Urinary Tract Infections in children Rakovska L. Ass.

18200-10.1_uti_2015.ppt
- Количество слайдов: 98
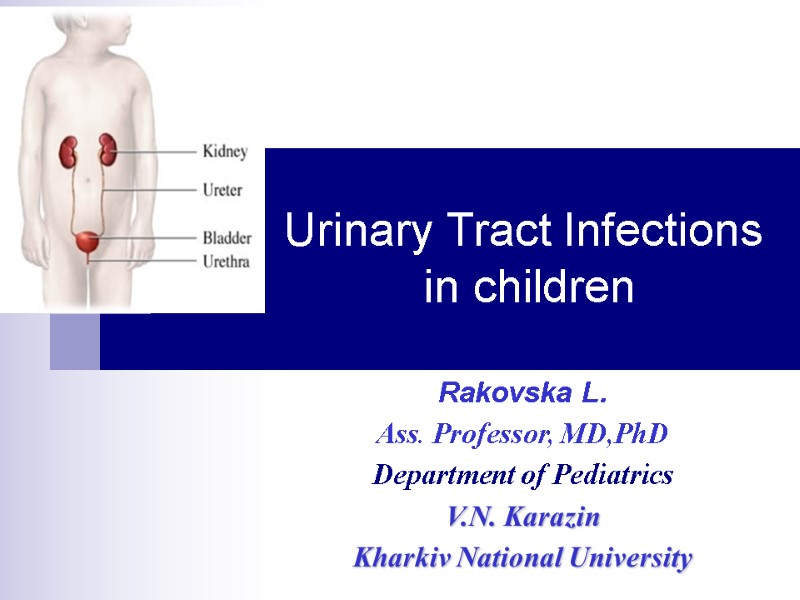
 Urinary Tract Infections in children Rakovska L. Ass. Professor, MD,PhD Department of Pediatrics V.N. Karazin Kharkiv National University
Urinary Tract Infections in children Rakovska L. Ass. Professor, MD,PhD Department of Pediatrics V.N. Karazin Kharkiv National University
 Urinary Tract Infections in children (UTI) a large group of diseases associated with microbial invasion and inflammation of the urinary system without indication of the localization
Urinary Tract Infections in children (UTI) a large group of diseases associated with microbial invasion and inflammation of the urinary system without indication of the localization
 Urinary Tract Infections in children (UTI) The 3 basic forms: Pyelonephritis, Cystitis, Asymptomatic bacteriuria
Urinary Tract Infections in children (UTI) The 3 basic forms: Pyelonephritis, Cystitis, Asymptomatic bacteriuria
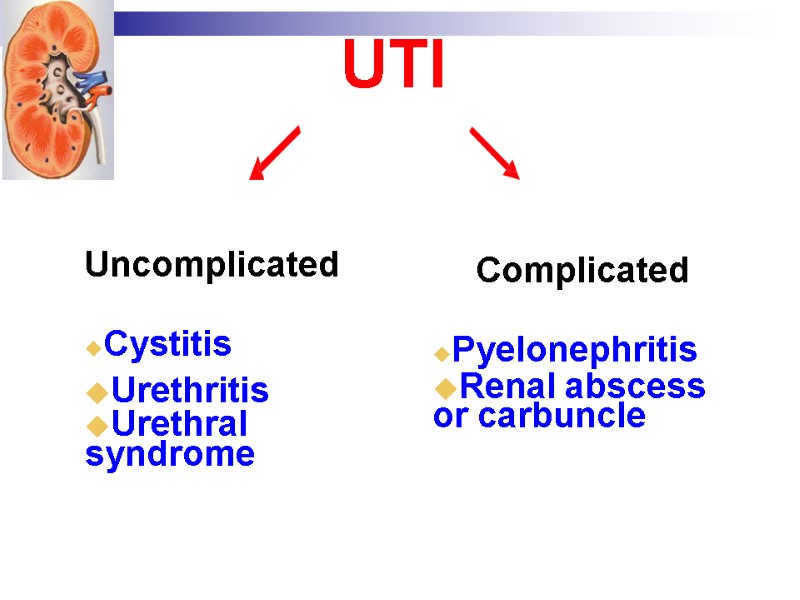
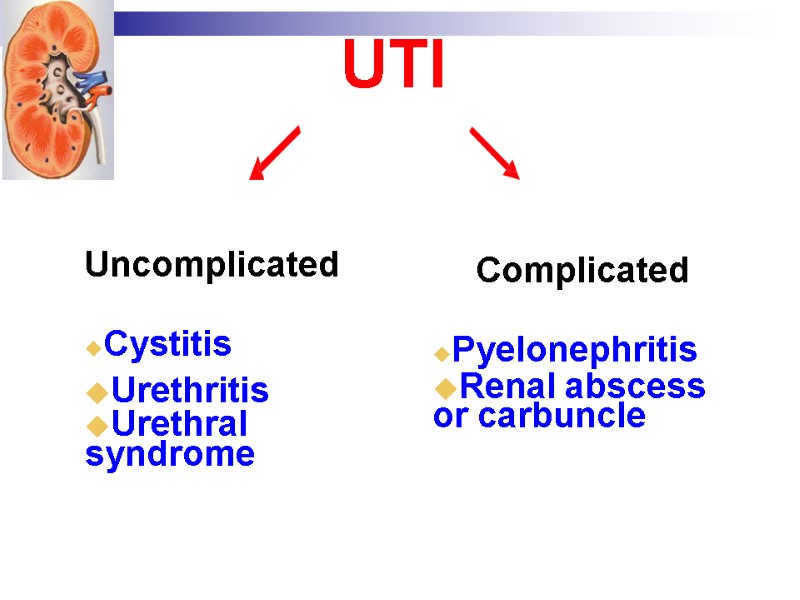 UTI Uncomplicated Cystitis Urethritis Urethral syndrome Complicated Pyelonephritis Renal abscess or carbuncle
UTI Uncomplicated Cystitis Urethritis Urethral syndrome Complicated Pyelonephritis Renal abscess or carbuncle
 UTI. Epidemiology. UTI is common in infants and children. Morbidity varies by age, sex, race In newborns – males : females incidence = 2:1 In childhood – 1:10.
UTI. Epidemiology. UTI is common in infants and children. Morbidity varies by age, sex, race In newborns – males : females incidence = 2:1 In childhood – 1:10.
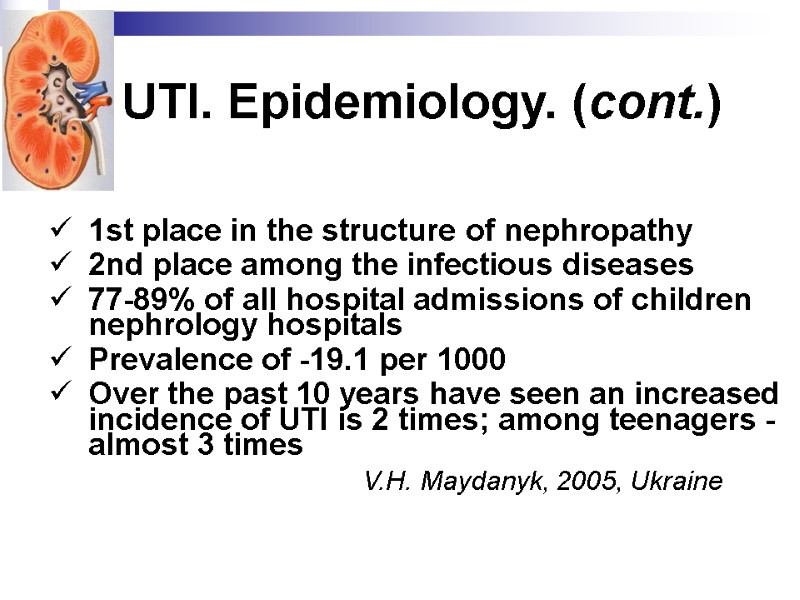 UTI. Epidemiology. (cont.) 1st place in the structure of nephropathy 2nd place among the infectious diseases 77-89% of all hospital admissions of children nephrology hospitals Prevalence of -19.1 per 1000 Over the past 10 years have seen an increased incidence of UTI is 2 times; among teenagers - almost 3 times V.H. Maydanyk, 2005, Ukraine
UTI. Epidemiology. (cont.) 1st place in the structure of nephropathy 2nd place among the infectious diseases 77-89% of all hospital admissions of children nephrology hospitals Prevalence of -19.1 per 1000 Over the past 10 years have seen an increased incidence of UTI is 2 times; among teenagers - almost 3 times V.H. Maydanyk, 2005, Ukraine
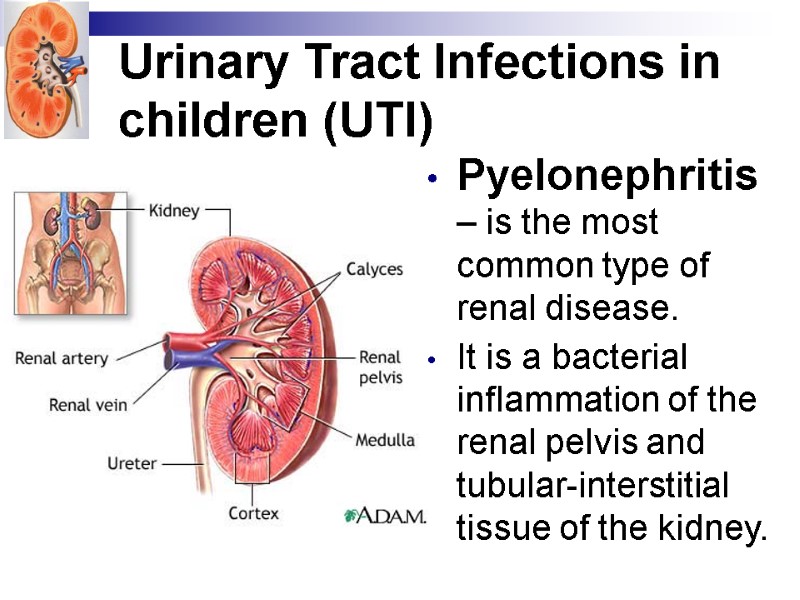
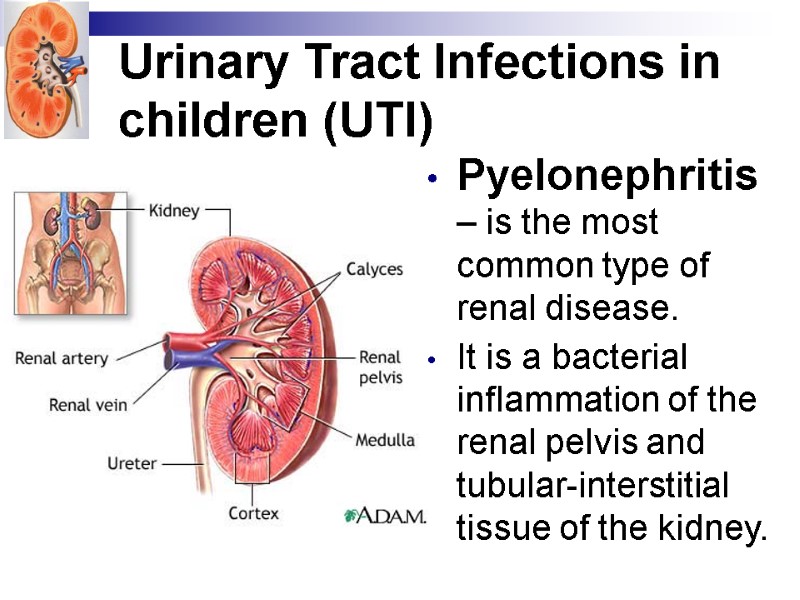 Urinary Tract Infections in children (UTI) Pyelonephritis – is the most common type of renal disease. It is a bacterial inflammation of the renal pelvis and tubular-interstitial tissue of the kidney.
Urinary Tract Infections in children (UTI) Pyelonephritis – is the most common type of renal disease. It is a bacterial inflammation of the renal pelvis and tubular-interstitial tissue of the kidney.
 UTI. Pyelonephritis leading place in a structure of renal pathology, main cause of progressive kidney failure, undulation course, exacerbation of disease due to various provocative factors gradual progress, followed by the future damage of vascular system of kidney with chronic ischemia. Chronic pyelonephritis are the cause of arterial hypertension.
UTI. Pyelonephritis leading place in a structure of renal pathology, main cause of progressive kidney failure, undulation course, exacerbation of disease due to various provocative factors gradual progress, followed by the future damage of vascular system of kidney with chronic ischemia. Chronic pyelonephritis are the cause of arterial hypertension.
 UTI. Etiology E. Coli – 90% Proteus mirabilis, Klebsiella, Enterococcus, Pseudomonas aeruginosa, Staph. saprophyticus, faecalis, aureus – 8% Other –2% sciencephoto.com
UTI. Etiology E. Coli – 90% Proteus mirabilis, Klebsiella, Enterococcus, Pseudomonas aeruginosa, Staph. saprophyticus, faecalis, aureus – 8% Other –2% sciencephoto.com
 UTI. Pyelonephritis. Etiology and pathogenesis Routes of contagion Ascending route (the most common) Hematogenous route (common in the neonatal period) Other routes (rare)
UTI. Pyelonephritis. Etiology and pathogenesis Routes of contagion Ascending route (the most common) Hematogenous route (common in the neonatal period) Other routes (rare)
 UTI. Pyelonephritis. Etiology and pathogenesis Routes of contagion (cont.) Ascending route (the most common) Fecal flora ascend through the urethra to the urinary bladder cystitis. If Pyelonephritis occurs, this means that organisms have ascended the ureters by vesicoureteric reflux (retrograde flow of urine from bladder up the ureters). The most common organisms are E.Coli, Klebsiella species, Proteus species, Enterococcus species, Staphylococcus faecalis, Pseudomonas aeruginosa.
UTI. Pyelonephritis. Etiology and pathogenesis Routes of contagion (cont.) Ascending route (the most common) Fecal flora ascend through the urethra to the urinary bladder cystitis. If Pyelonephritis occurs, this means that organisms have ascended the ureters by vesicoureteric reflux (retrograde flow of urine from bladder up the ureters). The most common organisms are E.Coli, Klebsiella species, Proteus species, Enterococcus species, Staphylococcus faecalis, Pseudomonas aeruginosa.
 UTI. Pyelonephritis. Etiology and pathogenesis Routes of contagion (cont.) Hematogenous route (common in the neonatal period) Organisms are blood borne to the kidney from GIT, respiratory tract, osteomyelitis or skin infection. In addition to Gram negative organisms, Gram+ve as Staphylococcus aureus and Streptococcus viridans may cause the infection. Other routes (rare) By lymphatics or direct spread from perinephric abscess.
UTI. Pyelonephritis. Etiology and pathogenesis Routes of contagion (cont.) Hematogenous route (common in the neonatal period) Organisms are blood borne to the kidney from GIT, respiratory tract, osteomyelitis or skin infection. In addition to Gram negative organisms, Gram+ve as Staphylococcus aureus and Streptococcus viridans may cause the infection. Other routes (rare) By lymphatics or direct spread from perinephric abscess.
 UTI. Pyelonephritis. Pathogenesis Adhesion of microorganisms Primary alteration and nonspecific inflammation Specific immunologic phase All phases are interrelated and represent a single mechanism of pathological process
UTI. Pyelonephritis. Pathogenesis Adhesion of microorganisms Primary alteration and nonspecific inflammation Specific immunologic phase All phases are interrelated and represent a single mechanism of pathological process
 UTI. Pyelonephritis. Pathogenesis Adhesion of microorganisms on epithelium of upper urinary tract leads to functional obstruction. Intrapelvis and intraureter pressure increases, which leads to obstruction calyces and tubules and cause pyelo-tubular reflux, resulting the bacteria penetrate the kidney, and inflammation occurs.
UTI. Pyelonephritis. Pathogenesis Adhesion of microorganisms on epithelium of upper urinary tract leads to functional obstruction. Intrapelvis and intraureter pressure increases, which leads to obstruction calyces and tubules and cause pyelo-tubular reflux, resulting the bacteria penetrate the kidney, and inflammation occurs.
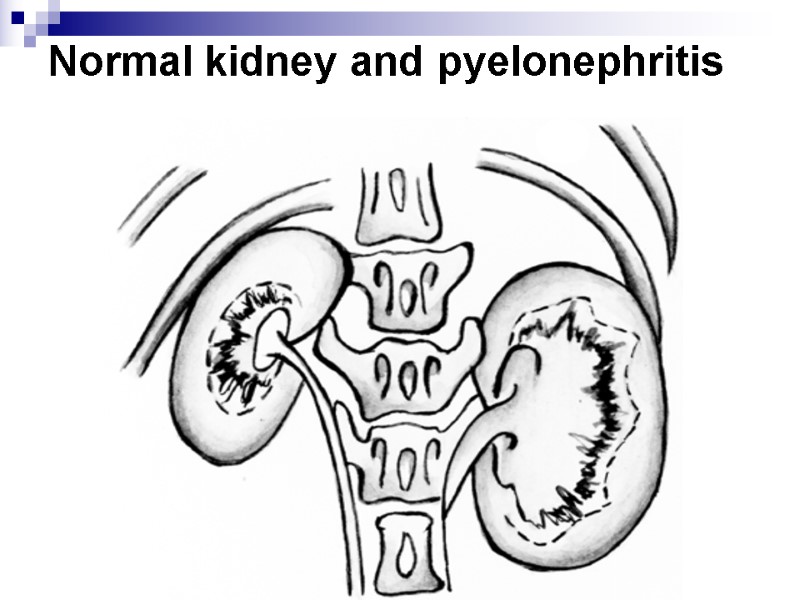
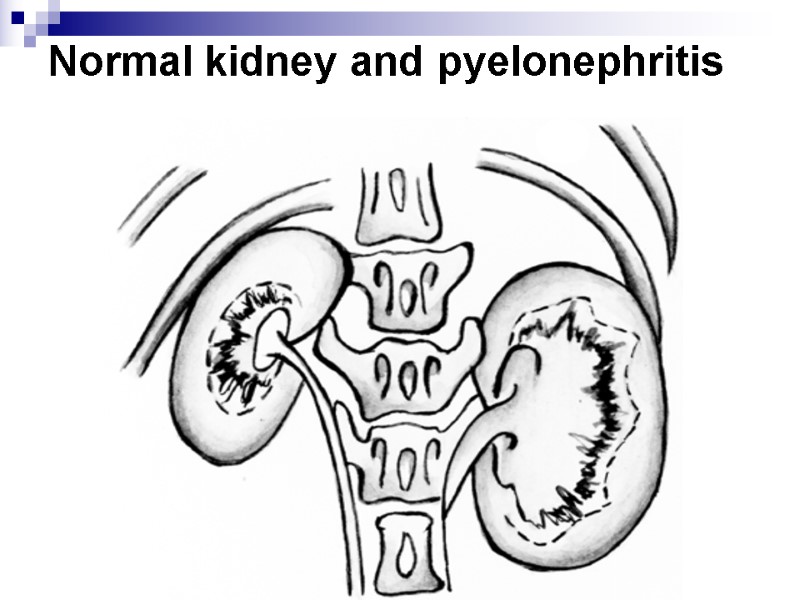 Normal kidney and pyelonephritis
Normal kidney and pyelonephritis
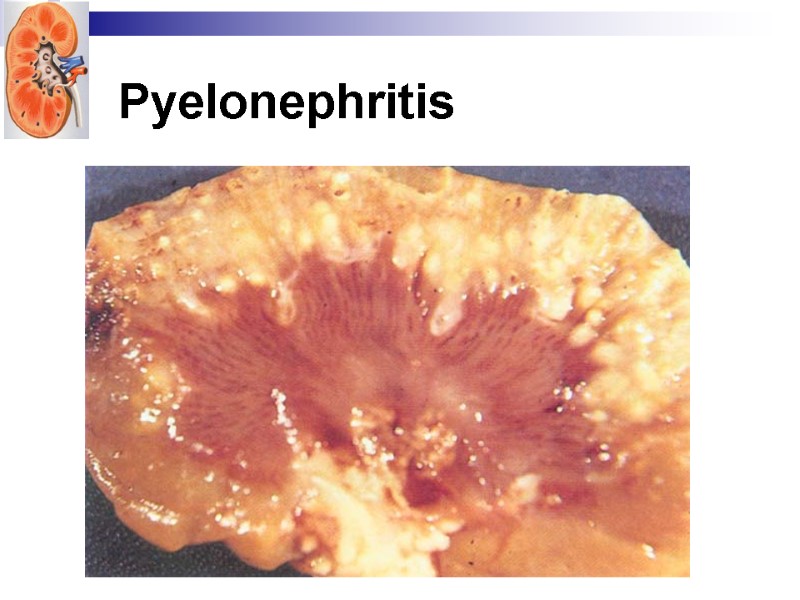
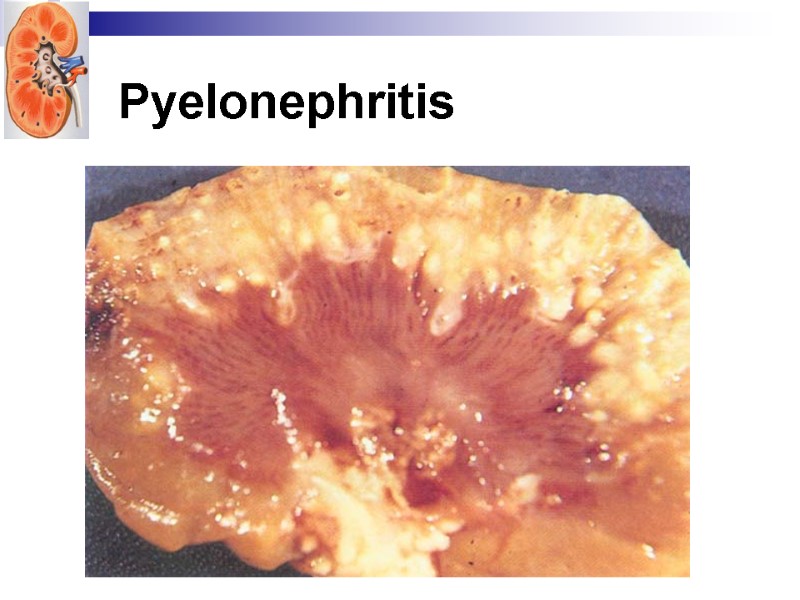 Pyelonephritis
Pyelonephritis
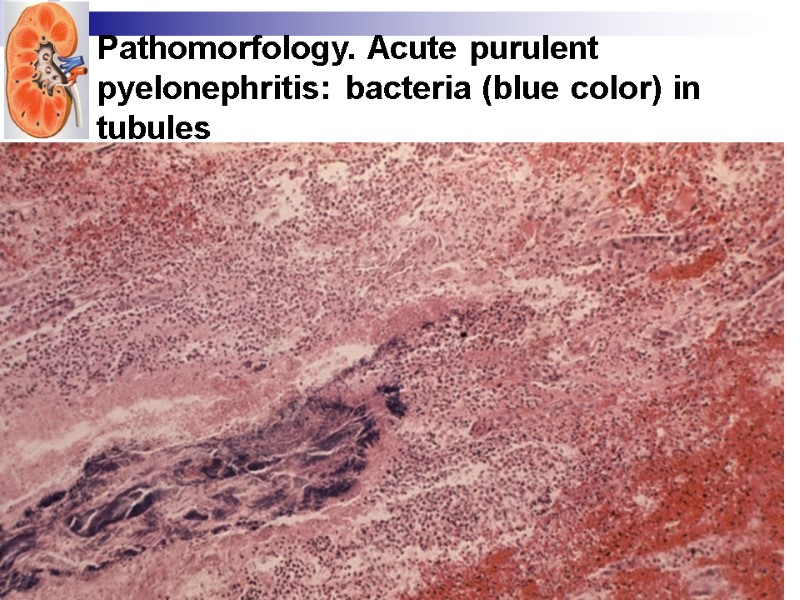
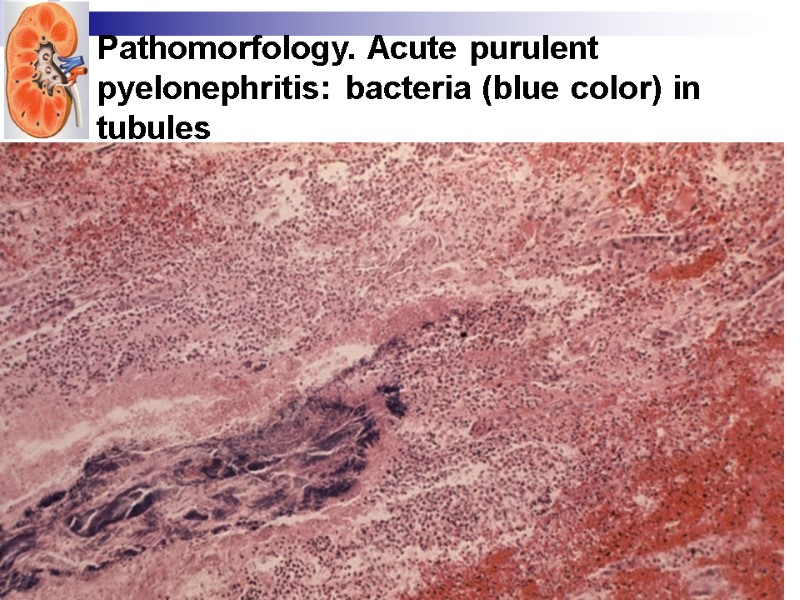 Pathomorfology. Acute purulent pyelonephritis: bacteria (blue color) in tubules
Pathomorfology. Acute purulent pyelonephritis: bacteria (blue color) in tubules
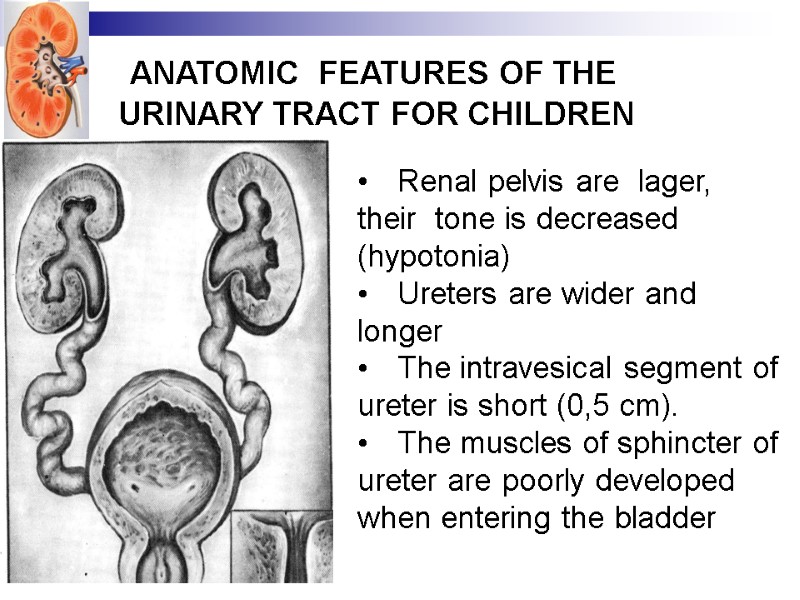
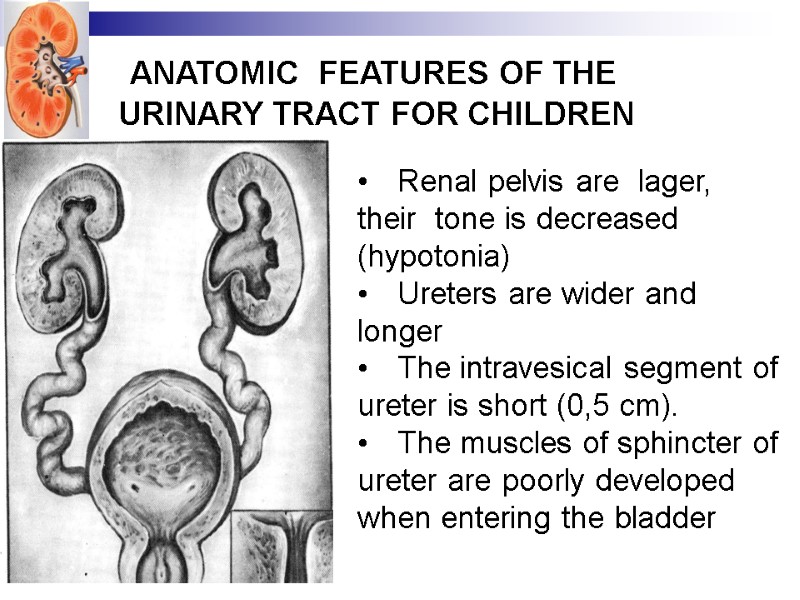 АНАТОМИЧЕСКИЕ ANATOMIC FEATURES OF THE URINARY TRACT FOR CHILDREN Renal pelvis are lager, their tone is decreased (hypotonia) Ureters are wider and longer The intravesical segment of ureter is short (0,5 cm). The muscles of sphincter of ureter are poorly developed when entering the bladder
АНАТОМИЧЕСКИЕ ANATOMIC FEATURES OF THE URINARY TRACT FOR CHILDREN Renal pelvis are lager, their tone is decreased (hypotonia) Ureters are wider and longer The intravesical segment of ureter is short (0,5 cm). The muscles of sphincter of ureter are poorly developed when entering the bladder
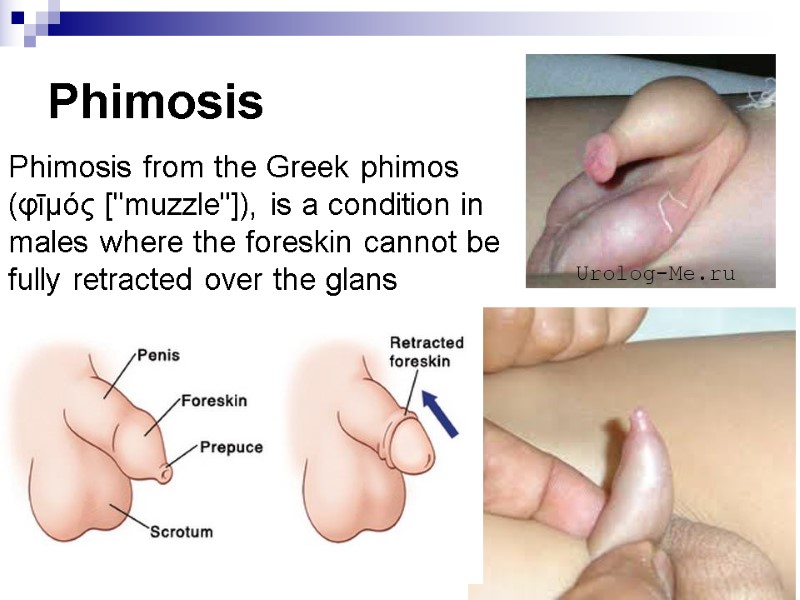
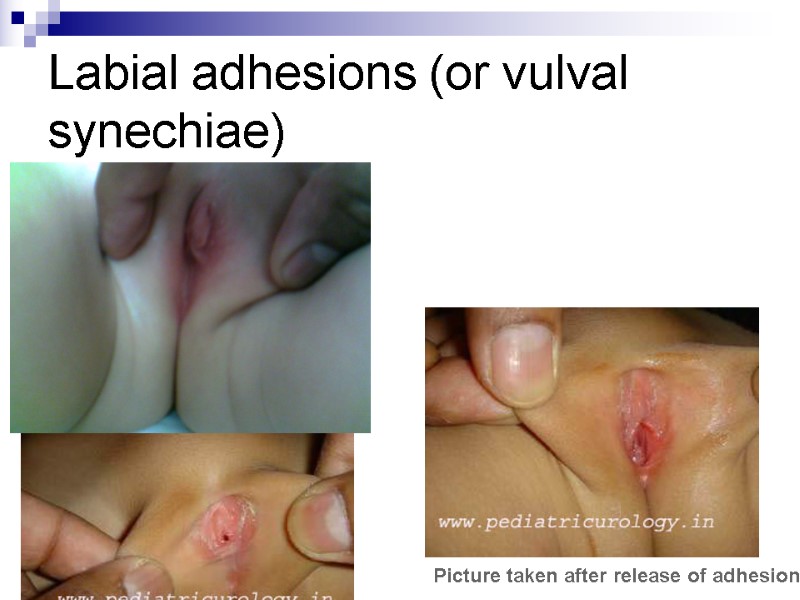
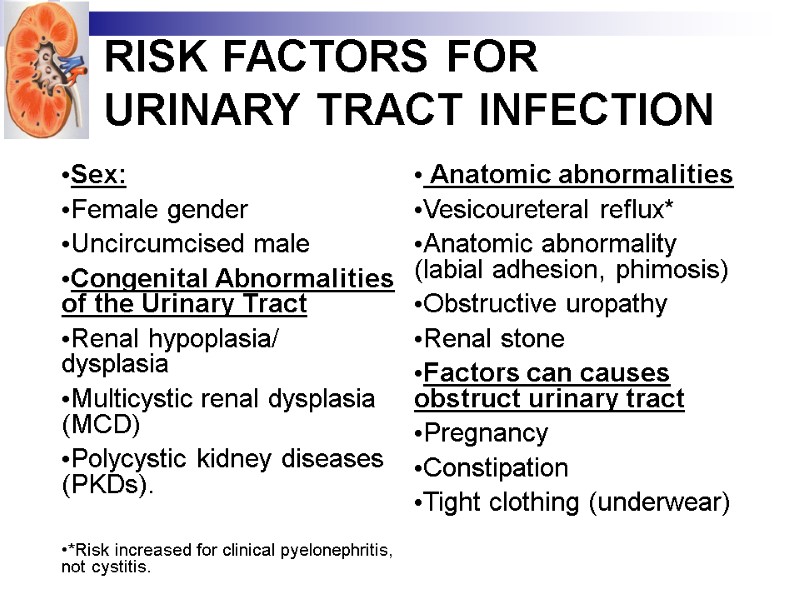 RISK FACTORS FOR URINARY TRACT INFECTION Sex: Female gender Uncircumcised male Congenital Abnormalities of the Urinary Tract Renal hypoplasia/ dysplasia Multicystic renal dysplasia (MCD) Polycystic kidney diseases (PKDs). *Risk increased for clinical pyelonephritis, not cystitis. Anatomic abnormalities Vesicoureteral reflux* Anatomic abnormality (labial adhesion, phimosis) Obstructive uropathy Renal stone Factors can causes obstruct urinary tract Pregnancy Constipation Tight clothing (underwear)
RISK FACTORS FOR URINARY TRACT INFECTION Sex: Female gender Uncircumcised male Congenital Abnormalities of the Urinary Tract Renal hypoplasia/ dysplasia Multicystic renal dysplasia (MCD) Polycystic kidney diseases (PKDs). *Risk increased for clinical pyelonephritis, not cystitis. Anatomic abnormalities Vesicoureteral reflux* Anatomic abnormality (labial adhesion, phimosis) Obstructive uropathy Renal stone Factors can causes obstruct urinary tract Pregnancy Constipation Tight clothing (underwear)
