f9cefb20aef818057a25c7b867ae3e29.ppt
- Количество слайдов: 48
Unexpected Problems in CDI: Managing CEOs, CFOs, CMOs, COOs, & CQOs Trey La Charité, MD, FACP Medical Director for Clinical Documentation Integrity and Coding
Objectives: 1. Review many unanticipated interdepartmental (mostly) problems that have effected or influenced UTMC’s CDI program: – Compliance – Human Resources – Medical Records – Performance Improvement – Revenue Cycle (including Denials Management) – Risk Management – And. . . Other More Esoteric Issues 2. Review mitigation strategies that were employed to address those problems
What you wish you knew. . . • Remember this? ☻“How would you like to run the hospital’s new CDI program? ” – “All you have to do is help the medical staff improve their documentation” – “It’s an opportunity to really make a positive impact on the hospital” – They heaped lots of praise on you for your other accomplishments – Maybe they offered you a raise, an extra stipend, change of scenery, time off from clinical responsibilities, a better parking space, etc. ? • And you fell it for it hook, line, and sinker!
Some things you expected. . . • Provider Push Back – “I don’t have time for this!” – “The way I see it, this only benefits the hospital. How does this help me? ” – “How does this help my patients? ” – “Everything that needs to be said about my patients is already in the chart!” – “It’s obviously already in the record. Why should I have to say it your way? ” – “Why are you reviewing my charts again? ” – “I didn’t say anything like that. Your coders got it wrong. . . again!” again
Some things you expected. . . • You were going to have to attend some more meetings (though it turned out to be a lot more than you ever possibly imagined) • You were going to have to routinely speak to groups of docs/NPs/PAs/residents and prepare Power. Point presentations • You were going to have to review a lot of charts • You were going to have to serve as this new program’s leader, shepherd, and “creative director” • But what about all of those other problems you just didn’t see coming. . .
Compliance Problems • PEPPER numbers will change! PEPPER (Program for Evaluating Payment Patterns Electronic Report) – Many categories will increase with your CDI efforts • • Number of medical DRGs with CC/MCC Number of surgical DRGs with CC/MCC Number of cases with “sepsis” as principal diagnosis Number of cases with single CC or MCC • Therefore. . . compliance officer may need a PPI, some Prozac, and a little hand-holding and ☻Remember! PEPPER should not matter if the documentation is solid and all diagnostic criteria is present
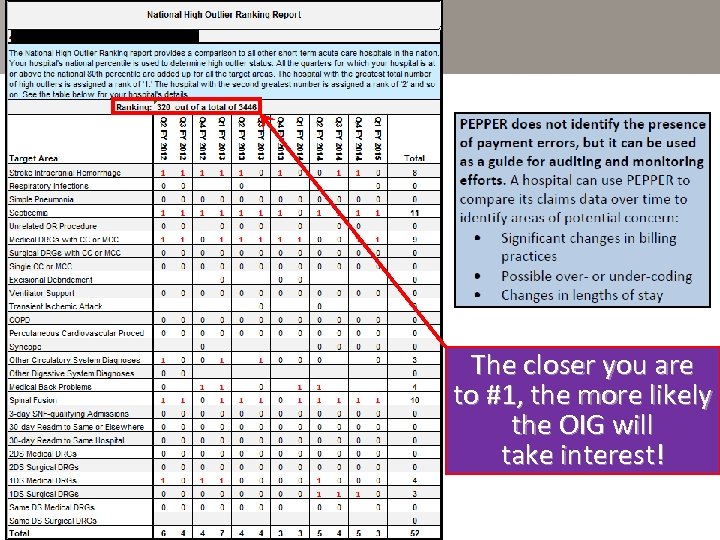
The closer you are to #1, the more likely the OIG will take interest!
More Compliance Problems • “Cloning” = repeatedly producing a “new note” Cloning that is exact duplication of previous day’s note on multiple, successive days – Daily progress note most common victim – Facilitated by Cut and Paste function of EHRs ‼ Huge potential fraud issue !! ? If cloning, is provider really providing a new service for which he/she can legally bill ? • Consider turning this function off (if able) or limiting the amount or sections of a note that can be copied forward LAuditors already attuned to this issue!
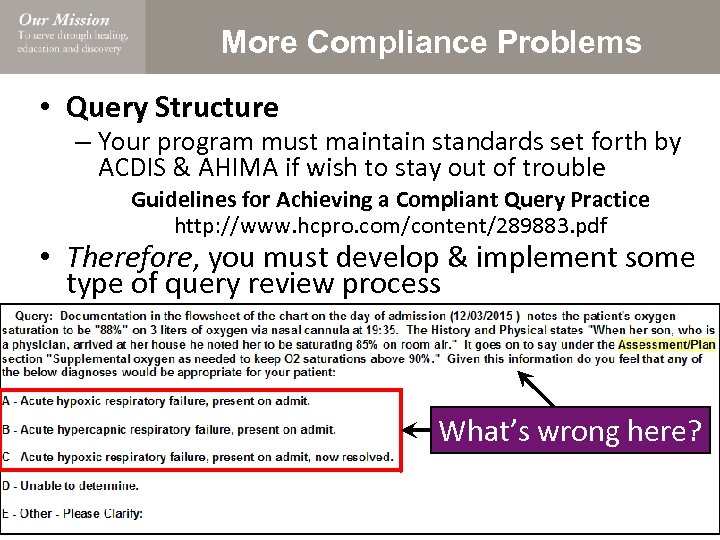
More Compliance Problems • Query Structure – Your program must maintain standards set forth by ACDIS & AHIMA if wish to stay out of trouble Guidelines for Achieving a Compliant Query Practice http: //www. hcpro. com/content/289883. pdf • Therefore, you must develop & implement some type of query review process What’s wrong here?
