DM classifocation up date.ppt
- Количество слайдов: 47
UPDATE ON CLASSIFICATION AND DIAGNOSIS OF DIABETES MELLITUS
TYPE 1 DIABETES MELLITUS • PREVIOUS NAMES: 1. JUVENILE D. M. 2. IDDM
• COMPLETE DESTRUCTION OF -Cells

• AUTOIMMUNE, CELL - MEDIATED -Cell DESTRUCTION

MARKERS OF AUTOIMMUNE DESTRUCTION • ISLET CELL ANTIBODIES (ICAS). • INSULIN ANTIBODIES (IAAS). • GLUTAMIC ACID DECARBOXYLASE ANTIBODIES (GAD). • TYROSINE PHOSPHATE ANTIBODIES.
• ONE OR MORE IS PRESENT IN 85 -90% OF CASES WHEN HYPERGLYCEMIA DETECTED. IS FASTING INITIALLY
INVIRONMENTAL FACTORS • NOT WELL DEFINED - VIRUSES - TOXINS

PRESENTATION • RATE OF -CELL DESTRUCTION IS VARIABLE: 1 - RAPID IN SOME ESP. : INFANTS & CHILDREN 2 - SLOW ESP. : ADULTS
• MAY PRESENT INITIALLY WITH DKA. • OTHERS MAY PRESENT WITH MODEST HYPERGLYCEMIA, & MAY DECOMPENSATE TO DKA WHEN THERE IS INFECTION OR OTHER STRESS.
• OTHERS (esp. ADULTS): MAY RETAIN SOME RESIDUAL B-CELL FUNCTION, TO PREVENT DKA, FOR YEARS!. YEARS LATER, THEY EVENTUALLY END UP WITH COMPLETE B-CELL DESTRUCTION.
IDIOPATHIC DIABETES • • • A MINORITY OF TYPE 1 D. M. AFRICAN OR ASIAN ORIGIN. NO EVIDENCE OF AUTOIMMUNITY. NOT HLA ASSOCIATED. STRONGLY INHERITED. ABSOLUTE REQUIREMENT FOR INSULIN THERAPY MAY COME & GO!
TYPE 2 DIABETES MELLITUS • PREVIOUS NAMES: - NIDDM - ADULT ONSET DM.
ETIOLOGY • INSULIN RESISTANCE & • RELATIVE INSULIN DEFECIENCY
• SPECIFIC ETIOLOGIES: NOT CLEARLY KNOWN, BUT: – NO AUTOIMMUNE DESTRUCTION OF CELLS. – OBESITY – CENTRAL OR VISCERAL FAT DESTRIBUTION. – AGE – LACK OF EXERCISE
• DKA DOES NOT OCCUR BUT, IF IT OCCURS: LOOK FOR MAJOR STRESS! e. g. 1. M. I 2. INFECTION BE VERY CAREFULL!!
• STRONG GENETIC PREDISPOSITION THE GENETICS: ARE COMPLEX & NOT CLEARLY DEFINED
NEW CRITERIA • FPG > 126 mg/dl (7. 0 mmol/l). Fasting is defined as no caloric intake for at least 8 h. Or • 2 -h PG > 200 mg/dl (11. 1 mmol/l) during an OGTT. The test should be performed as described by WHO, using a glucose load containing the equivalent of 75 -g anhydrous glucose dissolved in water.

