Urogynaecology; An Introduction Ismaiel Abu Mahfouz MSc, MRCOG,

Urogynaecology; An Introduction Ismaiel Abu Mahfouz MSc, MRCOG, CCT
Richard Turner-Warwick
Urogynaecology “Neither the general urologist nor the general obstetrician and gynaecologist, but someone who has special training and expertise in genitourinary problems in women” “We should expand this definition to include urogynaecology and reconstructive pelvic surgery. Such a description implies a surgeon with specialized training in the conservative and surgical management of women with urinary or faecal incontinence, persistent genitourinary complaints, and disorders of pelvic floor supports” Turner-Warwick 1986
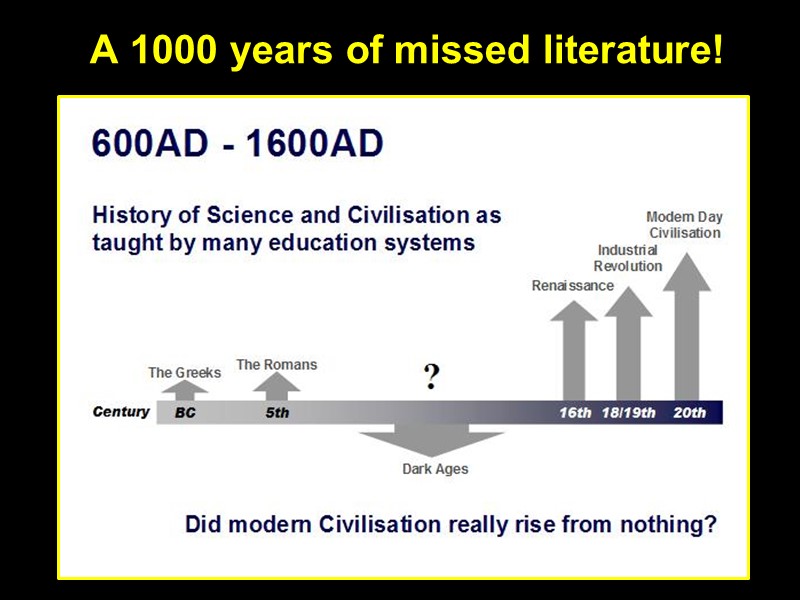
A 1000 years of missed literature!
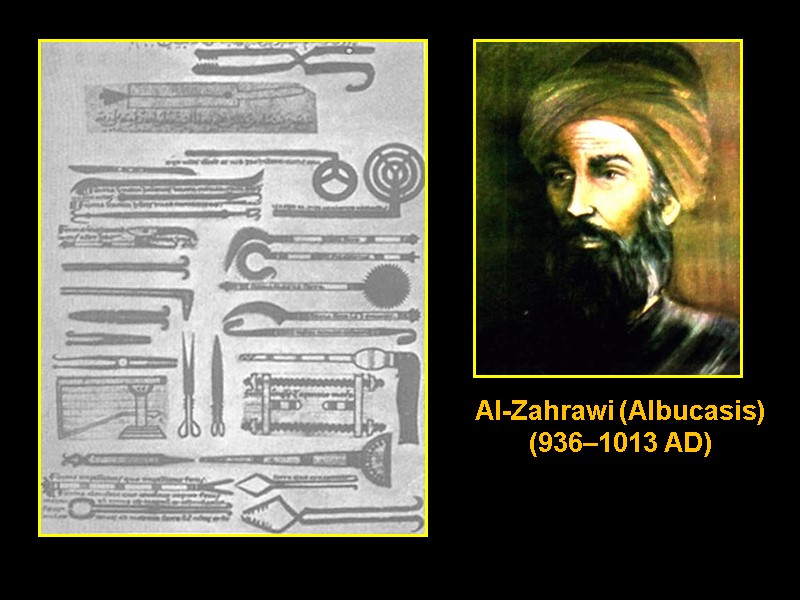
Al-Zahrawi (Albucasis) (936–1013 AD)
Cystolithotomy in women Instruments to visualise the interior of the urethra


Introduction Terminology Patients’ Assessment Urinary Incontinence (UI) Pelvic Organ Prolapse (POP)
Terminology
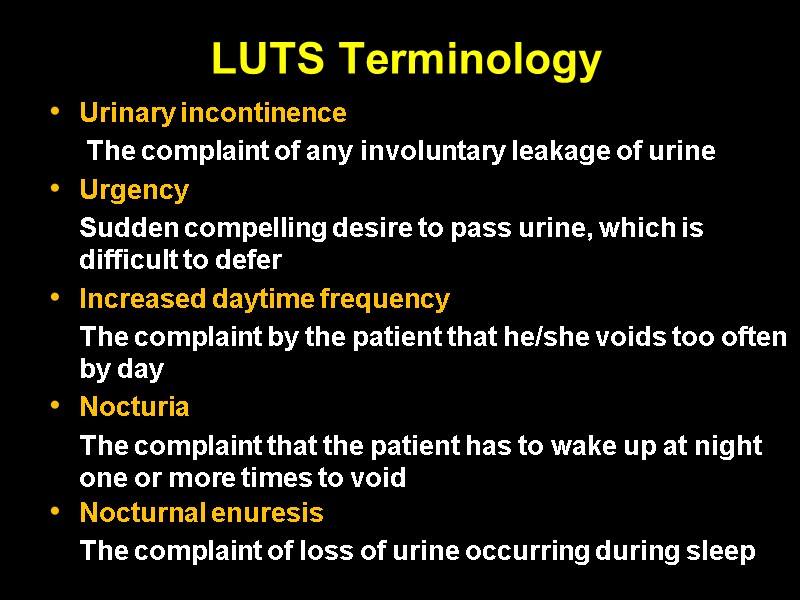
LUTS Terminology Urinary incontinence The complaint of any involuntary leakage of urine Urgency Sudden compelling desire to pass urine, which is difficult to defer Increased daytime frequency The complaint by the patient that he/she voids too often by day Nocturia The complaint that the patient has to wake up at night one or more times to void Nocturnal enuresis The complaint of loss of urine occurring during sleep
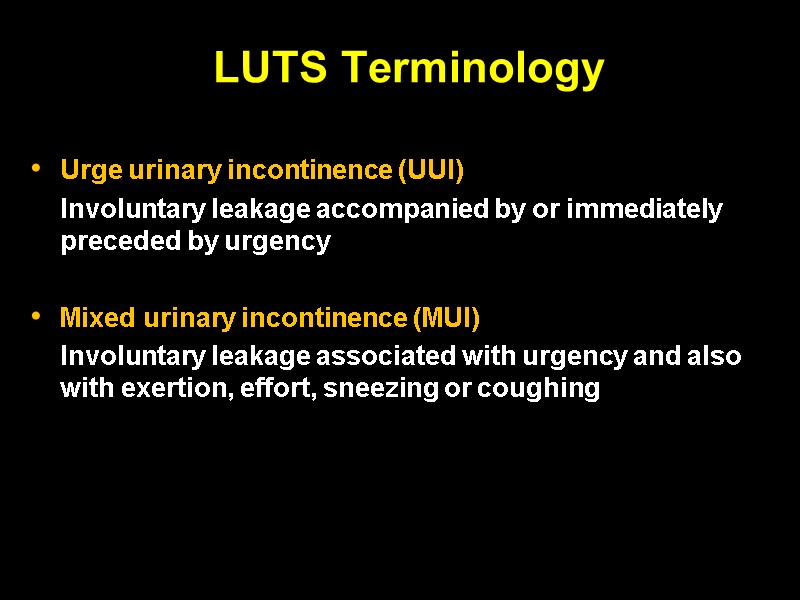
LUTS Terminology Urge urinary incontinence (UUI) Involuntary leakage accompanied by or immediately preceded by urgency Mixed urinary incontinence (MUI) Involuntary leakage associated with urgency and also with exertion, effort, sneezing or coughing
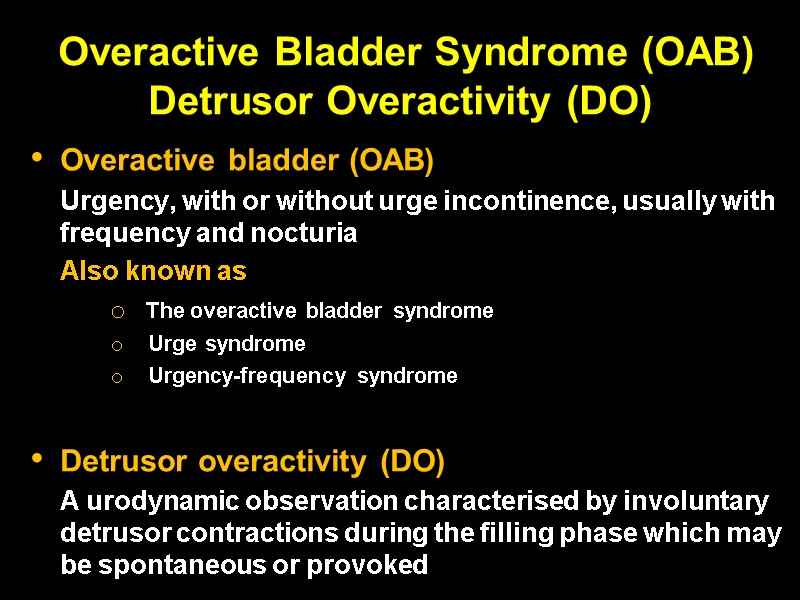
Overactive Bladder Syndrome (OAB) Detrusor Overactivity (DO) Overactive bladder (OAB) Urgency, with or without urge incontinence, usually with frequency and nocturia Also known as The overactive bladder syndrome Urge syndrome Urgency-frequency syndrome Detrusor overactivity (DO) A urodynamic observation characterised by involuntary detrusor contractions during the filling phase which may be spontaneous or provoked
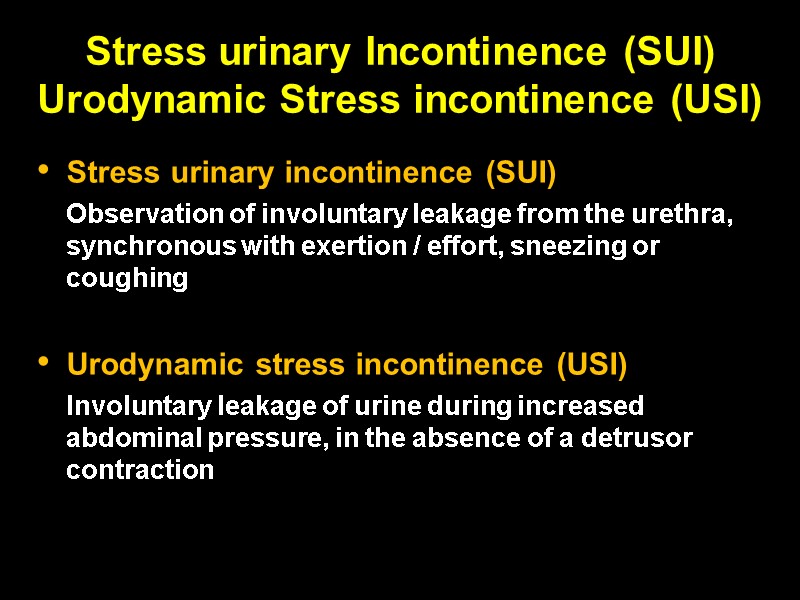
Stress urinary Incontinence (SUI) Urodynamic Stress incontinence (USI) Stress urinary incontinence (SUI) Observation of involuntary leakage from the urethra, synchronous with exertion / effort, sneezing or coughing Urodynamic stress incontinence (USI) Involuntary leakage of urine during increased abdominal pressure, in the absence of a detrusor contraction
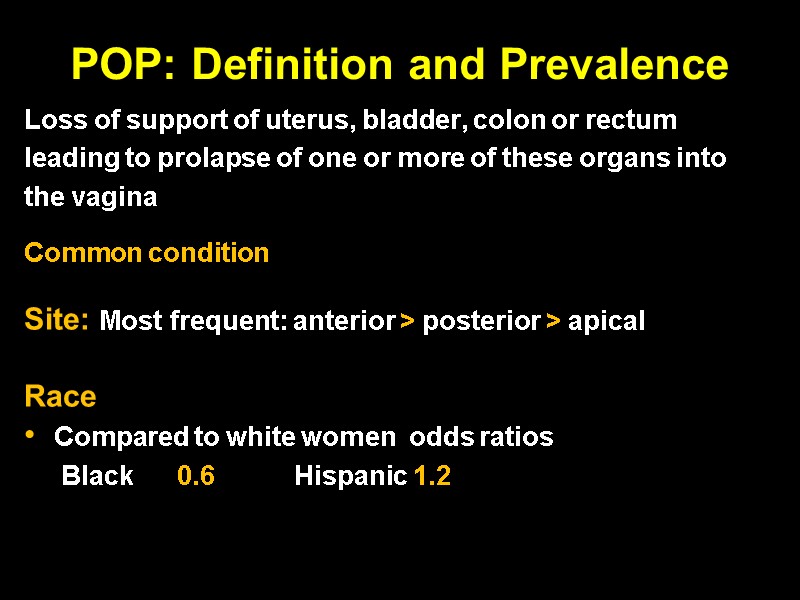
POP: Definition and Prevalence Loss of support of uterus, bladder, colon or rectum leading to prolapse of one or more of these organs into the vagina Common condition Site: Most frequent: anterior > posterior > apical Race Compared to white women odds ratios Black 0.6 Hispanic 1.2
