0cced713aeb29fee6f4563d84fb46f1c.ppt
- Количество слайдов: 53
 Understanding the Patient Journey Process Mapping and Value Stream / Flow Analysis
Understanding the Patient Journey Process Mapping and Value Stream / Flow Analysis
 Some context ‘ 80% of the problem is in the system not the people’ Deming We design in the system capability
Some context ‘ 80% of the problem is in the system not the people’ Deming We design in the system capability
 Why do Process Mapping?
Why do Process Mapping?
 Process Mapping • Views the system from the patient perspective following their journey across organisational boundaries • Helps staff understand how complex and confusing processes are • Diagnostic and used as a basis for redesign, actively involving frontline staff in the process
Process Mapping • Views the system from the patient perspective following their journey across organisational boundaries • Helps staff understand how complex and confusing processes are • Diagnostic and used as a basis for redesign, actively involving frontline staff in the process
 Looking at patient processes • 30 - 70% of work doesn’t add value for patient • up to 50% of process steps involve a ‘hand-off’, leading to error, duplication or delay • no one is accountable for the patient’s ‘end to end’ experience • job roles tend to be narrow and fragmented
Looking at patient processes • 30 - 70% of work doesn’t add value for patient • up to 50% of process steps involve a ‘hand-off’, leading to error, duplication or delay • no one is accountable for the patient’s ‘end to end’ experience • job roles tend to be narrow and fragmented
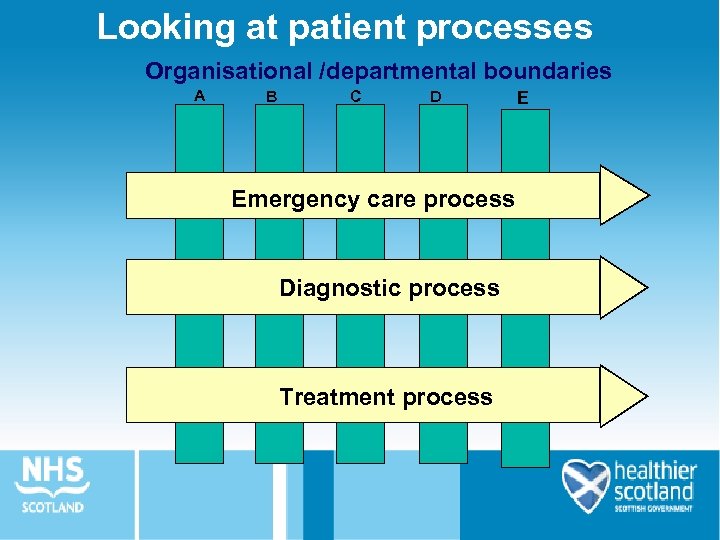 Looking at patient processes Organisational /departmental boundaries A B C D Emergency care process Diagnostic process Treatment process E