CRITERIA FOR THE DIAGNOSIS OF DIABETES MELLITUS • Normoglycemia IFG D. M • FPG <110 mg/dl FPG>110 mg/dl & FPG>126 mg/dl <126 mg/dl (IFG) • 2 -h PG+<140 mg/dl 2 -h PG+>200 mg/dl & <200 mg/dl (IGT) • --- Symptoms of DM & casual plasma glucose concentration >200 mg/dl
Or • Symptoms of diabetes plus casual plasma glucose concentration > 200 mg/dl (11. 1 mmol/l). Casual is defined as any time of day without regard to time since last meal. The classic symptoms of diabetes include polyria, polydipsia, and unexplained weight loss.
• THE NEW DIAGNOSTIC CRITERIA FOR DIABETES MELLITUS WERE LARGELY BASED ON CLINICAL CONSIDERATIONS: • AROUND FASTING PLASMA GLUCOSE OF 110 MG% (6. 1 MMOL/1) THE EARLY PHASE OF INSULIN SECRETION STARTS TO BE IMPAIRED.
• AROUND FASTING PLASMA GLUCOSE OF 126 mg% (7. 0 mmol/1), THE RISK OF MICROVASCULAR COMPLICATIONS INCREASES SIGNIFICANTLY. • THERE IS STRONG ASSOCIATION BETWEEN THE FOLLOWING PARAMETERS IN CAUSING MICROAGNIOPATHY: – FPG. – 2 HR PLASMA GLUCOSE. – Hb. Aic
LOWERING BLOOD GLUCOSE BELAYED THE ONSET, AND SLOWED THE PROGRESSION, OF MICROVASCULAR COMPLICATIONS
IS TIGHT CONTROL OF BLOOD GLUCOSE DANGEROUS ? ?
1 - HYPOGLYCEMIA BE CAREFUL • FREQUENT PG MONITORING • ADJUSTMENT OF INSULIN DOSE, TIMING AND FREQUENCY • ADJUSTMENT OF MEALS, CONTENT & TIMING • ADJUSTMENT OF EXERCISE/ACTIVITY
FOR EVERY 1% DECREASE IN Hb. AIC (e. g. FROM 9 TO 8%): THERE WAS A 25% REDUCTION IN DIABETES - RELATED DEATHS.

DIABETES & B. P • OPTIMUM B. P 120/80. • SYSTOLIC B. P SHOULD BE: < 130 mm. Hg • DIASTOLIC B. P SHOULD BE: < 80 mm. Hg ---------- • SYSTOLIC B. P: 130 -139 OR • DIASTOLIC B. P: 80 -90

