43d3963b14437c177e4d4e43b211efc7.ppt
- Количество слайдов: 66
 UCAPD Low Intensity Assessment and Intervention Skills for Psychological Wellbeing Practice PROGRAMME HANDBOOK January 2017
UCAPD Low Intensity Assessment and Intervention Skills for Psychological Wellbeing Practice PROGRAMME HANDBOOK January 2017
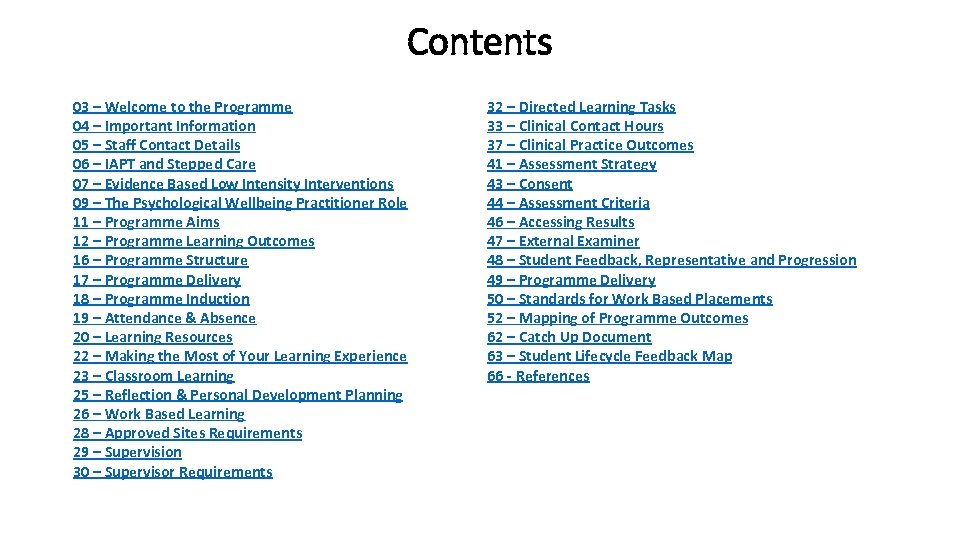 Contents 03 – Welcome to the Programme 04 – Important Information 05 – Staff Contact Details 06 – IAPT and Stepped Care 07 – Evidence Based Low Intensity Interventions 09 – The Psychological Wellbeing Practitioner Role 11 – Programme Aims 12 – Programme Learning Outcomes 16 – Programme Structure 17 – Programme Delivery 18 – Programme Induction 19 – Attendance & Absence 20 – Learning Resources 22 – Making the Most of Your Learning Experience 23 – Classroom Learning 25 – Reflection & Personal Development Planning 26 – Work Based Learning 28 – Approved Sites Requirements 29 – Supervision 30 – Supervisor Requirements 32 – Directed Learning Tasks 33 – Clinical Contact Hours 37 – Clinical Practice Outcomes 41 – Assessment Strategy 43 – Consent 44 – Assessment Criteria 46 – Accessing Results 47 – External Examiner 48 – Student Feedback, Representative and Progression 49 – Programme Delivery 50 – Standards for Work Based Placements 52 – Mapping of Programme Outcomes 62 – Catch Up Document 63 – Student Lifecycle Feedback Map 66 - References
Contents 03 – Welcome to the Programme 04 – Important Information 05 – Staff Contact Details 06 – IAPT and Stepped Care 07 – Evidence Based Low Intensity Interventions 09 – The Psychological Wellbeing Practitioner Role 11 – Programme Aims 12 – Programme Learning Outcomes 16 – Programme Structure 17 – Programme Delivery 18 – Programme Induction 19 – Attendance & Absence 20 – Learning Resources 22 – Making the Most of Your Learning Experience 23 – Classroom Learning 25 – Reflection & Personal Development Planning 26 – Work Based Learning 28 – Approved Sites Requirements 29 – Supervision 30 – Supervisor Requirements 32 – Directed Learning Tasks 33 – Clinical Contact Hours 37 – Clinical Practice Outcomes 41 – Assessment Strategy 43 – Consent 44 – Assessment Criteria 46 – Accessing Results 47 – External Examiner 48 – Student Feedback, Representative and Progression 49 – Programme Delivery 50 – Standards for Work Based Placements 52 – Mapping of Programme Outcomes 62 – Catch Up Document 63 – Student Lifecycle Feedback Map 66 - References
 Welcome to the Programme • Welcome to the Postgraduate Certificate (Pg. C) for Psychological Wellbeing Practice and to Teesside University. This Programme Handbook is intended to answer any questions that you might have about the programme. It provides information about the course in terms of its aims, structure and content and offers guidance for you to make the most of this learning experience, signposting you to other sources of support and information. A Supervisor Handbook is also available and it is essential that you ensure your supervisor receives a copy of this. • This document should be read in conjunction with the programme’s three Module Guides, which provide more detailed information about each specific module, including assessment criteria and submission dates and teaching timetables.
Welcome to the Programme • Welcome to the Postgraduate Certificate (Pg. C) for Psychological Wellbeing Practice and to Teesside University. This Programme Handbook is intended to answer any questions that you might have about the programme. It provides information about the course in terms of its aims, structure and content and offers guidance for you to make the most of this learning experience, signposting you to other sources of support and information. A Supervisor Handbook is also available and it is essential that you ensure your supervisor receives a copy of this. • This document should be read in conjunction with the programme’s three Module Guides, which provide more detailed information about each specific module, including assessment criteria and submission dates and teaching timetables.
 Important Information • It is important that you access and make use of the School of Health & Social Care Student Essential Guide (School Handbook), which provides information and guidance regarding University regulations and processes. • An electronic version of these documents is available for you via the Virtual Learning Environment (VLE) e-learning@tees. It is recommended that both you and your Practice Supervisor become familiar with all of these documents to best enhance your success.
Important Information • It is important that you access and make use of the School of Health & Social Care Student Essential Guide (School Handbook), which provides information and guidance regarding University regulations and processes. • An electronic version of these documents is available for you via the Virtual Learning Environment (VLE) e-learning@tees. It is recommended that both you and your Practice Supervisor become familiar with all of these documents to best enhance your success.
 Staff Contact Details Programme Leader Module Tutor Deborah Rafter Room H 1. 12 Centuria Building Tel: 01642 738165 Email: Paul Thompson Room H 1. 20 Centuria Building Tel: 01642 384536 Email: Sarah Fishburn Room H Centuria Building Tel: 01642 Email: D. Rafter@tees. ac. uk Paul. Thompson@tees. ac. uk S. Fishburn@tees. ac. uk
Staff Contact Details Programme Leader Module Tutor Deborah Rafter Room H 1. 12 Centuria Building Tel: 01642 738165 Email: Paul Thompson Room H 1. 20 Centuria Building Tel: 01642 384536 Email: Sarah Fishburn Room H Centuria Building Tel: 01642 Email: D. Rafter@tees. ac. uk Paul. Thompson@tees. ac. uk S. Fishburn@tees. ac. uk
 IAPT and Stepped Care • The Psychological Wellbeing Practitioner (PWP) role was created as part of the Improving Access to Psychological Therapies (IAPT 2008) in order to improve the capacity of psychological therapy services for people with common mental health problems. • Psychological therapies should be delivered within a stepped care system (National Institute for Health and Care Excellence (NICE) which works on the principle of offering the least intrusive most effective treatment in the first instance and increasing the intensity of treatment as required.
IAPT and Stepped Care • The Psychological Wellbeing Practitioner (PWP) role was created as part of the Improving Access to Psychological Therapies (IAPT 2008) in order to improve the capacity of psychological therapy services for people with common mental health problems. • Psychological therapies should be delivered within a stepped care system (National Institute for Health and Care Excellence (NICE) which works on the principle of offering the least intrusive most effective treatment in the first instance and increasing the intensity of treatment as required.
