ad25a3a8e5759d1f8c1c8cd2993682e4.ppt
- Количество слайдов: 21
 Understanding ACO’s in 30 Minutes – A Physician’s Guide - Mike Segal, Esq. msegal@broadandcassel. com Pariksith Singh, M. D. psingh@accesshealthcarellc. net Alan S. Gassman, Esq. agassman@gassmanpa. com Lester J. Perling, Esq. lperling@broadandcassel. com Thursday, April 21, 2011 5: 30 p. m. Replays of this webinar and additional materials can be found at: www. gassmanbateslawgroup. com/media. html Copyright © 2011 1
Understanding ACO’s in 30 Minutes – A Physician’s Guide - Mike Segal, Esq. msegal@broadandcassel. com Pariksith Singh, M. D. psingh@accesshealthcarellc. net Alan S. Gassman, Esq. agassman@gassmanpa. com Lester J. Perling, Esq. lperling@broadandcassel. com Thursday, April 21, 2011 5: 30 p. m. Replays of this webinar and additional materials can be found at: www. gassmanbateslawgroup. com/media. html Copyright © 2011 1
 PROPOSED REGULATIONS SUMMARY REQUIREMENTS FOR ALL ACOs Must have 5, 000 or more primary care patients treated by designated ACO primary care physicians – internists, family practice doctors, and gerentologists. The total Medicare costs incurred for the ACO primary care patients will be measured each year. The ACO will receive 50 or 60 percent of total Medicare savings on those patients if other qualifications are met. All participants in the ACO may be paid directly by Medicare Part A and Part B for the actual services that they provide to patients. ACO must meet the 65 Quality Measures. Mandatory 25% Withholding of savings payments. Copyright © 2011 2
PROPOSED REGULATIONS SUMMARY REQUIREMENTS FOR ALL ACOs Must have 5, 000 or more primary care patients treated by designated ACO primary care physicians – internists, family practice doctors, and gerentologists. The total Medicare costs incurred for the ACO primary care patients will be measured each year. The ACO will receive 50 or 60 percent of total Medicare savings on those patients if other qualifications are met. All participants in the ACO may be paid directly by Medicare Part A and Part B for the actual services that they provide to patients. ACO must meet the 65 Quality Measures. Mandatory 25% Withholding of savings payments. Copyright © 2011 2
 PRIMARY FINANCIAL COMPENSATION RULES Track 1 Rules (No loss participation in first two years) Savings Rate Threshold (Must exceed the below percentages to qualify for shared savings payment) Year 1 2% - 3. 9% depending number of patients Year 2 2% - 3. 9% depending number of patients Year 3 2%? * Shared Savings Rate 50% 60%? * Shared Savings Rate is Increased Based on Visits to Federally Qualified Health Center or Rural Health Center Shared Loss Cap Up to 2. 5% No shared losses Track 2 Rules (Loss participation exposure every year) Savings Rate Threshold (Must exceed the below percentages to qualify for shared savings payment) Year 1 Up to 2. 5% No shared losses Up to 5%? * 5% of the benchmark* Shared Savings Rate is Increased Based on Visits to Federally Qualified Health Center or Rural Health Center Shared Loss Cap 2% 60% Up to 5% 5% Year 2 2% 60% Up to 5% 7. 50% Year 3 2% 60% Up to 5% 10% *NOTE: The ACO under Track 1 “converts” from a One-Sided Model to a Two-Sided Model in the third year. Copyright © 2011 3
PRIMARY FINANCIAL COMPENSATION RULES Track 1 Rules (No loss participation in first two years) Savings Rate Threshold (Must exceed the below percentages to qualify for shared savings payment) Year 1 2% - 3. 9% depending number of patients Year 2 2% - 3. 9% depending number of patients Year 3 2%? * Shared Savings Rate 50% 60%? * Shared Savings Rate is Increased Based on Visits to Federally Qualified Health Center or Rural Health Center Shared Loss Cap Up to 2. 5% No shared losses Track 2 Rules (Loss participation exposure every year) Savings Rate Threshold (Must exceed the below percentages to qualify for shared savings payment) Year 1 Up to 2. 5% No shared losses Up to 5%? * 5% of the benchmark* Shared Savings Rate is Increased Based on Visits to Federally Qualified Health Center or Rural Health Center Shared Loss Cap 2% 60% Up to 5% 5% Year 2 2% 60% Up to 5% 7. 50% Year 3 2% 60% Up to 5% 10% *NOTE: The ACO under Track 1 “converts” from a One-Sided Model to a Two-Sided Model in the third year. Copyright © 2011 3