Looking at patient processes Organisational /departmental boundaries A B C D Emergency care process Diagnostic process Treatment process E
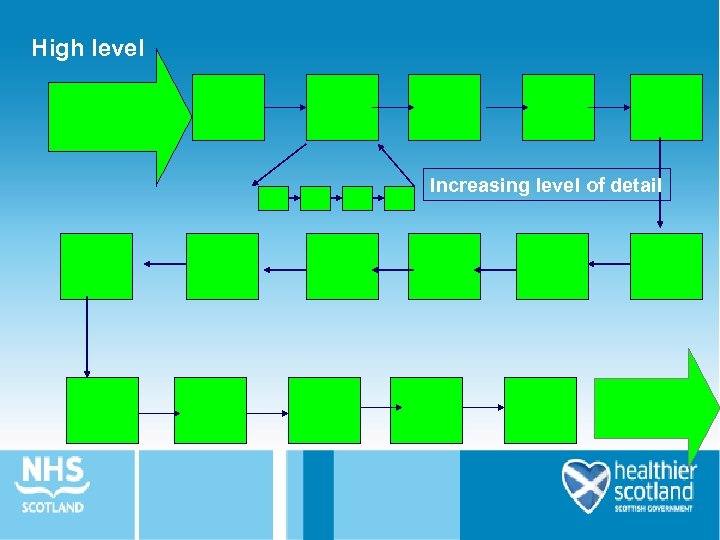 High level Increasing level of detail
High level Increasing level of detail
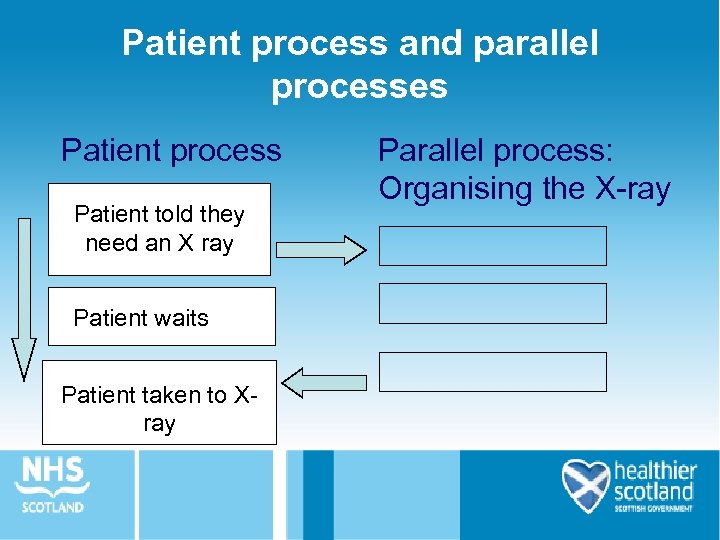 Patient process and parallel processes Patient process Patient told they need an X ray Patient waits Patient taken to Xray Parallel process: Organising the X-ray
Patient process and parallel processes Patient process Patient told they need an X ray Patient waits Patient taken to Xray Parallel process: Organising the X-ray
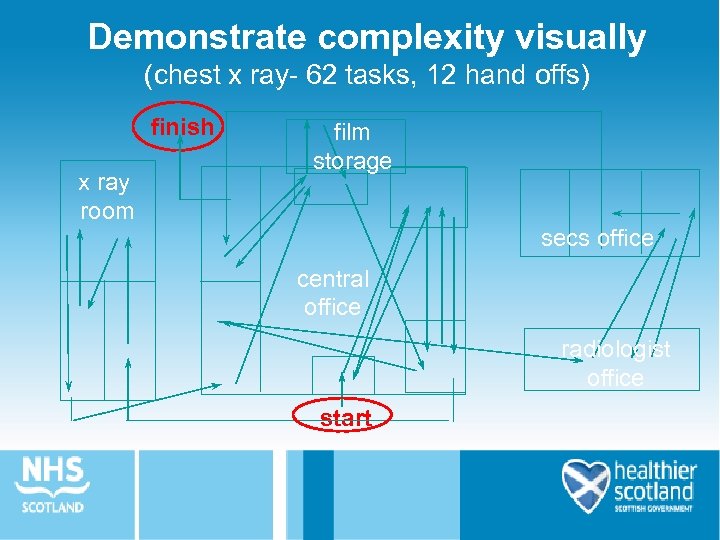 Demonstrate complexity visually (chest x ray- 62 tasks, 12 hand offs) finish x ray room film storage secs office central office radiologist office start
Demonstrate complexity visually (chest x ray- 62 tasks, 12 hand offs) finish x ray room film storage secs office central office radiologist office start
 Remember the following. . . • Define where the process starts and ends • Consider who you would involve in the mapping exercise • Use post-its to record the activities including time • Assemble the post-its to create the journey (remembering that some activities happen in parallel) • Keep a note of issues and opportunities
Remember the following. . . • Define where the process starts and ends • Consider who you would involve in the mapping exercise • Use post-its to record the activities including time • Assemble the post-its to create the journey (remembering that some activities happen in parallel) • Keep a note of issues and opportunities
 Analysing the Map • • How many steps in your process? How many duplications? How many hand-offs? What is the approx. time of, or between, each step? Where are possible delays? Where are major bottlenecks? How many steps do not ‘add value’ for patient? Where are the problems for patients and staff?