More Compliance Problems • What happens when the OIG does show up? LYou will be dragged into this! this • UTMC OIG experience: – OIG calls early 2015; says will come in 6 weeks • They state will give list of records to be reviewed 2 weeks before they arrive • Send list in late afternoon the Friday before the Monday they are scheduled to arrive – 2 auditors arrive: • • • One has done 3 hospital audits: the other has done 5 Neither of them have any clinical experience Neither of them have any coding experience One is a CFE First sentence was “we are just making sure you are Medicare compliant” with your billing practices LSecond sentence was “we will extrapolate”
More Compliance Problems • UTMC OIG results: – Reviewed 236 claims (117 IP, 119 OP) “strategically” selected based upon their data mining results – IP error rate so low, OIG unable to extrapolate! • Only 3 IP claims required adjustments for “overpayments” – OP error rate higher which did allow extrapolation ☻However, total OIG payback only $55, 164!! – Overall error rate for UTMC audit = 0. 0678% • OIG uses a 5% as benchmark error rate in establishing need for corrective action plan LCompliance officer taken off suicide precautions and promptly retired
More Compliance Problems • Service-line documentation template construction/review – “The ____ surgeons were hoping you could provide all of the ‘buzz words’ they need for their new pre-op H&P template. ” • Translation: They just want the CCs/MCCs listed that impact their SOI scores so they can circle them or put-an-X-in-the-box L Many people (still!) confuse our CDI role with E&M education & compliance maintenance – “Could you review this proposed new admission &/or consult template for ____ service-line? ” – “Could you show Dr. X how to improve his/her documentation to support his/her charge levels? ”
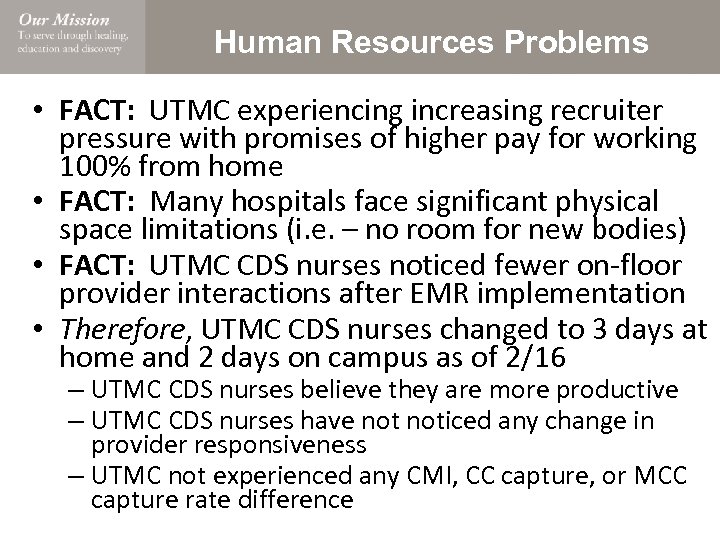
Human Resources Problems • FACT: UTMC experiencing increasing recruiter pressure with promises of higher pay for working 100% from home • FACT: Many hospitals face significant physical space limitations (i. e. – no room for new bodies) • FACT: UTMC CDS nurses noticed fewer on-floor provider interactions after EMR implementation • Therefore, UTMC CDS nurses changed to 3 days at home and 2 days on campus as of 2/16 – UTMC CDS nurses believe they are more productive – UTMC CDS nurses have noticed any change in provider responsiveness – UTMC not experienced any CMI, CC capture, or MCC capture rate difference
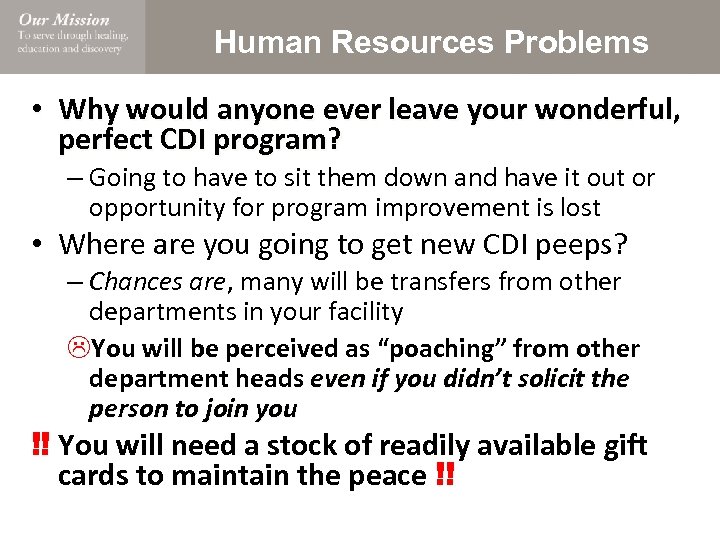
Human Resources Problems • Why would anyone ever leave your wonderful, perfect CDI program? – Going to have to sit them down and have it out or opportunity for program improvement is lost • Where are you going to get new CDI peeps? – Chances are, many will be transfers from other departments in your facility LYou will be perceived as “poaching” from other department heads even if you didn’t solicit the person to join you ‼ You will need a stock of readily available gift cards to maintain the peace !!
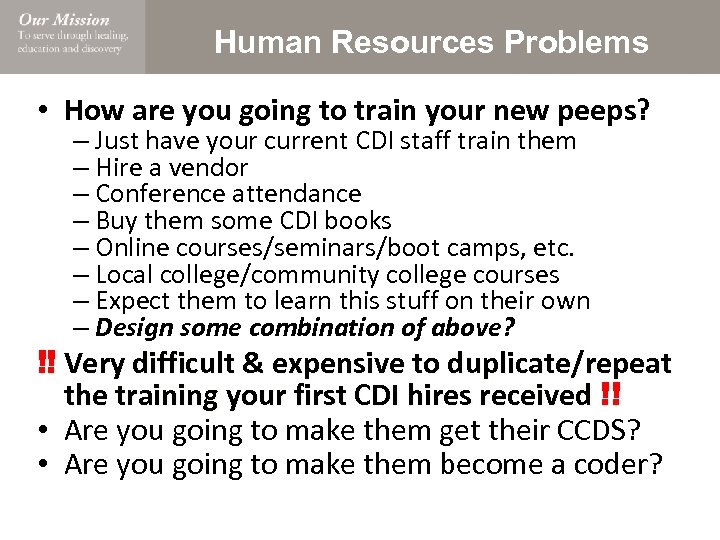
Human Resources Problems • How are you going to train your new peeps? – Just have your current CDI staff train them – Hire a vendor – Conference attendance – Buy them some CDI books – Online courses/seminars/boot camps, etc. – Local college/community college courses – Expect them to learn this stuff on their own – Design some combination of above? ‼ Very difficult & expensive to duplicate/repeat the training your first CDI hires received !! • Are you going to make them get their CCDS? • Are you going to make them become a coder?