 What are the GOALs of an ACO? Better Care for Individuals Better Health for Populations Lower Growth in Expenditure BETTER QUALITY OF CARE AT A LOWER COST! Copyright © 2011 4
What are the GOALs of an ACO? Better Care for Individuals Better Health for Populations Lower Growth in Expenditure BETTER QUALITY OF CARE AT A LOWER COST! Copyright © 2011 4
 ACO Regulations Some of the new ACO regulations issued March 31 st: ◦ PCPs, Internists, Family Practitioners, and General Practitioners are limited to one ACO! ◦ A Board certified physician must serve as the medical director ◦ ACO participants hold at least 75% control of the governing body ◦ Certain ACOs are required to get anti-trust approval ◦ Early termination of ACO status = forfeit 25% of withheld shared savings ◦ Patients need to be told that you are part of an ACO ◦ Patients are not bound to one ACO ◦ CMS will require documentation setting forth the division of shared savings and ability to pay for losses Copyright © 2011 5
ACO Regulations Some of the new ACO regulations issued March 31 st: ◦ PCPs, Internists, Family Practitioners, and General Practitioners are limited to one ACO! ◦ A Board certified physician must serve as the medical director ◦ ACO participants hold at least 75% control of the governing body ◦ Certain ACOs are required to get anti-trust approval ◦ Early termination of ACO status = forfeit 25% of withheld shared savings ◦ Patients need to be told that you are part of an ACO ◦ Patients are not bound to one ACO ◦ CMS will require documentation setting forth the division of shared savings and ability to pay for losses Copyright © 2011 5
 HI-TECH Act and Electronic Health Records Quality/Cost Initiative fueled by the ability to review patient records electronically, file claims electronically, and to create meaningful data to closely monitor quality and cost DATA, DATA - IT’S ALL ABOUT THE DATA Meaningful use - ARRA rebates for achieving standards begins this year. Copyright © 2011 6
HI-TECH Act and Electronic Health Records Quality/Cost Initiative fueled by the ability to review patient records electronically, file claims electronically, and to create meaningful data to closely monitor quality and cost DATA, DATA - IT’S ALL ABOUT THE DATA Meaningful use - ARRA rebates for achieving standards begins this year. Copyright © 2011 6
 Clinical Integration – Why is it important? What is it? The Advisory Board Company defines Clinical Integration as “a strategy in which physicians – often in partnership with a hospital or health system – make a significant collective commitment to performance improvement and investment in infrastructure to facilitate these quality and efficiency gains” CI designed to bring together different specialties under common governance and incentive structures to create – and reward – collaboration between groups of physicians who may not currently work together CI an imperative for a successful ACO Copyright © 2011 7
Clinical Integration – Why is it important? What is it? The Advisory Board Company defines Clinical Integration as “a strategy in which physicians – often in partnership with a hospital or health system – make a significant collective commitment to performance improvement and investment in infrastructure to facilitate these quality and efficiency gains” CI designed to bring together different specialties under common governance and incentive structures to create – and reward – collaboration between groups of physicians who may not currently work together CI an imperative for a successful ACO Copyright © 2011 7
 Clinical Integration 1996 - FTC and DOJ issues joint guidelines regarding antitrust issues for health care combinations Guidelines require, in network where not all physicians are members of same medical group, that physician members be “clinically integrated” in order to share financial information and jointly negotiate fee for service contracts There have been three FTC opinions since 2002 holding that CI in network was achieved (see, e. . g. , www. tristatehealth. com) Copyright © 2011 8