Analysing the Map • • How many steps in your process? How many duplications? How many hand-offs? What is the approx. time of, or between, each step? Where are possible delays? Where are major bottlenecks? How many steps do not ‘add value’ for patient? Where are the problems for patients and staff?
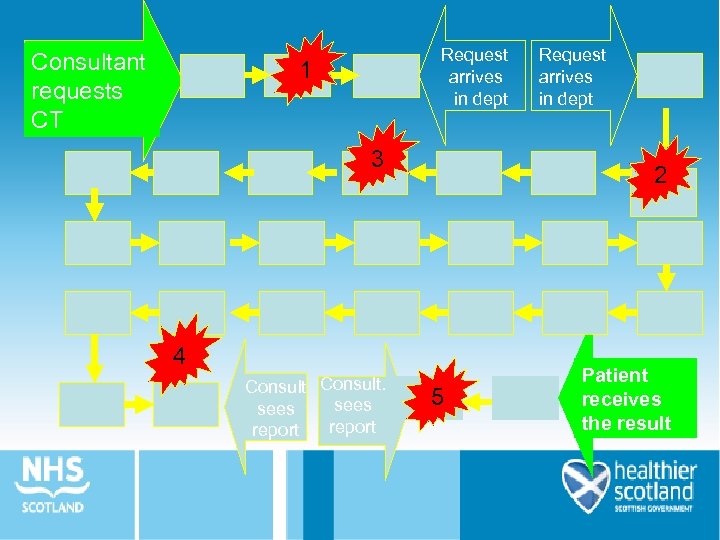 Consultant requests CT Request arrives in dept 1 3 2 4 Consult. sees report Request arrives in dept 5 Patient receives the result
Consultant requests CT Request arrives in dept 1 3 2 4 Consult. sees report Request arrives in dept 5 Patient receives the result
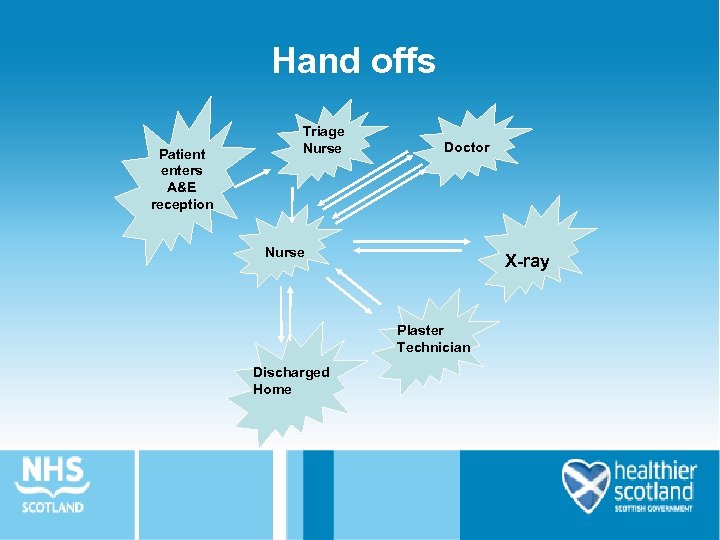 Hand offs Patient enters A&E reception Triage Nurse Doctor Nurse X-ray Plaster Technician Discharged Home
Hand offs Patient enters A&E reception Triage Nurse Doctor Nurse X-ray Plaster Technician Discharged Home
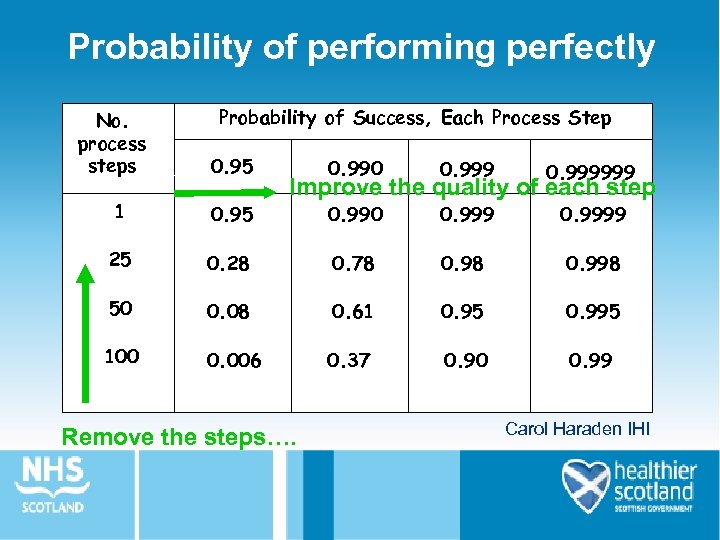 Probability of performing perfectly No. process steps Probability of Success, Each Process Step 0. 95 0. 990 0. 999999 Improve the quality of each step 1 0. 95 0. 990 0. 9999 25 0. 28 0. 78 0. 998 50 0. 08 0. 61 0. 95 0. 995 100 0. 006 0. 37 0. 90 0. 99 Remove the steps…. Carol Haraden IHI
Probability of performing perfectly No. process steps Probability of Success, Each Process Step 0. 95 0. 990 0. 999999 Improve the quality of each step 1 0. 95 0. 990 0. 9999 25 0. 28 0. 78 0. 998 50 0. 08 0. 61 0. 95 0. 995 100 0. 006 0. 37 0. 90 0. 99 Remove the steps…. Carol Haraden IHI
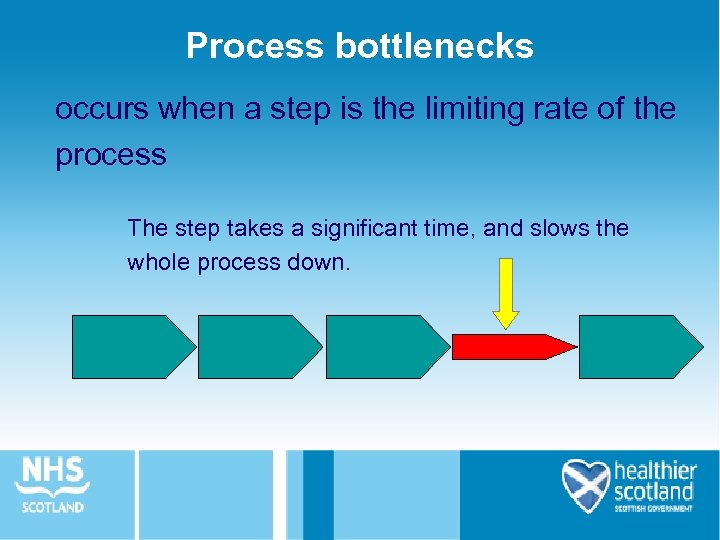 Process bottlenecks occurs when a step is the limiting rate of the process The step takes a significant time, and slows the whole process down.
Process bottlenecks occurs when a step is the limiting rate of the process The step takes a significant time, and slows the whole process down.