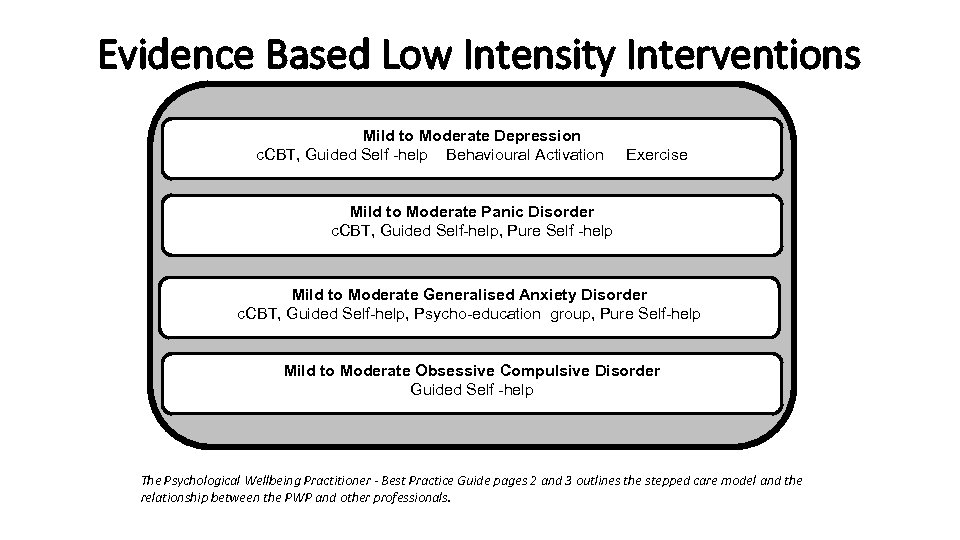 Evidence Based Low Intensity Interventions Mild to Moderate Depression c. CBT, Guided Self -help Behavioural Activation Exercise Mild to Moderate Panic Disorder c. CBT, Guided Self-help, Pure Self -help Mild to Moderate Generalised Anxiety Disorder c. CBT, Guided Self-help, Psycho-education group, Pure Self-help Mild to Moderate Obsessive Compulsive Disorder Guided Self -help The Psychological Wellbeing Practitioner - Best Practice Guide pages 2 and 3 outlines the stepped care model and the relationship between the PWP and other professionals.
Evidence Based Low Intensity Interventions Mild to Moderate Depression c. CBT, Guided Self -help Behavioural Activation Exercise Mild to Moderate Panic Disorder c. CBT, Guided Self-help, Pure Self -help Mild to Moderate Generalised Anxiety Disorder c. CBT, Guided Self-help, Psycho-education group, Pure Self-help Mild to Moderate Obsessive Compulsive Disorder Guided Self -help The Psychological Wellbeing Practitioner - Best Practice Guide pages 2 and 3 outlines the stepped care model and the relationship between the PWP and other professionals.
 Evidence Based Low Intensity Interventions • The PWP provides low intensity assessment and treatment at ‘step 2’ of this model for people with mild to moderate depression and anxiety problems. Low intensity interventions are designed to be brief with a focus upon a self-management approach. Interventions can be delivered through a range of modes such as telephone, computerized, group or individual face to face. • The PWP works alongside other professionals providing a range of interventions across the stepped care model and including High Intensity Interventions at ‘step 3’.
Evidence Based Low Intensity Interventions • The PWP provides low intensity assessment and treatment at ‘step 2’ of this model for people with mild to moderate depression and anxiety problems. Low intensity interventions are designed to be brief with a focus upon a self-management approach. Interventions can be delivered through a range of modes such as telephone, computerized, group or individual face to face. • The PWP works alongside other professionals providing a range of interventions across the stepped care model and including High Intensity Interventions at ‘step 3’.
 Psychological Wellbeing Practitioner Role • Low intensity interventions are intended to enable a high volume of people experiencing mild to moderate common mental health problems to receive treatment. To achieve this the PWP typically has a predetermined and managed number of sessions with individuals (average number of sessions being around 5 sessions).
Psychological Wellbeing Practitioner Role • Low intensity interventions are intended to enable a high volume of people experiencing mild to moderate common mental health problems to receive treatment. To achieve this the PWP typically has a predetermined and managed number of sessions with individuals (average number of sessions being around 5 sessions).
 • • The PWP will: Have a substantial administrative workload due to the high volume cases Often the first point of contact for people accessing the service Conduct triage or screening assessments Enable and motivate the people to use self-help approaches Work via telephone, group, computer and face-to-face contact Work with people with mild to moderate common mental health problems Provide support for people with long-term conditions and medically unexplained symptoms • The PWP will not: • X Assess and triage patients for secondary mental health services or treat people with severe, complex and enduring mental health problems • X Treat people with high levels of risk or needing a higher level of care • X Work in isolation including from step 3 colleagues e. g. if in other organisations • X Carry out high intensity treatment or support non evidence based treatments at step 2 • X Hold high intensity or other waiting lists • X Operate without appropriate supervision National IAPT team/ NHS England/Department of Health (2015) Psychological Wellbeing Practitioner: Best Practice Guide. Convened by University College London
• • The PWP will: Have a substantial administrative workload due to the high volume cases Often the first point of contact for people accessing the service Conduct triage or screening assessments Enable and motivate the people to use self-help approaches Work via telephone, group, computer and face-to-face contact Work with people with mild to moderate common mental health problems Provide support for people with long-term conditions and medically unexplained symptoms • The PWP will not: • X Assess and triage patients for secondary mental health services or treat people with severe, complex and enduring mental health problems • X Treat people with high levels of risk or needing a higher level of care • X Work in isolation including from step 3 colleagues e. g. if in other organisations • X Carry out high intensity treatment or support non evidence based treatments at step 2 • X Hold high intensity or other waiting lists • X Operate without appropriate supervision National IAPT team/ NHS England/Department of Health (2015) Psychological Wellbeing Practitioner: Best Practice Guide. Convened by University College London
 The Programme Aims • Enabling you to gain substantial knowledge appropriate to Masters level (7) • Facilitating the acquisition of core therapeutic and technical skills that underpin low intensity assessment and interventions planning and delivery. • Developing you to have a positive attitude and commitment towards life-long learning, personal and development planning. • Providing opportunities that will prepare you to meet the challenges of current and future contemporary primary care mental health services. • Providing opportunities that will prepare you to acquire cultural competence and to meet the challenges of contemporary practice
The Programme Aims • Enabling you to gain substantial knowledge appropriate to Masters level (7) • Facilitating the acquisition of core therapeutic and technical skills that underpin low intensity assessment and interventions planning and delivery. • Developing you to have a positive attitude and commitment towards life-long learning, personal and development planning. • Providing opportunities that will prepare you to meet the challenges of current and future contemporary primary care mental health services. • Providing opportunities that will prepare you to acquire cultural competence and to meet the challenges of contemporary practice
 Programme Learning Outcomes Knowledge and Understanding • KU 1 Critically evaluate service culture, structures, policies and procedures in relation to mental health practice in primary care. • KU 2 Demonstrate comprehensive and critical understanding of recovery, collaborative working and clientcentred approaches in relation to all aspects of therapeutic process for people with common mental health problems. • KU 3 Demonstrate systematic and critical understanding of a range of social, medical and psychological explanatory models in mental health and mental illness and a practical understanding of diagnostic category systems used in mental health. • KU 4 Demonstrate systematic and critical knowledge of positive risk management. • KU 5 Demonstrate comprehensive and critical knowledge of evidence-based low intensity interventions for people with common mental health problems • KU 6 Demonstrate comprehensive and critical knowledge of social inclusion and non-discriminatory practice. • KU 7 Demonstrate a comprehensive and critical understanding of the roles and responsibilities of the various professional and non-professional workers in primary mental health care. • KU 8 Demonstrate comprehensive and critical knowledge of the complex relationship between health and occupation, employment and wellbeing. • KU 9 Demonstrate comprehensive and critical knowledge, behaviour change theory and its application to common mental health problems
Programme Learning Outcomes Knowledge and Understanding • KU 1 Critically evaluate service culture, structures, policies and procedures in relation to mental health practice in primary care. • KU 2 Demonstrate comprehensive and critical understanding of recovery, collaborative working and clientcentred approaches in relation to all aspects of therapeutic process for people with common mental health problems. • KU 3 Demonstrate systematic and critical understanding of a range of social, medical and psychological explanatory models in mental health and mental illness and a practical understanding of diagnostic category systems used in mental health. • KU 4 Demonstrate systematic and critical knowledge of positive risk management. • KU 5 Demonstrate comprehensive and critical knowledge of evidence-based low intensity interventions for people with common mental health problems • KU 6 Demonstrate comprehensive and critical knowledge of social inclusion and non-discriminatory practice. • KU 7 Demonstrate a comprehensive and critical understanding of the roles and responsibilities of the various professional and non-professional workers in primary mental health care. • KU 8 Demonstrate comprehensive and critical knowledge of the complex relationship between health and occupation, employment and wellbeing. • KU 9 Demonstrate comprehensive and critical knowledge, behaviour change theory and its application to common mental health problems
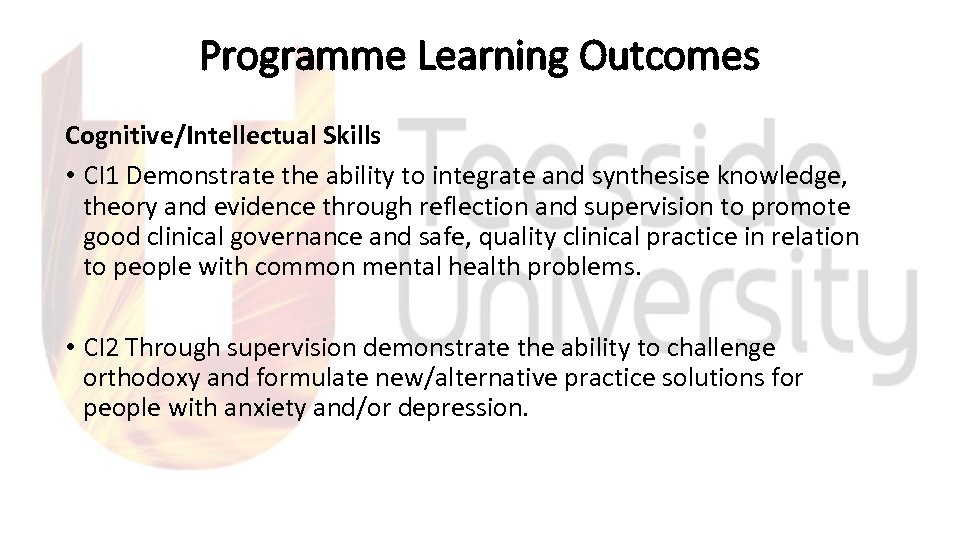 Programme Learning Outcomes Cognitive/Intellectual Skills • CI 1 Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. • CI 2 Through supervision demonstrate the ability to challenge orthodoxy and formulate new/alternative practice solutions for people with anxiety and/or depression.