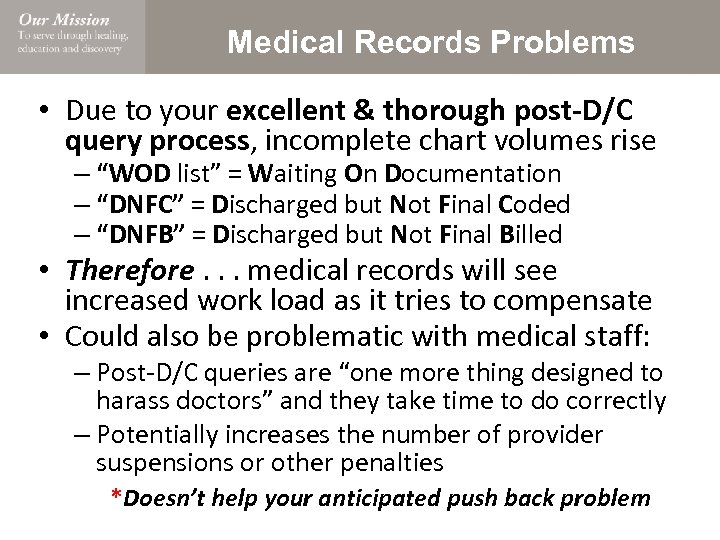
Medical Records Problems • Due to your excellent & thorough post-D/C query process, incomplete chart volumes rise – “WOD list” = Waiting On Documentation – “DNFC” = Discharged but Not Final Coded – “DNFB” = Discharged but Not Final Billed • Therefore. . . medical records will see increased work load as it tries to compensate • Could also be problematic with medical staff: – Post-D/C queries are “one more thing designed to harass doctors” and they take time to do correctly – Potentially increases the number of provider suspensions or other penalties *Doesn’t help your anticipated push back problem
Performance Improvement Problems • PI may see rates for some AHRQ Patient Safety Indicators (PSI) increase – Postoperative Hemorrhage or Hematoma (#9) – Postoperative Respiratory Failure (#11) – Postoperative Sepsis (#13) LTherefore. . . suggestion may be made to “adjust” CDI program focus to normalize these – While this decision is above your pay grade, you and your program are technically responsible ☻Be prepared to answer these challenges!! – Remember: These problems have arisen because of increased disease recognition, not because of increased disease prevalence
Performance Improvement Problems • However. . . CDI may also be approached by PI department to see if can help with other PSIs LYou just got a whole lot of new work!! • Ex: UTMC had higher than average PSI #2 rate (deaths in low-weighted DRGs) • Problem: Trauma Service taking significant hit in Multi-System Trauma (MST) DRGs when incorrect &/or low-weighted Principal Diagnosis chosen by coding – Coders generally do not have clinical knowledge &/or experience to discern what is most lifethreatening issue in an MST case – Coders also much happier when principal diagnosis & principle procedure are congruent
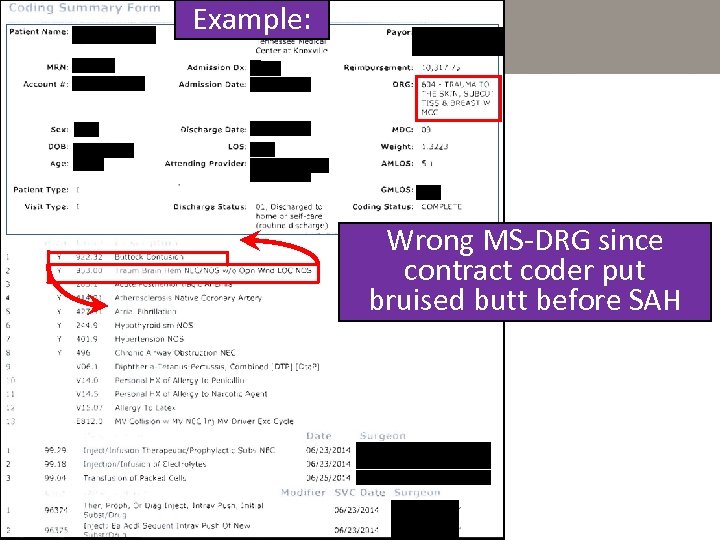
Example: Wrong MS-DRG since contract coder put bruised butt before SAH