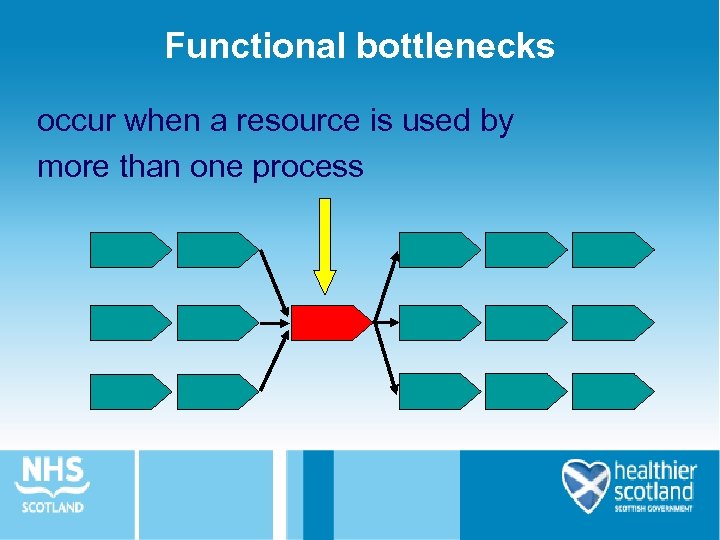 Functional bottlenecks occur when a resource is used by more than one process
Functional bottlenecks occur when a resource is used by more than one process
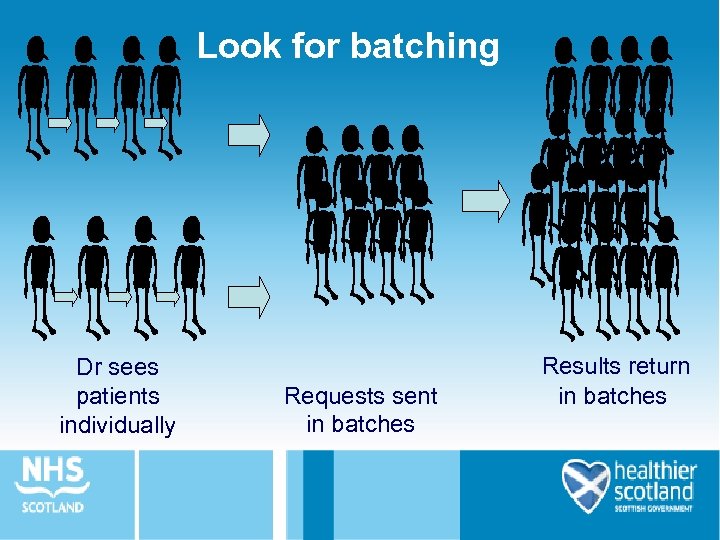 Look for batching Dr sees patients individually Requests sent in batches Results return in batches
Look for batching Dr sees patients individually Requests sent in batches Results return in batches
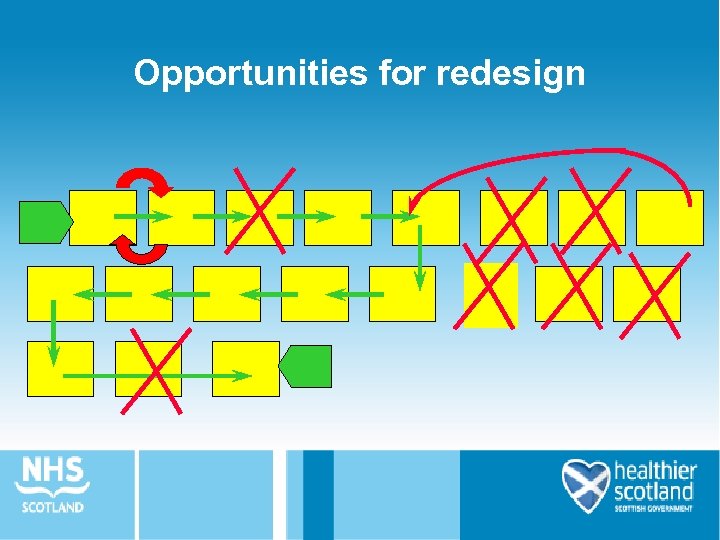 Opportunities for redesign
Opportunities for redesign
 When undertaking a Process Mapping session think about… • Scope - where does the process start and where does it end? • Who to involve in the mapping exercise? • Decide the level of detail
When undertaking a Process Mapping session think about… • Scope - where does the process start and where does it end? • Who to involve in the mapping exercise? • Decide the level of detail
 • High level process map - 6 -12 steps – generate in set time e. g. 20 minutes – use to establish scope and identify problems – no rework loops and minimum complexity • Detailed process map - dozens of steps – to establish loops and complexity – good to establish roles and relationships within process – use again in later phase to effect show of redesign
• High level process map - 6 -12 steps – generate in set time e. g. 20 minutes – use to establish scope and identify problems – no rework loops and minimum complexity • Detailed process map - dozens of steps – to establish loops and complexity – good to establish roles and relationships within process – use again in later phase to effect show of redesign
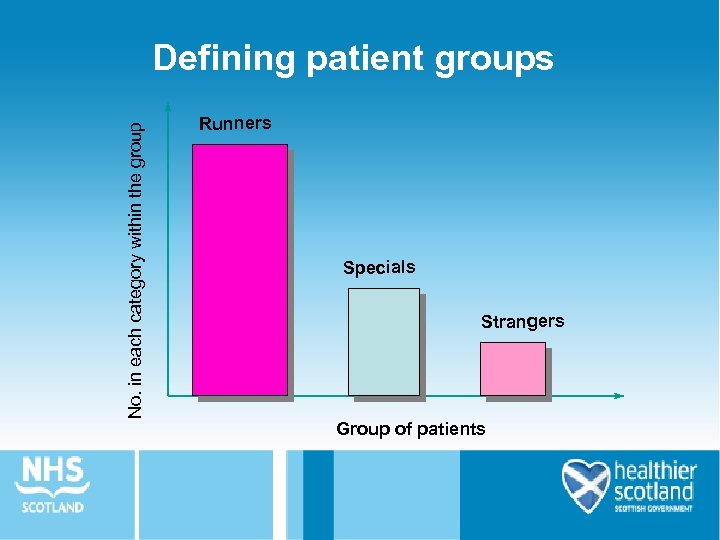 No. in each category within the group Defining patient groups Runners Specials Strangers Group of patients
No. in each category within the group Defining patient groups Runners Specials Strangers Group of patients
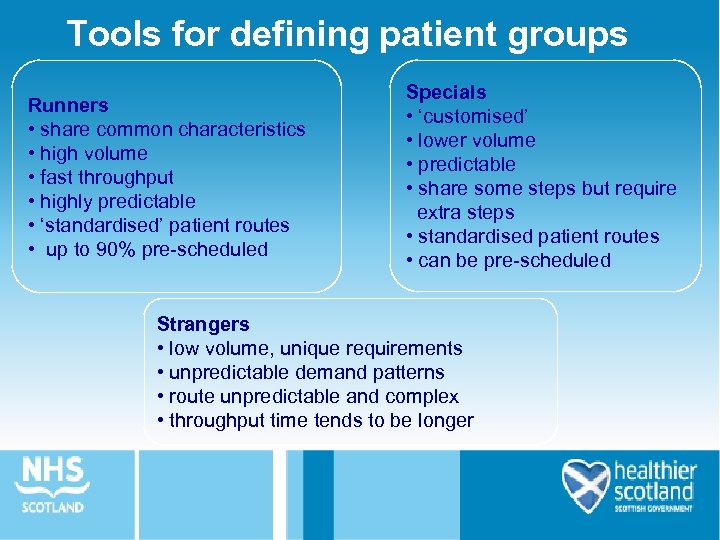 Tools for defining patient groups Runners • share common characteristics • high volume • fast throughput • highly predictable • ‘standardised’ patient routes • up to 90% pre-scheduled Specials • ‘customised’ • lower volume • predictable • share some steps but require extra steps • standardised patient routes • can be pre-scheduled Strangers • low volume, unique requirements • unpredictable demand patterns • route unpredictable and complex • throughput time tends to be longer
Tools for defining patient groups Runners • share common characteristics • high volume • fast throughput • highly predictable • ‘standardised’ patient routes • up to 90% pre-scheduled Specials • ‘customised’ • lower volume • predictable • share some steps but require extra steps • standardised patient routes • can be pre-scheduled Strangers • low volume, unique requirements • unpredictable demand patterns • route unpredictable and complex • throughput time tends to be longer