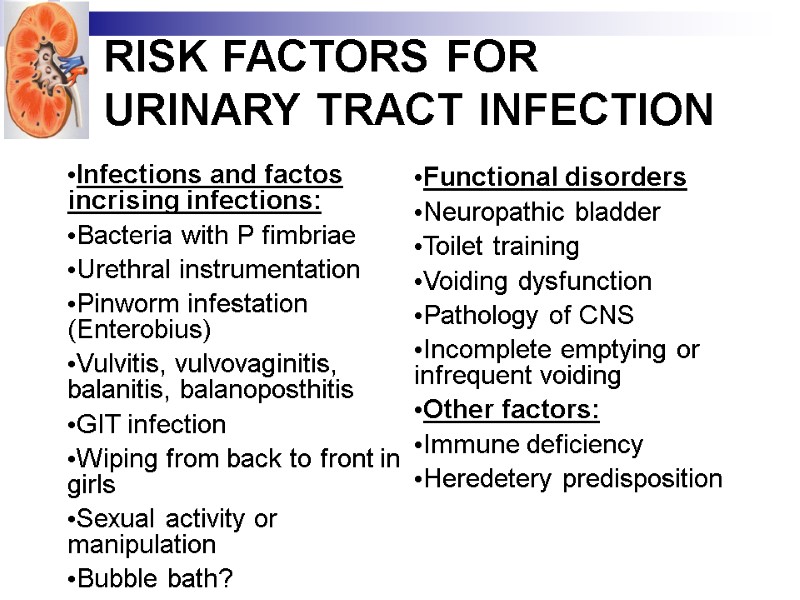 RISK FACTORS FOR URINARY TRACT INFECTION Infections and factos incrising infections: Bacteria with P fimbriae Urethral instrumentation Pinworm infestation (Enterobius) Vulvitis, vulvovaginitis, balanitis, balanoposthitis GIT infection Wiping from back to front in girls Sexual activity or manipulation Bubble bath? *Risk increased for clinical pyelonephritis, not cystitis. Functional disorders Neuropathic bladder Toilet training Voiding dysfunction Pathology of CNS Incomplete emptying or infrequent voiding Other factors: Immune deficiency Heredetery predisposition
RISK FACTORS FOR URINARY TRACT INFECTION Infections and factos incrising infections: Bacteria with P fimbriae Urethral instrumentation Pinworm infestation (Enterobius) Vulvitis, vulvovaginitis, balanitis, balanoposthitis GIT infection Wiping from back to front in girls Sexual activity or manipulation Bubble bath? *Risk increased for clinical pyelonephritis, not cystitis. Functional disorders Neuropathic bladder Toilet training Voiding dysfunction Pathology of CNS Incomplete emptying or infrequent voiding Other factors: Immune deficiency Heredetery predisposition
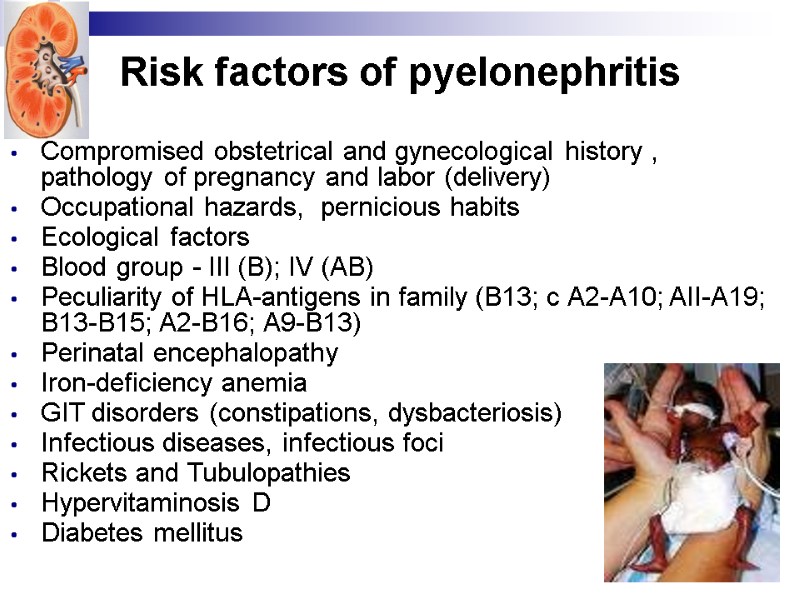 Compromised obstetrical and gynecological history , pathology of pregnancy and labor (delivery) Occupational hazards, pernicious habits Ecological factors Blood group - III (В); IV (АВ) Peculiarity of HLA-antigens in family (В13; с А2-А10; AII-A19; В13-В15; А2-В16; А9-В13) Perinatal encephalopathy Iron-deficiency anemia GIT disorders (constipations, dysbacteriosis) Infectious diseases, infectious foci Rickets and Tubulopathies Hypervitaminosis D Diabetes mellitus Risk factors of pyelonephritis
Compromised obstetrical and gynecological history , pathology of pregnancy and labor (delivery) Occupational hazards, pernicious habits Ecological factors Blood group - III (В); IV (АВ) Peculiarity of HLA-antigens in family (В13; с А2-А10; AII-A19; В13-В15; А2-В16; А9-В13) Perinatal encephalopathy Iron-deficiency anemia GIT disorders (constipations, dysbacteriosis) Infectious diseases, infectious foci Rickets and Tubulopathies Hypervitaminosis D Diabetes mellitus Risk factors of pyelonephritis
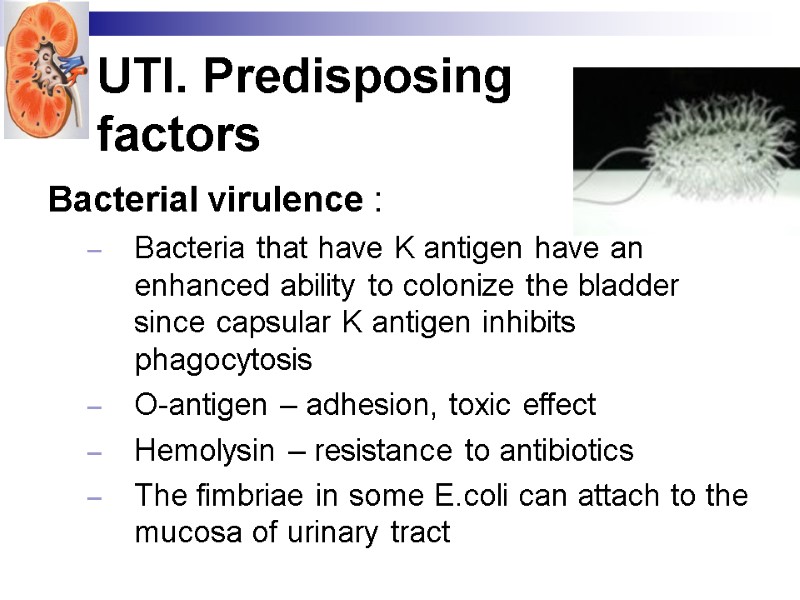 UTI. Predisposing factors Bacterial virulence : Bacteria that have K antigen have an enhanced ability to colonize the bladder since capsular K antigen inhibits phagocytosis O-antigen – adhesion, toxic effect Hemolysin – resistance to antibiotics The fimbriae in some E.coli can attach to the mucosa of urinary tract
UTI. Predisposing factors Bacterial virulence : Bacteria that have K antigen have an enhanced ability to colonize the bladder since capsular K antigen inhibits phagocytosis O-antigen – adhesion, toxic effect Hemolysin – resistance to antibiotics The fimbriae in some E.coli can attach to the mucosa of urinary tract
 UTI. Anatomical Predisposing factors Females have a relatively short urethra. Urethral orifice can be easily contaminated by feces.
UTI. Anatomical Predisposing factors Females have a relatively short urethra. Urethral orifice can be easily contaminated by feces.
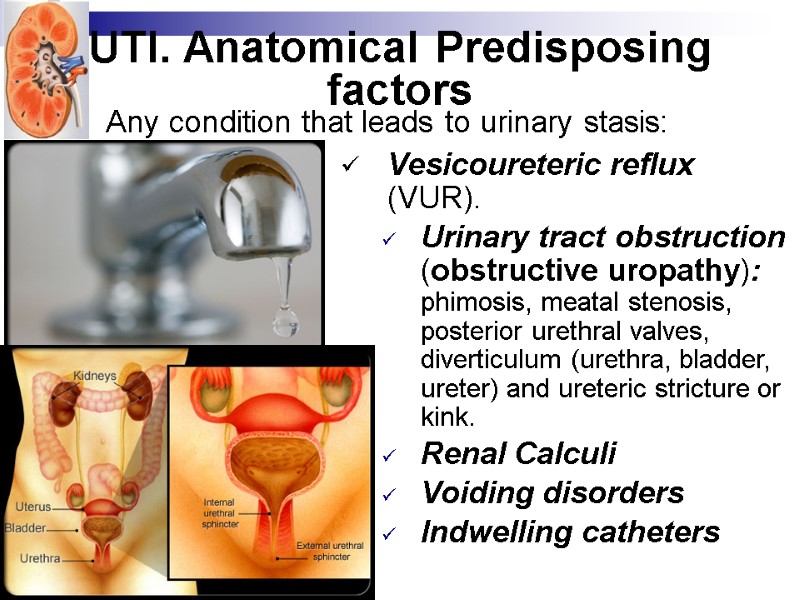
 UTI. Anatomical Predisposing factors Vesicoureteric reflux (VUR). Urinary tract obstruction (obstructive uropathy): phimosis, meatal stenosis, posterior urethral valves, diverticulum (urethra, bladder, ureter) and ureteric stricture or kink. Renal Calculi Voiding disorders Indwelling catheters Any condition that leads to urinary stasis:
UTI. Anatomical Predisposing factors Vesicoureteric reflux (VUR). Urinary tract obstruction (obstructive uropathy): phimosis, meatal stenosis, posterior urethral valves, diverticulum (urethra, bladder, ureter) and ureteric stricture or kink. Renal Calculi Voiding disorders Indwelling catheters Any condition that leads to urinary stasis:
 Congenital and Developmental Abnormalities of the Urinary Tract Renal hypoplasia/dysplasia Multicystic renal dysplasia (MCD) Polycystic kidney diseases (PKDs). sciencephoto.com
Congenital and Developmental Abnormalities of the Urinary Tract Renal hypoplasia/dysplasia Multicystic renal dysplasia (MCD) Polycystic kidney diseases (PKDs). sciencephoto.com
 UTI. Predisposing factors Host factors Functional disorders – Neurogenic bladder in spina bifida. Inappropriate detrusor contraction against closed sphincter increases the pressure inside bladder secondary VUR and renal damage. Immunologic – immune deficiency. Hereditary predisposition
UTI. Predisposing factors Host factors Functional disorders – Neurogenic bladder in spina bifida. Inappropriate detrusor contraction against closed sphincter increases the pressure inside bladder secondary VUR and renal damage. Immunologic – immune deficiency. Hereditary predisposition
 Classification of pyelonephritis Form Primary or secondary (obstructive, dysembriogenetic, dysmetabolic); Complicated or uncomplicated Course Acute or chronic (manifest recurrent or latent form). Phase or Period active or inactive; exacerbation, partial remission or remission. Renal function without function’s disorders, with function’s disorders, chronic renal insufficiency.
Classification of pyelonephritis Form Primary or secondary (obstructive, dysembriogenetic, dysmetabolic); Complicated or uncomplicated Course Acute or chronic (manifest recurrent or latent form). Phase or Period active or inactive; exacerbation, partial remission or remission. Renal function without function’s disorders, with function’s disorders, chronic renal insufficiency.
 UTI. Clinical symptoms Upper urinary tract infection (pyelonephritis) fever, loin pain and tenderness. Lower UTI (cystitis) bladder symptoms as urgency, frequency, dysuria, enuresis and dribbling
UTI. Clinical symptoms Upper urinary tract infection (pyelonephritis) fever, loin pain and tenderness. Lower UTI (cystitis) bladder symptoms as urgency, frequency, dysuria, enuresis and dribbling
 PYELONEPHRITIS. Clinical manifestations. Syndrome of intoxication fever, malaise, anorexia, nausea, vomiting; and, occasionally, diarrhea. Fever may be the only manifestation Painful syndrome pains in abdomen or lumbar region, positive Pasternatskiy symptom Syndrome of dysuria frequent and painful micturitions, incontinence.
PYELONEPHRITIS. Clinical manifestations. Syndrome of intoxication fever, malaise, anorexia, nausea, vomiting; and, occasionally, diarrhea. Fever may be the only manifestation Painful syndrome pains in abdomen or lumbar region, positive Pasternatskiy symptom Syndrome of dysuria frequent and painful micturitions, incontinence.
 ACUTE PYELONEPHRITIS. Clinical symptoms. A large proportion of children with active UTI are asymptomatic. The complaints when present may or may not be related to the urinary tract. In the neonatal period: a picture resembling sepsis: poor feeding; abnormal temperature; jaundice; hepatomegaly; or there may be an insidious onset with low grade fever, irritability, failure to gain weight.
ACUTE PYELONEPHRITIS. Clinical symptoms. A large proportion of children with active UTI are asymptomatic. The complaints when present may or may not be related to the urinary tract. In the neonatal period: a picture resembling sepsis: poor feeding; abnormal temperature; jaundice; hepatomegaly; or there may be an insidious onset with low grade fever, irritability, failure to gain weight.
 ACUTE PYELONEPHRITIS. Clinical symptoms. In infancy: The onset is usually sudden and severe with high fever, irritability, vomiting, anorexia and may be diarrhea. Meningismus and even convulsion may occur. Except for frequency and foul smelling (malodorous) urine, signs referable to the urinary tract are rare.
ACUTE PYELONEPHRITIS. Clinical symptoms. In infancy: The onset is usually sudden and severe with high fever, irritability, vomiting, anorexia and may be diarrhea. Meningismus and even convulsion may occur. Except for frequency and foul smelling (malodorous) urine, signs referable to the urinary tract are rare.
 Cystitis. Clinical manifestations. Dysuria, urgency, frequency Suprapubic pain, Incontinence, Malodorous urine (not specific for a UTI). Cystitis does not cause fever and does not result in renal injury.
Cystitis. Clinical manifestations. Dysuria, urgency, frequency Suprapubic pain, Incontinence, Malodorous urine (not specific for a UTI). Cystitis does not cause fever and does not result in renal injury.
 UTI. Asymptomatic bacteriuria refers to a condition in which there is a positive urine culture without any manifestations of infection. It is most common in preschool and school-age girls and is rare in boys. The incidence declines with increasing age. This condition is benign and does not cause renal injury, except in pregnant women, in whom asymptomatic bacteriuria, if left untreated, can result in a symptomatic UTI.
UTI. Asymptomatic bacteriuria refers to a condition in which there is a positive urine culture without any manifestations of infection. It is most common in preschool and school-age girls and is rare in boys. The incidence declines with increasing age. This condition is benign and does not cause renal injury, except in pregnant women, in whom asymptomatic bacteriuria, if left untreated, can result in a symptomatic UTI.
