a5d3e1bc8a9d86a50591ac3c39d11709.ppt
- Количество слайдов: 41
 Update Management of Adrenal Incidentaloma Joint Hospital Surgical Grand Round 21/10/2017 LEUNG Lai Ying, Sandy North District Hospital
Update Management of Adrenal Incidentaloma Joint Hospital Surgical Grand Round 21/10/2017 LEUNG Lai Ying, Sandy North District Hospital
 Outline What is an adrenal incidentaloma? How to manage them? How should we follow-up?
Outline What is an adrenal incidentaloma? How to manage them? How should we follow-up?
 What is an adrenal incidentaloma? Asymptomatic adrenal mass greater than 1 cm that is discovered incidentally on imaging performed for nonadrenal problem Thompson et al. “Adrenal incidentaloma. ” Current Opinion in Oncology 2003, 15(1), 84 -90.
What is an adrenal incidentaloma? Asymptomatic adrenal mass greater than 1 cm that is discovered incidentally on imaging performed for nonadrenal problem Thompson et al. “Adrenal incidentaloma. ” Current Opinion in Oncology 2003, 15(1), 84 -90.
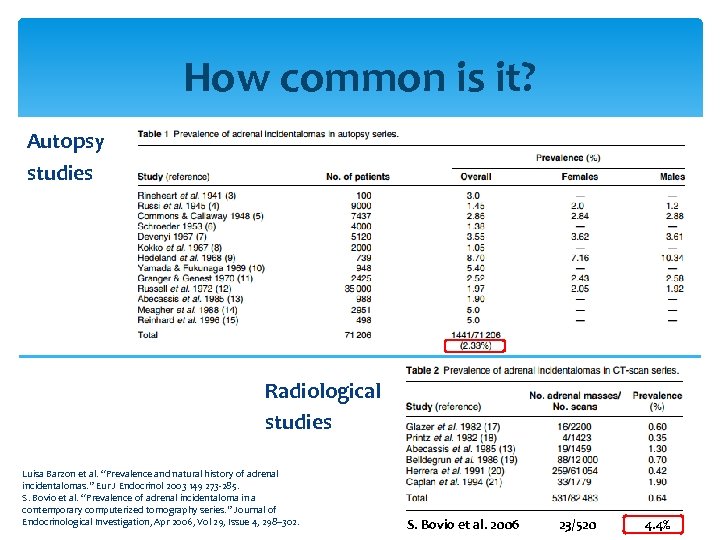 How common is it? Autopsy studies Radiological studies Luisa Barzon et al. “Prevalence and natural history of adrenal incidentalomas. ” Eur J Endocrinol 2003 149 273 -285. S. Bovio et al. “Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. ” Journal of Endocrinological Investigation, Apr 2006, Vol 29, Issue 4, 298– 302. S. Bovio et al. 2006 23/520 4. 4%
How common is it? Autopsy studies Radiological studies Luisa Barzon et al. “Prevalence and natural history of adrenal incidentalomas. ” Eur J Endocrinol 2003 149 273 -285. S. Bovio et al. “Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. ” Journal of Endocrinological Investigation, Apr 2006, Vol 29, Issue 4, 298– 302. S. Bovio et al. 2006 23/520 4. 4%
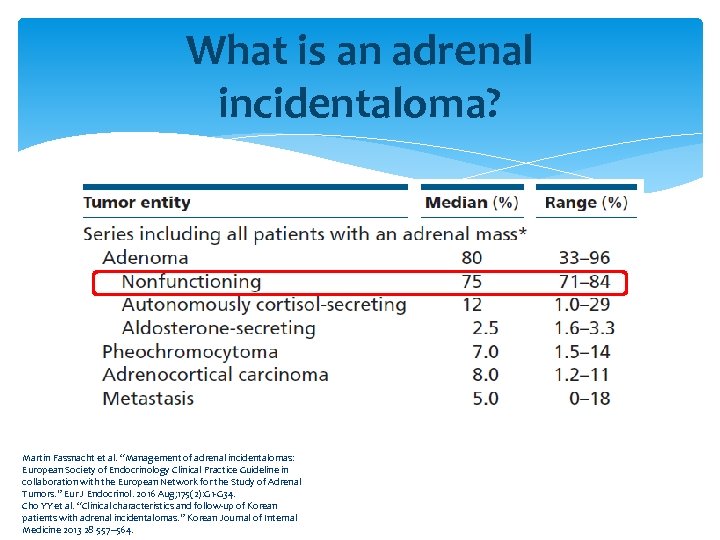 What is an adrenal incidentaloma? Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34. Cho YY et al. “Clinical characteristics and follow-up of Korean patients with adrenal incidentalomas. ” Korean Journal of Internal Medicine 2013 28 557– 564.
What is an adrenal incidentaloma? Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34. Cho YY et al. “Clinical characteristics and follow-up of Korean patients with adrenal incidentalomas. ” Korean Journal of Internal Medicine 2013 28 557– 564.
 How to manage them? Clinical exam Biochemical workup Radiological workup
How to manage them? Clinical exam Biochemical workup Radiological workup
 Biochemical workup - Screening Phaeochromocytoma 24 -hour urine for metanephrines and catecholamines Conn’s syndrome Aldosterone-renin ratio Cushing’s syndrome 1 mg overnight dexamethasone suppression test
Biochemical workup - Screening Phaeochromocytoma 24 -hour urine for metanephrines and catecholamines Conn’s syndrome Aldosterone-renin ratio Cushing’s syndrome 1 mg overnight dexamethasone suppression test
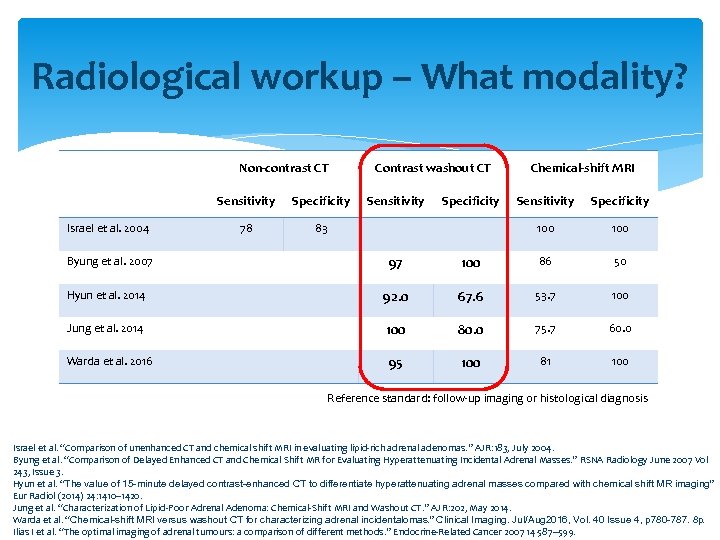 Radiological workup – What modality? Non-contrast CT Sensitivity Israel et al. 2004 Byung et al. 2007 Specificity 78 Contrast washout CT Sensitivity 83 0 Sensitivity Specificity 100 97 Specificity Chemical-shift MRI 100 86 50 Hyun et al. 2014 92. 0 67. 6 53. 7 100 Jung et al. 2014 100 80. 0 75. 7 60. 0 Warda et al. 2016 95 100 81 100 Reference standard: follow-up imaging or histological diagnosis Israel et al. “Comparison of unenhanced CT and chemical shift MRI in evaluating lipid-rich adrenal adenomas. ” AJR: 183, July 2004. Byung et al. “Comparison of Delayed Enhanced CT and Chemical Shift MR for Evaluating Hyperattenuating Incidental Adrenal Masses. ” RSNA Radiology June 2007 Vol 243, Issue 3. Hyun et al. “The value of 15 -minute delayed contrast-enhanced CT to differentiate hyperattenuating adrenal masses compared with chemical shift MR imaging. ” Eur Radiol (2014) 24: 1410– 1420. Jung et al. “Characterization of Lipid-Poor Adrenal Adenoma: Chemical-Shift MRI and Washout CT. ” AJR: 202, May 2014. Warda et al. “Chemical-shift MRI versus washout CT for characterizing adrenal incidentalomas. ” Clinical Imaging. Jul/Aug 2016, Vol. 40 Issue 4, p 780 -787. 8 p. Ilias I et al. “The optimal imaging of adrenal tumours: a comparison of different methods. ” Endocrine-Related Cancer 2007 14 587– 599.