UTMC Solution • FACT: “When multiple injuries exist, the code for the most severe injury as determined by the attending physician is sequenced first” -AHA Coding Clinic, 2 nd quarter, 1990 • CDI program developed MST Attestation Form: “I, _________, MD/DO am the attending physician for __________. This patient’s most significant, life threatening injury is_______________. ” ☻UTMC PSI#2 rate now below national average • And. . . added bonus of being auditor proof as RA can’t downgrade DRG by trying to change the principal diagnosis
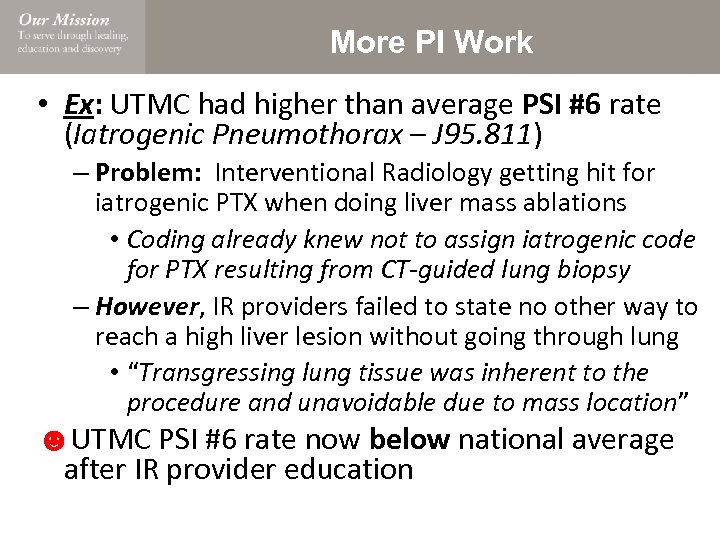
More PI Work • Ex: UTMC had higher than average PSI #6 rate (Iatrogenic Pneumothorax – J 95. 811) – Problem: Interventional Radiology getting hit for iatrogenic PTX when doing liver mass ablations • Coding already knew not to assign iatrogenic code for PTX resulting from CT-guided lung biopsy – However, IR providers failed to state no other way to reach a high liver lesion without going through lung • “Transgressing lung tissue was inherent to the procedure and unavoidable due to mass location” ☻UTMC PSI #6 rate now below national average after IR provider education
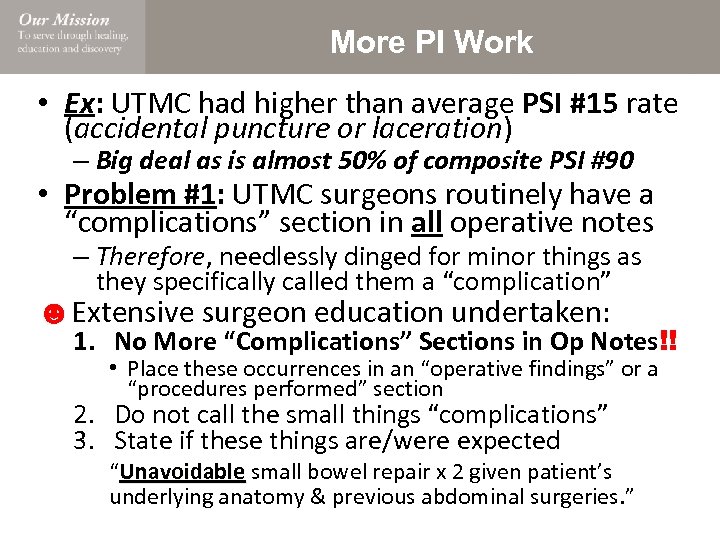
More PI Work • Ex: UTMC had higher than average PSI #15 rate (accidental puncture or laceration) – Big deal as is almost 50% of composite PSI #90 • Problem #1: UTMC surgeons routinely have a “complications” section in all operative notes – Therefore, needlessly dinged for minor things as they specifically called them a “complication” ☻Extensive surgeon education undertaken: 1. No More “Complications” Sections in Op Notes!! • Place these occurrences in an “operative findings” or a “procedures performed” section 2. Do not call the small things “complications” 3. State if these things are/were expected “Unavoidable small bowel repair x 2 given patient’s underlying anatomy & previous abdominal surgeries. ”
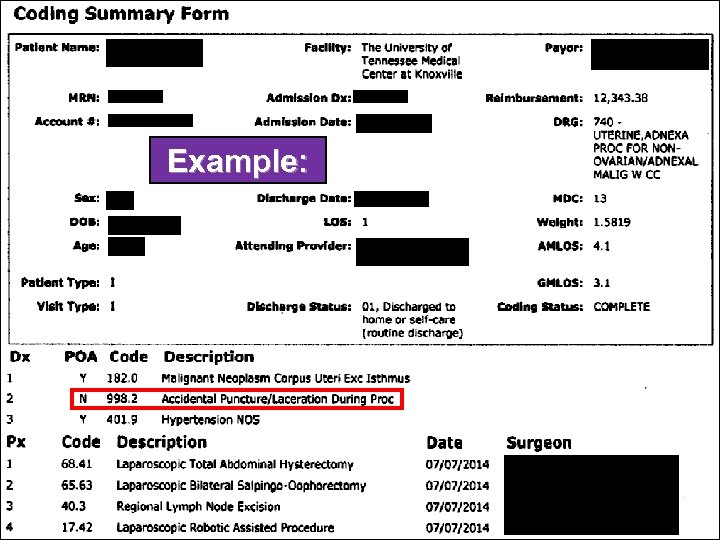
Example:
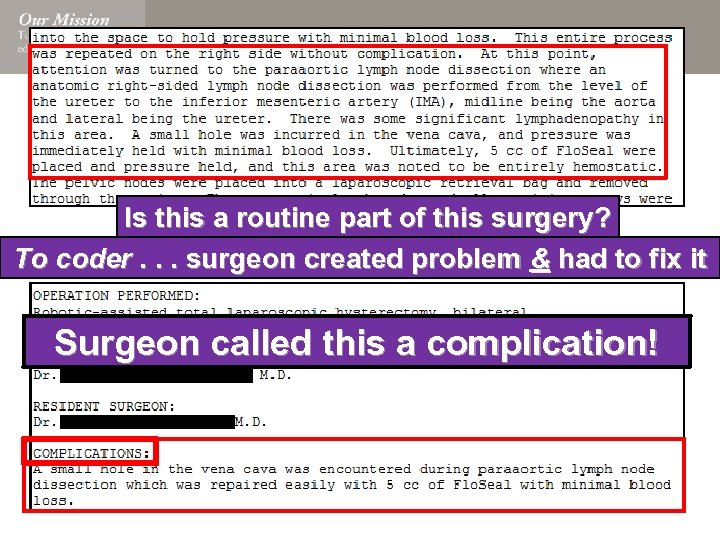
Is this a routine part of this surgery? To coder. . . surgeon created problem & had to fix it Surgeon called this a complication!