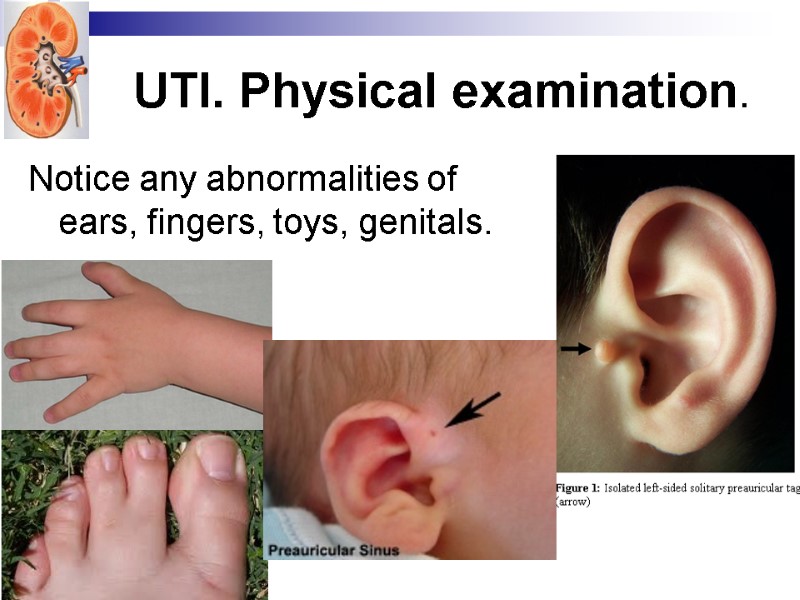
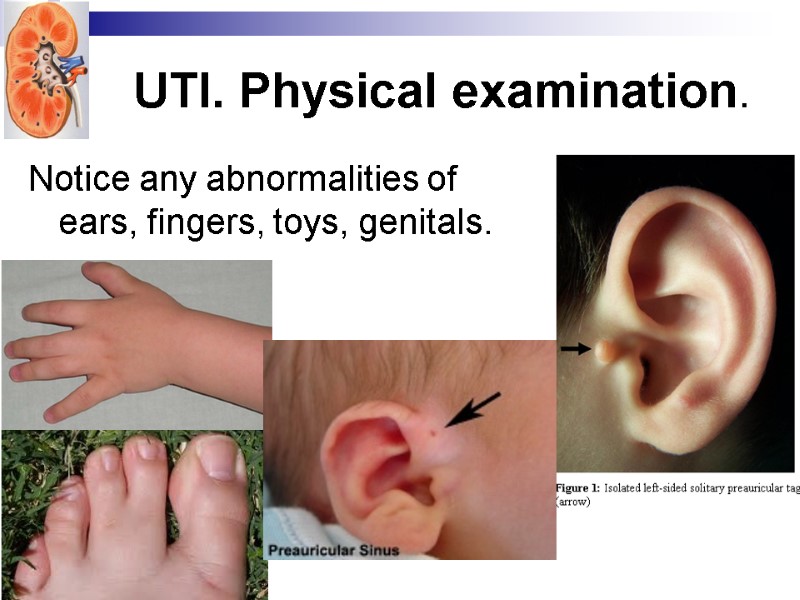 UTI. Physical examination. Notice any abnormalities of ears, fingers, toys, genitals.
UTI. Physical examination. Notice any abnormalities of ears, fingers, toys, genitals.
 Physical Examination MUST do a genital examination for children with abdominal pain or urinary tract symptoms Common findings Erythema secondary to vulvovaginitis Possible foreign body (external retained toilet paper) Evidence of sexual abuse (disrupted hymen, discharge) Pinworms Circumcision status Labial adhesions Prolapsed urethra
Physical Examination MUST do a genital examination for children with abdominal pain or urinary tract symptoms Common findings Erythema secondary to vulvovaginitis Possible foreign body (external retained toilet paper) Evidence of sexual abuse (disrupted hymen, discharge) Pinworms Circumcision status Labial adhesions Prolapsed urethra
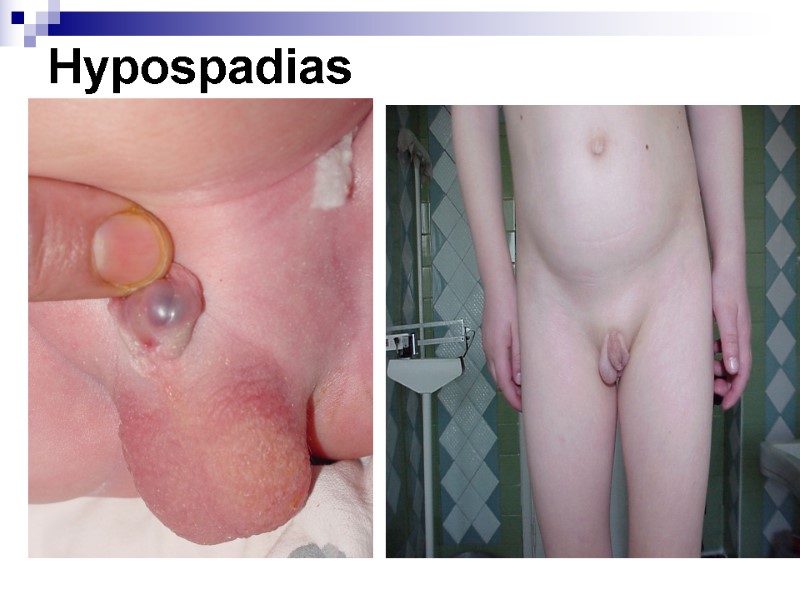
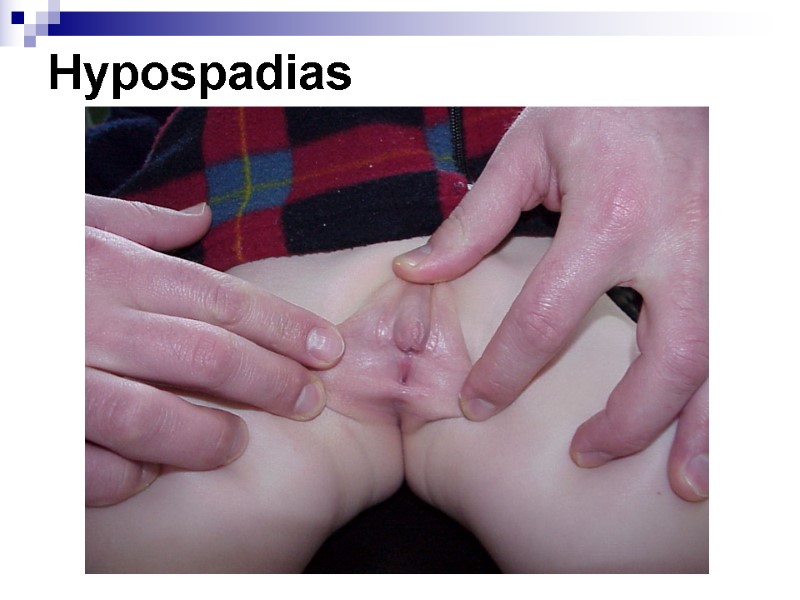
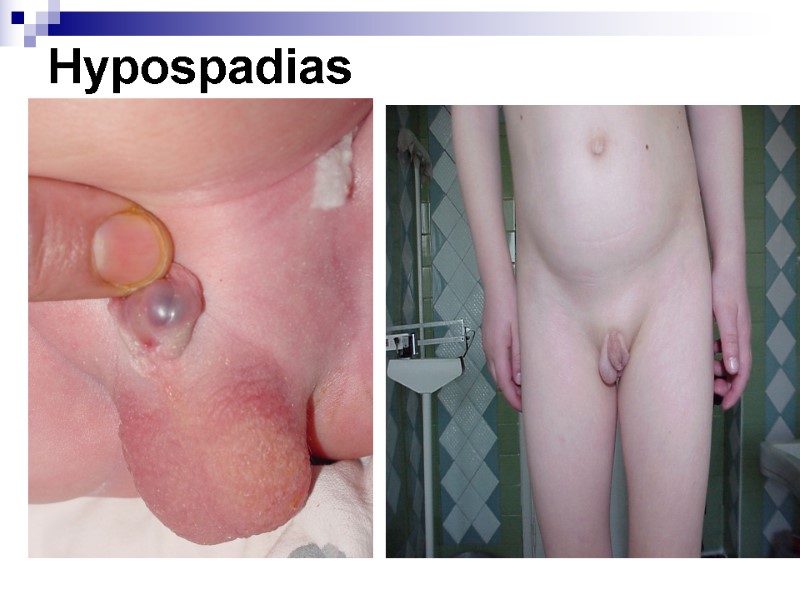 Hypospadias
Hypospadias
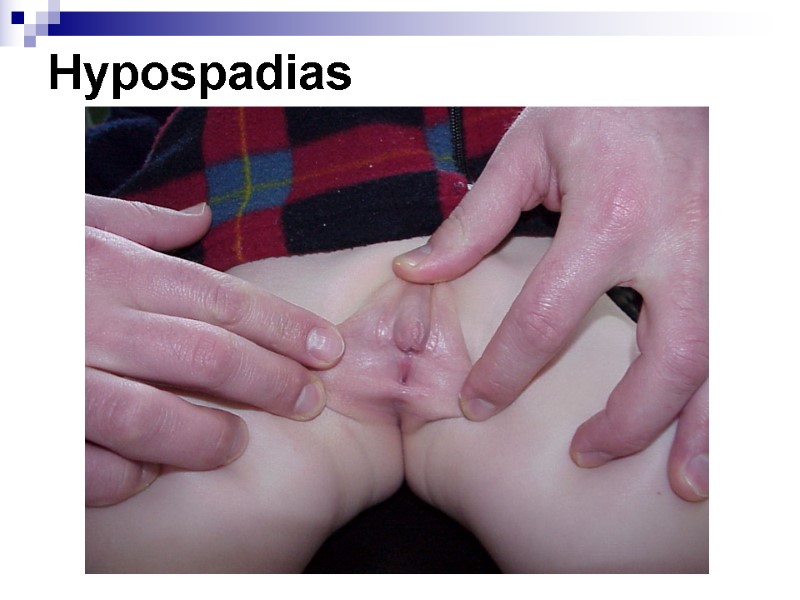 Hypospadias
Hypospadias
 Difficulty of urination DISORDERS OF MICTURITION
Difficulty of urination DISORDERS OF MICTURITION
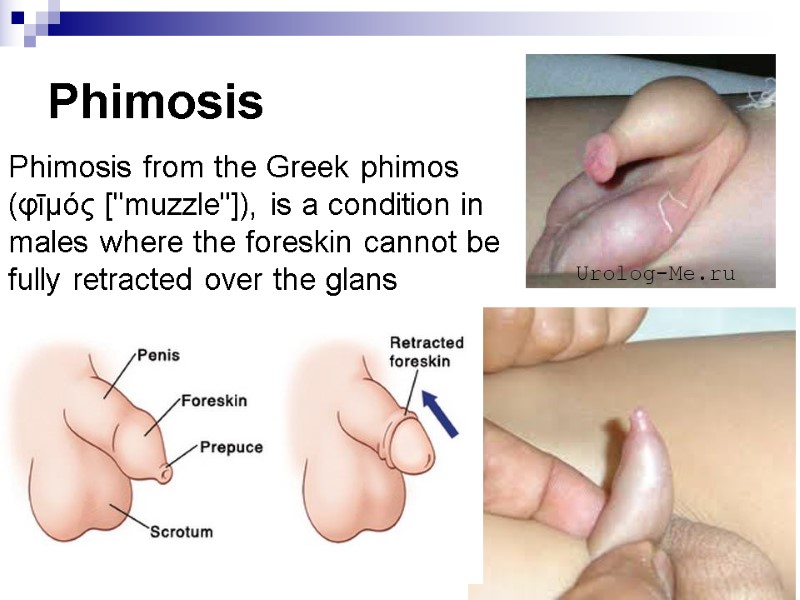 Phimosis Phimosis from the Greek phimos (φῑμός ["muzzle"]), is a condition in males where the foreskin cannot be fully retracted over the glans penis.
Phimosis Phimosis from the Greek phimos (φῑμός ["muzzle"]), is a condition in males where the foreskin cannot be fully retracted over the glans penis.
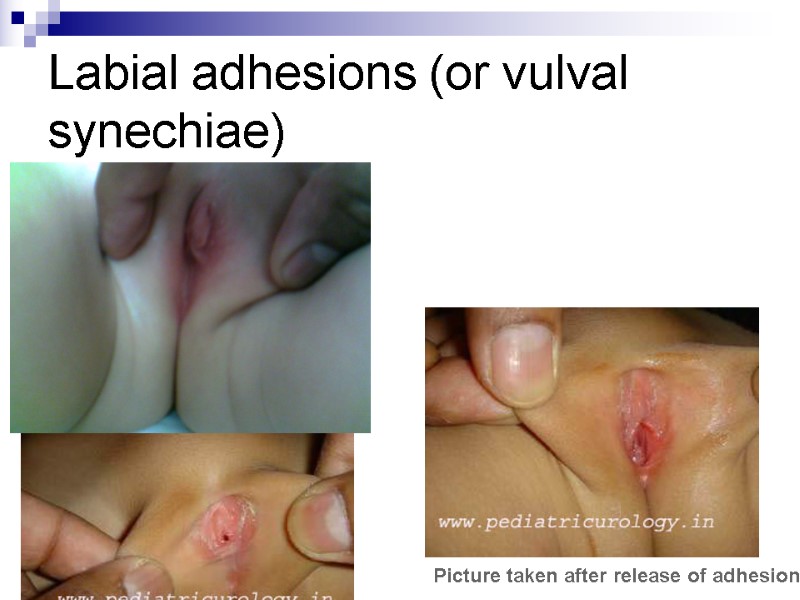 Labial adhesions (or vulval synechiae) Picture taken after release of adhesions
Labial adhesions (or vulval synechiae) Picture taken after release of adhesions
 UTI. Laboratory tests Urine analysis (UA) Nechiporenko test Urine culture CBC
UTI. Laboratory tests Urine analysis (UA) Nechiporenko test Urine culture CBC
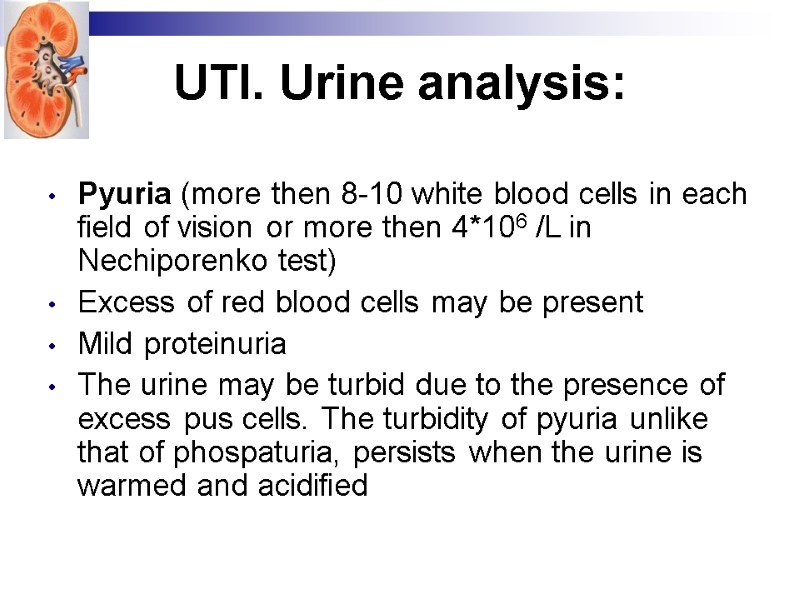 UTI. Urine analysis: Pyuria (more then 8-10 white blood cells in each field of vision or more then 4*106 /L in Nechiporenko test) Excess of red blood cells may be present Mild proteinuria The urine may be turbid due to the presence of excess pus cells. The turbidity of pyuria unlike that of phospaturia, persists when the urine is warmed and acidified
UTI. Urine analysis: Pyuria (more then 8-10 white blood cells in each field of vision or more then 4*106 /L in Nechiporenko test) Excess of red blood cells may be present Mild proteinuria The urine may be turbid due to the presence of excess pus cells. The turbidity of pyuria unlike that of phospaturia, persists when the urine is warmed and acidified
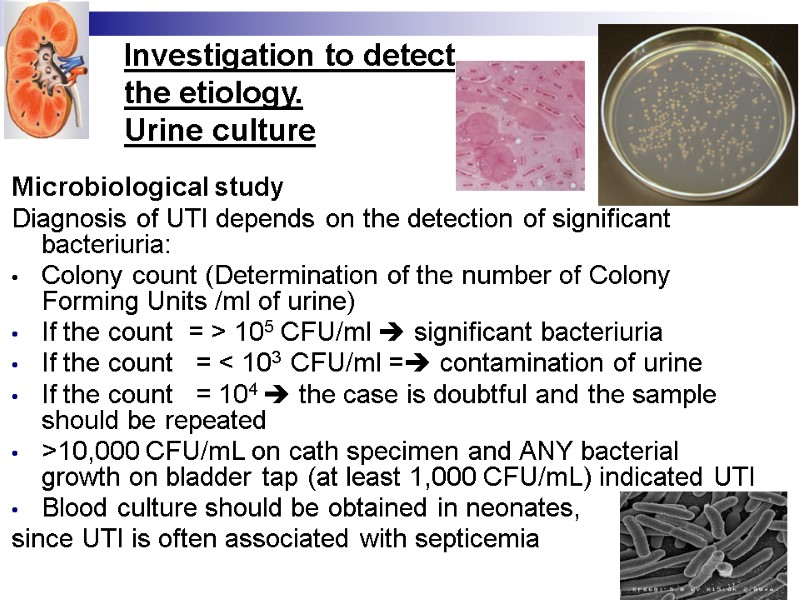
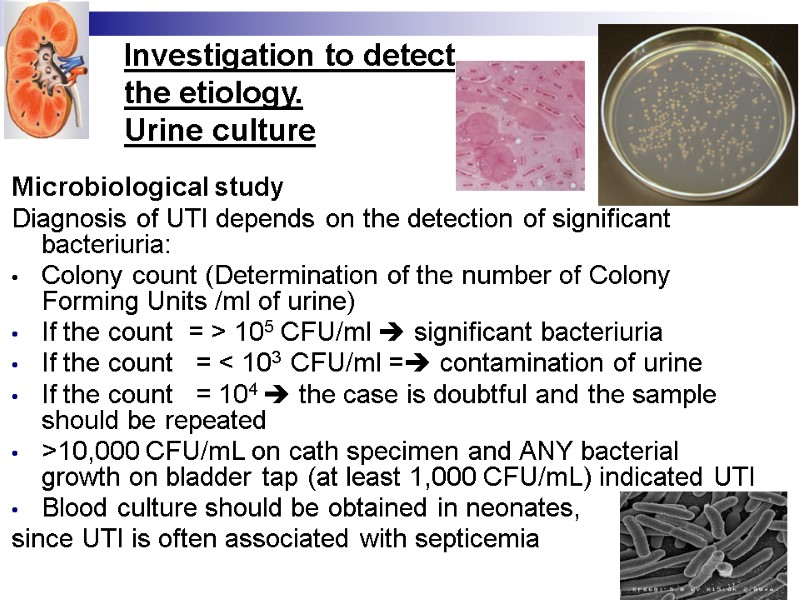 Investigation to detect the etiology. Urine culture Microbiological study Diagnosis of UTI depends on the detection of significant bacteriuria: Colony count (Determination of the number of Colony Forming Units /ml of urine) If the count = > 105 CFU/ml significant bacteriuria If the count = < 103 CFU/ml = contamination of urine If the count = 104 the case is doubtful and the sample should be repeated >10,000 CFU/mL on cath specimen and ANY bacterial growth on bladder tap (at least 1,000 CFU/mL) indicated UTI Blood culture should be obtained in neonates, since UTI is often associated with septicemia
Investigation to detect the etiology. Urine culture Microbiological study Diagnosis of UTI depends on the detection of significant bacteriuria: Colony count (Determination of the number of Colony Forming Units /ml of urine) If the count = > 105 CFU/ml significant bacteriuria If the count = < 103 CFU/ml = contamination of urine If the count = 104 the case is doubtful and the sample should be repeated >10,000 CFU/mL on cath specimen and ANY bacterial growth on bladder tap (at least 1,000 CFU/mL) indicated UTI Blood culture should be obtained in neonates, since UTI is often associated with septicemia
 Rapid screening test for UTI Dipstick nitrate test (Urinary nitrates +Bacteria = nitrites >> positive test = bacteriuria) Dipstick leukocyte esterase test (positive test = excess WBC in urine) These tests have false positive and false negative results. They must be confirmed by urine culture
Rapid screening test for UTI Dipstick nitrate test (Urinary nitrates +Bacteria = nitrites >> positive test = bacteriuria) Dipstick leukocyte esterase test (positive test = excess WBC in urine) These tests have false positive and false negative results. They must be confirmed by urine culture
 Diagnosis of the Urinary Tract Infections Investigations to prove UTI Collection of urine sample Collection of the urine sample for analysis should follow the following precautions: Proper disinfection of genitalia with soap and water, antiseptic solution, sterile water or saline; The first morning sample of urine is preferred. The urine is collected in a clean sterile container and cultured within ½ an hour or kept refrigerated at 4 C not more than 24h.
Diagnosis of the Urinary Tract Infections Investigations to prove UTI Collection of urine sample Collection of the urine sample for analysis should follow the following precautions: Proper disinfection of genitalia with soap and water, antiseptic solution, sterile water or saline; The first morning sample of urine is preferred. The urine is collected in a clean sterile container and cultured within ½ an hour or kept refrigerated at 4 C not more than 24h.
 Methods of urine collection: Midstream clean catch sample in toilet trained children In infants: a sterile urine collection bag may be attached to perineum around penis or vulva. Urinary bladder catheterization Suprapubic bladder aspiration in neonates and young infants.
Methods of urine collection: Midstream clean catch sample in toilet trained children In infants: a sterile urine collection bag may be attached to perineum around penis or vulva. Urinary bladder catheterization Suprapubic bladder aspiration in neonates and young infants.