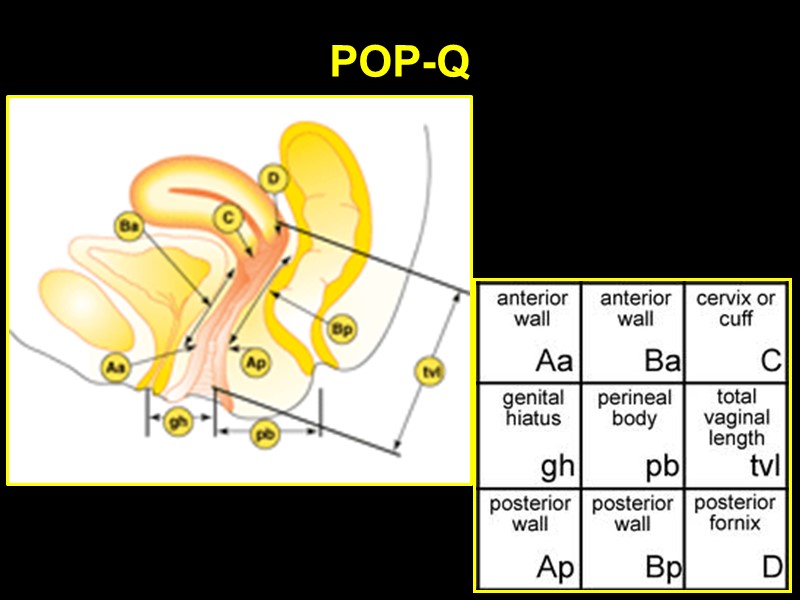
POP-Q
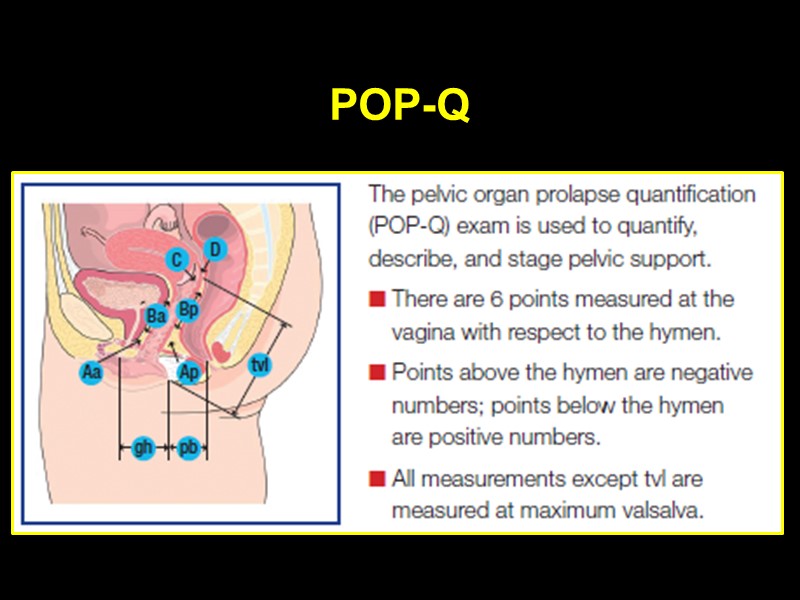
POP-Q
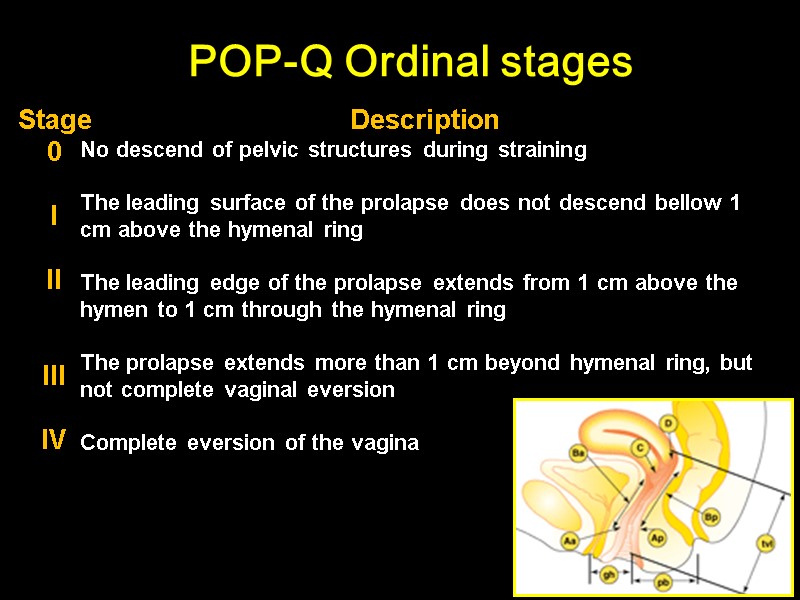
POP-Q Ordinal stages Stage 0 I II III IV Description No descend of pelvic structures during straining The leading surface of the prolapse does not descend bellow 1 cm above the hymenal ring The leading edge of the prolapse extends from 1 cm above the hymen to 1 cm through the hymenal ring The prolapse extends more than 1 cm beyond hymenal ring, but not complete vaginal eversion Complete eversion of the vagina
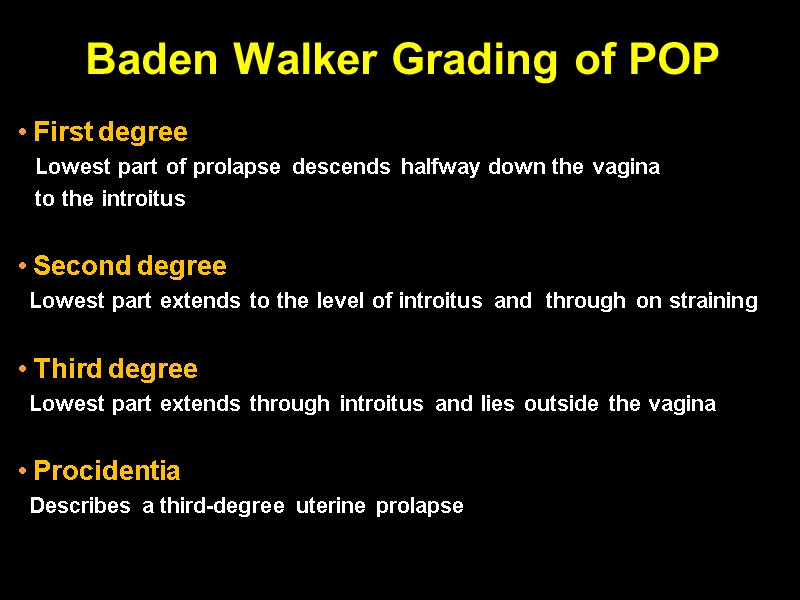
Baden Walker Grading of POP First degree Lowest part of prolapse descends halfway down the vagina to the introitus Second degree Lowest part extends to the level of introitus and through on straining Third degree Lowest part extends through introitus and lies outside the vagina Procidentia Describes a third-degree uterine prolapse
Assessment
Clinical evaluation
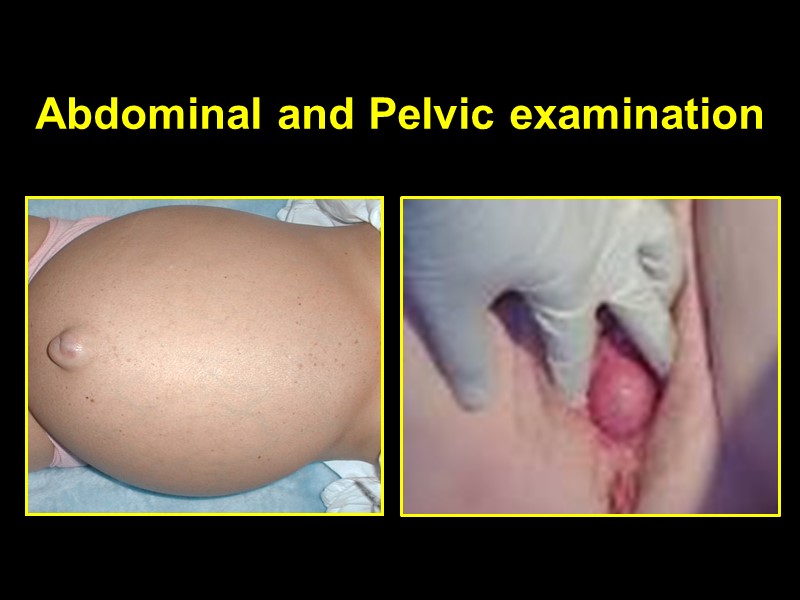
Abdominal and Pelvic examination
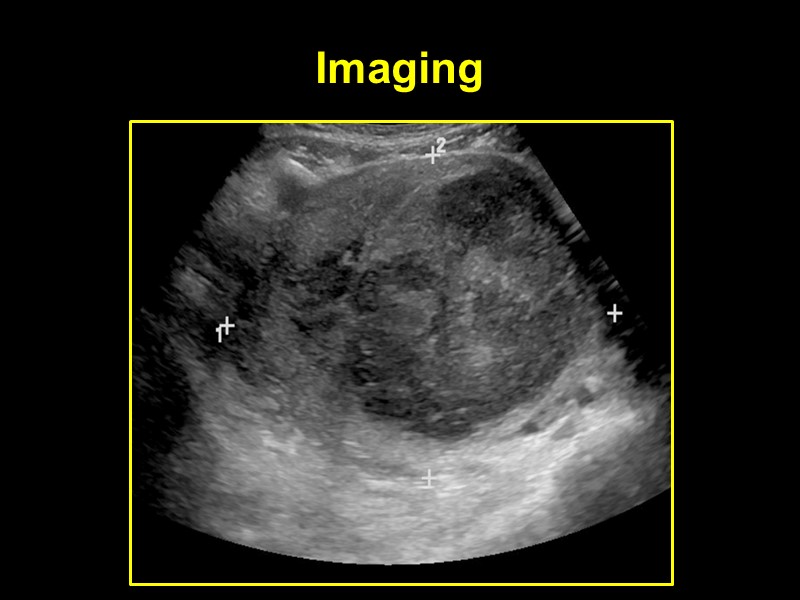
Imaging
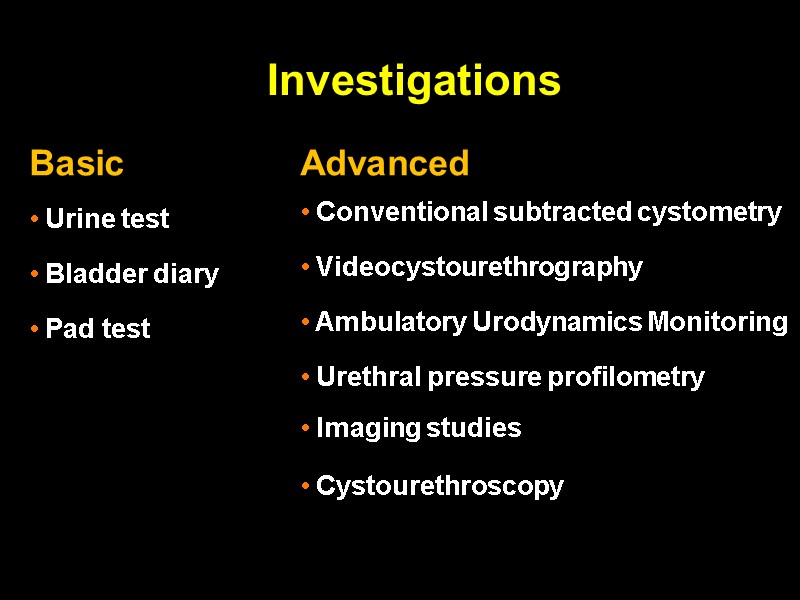
Investigations
Basic investigations
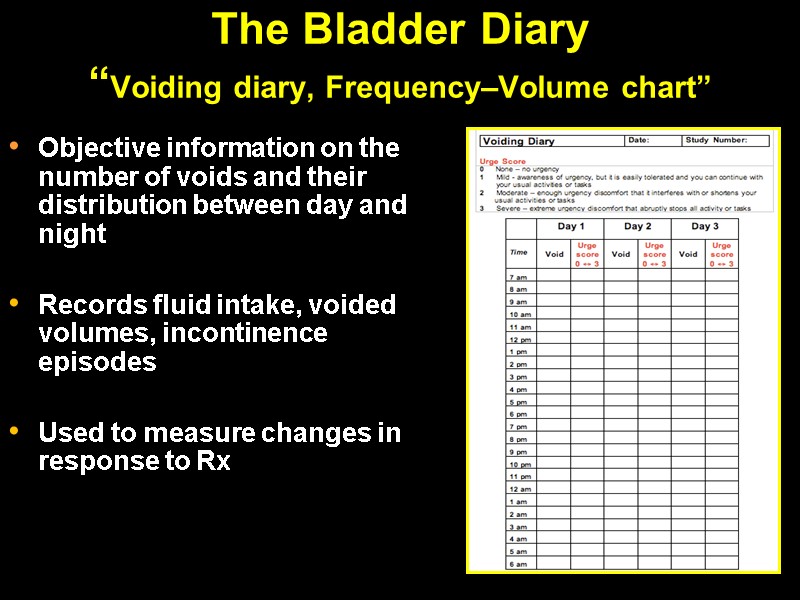
The Bladder Diary “Voiding diary, Frequency–Volume chart” Objective information on the number of voids and their distribution between day and night Records fluid intake, voided volumes, incontinence episodes Used to measure changes in response to Rx
The Pad Test Objective Non-invasive 1hr, 4hr, 12hr, 24hr and 48hr The ICS 1 Hour Standardised Test Pre-weigh pad Drink 500mls Rest 15 mins Moderate exercise 30 mins 15 mins provocative exercises Positive test >2g increase Severe incontinence >10g increase
Advanced investigations
Urodynamics Studies (UDS) Definition Studies of lower urinary tract function and dysfunction Why urodynamics? The UDS Free flow study Filling Cystometry Voiding cystometry
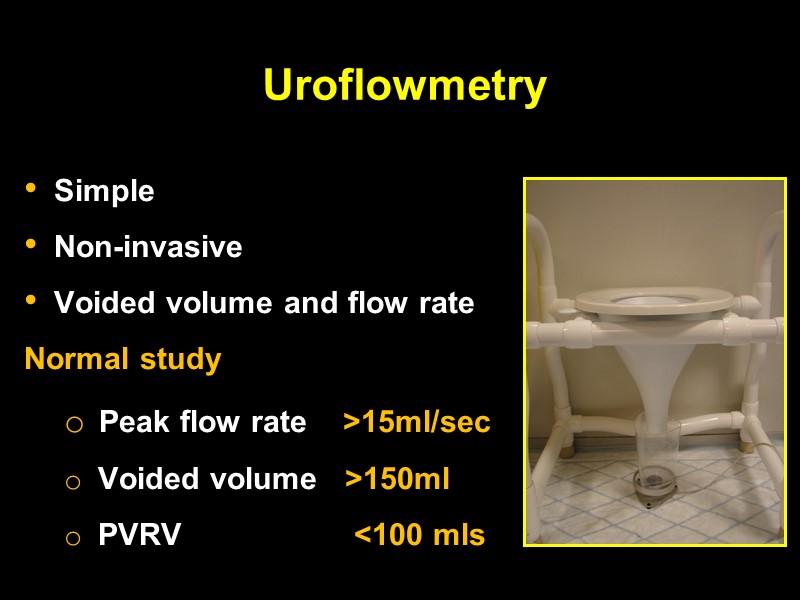
Uroflowmetry Simple Non-invasive Voided volume and flow rate Normal study Peak flow rate >15ml/sec Voided volume >150ml PVRV <100 mls
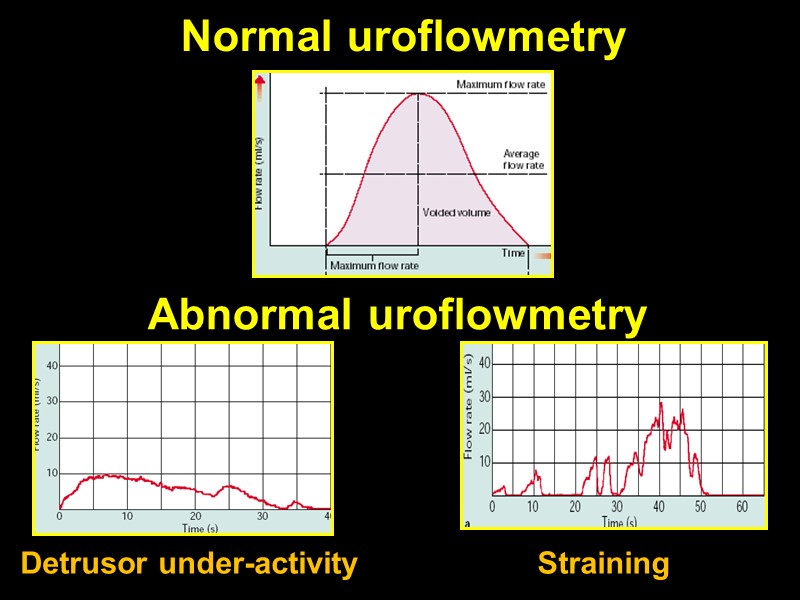
Normal uroflowmetry Abnormal uroflowmetry Straining Detrusor under-activity
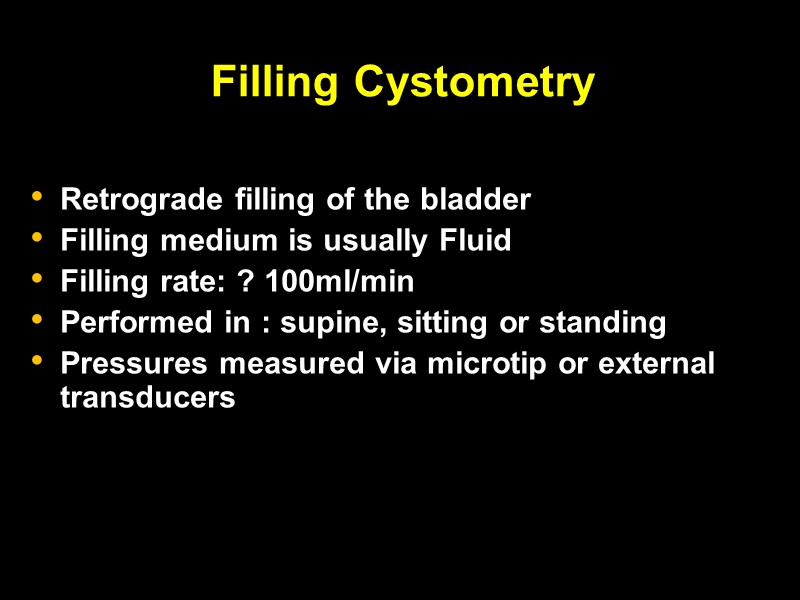
Filling Cystometry Retrograde filling of the bladder Filling medium is usually Fluid Filling rate: ? 100ml/min Performed in : supine, sitting or standing Pressures measured via microtip or external transducers
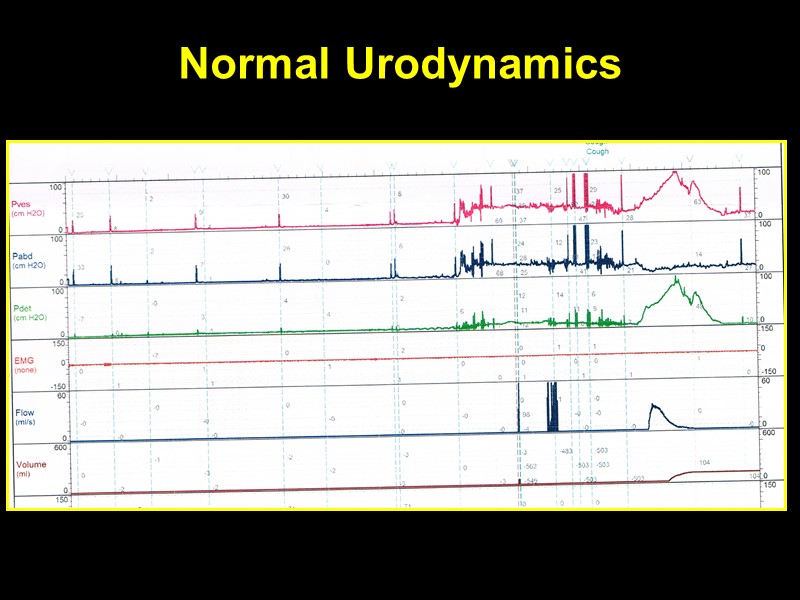
Normal Urodynamics
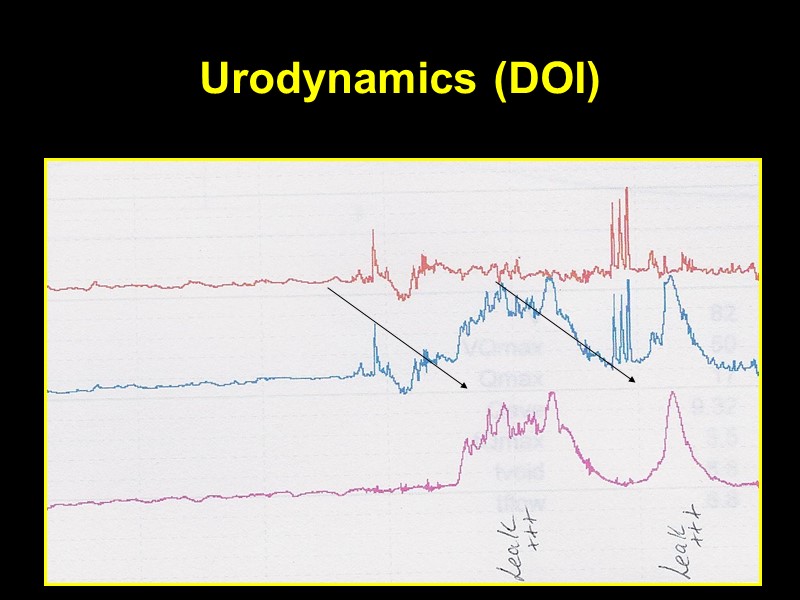
Urodynamics (DOI)
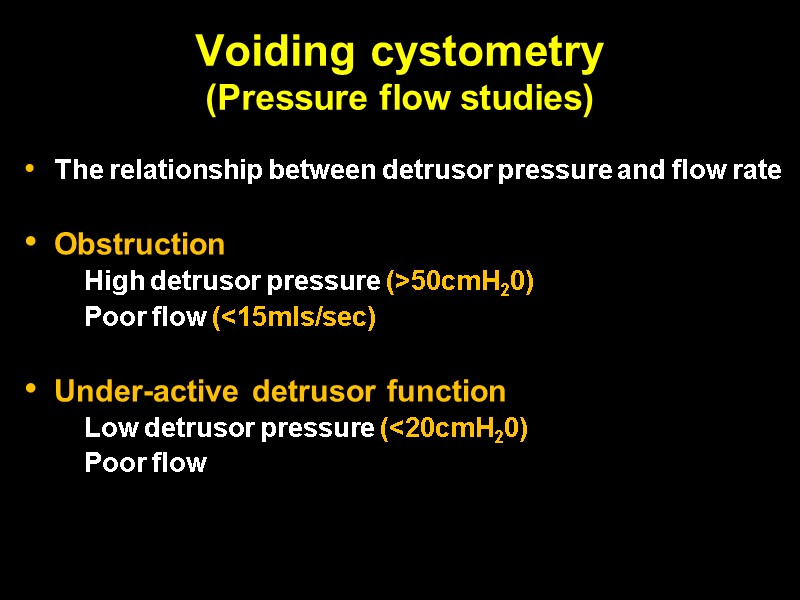
Voiding cystometry (Pressure flow studies) The relationship between detrusor pressure and flow rate Obstruction High detrusor pressure (>50cmH20) Poor flow (<15mls/sec) Under-active detrusor function Low detrusor pressure (<20cmH20) Poor flow
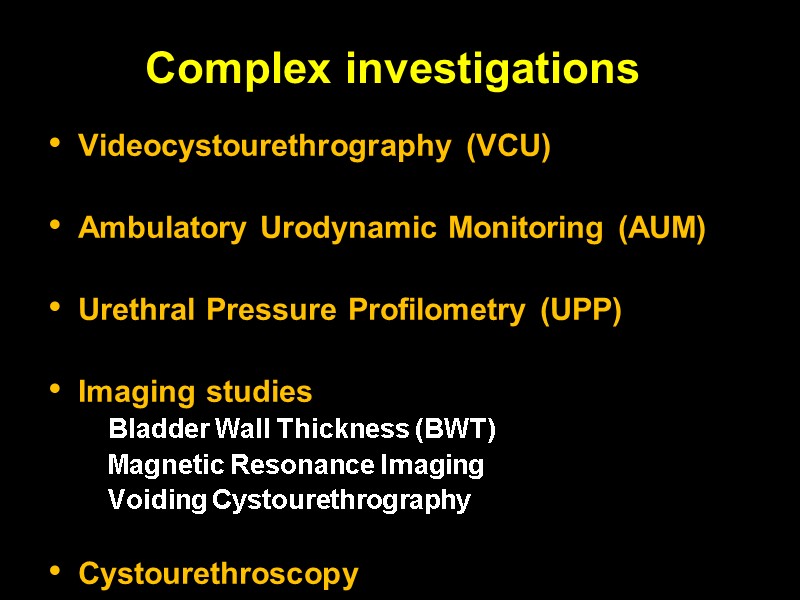