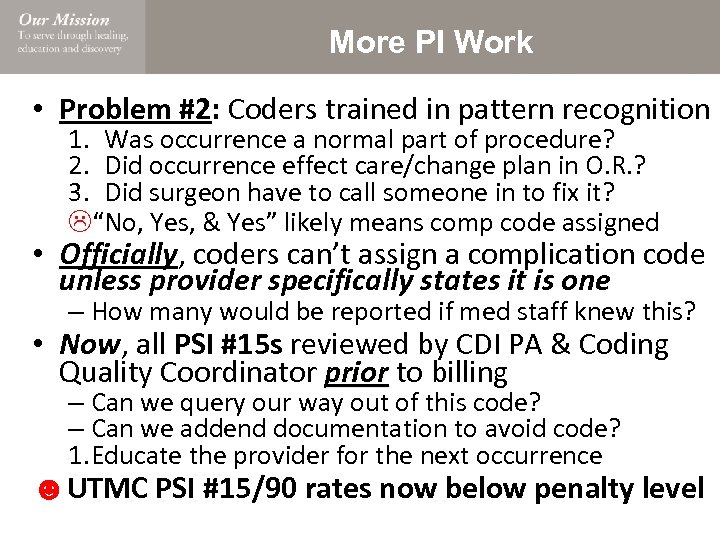
More PI Work • Problem #2: Coders trained in pattern recognition 1. Was occurrence a normal part of procedure? 2. Did occurrence effect care/change plan in O. R. ? 3. Did surgeon have to call someone in to fix it? L“No, Yes, & Yes” likely means comp code assigned • Officially, coders can’t assign a complication code unless provider specifically states it is one – How many would be reported if med staff knew this? • Now, all PSI #15 s reviewed by CDI PA & Coding Quality Coordinator prior to billing prior – Can we query our way out of this code? – Can we addend documentation to avoid code? 1. Educate the provider for the next occurrence ☻UTMC PSI #15/90 rates now below penalty level
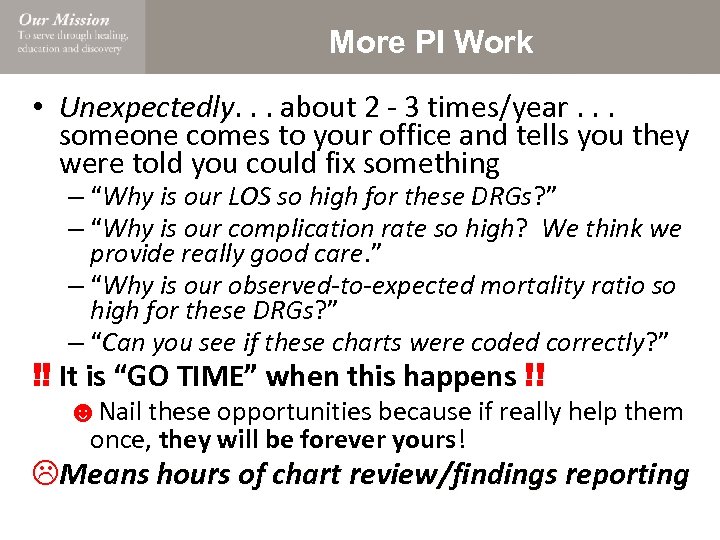
More PI Work • Unexpectedly. . . about 2 - 3 times/year. . . Unexpectedly someone comes to your office and tells you they were told you could fix something – “Why is our LOS so high for these DRGs? ” – “Why is our complication rate so high? We think we provide really good care. ” – “Why is our observed-to-expected mortality ratio so high for these DRGs? ” – “Can you see if these charts were coded correctly? ” ‼ It is “GO TIME” when this happens !! ☻Nail these opportunities because if really help them once, they will be forever yours! LMeans hours of chart review/findings reporting
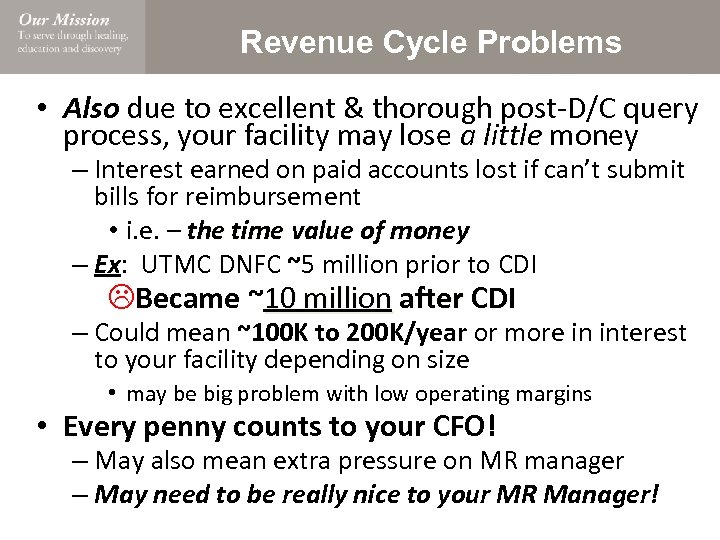
Revenue Cycle Problems • Also due to excellent & thorough post-D/C query process, your facility may lose a little money – Interest earned on paid accounts lost if can’t submit bills for reimbursement • i. e. – the time value of money – Ex: UTMC DNFC ~5 million prior to CDI LBecame ~10 million after CDI 10 million – Could mean ~100 K to 200 K/year or more in interest to your facility depending on size • may be big problem with low operating margins • Every penny counts to your CFO! – May also mean extra pressure on MR manager – May need to be really nice to your MR Manager!
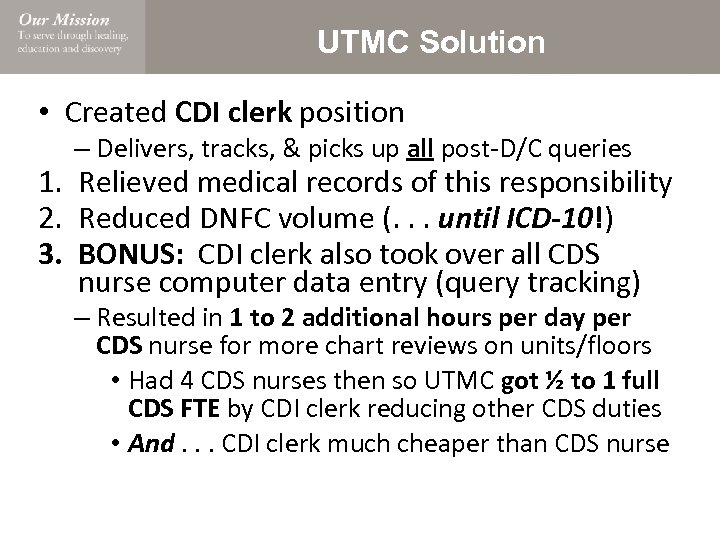
UTMC Solution • Created CDI clerk position – Delivers, tracks, & picks up all post-D/C queries 1. Relieved medical records of this responsibility 2. Reduced DNFC volume (. . . until ICD-10!) 3. BONUS: CDI clerk also took over all CDS nurse computer data entry (query tracking) – Resulted in 1 to 2 additional hours per day per CDS nurse for more chart reviews on units/floors • Had 4 CDS nurses then so UTMC got ½ to 1 full CDS FTE by CDI clerk reducing other CDS duties • And. . . CDI clerk much cheaper than CDS nurse
More Revenue Cycle Problems • Your CFO makes next year’s hospital budget based on the current year’s performance – CMI is a big part of that calculation! • What happens if/when next year’s CMI is actually less than predicted? . . . and your CFO has to explain that to the board • What happens if the 2, 3, or 4 year CMI trend is down (if only by 1 or 2 hundredths/year)? – You will be expected to provide answers – You and your CDI program may get reviewed by an outside consulting firm (. . . or 2, or 3, or. . . ) ‼ Maintaining CMI program success (i. e. – the CMI) may be the hardest part of job !!
