models n Select model for optimum training of each cluster l Linear & Nonlinear / Regression, Neural Networks…. , Source: MEDai Inc. 29
Overview n Cost and Quality Trends n Disease Management and Modeling n Predictive Modeling Fundamentals n Accuracy of Models - Case Study 30
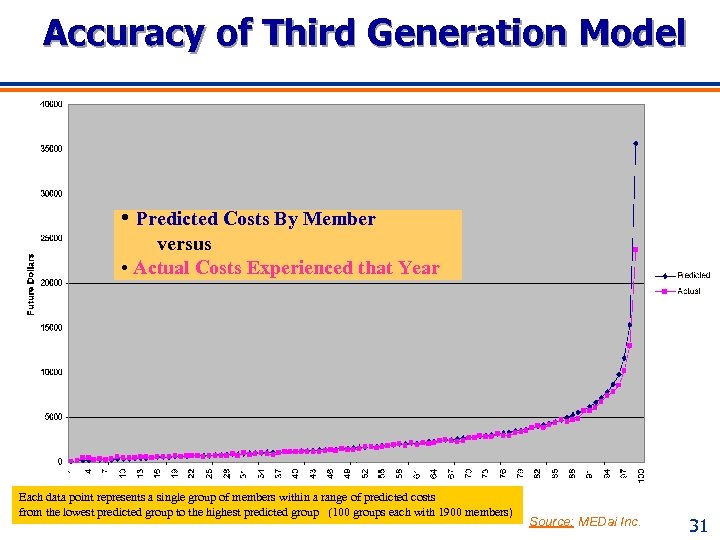
Accuracy of Third Generation Model • Predicted Costs By Member versus • Actual Costs Experienced that Year Each data point represents a single group of members within a range of predicted costs from the lowest predicted group to the highest predicted group (100 groups each with 1900 members) Source: MEDai Inc. 31
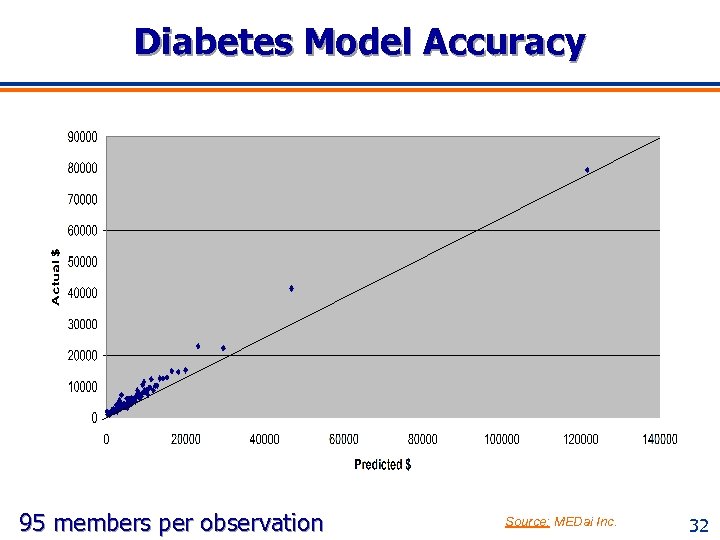
Diabetes Model Accuracy 95 members per observation Source: MEDai Inc. 32
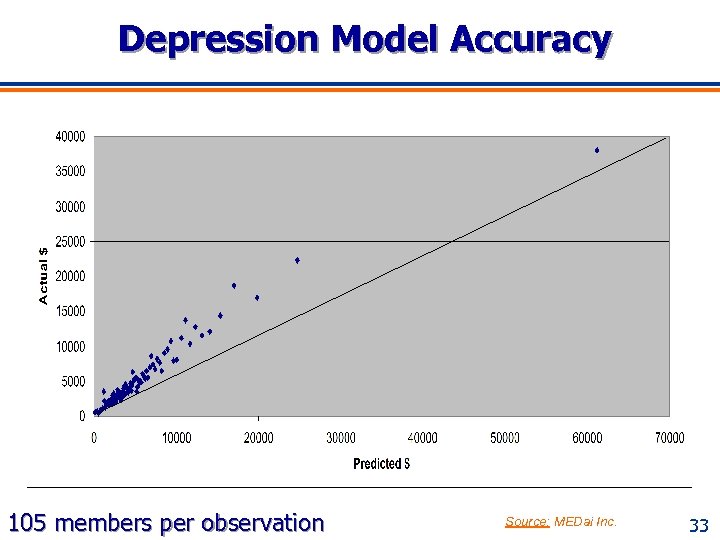
Depression Model Accuracy 105 members per observation Source: MEDai Inc. 33
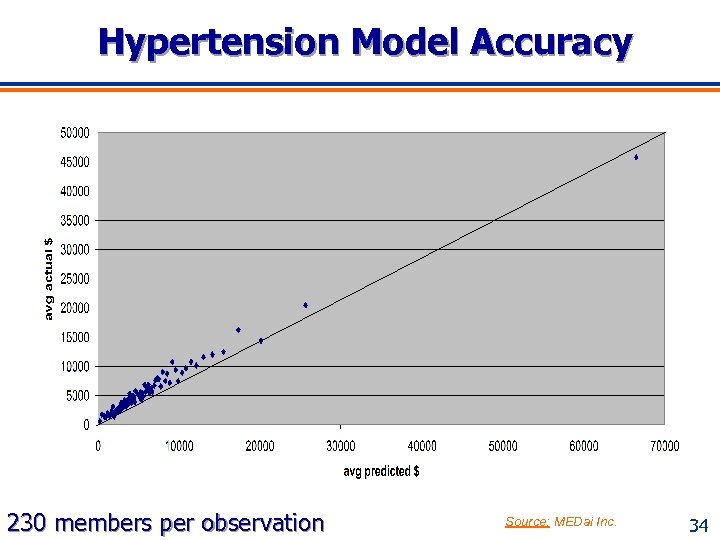
Hypertension Model Accuracy 230 members per observation Source: MEDai Inc. 34
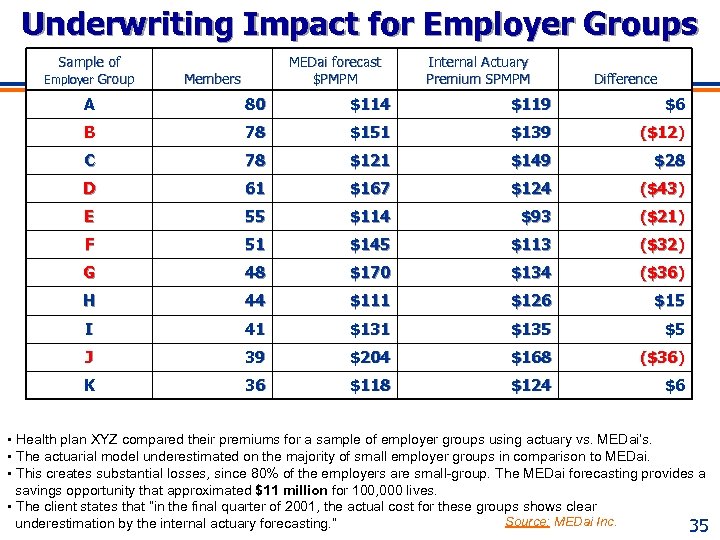
Underwriting Impact for Employer Groups Sample of Employer Group MEDai forecast $PMPM Members Internal Actuary Premium SPMPM Difference A 80 $114 $119 $6 B 78 $151 $139 ($12) C 78 $121 $149 $28 D 61 $167 $124 ($43) E 55 $114 $93 ($21) F 51 $145 $113 ($32) G 48 $170 $134 ($36) H 44 $111 $126 $15 I 41 $135 $5 J 39 $204 $168 ($36) K 36 $118 $124 $6 • Health plan XYZ compared their premiums for a sample of employer groups using actuary vs. MEDai’s. • The actuarial model underestimated on the majority of small employer groups in comparison to MEDai. • This creates substantial losses, since 80% of the employers are small-group. The MEDai forecasting provides a savings opportunity that approximated $11 million for 100, 000 lives. • The client states that “in the final quarter of 2001, the actual cost for these groups shows clear Source: MEDai Inc. underestimation by the internal actuary forecasting. ” 35
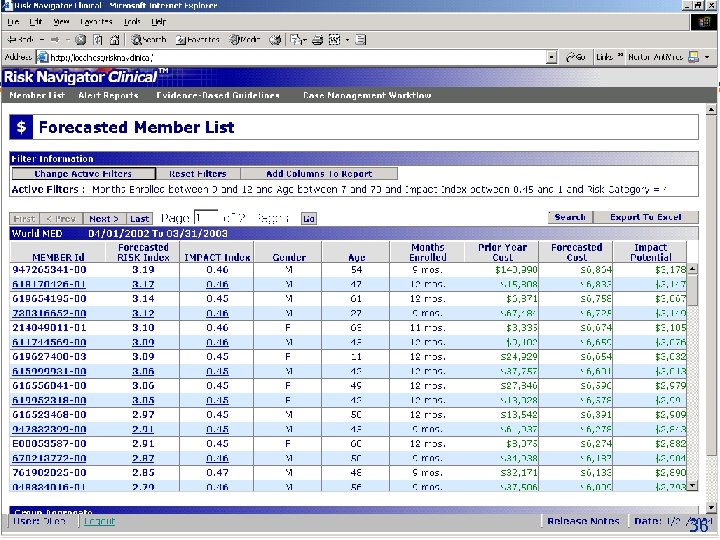
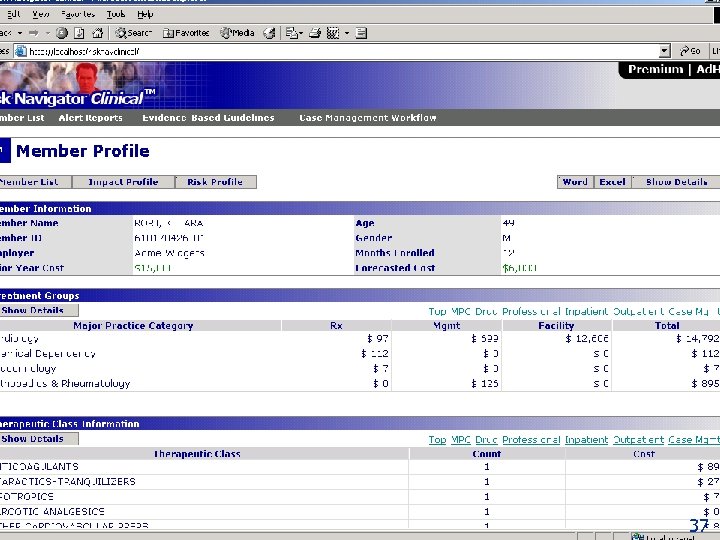
36
37
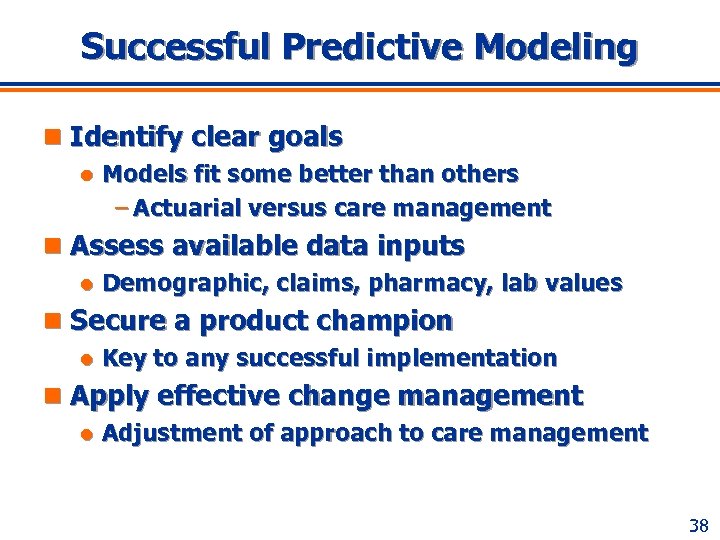
Successful Predictive Modeling n Identify clear goals l Models fit some better than others – Actuarial versus care management n Assess available data inputs l Demographic, claims, pharmacy, lab values n Secure a product champion l Key to any successful implementation n Apply effective change management l Adjustment of approach to care management 38
References n Monheit AC, Persistence in health expenditures in the short run: n n n Prevalence and consequences, Medical Care 41, supplement 7 (2003): III 53–III 64. Strunk B, Ginsburg P, Tracking health care costs: Trends stabilize but remain high in 2002, Health Affairs (Web Exclusive June 11, 2003) Strunk B, Ginsburg