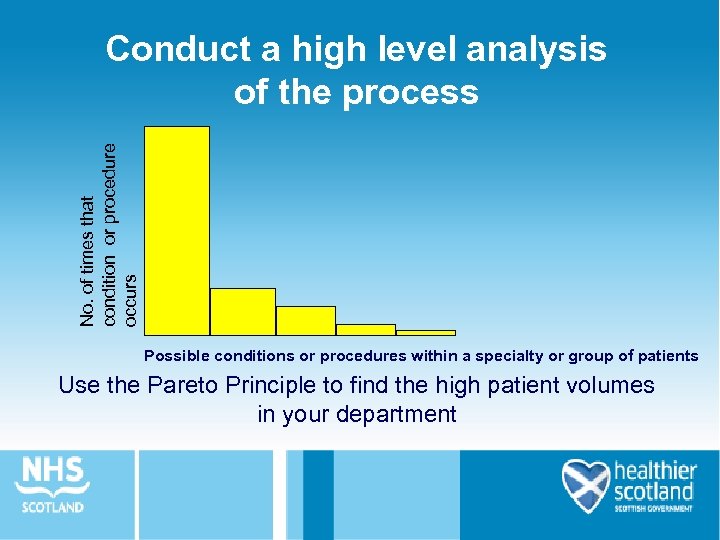 No. of times that condition or procedure occurs Conduct a high level analysis of the process Possible conditions or procedures within a specialty or group of patients Use the Pareto Principle to find the high patient volumes in your department
No. of times that condition or procedure occurs Conduct a high level analysis of the process Possible conditions or procedures within a specialty or group of patients Use the Pareto Principle to find the high patient volumes in your department
 ‘Ground rules’ for the Process Mapping workshop • • Everything is confidential Everyone has a valuable contribution to make Value the diversity of the group Think creatively/generate ideas Focus on ideas and opportunities ‘Park’ issues Keep to time
‘Ground rules’ for the Process Mapping workshop • • Everything is confidential Everyone has a valuable contribution to make Value the diversity of the group Think creatively/generate ideas Focus on ideas and opportunities ‘Park’ issues Keep to time
 Patient tracking • Validate or challenge Process Map • High volume runners • Blank sheet to record process steps and true complexity of journey • At least 25 patients to be tracked per high volume runner group
Patient tracking • Validate or challenge Process Map • High volume runners • Blank sheet to record process steps and true complexity of journey • At least 25 patients to be tracked per high volume runner group
 Walk the patient journey for yourself
Walk the patient journey for yourself
 What do we mean by patient flow?
What do we mean by patient flow?
 About patient flows: • Defined by process not clinical conditions • Reflect systematic process steps required by the majority of patients (high volume groups), total length of journey and complexity across whole systems • Apply the 80: 20 rule to redesign for maximum impact • Consider patient need not service provision • Ensures that you do not improve one part of the service at the expense of another
About patient flows: • Defined by process not clinical conditions • Reflect systematic process steps required by the majority of patients (high volume groups), total length of journey and complexity across whole systems • Apply the 80: 20 rule to redesign for maximum impact • Consider patient need not service provision • Ensures that you do not improve one part of the service at the expense of another
 Improving flow • Understand the processes and the system • Identify measures for improvement • Simplify and standardise the process • Control the variation • Reduce the variation • Make the system safe
Improving flow • Understand the processes and the system • Identify measures for improvement • Simplify and standardise the process • Control the variation • Reduce the variation • Make the system safe
 What is flow analysis?
What is flow analysis?