Programme Learning Outcomes Cognitive/Intellectual Skills • CI 1 Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. • CI 2 Through supervision demonstrate the ability to challenge orthodoxy and formulate new/alternative practice solutions for people with anxiety and/or depression.
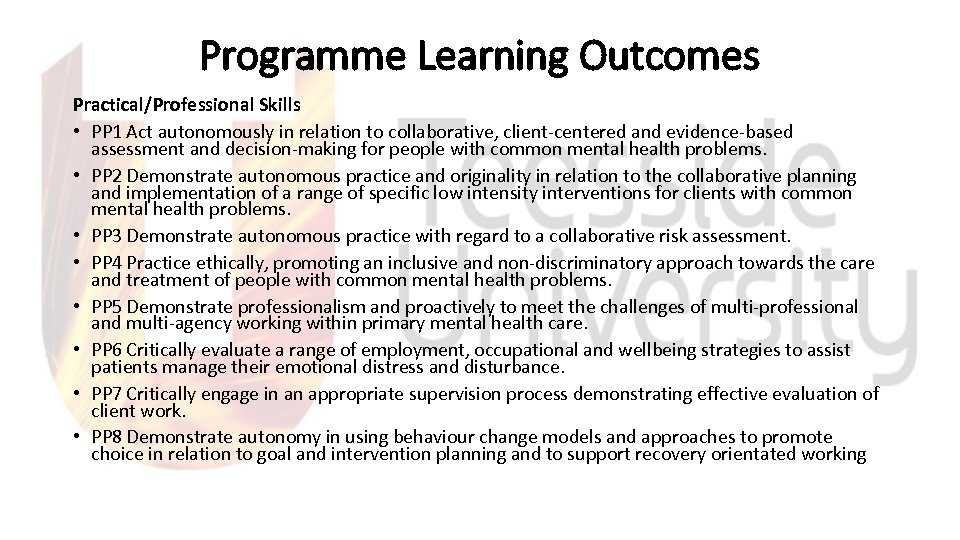 Programme Learning Outcomes Practical/Professional Skills • PP 1 Act autonomously in relation to collaborative, client-centered and evidence-based assessment and decision-making for people with common mental health problems. • PP 2 Demonstrate autonomous practice and originality in relation to the collaborative planning and implementation of a range of specific low intensity interventions for clients with common mental health problems. • PP 3 Demonstrate autonomous practice with regard to a collaborative risk assessment. • PP 4 Practice ethically, promoting an inclusive and non-discriminatory approach towards the care and treatment of people with common mental health problems. • PP 5 Demonstrate professionalism and proactively to meet the challenges of multi-professional and multi-agency working within primary mental health care. • PP 6 Critically evaluate a range of employment, occupational and wellbeing strategies to assist patients manage their emotional distress and disturbance. • PP 7 Critically engage in an appropriate supervision process demonstrating effective evaluation of client work. • PP 8 Demonstrate autonomy in using behaviour change models and approaches to promote choice in relation to goal and intervention planning and to support recovery orientated working
Programme Learning Outcomes Practical/Professional Skills • PP 1 Act autonomously in relation to collaborative, client-centered and evidence-based assessment and decision-making for people with common mental health problems. • PP 2 Demonstrate autonomous practice and originality in relation to the collaborative planning and implementation of a range of specific low intensity interventions for clients with common mental health problems. • PP 3 Demonstrate autonomous practice with regard to a collaborative risk assessment. • PP 4 Practice ethically, promoting an inclusive and non-discriminatory approach towards the care and treatment of people with common mental health problems. • PP 5 Demonstrate professionalism and proactively to meet the challenges of multi-professional and multi-agency working within primary mental health care. • PP 6 Critically evaluate a range of employment, occupational and wellbeing strategies to assist patients manage their emotional distress and disturbance. • PP 7 Critically engage in an appropriate supervision process demonstrating effective evaluation of client work. • PP 8 Demonstrate autonomy in using behaviour change models and approaches to promote choice in relation to goal and intervention planning and to support recovery orientated working
 Programme Learning Outcomes Key Transferable Skills • KT 1 Communicate complex professional issues clearly to specialist and non-specialist audiences. • KT 2 Demonstrate the independent learning ability required for continuing professional development.
Programme Learning Outcomes Key Transferable Skills • KT 1 Communicate complex professional issues clearly to specialist and non-specialist audiences. • KT 2 Demonstrate the independent learning ability required for continuing professional development.
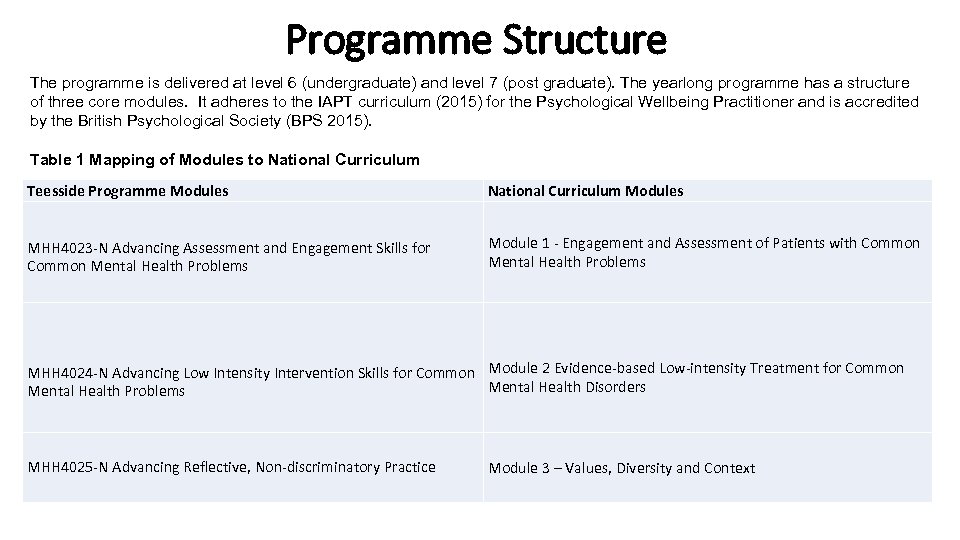 Programme Structure The programme is delivered at level 6 (undergraduate) and level 7 (post graduate). The yearlong programme has a structure of three core modules. It adheres to the IAPT curriculum (2015) for the Psychological Wellbeing Practitioner and is accredited by the British Psychological Society (BPS 2015). Table 1 Mapping of Modules to National Curriculum Teesside Programme Modules National Curriculum Modules MHH 4023 -N Advancing Assessment and Engagement Skills for Common Mental Health Problems Module 1 - Engagement and Assessment of Patients with Common Mental Health Problems MHH 4024 -N Advancing Low Intensity Intervention Skills for Common Module 2 Evidence-based Low-intensity Treatment for Common Mental Health Disorders Mental Health Problems MHH 4025 -N Advancing Reflective, Non-discriminatory Practice Module 3 – Values, Diversity and Context
Programme Structure The programme is delivered at level 6 (undergraduate) and level 7 (post graduate). The yearlong programme has a structure of three core modules. It adheres to the IAPT curriculum (2015) for the Psychological Wellbeing Practitioner and is accredited by the British Psychological Society (BPS 2015). Table 1 Mapping of Modules to National Curriculum Teesside Programme Modules National Curriculum Modules MHH 4023 -N Advancing Assessment and Engagement Skills for Common Mental Health Problems Module 1 - Engagement and Assessment of Patients with Common Mental Health Problems MHH 4024 -N Advancing Low Intensity Intervention Skills for Common Module 2 Evidence-based Low-intensity Treatment for Common Mental Health Disorders Mental Health Problems MHH 4025 -N Advancing Reflective, Non-discriminatory Practice Module 3 – Values, Diversity and Context
 Programme Delivery • The curriculum includes both classroom and workplace learning delivered in 45 days across the three modules. There will be an additional five day induction totaling 50 days overall. You will also have access to a range of university resources to support your learning and your biggest learning resource is you. It is essential that you take responsibility for your own learning and make the most of the learning opportunities presented to you.