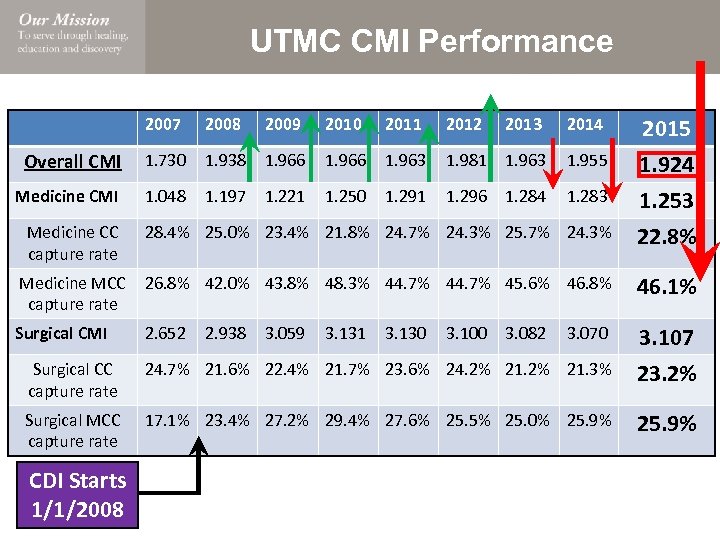
UTMC CMI Performance 2007 2008 2009 2010 2011 2012 2013 2014 2015 Overall CMI 1. 730 1. 938 1. 966 1. 963 1. 981 1. 963 1. 955 1. 924 Medicine CMI 1. 048 1. 197 1. 221 1. 250 1. 291 1. 296 1. 284 1. 283 1. 253 28. 4% 25. 0% 23. 4% 21. 8% 24. 7% 24. 3% 25. 7% 24. 3% 22. 8% Medicine MCC 26. 8% 42. 0% 43. 8% 48. 3% 44. 7% 45. 6% 46. 8% capture rate 46. 1% Surgical CMI 3. 070 3. 107 Surgical CC capture rate 24. 7% 21. 6% 22. 4% 21. 7% 23. 6% 24. 2% 21. 3% 23. 2% Surgical MCC capture rate 17. 1% 23. 4% 27. 2% 29. 4% 27. 6% 25. 5% 25. 0% 25. 9% Medicine CC capture rate CDI Starts 1/1/2008 2. 652 2. 938 3. 059 3. 131 3. 130 3. 100 3. 082
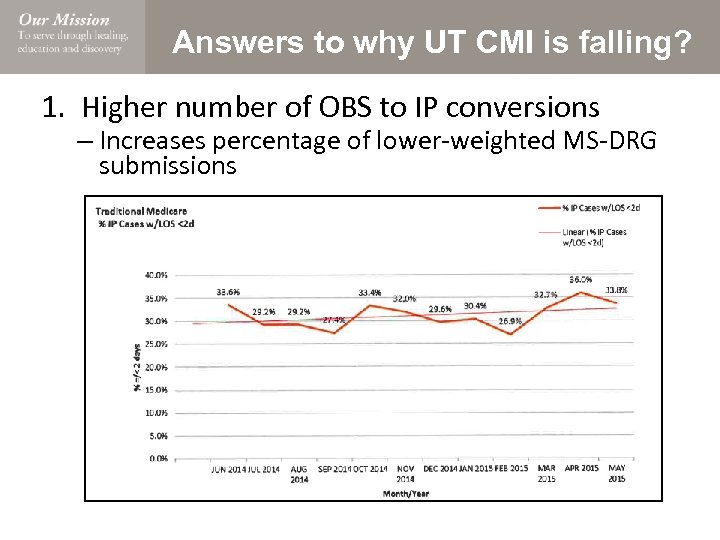
Answers to why UT CMI is falling? 1. Higher number of OBS to IP conversions – Increases percentage of lower-weighted MS-DRG submissions
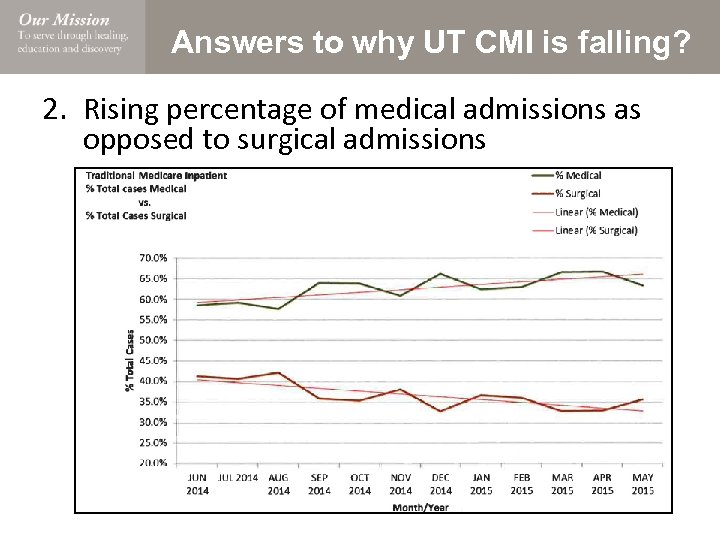
Answers to why UT CMI is falling? 2. Rising percentage of medical admissions as opposed to surgical admissions
Answers to why UT CMI is falling? 3. Hospital kept expanding but did not add new CDS nurses at compensatory rate – Started 2008 with 3 CDS nurses for 475 licensed beds – Granted 4 rth CDS nurse in 2010 to expand reviews to all MS-DRG payers – When (Finally!) granted 3 additional new CDS nurse hires 3 rd qtr. 2015, UTMC at 625 licensed beds – Planning to build another 90 beds in next 2 years 4. Hired lots of new surgeons who only do scheduled operations on stable patients – They don’t take patients with MCCs to the O. R. – Results in lower percentage of emergent IP surgeries – Surgical MCCs count way more than medical MCCs
Answers to why UT CMI is falling? 5. Most UTMC attendings hired in last 5 years have not had formal CDI training not – Readdressed multiple times without improvement – Made “mandatory” part of credentialing/recredentialing process without improvement – Suggestions? 6. CDI PA unable to implement new initiatives due to time taken for other hospital assignments * Note to CDI leaders: Avoid other areas of hospital management that might. . . 1. Negatively impact your CDI efforts 2. Reduce amount of time available for CDI program
More Revenue Cycle Problems LDenials Management!! – Did anyone ever mention writing appeal letters would be part of your responsibilities? – How much time does denials management consume from your normal CDI responsibilities? – How many new policies/procedures have you enacted solely to reduce your auditor exposure? – Can you believe the !$&@*#^%! the recovery auditors try to get away with? – Why can’t anyone in the C-suite put a stop to these blatant cases of Theft by Deception? LUgh!!
