f001ed75432e9effb93b2615c77ea277.ppt
- Количество слайдов: 28
Using Personal Reflective Debrief To Promote Resilience from Compassion Fatigue Madeline Schmidt, MSN, APNP Marquette University
Disclosure Information for this presentation • There are no relevant financial relationships related to this presentation/program. • There is no sponsorship/commercial support of this presentation/program. • The content being presented will be fair, wellbalanced and evidence-based. • Learners must have signed the attendance roster at registration this morning and will need to complete the on-line evaluation after the conference to successfully complete this program and receive the contact hours certificate.
Presentation Objectives • • Problem in healthcare-Compassion fatigue Literature synthesis My capstone project Implications for future projects
Compassion Fatigue • Occupational hazard of providing empathetic, relationship-based care is compassion fatigue • Comprised of compassion satisfaction, secondary traumatic stress and burnout • Nurses are at high risk of development based on internal and external stresses as well as compassionate care (Berg, Harshbarger, Ahlers-Schmidt, & Lippoldt, 2016; Duffy, Avalos, & Dowling, 2014)
Literature Synthesis • Repeated exposure to chaos, high acuity patients, workplace violence, trauma and death can be challenging and emotionally draining • All healthcare providers should receive prevention and treatment and support should be normal and not a weakness • “Millennial” generation more likely to experience burnout than “baby boomers” • Professional Quality of Life (Pro. QOL) survey was most widely way to assess compassion fatigue in nurses (Flarity, Gentry, Mesnikoff, 2013; Hinderer, et al, 2014; Hunsacker, Chen, Maughan & Heaston, 2014; Kelly, et al. , 2015; Sacco, Ciurzynski, Harvey & Ingersoll, 2015).