Programme Delivery • The curriculum includes both classroom and workplace learning delivered in 45 days across the three modules. There will be an additional five day induction totaling 50 days overall. You will also have access to a range of university resources to support your learning and your biggest learning resource is you. It is essential that you take responsibility for your own learning and make the most of the learning opportunities presented to you.
 Programme Induction • During induction you will be enrolled as a Teesside University student and will be allocated an IT account. This will enable you to access the Modules Blackboard site where you will be able to access University, Programme, Module and Student information including Student Essential Guide; Supervisor Handbook; Module Guide; Campus Maps; Learning Materials; Assessment Information • During induction there will be a number of activities designed for you to get to know each other and also activities to introduce role-play as well as being video recorded. • There will be a supervisor workshop (your supervisor should attend this with you) in order to gain further information about the role of supervision in relation to your learning and for your supervisor to clarify any issues that they have regarding the role of supervisor. • You will be given information to support your learning, including consideration of degree/masters study skills. There a number of university resources available to support your learning.
Programme Induction • During induction you will be enrolled as a Teesside University student and will be allocated an IT account. This will enable you to access the Modules Blackboard site where you will be able to access University, Programme, Module and Student information including Student Essential Guide; Supervisor Handbook; Module Guide; Campus Maps; Learning Materials; Assessment Information • During induction there will be a number of activities designed for you to get to know each other and also activities to introduce role-play as well as being video recorded. • There will be a supervisor workshop (your supervisor should attend this with you) in order to gain further information about the role of supervision in relation to your learning and for your supervisor to clarify any issues that they have regarding the role of supervisor. • You will be given information to support your learning, including consideration of degree/masters study skills. There a number of university resources available to support your learning.
 Attendance and Absence • Attendance and Absence • 100 % classroom attendance is a requirement of the programme. In certain circumstances leave of absence may be granted, however this must be discussed with the Module Leader and the appropriate documentation completed (slide 59). Equally if you are unable to attend a session because of illness it is important that you inform the Module Leader. Absence will be recorded, monitored and managed following the Schools sickness and absence and fitness to practice procedures. In the case of persistent absence the University can withdraw a student from the programme. • A copy of the teaching timetable for each calendar month and the Students Essential Guide is available to you on the VLE e-learning@tees site in order for you to manage your attendance accordingly. You are expected to commit to this schedule. A session catch up procedure is available for a single absence
Attendance and Absence • Attendance and Absence • 100 % classroom attendance is a requirement of the programme. In certain circumstances leave of absence may be granted, however this must be discussed with the Module Leader and the appropriate documentation completed (slide 59). Equally if you are unable to attend a session because of illness it is important that you inform the Module Leader. Absence will be recorded, monitored and managed following the Schools sickness and absence and fitness to practice procedures. In the case of persistent absence the University can withdraw a student from the programme. • A copy of the teaching timetable for each calendar month and the Students Essential Guide is available to you on the VLE e-learning@tees site in order for you to manage your attendance accordingly. You are expected to commit to this schedule. A session catch up procedure is available for a single absence
 Learning Resources • The Learning Hub, which is located on the ground floor of the Library where guidance is offered to all students on developing their skills as independent learners. • • The Library website http: //www. tees. ac. uk/lis/ provides details of services available and gives you access to wide range of electronic learning resources such as the catalogue, subject guides, searchable databases, electronic books and electronic journals. Online information on topics such as referencing, writing essays and information literacy can also be accessed electronically as well as online tutorials and fact sheets or you can contact the Library by telephoning 01642 342100
Learning Resources • The Learning Hub, which is located on the ground floor of the Library where guidance is offered to all students on developing their skills as independent learners. • • The Library website http: //www. tees. ac. uk/lis/ provides details of services available and gives you access to wide range of electronic learning resources such as the catalogue, subject guides, searchable databases, electronic books and electronic journals. Online information on topics such as referencing, writing essays and information literacy can also be accessed electronically as well as online tutorials and fact sheets or you can contact the Library by telephoning 01642 342100
 Learning Resources • There is an electronic Blackboard for each of the three modules. You can locate module information, learning materials, timetables, assessment information and announcements. The module leader will also send emails regarding the module via Blackboard to your student email address • Tutorial support is available throughout the programme and you are encouraged to utilise this support. Please refer to the Student’s Essential Guide for guidelines regarding tutorial support.
Learning Resources • There is an electronic Blackboard for each of the three modules. You can locate module information, learning materials, timetables, assessment information and announcements. The module leader will also send emails regarding the module via Blackboard to your student email address • Tutorial support is available throughout the programme and you are encouraged to utilise this support. Please refer to the Student’s Essential Guide for guidelines regarding tutorial support.
 Making the Most of Your Learning Experience • At the beginning of each module make sure that you are clear about the timetable, learning outcomes, content and what is expected from you • Make sure that you fully understand the assessment requirement, including criteria and submission details. Make use of all recommended materials and resources (guides available via elearning tees)
Making the Most of Your Learning Experience • At the beginning of each module make sure that you are clear about the timetable, learning outcomes, content and what is expected from you • Make sure that you fully understand the assessment requirement, including criteria and submission details. Make use of all recommended materials and resources (guides available via elearning tees)
 Classroom Learning • There will be a range of strategies used to support your learning in the classroom including short lectures, presentations, role-plays and other activities. However your active participation is essential and you are expected to: • Share your experiences and learning with other students (without breaching client confidentiality) • Deliver presentations and are encouraged to use effective information giving techniques • Use self-administered workbooks (electronic and manual) that are designed to support learning in relation to subject knowledge whilst also encouraging students to reflect upon the use of self-help strategies • Participate in problem based learning to develop decision making and problem solving skills
Classroom Learning • There will be a range of strategies used to support your learning in the classroom including short lectures, presentations, role-plays and other activities. However your active participation is essential and you are expected to: • Share your experiences and learning with other students (without breaching client confidentiality) • Deliver presentations and are encouraged to use effective information giving techniques • Use self-administered workbooks (electronic and manual) that are designed to support learning in relation to subject knowledge whilst also encouraging students to reflect upon the use of self-help strategies • Participate in problem based learning to develop decision making and problem solving skills
 Classroom Learning • Complete directed practice tasks in the workplace to encourage skill application and practice • Use personal reflection and personal development planning • Participate fully in simulation activities and make use of feedback from peers, module tutors and practice supervisors • Be challenged in order to develop emotional intelligence • Use self-assessment tools (technical and emotional intelligence skills) • Be gradually exposed to being video recorded in tasks, activities and role-play
Classroom Learning • Complete directed practice tasks in the workplace to encourage skill application and practice • Use personal reflection and personal development planning • Participate fully in simulation activities and make use of feedback from peers, module tutors and practice supervisors • Be challenged in order to develop emotional intelligence • Use self-assessment tools (technical and emotional intelligence skills) • Be gradually exposed to being video recorded in tasks, activities and role-play
 Reflection and Personal Development Planning • The program is designed so that you can become a more confident and independent practitioner. It also aims for you to be able to plan and evaluate your own development. There a number of opportunities throughout each module for you to reflect and plan personal development e. g. : • • • Participation in role-plays Completion practice tasks Supervision in practice Working with clients Learning Contracts
Reflection and Personal Development Planning • The program is designed so that you can become a more confident and independent practitioner. It also aims for you to be able to plan and evaluate your own development. There a number of opportunities throughout each module for you to reflect and plan personal development e. g. : • • • Participation in role-plays Completion practice tasks Supervision in practice Working with clients Learning Contracts
 Work Based Learning • Theoretical learning gained in the classroom has to be applied in practice and it is essential that you be provided with opportunities to develop skills and practices that underpin your role as a psychological well-being practitioner. • Equally knowledge is generated in the workplace through research and development activities and it is important that this learning is accessed and integrated into your own practice.