More Revenue Cycle Problems ‼ Remember: It is significantly easier and infinitely easier and cheaper to prevent a denial than it is to fight through the appeals process !! – Ex: UTMC cost to appeal one DRG-validation denial: • Redetermination/First level – 1. 5 to 3 hours for appeal formulation (CDI PA & Coding Quality Coordinator) and actually crafting the letter and • Second level – 1 to 2 hours for same things • Third level – 1 to 2 hours for same things • ALJ (if Medicare) – Can’t even imagine! LWhat if you get 5 to 10 denials a week?
Risk Management Problems • FACT: Not every doctor was created equally and not every service-line provides enough NP, PA, or resident supervision LEvery once in a while. . . your clinically experienced CDI peeps will discover undesired gaps in the quality of care provided at your facility – If you are the program’s leader, they will bring these cases to your attention – Figure out how your Risk Management Department wants to be contacted • Hint: They don’t like e-mail! • What does the “e” stand for? Evidence!
Terminology/Dz. Criteria Changes • Fact: Disease definitions, classification systems, and diagnostic criteria are rarely stagnant! stagnant – However, ICD system very slow in creating equivalent/corresponding codes in response – Recovery auditors very quick to jump on any criteria change that might increase their denial rate LHow do you tell your colleagues not to use what their representative professional societies recommend? • These situations require significant education efforts and plenty of patience – Must show them the actual current ICD codes – Must show the negative impacts of new terminology or criteria implementation without supporting codes
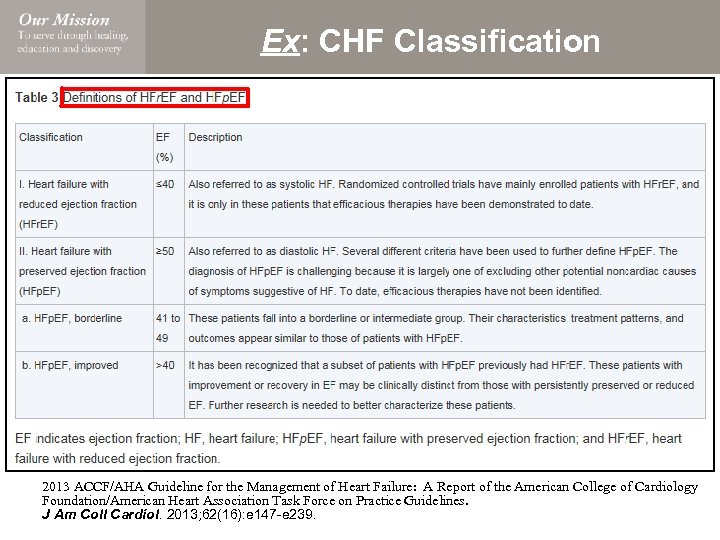
Ex: CHF Classification 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; 62(16): e 147 -e 239.
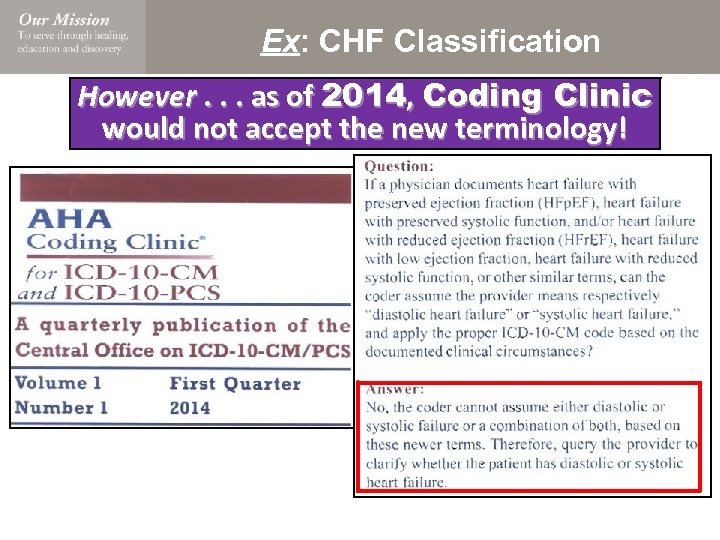
Ex: CHF Classification However. . . as of 2014, Coding Clinic would not accept the new terminology!