Radiological workup – What modality? Non-contrast CT Sensitivity Israel et al. 2004 Byung et al. 2007 Specificity 78 Contrast washout CT Sensitivity 83 0 Sensitivity Specificity 100 97 Specificity Chemical-shift MRI 100 86 50 Hyun et al. 2014 92. 0 67. 6 53. 7 100 Jung et al. 2014 100 80. 0 75. 7 60. 0 Warda et al. 2016 95 100 81 100 Reference standard: follow-up imaging or histological diagnosis Israel et al. “Comparison of unenhanced CT and chemical shift MRI in evaluating lipid-rich adrenal adenomas. ” AJR: 183, July 2004. Byung et al. “Comparison of Delayed Enhanced CT and Chemical Shift MR for Evaluating Hyperattenuating Incidental Adrenal Masses. ” RSNA Radiology June 2007 Vol 243, Issue 3. Hyun et al. “The value of 15 -minute delayed contrast-enhanced CT to differentiate hyperattenuating adrenal masses compared with chemical shift MR imaging. ” Eur Radiol (2014) 24: 1410– 1420. Jung et al. “Characterization of Lipid-Poor Adrenal Adenoma: Chemical-Shift MRI and Washout CT. ” AJR: 202, May 2014. Warda et al. “Chemical-shift MRI versus washout CT for characterizing adrenal incidentalomas. ” Clinical Imaging. Jul/Aug 2016, Vol. 40 Issue 4, p 780 -787. 8 p. Ilias I et al. “The optimal imaging of adrenal tumours: a comparison of different methods. ” Endocrine-Related Cancer 2007 14 587– 599.
 Radiological features of malignancy Gross Signs of Malignancy Heterogeneity Irregular margin Peripheral invasion Regional lymph node Distant metastasis Size Hounsfield units (on plain scan) Contrast washout value (on contrast scan)
Radiological features of malignancy Gross Signs of Malignancy Heterogeneity Irregular margin Peripheral invasion Regional lymph node Distant metastasis Size Hounsfield units (on plain scan) Contrast washout value (on contrast scan)
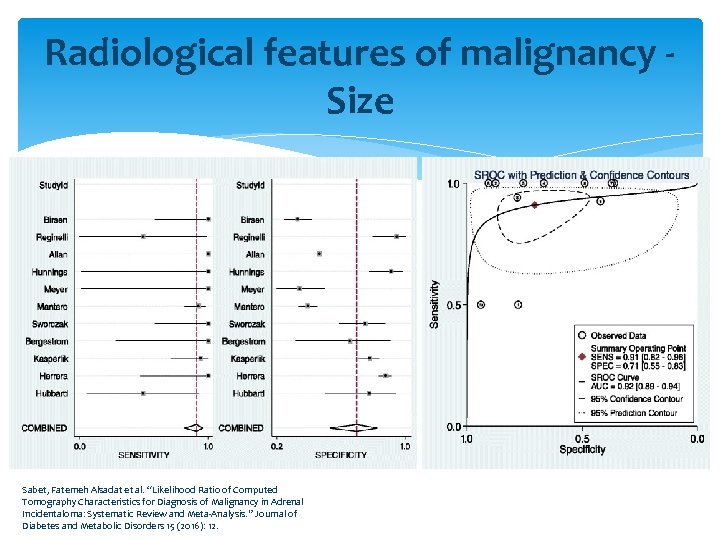 Radiological features of malignancy - Size Sabet, Fatemeh Alsadat et al. “Likelihood Ratio of Computed Tomography Characteristics for Diagnosis of Malignancy in Adrenal Incidentaloma: Systematic Review and Meta-Analysis. ” Journal of Diabetes and Metabolic Disorders 15 (2016): 12.
Radiological features of malignancy - Size Sabet, Fatemeh Alsadat et al. “Likelihood Ratio of Computed Tomography Characteristics for Diagnosis of Malignancy in Adrenal Incidentaloma: Systematic Review and Meta-Analysis. ” Journal of Diabetes and Metabolic Disorders 15 (2016): 12.
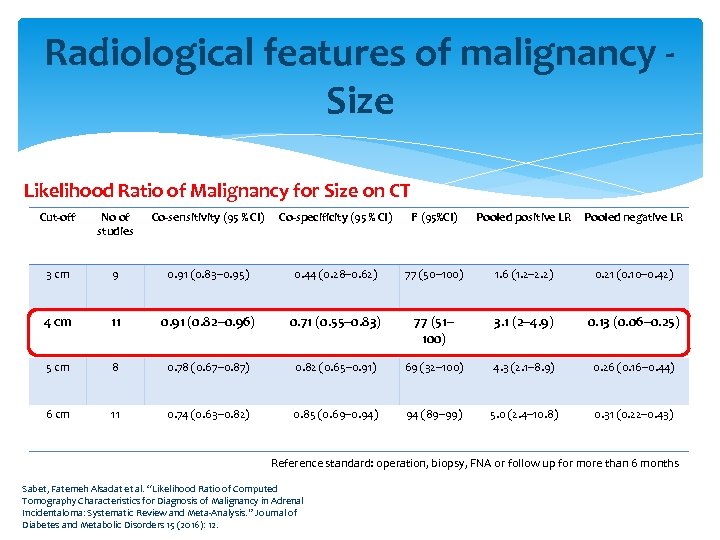 Radiological features of malignancy - Size Likelihood Ratio of Malignancy for Size on CT Cut-off No of studies Co-sensitivity (95 % CI) Co-specificity (95 % CI) I 2 (95%CI) Pooled positive LR Pooled negative LR 3 cm 9 0. 91 (0. 83– 0. 95) 0. 44 (0. 28– 0. 62) 77 (50– 100) 1. 6 (1. 2– 2. 2) 0. 21 (0. 10– 0. 42) 4 cm 11 0. 91 (0. 82– 0. 96) 0. 71 (0. 55– 0. 83) 77 (51– 100) 3. 1 (2– 4. 9) 0. 13 (0. 06– 0. 25) 5 cm 8 0. 78 (0. 67– 0. 87) 0. 82 (0. 65– 0. 91) 69 (32– 100) 4. 3 (2. 1– 8. 9) 0. 26 (0. 16– 0. 44) 6 cm 11 0. 74 (0. 63– 0. 82) 0. 85 (0. 69– 0. 94) 94 (89– 99) 5. 0 (2. 4– 10. 8) 0. 31 (0. 22– 0. 43) Reference standard: operation, biopsy, FNA or follow up for more than 6 months Sabet, Fatemeh Alsadat et al. “Likelihood Ratio of Computed Tomography Characteristics for Diagnosis of Malignancy in Adrenal Incidentaloma: Systematic Review and Meta-Analysis. ” Journal of Diabetes and Metabolic Disorders 15 (2016): 12.