Work Based Learning • Theoretical learning gained in the classroom has to be applied in practice and it is essential that you be provided with opportunities to develop skills and practices that underpin your role as a psychological well-being practitioner. • Equally knowledge is generated in the workplace through research and development activities and it is important that this learning is accessed and integrated into your own practice.
 Work Based Learning • A substantial part of this programme involves work-based learning and there a number of important features for you to be aware of, which are briefly outlined here and discussed in more detail as required in the module guides • • Approved training requirements Supervision hours Practice supervisor Directed learning tasks Clinical hours Assessed clinical practice outcomes
Work Based Learning • A substantial part of this programme involves work-based learning and there a number of important features for you to be aware of, which are briefly outlined here and discussed in more detail as required in the module guides • • Approved training requirements Supervision hours Practice supervisor Directed learning tasks Clinical hours Assessed clinical practice outcomes
 Approved Sites Requirements • The programme requires for you to be working in a fully functioning IAPT service so as part of the quality assurance process, services must meet the appropriate standards • In order to host trainee practitioners (IAPT 2015). The local ‘IAPT Consortium’ with bi-monthly meetings has been created to discuss generic programme and/or workplace issues and development
Approved Sites Requirements • The programme requires for you to be working in a fully functioning IAPT service so as part of the quality assurance process, services must meet the appropriate standards • In order to host trainee practitioners (IAPT 2015). The local ‘IAPT Consortium’ with bi-monthly meetings has been created to discuss generic programme and/or workplace issues and development
 Supervision • It is crucial for the safe and effective practice and learning and you must receive clinical skills and clinical case management supervision: • Clinical Case Management Supervision – at least 1 -hour every week in which all patients on the caseload are reviewed. • Clinical Skills Supervision - 1 -hour, every 2 weeks which could be provided on an individual basis or as part of a group. • Supervision Hours • By the end of the programme you must evidence at least 40 hours of supervision. Refer to the Assessment Strategy section of this guide for further information regarding this.
Supervision • It is crucial for the safe and effective practice and learning and you must receive clinical skills and clinical case management supervision: • Clinical Case Management Supervision – at least 1 -hour every week in which all patients on the caseload are reviewed. • Clinical Skills Supervision - 1 -hour, every 2 weeks which could be provided on an individual basis or as part of a group. • Supervision Hours • By the end of the programme you must evidence at least 40 hours of supervision. Refer to the Assessment Strategy section of this guide for further information regarding this.
 Supervisor Requirements • Your supervisor in practice will have a very busy workload however there full participation is essential for your learning and assessment. There a number of modalities and opportunities to help keep your supervisor informed and supported. • Supervision module – this is a requirement for an accredited PWP supervisor. The module is delivered annually commencing in the January. • Supervisor workshop – this takes place during induction. It is designed to keep supervisors up-to-date with PWP education and training requirements
Supervisor Requirements • Your supervisor in practice will have a very busy workload however there full participation is essential for your learning and assessment. There a number of modalities and opportunities to help keep your supervisor informed and supported. • Supervision module – this is a requirement for an accredited PWP supervisor. The module is delivered annually commencing in the January. • Supervisor workshop – this takes place during induction. It is designed to keep supervisors up-to-date with PWP education and training requirements
 Supervisor Requirements • Supervisor handbook – this document Is available online by your blackboard site all the supervisors support site • Online supervisor support site – an online support site to keep supervisors up-to-date with information about the programme and its modules • Tripartite communication – Communication between tutor, student and supervisor using electronic, telephone or face to face methods
Supervisor Requirements • Supervisor handbook – this document Is available online by your blackboard site all the supervisors support site • Online supervisor support site – an online support site to keep supervisors up-to-date with information about the programme and its modules • Tripartite communication – Communication between tutor, student and supervisor using electronic, telephone or face to face methods
 Directed Learning tasks • One full day each week of your work-based learning will be directed by the university through specific tasks and activities, for example shadowing and observation; role-play with peers and supervisors and colleagues; supervised practice; reflection and directed problembased learning. A ‘Directed Practice Learning Task Booklet’ (that outlines the task and essential evidence) is required for completion during each module.
Directed Learning tasks • One full day each week of your work-based learning will be directed by the university through specific tasks and activities, for example shadowing and observation; role-play with peers and supervisors and colleagues; supervised practice; reflection and directed problembased learning. A ‘Directed Practice Learning Task Booklet’ (that outlines the task and essential evidence) is required for completion during each module.
 Clinical Contact Hours • In addition to the learning tasks you are required to evidence a minimum of 80 clinical contact hours with patients (face-to-face or on the telephone) within an IAPT service. You will not be expected to work with clients independently immediately. It is important that you approach client work gradually and in a planned manner with your supervisor. A learning contract will be used in order to facilitate this process.
Clinical Contact Hours • In addition to the learning tasks you are required to evidence a minimum of 80 clinical contact hours with patients (face-to-face or on the telephone) within an IAPT service. You will not be expected to work with clients independently immediately. It is important that you approach client work gradually and in a planned manner with your supervisor. A learning contract will be used in order to facilitate this process.
 Clinical Contact Hours • The client should be aware of your trainee status and this should be done following your organisations policies and procedures • Client confidentiality should be maintained at all times and clients should not be discussed without obtaining consent following the correct University Procedures. • It is essential that you acknowledge and work within your own limitations and abilities when working with clients. The Practice Supervisor and the module tutors are available for advice and support regarding client work.
Clinical Contact Hours • The client should be aware of your trainee status and this should be done following your organisations policies and procedures • Client confidentiality should be maintained at all times and clients should not be discussed without obtaining consent following the correct University Procedures. • It is essential that you acknowledge and work within your own limitations and abilities when working with clients. The Practice Supervisor and the module tutors are available for advice and support regarding client work.