Clinical Integration 1996 - FTC and DOJ issues joint guidelines regarding antitrust issues for health care combinations Guidelines require, in network where not all physicians are members of same medical group, that physician members be “clinically integrated” in order to share financial information and jointly negotiate fee for service contracts There have been three FTC opinions since 2002 holding that CI in network was achieved (see, e. . g. , www. tristatehealth. com) Copyright © 2011 8
 Three part FTC/DOJ standard Participants must demonstrate significant commitment (both in time and money) to cost control and quality improvement, with realistic opportunity to achieve goals Joint fee for service contracting with payers, must be reasonably necessary to support network’s infrastructure and support greater collaboration (in other words, network may negotiate higher prices, but only if this is directly connected with offering a more effective CI product) Network cannot have too much market power Copyright © 2011 9
Three part FTC/DOJ standard Participants must demonstrate significant commitment (both in time and money) to cost control and quality improvement, with realistic opportunity to achieve goals Joint fee for service contracting with payers, must be reasonably necessary to support network’s infrastructure and support greater collaboration (in other words, network may negotiate higher prices, but only if this is directly connected with offering a more effective CI product) Network cannot have too much market power Copyright © 2011 9
 8 Key CI Program Components The Advisory Board Company identifies 8 critical components for a CI network: (1) Selective Physician Partners (2) Physician Oversight (3) Meaningful Performance Metrics (4) Optimized IT Infrastructure – (EHR not absolutely necessary – registries or web-based data may suffice) (5) Support for Clinical Redesign (6) Performance Monitoring (7) Payer Engagement (8) Performance-Based Incentive Pool Copyright © 2011 10
8 Key CI Program Components The Advisory Board Company identifies 8 critical components for a CI network: (1) Selective Physician Partners (2) Physician Oversight (3) Meaningful Performance Metrics (4) Optimized IT Infrastructure – (EHR not absolutely necessary – registries or web-based data may suffice) (5) Support for Clinical Redesign (6) Performance Monitoring (7) Payer Engagement (8) Performance-Based Incentive Pool Copyright © 2011 10
 PPACA Requirements Pursuant to PPACA, an ACO must, among other things: Formal Legal Structure Leadership and management Minimum of 5000 Medicare beneficiaries 3 year contract with Medicare Primary care participation is a MUST! Processes and procedures to enhance quality/reduce costs ◦ Clinical and administrative systems to report on quality/cost measures ◦ Demonstrate it meets patient-centeredness criteria ◦ ◦ ◦ Copyright © 2011 11
PPACA Requirements Pursuant to PPACA, an ACO must, among other things: Formal Legal Structure Leadership and management Minimum of 5000 Medicare beneficiaries 3 year contract with Medicare Primary care participation is a MUST! Processes and procedures to enhance quality/reduce costs ◦ Clinical and administrative systems to report on quality/cost measures ◦ Demonstrate it meets patient-centeredness criteria ◦ ◦ ◦ Copyright © 2011 11
 WHO MAY PARTICIPATE IN AN ACO? Possible Participants: ◦ integrated delivery systems ◦ primary care medical groups ◦ single specialty medical groups ◦ multi specialty medical group ◦ hospital-based systems ◦ virtual networks of physicians ◦ hospitals (strongly encouraged) ◦ health plan management companies Copyright © 2011 12
WHO MAY PARTICIPATE IN AN ACO? Possible Participants: ◦ integrated delivery systems ◦ primary care medical groups ◦ single specialty medical groups ◦ multi specialty medical group ◦ hospital-based systems ◦ virtual networks of physicians ◦ hospitals (strongly encouraged) ◦ health plan management companies Copyright © 2011 12
 Forms of Accountable Care Organizations ACOs may involve a variety of configurations of the possible participants Don’t get caught up with the acronyms (IPA, PHO, SSGP, MSGP, HPPO, etc. ), focus on the ◦ ◦ (i) forming the necessary relationships (ii) achieving the necessary level of integration (iii) governance (iv) data collection and analysis Copyright © 2011 13