 Determination of inflammatory markers Blood test - elevation of WBC, ESR C-reacrive protein level Serum procalcitonin Serum and urinary interleukin 6, 8 (infants and children)
Determination of inflammatory markers Blood test - elevation of WBC, ESR C-reacrive protein level Serum procalcitonin Serum and urinary interleukin 6, 8 (infants and children)
 Renal function testing Evaluation of renal function by Blood urea nitrogen (BUN) Serum creatinine, GFR, Zimnitskiy test
Renal function testing Evaluation of renal function by Blood urea nitrogen (BUN) Serum creatinine, GFR, Zimnitskiy test
 Imaging of the urinary tract
Imaging of the urinary tract
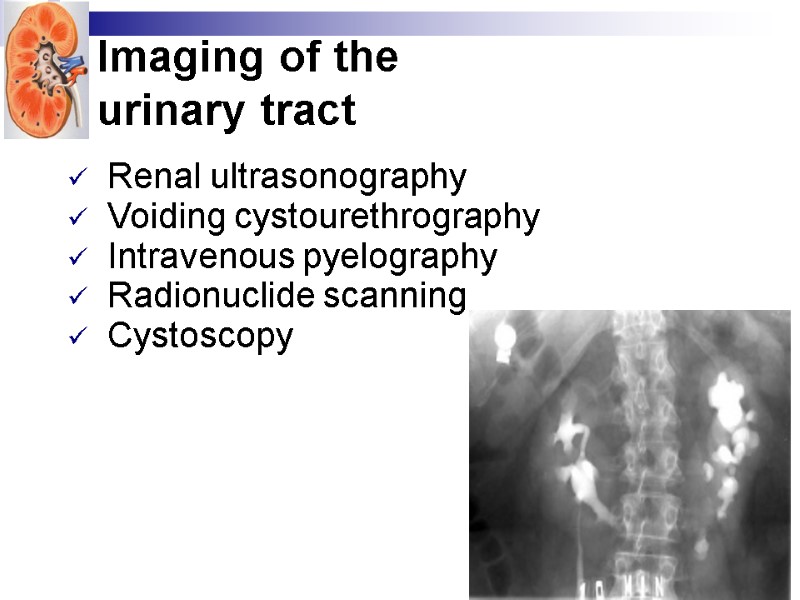
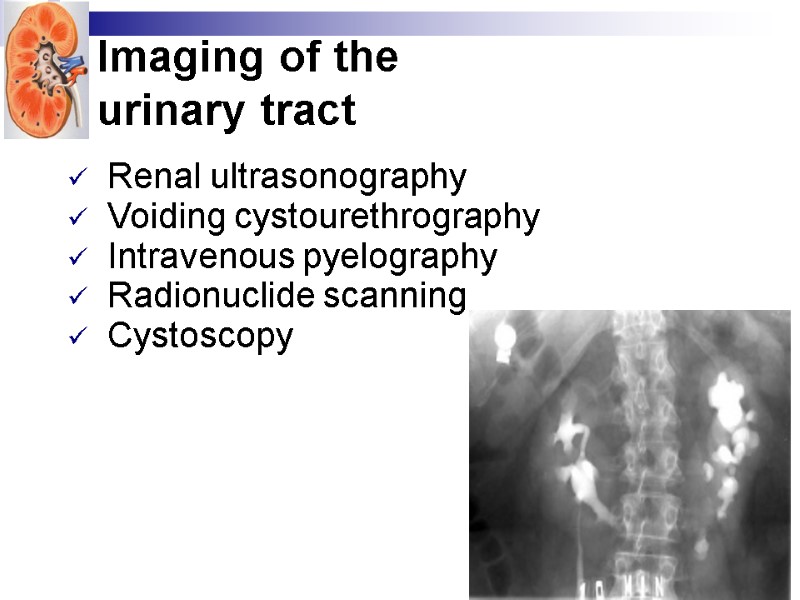 Imaging of the urinary tract Renal ultrasonography Voiding cystourethrography Intravenous pyelography Radionuclide scanning Cystoscopy
Imaging of the urinary tract Renal ultrasonography Voiding cystourethrography Intravenous pyelography Radionuclide scanning Cystoscopy
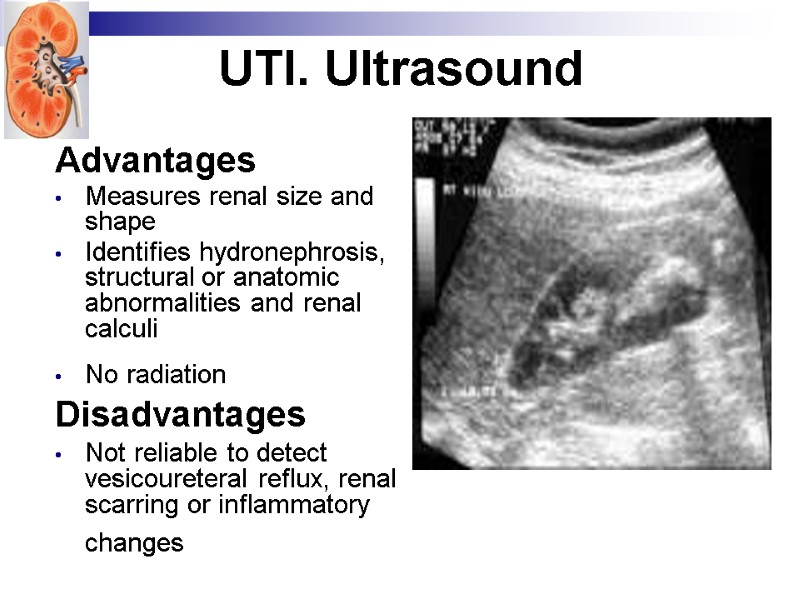
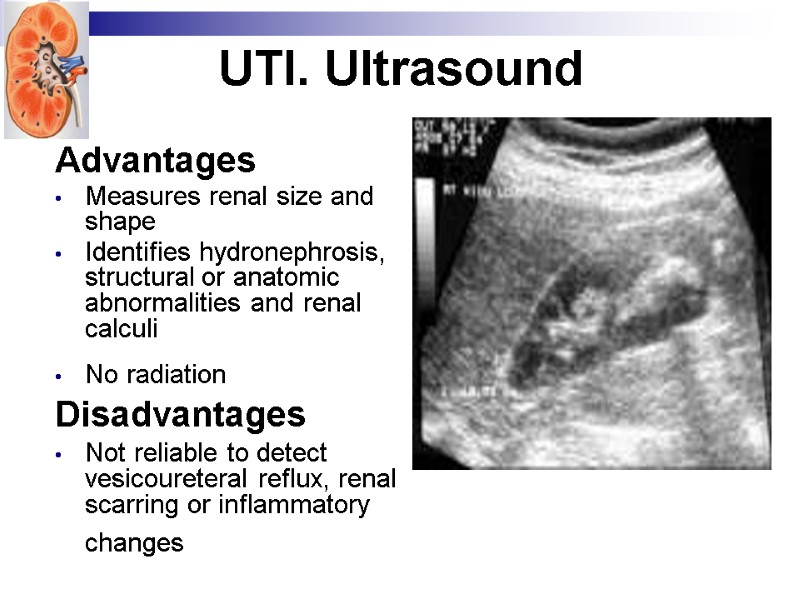 UTI. Ultrasound Advantages Measures renal size and shape Identifies hydronephrosis, structural or anatomic abnormalities and renal calculi No radiation Disadvantages Not reliable to detect vesicoureteral reflux, renal scarring or inflammatory changes
UTI. Ultrasound Advantages Measures renal size and shape Identifies hydronephrosis, structural or anatomic abnormalities and renal calculi No radiation Disadvantages Not reliable to detect vesicoureteral reflux, renal scarring or inflammatory changes
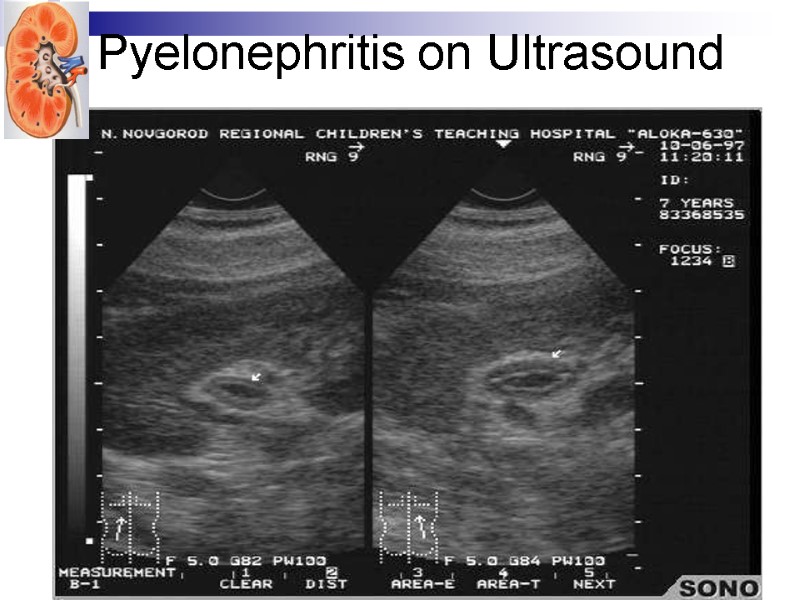
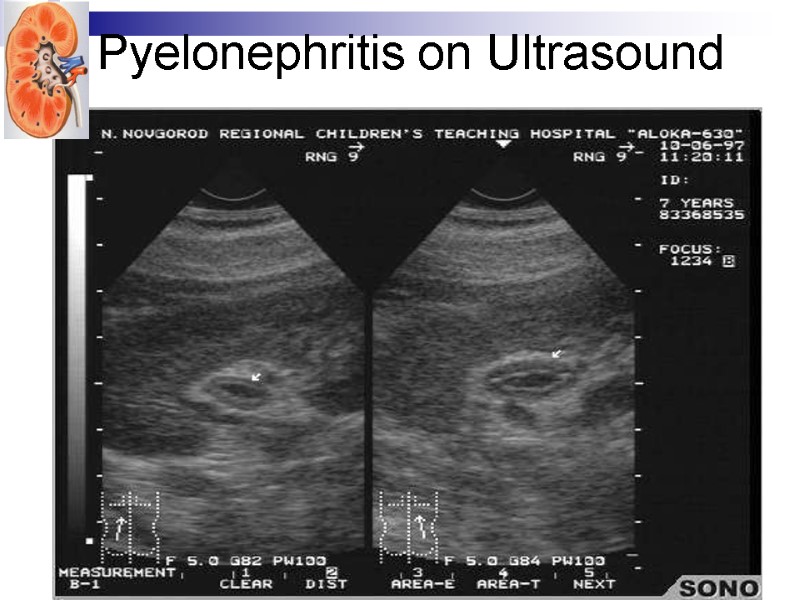 Pyelonephritis on Ultrasound
Pyelonephritis on Ultrasound
 Imaging of the urinary tract Indications for intravenous urography (pyelography) and voiding cystourethrography In males – in the first symptomatic UTI In female - < 6 y in first attack; > 6 y if recurrent upper UTI Family history of VUR Abnormal voiding pattern Poor growth or hypertension
Imaging of the urinary tract Indications for intravenous urography (pyelography) and voiding cystourethrography In males – in the first symptomatic UTI In female - < 6 y in first attack; > 6 y if recurrent upper UTI Family history of VUR Abnormal voiding pattern Poor growth or hypertension
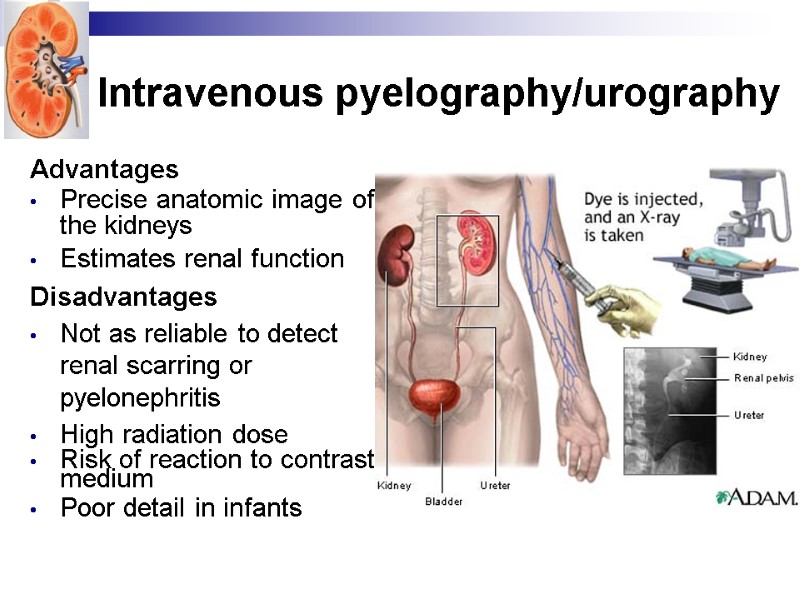
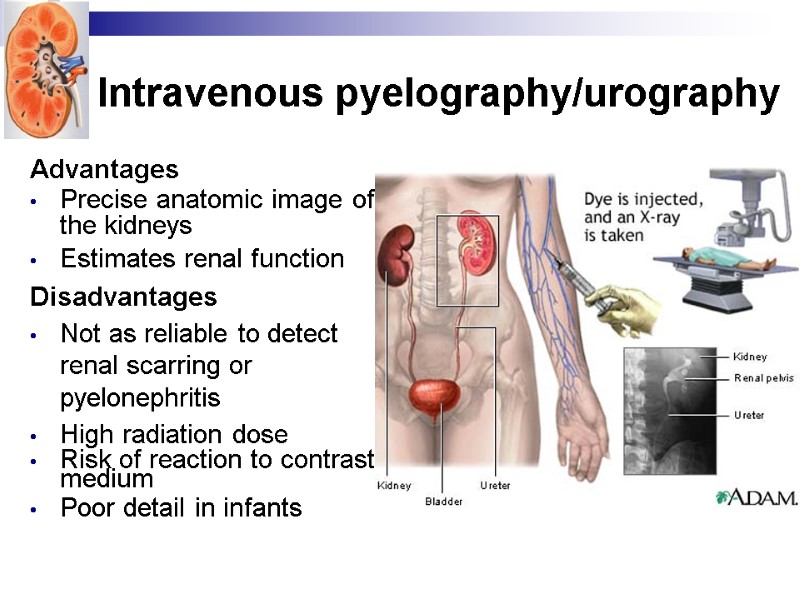 Intravenous pyelography/urography Advantages Precise anatomic image of the kidneys Estimates renal function Disadvantages Not as reliable to detect renal scarring or pyelonephritis High radiation dose Risk of reaction to contrast medium Poor detail in infants
Intravenous pyelography/urography Advantages Precise anatomic image of the kidneys Estimates renal function Disadvantages Not as reliable to detect renal scarring or pyelonephritis High radiation dose Risk of reaction to contrast medium Poor detail in infants
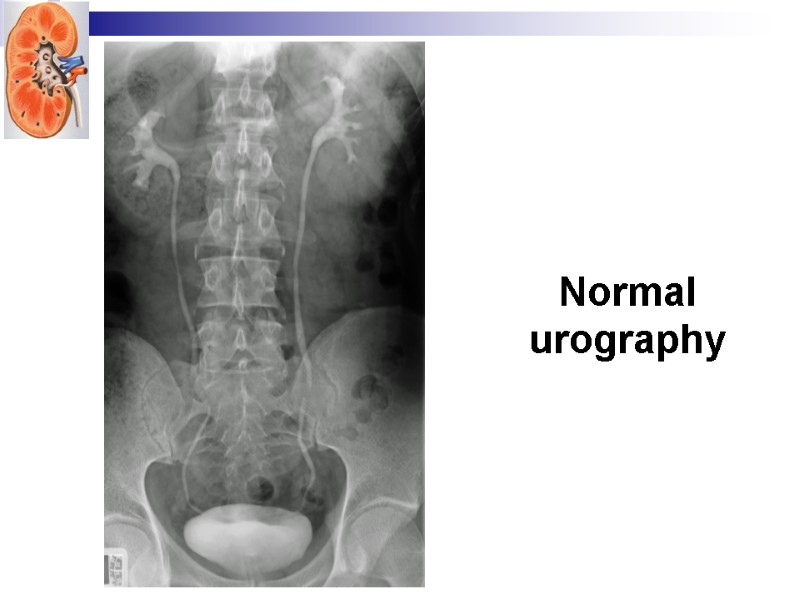
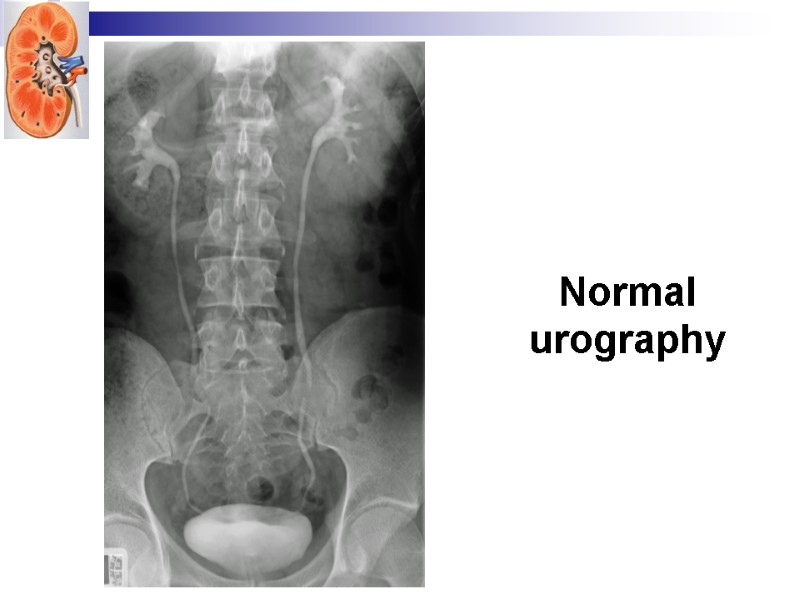 Normal urography
Normal urography
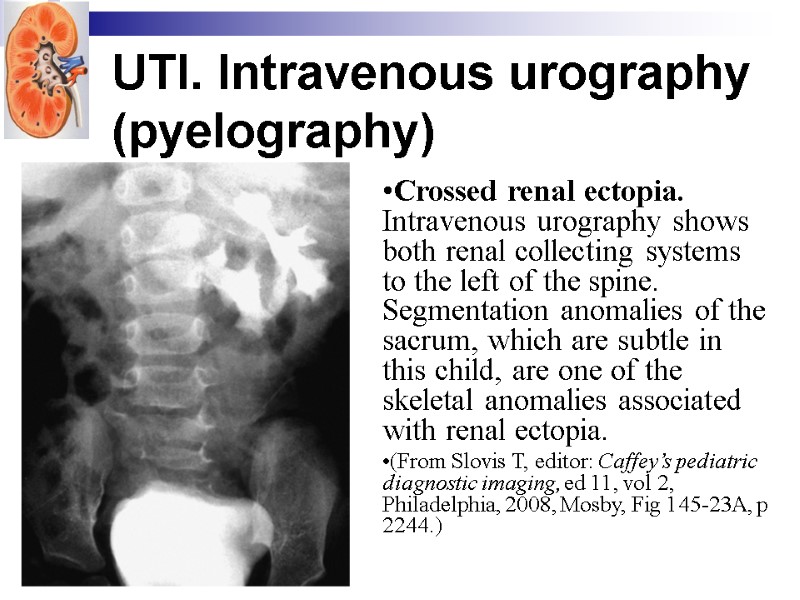
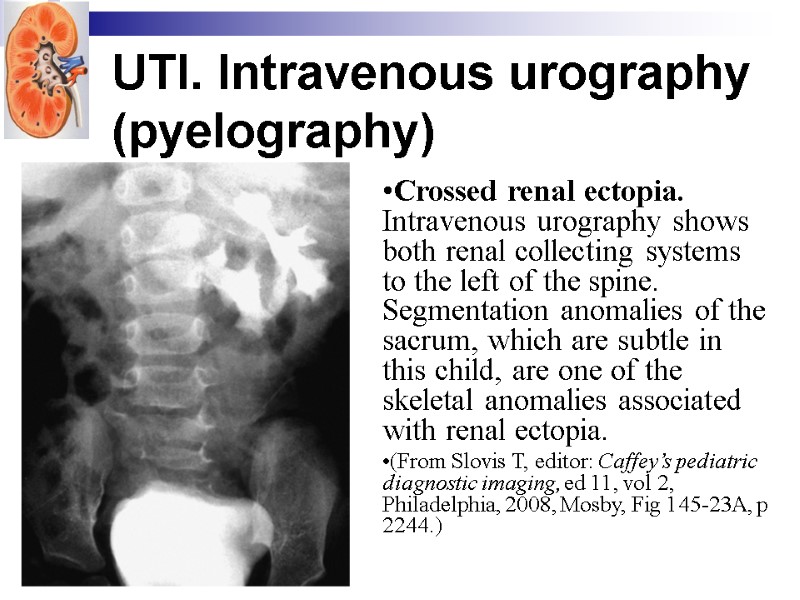 UTI. Intravenous urography (pyelography) Crossed renal ectopia. Intravenous urography shows both renal collecting systems to the left of the spine. Segmentation anomalies of the sacrum, which are subtle in this child, are one of the skeletal anomalies associated with renal ectopia. (From Slovis T, editor: Caffey’s pediatric diagnostic imaging, ed 11, vol 2, Philadelphia, 2008, Mosby, Fig 145-23A, p 2244.)
UTI. Intravenous urography (pyelography) Crossed renal ectopia. Intravenous urography shows both renal collecting systems to the left of the spine. Segmentation anomalies of the sacrum, which are subtle in this child, are one of the skeletal anomalies associated with renal ectopia. (From Slovis T, editor: Caffey’s pediatric diagnostic imaging, ed 11, vol 2, Philadelphia, 2008, Mosby, Fig 145-23A, p 2244.)