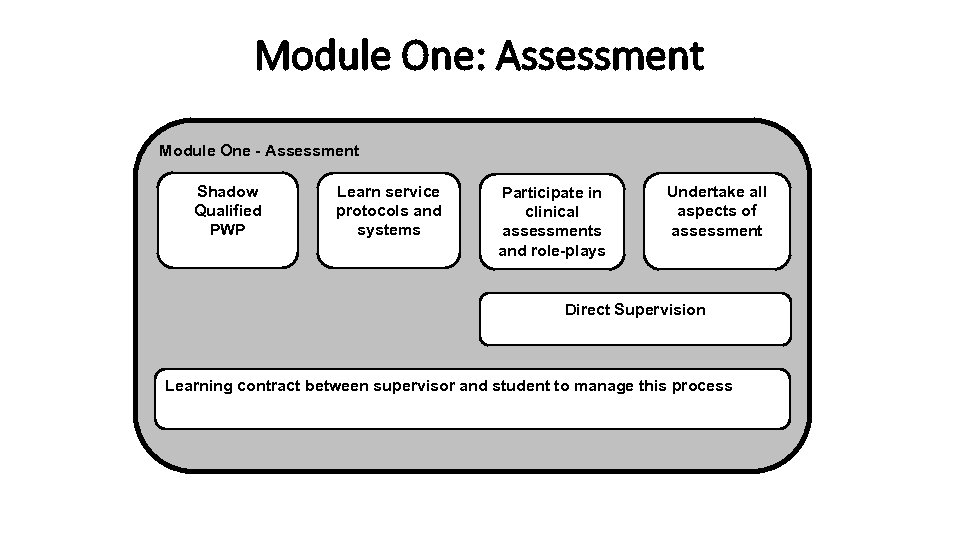 Module One: Assessment Module One - Assessment Shadow Qualified PWP Learn service protocols and systems Participate in clinical assessments and role-plays Undertake all aspects of assessment Direct Supervision Learning contract between supervisor and student to manage this process
Module One: Assessment Module One - Assessment Shadow Qualified PWP Learn service protocols and systems Participate in clinical assessments and role-plays Undertake all aspects of assessment Direct Supervision Learning contract between supervisor and student to manage this process
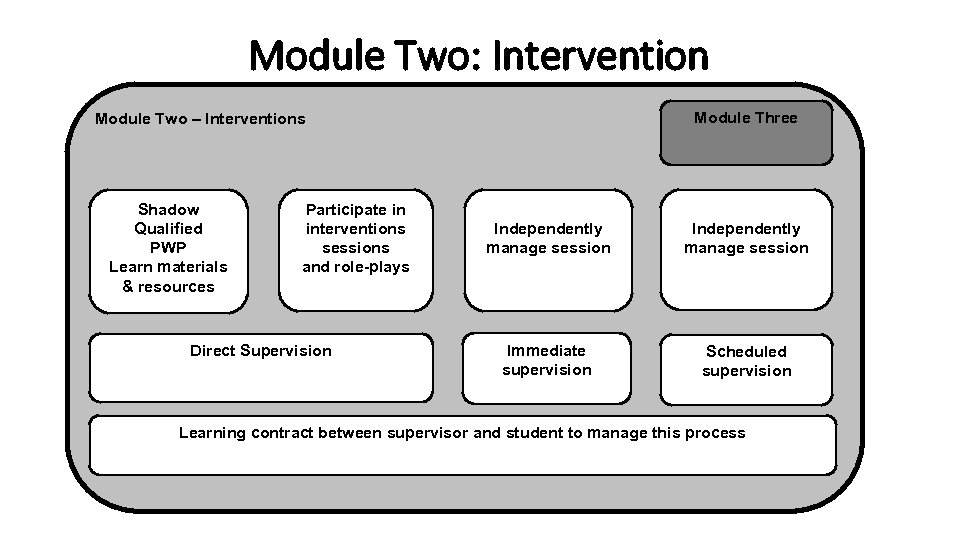 Module Two: Intervention Module Three Module Two – Interventions Shadow Qualified PWP Learn materials & resources Participate in interventions sessions and role-plays Direct Supervision Independently manage session Immediate supervision Scheduled supervision Learning contract between supervisor and student to manage this process
Module Two: Intervention Module Three Module Two – Interventions Shadow Qualified PWP Learn materials & resources Participate in interventions sessions and role-plays Direct Supervision Independently manage session Immediate supervision Scheduled supervision Learning contract between supervisor and student to manage this process
 Clinical Practice Outcomes • In order to pass the programme, you must demonstrate achievement of the ‘Clinical Practice Outcomes’ (PWP Curriculum 2015) • Your Practice Supervisor will both support and assess you in relation to this (for example direct observation, the use of audio tapes of clinical interviews, and reflections). • It is your responsibility to provide evidence of achievement to the supervisor so that the supervisor is satisfied that you have met the outcomes. For further detail refer to the module guide
Clinical Practice Outcomes • In order to pass the programme, you must demonstrate achievement of the ‘Clinical Practice Outcomes’ (PWP Curriculum 2015) • Your Practice Supervisor will both support and assess you in relation to this (for example direct observation, the use of audio tapes of clinical interviews, and reflections). • It is your responsibility to provide evidence of achievement to the supervisor so that the supervisor is satisfied that you have met the outcomes. For further detail refer to the module guide
 Clinical Practice Outcomes • Module One • Demonstrates competency in undertaking and recording a range of assessment formats. This should include both triage within an IAPT service and problem focused assessments. • Demonstrates experience and competence in the assessment of presenting problems across a range of problem descriptor including depression and two or more anxiety disorders. • Demonstrates the common factor competencies necessary to engage patients across the range of assessment formats
Clinical Practice Outcomes • Module One • Demonstrates competency in undertaking and recording a range of assessment formats. This should include both triage within an IAPT service and problem focused assessments. • Demonstrates experience and competence in the assessment of presenting problems across a range of problem descriptor including depression and two or more anxiety disorders. • Demonstrates the common factor competencies necessary to engage patients across the range of assessment formats
 Clinical Practice Outcomes • Module Two • Demonstrates experience and competence in the selection and delivery of treatment of a range of presenting problems using evidence based low- intensity interventions across a range of problem descriptor including depression and two or more anxiety disorders • Demonstrates the ability to use common factor competencies to manage emotional distress and maintain therapeutic alliances to support patients using low-intensity interventions • Demonstrates high quality case recording and systematic evaluation of the process and outcomes of mental health interventions, adapting care on the basis of these evaluations
Clinical Practice Outcomes • Module Two • Demonstrates experience and competence in the selection and delivery of treatment of a range of presenting problems using evidence based low- intensity interventions across a range of problem descriptor including depression and two or more anxiety disorders • Demonstrates the ability to use common factor competencies to manage emotional distress and maintain therapeutic alliances to support patients using low-intensity interventions • Demonstrates high quality case recording and systematic evaluation of the process and outcomes of mental health interventions, adapting care on the basis of these evaluations
 Clinical Practice Outcomes • Module Three • Demonstrates the ability to engage with people from diverse demographic, social and cultural backgrounds in assessment and low-intensity interventions. This could include adaptations to practice working with older adults, using interpretation services/self-help materials for people whose first language is not English, and/or adapting self-help materials for people with learning or literacy difficulties. • Demonstrates the ability to effectively manage a caseload including referral to step up, employment and signposted services • Demonstrates the ability to use supervision to the benefit of effective (a) case management and (b) clinical skills development. This should include: a) a report on a case management supervision session demonstrating ability to review caseload, bring patients at agreed pre-determined thresholds and provide comprehensive and succinct case material; b) a report on use of clinical skills supervision including details of clinical skills questions brought, learning and implementation.
Clinical Practice Outcomes • Module Three • Demonstrates the ability to engage with people from diverse demographic, social and cultural backgrounds in assessment and low-intensity interventions. This could include adaptations to practice working with older adults, using interpretation services/self-help materials for people whose first language is not English, and/or adapting self-help materials for people with learning or literacy difficulties. • Demonstrates the ability to effectively manage a caseload including referral to step up, employment and signposted services • Demonstrates the ability to use supervision to the benefit of effective (a) case management and (b) clinical skills development. This should include: a) a report on a case management supervision session demonstrating ability to review caseload, bring patients at agreed pre-determined thresholds and provide comprehensive and succinct case material; b) a report on use of clinical skills supervision including details of clinical skills questions brought, learning and implementation.
 Assessment Strategy • The assessment strategy has been developed to meet the standards of the National Curriculum for Psychological wellbeing practitioners (IAPT 2015). it is also important to have an accurate overview of your assessment schedule throughout your studies. The table on the next slide summarises the assessment requirements for this programme. • Formative and Summative Assessment • The aim of formative assessment is to monitor your progress and provide feedback that you can use to improve your learning and performance. Summative assessment is used to evaluate your overall progress and will determine your achievement of the learning outcomes for the module.
Assessment Strategy • The assessment strategy has been developed to meet the standards of the National Curriculum for Psychological wellbeing practitioners (IAPT 2015). it is also important to have an accurate overview of your assessment schedule throughout your studies. The table on the next slide summarises the assessment requirements for this programme. • Formative and Summative Assessment • The aim of formative assessment is to monitor your progress and provide feedback that you can use to improve your learning and performance. Summative assessment is used to evaluate your overall progress and will determine your achievement of the learning outcomes for the module.