Forms of Accountable Care Organizations ACOs may involve a variety of configurations of the possible participants Don’t get caught up with the acronyms (IPA, PHO, SSGP, MSGP, HPPO, etc. ), focus on the ◦ ◦ (i) forming the necessary relationships (ii) achieving the necessary level of integration (iii) governance (iv) data collection and analysis Copyright © 2011 13
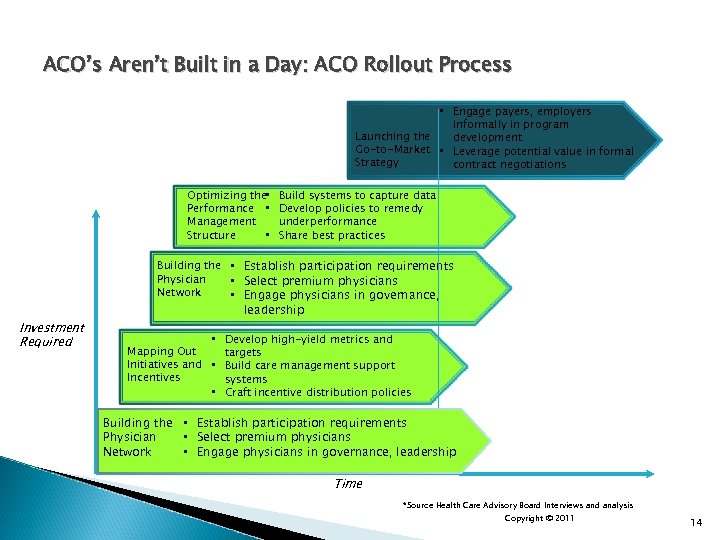 ACO’s Aren’t Built in a Day: ACO Rollout Process • Engage payers, employers informally in program Launching the development Go-to-Market • Leverage potential value in formal Strategy contract negotiations Optimizing the • Performance • Management Structure • Build systems to capture data Develop policies to remedy underperformance Share best practices Building the • Establish participation requirements Physician • Select premium physicians Network • Engage physicians in governance, Investment Required leadership • Develop high-yield metrics and Mapping Out targets Initiatives and • Build care management support Incentives systems • Craft incentive distribution policies Building the • Establish participation requirements Physician • Select premium physicians Network • Engage physicians in governance, leadership Time *Source Health Care Advisory Board Interviews and analysis Copyright © 2011 14
ACO’s Aren’t Built in a Day: ACO Rollout Process • Engage payers, employers informally in program Launching the development Go-to-Market • Leverage potential value in formal Strategy contract negotiations Optimizing the • Performance • Management Structure • Build systems to capture data Develop policies to remedy underperformance Share best practices Building the • Establish participation requirements Physician • Select premium physicians Network • Engage physicians in governance, Investment Required leadership • Develop high-yield metrics and Mapping Out targets Initiatives and • Build care management support Incentives systems • Craft incentive distribution policies Building the • Establish participation requirements Physician • Select premium physicians Network • Engage physicians in governance, leadership Time *Source Health Care Advisory Board Interviews and analysis Copyright © 2011 14
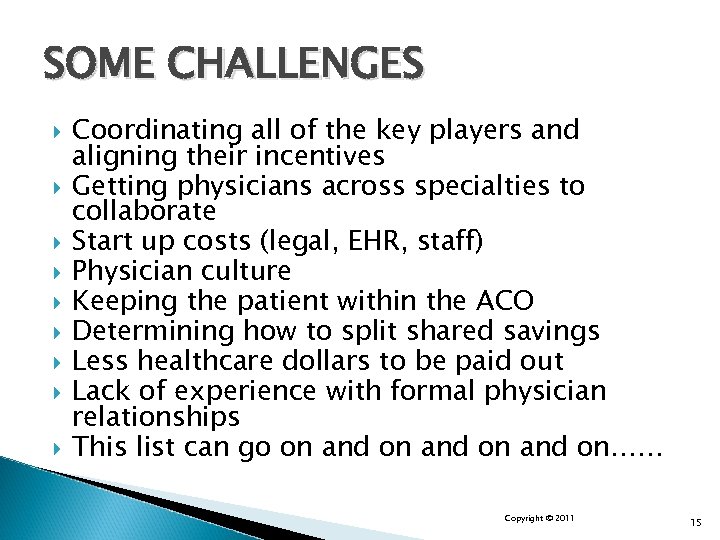 SOME CHALLENGES Coordinating all of the key players and aligning their incentives Getting physicians across specialties to collaborate Start up costs (legal, EHR, staff) Physician culture Keeping the patient within the ACO Determining how to split shared savings Less healthcare dollars to be paid out Lack of experience with formal physician relationships This list can go on and on…… Copyright © 2011 15
SOME CHALLENGES Coordinating all of the key players and aligning their incentives Getting physicians across specialties to collaborate Start up costs (legal, EHR, staff) Physician culture Keeping the patient within the ACO Determining how to split shared savings Less healthcare dollars to be paid out Lack of experience with formal physician relationships This list can go on and on…… Copyright © 2011 15
 Aligning Staff with Accountable Care Goals Central Challenge Internal Obstacles to ACO Development As rated by CEOs No Small Undertaking. “Navigating this migration is our central management challenge for the next decade. Transitions are always messy, and we’re in a transition period. You can’t have one foot in two boats forever. ” Chief Executive Officer 10 -Hospital Health System *Source Gates, S. “HR’s Role in Building a Culture of Innovation, ” The Conference Board, 2005; Advisory Board Interviews and analysis 16
Aligning Staff with Accountable Care Goals Central Challenge Internal Obstacles to ACO Development As rated by CEOs No Small Undertaking. “Navigating this migration is our central management challenge for the next decade. Transitions are always messy, and we’re in a transition period. You can’t have one foot in two boats forever. ” Chief Executive Officer 10 -Hospital Health System *Source Gates, S. “HR’s Role in Building a Culture of Innovation, ” The Conference Board, 2005; Advisory Board Interviews and analysis 16