• Rx: 3 MONTH TRIAL OF : LIFESTYLE/BEHAVIORAL THERAPY (LBT). IF TARGET NOT ACIEVED: ---> ADD PHARMACOTHERAPY
LBT • DIET: SODIUM BODY WEIGHT D/C ALCOHOL • D/C SMOKING • INCREASE PHYSICAL ACTIVITY.
SYSTOLIC B. P > 140 OR DIASTOLIC B. P > 90 SHOULD RECEIVE DRUG THERAPY IN ADDITION TO (LBT). • USE 1, 2, 3 OR MORE ANTIHYPERTENSIVE DRUGS AS NEEDED TO CONTROL B. P
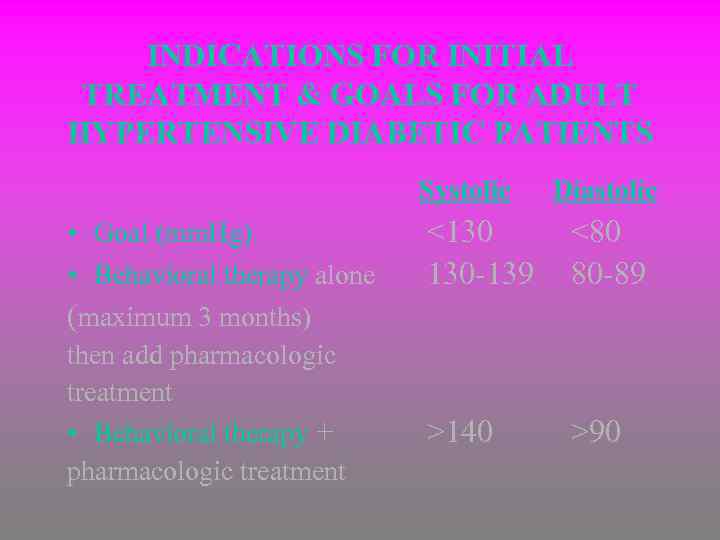
INDICATIONS FOR INITIAL TREATMENT & GOALS FOR ADULT HYPERTENSIVE DIABETIC PATIENTS Systolic • Goal (mm. Hg) • Behavioral therapy alone (maximum 3 months) then add pharmacologic treatment • Behavioral therapy + pharmacologic treatment Diastolic <130 130 -139 <80 80 -89 >140 >90
DIABETES & LIPID MANAGEMETN • LOWERING LDL CHOLESTEROL. • LOWERIND TGD & INCREASING HDL CHOLESTEROL: IS ASSOCIATED WITH A REDUCTION IN CARDIOVASCULAR EVENTS.
• LDL GOAL: < 100 mg/dl (2. 6 mmol/l) • LDL 100 -129 mg/dl AGGRESSIVE DIET, EXERCISE TO Wt. + STATIN
• HDL < 45 mg/dl IN MALES < 55 mg/dl IN FEMALES EXERCISE Wt. REDUCTION STOP SMOKING ? FIBRIC ACID ? NIACIN
• TGD: GOAL: < 150 mg/dl – DIET, Wt. , CONTROL D. M – DRUGS: FIBRIC ACID
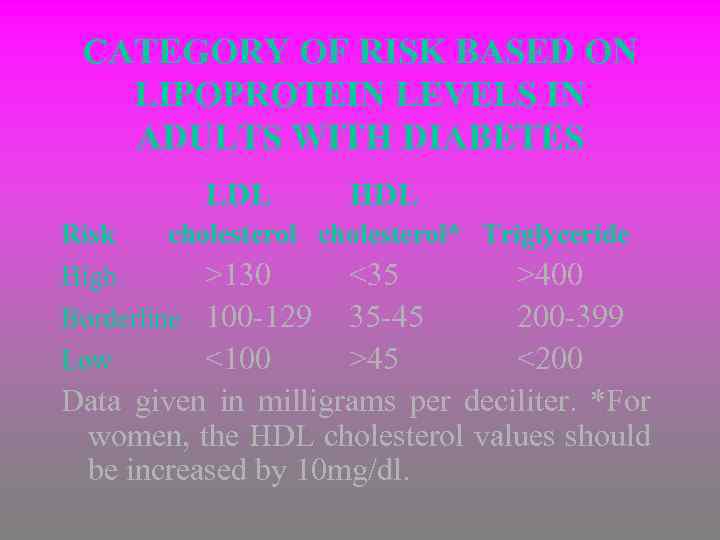
CATEGORY OF RISK BASED ON LIPOPROTEIN LEVELS IN ADULTS WITH DIABETES LDL Risk High HDL cholesterol* Triglyceride >130 <35 >400 Borderline 100 -129 35 -45 200 -399 Low <100 >45 <200 Data given in milligrams per deciliter. *For women, the HDL cholesterol values should be increased by 10 mg/dl.
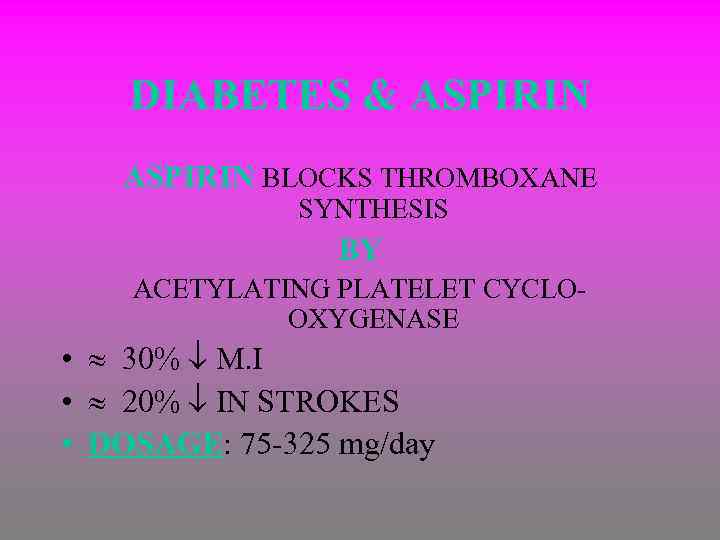
DIABETES & ASPIRIN BLOCKS THROMBOXANE SYNTHESIS BY ACETYLATING PLATELET CYCLOOXYGENASE • 30% M. I • 20% IN STROKES • DOSAGE: 75 -325 mg/day
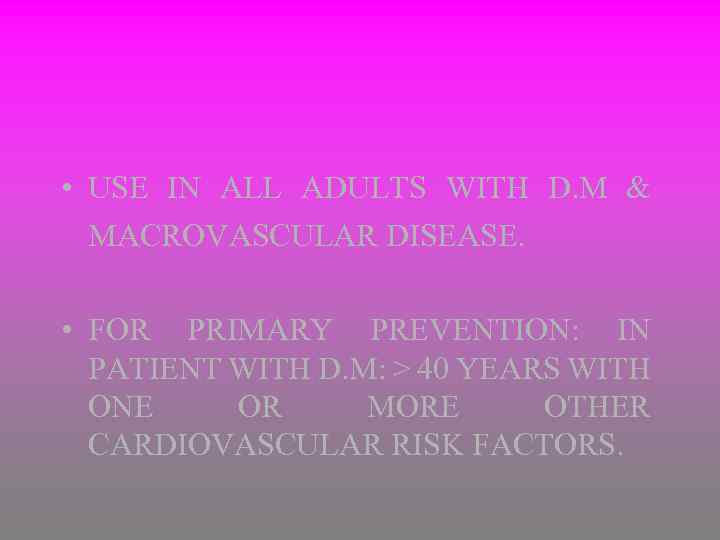
• USE IN ALL ADULTS WITH D. M & MACROVASCULAR DISEASE. • FOR PRIMARY PREVENTION: IN PATIENT WITH D. M: > 40 YEARS WITH ONE OR MORE OTHER CARDIOVASCULAR RISK FACTORS.
CORONARY HEAR DISEASE SCREENING IN D. M • TO IDENTIFY THE PRESENCE OF CHD IN DIABETIC PATIENTS WITH NO SYMPTOMS OF CHD.