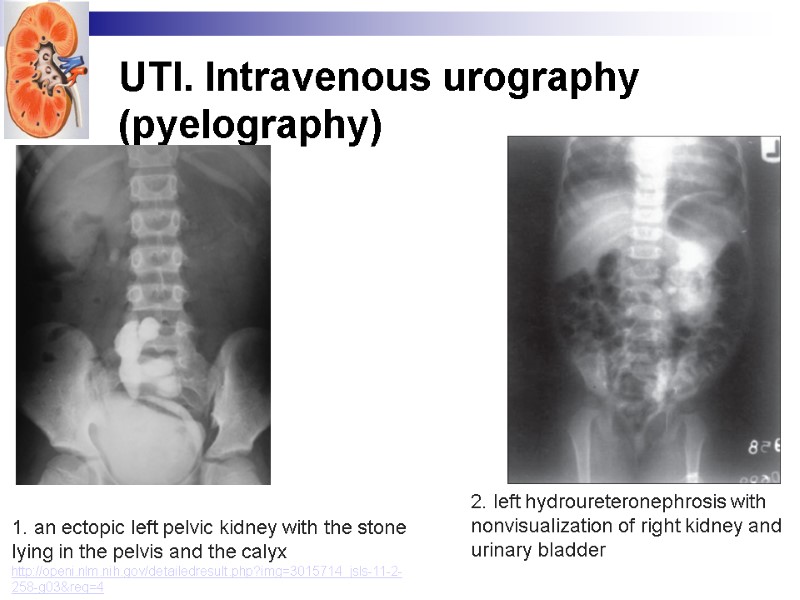
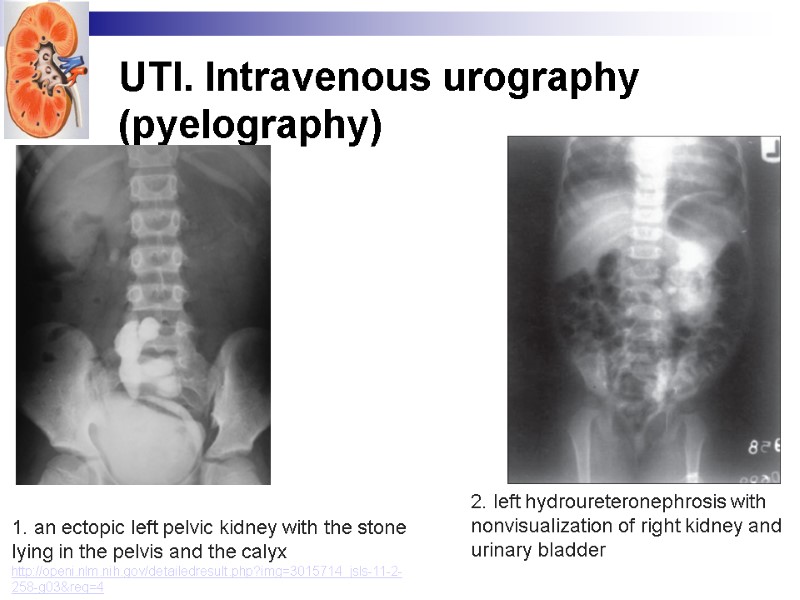 UTI. Intravenous urography (pyelography) 1. an ectopic left pelvic kidney with the stone lying in the pelvis and the calyx http://openi.nlm.nih.gov/detailedresult.php?img=3015714_jsls-11-2-258-g03&req=4 2. left hydroureteronephrosis with nonvisualization of right kidney and urinary bladder
UTI. Intravenous urography (pyelography) 1. an ectopic left pelvic kidney with the stone lying in the pelvis and the calyx http://openi.nlm.nih.gov/detailedresult.php?img=3015714_jsls-11-2-258-g03&req=4 2. left hydroureteronephrosis with nonvisualization of right kidney and urinary bladder
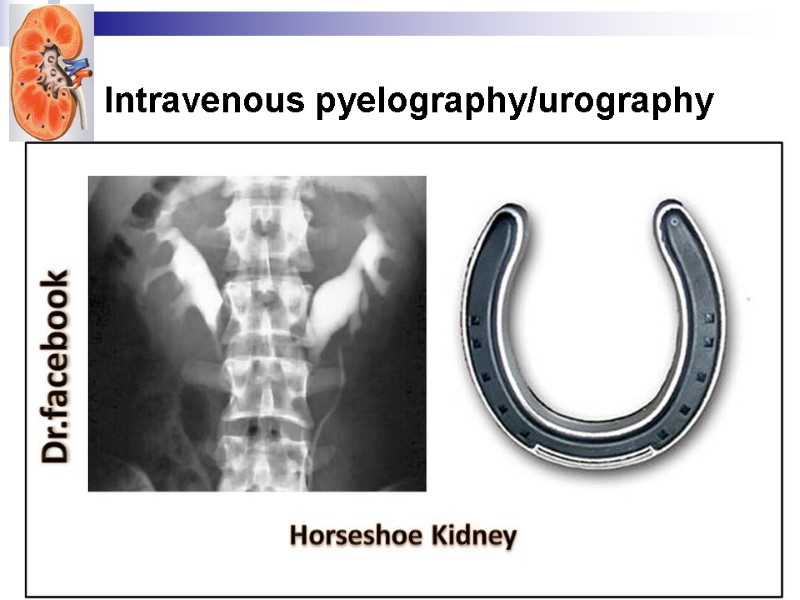
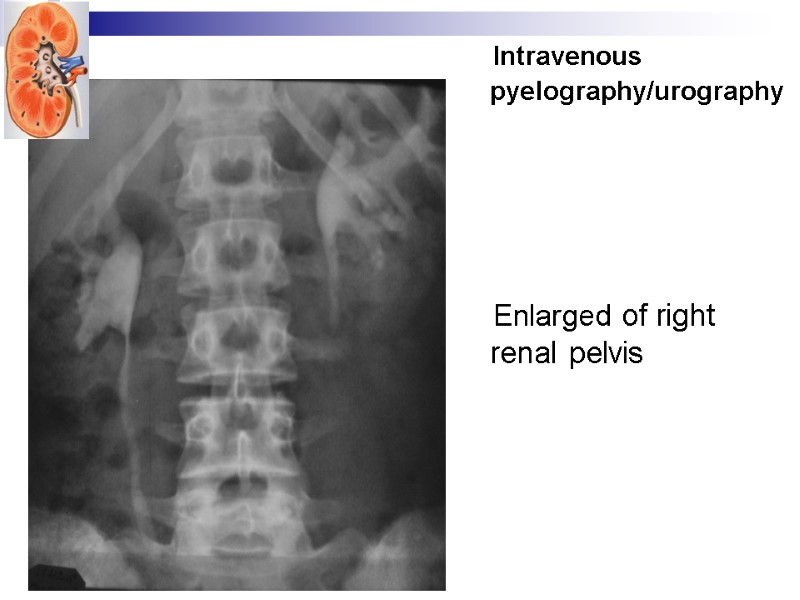
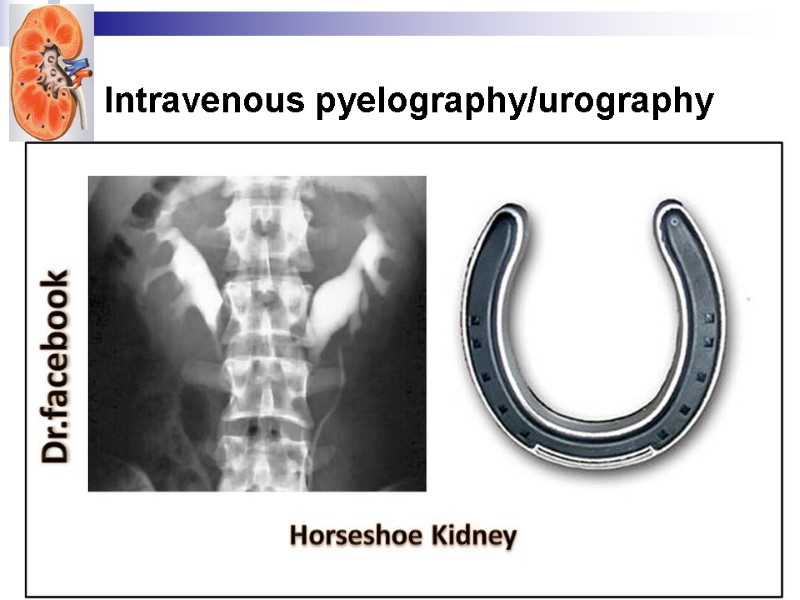 Intravenous pyelography/urography
Intravenous pyelography/urography
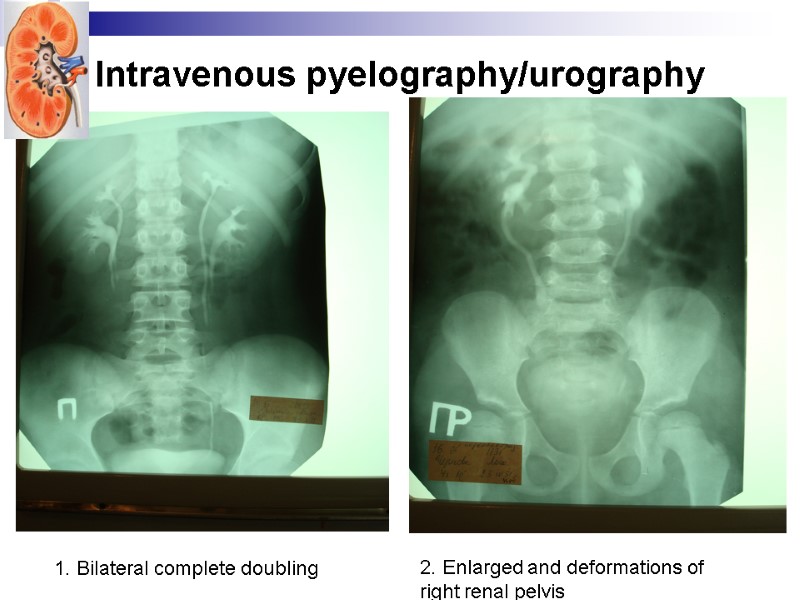
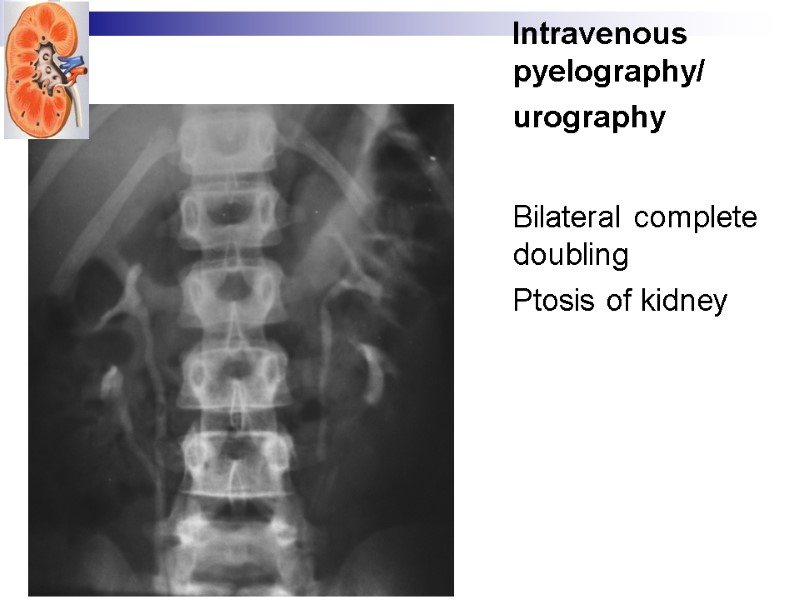
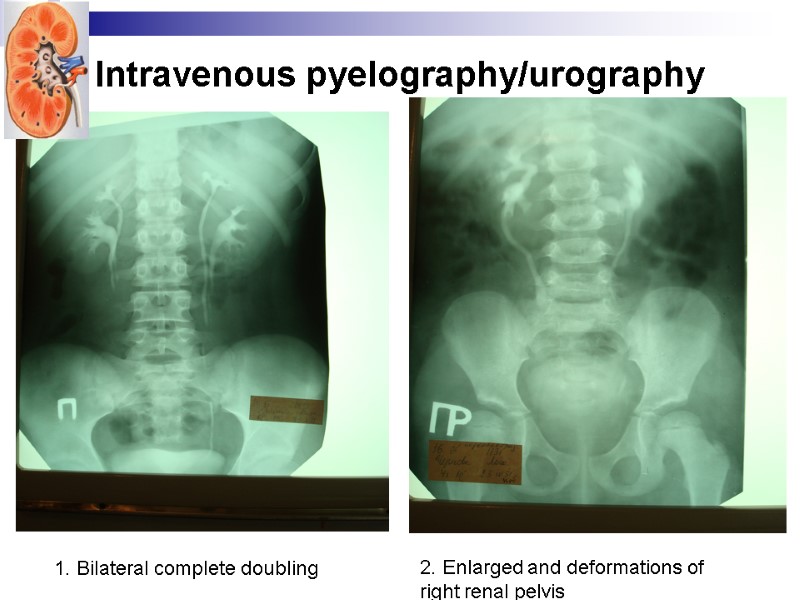 Intravenous pyelography/urography 1. Bilateral complete doubling 2. Enlarged and deformations of right renal pelvis
Intravenous pyelography/urography 1. Bilateral complete doubling 2. Enlarged and deformations of right renal pelvis
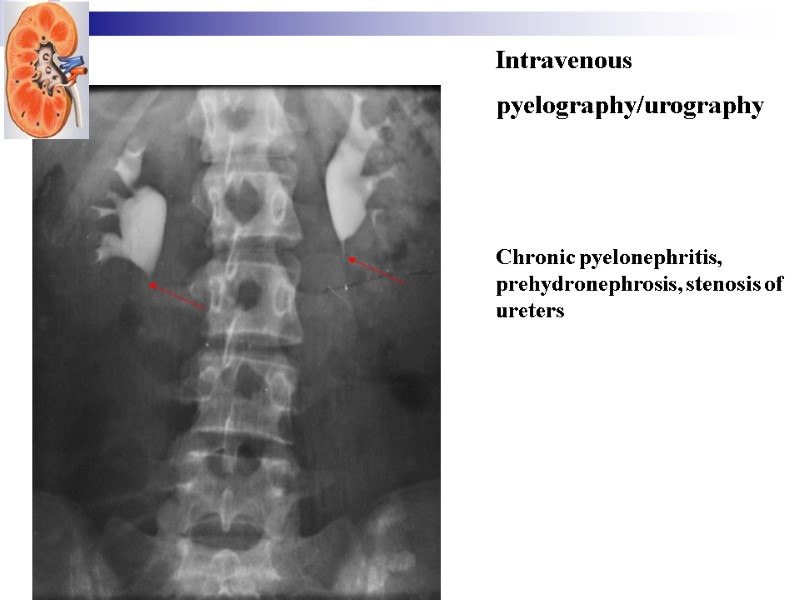
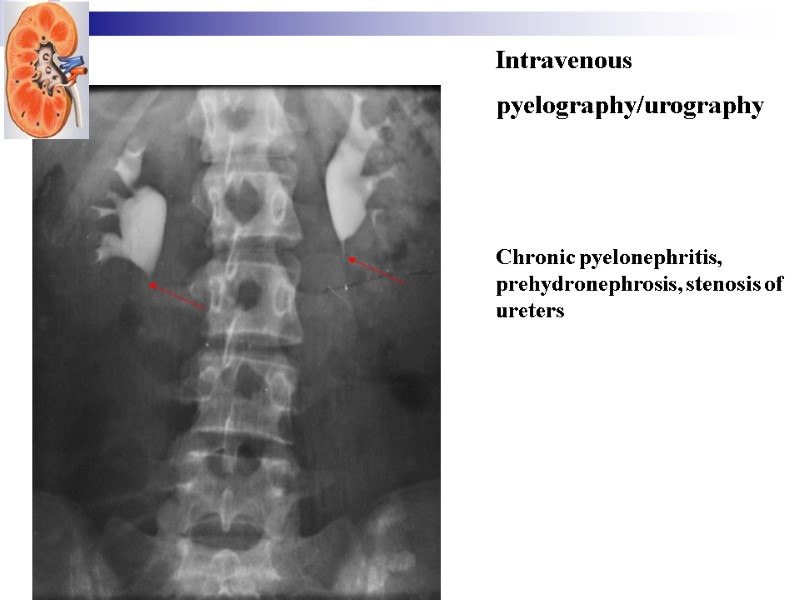 Intravenous pyelography/urography Chronic pyelonephritis, prehydronephrosis, stenosis of ureters
Intravenous pyelography/urography Chronic pyelonephritis, prehydronephrosis, stenosis of ureters
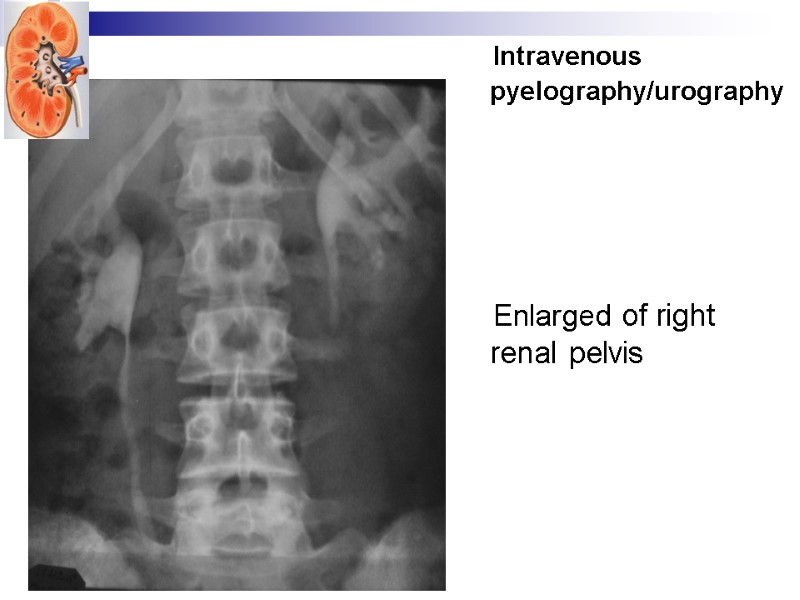 Intravenous pyelography/urography Enlarged of right renal pelvis
Intravenous pyelography/urography Enlarged of right renal pelvis
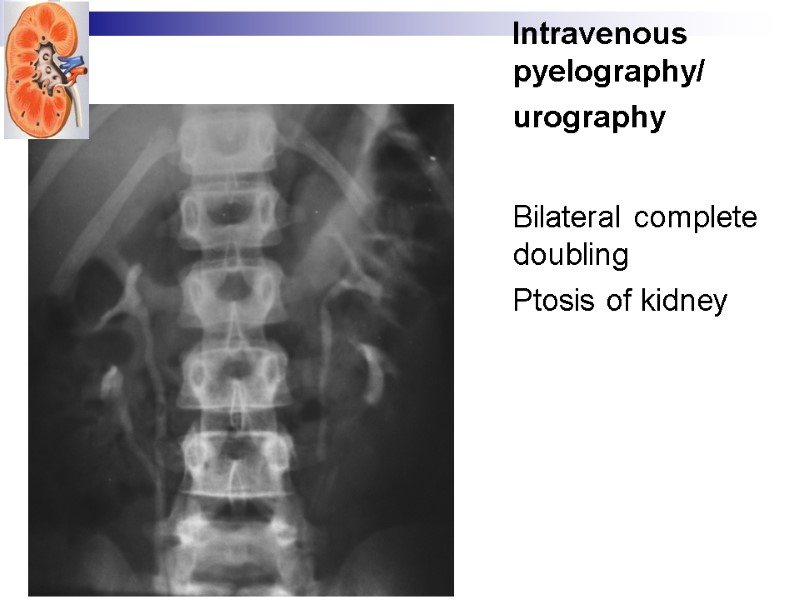 Intravenous pyelography/ urography Bilateral complete doubling Ptosis of kidney
Intravenous pyelography/ urography Bilateral complete doubling Ptosis of kidney
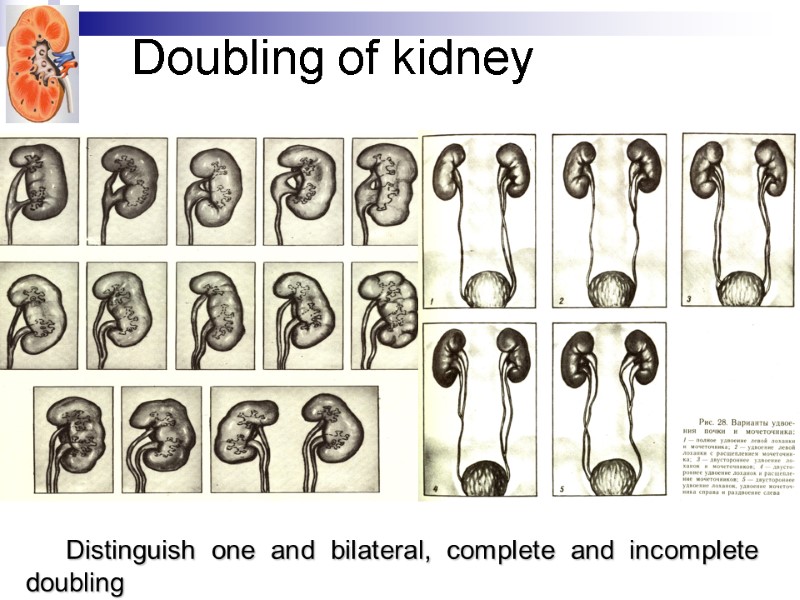
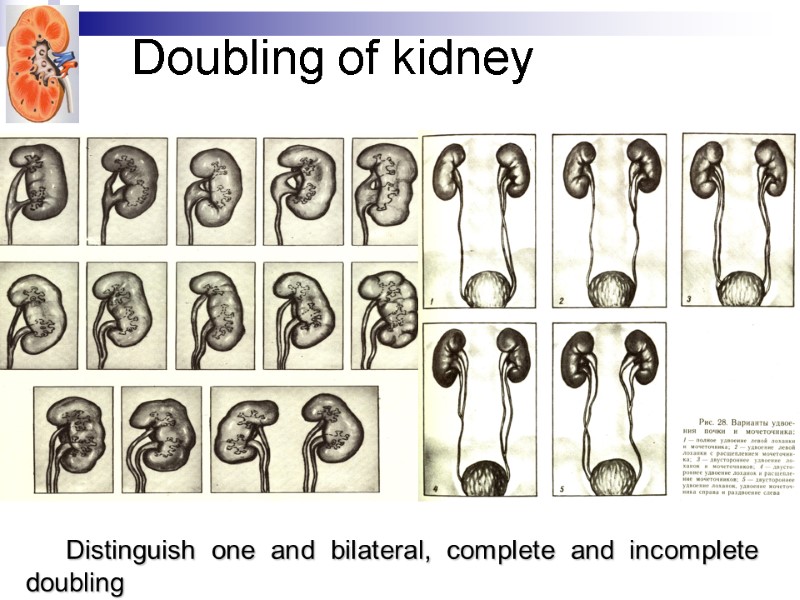 Doubling of kidney Distinguish one and bilateral, complete and incomplete doubling
Doubling of kidney Distinguish one and bilateral, complete and incomplete doubling
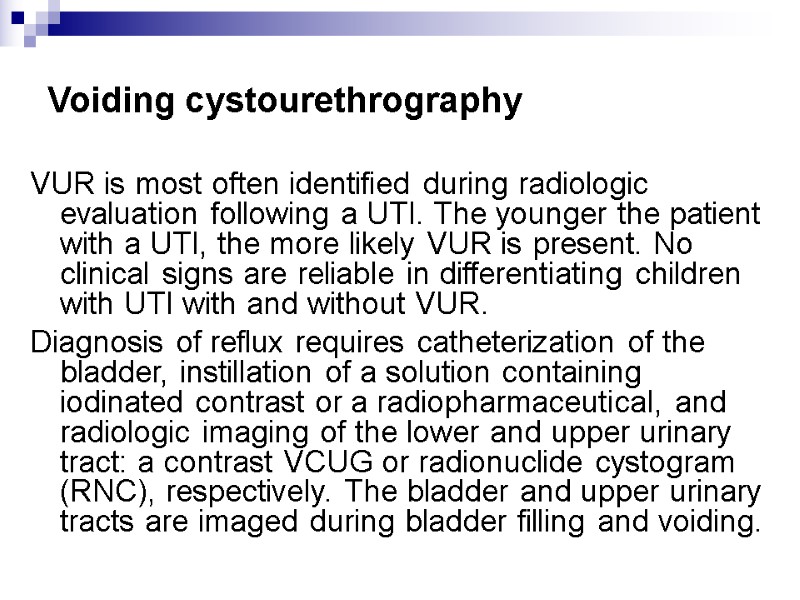
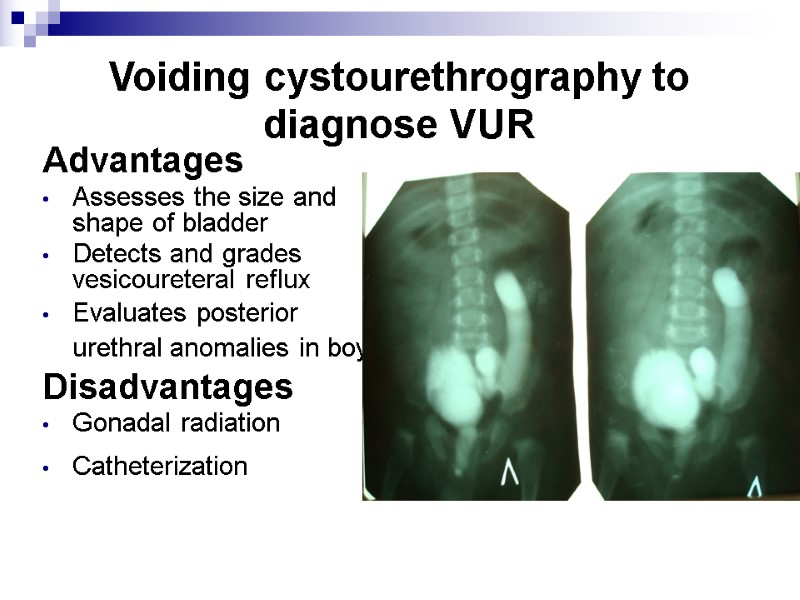
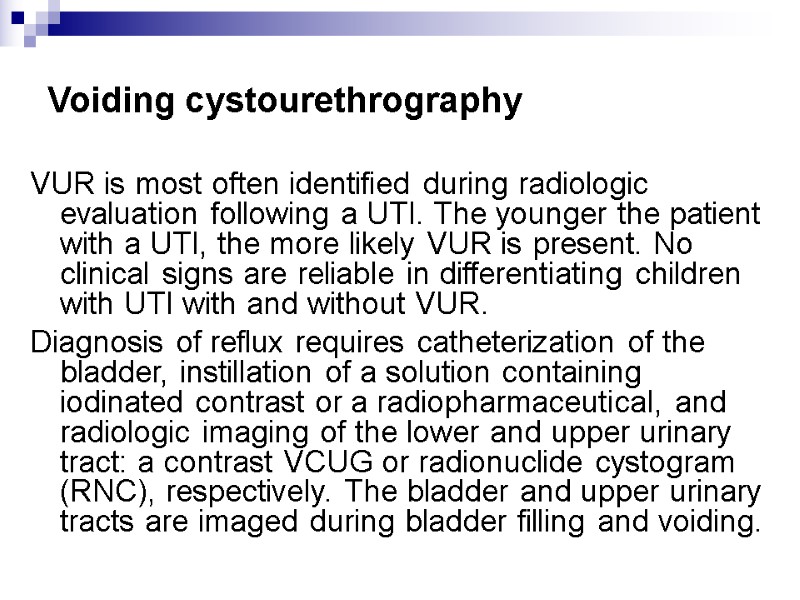 Voiding cystourethrography VUR is most often identified during radiologic evaluation following a UTI. The younger the patient with a UTI, the more likely VUR is present. No clinical signs are reliable in differentiating children with UTI with and without VUR. Diagnosis of reflux requires catheterization of the bladder, instillation of a solution containing iodinated contrast or a radiopharmaceutical, and radiologic imaging of the lower and upper urinary tract: a contrast VCUG or radionuclide cystogram (RNC), respectively. The bladder and upper urinary tracts are imaged during bladder filling and voiding.
Voiding cystourethrography VUR is most often identified during radiologic evaluation following a UTI. The younger the patient with a UTI, the more likely VUR is present. No clinical signs are reliable in differentiating children with UTI with and without VUR. Diagnosis of reflux requires catheterization of the bladder, instillation of a solution containing iodinated contrast or a radiopharmaceutical, and radiologic imaging of the lower and upper urinary tract: a contrast VCUG or radionuclide cystogram (RNC), respectively. The bladder and upper urinary tracts are imaged during bladder filling and voiding.