Complex investigations Videocystourethrography (VCU) Ambulatory Urodynamic Monitoring (AUM) Urethral Pressure Profilometry (UPP) Imaging studies Bladder Wall Thickness (BWT) Magnetic Resonance Imaging Voiding Cystourethrography Cystourethroscopy
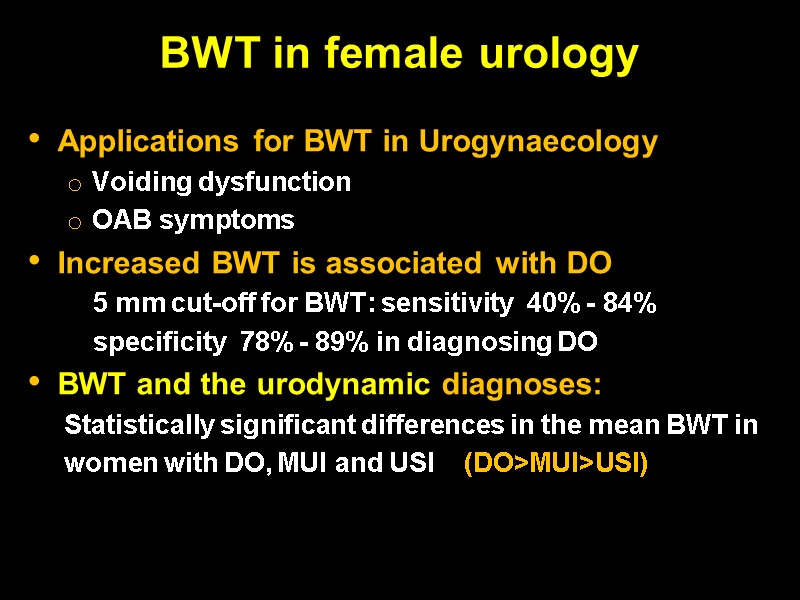
BWT in female urology Applications for BWT in Urogynaecology Voiding dysfunction OAB symptoms Increased BWT is associated with DO 5 mm cut-off for BWT: sensitivity 40% - 84% specificity 78% - 89% in diagnosing DO BWT and the urodynamic diagnoses: Statistically significant differences in the mean BWT in women with DO, MUI and USI (DO>MUI>USI)
Urinary Incontinence
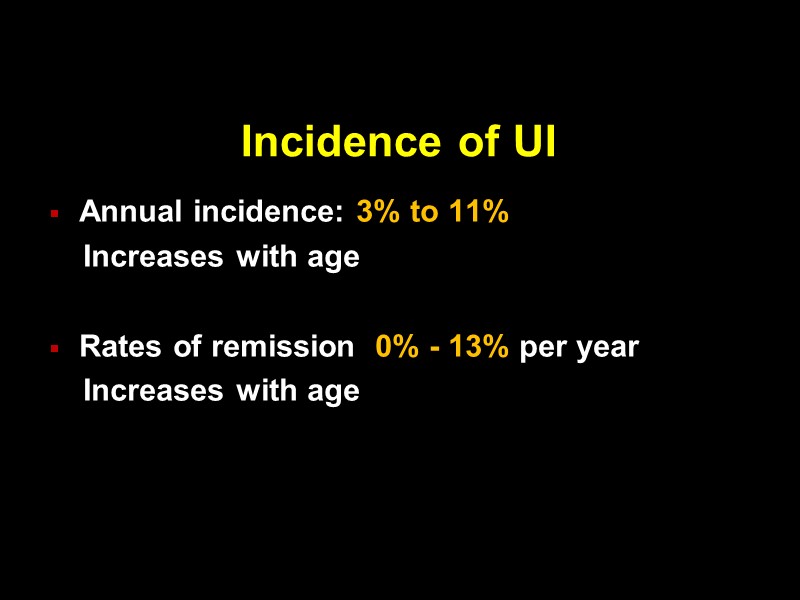
Incidence of UI Annual incidence: 3% to 11% Increases with age Rates of remission 0% - 13% per year Increases with age
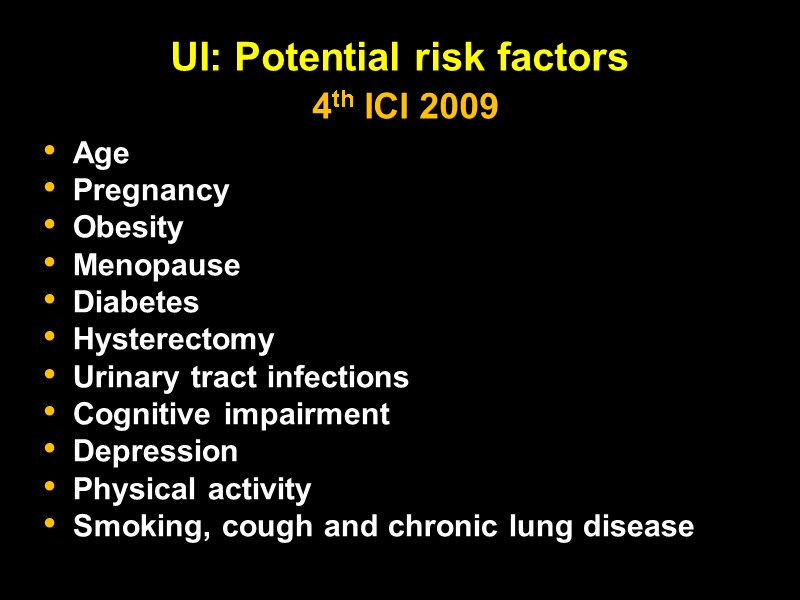
UI: Potential risk factors 4th ICI 2009 Age Pregnancy Obesity Menopause Diabetes Hysterectomy Urinary tract infections Cognitive impairment Depression Physical activity Smoking, cough and chronic lung disease
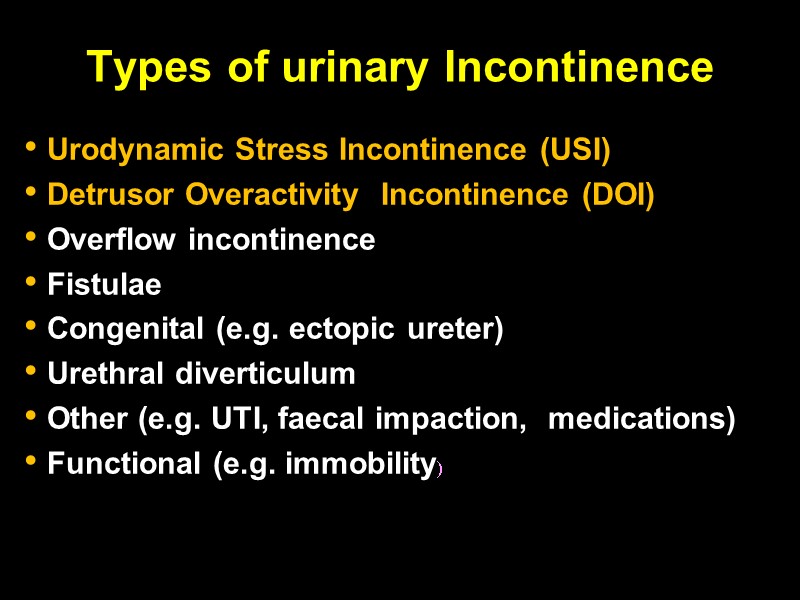
Types of urinary Incontinence Urodynamic Stress Incontinence (USI) Detrusor Overactivity Incontinence (DOI) Overflow incontinence Fistulae Congenital (e.g. ectopic ureter) Urethral diverticulum Other (e.g. UTI, faecal impaction, medications) Functional (e.g. immobility)
Rx: All about balance
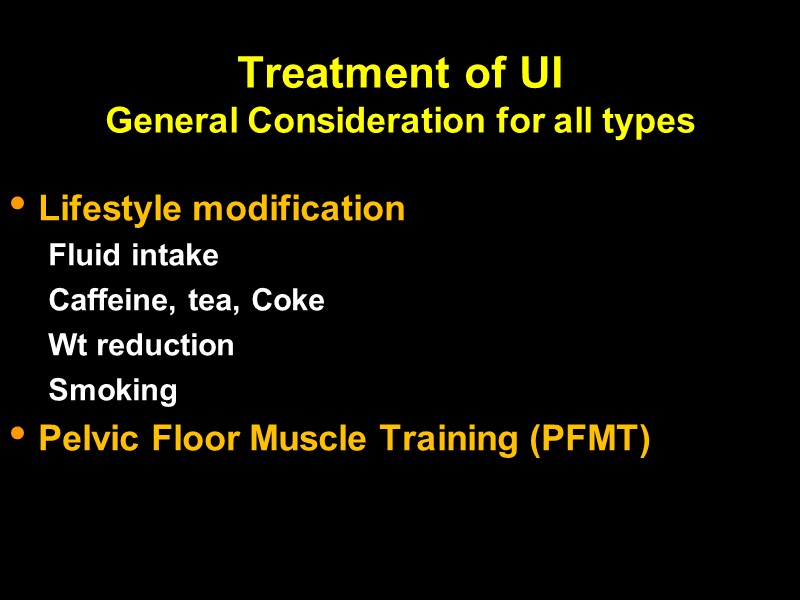
Treatment of UI General Consideration for all types Lifestyle modification Fluid intake Caffeine, tea, Coke Wt reduction Smoking Pelvic Floor Muscle Training (PFMT)
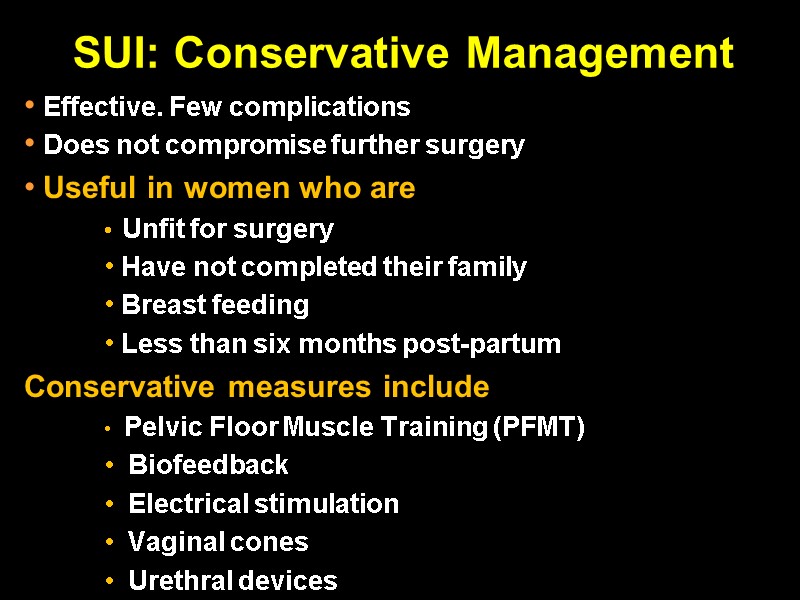
SUI: Conservative Management Effective. Few complications Does not compromise further surgery Useful in women who are Unfit for surgery Have not completed their family Breast feeding Less than six months post-partum Conservative measures include Pelvic Floor Muscle Training (PFMT) Biofeedback Electrical stimulation Vaginal cones Urethral devices
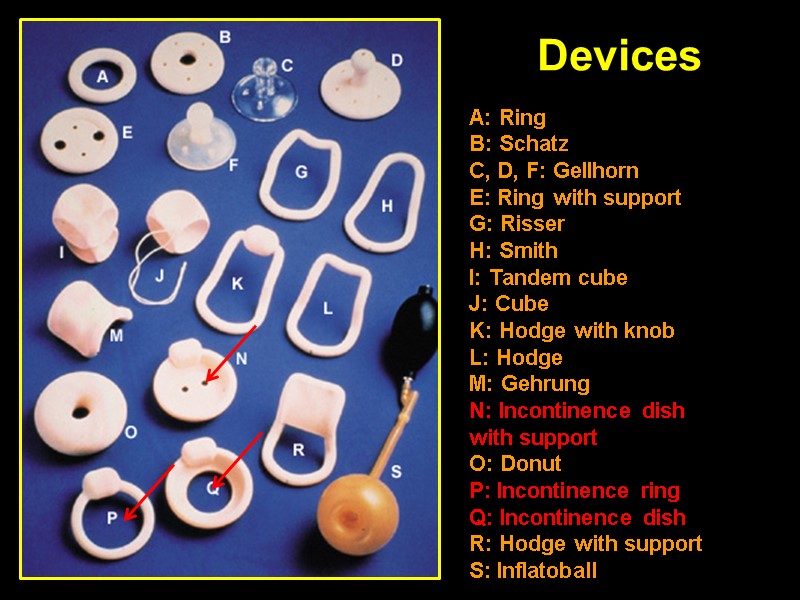
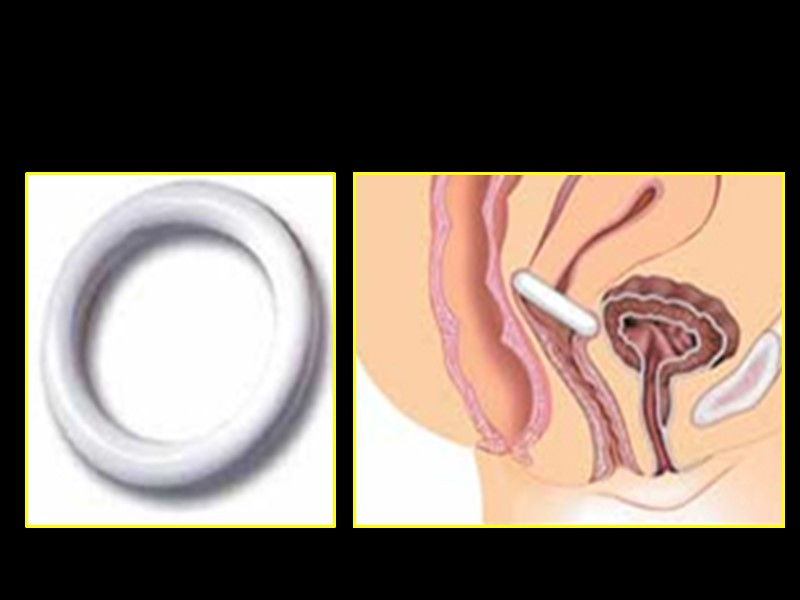
Devices A: Ring B: Schatz C, D, F: Gellhorn E: Ring with support G: Risser H: Smith I: Tandem cube J: Cube K: Hodge with knob L: Hodge M: Gehrung N: Incontinence dish with support O: Donut P: Incontinence ring Q: Incontinence dish R: Hodge with support S: Inflatoball
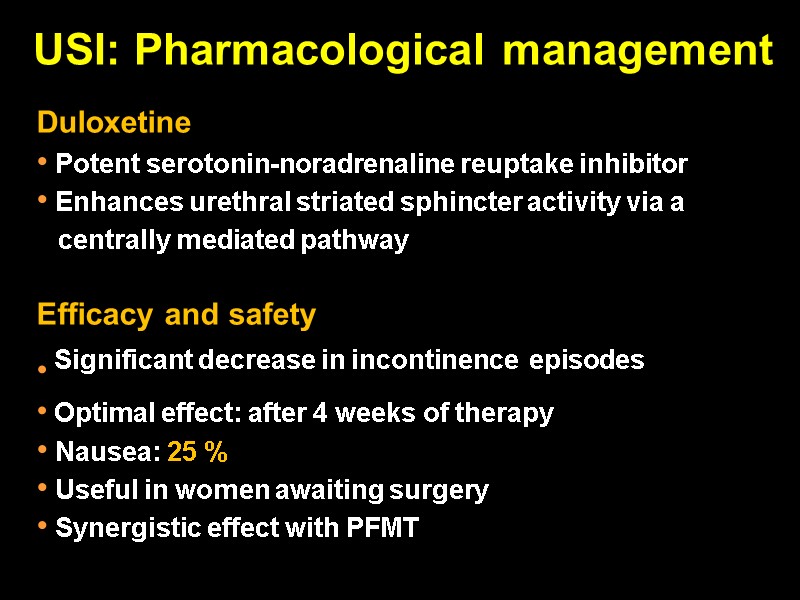
USI: Pharmacological management Duloxetine Potent serotonin-noradrenaline reuptake inhibitor Enhances urethral striated sphincter activity via a centrally mediated pathway Efficacy and safety Significant decrease in incontinence episodes Optimal effect: after 4 weeks of therapy Nausea: 25 % Useful in women awaiting surgery Synergistic effect with PFMT
USI: Surgical management Colposuspension Sub-urethral tapes (TVT/TOT) Urethral bulking agents
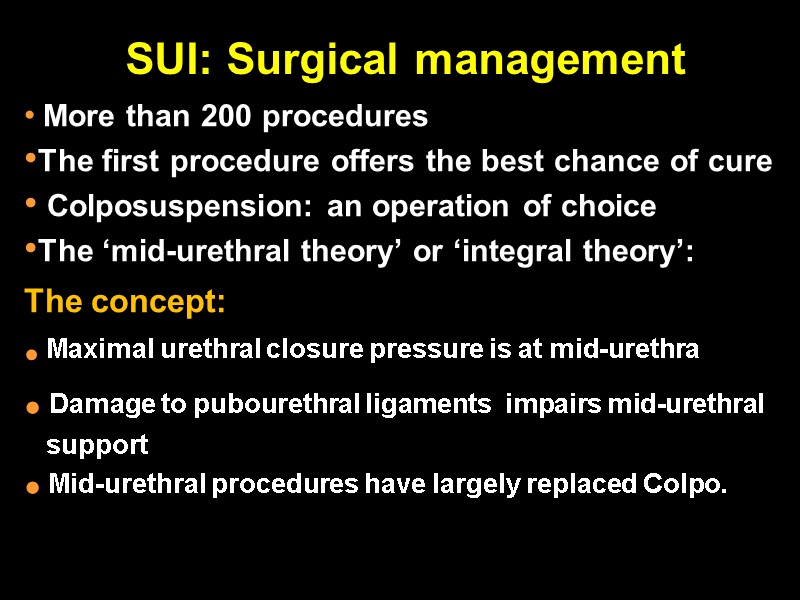