Radiological features of malignancy - Size Likelihood Ratio of Malignancy for Size on CT Cut-off No of studies Co-sensitivity (95 % CI) Co-specificity (95 % CI) I 2 (95%CI) Pooled positive LR Pooled negative LR 3 cm 9 0. 91 (0. 83– 0. 95) 0. 44 (0. 28– 0. 62) 77 (50– 100) 1. 6 (1. 2– 2. 2) 0. 21 (0. 10– 0. 42) 4 cm 11 0. 91 (0. 82– 0. 96) 0. 71 (0. 55– 0. 83) 77 (51– 100) 3. 1 (2– 4. 9) 0. 13 (0. 06– 0. 25) 5 cm 8 0. 78 (0. 67– 0. 87) 0. 82 (0. 65– 0. 91) 69 (32– 100) 4. 3 (2. 1– 8. 9) 0. 26 (0. 16– 0. 44) 6 cm 11 0. 74 (0. 63– 0. 82) 0. 85 (0. 69– 0. 94) 94 (89– 99) 5. 0 (2. 4– 10. 8) 0. 31 (0. 22– 0. 43) Reference standard: operation, biopsy, FNA or follow up for more than 6 months Sabet, Fatemeh Alsadat et al. “Likelihood Ratio of Computed Tomography Characteristics for Diagnosis of Malignancy in Adrenal Incidentaloma: Systematic Review and Meta-Analysis. ” Journal of Diabetes and Metabolic Disorders 15 (2016): 12.
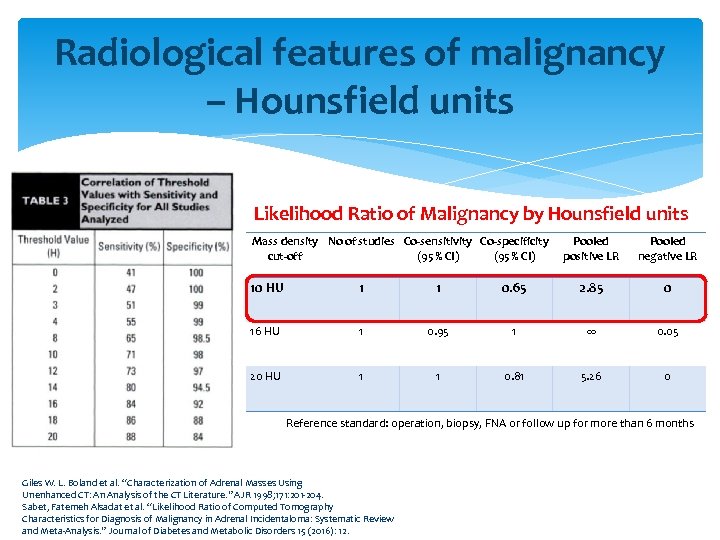 Radiological features of malignancy – Hounsfield units Likelihood Ratio of Malignancy by Hounsfield units Mass density No of studies Co-sensitivity Co-specificity Pooled cut-off (95 % CI) positive LR Pooled negative LR 10 HU 1 1 0. 65 2. 85 0 16 HU 1 0. 95 1 ∞ 0. 05 20 HU 1 1 0. 81 5. 26 0 Reference standard: operation, biopsy, FNA or follow up for more than 6 months Giles W. L. Boland et al. “Characterization of Adrenal Masses Using Unenhanced CT: An Analysis of the CT Literature. ” AJR 1998; 171: 201 -204. Sabet, Fatemeh Alsadat et al. “Likelihood Ratio of Computed Tomography Characteristics for Diagnosis of Malignancy in Adrenal Incidentaloma: Systematic Review and Meta-Analysis. ” Journal of Diabetes and Metabolic Disorders 15 (2016): 12.
Radiological features of malignancy – Hounsfield units Likelihood Ratio of Malignancy by Hounsfield units Mass density No of studies Co-sensitivity Co-specificity Pooled cut-off (95 % CI) positive LR Pooled negative LR 10 HU 1 1 0. 65 2. 85 0 16 HU 1 0. 95 1 ∞ 0. 05 20 HU 1 1 0. 81 5. 26 0 Reference standard: operation, biopsy, FNA or follow up for more than 6 months Giles W. L. Boland et al. “Characterization of Adrenal Masses Using Unenhanced CT: An Analysis of the CT Literature. ” AJR 1998; 171: 201 -204. Sabet, Fatemeh Alsadat et al. “Likelihood Ratio of Computed Tomography Characteristics for Diagnosis of Malignancy in Adrenal Incidentaloma: Systematic Review and Meta-Analysis. ” Journal of Diabetes and Metabolic Disorders 15 (2016): 12.
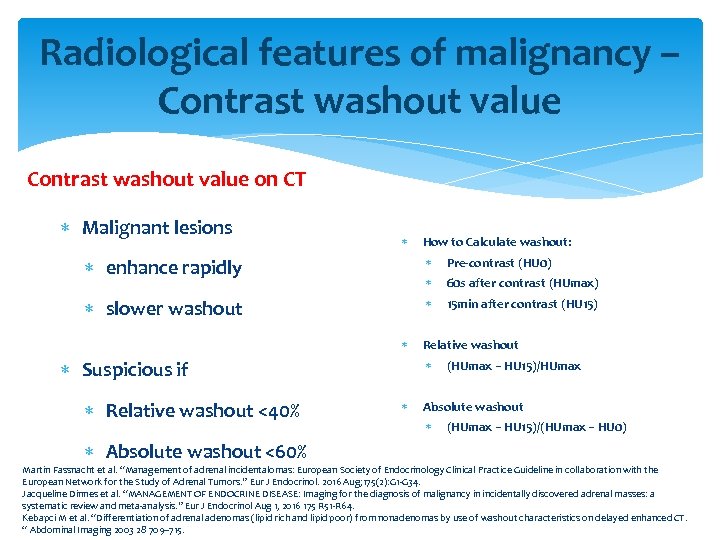 Radiological features of malignancy – Contrast washout value on CT Malignant lesions How to Calculate washout: enhance rapidly Pre-contrast (HU 0) 60 s after contrast (HUmax) slower washout 15 min after contrast (HU 15) Suspicious if Relative washout <40% Relative washout (HUmax − HU 15)/HUmax Absolute washout (HUmax − HU 15)/(HUmax − HU 0) Absolute washout <60% Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34. Jacqueline Dinnes et al. “MANAGEMENT OF ENDOCRINE DISEASE: Imaging for the diagnosis of malignancy in incidentally discovered adrenal masses: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016 175 R 51 -R 64. Kebapci M et al. “Differentiation of adrenal adenomas (lipid rich and lipid poor) from nonadenomas by use of washout characteristics on delayed enhanced CT. “ Abdominal Imaging 2003 28 709– 715.
Radiological features of malignancy – Contrast washout value on CT Malignant lesions How to Calculate washout: enhance rapidly Pre-contrast (HU 0) 60 s after contrast (HUmax) slower washout 15 min after contrast (HU 15) Suspicious if Relative washout <40% Relative washout (HUmax − HU 15)/HUmax Absolute washout (HUmax − HU 15)/(HUmax − HU 0) Absolute washout <60% Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34. Jacqueline Dinnes et al. “MANAGEMENT OF ENDOCRINE DISEASE: Imaging for the diagnosis of malignancy in incidentally discovered adrenal masses: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016 175 R 51 -R 64. Kebapci M et al. “Differentiation of adrenal adenomas (lipid rich and lipid poor) from nonadenomas by use of washout characteristics on delayed enhanced CT. “ Abdominal Imaging 2003 28 709– 715.