Coping Strategies in Literature • Education, meditation and debrief have all been discussed in the literature as ways to prevent the emotions of compassion fatigue • Resilience is the ability to cope successfully despite adversity; it is a dynamic and modifiable process (Earvolino-Ramirez, 2007; Flarity, Gentry, Mesnikoff, 2013; Hevezi, 2015; Polk, 1997; Potter, et al. , 2013)
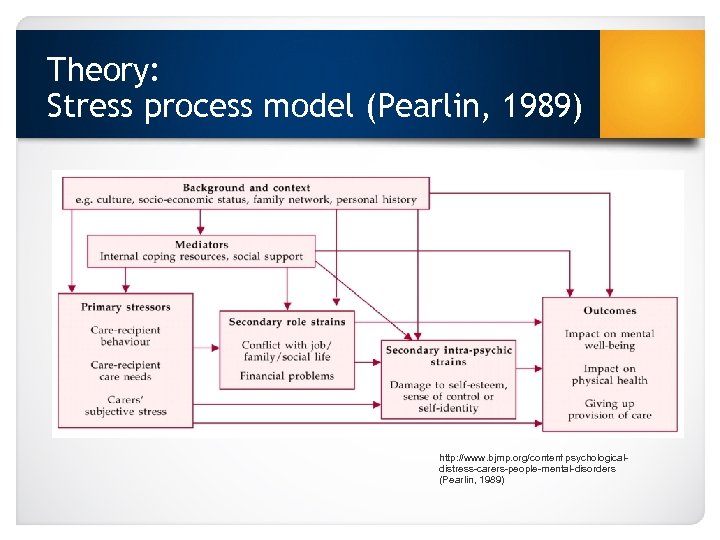
Theory: Stress process model (Pearlin, 1989) http: //www. bjmp. org/content/psychologicaldistress-carers-people-mental-disorders (Pearlin, 1989)
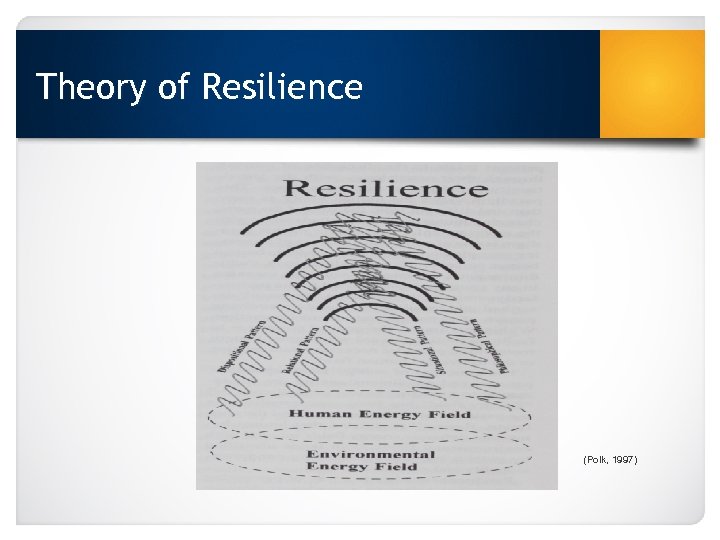
Theory of Resilience (Polk, 1997)
Personal Reflective Debrief • Structured debrief o Proactively o Personal Goals • Personal reflection o Learning about self o Coping mechanisms • Social support o Supporting and learning as a team (Earvolino-Ramirez, 2007; Flarity, Gentry, Mesnikoff, 2013; Hevezi, 2015; Polk, 1997; Potter, et al. , 2013)
International Association of Trauma Professionals (IATP) • Certified Compassion Fatigue Professional (CCFP)
DNP project proposal: Objectives and goals • • Evaluate levels of compassion fatigue Implement personal reflective debrief sessions Reassess levels of compassion fatigue Analyze and disseminate findings
Site Information • • • Level 2 trauma center 25 bed emergency department Midwestern hospital Urban environment High acuity/high volume 62 nurses (both Full and Part time)
Key Stakeholders • • Manager Director Charge nurses Staff nurses
Resources and Budget • • Creation of intervention- part of course work International Review Board- in kind Staff time-in kind Conference room space Access to unit manager Fliers- $25 Food-$200 Statistician- in kind