SUI: Surgical management More than 200 procedures The first procedure offers the best chance of cure Colposuspension: an operation of choice The ‘mid-urethral theory’ or ‘integral theory’: The concept: Maximal urethral closure pressure is at mid-urethra Damage to pubourethral ligaments impairs mid-urethral support Mid-urethral procedures have largely replaced Colpo.
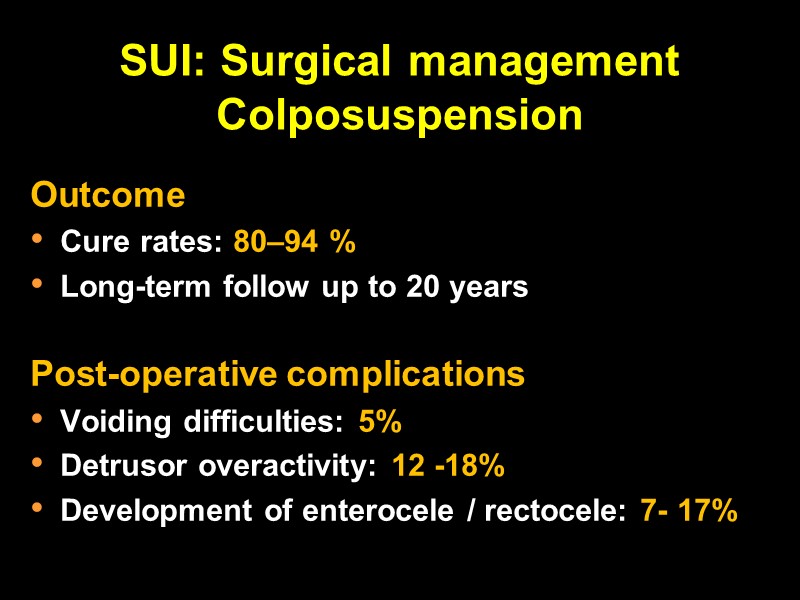
SUI: Surgical management Colposuspension Outcome Cure rates: 80–94 % Long-term follow up to 20 years Post-operative complications Voiding difficulties: 5% Detrusor overactivity: 12 -18% Development of enterocele / rectocele: 7- 17%
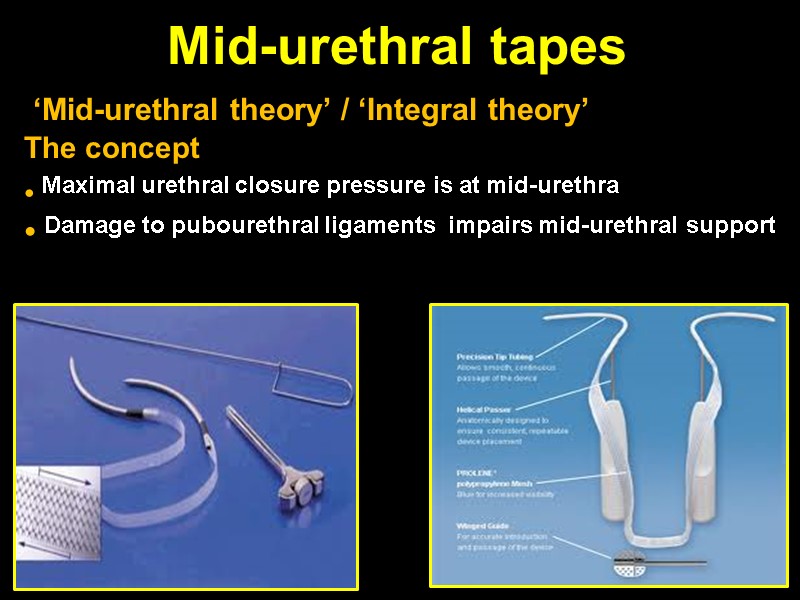
Mid-urethral tapes ‘Mid-urethral theory’ / ‘Integral theory’ The concept Maximal urethral closure pressure is at mid-urethra Damage to pubourethral ligaments impairs mid-urethral support
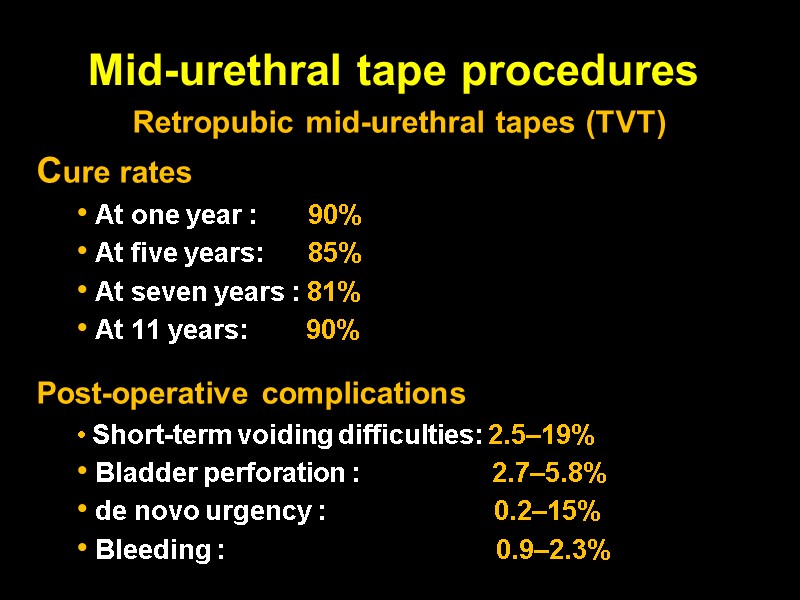
Mid-urethral tape procedures Retropubic mid-urethral tapes (TVT) Cure rates At one year : 90% At five years: 85% At seven years : 81% At 11 years: 90% Post-operative complications Short-term voiding difficulties: 2.5–19% Bladder perforation : 2.7–5.8% de novo urgency : 0.2–15% Bleeding : 0.9–2.3%
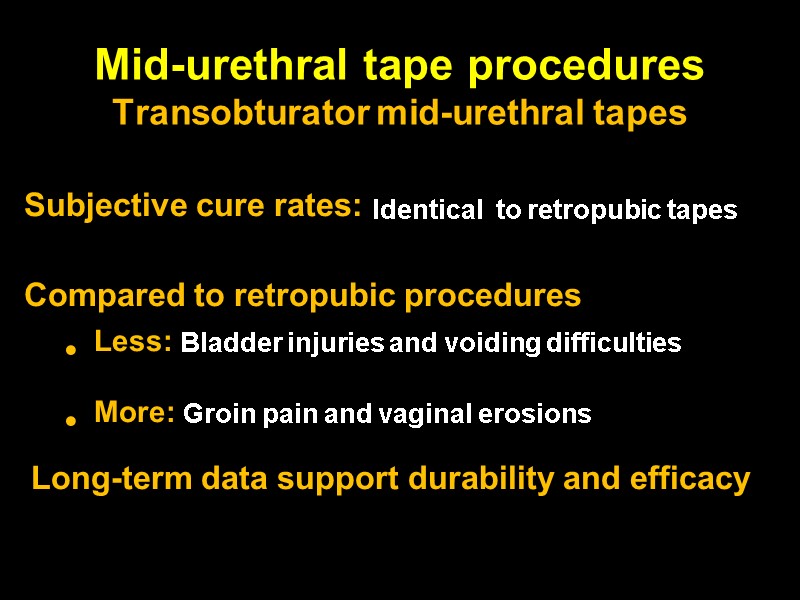
Mid-urethral tape procedures Transobturator mid-urethral tapes Subjective cure rates: Identical to retropubic tapes Compared to retropubic procedures Less: Bladder injuries and voiding difficulties More: Groin pain and vaginal erosions Long-term data support durability and efficacy

Urethral Bulking agents
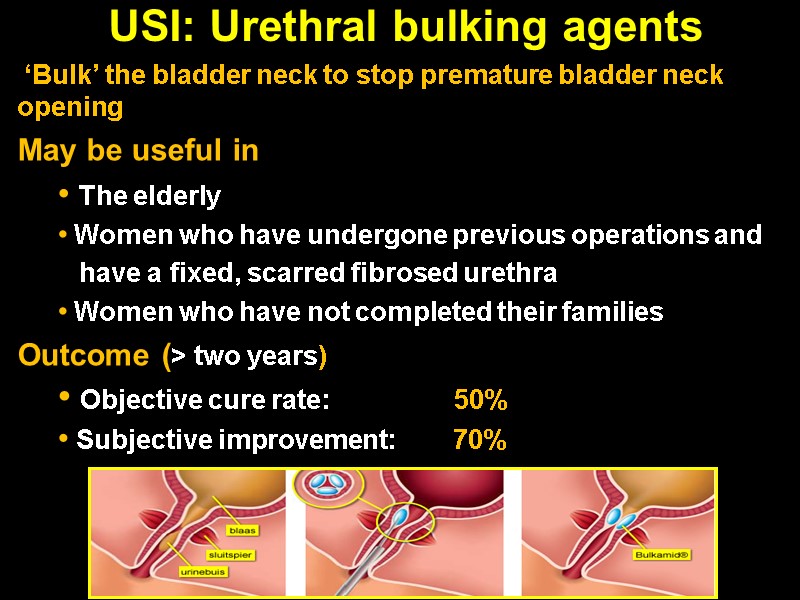
USI: Urethral bulking agents ‘Bulk’ the bladder neck to stop premature bladder neck opening May be useful in The elderly Women who have undergone previous operations and have a fixed, scarred fibrosed urethra Women who have not completed their families Outcome (> two years) Objective cure rate: 50% Subjective improvement: 70%
Overactive Bladder (OAB) Detrusor overactivity (DO)
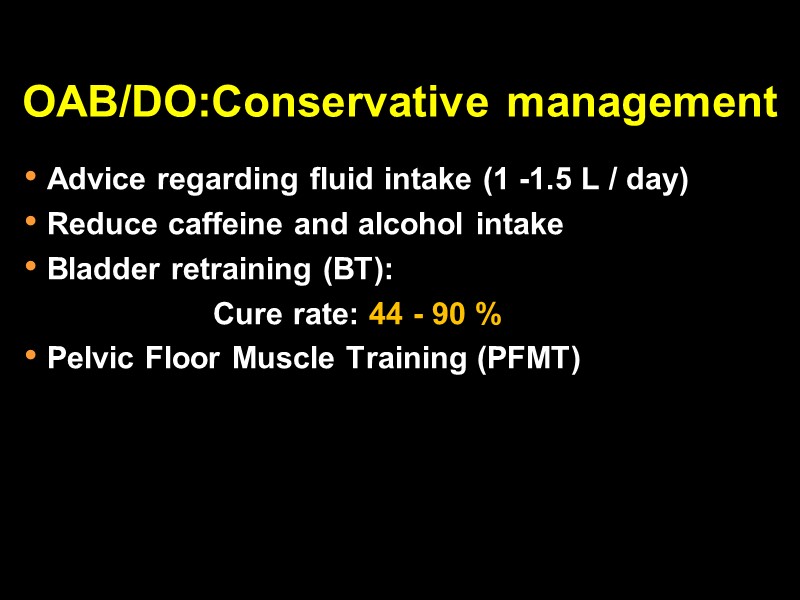
OAB/DO:Conservative management Advice regarding fluid intake (1 -1.5 L / day) Reduce caffeine and alcohol intake Bladder retraining (BT): Cure rate: 44 - 90 % Pelvic Floor Muscle Training (PFMT)
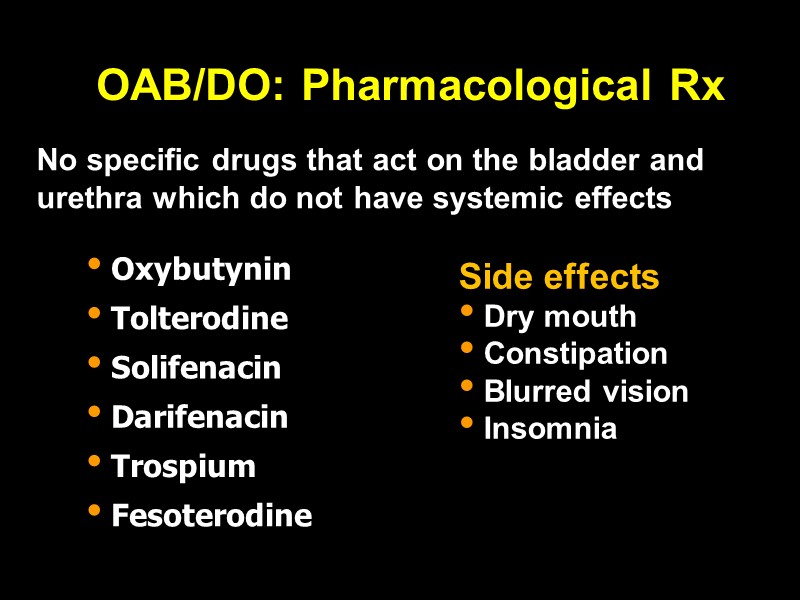
OAB/DO: Pharmacological Rx No specific drugs that act on the bladder and urethra which do not have systemic effects Side effects Dry mouth Constipation Blurred vision Insomnia
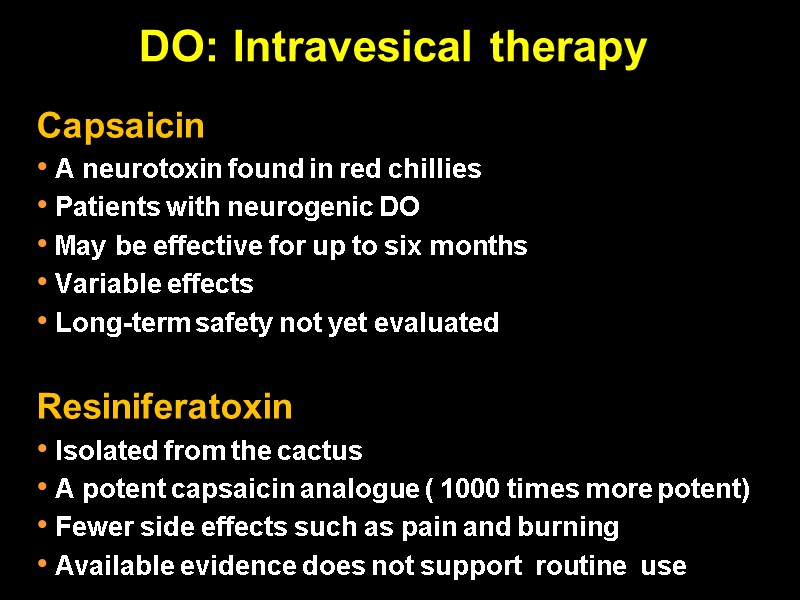
DO: Intravesical therapy Capsaicin A neurotoxin found in red chillies Patients with neurogenic DO May be effective for up to six months Variable effects Long-term safety not yet evaluated Resiniferatoxin Isolated from the cactus A potent capsaicin analogue ( 1000 times more potent) Fewer side effects such as pain and burning Available evidence does not support routine use

DO: Intravesical therapy Botulinum Toxin
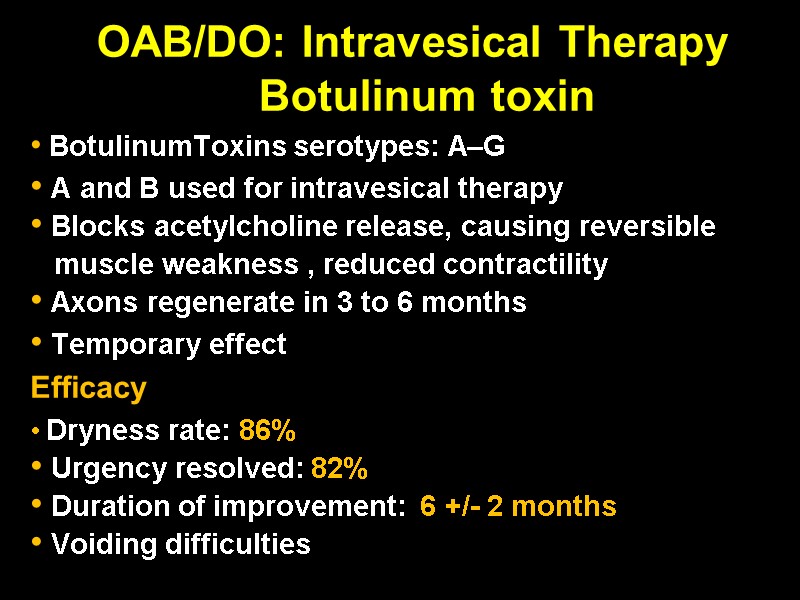
OAB/DO: Intravesical Therapy Botulinum toxin BotulinumToxins serotypes: A–G A and B used for intravesical therapy Blocks acetylcholine release, causing reversible muscle weakness , reduced contractility Axons regenerate in 3 to 6 months Temporary effect Efficacy Dryness rate: 86% Urgency resolved: 82% Duration of improvement: 6 +/- 2 months Voiding difficulties