P, Tracking health care costs: Trends slow in first half of 2003, Center for Studying Health System Change, December 2003. Heffler et al. , Health spending projections for 2002 -2012, Health Affairs (Web Exclusive February 7, 2003) for 1985– 2001. Heffler et al. , Employer health benefits 2003 annual survey, The Kaiser Family Foundation and Health Research and Educational Trust, September 2003 for 2002– 2003. Mc. Glynn et al. , “The Quality of Health Care Delivered to Adults in the United States, ” The New England Journal of Medicine (June 26, 2003): 2635– 2645 39
References n Weiner JP, “Predictive modeling and risk measurement: n n n Paradigms, potential and pitfalls. ” Presented at a symposium on “Predictive Modeling” sponsored by the National Blue Cross/Blue Shield Association, Chicago, January 30, 2003. Forrest CB, “Population-based predictive modeling using ACGs: Application to disease and case management, ” International ACG User’s Conference, November 11, 2003. Le. Grow G, Metzger J, E-Disease Management, First Consulting Group, © 2001, California Health. Care Foundation Couch JB, The Physician’s Guide to Disease Management. © 1997, Aspen Publishing, Inc. , Gaithersburg, MD Kongstevdt PR, The Managed Health Care Handbook, 3 rd. © 1996, Aspen Publishers, Inc. , Gaithersburg, MD www. medai. com 40
27a0ec2a51c48c37f353d7305dc3f4d9.ppt