DNP Project: Methods • IRB approval (December 2016) • Create survey link (December 2016) • Set up dates for personal reflective debrief sessions (January 2017) • Advertise through emails and fliers (January 2017) • Send out initial Pro. QOL survey (January 2017)
Generate: Baseline Needs Assessment • Professional Quality of Life Scale (Pro. QOL) • Validated and Reliable • Balance between symptoms of: o compassion satisfaction o secondary traumatic stress o burnout • Gives overall compassion fatigue score. • (Stamm, 2016)
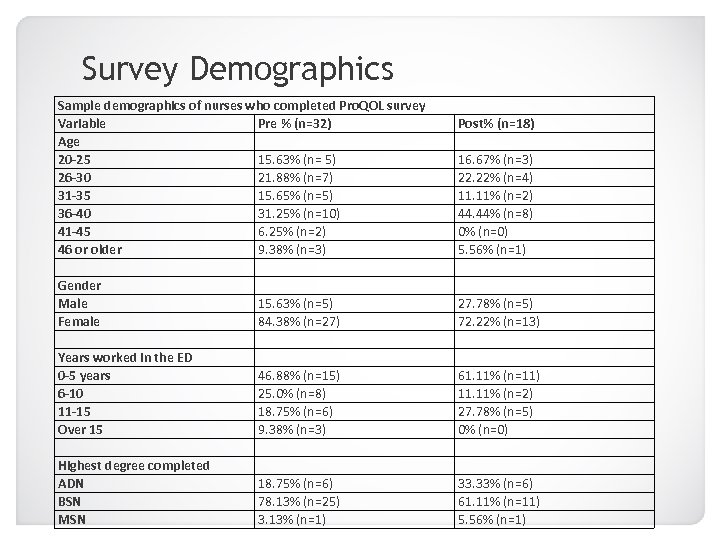
Survey Demographics Sample demographics of nurses who completed Pro. QOL survey Variable Pre % (n=32) Age 20 -25 15. 63% (n= 5) 26 -30 21. 88% (n=7) 31 -35 15. 65% (n=5) 36 -40 31. 25% (n=10) 41 -45 6. 25% (n=2) 46 or older 9. 38% (n=3) Gender Male 15. 63% (n=5) Female 84. 38% (n=27) Years worked in the ED 0 -5 years 46. 88% (n=15) 6 -10 25. 0% (n=8) 11 -15 18. 75% (n=6) Over 15 9. 38% (n=3) Highest degree completed ADN 18. 75% (n=6) BSN 78. 13% (n=25) MSN 3. 13% (n=1) Post% (n=18) 16. 67% (n=3) 22. 22% (n=4) 11. 11% (n=2) 44. 44% (n=8) 0% (n=0) 5. 56% (n=1) 27. 78% (n=5) 72. 22% (n=13) 61. 11% (n=11) 11. 11% (n=2) 27. 78% (n=5) 0% (n=0) 33. 33% (n=6) 61. 11% (n=11) 5. 56% (n=1)
Implement: Personal Reflective Debrief • Implement the personal reflective debrief sessions (February 2017) • Debrief o Individual story, group support • Reflection • Coping mechanisms • Thank you to nurses
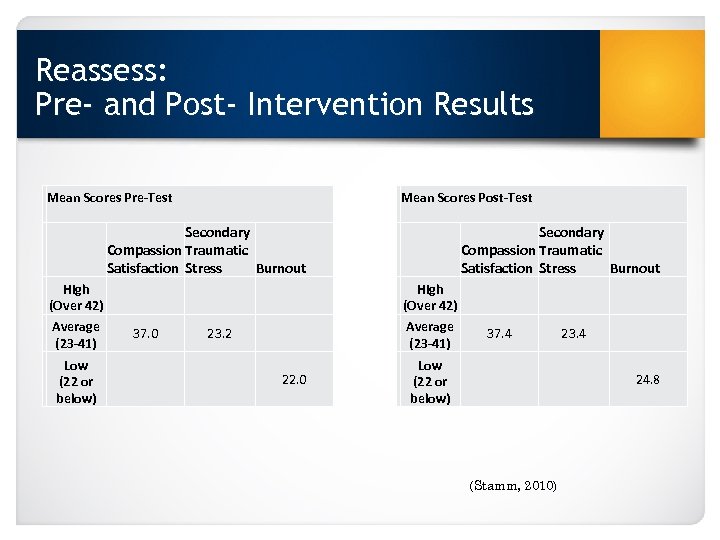