 3 stages to flow improvement 1 - See the current state 2 - Analysis 3 - Take action to apply flow improvement principles
3 stages to flow improvement 1 - See the current state 2 - Analysis 3 - Take action to apply flow improvement principles
 Stage 1: Current state
Stage 1: Current state
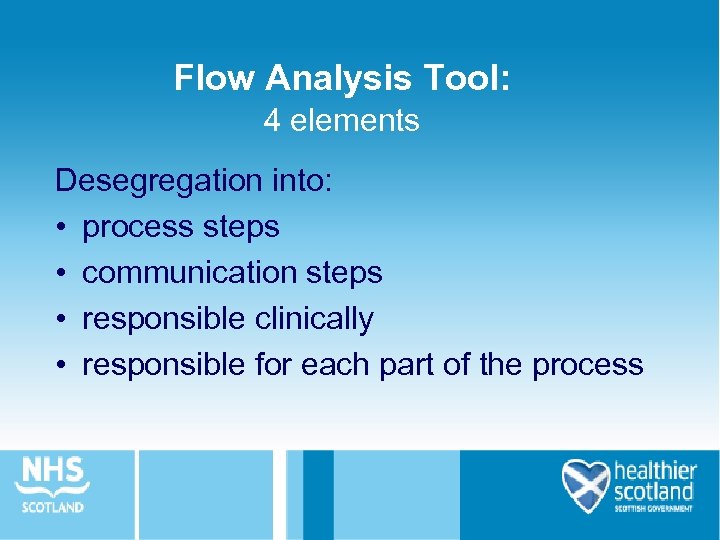 Flow Analysis Tool: 4 elements Desegregation into: • process steps • communication steps • responsible clinically • responsible for each part of the process
Flow Analysis Tool: 4 elements Desegregation into: • process steps • communication steps • responsible clinically • responsible for each part of the process
 Flow Analysis Tool: Process steps
Flow Analysis Tool: Process steps
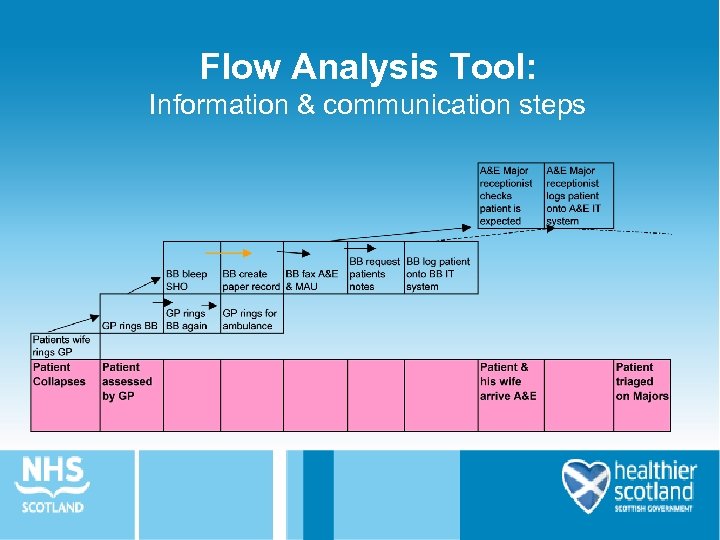 Flow Analysis Tool: Information & communication steps
Flow Analysis Tool: Information & communication steps
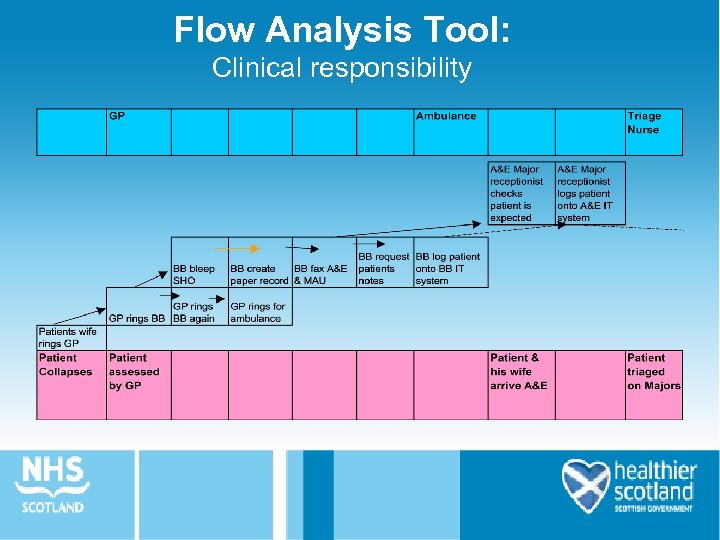 Flow Analysis Tool: Clinical responsibility
Flow Analysis Tool: Clinical responsibility
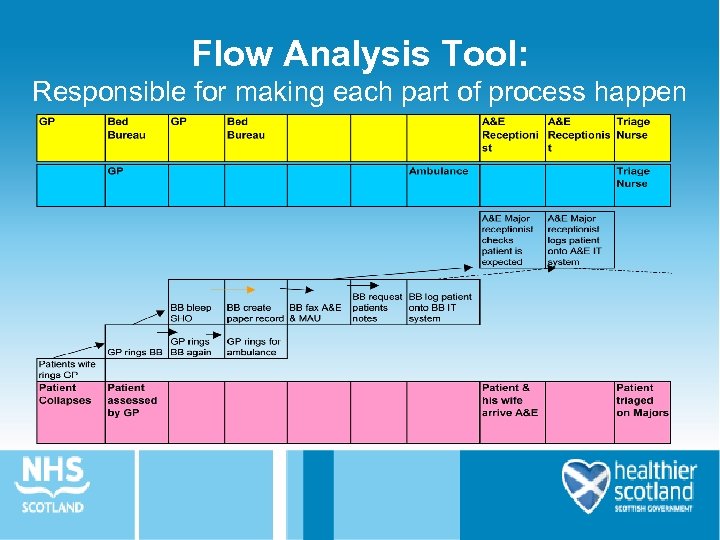 Flow Analysis Tool: Responsible for making each part of process happen
Flow Analysis Tool: Responsible for making each part of process happen
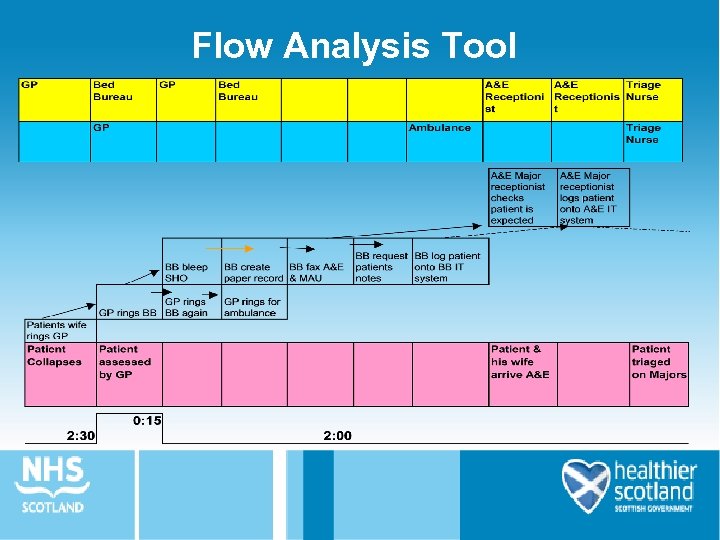 Flow Analysis Tool
Flow Analysis Tool
 Stage 2: Analysis
Stage 2: Analysis
 Understanding your map Add value Remove waste
Understanding your map Add value Remove waste
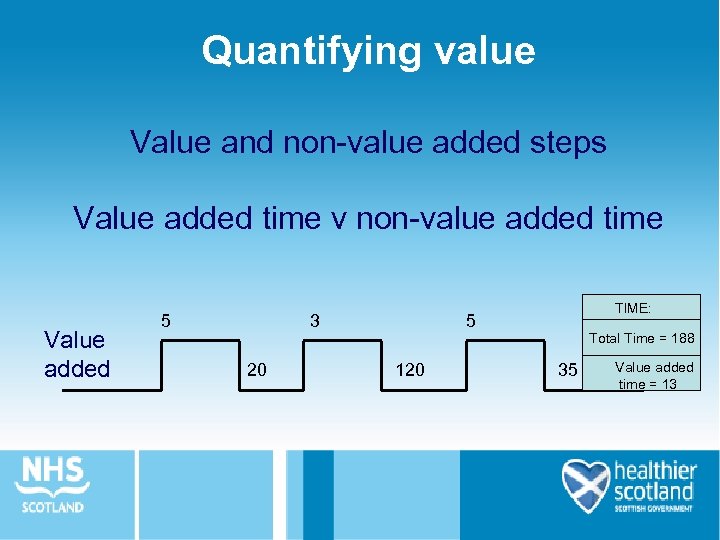 Quantifying value Value and non-value added steps Value added time v non-value added time Value added 3 5 20 TIME: 5 120 Total Time = 188 35 Value added time = 13
Quantifying value Value and non-value added steps Value added time v non-value added time Value added 3 5 20 TIME: 5 120 Total Time = 188 35 Value added time = 13
 Opportunities to remove waste • • Waiting Mistakes Uncoordinated activity Stock Transportation Motion Inappropriate processing