 Regulatory Issues With ACOs and Networks Stark Anti-kickback and CMP (reducing care issues) Anti-Trust Law - will consolidation cause prices to rise? How much market share do you have (less than 30%, more than 50%) On April 7, 2011, CMS and OIG published proposed waivers of the Stark law, the antikickback statute and CMP law. Comments period ends June 6, 2011. ◦ ◦ Stark waiver only for the ACO’s distribution of shared savings AKS and CMP waivers for all financial relationships in ACO Copyright © 2011 17
Regulatory Issues With ACOs and Networks Stark Anti-kickback and CMP (reducing care issues) Anti-Trust Law - will consolidation cause prices to rise? How much market share do you have (less than 30%, more than 50%) On April 7, 2011, CMS and OIG published proposed waivers of the Stark law, the antikickback statute and CMP law. Comments period ends June 6, 2011. ◦ ◦ Stark waiver only for the ACO’s distribution of shared savings AKS and CMP waivers for all financial relationships in ACO Copyright © 2011 17
 Further Resources The proposed Regulations are available at: http: //www. cms. gov/sharedsavingsprogram An easier to read version of the proposed regulations, with acronym definitions throughout the text, a table of contents with page numbers, and an index, is available from Gassman, Bates & Associates, P. A. To sign up to receive the Broad and Cassel Integration Update emails, please contact Alicia Florio at amflorio@broadandcassel. com It’s all in the Math: Financial Mechanisms, Structures and Questions Under the Accountable Care Organization Proposed Regulations by Alan S. Gassman, Mike Segal, Dr. Pariksith Singh and Martha Sosa, soon to be published in the American Bar Association Health e. Source Newsletter. You do not have to be an ABA Health Law Section member to receive the ABA Health e. Source Newsletter. Sign up at http: //www. americanbarassociation. org/content/newsletter/publications/aba_health_esource_ home. html Accountable Care Organizations Proposed Regulations Reveal Significant Financial Opportunities and Structural Requirements by Alan S. Gassman and Martha Sosa, published in the American Bar Association Health e. Source Newsletter. Available at http: //www. americanbarassociation. org/content/newsletter/publications/aba_health_esource_ home/aba_health_law_esource_2011_april_volume_7_issue_8. html ACO’s: A Work in Progress by Mike Segal and Heather Siegal Miller, published in the Florida Bar Health Law Section Newsletter. http: //www. floridabar. org/TFBResources. nsf/Attachments/8009082626 D 825 D 78525782 010054293 C/$FILE/Final%20 copy%202, pdf? Open. Element Copyright © 2011 18
Further Resources The proposed Regulations are available at: http: //www. cms. gov/sharedsavingsprogram An easier to read version of the proposed regulations, with acronym definitions throughout the text, a table of contents with page numbers, and an index, is available from Gassman, Bates & Associates, P. A. To sign up to receive the Broad and Cassel Integration Update emails, please contact Alicia Florio at amflorio@broadandcassel. com It’s all in the Math: Financial Mechanisms, Structures and Questions Under the Accountable Care Organization Proposed Regulations by Alan S. Gassman, Mike Segal, Dr. Pariksith Singh and Martha Sosa, soon to be published in the American Bar Association Health e. Source Newsletter. You do not have to be an ABA Health Law Section member to receive the ABA Health e. Source Newsletter. Sign up at http: //www. americanbarassociation. org/content/newsletter/publications/aba_health_esource_ home. html Accountable Care Organizations Proposed Regulations Reveal Significant Financial Opportunities and Structural Requirements by Alan S. Gassman and Martha Sosa, published in the American Bar Association Health e. Source Newsletter. Available at http: //www. americanbarassociation. org/content/newsletter/publications/aba_health_esource_ home/aba_health_law_esource_2011_april_volume_7_issue_8. html ACO’s: A Work in Progress by Mike Segal and Heather Siegal Miller, published in the Florida Bar Health Law Section Newsletter. http: //www. floridabar. org/TFBResources. nsf/Attachments/8009082626 D 825 D 78525782 010054293 C/$FILE/Final%20 copy%202, pdf? Open. Element Copyright © 2011 18