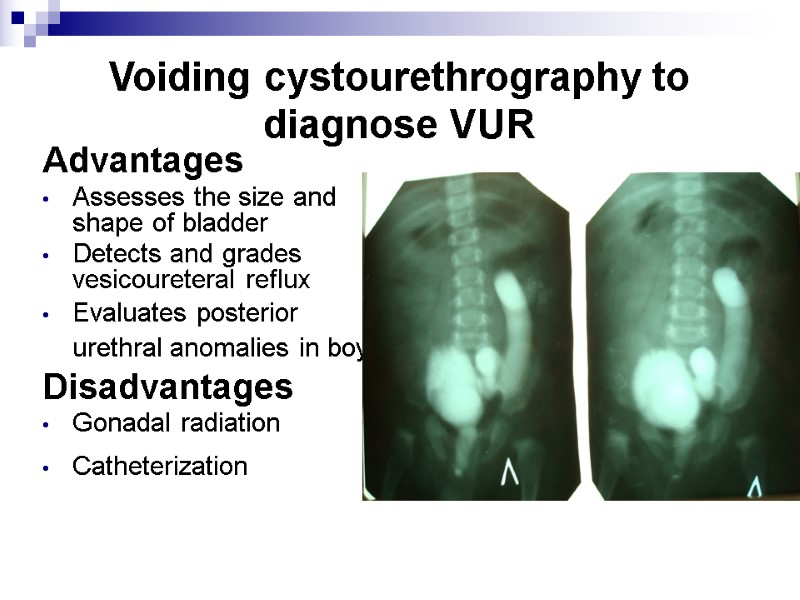 Voiding cystourethrography to diagnose VUR Advantages Assesses the size and shape of bladder Detects and grades vesicoureteral reflux Evaluates posterior urethral anomalies in boys Disadvantages Gonadal radiation Catheterization
Voiding cystourethrography to diagnose VUR Advantages Assesses the size and shape of bladder Detects and grades vesicoureteral reflux Evaluates posterior urethral anomalies in boys Disadvantages Gonadal radiation Catheterization
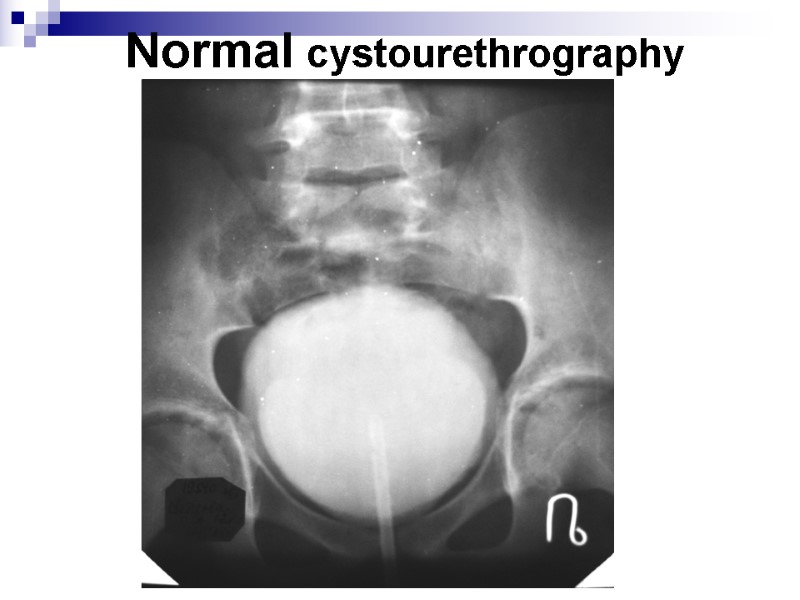
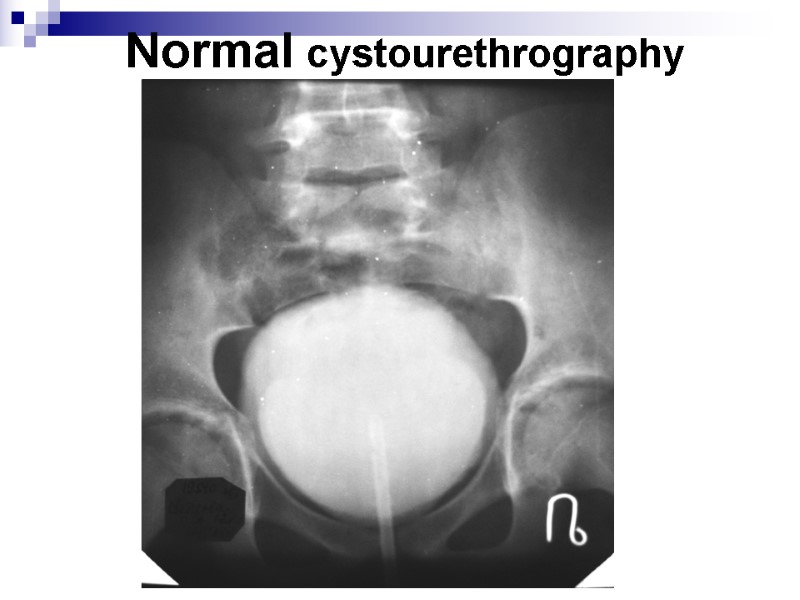 Normal cystourethrography
Normal cystourethrography
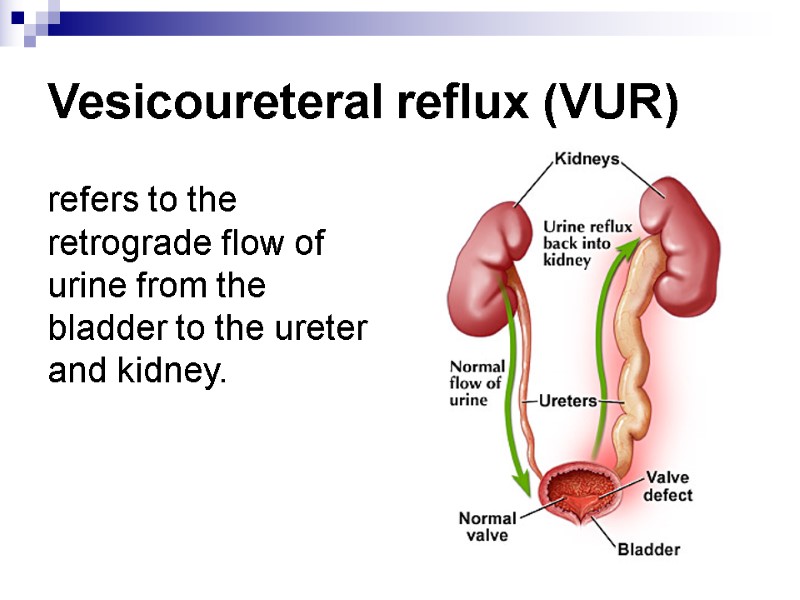
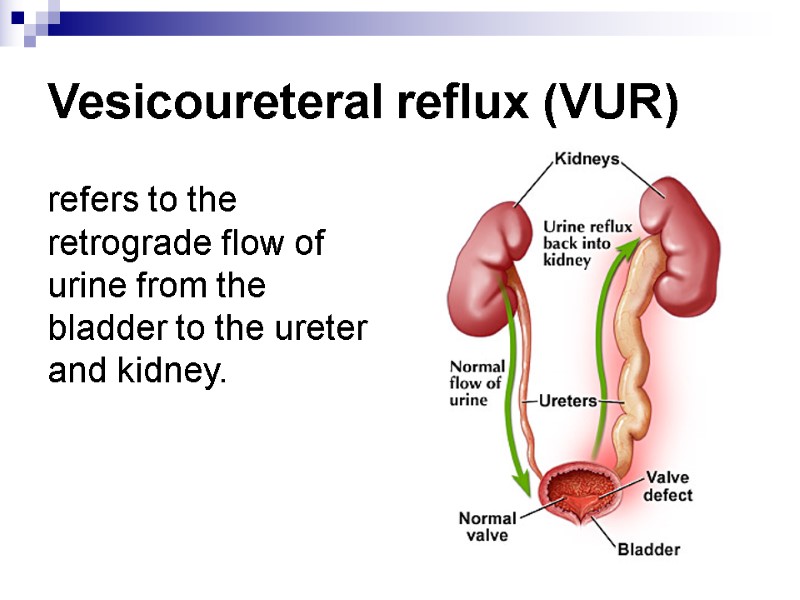 Vesicoureteral reflux (VUR) refers to the retrograde flow of urine from the bladder to the ureter and kidney.
Vesicoureteral reflux (VUR) refers to the retrograde flow of urine from the bladder to the ureter and kidney.
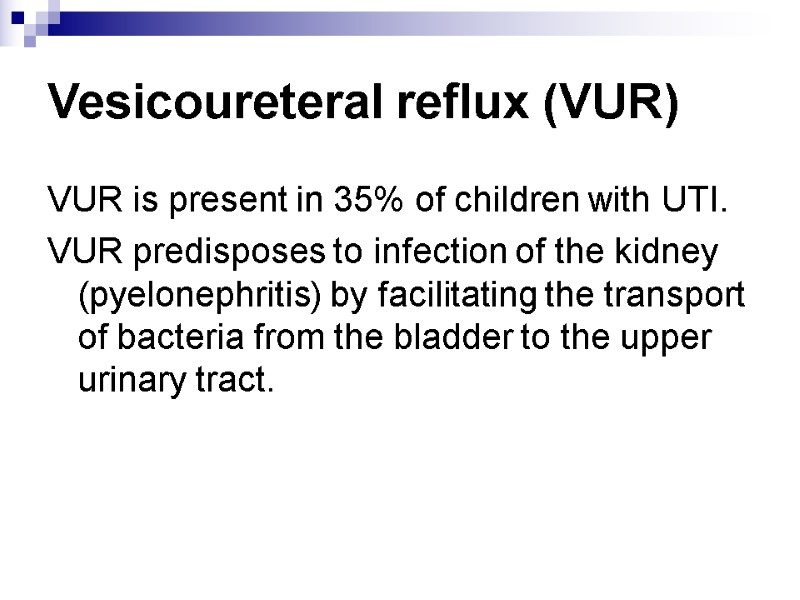
 Vesicoureteral reflux (VUR) VUR is present in 35% of children with UTI. VUR predisposes to infection of the kidney (pyelonephritis) by facilitating the transport of bacteria from the bladder to the upper urinary tract.
Vesicoureteral reflux (VUR) VUR is present in 35% of children with UTI. VUR predisposes to infection of the kidney (pyelonephritis) by facilitating the transport of bacteria from the bladder to the upper urinary tract.
 Vesicoureteric reflux (VUR) Reflux severity is graded using the International Reflux Study Classification of I to V and is based on the appearance of the urinary tract on a contrast voiding cystourethrogram (VCUG).
Vesicoureteric reflux (VUR) Reflux severity is graded using the International Reflux Study Classification of I to V and is based on the appearance of the urinary tract on a contrast voiding cystourethrogram (VCUG).
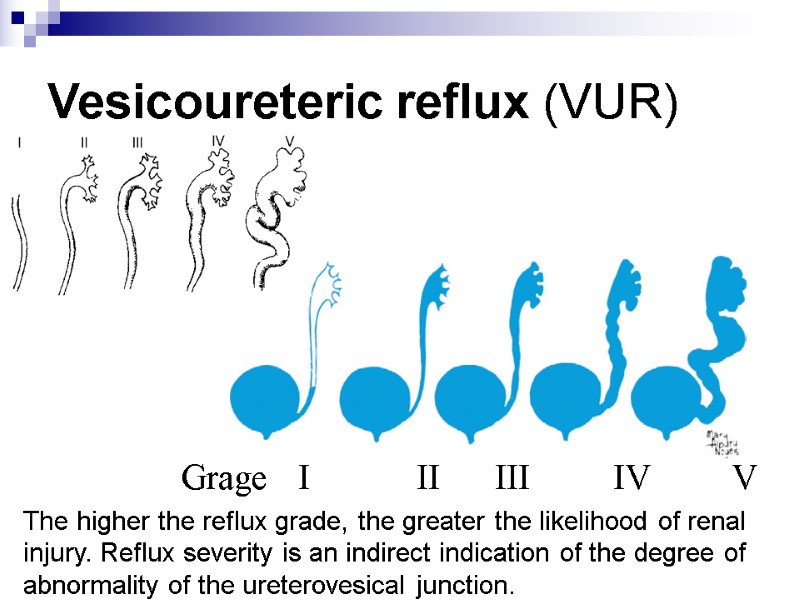
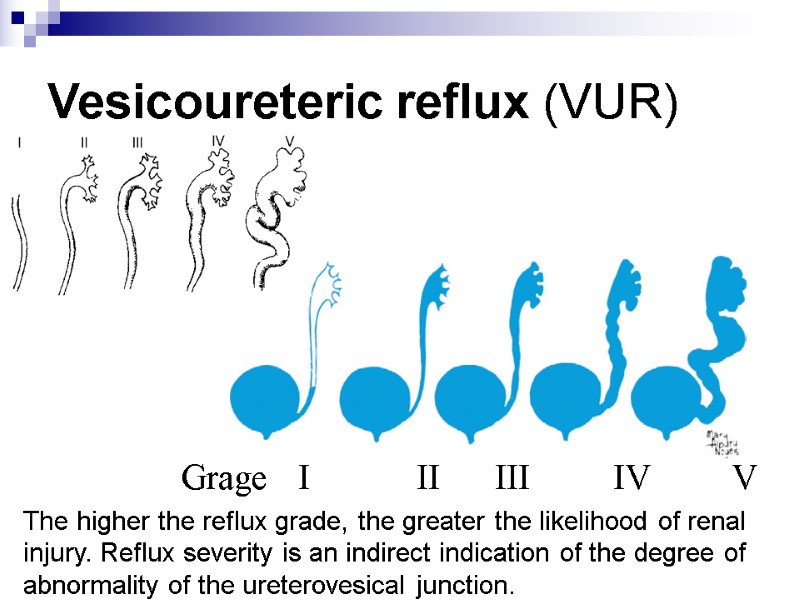 Vesicoureteric reflux (VUR) Grage I II III IV V The higher the reflux grade, the greater the likelihood of renal injury. Reflux severity is an indirect indication of the degree of abnormality of the ureterovesical junction. G
Vesicoureteric reflux (VUR) Grage I II III IV V The higher the reflux grade, the greater the likelihood of renal injury. Reflux severity is an indirect indication of the degree of abnormality of the ureterovesical junction. G
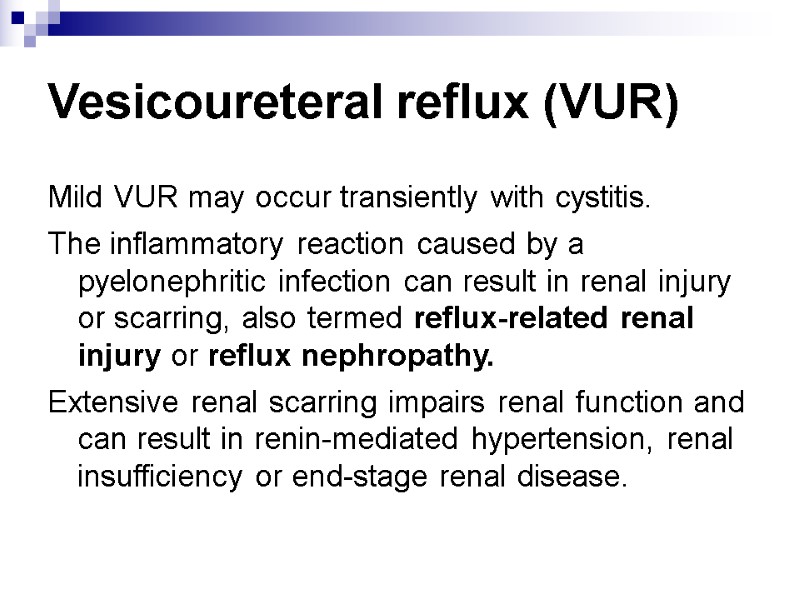 Vesicoureteral reflux (VUR) Mild VUR may occur transiently with cystitis. The inflammatory reaction caused by a pyelonephritic infection can result in renal injury or scarring, also termed reflux-related renal injury or reflux nephropathy. Extensive renal scarring impairs renal function and can result in renin-mediated hypertension, renal insufficiency or end-stage renal disease.
Vesicoureteral reflux (VUR) Mild VUR may occur transiently with cystitis. The inflammatory reaction caused by a pyelonephritic infection can result in renal injury or scarring, also termed reflux-related renal injury or reflux nephropathy. Extensive renal scarring impairs renal function and can result in renin-mediated hypertension, renal insufficiency or end-stage renal disease.
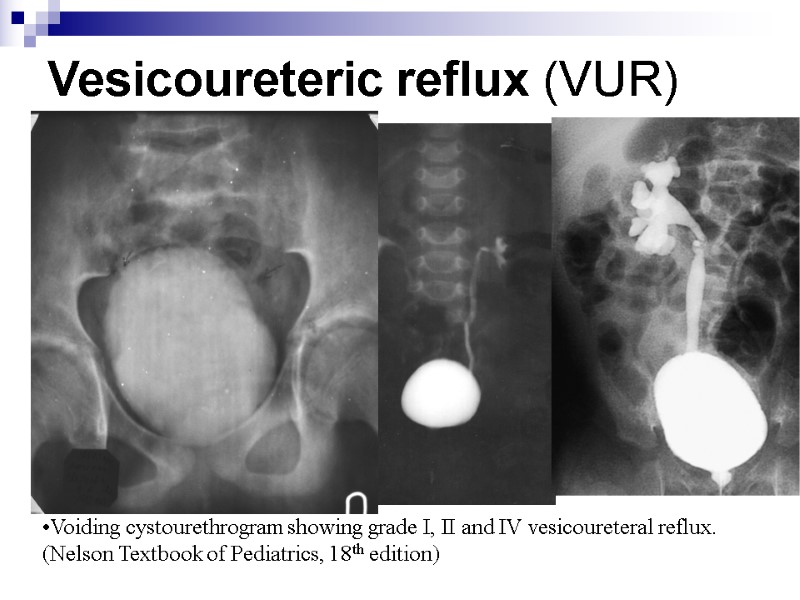
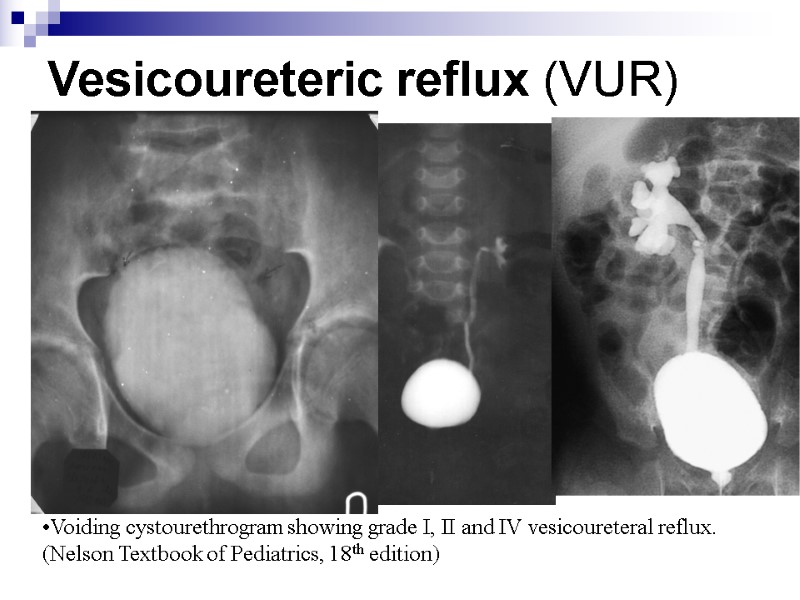 Vesicoureteric reflux (VUR) Voiding cystourethrogram showing grade I, II and IV vesicoureteral reflux. (Nelson Textbook of Pediatrics, 18th edition)
Vesicoureteric reflux (VUR) Voiding cystourethrogram showing grade I, II and IV vesicoureteral reflux. (Nelson Textbook of Pediatrics, 18th edition)
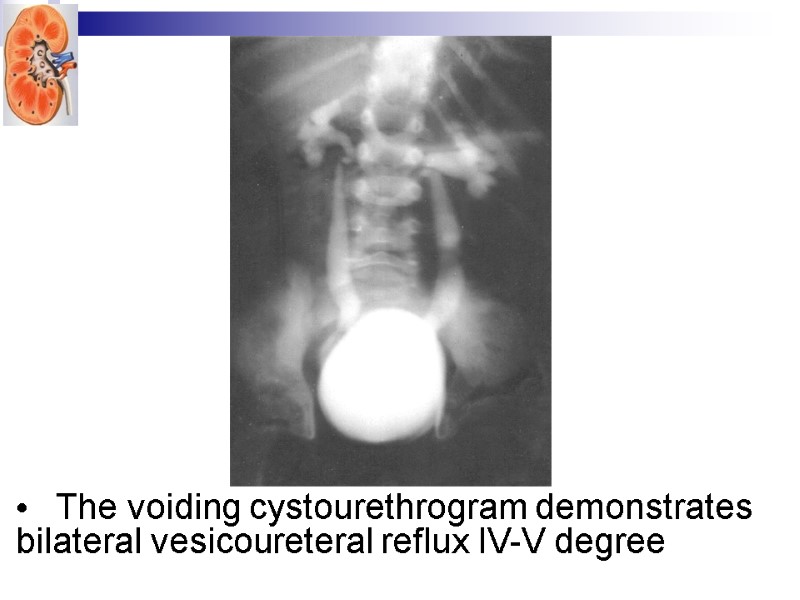
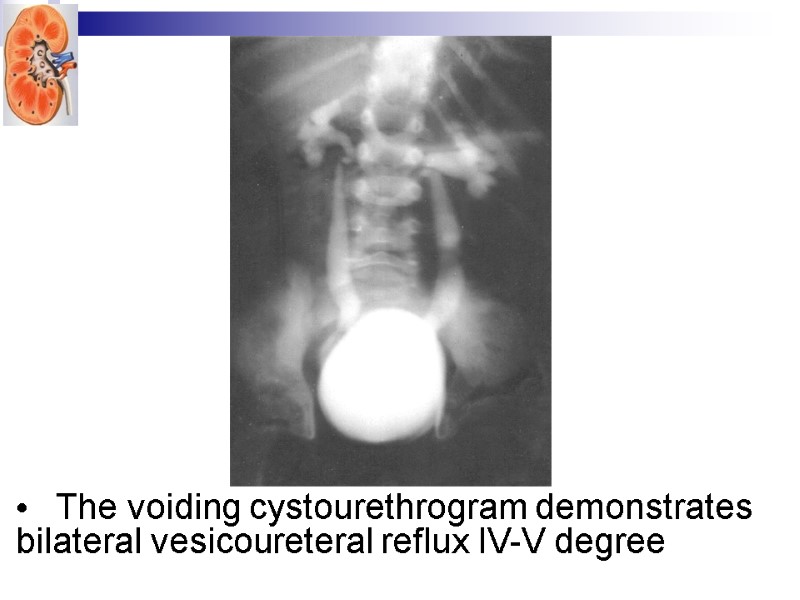 The voiding cystourethrogram demonstrates bilateral vesicoureteral reflux IV-V degree
The voiding cystourethrogram demonstrates bilateral vesicoureteral reflux IV-V degree
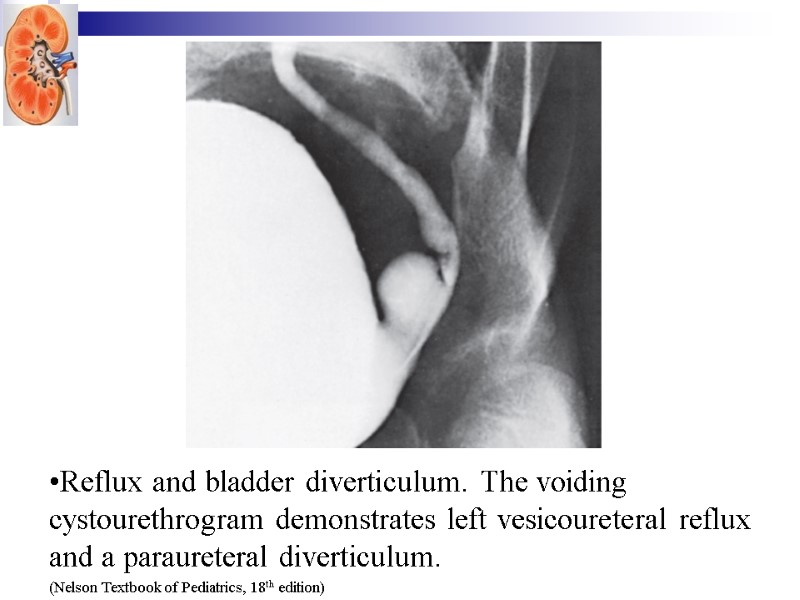
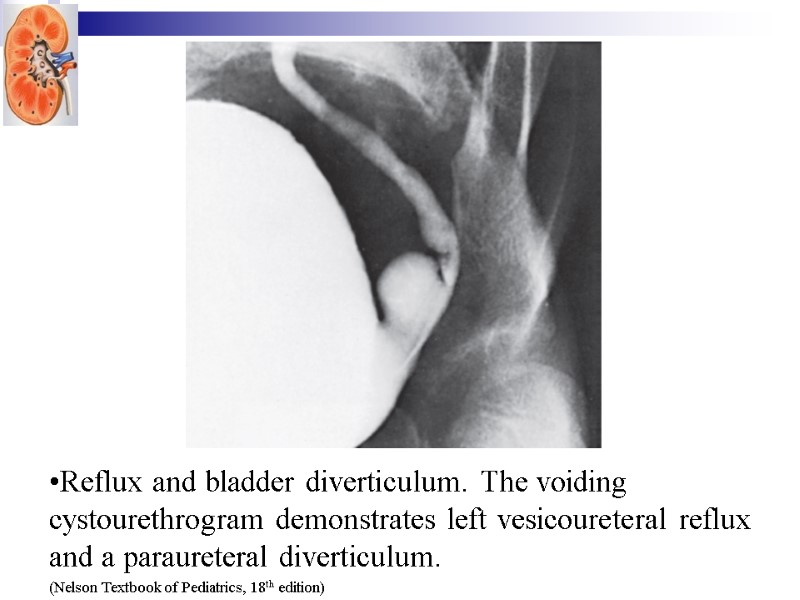 Reflux and bladder diverticulum. The voiding cystourethrogram demonstrates left vesicoureteral reflux and a paraureteral diverticulum. (Nelson Textbook of Pediatrics, 18th edition)
Reflux and bladder diverticulum. The voiding cystourethrogram demonstrates left vesicoureteral reflux and a paraureteral diverticulum. (Nelson Textbook of Pediatrics, 18th edition)
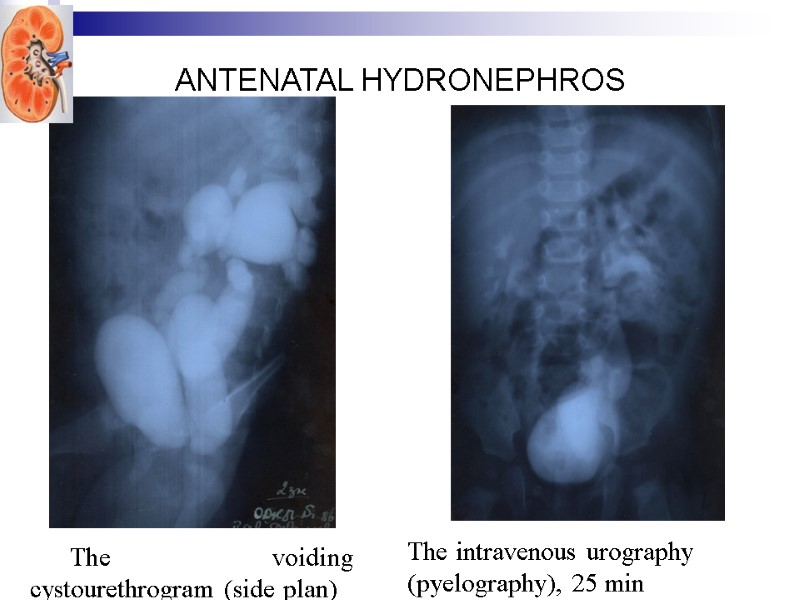
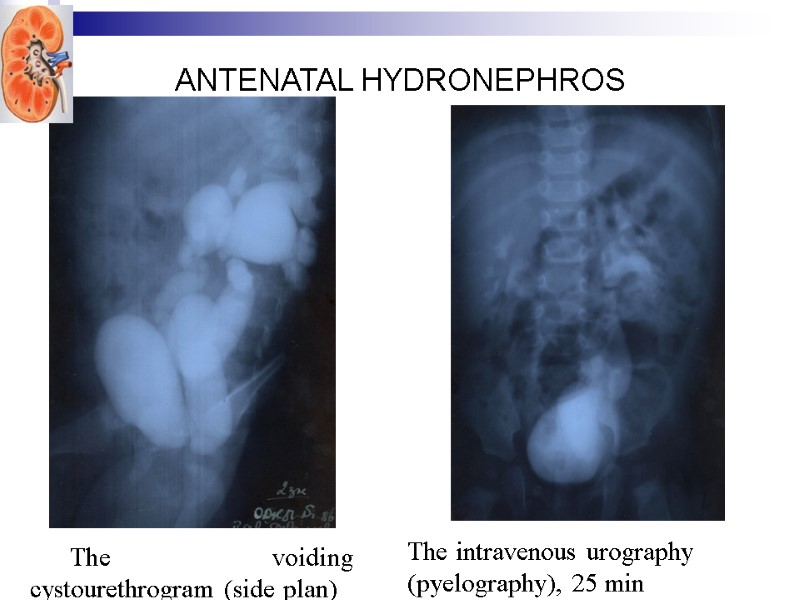 ANTENATAL HYDRONEPHROS The voiding cystourethrogram (side plan) The intravenous urography (pyelography), 25 min
ANTENATAL HYDRONEPHROS The voiding cystourethrogram (side plan) The intravenous urography (pyelography), 25 min
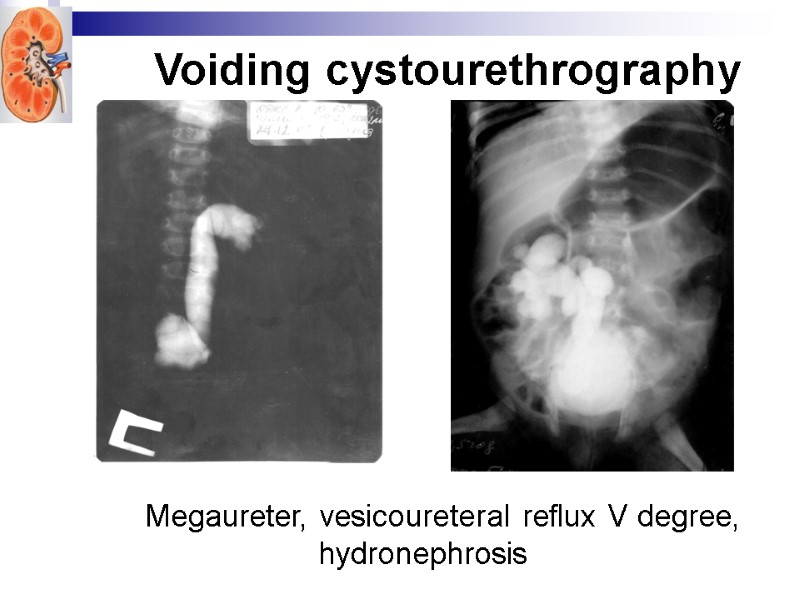
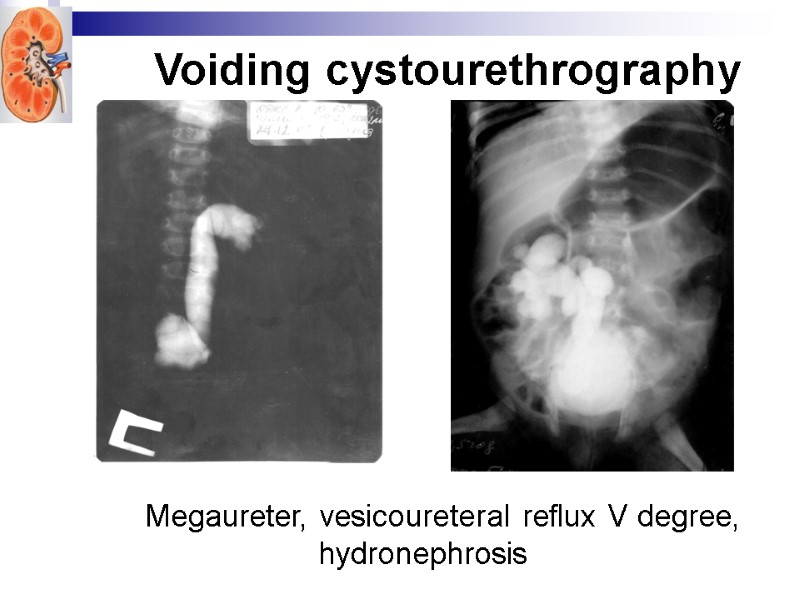 Megaureter, vesicoureteral reflux V degree, hydronephrosis Voiding cystourethrography
Megaureter, vesicoureteral reflux V degree, hydronephrosis Voiding cystourethrography
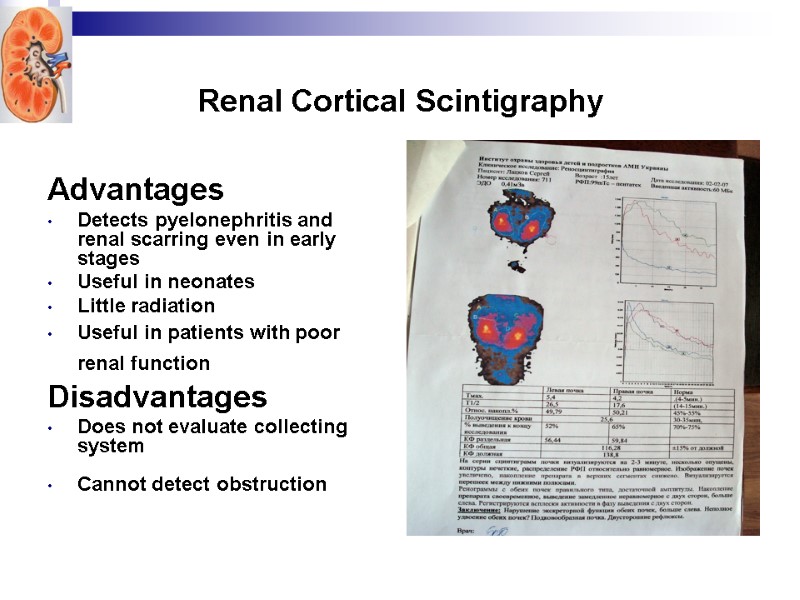
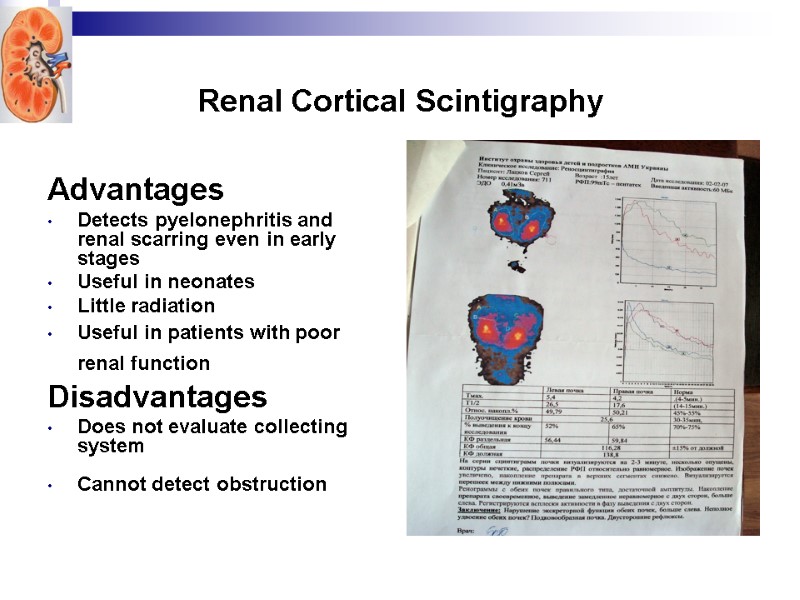 Renal Cortical Scintigraphy Advantages Detects pyelonephritis and renal scarring even in early stages Useful in neonates Little radiation Useful in patients with poor renal function Disadvantages Does not evaluate collecting system Cannot detect obstruction
Renal Cortical Scintigraphy Advantages Detects pyelonephritis and renal scarring even in early stages Useful in neonates Little radiation Useful in patients with poor renal function Disadvantages Does not evaluate collecting system Cannot detect obstruction