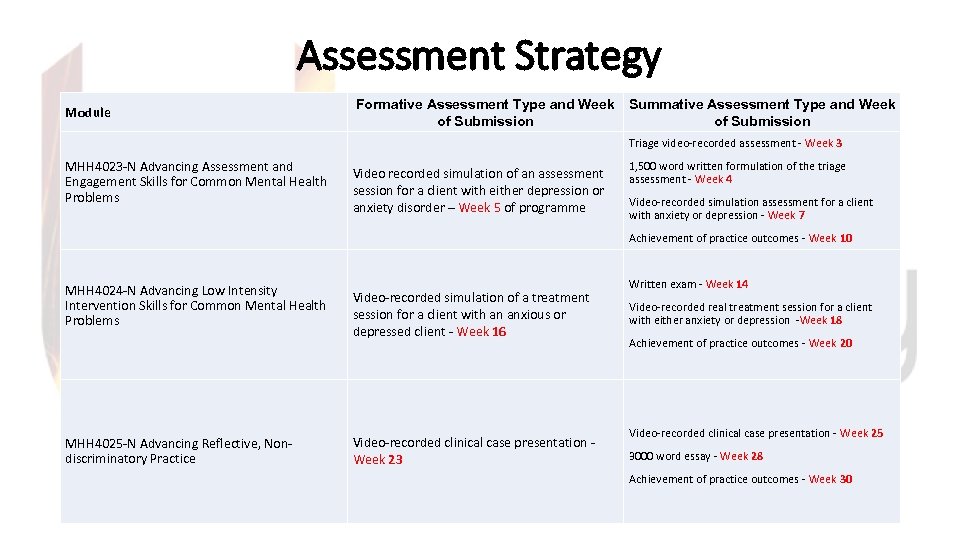 Assessment Strategy Module • . Formative Assessment Type and Week Summative Assessment Type and Week of Submission Triage video-recorded assessment - Week 3 MHH 4023 -N Advancing Assessment and Engagement Skills for Common Mental Health Problems Video recorded simulation of an assessment session for a client with either depression or anxiety disorder – Week 5 of programme 1, 500 word written formulation of the triage assessment - Week 4 Video-recorded simulation assessment for a client with anxiety or depression - Week 7 Achievement of practice outcomes - Week 10 MHH 4024 -N Advancing Low Intensity Intervention Skills for Common Mental Health Problems Video-recorded simulation of a treatment session for a client with an anxious or depressed client - Week 16 MHH 4025 -N Advancing Reflective, Nondiscriminatory Practice Video-recorded clinical case presentation - Week 23 Written exam - Week 14 Video-recorded real treatment session for a client with either anxiety or depression -Week 18 Achievement of practice outcomes - Week 20 Video-recorded clinical case presentation - Week 25 3000 word essay - Week 28 Achievement of practice outcomes - Week 30
Assessment Strategy Module • . Formative Assessment Type and Week Summative Assessment Type and Week of Submission Triage video-recorded assessment - Week 3 MHH 4023 -N Advancing Assessment and Engagement Skills for Common Mental Health Problems Video recorded simulation of an assessment session for a client with either depression or anxiety disorder – Week 5 of programme 1, 500 word written formulation of the triage assessment - Week 4 Video-recorded simulation assessment for a client with anxiety or depression - Week 7 Achievement of practice outcomes - Week 10 MHH 4024 -N Advancing Low Intensity Intervention Skills for Common Mental Health Problems Video-recorded simulation of a treatment session for a client with an anxious or depressed client - Week 16 MHH 4025 -N Advancing Reflective, Nondiscriminatory Practice Video-recorded clinical case presentation - Week 23 Written exam - Week 14 Video-recorded real treatment session for a client with either anxiety or depression -Week 18 Achievement of practice outcomes - Week 20 Video-recorded clinical case presentation - Week 25 3000 word essay - Week 28 Achievement of practice outcomes - Week 30
 Consent • It is essential that you obtain full consent from clients, relatives, carers and staff working in practice before referring to personal information in your assignments. The procedure to follow is available in the Students Essential Guide
Consent • It is essential that you obtain full consent from clients, relatives, carers and staff working in practice before referring to personal information in your assignments. The procedure to follow is available in the Students Essential Guide
 Assessment Criteria • Assessment Criteria for level 7 • Detailed guidance regarding level 7 assessment criteria, referencing guidelines, presentation guidelines, academic writing guidelines, student support and other assessment information can be found in the SOHSC Student Essential Guide • Additional information on module-specific assessment criteria including submission dates and arrangements, can be found in the Module Guides available on Blackboard
Assessment Criteria • Assessment Criteria for level 7 • Detailed guidance regarding level 7 assessment criteria, referencing guidelines, presentation guidelines, academic writing guidelines, student support and other assessment information can be found in the SOHSC Student Essential Guide • Additional information on module-specific assessment criteria including submission dates and arrangements, can be found in the Module Guides available on Blackboard
 Assessment Criteria • Reasonable Adjustments • Reasonable adjustments will be made to assessment strategies on an individual basis if necessary, to ensure that any students with special educational needs are not disadvantaged link to disability services. Additional support may be obtained from the School’s Disability Co- coordinator: Mary van Loo, Senior Lecturer, M. Vanloo@tees. ac. uk • Deferrals and Extensions • Information regarding mitigation, short and long extensions can be found in the Students Essential Guide
Assessment Criteria • Reasonable Adjustments • Reasonable adjustments will be made to assessment strategies on an individual basis if necessary, to ensure that any students with special educational needs are not disadvantaged link to disability services. Additional support may be obtained from the School’s Disability Co- coordinator: Mary van Loo, Senior Lecturer, M. Vanloo@tees. ac. uk • Deferrals and Extensions • Information regarding mitigation, short and long extensions can be found in the Students Essential Guide
 Accessing Results • Accessing Assessment Results and Feedback • It is your responsibility to access your results • Assessment feedback can be found at SOHSC Intranet Site • Ratified Results can be found at https: //e-vision. tees. ac. uk/you will be able to log-in using your usual username and password. You will be informed by email when online access to your ratified results is available. This notification will be sent to your University email account confirming that your results are available online. You will not be able to access your results before you have received this email.
Accessing Results • Accessing Assessment Results and Feedback • It is your responsibility to access your results • Assessment feedback can be found at SOHSC Intranet Site • Ratified Results can be found at https: //e-vision. tees. ac. uk/you will be able to log-in using your usual username and password. You will be informed by email when online access to your ratified results is available. This notification will be sent to your University email account confirming that your results are available online. You will not be able to access your results before you have received this email.
 External Examiner • An External Examiner is lecturer from another University with experience of teaching and assessing PWP trainees who offers an independent view as to whether the work of students on the course is of the correct standard. The External Examiner does this by looking at a sample of work (e. g. assignments, exam answers, role-plays), discussing the work with your lecturers and attending the Assessment Boards to endorse results. The external examiner produces an annual report as part of programme evaluation and development, which highlights strengths of the programme and areas for development.
External Examiner • An External Examiner is lecturer from another University with experience of teaching and assessing PWP trainees who offers an independent view as to whether the work of students on the course is of the correct standard. The External Examiner does this by looking at a sample of work (e. g. assignments, exam answers, role-plays), discussing the work with your lecturers and attending the Assessment Boards to endorse results. The external examiner produces an annual report as part of programme evaluation and development, which highlights strengths of the programme and areas for development.
 Student feedback, Representative & Progression Student feedback • is an essential aspect of programme evaluation so the programme team can be assured that the course is providing a meaningful and appropriate learning experience for the student PWP. Your feedback is very important to us and we will invite you to give constructive feedback on your learning experiences both formally and informally at various points in your programme of study, for example by evaluating your University teaching during and at the end of each module. Student Representative • Within the first few days of your programme you will be given information relating to the nomination of a programme student representative. Further information regarding this may be found within the School of Health & Social Care Student Essential Guide. Progression • On completion of the programme you will be invited to attend an ‘Exit Interview’ whereby you will be able to discuss your future plans with regards to further study. You will then be signposted to relevant student advice services.
Student feedback, Representative & Progression Student feedback • is an essential aspect of programme evaluation so the programme team can be assured that the course is providing a meaningful and appropriate learning experience for the student PWP. Your feedback is very important to us and we will invite you to give constructive feedback on your learning experiences both formally and informally at various points in your programme of study, for example by evaluating your University teaching during and at the end of each module. Student Representative • Within the first few days of your programme you will be given information relating to the nomination of a programme student representative. Further information regarding this may be found within the School of Health & Social Care Student Essential Guide. Progression • On completion of the programme you will be invited to attend an ‘Exit Interview’ whereby you will be able to discuss your future plans with regards to further study. You will then be signposted to relevant student advice services.