 Thoughts from Dr. Singh – Page 1 Who will be initiating the formation of these ACOs? Where will a physician turn to join one, and how will they know what the options are? ACOs will be initiated only by hospitals, HMOs, large physician groups, big medical corporate entities that can sign up physicians, or consultants who have a big network that can influence physicians and sign them up. People will have to have resources to pull together ACOs. Only the strong will even file for them. There will be a lot of these entities initially, because for consultants, accountants, and lawyers, it is a windfall; they are charging physicians money to give lectures and seminars. Even right now, when all the regulations are unclear, they are giving lectures and charging $5, 000 to $7, 000 to explain the regulations. What will happen is that these consultants, accountants, lawyers, actuaries, and even other physicians will go around trying to sign up people, but the biggest strength will likely be with hospital groups, HMOs that are already present, and perhaps big physician groups. Is there a buy in for a physician joining an ACO? It is unlikely that there will be a buy in for primary care physicians. It depends on where the group is; there will certainly be some incentives offered. Maybe some ACOs or people who have stronger networks will establish a pyramid system, where the stronger physicians will make more money than the new physicians who are joining in. However, there should not be a buy-in unless an ACO is extremely successful, or unless the doctors are buying shares in the ACO. Copyright © 2011 19
Thoughts from Dr. Singh – Page 1 Who will be initiating the formation of these ACOs? Where will a physician turn to join one, and how will they know what the options are? ACOs will be initiated only by hospitals, HMOs, large physician groups, big medical corporate entities that can sign up physicians, or consultants who have a big network that can influence physicians and sign them up. People will have to have resources to pull together ACOs. Only the strong will even file for them. There will be a lot of these entities initially, because for consultants, accountants, and lawyers, it is a windfall; they are charging physicians money to give lectures and seminars. Even right now, when all the regulations are unclear, they are giving lectures and charging $5, 000 to $7, 000 to explain the regulations. What will happen is that these consultants, accountants, lawyers, actuaries, and even other physicians will go around trying to sign up people, but the biggest strength will likely be with hospital groups, HMOs that are already present, and perhaps big physician groups. Is there a buy in for a physician joining an ACO? It is unlikely that there will be a buy in for primary care physicians. It depends on where the group is; there will certainly be some incentives offered. Maybe some ACOs or people who have stronger networks will establish a pyramid system, where the stronger physicians will make more money than the new physicians who are joining in. However, there should not be a buy-in unless an ACO is extremely successful, or unless the doctors are buying shares in the ACO. Copyright © 2011 19
 Thoughts from Dr. Singh – Page 2 What do you think the chances of survival are for a physician who chooses not to join an ACO? Initially, physicians should be okay “going rogue”, because joining an ACO is not mandatory. But once the groups form, the direction for most primary care physicians will likely be toward joining an ACO. The physicians who will survive are the physicians who do not need Medicare, who do fee for service, who are already operating as cash practices. Primary care physicians who have a niche business may be able to stay the course outside the system. Specialists will have no choice but to work with ACOs, because they need referrals. So wherever you have ACOs, specialists will be signing up and