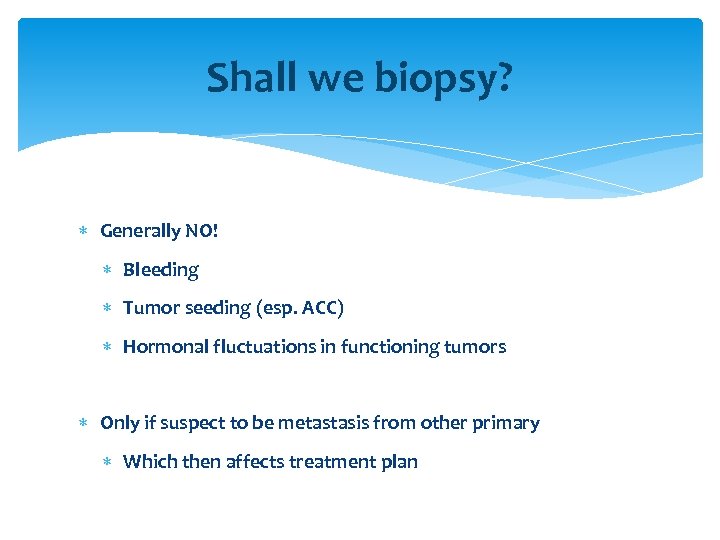 Shall we biopsy? Generally NO! Bleeding Tumor seeding (esp. ACC) Hormonal fluctuations in functioning tumors Only if suspect to be metastasis from other primary Which then affects treatment plan
Shall we biopsy? Generally NO! Bleeding Tumor seeding (esp. ACC) Hormonal fluctuations in functioning tumors Only if suspect to be metastasis from other primary Which then affects treatment plan
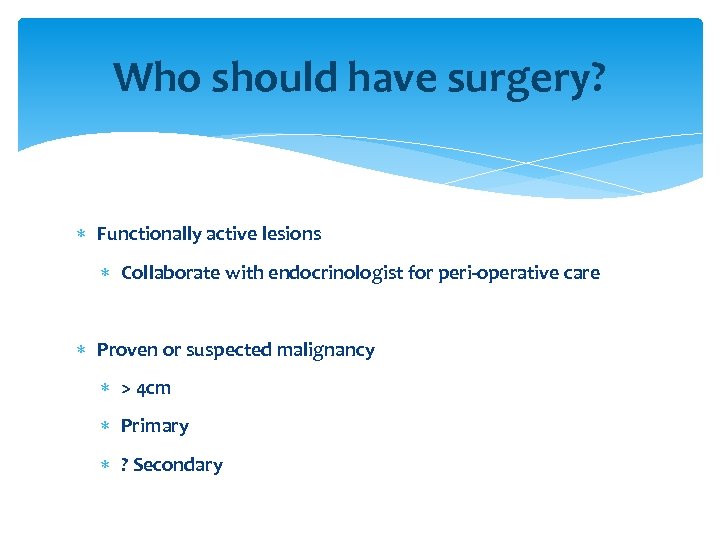 Who should have surgery? Functionally active lesions Collaborate with endocrinologist for peri-operative care Proven or suspected malignancy > 4 cm Primary ? Secondary
Who should have surgery? Functionally active lesions Collaborate with endocrinologist for peri-operative care Proven or suspected malignancy > 4 cm Primary ? Secondary
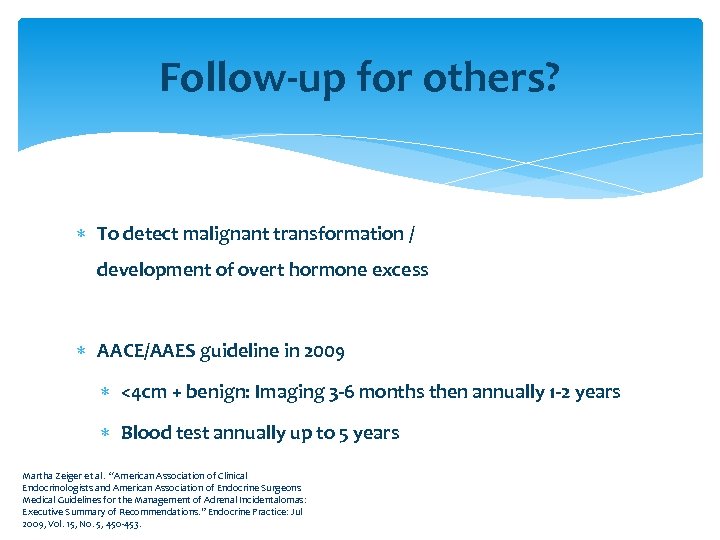 Follow-up for others? To detect malignant transformation / development of overt hormone excess AACE/AAES guideline in 2009 <4 cm + benign: Imaging 3 -6 months then annually 1 -2 years Blood test annually up to 5 years Martha Zeiger et al. “American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons Medical Guidelines for the Management of Adrenal Incidentalomas: Executive Summary of Recommendations. ” Endocrine Practice: Jul 2009, Vol. 15, No. 5, 450 -453.
Follow-up for others? To detect malignant transformation / development of overt hormone excess AACE/AAES guideline in 2009 <4 cm + benign: Imaging 3 -6 months then annually 1 -2 years Blood test annually up to 5 years Martha Zeiger et al. “American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons Medical Guidelines for the Management of Adrenal Incidentalomas: Executive Summary of Recommendations. ” Endocrine Practice: Jul 2009, Vol. 15, No. 5, 450 -453.
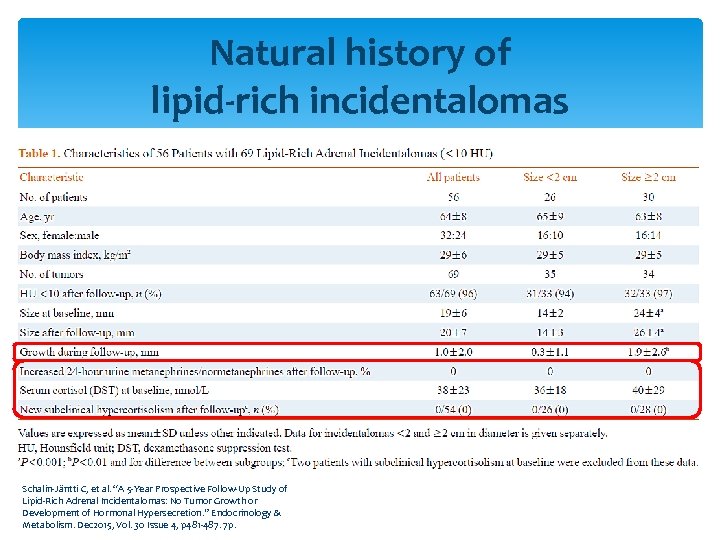 Natural history of lipid-rich incidentalomas Schalin-Jäntti C, et al. “A 5 -Year Prospective Follow-Up Study of Lipid-Rich Adrenal Incidentalomas: No Tumor Growth or Development of Hormonal Hypersecretion. ” Endocrinology & Metabolism. Dec 2015, Vol. 30 Issue 4, p 481 -487. 7 p.
Natural history of lipid-rich incidentalomas Schalin-Jäntti C, et al. “A 5 -Year Prospective Follow-Up Study of Lipid-Rich Adrenal Incidentalomas: No Tumor Growth or Development of Hormonal Hypersecretion. ” Endocrinology & Metabolism. Dec 2015, Vol. 30 Issue 4, p 481 -487. 7 p.