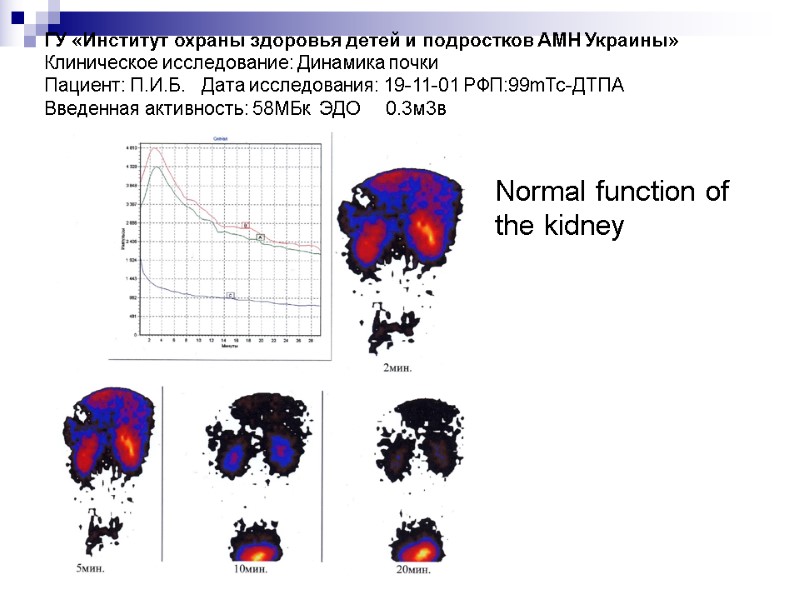
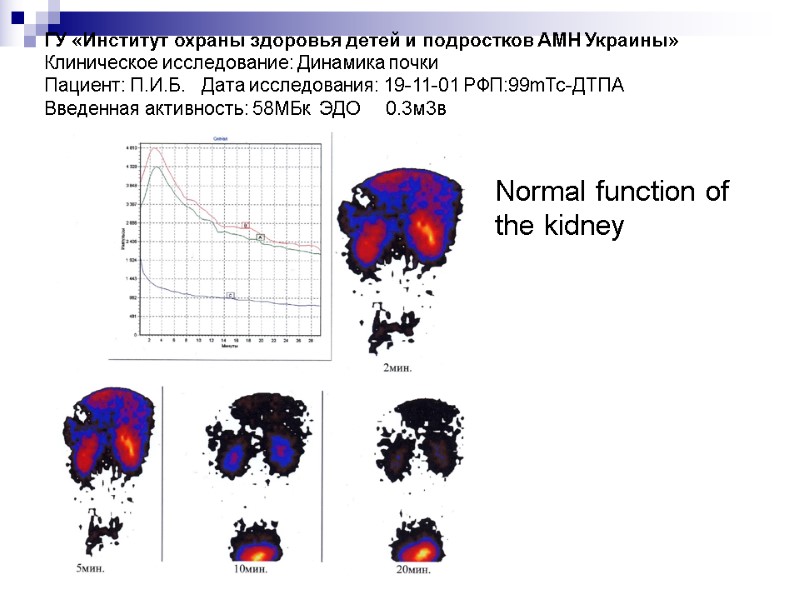 ГУ «Институт охраны здоровья детей и подростков АМН Украины» Клиническое исследование: Динамика почки Пациент: П.И.Б. Дата исследования: 19-11-01 РФП:99mТс-ДТПА Введенная активность: 58МБк ЭДО 0.3м3в Normal function of the kidney
ГУ «Институт охраны здоровья детей и подростков АМН Украины» Клиническое исследование: Динамика почки Пациент: П.И.Б. Дата исследования: 19-11-01 РФП:99mТс-ДТПА Введенная активность: 58МБк ЭДО 0.3м3в Normal function of the kidney
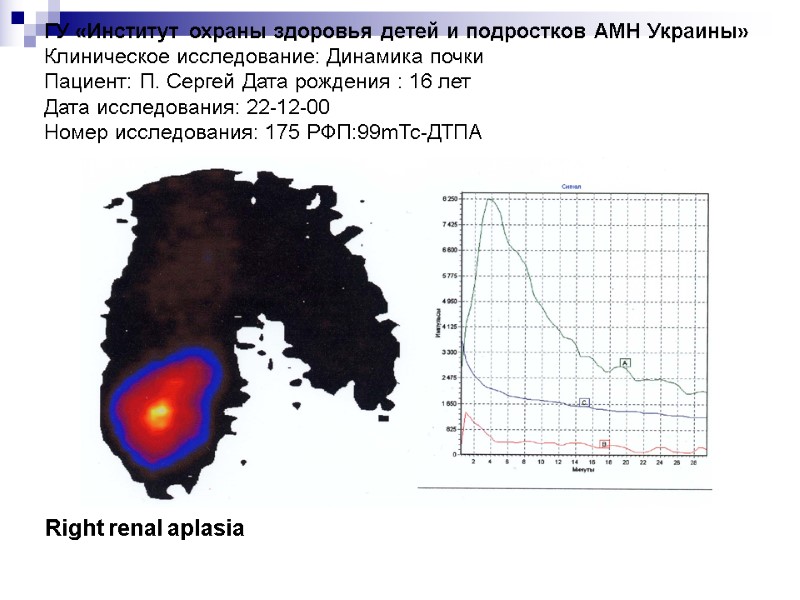
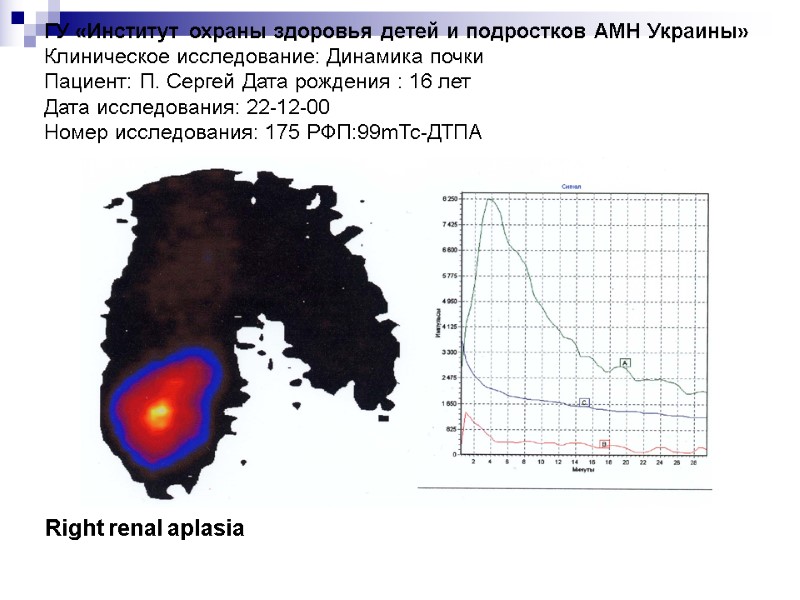 ГУ «Институт охраны здоровья детей и подростков АМН Украины» Клиническое исследование: Динамика почки Пациент: П. Сергей Дата рождения : 16 лет Дата исследования: 22-12-00 Номер исследования: 175 РФП:99mТс-ДТПА Right renal aplasia
ГУ «Институт охраны здоровья детей и подростков АМН Украины» Клиническое исследование: Динамика почки Пациент: П. Сергей Дата рождения : 16 лет Дата исследования: 22-12-00 Номер исследования: 175 РФП:99mТс-ДТПА Right renal aplasia
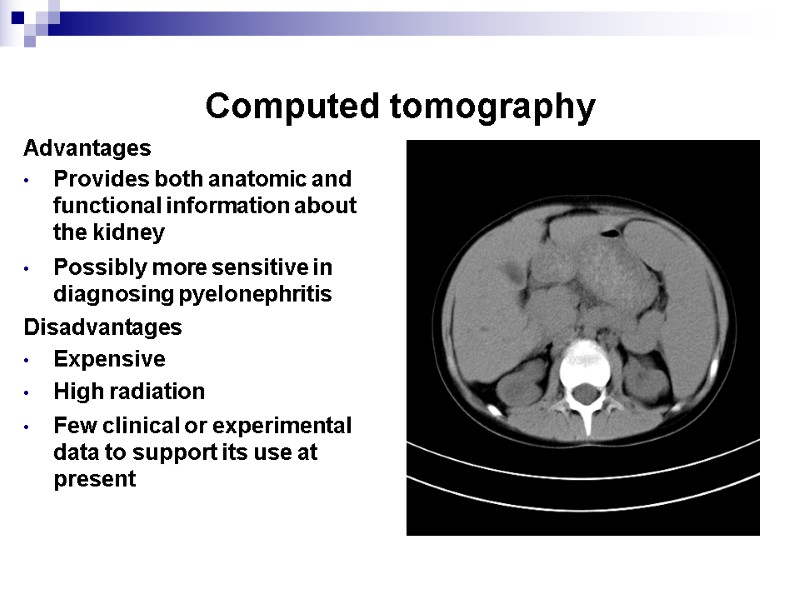
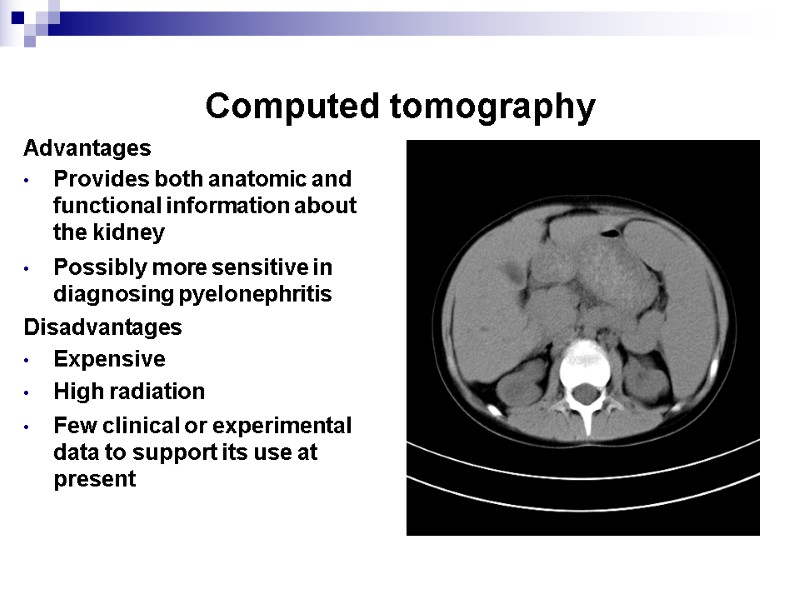 Computed tomography Advantages Provides both anatomic and functional information about the kidney Possibly more sensitive in diagnosing pyelonephritis Disadvantages Expensive High radiation Few clinical or experimental data to support its use at present
Computed tomography Advantages Provides both anatomic and functional information about the kidney Possibly more sensitive in diagnosing pyelonephritis Disadvantages Expensive High radiation Few clinical or experimental data to support its use at present
 Proper diagnosis of UTI needs the following: Prove the presence of UTI Detect the causative organisms and predisposing factors Differentiate between upper and lower UTI Differentiation between upper and lower UTI The following are in favor of upper UTI: High fever and intoxication Renal angle tenderness (positive Pasternatskiy symptom) Leukocytosis Bacteriemia High ESR Urinary WBC casts Impaired renal function (increased urea and creatinine) Impaired uptake or excretion of the radioisotope in radionuclide scanning
Proper diagnosis of UTI needs the following: Prove the presence of UTI Detect the causative organisms and predisposing factors Differentiate between upper and lower UTI Differentiation between upper and lower UTI The following are in favor of upper UTI: High fever and intoxication Renal angle tenderness (positive Pasternatskiy symptom) Leukocytosis Bacteriemia High ESR Urinary WBC casts Impaired renal function (increased urea and creatinine) Impaired uptake or excretion of the radioisotope in radionuclide scanning
 Complications of UTI Spread of infection – local - perinephral abscess; metastasis of infection – septicemia Chronic pyelonephritis chronic renal failure Transient VUR Malnutrition (in infants)
Complications of UTI Spread of infection – local - perinephral abscess; metastasis of infection – septicemia Chronic pyelonephritis chronic renal failure Transient VUR Malnutrition (in infants)
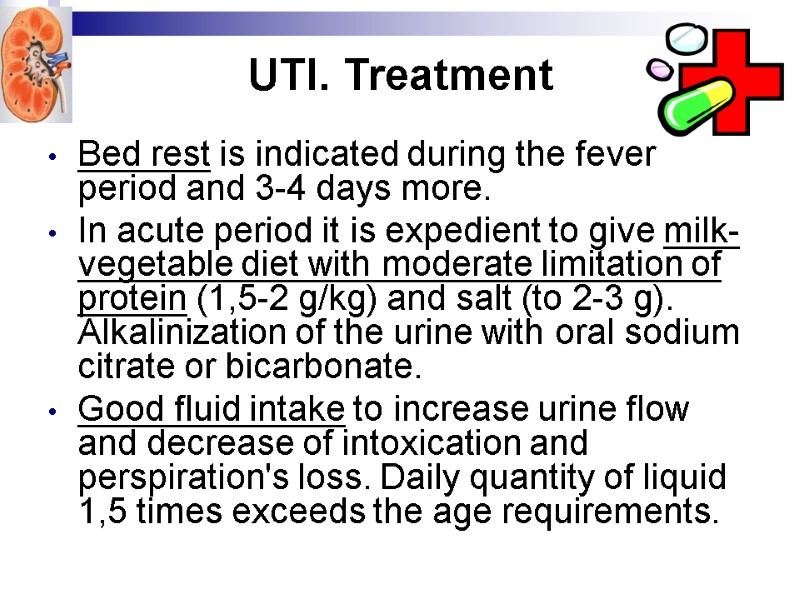 UTI. Treatment Bed rest is indicated during the fever period and 3-4 days more. In acute period it is expedient to give milk-vegetable diet with moderate limitation of protein (1,5-2 g/kg) and salt (to 2-3 g). Alkalinization of the urine with oral sodium citrate or bicarbonate. Good fluid intake to increase urine flow and decrease of intoxication and perspiration's loss. Daily quantity of liquid 1,5 times exceeds the age requirements.
UTI. Treatment Bed rest is indicated during the fever period and 3-4 days more. In acute period it is expedient to give milk-vegetable diet with moderate limitation of protein (1,5-2 g/kg) and salt (to 2-3 g). Alkalinization of the urine with oral sodium citrate or bicarbonate. Good fluid intake to increase urine flow and decrease of intoxication and perspiration's loss. Daily quantity of liquid 1,5 times exceeds the age requirements.
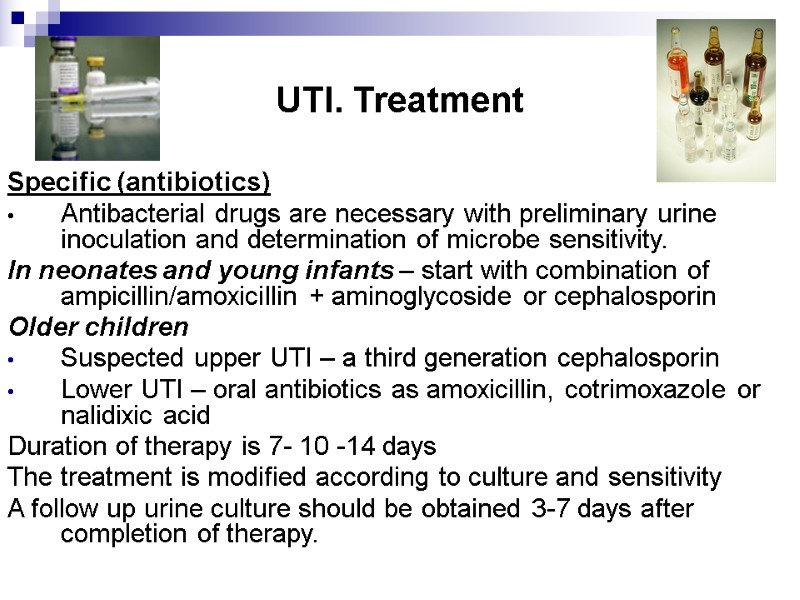 UTI. Treatment Specific (antibiotics) Antibacterial drugs are necessary with preliminary urine inoculation and determination of microbe sensitivity. In neonates and young infants – start with combination of ampicillin/amoxicillin + aminoglycoside or cephalosporin Older children Suspected upper UTI – a third generation cephalosporin Lower UTI – oral antibiotics as amoxicillin, cotrimoxazole or nalidixic acid Duration of therapy is 7- 10 -14 days The treatment is modified according to culture and sensitivity A follow up urine culture should be obtained 3-7 days after completion of therapy.
UTI. Treatment Specific (antibiotics) Antibacterial drugs are necessary with preliminary urine inoculation and determination of microbe sensitivity. In neonates and young infants – start with combination of ampicillin/amoxicillin + aminoglycoside or cephalosporin Older children Suspected upper UTI – a third generation cephalosporin Lower UTI – oral antibiotics as amoxicillin, cotrimoxazole or nalidixic acid Duration of therapy is 7- 10 -14 days The treatment is modified according to culture and sensitivity A follow up urine culture should be obtained 3-7 days after completion of therapy.