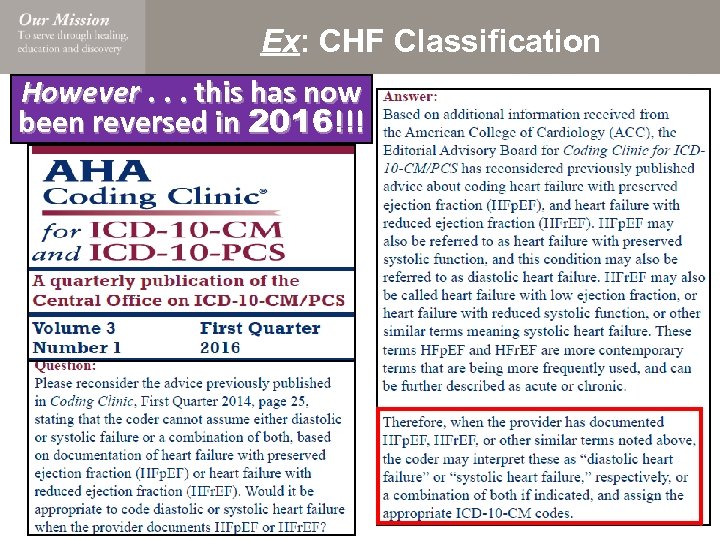
Ex: CHF Classification However. . . this has now been reversed in 2016!!!
Ex: New Sepsis Definition - 2016 Stay Tuned!
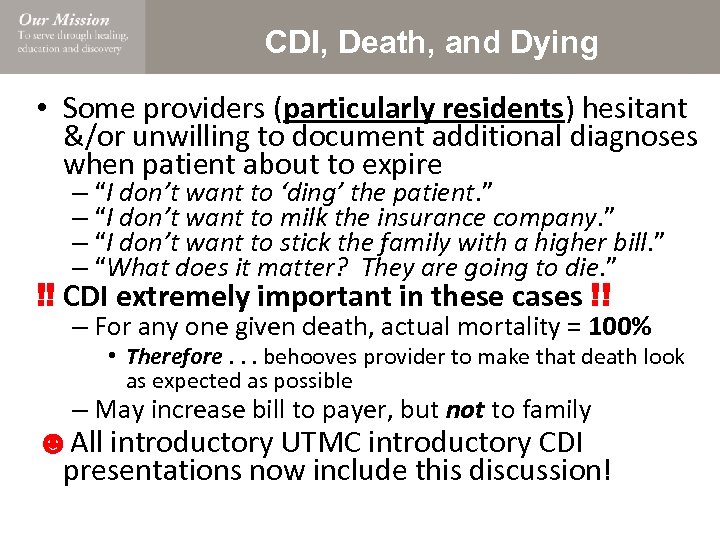
CDI, Death, and Dying • Some providers (particularly residents) hesitant &/or unwilling to document additional diagnoses when patient about to expire – “I don’t want to ‘ding’ the patient. ” – “I don’t want to milk the insurance company. ” – “I don’t want to stick the family with a higher bill. ” – “What does it matter? They are going to die. ” ‼ CDI extremely important in these cases !! – For any one given death, actual mortality = 100% • Therefore. . . behooves provider to make that death look as expected as possible – May increase bill to payer, but not to family ☻All introductory UTMC introductory CDI presentations now include this discussion!
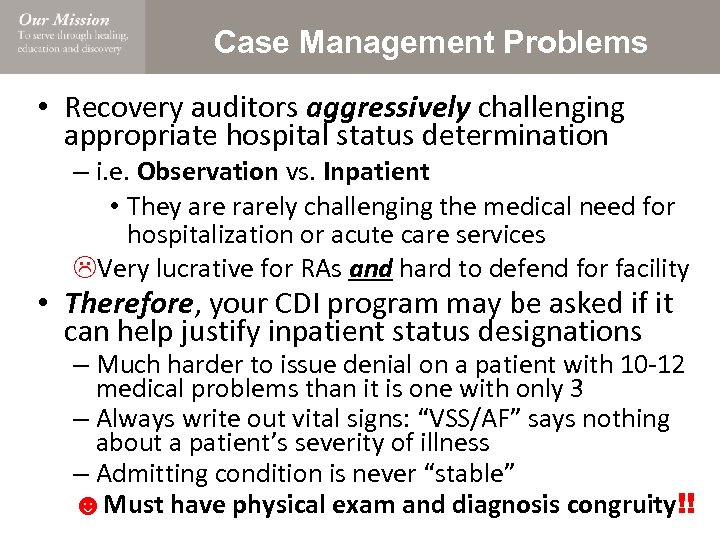
Case Management Problems • Recovery auditors aggressively challenging appropriate hospital status determination – i. e. Observation vs. Inpatient Observation • They are rarely challenging the medical need for hospitalization or acute care services LVery lucrative for RAs and hard to defend for facility • Therefore, your CDI program may be asked if it can help justify inpatient status designations – Much harder to issue denial on a patient with 10 -12 medical problems than it is one with only 3 – Always write out vital signs: “VSS/AF” says nothing about a patient’s severity of illness – Admitting condition is never “stable” ☻Must have physical exam and diagnosis congruity!!
Information Systems Problems • Increased recovery auditor liability inadvertently created with advent of EMR • Problem: Documented diagnoses may become incongruent with physical exam findings Ex: Provider says patient has “acute respiratory failure” in the assessment and plan – However, the physical exam section says: • GEN: A & O x 4; in no acute distress • Lungs: CTA Bilaterally w/out wheezes, rhonchi, or rales; respirations are unlabored LBusy provider did not change their pre-populated physical exam template in their EMR note ‼ The auditors have figured this one out !! – Must educate/re-educate all of your providers

Information Systems Problems • Many CDI program daily needs & proposed fixes start with proposed techonologcial solution – How much free time does your IS department have? LConstantly requesting IT changes that require IS resources may cause IS relationship to degrade – Query form structure and delivery – Query tracking tool development/improvements – Structure/delivery of CDI peeps’ daily work lists – Extended OBS case notifications to CDS nurses – Disease documentation templates – Pre-bill holds for chart review – Denial/Appeal tracking ‼ You will need a stock of readily available bribes. . . uh. . . gift cards to get stuff done !!
Summary • The lessons to be learned? ‼ No CDI program operates in a vacuum !! – Everything we do in CDI has implications somewhere else within our hospital system – And. . . as the success/impact of your CDI program grows and expands, the more of these potential problems with surface – Will have to become skilled negotiator to safely navigate many of these issues – Will have to learn to occasionally settle for less than you were hoping to receive in return ☻CDI remains a very rewarding endeavor (but it is not without its share of trials) trials
Questions?
f9cefb20aef818057a25c7b867ae3e29.ppt