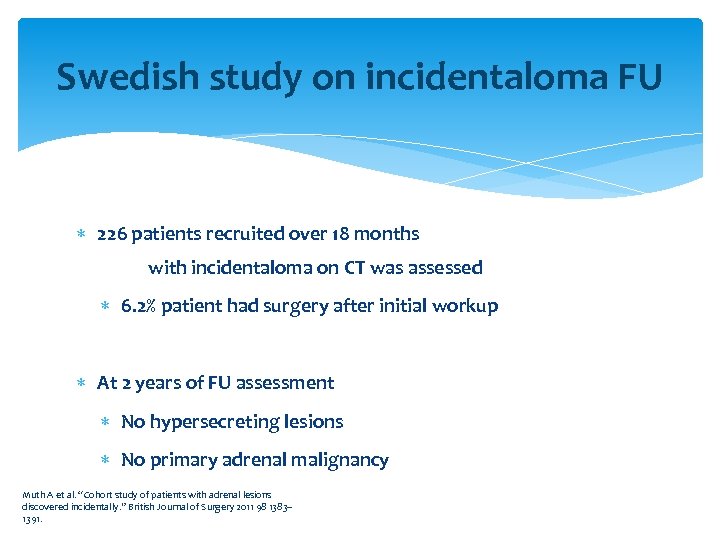 Swedish study on incidentaloma FU 226 patients recruited over 18 months with incidentaloma on CT was assessed 6. 2% patient had surgery after initial workup At 2 years of FU assessment No hypersecreting lesions No primary adrenal malignancy Muth A et al. “Cohort study of patients with adrenal lesions discovered incidentally. ” British Journal of Surgery 2011 98 1383– 1391.
Swedish study on incidentaloma FU 226 patients recruited over 18 months with incidentaloma on CT was assessed 6. 2% patient had surgery after initial workup At 2 years of FU assessment No hypersecreting lesions No primary adrenal malignancy Muth A et al. “Cohort study of patients with adrenal lesions discovered incidentally. ” British Journal of Surgery 2011 98 1383– 1391.
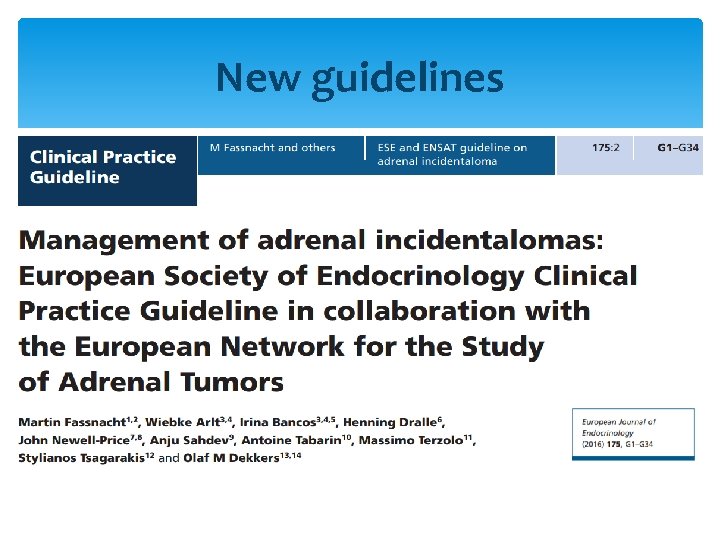 New guidelines
New guidelines
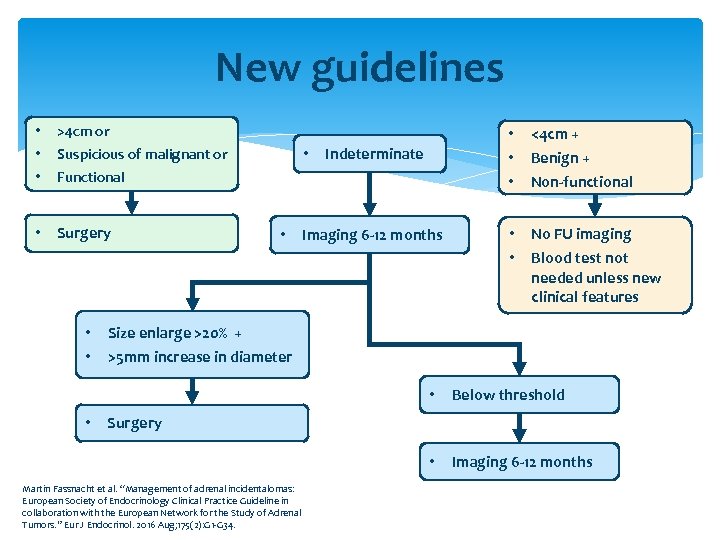 New guidelines • • • >4 cm or • Surgery • Suspicious of malignant or • • • Indeterminate Functional • • • Imaging 6 -12 months <4 cm + • • No FU imaging Benign + Non-functional Blood test not needed unless new clinical features Size enlarge >20% + >5 mm increase in diameter • • • Below threshold Imaging 6 -12 months Surgery Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
New guidelines • • • >4 cm or • Surgery • Suspicious of malignant or • • • Indeterminate Functional • • • Imaging 6 -12 months <4 cm + • • No FU imaging Benign + Non-functional Blood test not needed unless new clinical features Size enlarge >20% + >5 mm increase in diameter • • • Below threshold Imaging 6 -12 months Surgery Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
 Conclusion Adrenal incidentaloma is common. Both biochemical & specialized radiological investigations are mandatory. Contrast CT with measurement of washout is the preferred radiological investigation. Adrenal biopsy is usually not indicated. Functional lesions or lesions of size 4 cm or more should undergo surgery. Follow-up monitoring is necessary for indeterminate lesions.
Conclusion Adrenal incidentaloma is common. Both biochemical & specialized radiological investigations are mandatory. Contrast CT with measurement of washout is the preferred radiological investigation. Adrenal biopsy is usually not indicated. Functional lesions or lesions of size 4 cm or more should undergo surgery. Follow-up monitoring is necessary for indeterminate lesions.