Reassess: Pre- and Post- Intervention Results Mean Scores Pre-Test Mean Scores Post-Test Secondary Compassion Traumatic Satisfaction Stress Burnout High (Over 42) Average (23 -41) Low (22 or below) 37. 0 Secondary Compassion Traumatic Satisfaction Stress Burnout High (Over 42) Average (23 -41) 23. 2 22. 0 37. 4 Low (22 or below) 23. 4 24. 8 (Stamm, 2010)
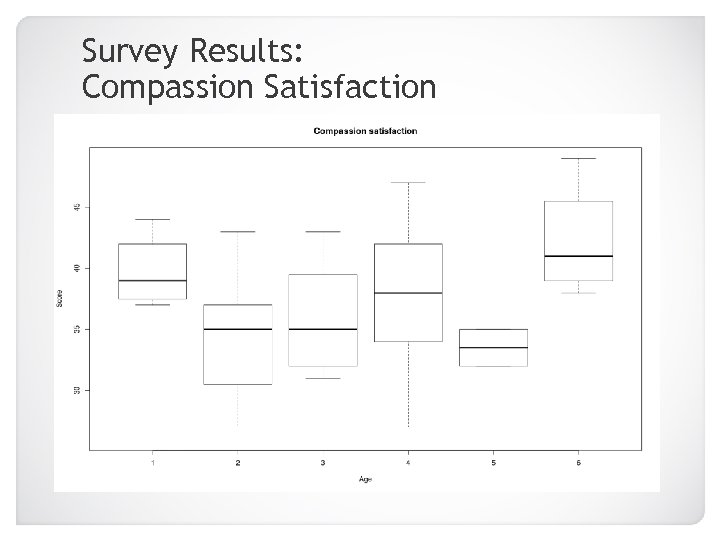
Survey Results: Compassion Satisfaction 20 -25 46+ 26 -30 31 -35 36 -40 41 -45
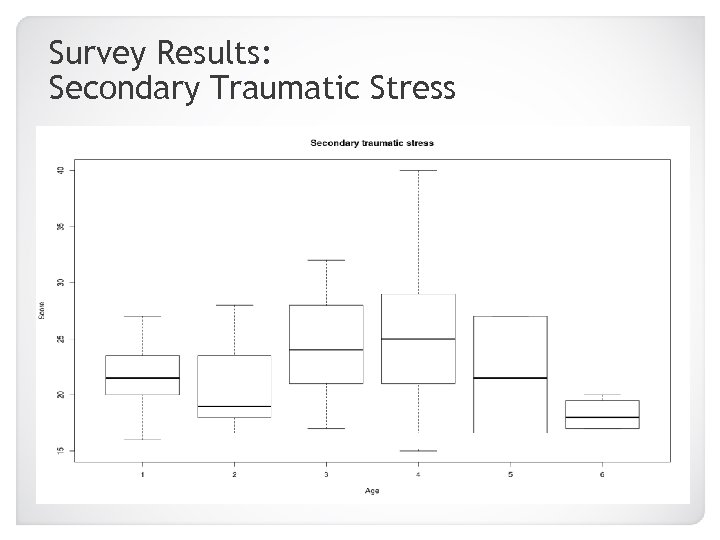
Survey Results: Secondary Traumatic Stress 20 -25 46+ 26 -30 31 -35 36 -40 41 -45
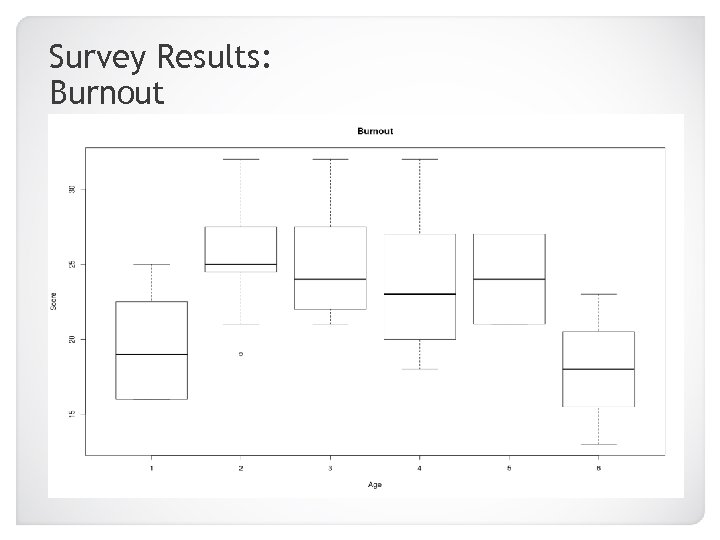
Survey Results: Burnout 20 -25 26 -30 31 -35 36 -40 41 -45 46+
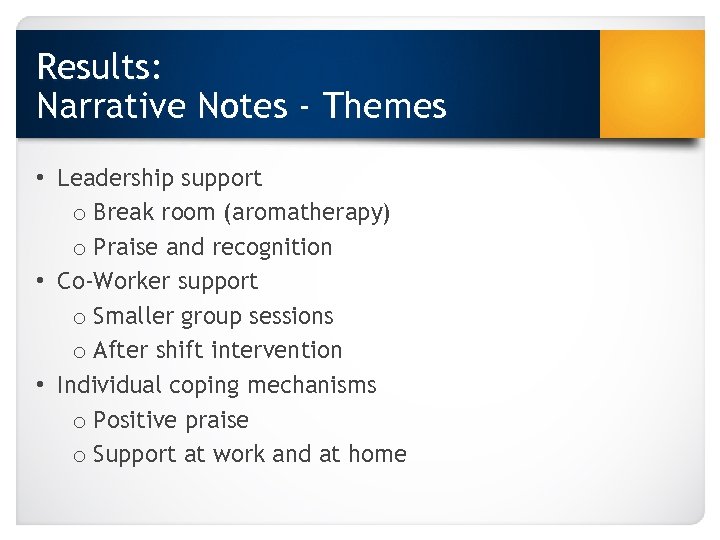
Results: Narrative Notes - Themes • Leadership support o Break room (aromatherapy) o Praise and recognition • Co-Worker support o Smaller group sessions o After shift intervention • Individual coping mechanisms o Positive praise o Support at work and at home
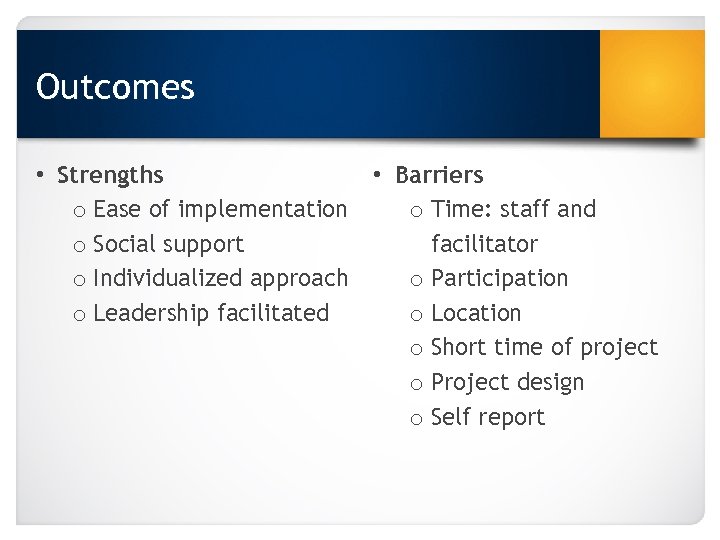
Outcomes • Strengths • Barriers o Ease of implementation o Time: staff and o Social support facilitator o Individualized approach o Participation o Leadership facilitated o Location o Short time of project o Project design o Self report
Implications • Evaluation o Impact • Findings are consistent with other studies that used the Pro. QOL with trauma nurses • APN leadership o Application • Next steps o Longer follow-up o More time between interventions o Different measurement tool o Other nursing subsets • Dissemination • Sustainability (Berg, 2016; Flarity et al, 2013; Hinderer et al. , 2014; Hevezi, 2015; Hunsacker, 2015; Potter et al. , 2013).
Questions