Opportunities to remove waste • • Waiting Mistakes Uncoordinated activity Stock Transportation Motion Inappropriate processing
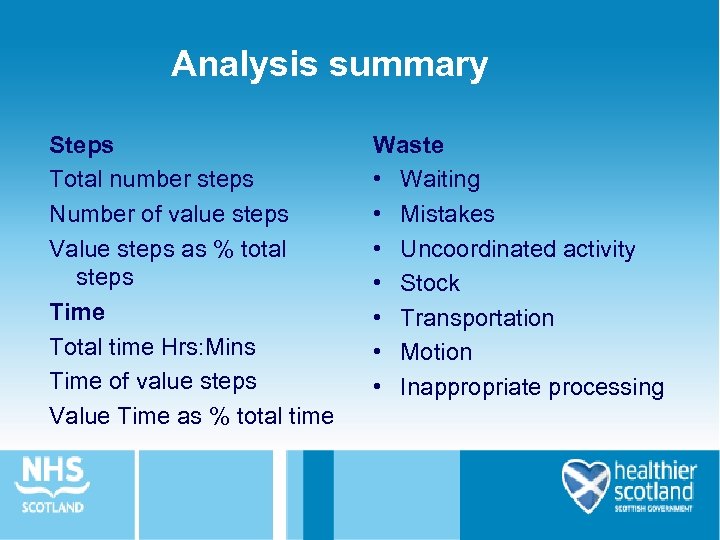 Analysis summary Steps Total number steps Number of value steps Value steps as % total steps Time Total time Hrs: Mins Time of value steps Value Time as % total time Waste • Waiting • Mistakes • Uncoordinated activity • Stock • Transportation • Motion • Inappropriate processing
Analysis summary Steps Total number steps Number of value steps Value steps as % total steps Time Total time Hrs: Mins Time of value steps Value Time as % total time Waste • Waiting • Mistakes • Uncoordinated activity • Stock • Transportation • Motion • Inappropriate processing
 Waiting is the most important of all the wastes because: ▲the process STOPS ▲it inhibits FLOW ▲it does not add value for the PATIENT
Waiting is the most important of all the wastes because: ▲the process STOPS ▲it inhibits FLOW ▲it does not add value for the PATIENT
 Stage 3: Take action to apply flow improvement principles
Stage 3: Take action to apply flow improvement principles
 Next - helping the value-adding steps flow 4 characteristics of smooth flow: 1 Small batch sizes 2 Linked processes 3 Setting the pace 4 Overall co-ordination
Next - helping the value-adding steps flow 4 characteristics of smooth flow: 1 Small batch sizes 2 Linked processes 3 Setting the pace 4 Overall co-ordination
 Linked processes • Current processes often operate in isolation from each other, particularly departments and directorates • Each area needs to be linked to the one before, to ensure that they always have capacity to deal with what they are receiving
Linked processes • Current processes often operate in isolation from each other, particularly departments and directorates • Each area needs to be linked to the one before, to ensure that they always have capacity to deal with what they are receiving