 Thank you
Thank you
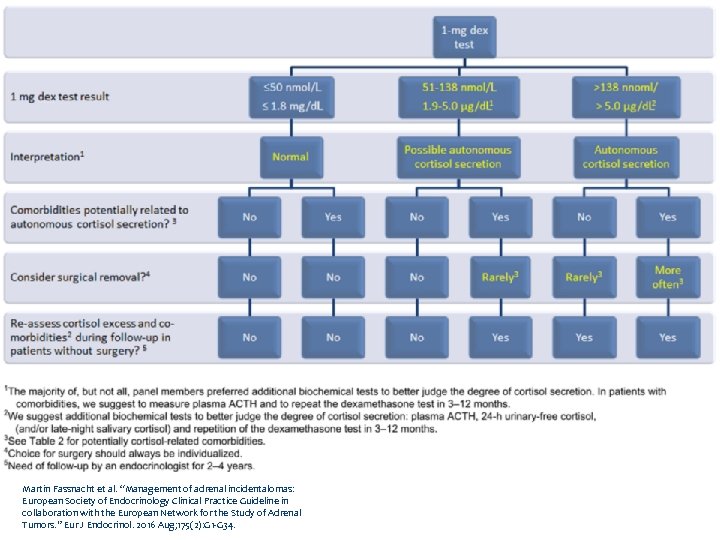
 New guidelines details
New guidelines details
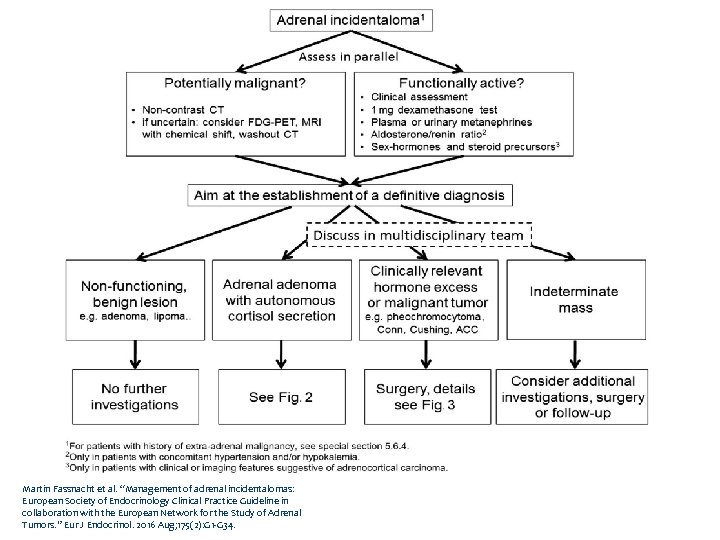 Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
 Flowchart Fig 2 Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
Flowchart Fig 2 Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
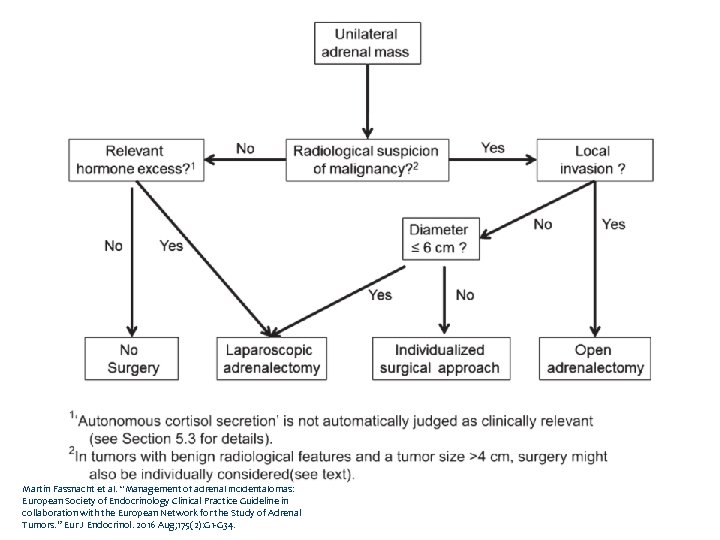 Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
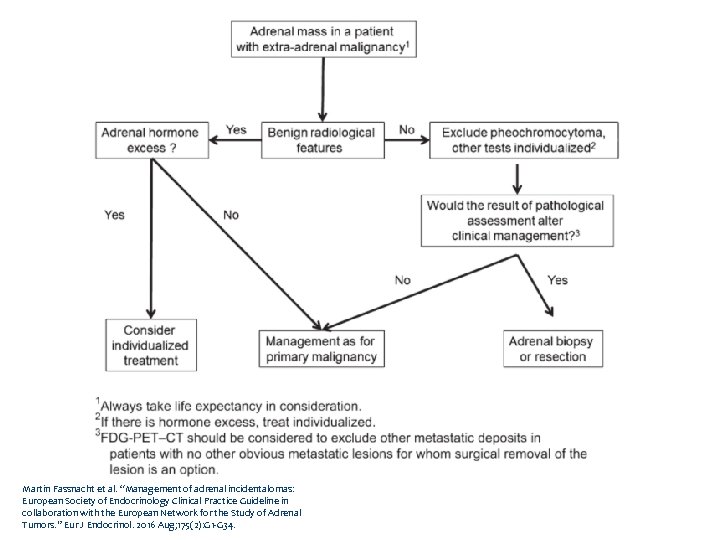 Flowchart Fig 4 Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
Flowchart Fig 4 Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34.
 Subclinical Hypercortisolism
Subclinical Hypercortisolism

 MRI Features
MRI Features
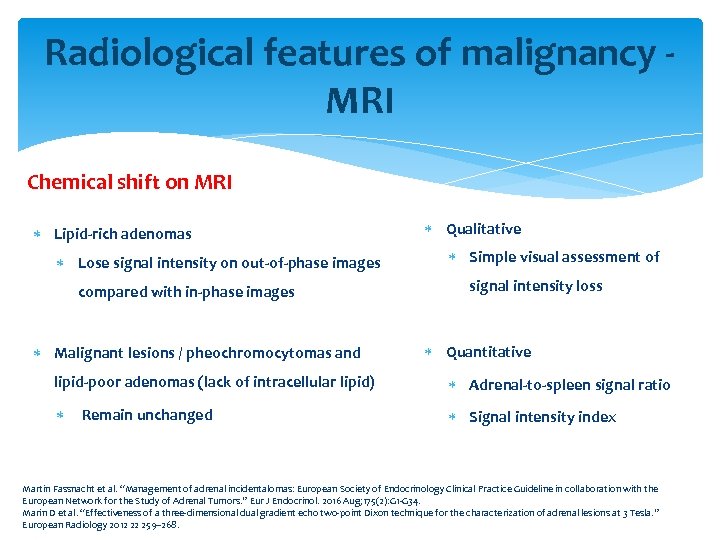 Radiological features of malignancy - MRI Chemical shift on MRI Lipid-rich adenomas Lose signal intensity on out-of-phase images compared with in-phase images Malignant lesions / pheochromocytomas and Qualitative Simple visual assessment of signal intensity loss Quantitative lipid-poor adenomas (lack of intracellular lipid) Adrenal-to-spleen signal ratio Remain unchanged Signal intensity index Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34. Marin D et al. “Effectiveness of a three-dimensional dual gradient echo two-point Dixon technique for the characterization of adrenal lesions at 3 Tesla. ” European Radiology 2012 22 259– 268.
Radiological features of malignancy - MRI Chemical shift on MRI Lipid-rich adenomas Lose signal intensity on out-of-phase images compared with in-phase images Malignant lesions / pheochromocytomas and Qualitative Simple visual assessment of signal intensity loss Quantitative lipid-poor adenomas (lack of intracellular lipid) Adrenal-to-spleen signal ratio Remain unchanged Signal intensity index Martin Fassnacht et al. “Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. ” Eur J Endocrinol. 2016 Aug; 175(2): G 1 -G 34. Marin D et al. “Effectiveness of a three-dimensional dual gradient echo two-point Dixon technique for the characterization of adrenal lesions at 3 Tesla. ” European Radiology 2012 22 259– 268.