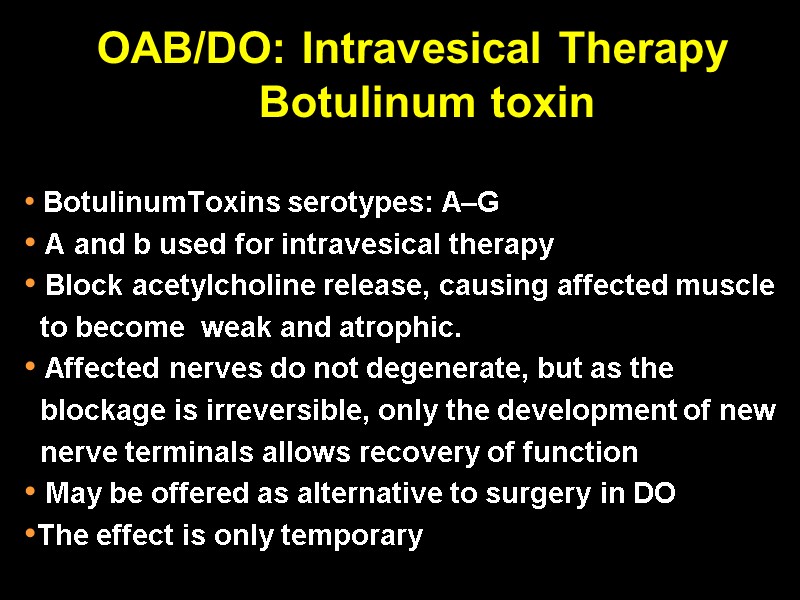
OAB/DO: Intravesical Therapy Botulinum toxin BotulinumToxins serotypes: A–G A and b used for intravesical therapy Block acetylcholine release, causing affected muscle to become weak and atrophic. Affected nerves do not degenerate, but as the blockage is irreversible, only the development of new nerve terminals allows recovery of function May be offered as alternative to surgery in DO The effect is only temporary
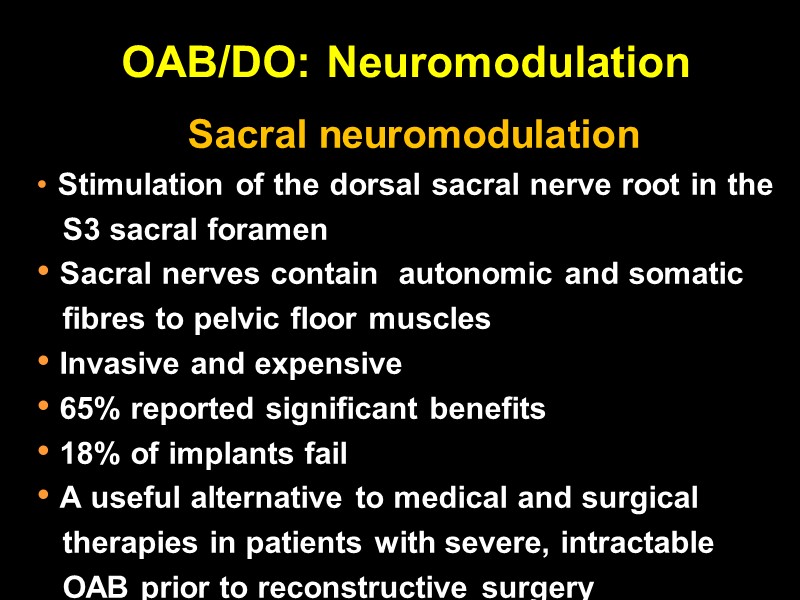
OAB/DO: Neuromodulation Sacral neuromodulation Stimulation of the dorsal sacral nerve root in the S3 sacral foramen Sacral nerves contain autonomic and somatic fibres to pelvic floor muscles Invasive and expensive 65% reported significant benefits 18% of implants fail A useful alternative to medical and surgical therapies in patients with severe, intractable OAB prior to reconstructive surgery
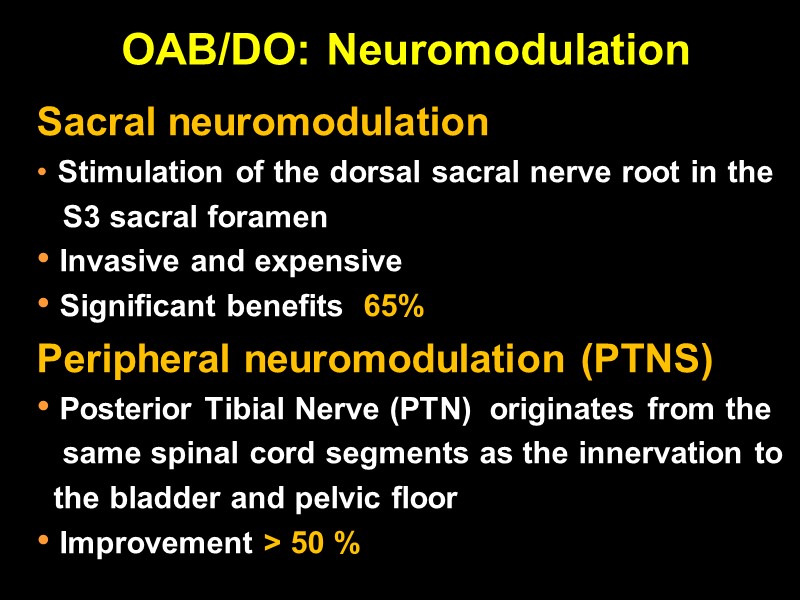
OAB/DO: Neuromodulation Sacral neuromodulation Stimulation of the dorsal sacral nerve root in the S3 sacral foramen Invasive and expensive Significant benefits 65% Peripheral neuromodulation (PTNS) Posterior Tibial Nerve (PTN) originates from the same spinal cord segments as the innervation to the bladder and pelvic floor Improvement > 50 %
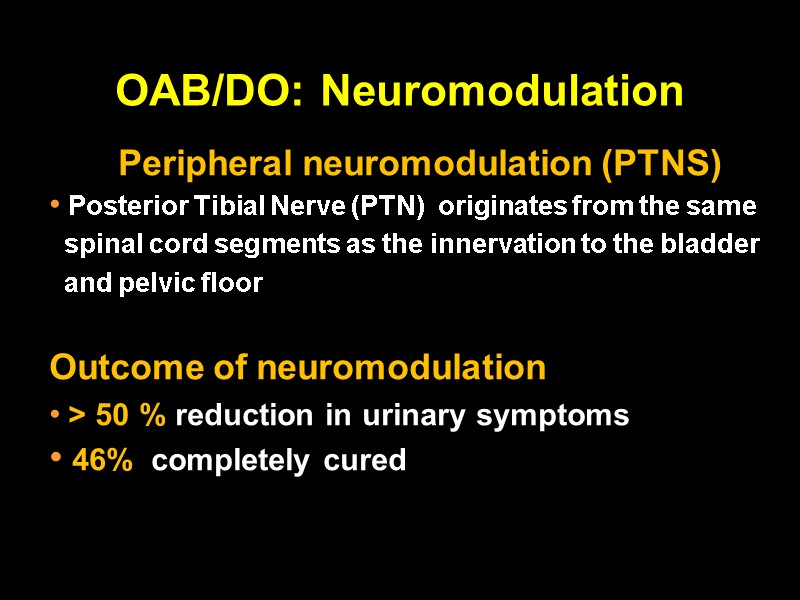
OAB/DO: Neuromodulation Peripheral neuromodulation (PTNS) Posterior Tibial Nerve (PTN) originates from the same spinal cord segments as the innervation to the bladder and pelvic floor Outcome of neuromodulation > 50 % reduction in urinary symptoms 46% completely cured
OAB/DO: Surgical management 10 % remain refractory to medical and behavioural therapy Different surgical techniques Augmentation Clam cystoplasty Auto-augmentation (Detrusor Myomectomy) Urinary Diversion
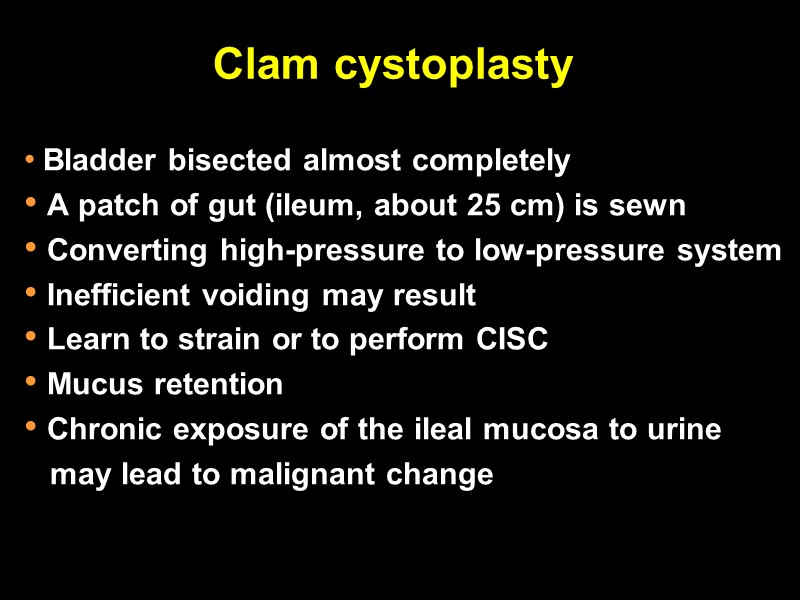
Clam cystoplasty Bladder bisected almost completely A patch of gut (ileum, about 25 cm) is sewn Converting high-pressure to low-pressure system Inefficient voiding may result Learn to strain or to perform CISC Mucus retention Chronic exposure of the ileal mucosa to urine may lead to malignant change
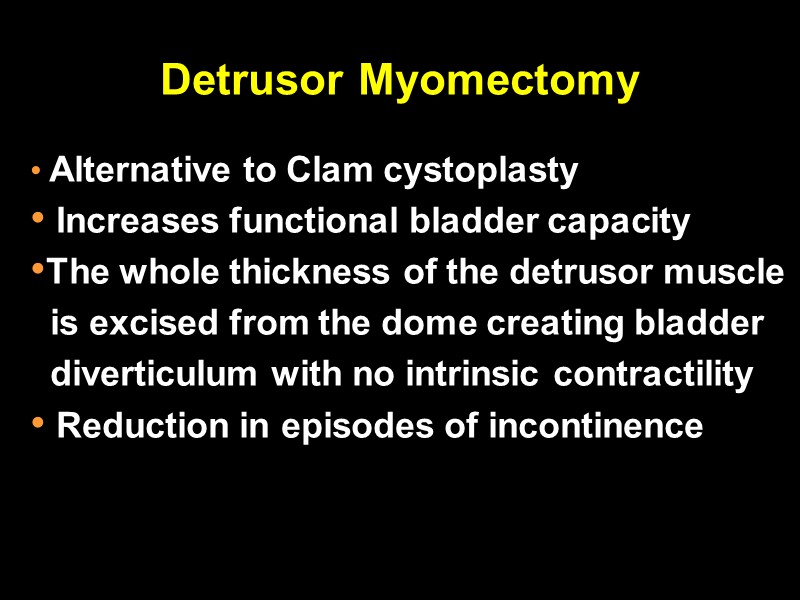
Detrusor Myomectomy Alternative to Clam cystoplasty Increases functional bladder capacity The whole thickness of the detrusor muscle is excised from the dome creating bladder diverticulum with no intrinsic contractility Reduction in episodes of incontinence
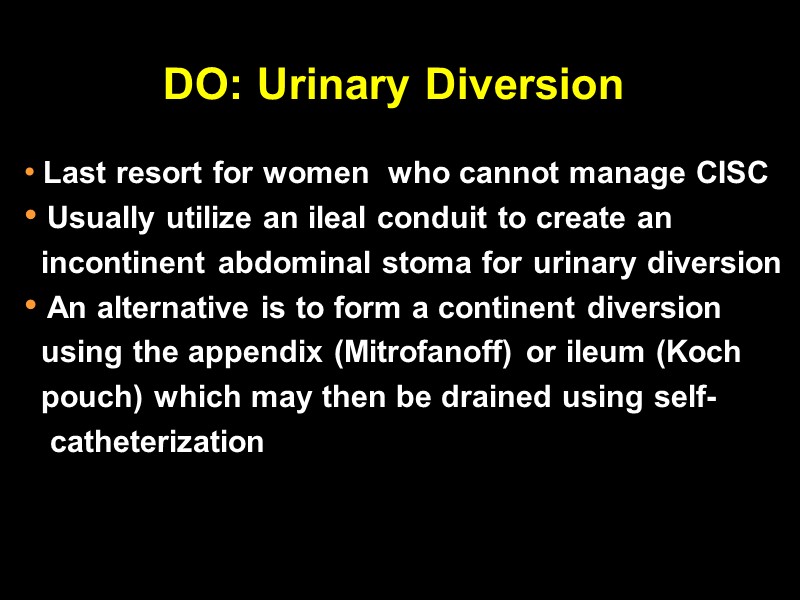
DO: Urinary Diversion Last resort for women who cannot manage CISC Usually utilize an ileal conduit to create an incontinent abdominal stoma for urinary diversion An alternative is to form a continent diversion using the appendix (Mitrofanoff) or ileum (Koch pouch) which may then be drained using self- catheterization