working with them, but primary care physicians may have the option, for a little while, to stay out and still succeed. It depends on how hard the government starts pushing the ACOs, and how deep the penetration of ACOs is in a certain area. For example, in California, every physician has to sign up and make sure they are part of a bigger managed care network. In Florida, there are certain areas where they have no choice, that even though they save much less than Medicare when they sign up with managed care companies, they will still sign up. In certain rural areas, solo physicians might be okay for a while. Bigger areas, where the networks are strong and ACOs have a bigger presence, it will be more and more difficult for them to survive on their own. It depends on several factors. An apt metaphor could be that of a hand caught in its own mousetrap. The government is setting a trap for the physicians, using incentives to sign them up with the ACOs. However, the government’s hand may be the one caught in the trap instead; it may end up taking huge losses on these ACOs if it is not done right. ACOs will have to be managed by very savvy people who understand this kind of goal-based care and healthcare where quality of care is not compromised, but also people who are very mindful of the costs involved with the care. That is going to be the key. Copyright © 2011 20
Thoughts from Dr. Singh – Page 2 What do you think the chances of survival are for a physician who chooses not to join an ACO? Initially, physicians should be okay “going rogue”, because joining an ACO is not mandatory. But once the groups form, the direction for most primary care physicians will likely be toward joining an ACO. The physicians who will survive are the physicians who do not need Medicare, who do fee for service, who are already operating as cash practices. Primary care physicians who have a niche business may be able to stay the course outside the system. Specialists will have no choice but to work with ACOs, because they need referrals. So wherever you have ACOs, specialists will be signing up and working with them, but primary care physicians may have the option, for a little while, to stay out and still succeed. It depends on how hard the government starts pushing the ACOs, and how deep the penetration of ACOs is in a certain area. For example, in California, every physician has to sign up and make sure they are part of a bigger managed care network. In Florida, there are certain areas where they have no choice, that even though they save much less than Medicare when they sign up with managed care companies, they will still sign up. In certain rural areas, solo physicians might be okay for a while. Bigger areas, where the networks are strong and ACOs have a bigger presence, it will be more and more difficult for them to survive on their own. It depends on several factors. An apt metaphor could be that of a hand caught in its own mousetrap. The government is setting a trap for the physicians, using incentives to sign them up with the ACOs. However, the government’s hand may be the one caught in the trap instead; it may end up taking huge losses on these ACOs if it is not done right. ACOs will have to be managed by very savvy people who understand this kind of goal-based care and healthcare where quality of care is not compromised, but also people who are very mindful of the costs involved with the care. That is going to be the key. Copyright © 2011 20
 Questions? ? ? Mike Segal, Esq. msegal@broadandcassel. com 305 -373 -9430 Dr. Pariksith Singh psingh@accesshealthcarellc. net 352 -688 -2883 Alan S. Gassman, Esq. agassman@gassmanpa. com 727 -442 -1200 Lester Perling, Esq. lperling@broadandcassel. com (954) 745 -5261 Martha Sosa, Esq. martha@gassmanpa. com 727 -442 -1200 Copyright © 2011 21
Questions? ? ? Mike Segal, Esq. msegal@broadandcassel. com 305 -373 -9430 Dr. Pariksith Singh psingh@accesshealthcarellc. net 352 -688 -2883 Alan S. Gassman, Esq. agassman@gassmanpa. com 727 -442 -1200 Lester Perling, Esq. lperling@broadandcassel. com (954) 745 -5261 Martha Sosa, Esq. martha@gassmanpa. com 727 -442 -1200 Copyright © 2011 21