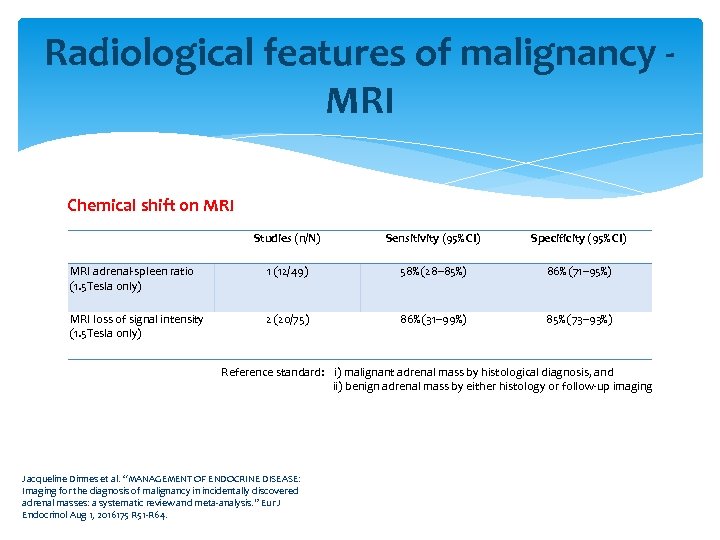 Radiological features of malignancy - MRI Chemical shift on MRI Studies (n/N) Sensitivity (95% CI) Specificity (95% CI) MRI adrenal-spleen ratio (1. 5 Tesla only) 1 (12/49) 58% (28– 85%) 86% (71– 95%) MRI loss of signal intensity (1. 5 Tesla only) 2 (20/75) 86% (31– 99%) 85% (73– 93%) Reference standard: i) malignant adrenal mass by histological diagnosis, and ii) benign adrenal mass by either histology or follow-up imaging Jacqueline Dinnes et al. “MANAGEMENT OF ENDOCRINE DISEASE: Imaging for the diagnosis of malignancy in incidentally discovered adrenal masses: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016175 R 51 -R 64.
Radiological features of malignancy - MRI Chemical shift on MRI Studies (n/N) Sensitivity (95% CI) Specificity (95% CI) MRI adrenal-spleen ratio (1. 5 Tesla only) 1 (12/49) 58% (28– 85%) 86% (71– 95%) MRI loss of signal intensity (1. 5 Tesla only) 2 (20/75) 86% (31– 99%) 85% (73– 93%) Reference standard: i) malignant adrenal mass by histological diagnosis, and ii) benign adrenal mass by either histology or follow-up imaging Jacqueline Dinnes et al. “MANAGEMENT OF ENDOCRINE DISEASE: Imaging for the diagnosis of malignancy in incidentally discovered adrenal masses: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016175 R 51 -R 64.
 Adrenal biopsy
Adrenal biopsy
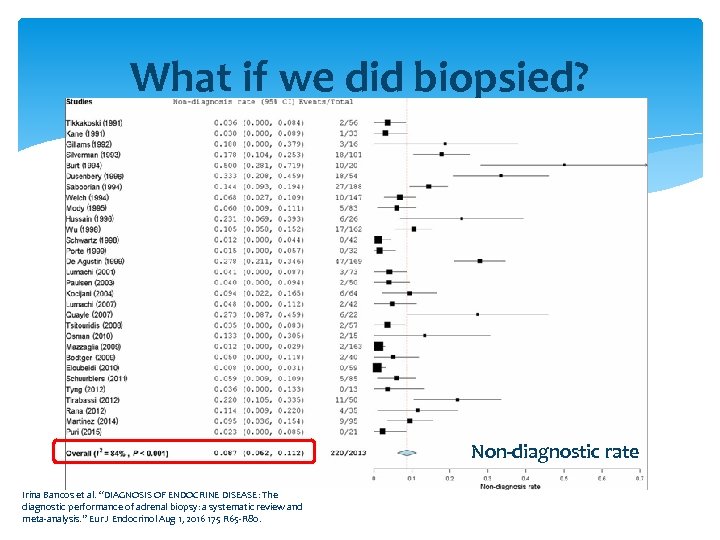 What if we did biopsied? Non-diagnostic rate Irina Bancos et al. “DIAGNOSIS OF ENDOCRINE DISEASE: The diagnostic performance of adrenal biopsy: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016 175 R 65 -R 80.
What if we did biopsied? Non-diagnostic rate Irina Bancos et al. “DIAGNOSIS OF ENDOCRINE DISEASE: The diagnostic performance of adrenal biopsy: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016 175 R 65 -R 80.
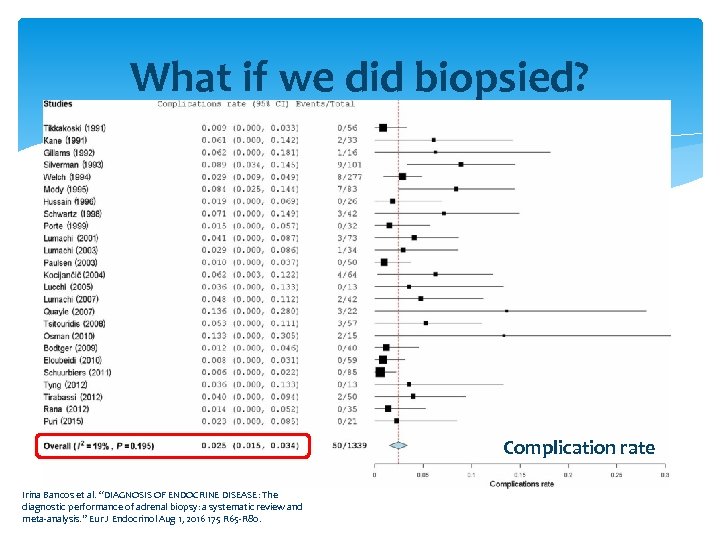 What if we did biopsied? Complication rate Irina Bancos et al. “DIAGNOSIS OF ENDOCRINE DISEASE: The diagnostic performance of adrenal biopsy: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016 175 R 65 -R 80.
What if we did biopsied? Complication rate Irina Bancos et al. “DIAGNOSIS OF ENDOCRINE DISEASE: The diagnostic performance of adrenal biopsy: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016 175 R 65 -R 80.
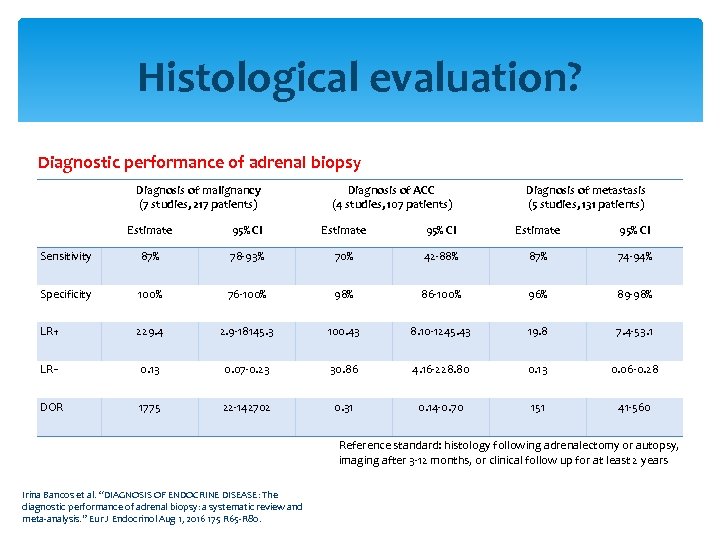 Histological evaluation? Diagnostic performance of adrenal biopsy Diagnosis of malignancy (7 studies, 217 patients) Diagnosis of ACC (4 studies, 107 patients) Diagnosis of metastasis (5 studies, 131 patients) Estimate 95% CI Sensitivity 87% 78 -93% 70% 42 -88% 87% 74 -94% Specificity 100% 76 -100% 98% 86 -100% 96% 89 -98% LR+ 229. 4 2. 9 -18145. 3 100. 43 8. 10 -1245. 43 19. 8 7. 4 -53. 1 LR− 0. 13 0. 07 -0. 23 30. 86 4. 16 -228. 80 0. 13 0. 06 -0. 28 DOR 1775 22 -142702 0. 31 0. 14 -0. 70 151 41 -560 Reference standard: histology following adrenalectomy or autopsy, imaging after 3 -12 months, or clinical follow up for at least 2 years Irina Bancos et al. “DIAGNOSIS OF ENDOCRINE DISEASE: The diagnostic performance of adrenal biopsy: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016 175 R 65 -R 80.