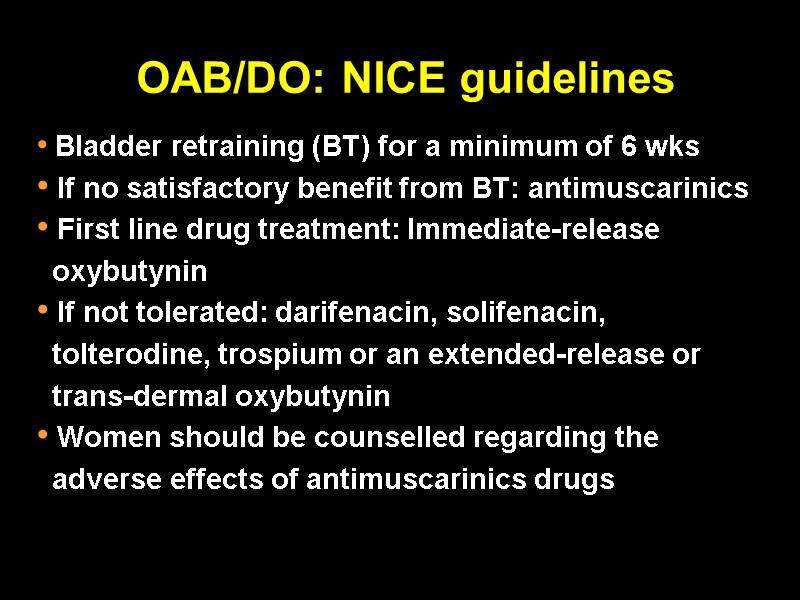
OAB/DO: NICE guidelines Bladder retraining (BT) for a minimum of 6 wks If no satisfactory benefit from BT: antimuscarinics First line drug treatment: Immediate-release oxybutynin If not tolerated: darifenacin, solifenacin, tolterodine, trospium or an extended-release or trans-dermal oxybutynin Women should be counselled regarding the adverse effects of antimuscarinics drugs
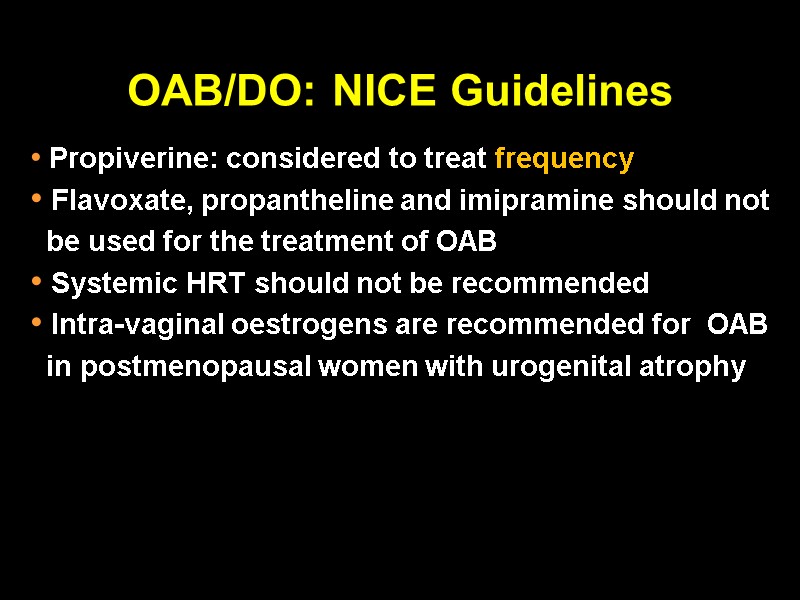
OAB/DO: NICE Guidelines Propiverine: considered to treat frequency Flavoxate, propantheline and imipramine should not be used for the treatment of OAB Systemic HRT should not be recommended Intra-vaginal oestrogens are recommended for OAB in postmenopausal women with urogenital atrophy
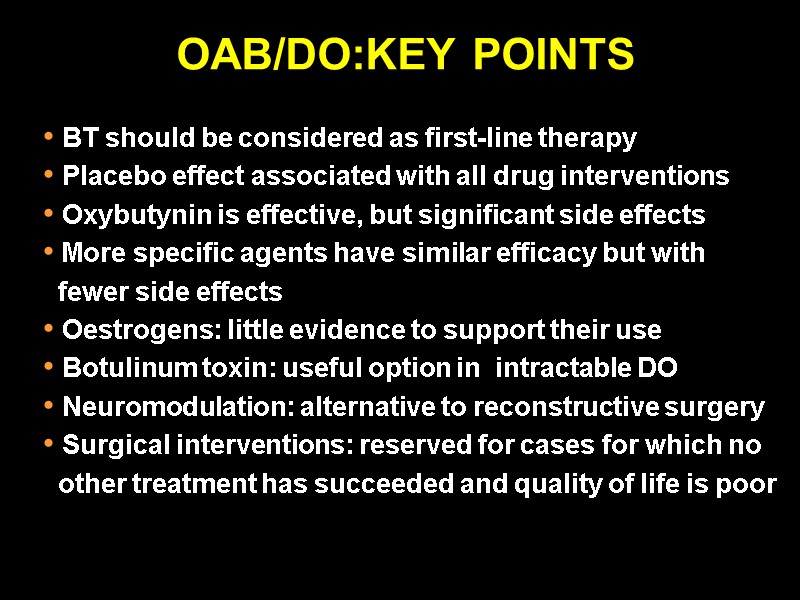
OAB/DO:KEY POINTS BT should be considered as first-line therapy Placebo effect associated with all drug interventions Oxybutynin is effective, but significant side effects More specific agents have similar efficacy but with fewer side effects Oestrogens: little evidence to support their use Botulinum toxin: useful option in intractable DO Neuromodulation: alternative to reconstructive surgery Surgical interventions: reserved for cases for which no other treatment has succeeded and quality of life is poor
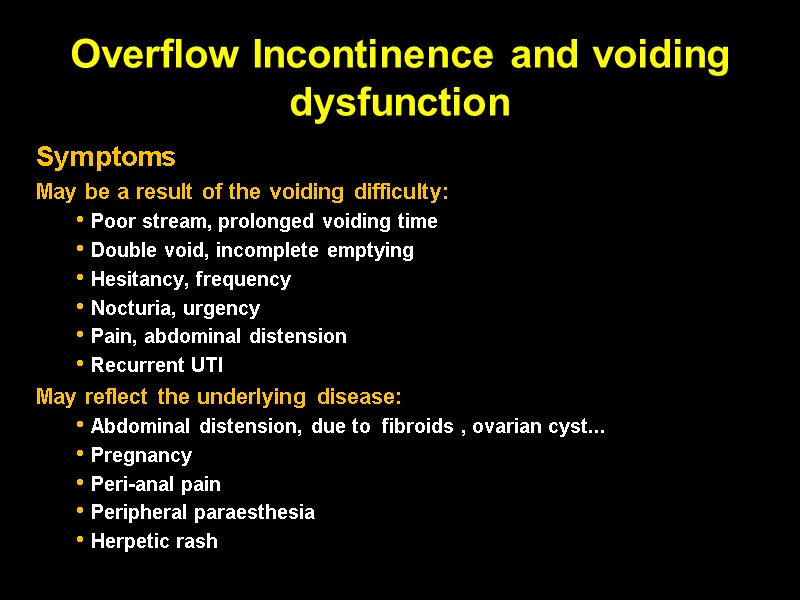
Overflow Incontinence and voiding dysfunction Symptoms May be a result of the voiding difficulty: Poor stream, prolonged voiding time Double void, incomplete emptying Hesitancy, frequency Nocturia, urgency Pain, abdominal distension Recurrent UTI May reflect the underlying disease: Abdominal distension, due to fibroids , ovarian cyst... Pregnancy Peri-anal pain Peripheral paraesthesia Herpetic rash
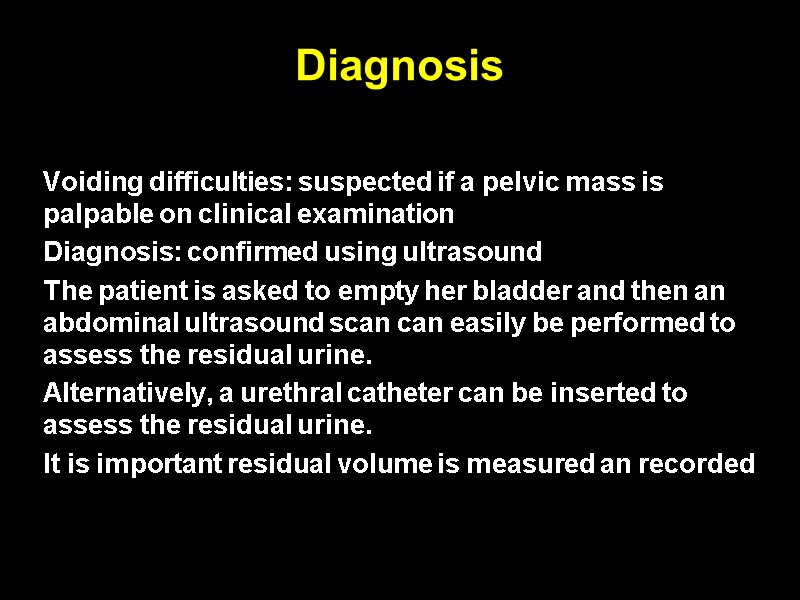
Diagnosis Voiding difficulties: suspected if a pelvic mass is palpable on clinical examination Diagnosis: confirmed using ultrasound The patient is asked to empty her bladder and then an abdominal ultrasound scan can easily be performed to assess the residual urine. Alternatively, a urethral catheter can be inserted to assess the residual urine. It is important residual volume is measured an recorded
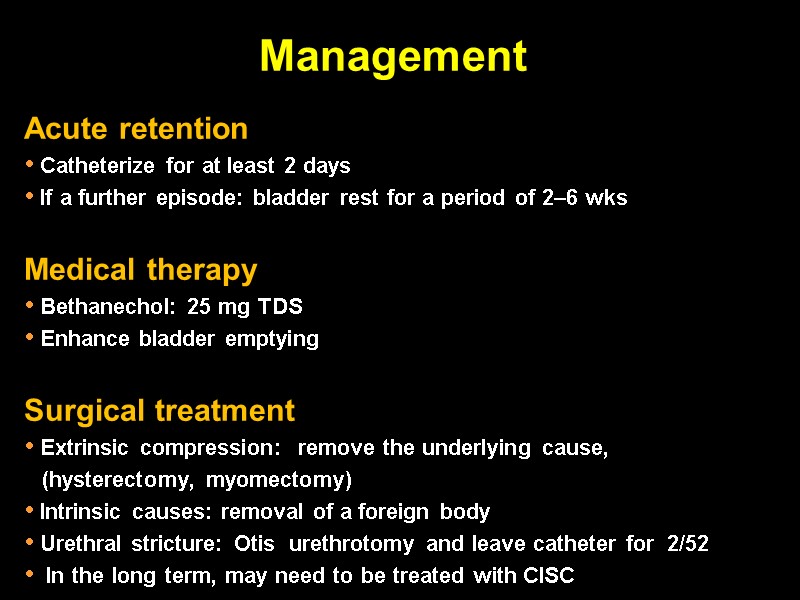
Management Acute retention Catheterize for at least 2 days If a further episode: bladder rest for a period of 2–6 wks Medical therapy Bethanechol: 25 mg TDS Enhance bladder emptying Surgical treatment Extrinsic compression: remove the underlying cause, (hysterectomy, myomectomy) Intrinsic causes: removal of a foreign body Urethral stricture: Otis urethrotomy and leave catheter for 2/52 In the long term, may need to be treated with CISC
Pelvic Organ Prolapse (POP)
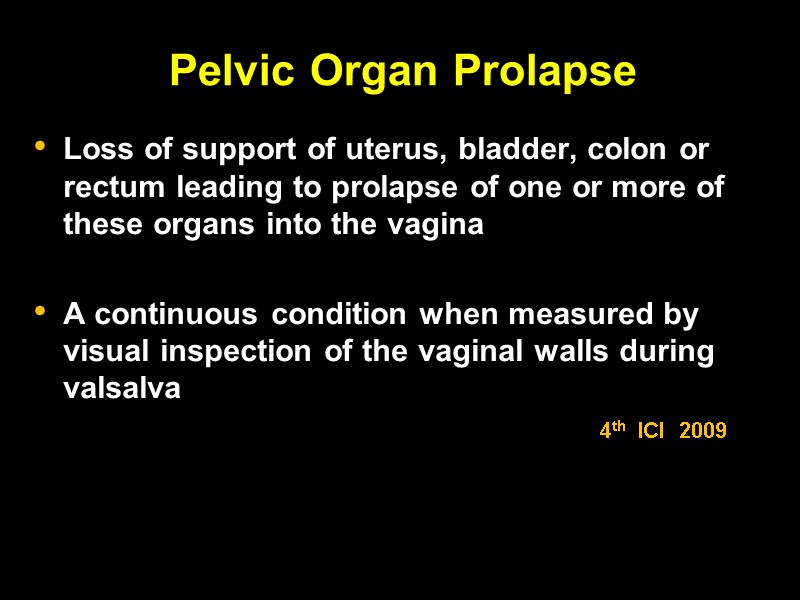
Pelvic Organ Prolapse Loss of support of uterus, bladder, colon or rectum leading to prolapse of one or more of these organs into the vagina A continuous condition when measured by visual inspection of the vaginal walls during valsalva 4th ICI 2009