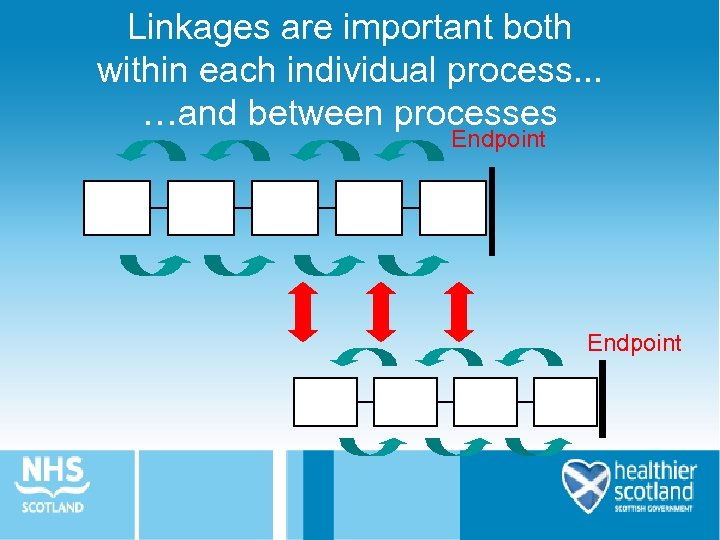 Linkages are important both within each individual process. . . …and between processes Endpoint
Linkages are important both within each individual process. . . …and between processes Endpoint
 Setting the pace • Key stages that need to be set or balanced are often identified by the value adding line • For example - clinical assessment investigations - clinical decision admission - treatment - discharge
Setting the pace • Key stages that need to be set or balanced are often identified by the value adding line • For example - clinical assessment investigations - clinical decision admission - treatment - discharge
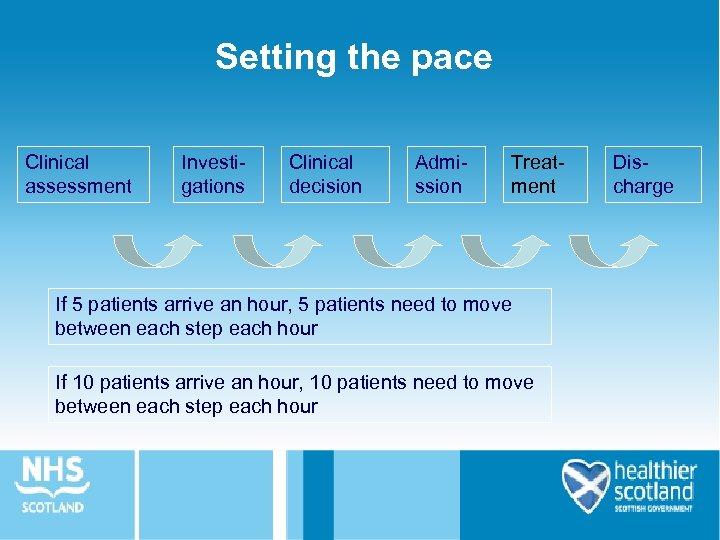 Setting the pace Clinical assessment Investigations Clinical decision Admission Treatment If 5 patients arrive an hour, 5 patients need to move between each step each hour If 10 patients arrive an hour, 10 patients need to move between each step each hour Discharge
Setting the pace Clinical assessment Investigations Clinical decision Admission Treatment If 5 patients arrive an hour, 5 patients need to move between each step each hour If 10 patients arrive an hour, 10 patients need to move between each step each hour Discharge
 Overall co-ordination • Flows that have a single individual/team/area responsible for the whole flow from start to finish work best • It makes clear the notion of the flow as the unit rather than each individual department as the unit • This enables action to be taken at the place where problems are being experienced quickly
Overall co-ordination • Flows that have a single individual/team/area responsible for the whole flow from start to finish work best • It makes clear the notion of the flow as the unit rather than each individual department as the unit • This enables action to be taken at the place where problems are being experienced quickly
 Remember always aim to: Add value Remove waste
Remember always aim to: Add value Remove waste
 Questions?
Questions?