NEPHROPATHY SCREENING AND D. M • DIABETIC NEPHROPATHY OCCURS IN 20 -40% IN DIABETICS • THE SINGLE LEADING CAUSE OF END -STAGE RENAL DISEASE (ESRD) • MICROAIBUNINURIA: 30 -299 mg/24 hr. : THE EARLIEST STAGE OF DIABETIC NEPHROPATHY. ALSO A MARKER FOR CVD.
• PERFORM A TEST FOR MICROAIBUMENURIA ANNUALLY, IN: 1 - TYPE 1 DIABETICS > 5 YEARS AFTER Dx. 2 - TYPE 2 DIABETICS: AT Dx. • USE ACE INHIBITORS OR/AND • ARBS

DEFINITIONS OF ABNORMALITIES IN ALBUMIN EXCRETION 24 -h collection Category Spot collection (mg/24 h) (µg/mg creatinine) ------------------------------------- Normal <30 Microalbuminuria 30 -299 Clinical albuminuria >300
RETINOPATHY & D. M • DIABETIC RETINOPATHY: THE MOST FREQUENT CAUSE OF BLINDNESS IN AGES 20 -74 YEARS. • PREVALANCE OF DIABETIC RETINOPATHY: IS STRONGLY RELATED TO THE DURATION OF DIABETES.
• AIM OF SCREENING: – EARLY DISCOVERY – EARLY MANAGEMENT – VALUE OF EARLY LASER PHOTOCOAGULATION IN PREVENTING VISUAL LOSS
• OPTIMAL GLYCEMIC CONTROL. • OPTIMAL B. P CONTROL. CAN REDUCE PROGRESSION OF DIABETIC RETINOPATHY

SCREENING RECOMMENDATIONS • TYPE 1 DIABETICS: INITIAL DILATED & COMPREHENSIVE FUNDUS EXAM. BY AN OPHTHALMOLOGIST WITHIN 3 -5 YEARS AFTER Dx. • TYPE 2 DIABETICS: SHORTLY AFTER Dx. IS MADE • SUBSEQUENT EXAMS: ANNUALLY EXCEPT ? ! • WHEN RETINOPATHY IS PROGRESSING
PREVENTION OF TYPE 1 D. M ALL RESEARCH ! -IN FIRST- DEGREE RELATIVES OF TYPE 1 DIABETICS • BECAUSE WE NOW HAVE THE ABILITY TO PREDICT DEVELOPMENT OF TYPE 1 D. M IN SOME PEOPLE: INVESTIGATIONS ARE GOING ON TO HALT OR EVEN PREVENT BCELL DESTRUCTION.
PANCREAS & ISLET CELL TRANSPLANTATION FOR TYPE 1 D. M • PANCREAS & KIDNEY TRANSPLANTS • PANCREAS ONLY TRANSPLANTS • ISOLATED ISLET CELL RESEARCH ONLY. TRANSPLANTATION:
DM classifocation up date.ppt