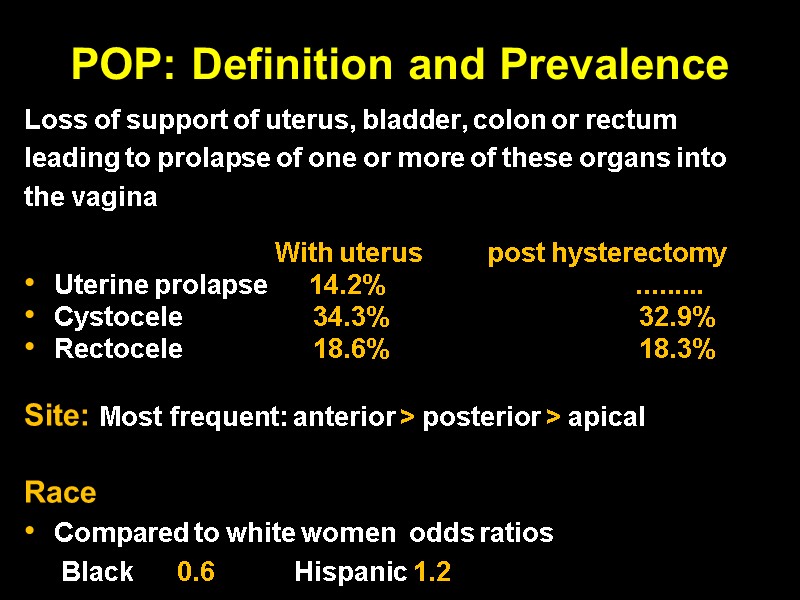
POP: Definition and Prevalence Loss of support of uterus, bladder, colon or rectum leading to prolapse of one or more of these organs into the vagina With uterus post hysterectomy Uterine prolapse 14.2% ......... Cystocele 34.3% 32.9% Rectocele 18.6% 18.3% Site: Most frequent: anterior > posterior > apical Race Compared to white women odds ratios Black 0.6 Hispanic 1.2
POP: Pathophysiology Injury to Neuromuscular tissue Connective tissue
Treatment of POP
Treatment of POP
Prevention of POP Avoid chronic increases in intra-abdominal pressure Constipation Chronic pulmonary diseases ?HRT: may decrease incidence to date (no studies) Smaller family size Improvements in antenatal and intrapartum care Role of C / section: studies showed mixed results Antenatal and postnatal PFMT : ? may be protective
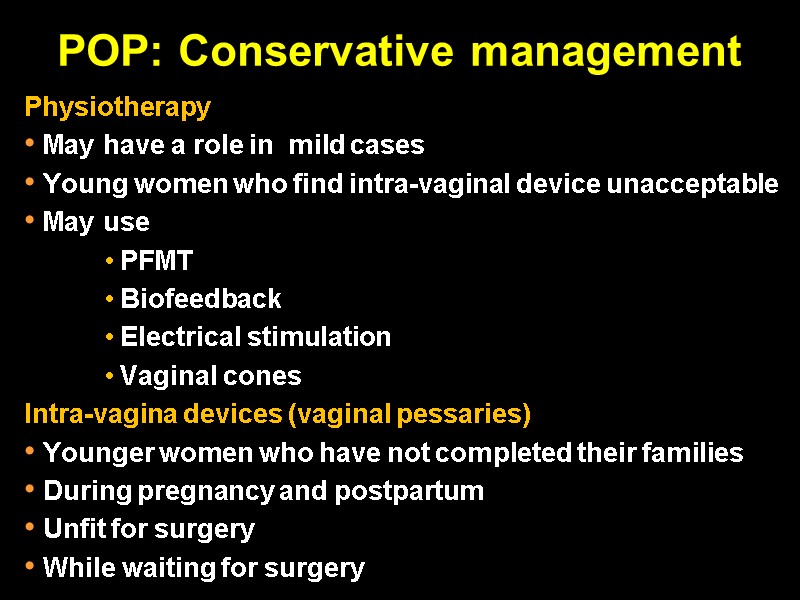
POP: Conservative management Physiotherapy May have a role in mild cases Young women who find intra-vaginal device unacceptable May use PFMT Biofeedback Electrical stimulation Vaginal cones Intra-vagina devices (vaginal pessaries) Younger women who have not completed their families During pregnancy and postpartum Unfit for surgery While waiting for surgery
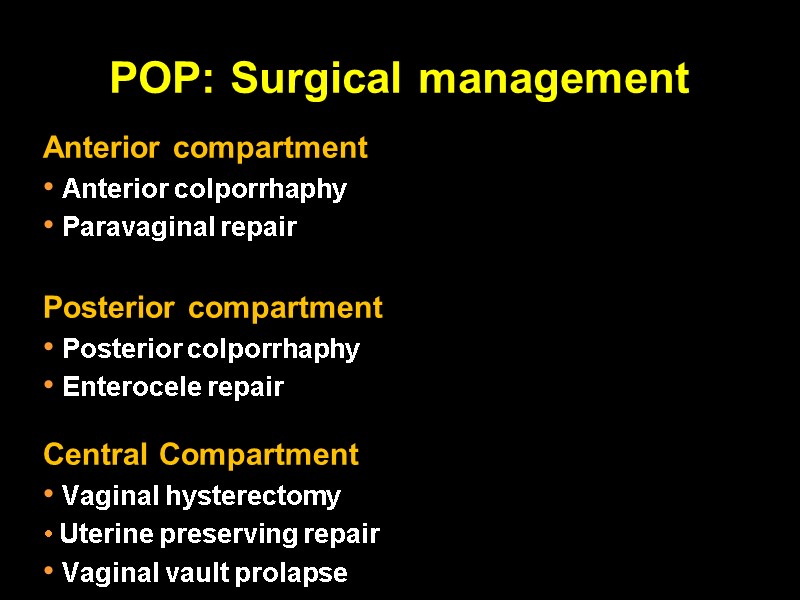
POP: Surgical management Anterior compartment Anterior colporrhaphy Paravaginal repair Posterior compartment Posterior colporrhaphy Enterocele repair Central Compartment Vaginal hysterectomy Uterine preserving repair Vaginal vault prolapse
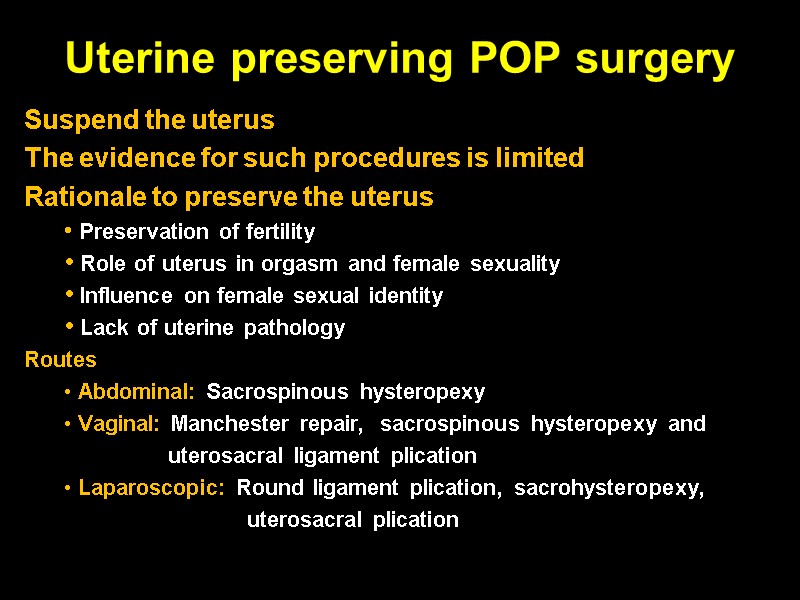
Uterine preserving POP surgery Suspend the uterus The evidence for such procedures is limited Rationale to preserve the uterus Preservation of fertility Role of uterus in orgasm and female sexuality Influence on female sexual identity Lack of uterine pathology Routes Abdominal: Sacrospinous hysteropexy Vaginal: Manchester repair, sacrospinous hysteropexy and uterosacral ligament plication Laparoscopic: Round ligament plication, sacrohysteropexy, uterosacral plication
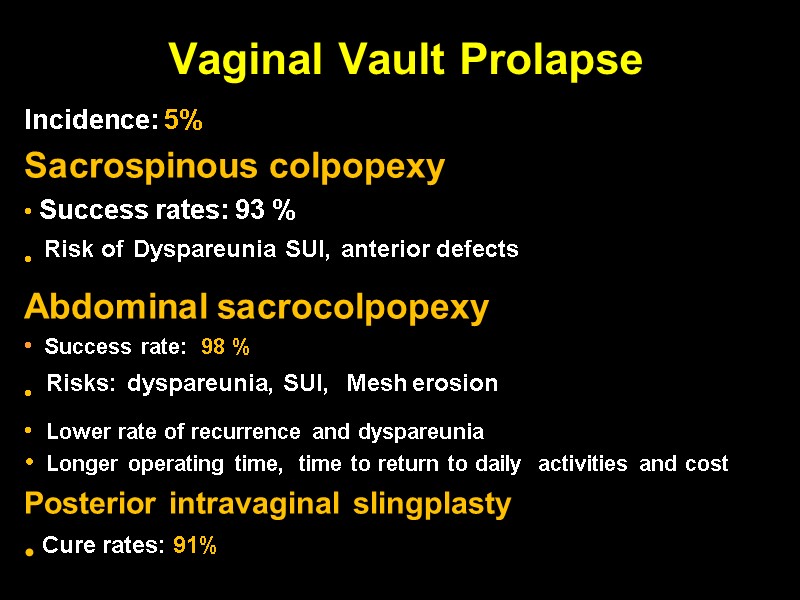
Vaginal Vault Prolapse Incidence: 5% Sacrospinous colpopexy Success rates: 93 % Risk of Dyspareunia SUI, anterior defects Abdominal sacrocolpopexy Success rate: 98 % Risks: dyspareunia, SUI, Mesh erosion Lower rate of recurrence and dyspareunia Longer operating time, time to return to daily activities and cost Posterior intravaginal slingplasty Cure rates: 91%
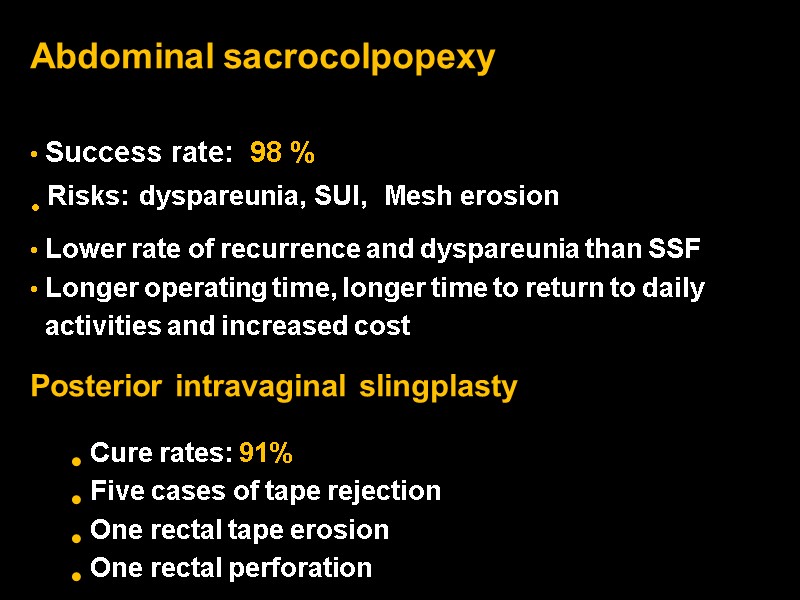
Abdominal sacrocolpopexy Success rate: 98 % Risks: dyspareunia, SUI, Mesh erosion Lower rate of recurrence and dyspareunia than SSF Longer operating time, longer time to return to daily activities and increased cost Posterior intravaginal slingplasty Cure rates: 91% Five cases of tape rejection One rectal tape erosion One rectal perforation
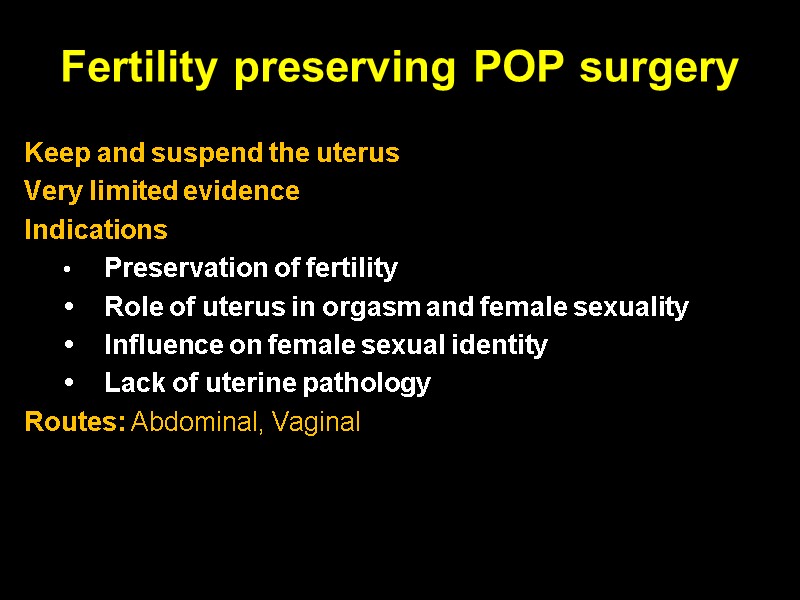