References • Berg, G. , Harshbarger, J. , Ahlers-Schmidt, C. , & Lippoldt, D. (2016). Exposing compassion fatigue and burnout syndrome in a trauma team: A qualitative study. Journal of Trauma Nursing, 23(1), 3 -10. doi: 10. 1097/JTN. 0000000172 • Duffy, E. , Avalos, G. , Dowling, M. (2014). Secondary traumatic stress among nurses: a cross sectional study. International Emergency Nursing, 23, 53 -58. doi: 10. 1016/j. ienj. 2014. 05. 001 • Earvolino-Ramirez, M. (2007). Resilience: A concept analysis. Nursing Forum, 42(2), 73 -82. • Flarity, K. , Gentry, J. , & Mesnikoff, N. (2013). The effectiveness of an educational program on prevention and treating compassion fatigue in emergency nurses. Advanced Emergency Nursing Journal, 35(3), 247 -258. doi: 10. 1097/TME. 0 b 013 e 31829 b 726 f • Hevezi, J. (2015). Evaluation of a meditation intervention to reduce the effects of stressors associated with compassion fatigue among nurses. Journal of Holistic Nursing, XX (X), 1 -8. doi: 10. 1177/0898010115615981
References cont. • Hinderer, K. , Von. Rueden, K. , Friedmann, E. , Mc. Quillan, K. , Gilmore, R. , Kramer, B. (2014). Burnout, compassion fatigue, compassion satisfaction, and secondary traumatic stress in trauma nurses. Journal of Trauma Nursing, 21(4), 160 -169. doi: 10. 1097/JTN. 000000055 • Hunsacker, S. , Chen, H. , Maughan, D. , & Heaston, S. (2014). Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. Journal of Nursing Scholarship, 47(2), 186 -194. doi: 10. 1111/jnu. 12122 • Pearlin, L. (1989). The sociological study of stress. Journal of Health and Social Behavior, 30(3), 241 -256. • Potter, P. , Deshields, T. , Allen, J. , Clarke, M. , Olsen, S. , Chen, L. (2013). Evaluation of a compassion fatigue resiliency program for oncology nurses. Oncology Nursing Standard, 40(2), 180 -187. • Stamm, B. H. (2010). The Concise Pro. QOL Manual, 2 nd Ed. Pocatello, ID: Pro. QOL. org.
f001ed75432e9effb93b2615c77ea277.ppt