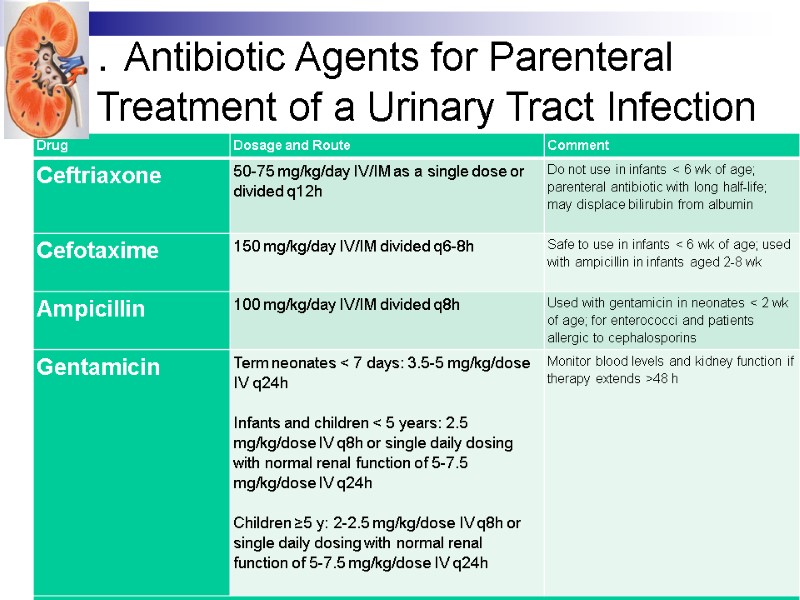
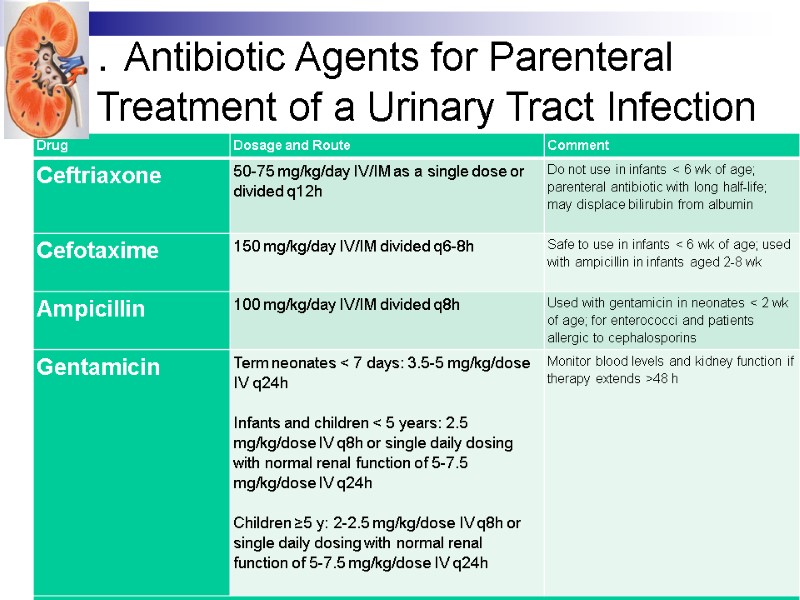 . Antibiotic Agents for Parenteral Treatment of a Urinary Tract Infection
. Antibiotic Agents for Parenteral Treatment of a Urinary Tract Infection
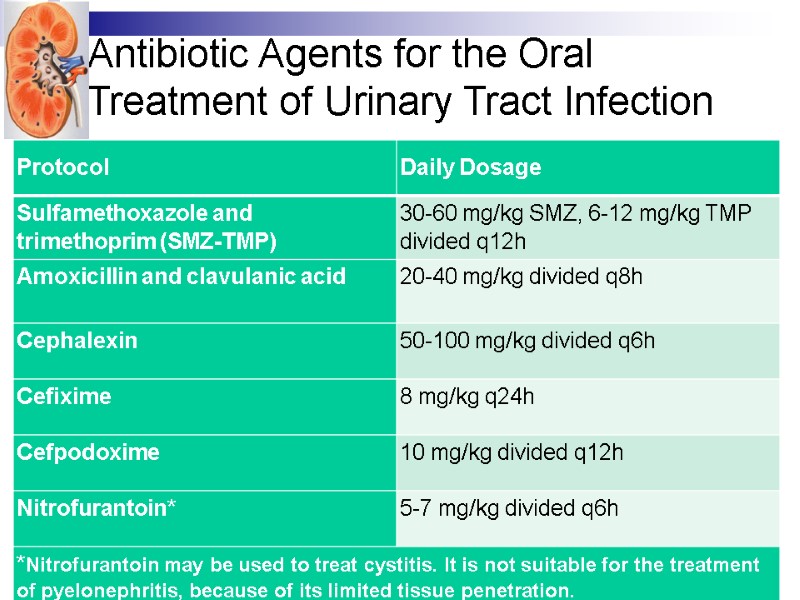
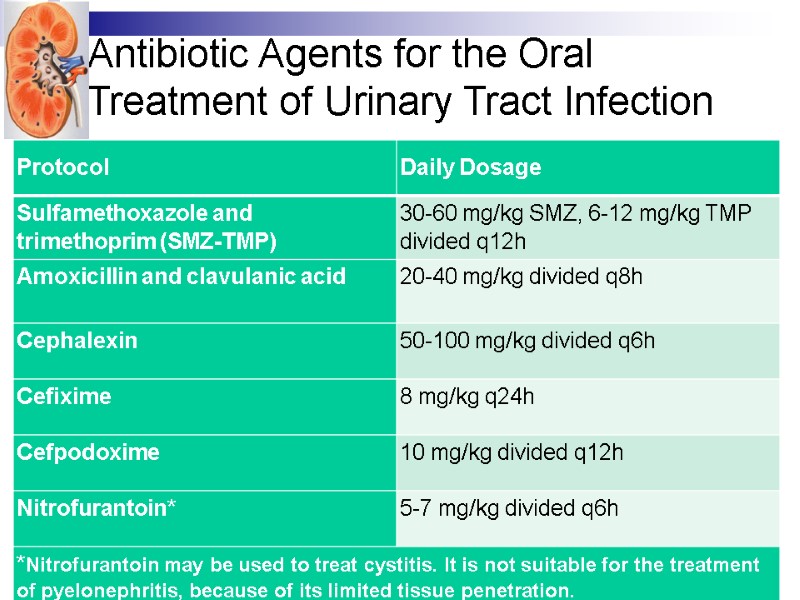 Antibiotic Agents for the Oral Treatment of Urinary Tract Infection
Antibiotic Agents for the Oral Treatment of Urinary Tract Infection
 UTI. Treatment Analgetic antipyretic – paracetamol – ibuprofen Antispastic therapy is prescribed in painful syndrome. Treatment of predisposing factors: Stone or obstructive lesions should be managed surgically VUR Dysmetabolic nephropathy Vaccines
UTI. Treatment Analgetic antipyretic – paracetamol – ibuprofen Antispastic therapy is prescribed in painful syndrome. Treatment of predisposing factors: Stone or obstructive lesions should be managed surgically VUR Dysmetabolic nephropathy Vaccines
 UTI. Criteria of effective treatment General state improves after 24-48 hr Bacteriuria disappears after 48-72 hr Normalization urine tests to 5 days
UTI. Criteria of effective treatment General state improves after 24-48 hr Bacteriuria disappears after 48-72 hr Normalization urine tests to 5 days
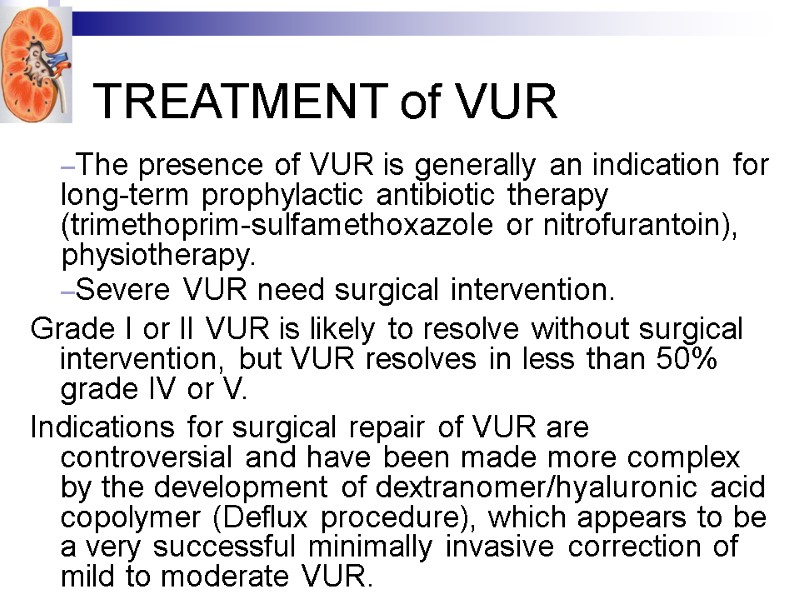
 TREATMENT of VUR The presence of VUR is generally an indication for long-term prophylactic antibiotic therapy (trimethoprim-sulfamethoxazole or nitrofurantoin), physiotherapy. Severe VUR need surgical intervention. Grade I or II VUR is likely to resolve without surgical intervention, but VUR resolves in less than 50% grade IV or V. Indications for surgical repair of VUR are controversial and have been made more complex by the development of dextranomer/hyaluronic acid copolymer (Deflux procedure), which appears to be a very successful minimally invasive correction of mild to moderate VUR.
TREATMENT of VUR The presence of VUR is generally an indication for long-term prophylactic antibiotic therapy (trimethoprim-sulfamethoxazole or nitrofurantoin), physiotherapy. Severe VUR need surgical intervention. Grade I or II VUR is likely to resolve without surgical intervention, but VUR resolves in less than 50% grade IV or V. Indications for surgical repair of VUR are controversial and have been made more complex by the development of dextranomer/hyaluronic acid copolymer (Deflux procedure), which appears to be a very successful minimally invasive correction of mild to moderate VUR.
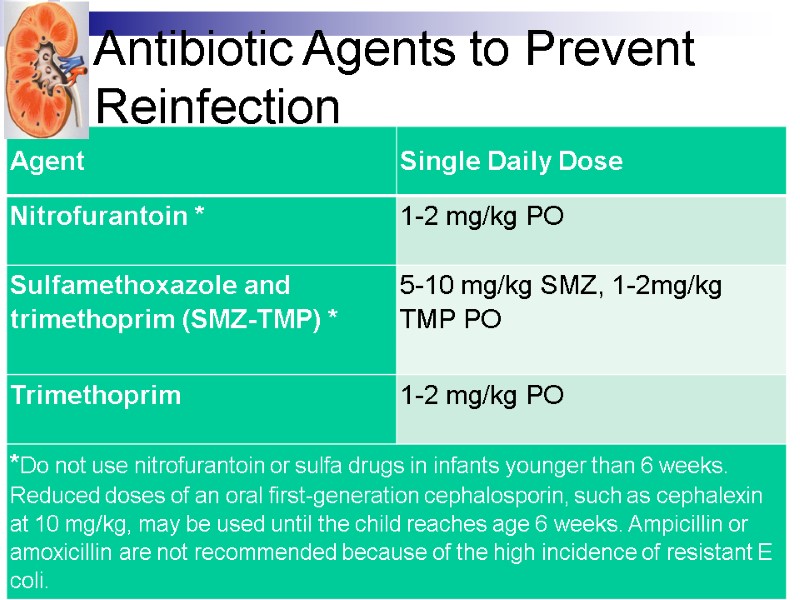
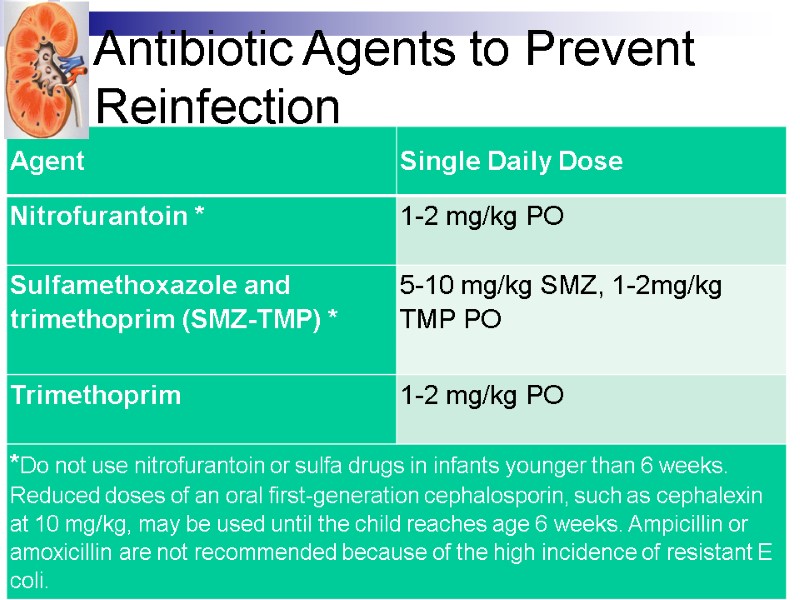 Antibiotic Agents to Prevent Reinfection
Antibiotic Agents to Prevent Reinfection
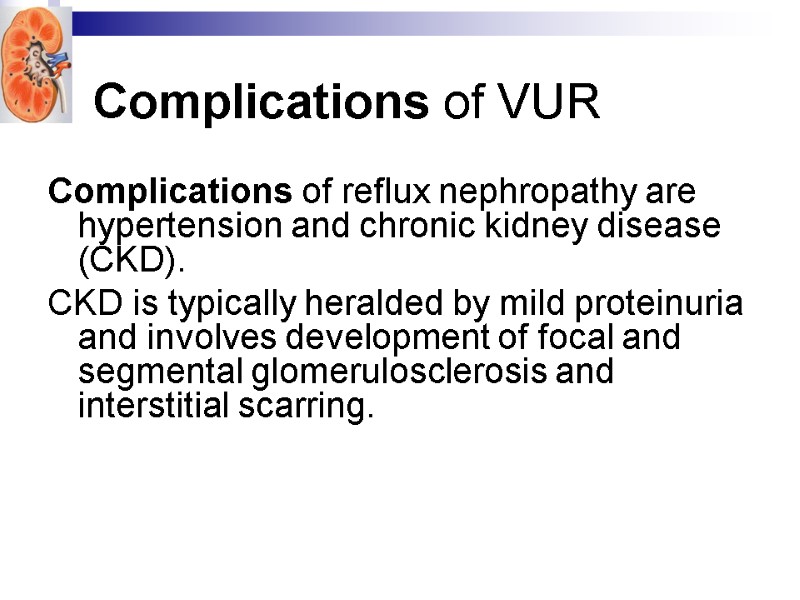
 Complications of VUR Complications of reflux nephropathy are hypertension and chronic kidney disease (CKD). CKD is typically heralded by mild proteinuria and involves development of focal and segmental glomerulosclerosis and interstitial scarring.
Complications of VUR Complications of reflux nephropathy are hypertension and chronic kidney disease (CKD). CKD is typically heralded by mild proteinuria and involves development of focal and segmental glomerulosclerosis and interstitial scarring.
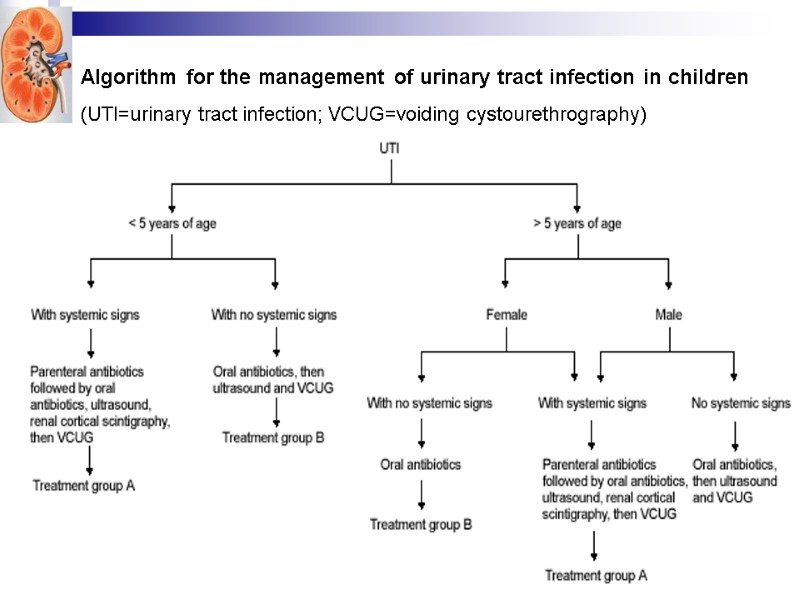
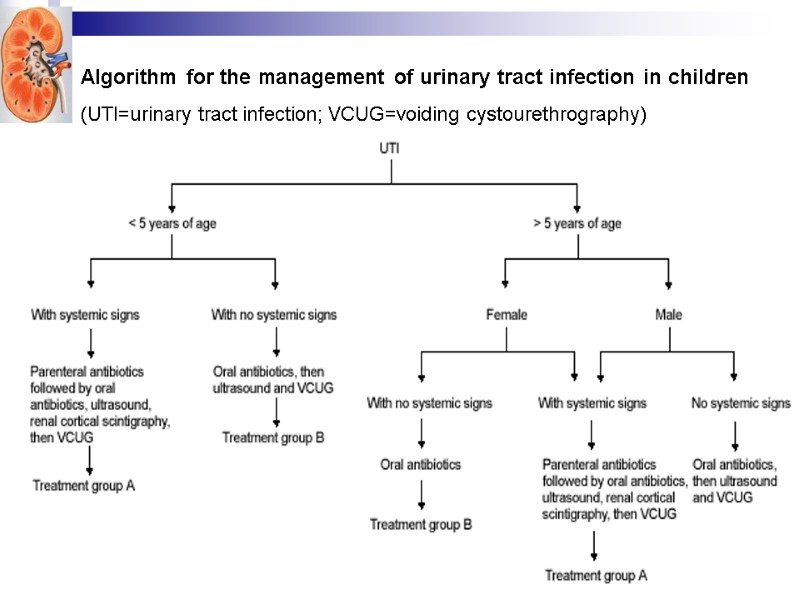 Algorithm for the management of urinary tract infection in children (UTI=urinary tract infection; VCUG=voiding cystourethrography)
Algorithm for the management of urinary tract infection in children (UTI=urinary tract infection; VCUG=voiding cystourethrography)
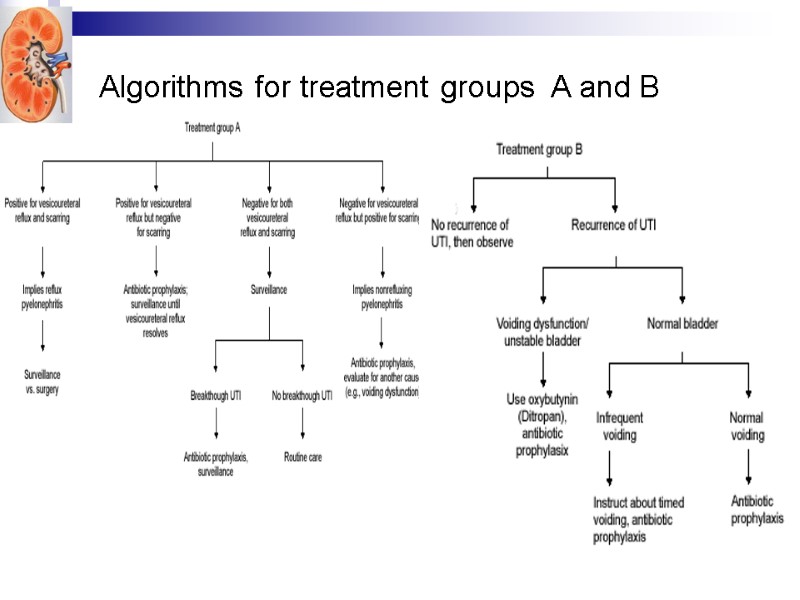
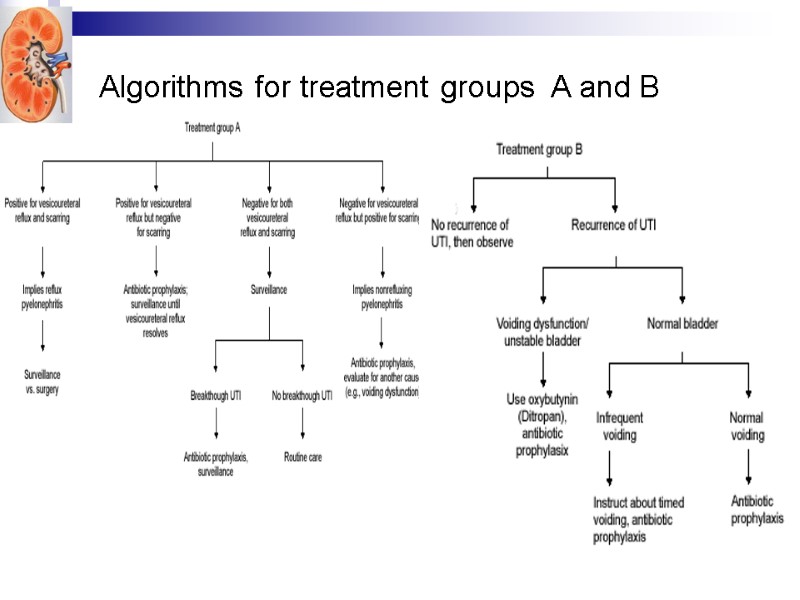 Algorithms for treatment groups A and B
Algorithms for treatment groups A and B
 Follow-up: Repeated urine culture every 3 months after recovery Long term follow-up with regular monitoring of blood pressure and kidney function
Follow-up: Repeated urine culture every 3 months after recovery Long term follow-up with regular monitoring of blood pressure and kidney function
 UTI. Prognosis No anatomic abnormalities and appropriate treatment – good prognosis No exacerbation during 3 years means recovery in child with acute pyelonephritis No progression chronic pyelonephritis during 5 years – good prognosis Chronic recurrent pyelonephritis – bad prognosis, chronic renal failure develops
UTI. Prognosis No anatomic abnormalities and appropriate treatment – good prognosis No exacerbation during 3 years means recovery in child with acute pyelonephritis No progression chronic pyelonephritis during 5 years – good prognosis Chronic recurrent pyelonephritis – bad prognosis, chronic renal failure develops
 Potential sequelae Renal scarring Chronic renal failure HTN (Hypertension)
Potential sequelae Renal scarring Chronic renal failure HTN (Hypertension)
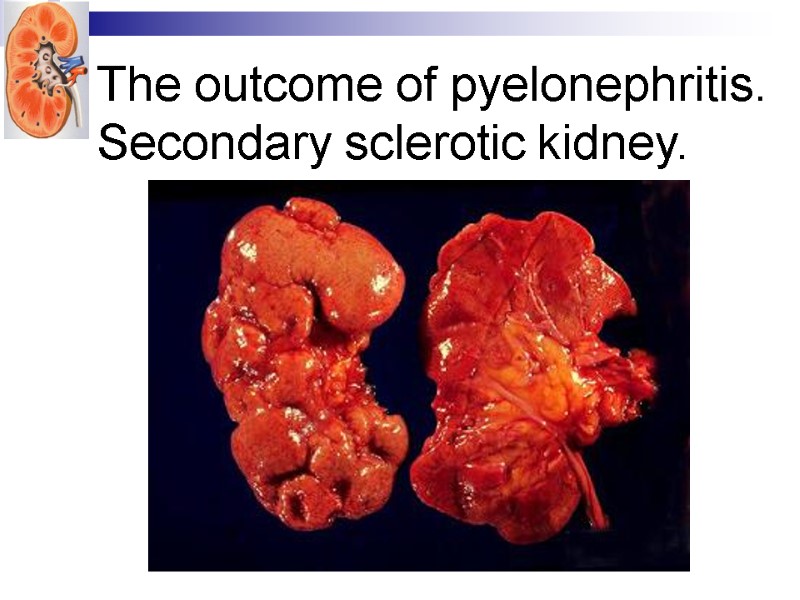
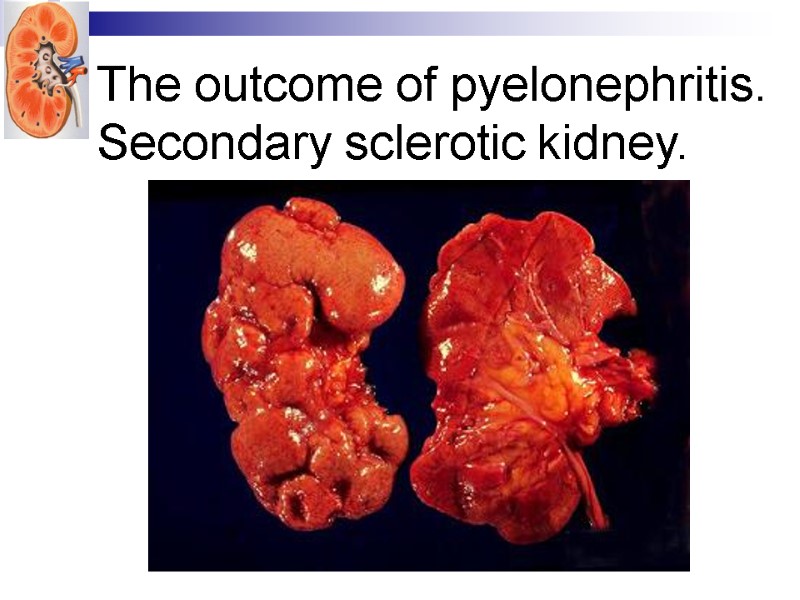 The outcome of pyelonephritis. Secondary sclerotic kidney.
The outcome of pyelonephritis. Secondary sclerotic kidney.
 THANKS
THANKS