Fertility preserving POP surgery Keep and suspend the uterus Very limited evidence Indications • Preservation of fertility • Role of uterus in orgasm and female sexuality • Influence on female sexual identity • Lack of uterine pathology Routes: Abdominal, Vaginal
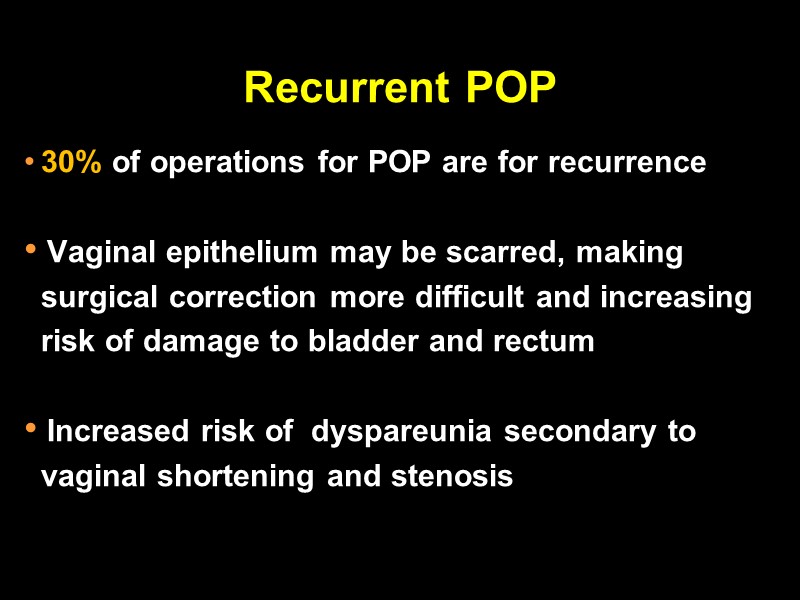
Recurrent POP 30% of operations for POP are for recurrence Vaginal epithelium may be scarred, making surgical correction more difficult and increasing risk of damage to bladder and rectum Increased risk of dyspareunia secondary to vaginal shortening and stenosis
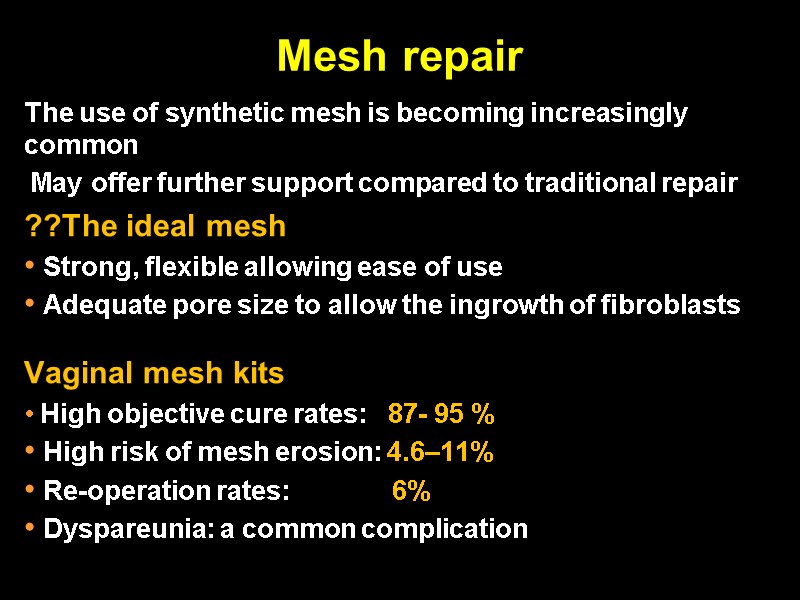
Mesh repair The use of synthetic mesh is becoming increasingly common May offer further support compared to traditional repair ??The ideal mesh Strong, flexible allowing ease of use Adequate pore size to allow the ingrowth of fibroblasts Vaginal mesh kits High objective cure rates: 87- 95 % High risk of mesh erosion: 4.6–11% Re-operation rates: 6% Dyspareunia: a common complication
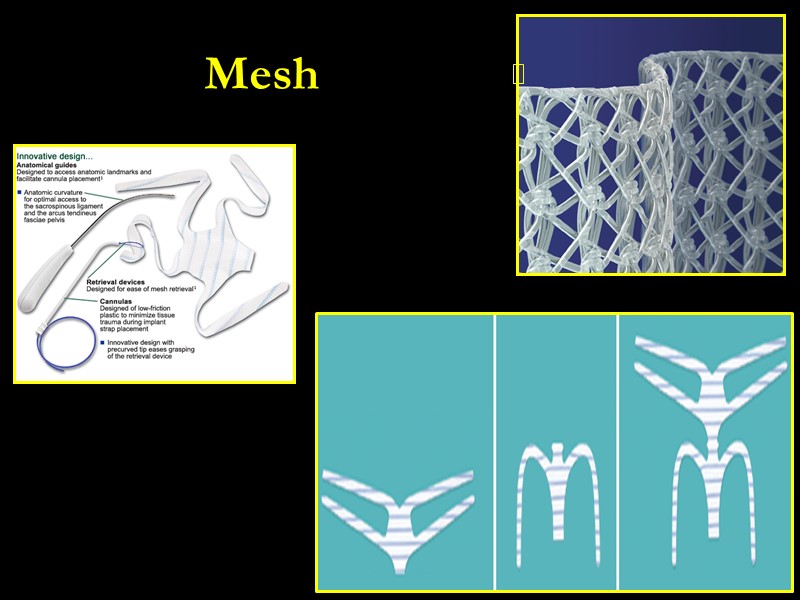
Mesh
OAB/DO: NICE Guidelines Propiverine: considered to treat frequency Flavoxate, propantheline and imipramine should not be used for the treatment of OAB Systemic HRT should not be recommended Intra-vaginal oestrogens are recommended for OAB in postmenopausal women with urogenital atrophy
Overactive bladder: summary BT should be considered as first-line therapy Placebo effect associated with all drug interventions Oxybutynin is effective, but significant side effects More specific agents have similar efficacy but with fewer side effects Oestrogens: little evidence to support their use Botulinum toxin: useful option in intractable DO Neuromodulation: alternative to reconstructive surgery Surgical interventions: reserved for cases for which no other treatment has succeeded and quality of life is poor
Stress urinary incontinence: summary PFMT of at least three months should be offered as first- line treatment to all women with SUI or MUI Retropubic tapes: recommended where conservative management failed Colposuspension: recommended alternatives Bulking agents: considered for the management of SUI if conservative management has failed Anterior repair, needle suspension procedures, paravaginal defect repair and the MMK procedure are not recommended
Pelvic organ prolapse: summary Common and associated with a high degree of morbidity Incidence increases with age and parity Lifetime risk of surgery is 11 % May be associated with urinary and faecal incontinence Conservative management : may be effective? Surgery: tailored to the needs of the individual patients Use of synthetic mesh for repeat procedures only High risk of recurrence, 30% require further surgery
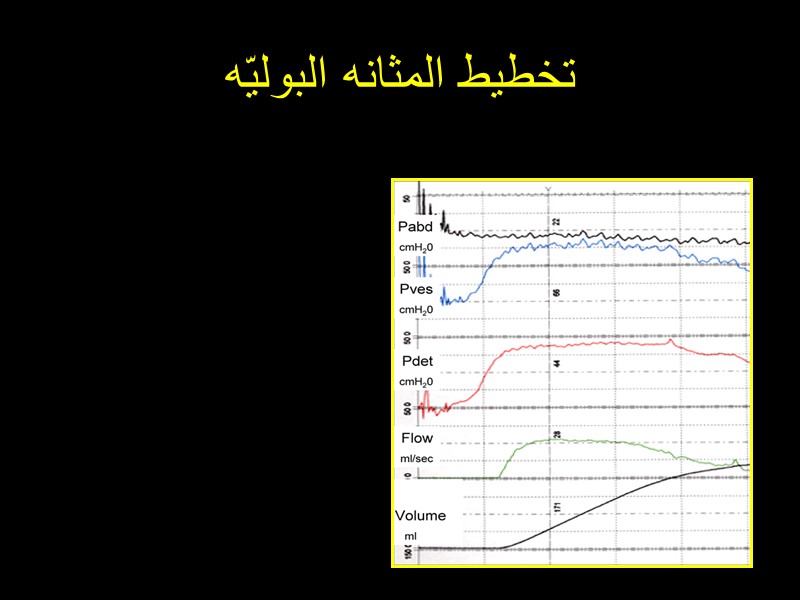
تخطيط المثانه البوليّه

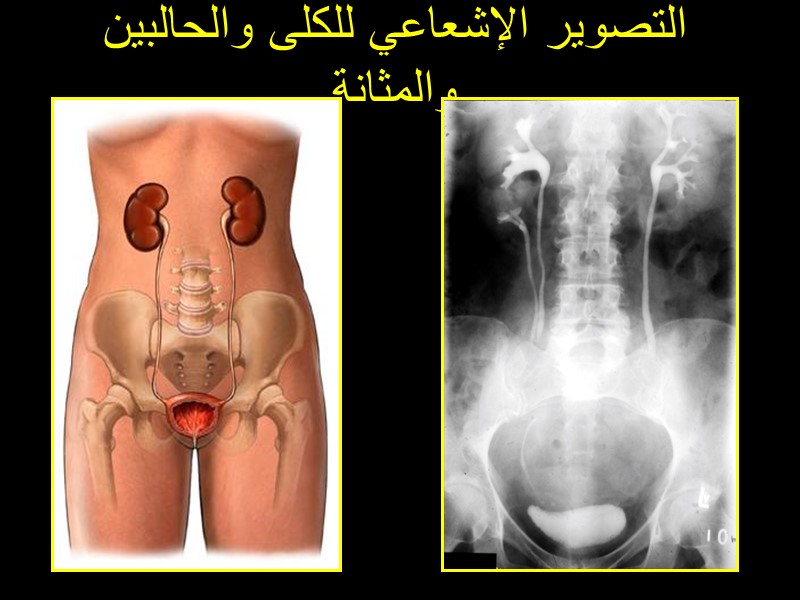
التصوير الإشعاعي للكلى والحالبين والمثانة
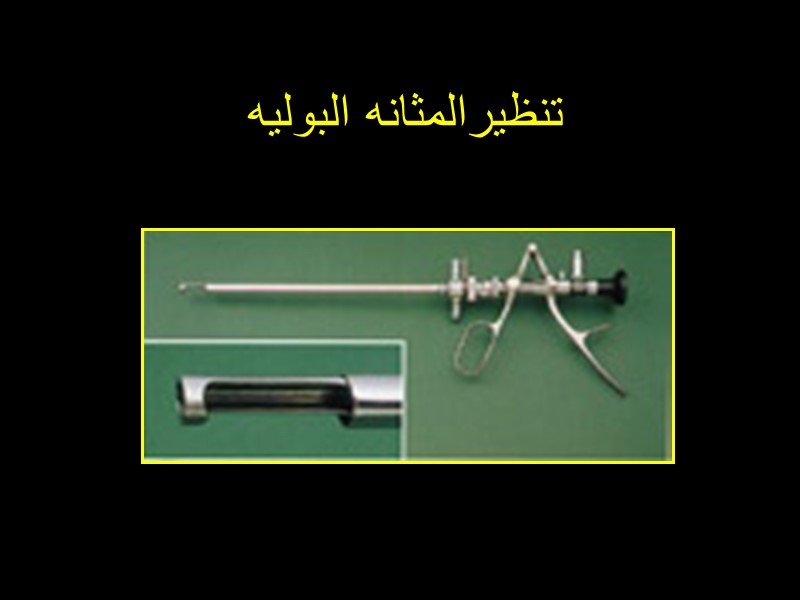
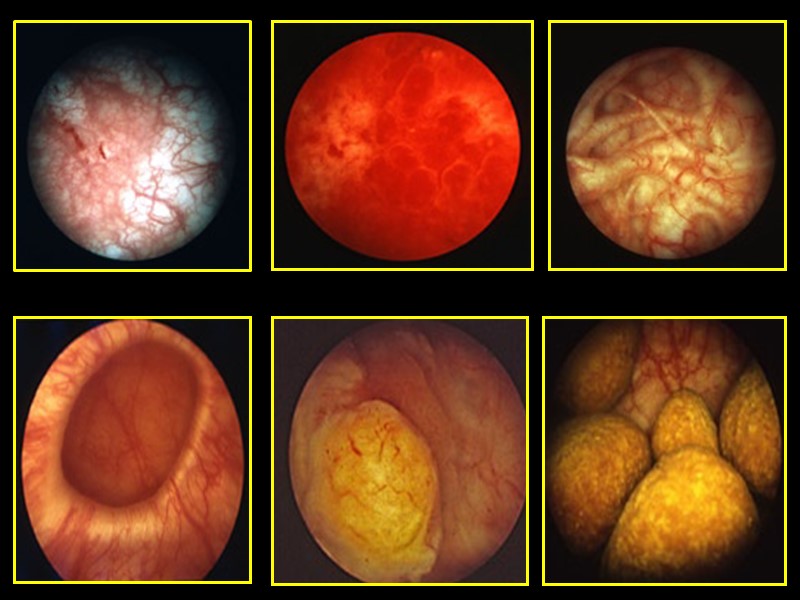
تنظيرالمثانه البوليه
35256-urogynaecology_an_introduction.ppt
- Количество слайдов: 103