Histological evaluation? Diagnostic performance of adrenal biopsy Diagnosis of malignancy (7 studies, 217 patients) Diagnosis of ACC (4 studies, 107 patients) Diagnosis of metastasis (5 studies, 131 patients) Estimate 95% CI Sensitivity 87% 78 -93% 70% 42 -88% 87% 74 -94% Specificity 100% 76 -100% 98% 86 -100% 96% 89 -98% LR+ 229. 4 2. 9 -18145. 3 100. 43 8. 10 -1245. 43 19. 8 7. 4 -53. 1 LR− 0. 13 0. 07 -0. 23 30. 86 4. 16 -228. 80 0. 13 0. 06 -0. 28 DOR 1775 22 -142702 0. 31 0. 14 -0. 70 151 41 -560 Reference standard: histology following adrenalectomy or autopsy, imaging after 3 -12 months, or clinical follow up for at least 2 years Irina Bancos et al. “DIAGNOSIS OF ENDOCRINE DISEASE: The diagnostic performance of adrenal biopsy: a systematic review and meta-analysis. ” Eur J Endocrinol Aug 1, 2016 175 R 65 -R 80.
 Others
Others
 Clinical exam Look for history or symptoms of functioning lesions Signs of Cushing’s syndrome Any hypertension (+/- hypokalemia) Classic triad of phaeochromocytoma Headaches, palpitations and sweating Hirsuitism Look for history suggestive of familial disease or syndromes
Clinical exam Look for history or symptoms of functioning lesions Signs of Cushing’s syndrome Any hypertension (+/- hypokalemia) Classic triad of phaeochromocytoma Headaches, palpitations and sweating Hirsuitism Look for history suggestive of familial disease or syndromes
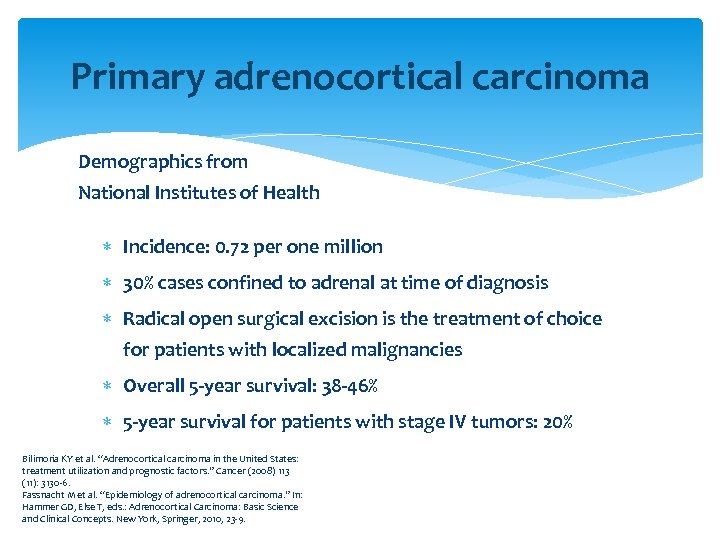 Primary adrenocortical carcinoma Demographics from National Institutes of Health Incidence: 0. 72 per one million 30% cases confined to adrenal at time of diagnosis Radical open surgical excision is the treatment of choice for patients with localized malignancies Overall 5 -year survival: 38 -46% 5 -year survival for patients with stage IV tumors: 20% Bilimoria KY et al. “Adrenocortical carcinoma in the United States: treatment utilization and prognostic factors. ” Cancer (2008) 113 (11): 3130 -6. Fassnacht M et al. “Epidemiology of adrenocortical carcinoma. ” In: Hammer GD, Else T, eds. : Adrenocortical Carcinoma: Basic Science and Clinical Concepts. New York, Springer, 2010, 23 -9.
Primary adrenocortical carcinoma Demographics from National Institutes of Health Incidence: 0. 72 per one million 30% cases confined to adrenal at time of diagnosis Radical open surgical excision is the treatment of choice for patients with localized malignancies Overall 5 -year survival: 38 -46% 5 -year survival for patients with stage IV tumors: 20% Bilimoria KY et al. “Adrenocortical carcinoma in the United States: treatment utilization and prognostic factors. ” Cancer (2008) 113 (11): 3130 -6. Fassnacht M et al. “Epidemiology of adrenocortical carcinoma. ” In: Hammer GD, Else T, eds. : Adrenocortical Carcinoma: Basic Science and Clinical Concepts. New York, Springer, 2010, 23 -9.
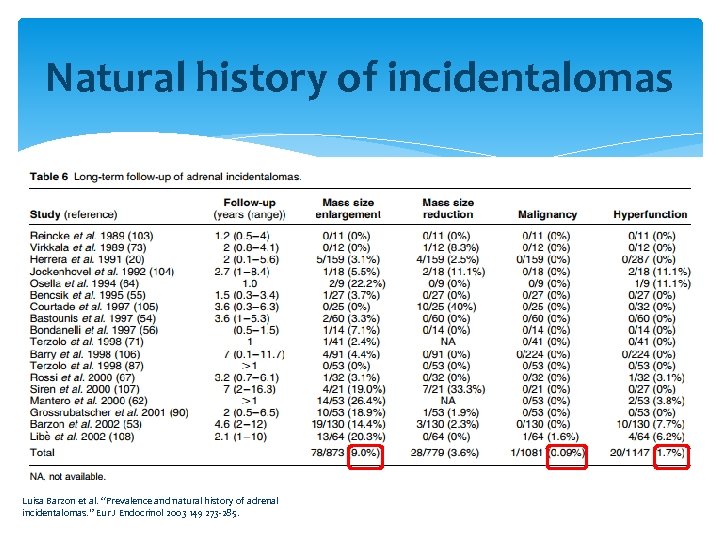 Natural history of incidentalomas Luisa Barzon et al. “Prevalence and natural history of adrenal incidentalomas. ” Eur J Endocrinol 2003 149 273 -285.
Natural history of incidentalomas Luisa Barzon et al. “Prevalence and natural history of adrenal incidentalomas. ” Eur J Endocrinol 2003 149 273 -285.
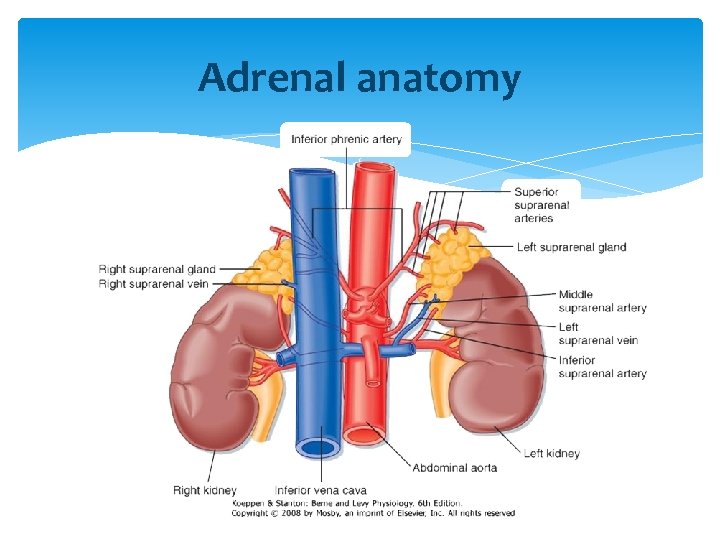 Adrenal anatomy
Adrenal anatomy