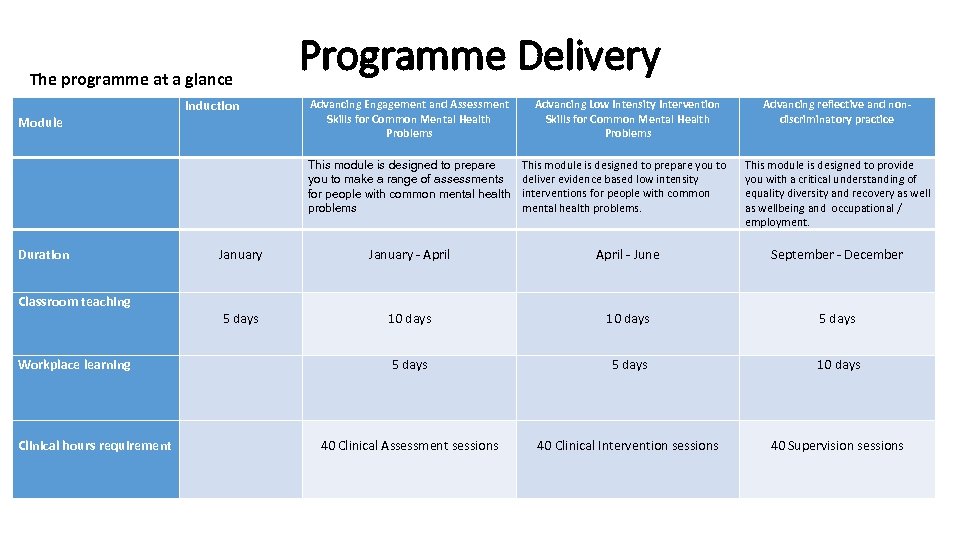 Programme Delivery The programme at a glance Module Induction Advancing Engagement and Assessment Skills for Common Mental Health Problems Advancing Low Intensity Intervention Skills for Common Mental Health Problems Advancing reflective and non- discriminatory practice This module is designed to prepare you to make a range of assessments for people with common mental health problems This module is designed to prepare you to deliver evidence based low intensity interventions for people with common mental health problems. This module is designed to provide you with a critical understanding of equality diversity and recovery as wellbeing and occupational / employment. Duration January - April - June September - December Classroom teaching 5 days 10 days 5 days Workplace learning 5 days 10 days Clinical hours requirement 40 Clinical Assessment sessions 40 Clinical Intervention sessions 40 Supervision sessions
Programme Delivery The programme at a glance Module Induction Advancing Engagement and Assessment Skills for Common Mental Health Problems Advancing Low Intensity Intervention Skills for Common Mental Health Problems Advancing reflective and non- discriminatory practice This module is designed to prepare you to make a range of assessments for people with common mental health problems This module is designed to prepare you to deliver evidence based low intensity interventions for people with common mental health problems. This module is designed to provide you with a critical understanding of equality diversity and recovery as wellbeing and occupational / employment. Duration January - April - June September - December Classroom teaching 5 days 10 days 5 days Workplace learning 5 days 10 days Clinical hours requirement 40 Clinical Assessment sessions 40 Clinical Intervention sessions 40 Supervision sessions
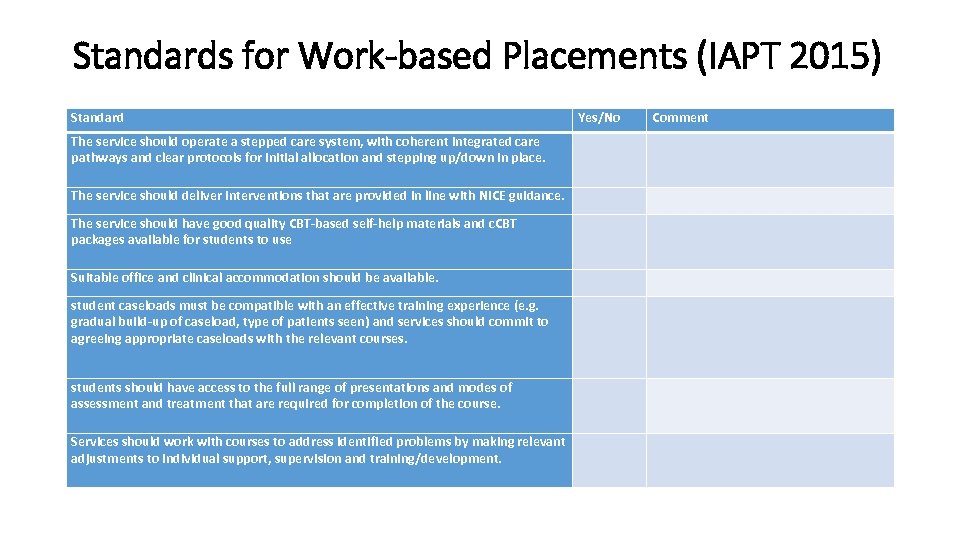 Standards for Work-based Placements (IAPT 2015) Standard Yes/No Comment The service should operate a stepped care system, with coherent integrated care pathways and clear protocols for initial allocation and stepping up/down in place. The service should deliver interventions that are provided in line with NICE guidance. The service should have good quality CBT-based self-help materials and c. CBT packages available for students to use Suitable office and clinical accommodation should be available. student caseloads must be compatible with an effective training experience (e. g. gradual build-up of caseload, type of patients seen) and services should commit to agreeing appropriate caseloads with the relevant courses. students should have access to the full range of presentations and modes of assessment and treatment that are required for completion of the course. Services should work with courses to address identified problems by making relevant adjustments to individual support, supervision and training/development.
Standards for Work-based Placements (IAPT 2015) Standard Yes/No Comment The service should operate a stepped care system, with coherent integrated care pathways and clear protocols for initial allocation and stepping up/down in place. The service should deliver interventions that are provided in line with NICE guidance. The service should have good quality CBT-based self-help materials and c. CBT packages available for students to use Suitable office and clinical accommodation should be available. student caseloads must be compatible with an effective training experience (e. g. gradual build-up of caseload, type of patients seen) and services should commit to agreeing appropriate caseloads with the relevant courses. students should have access to the full range of presentations and modes of assessment and treatment that are required for completion of the course. Services should work with courses to address identified problems by making relevant adjustments to individual support, supervision and training/development.
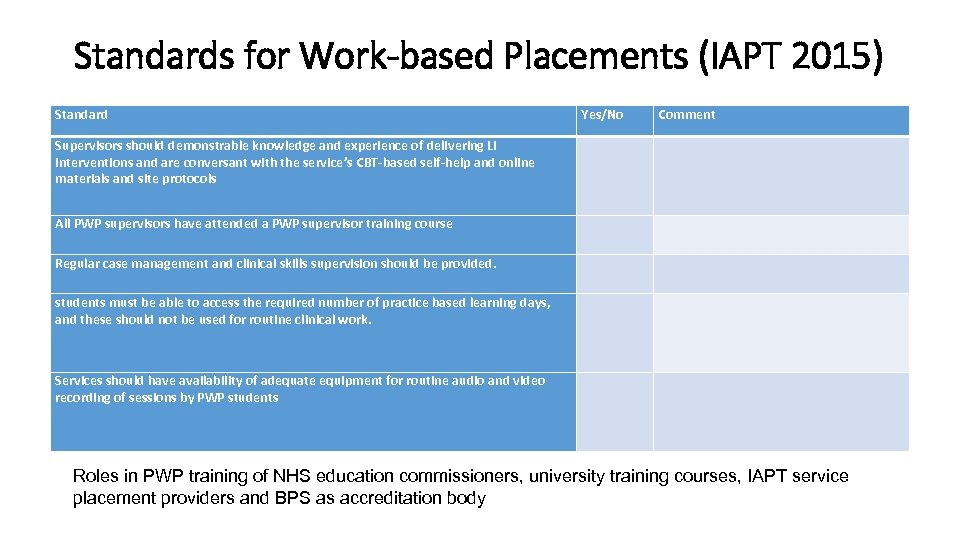 Standards for Work-based Placements (IAPT 2015) Standard Yes/No Comment Supervisors should demonstrable knowledge and experience of delivering LI interventions and are conversant with the service’s CBT-based self-help and online materials and site protocols All PWP supervisors have attended a PWP supervisor training course Regular case management and clinical skills supervision should be provided. students must be able to access the required number of practice based learning days, and these should not be used for routine clinical work. Services should have availability of adequate equipment for routine audio and video recording of sessions by PWP students Roles in PWP training of NHS education commissioners, university training courses, IAPT service placement providers and BPS as accreditation body
Standards for Work-based Placements (IAPT 2015) Standard Yes/No Comment Supervisors should demonstrable knowledge and experience of delivering LI interventions and are conversant with the service’s CBT-based self-help and online materials and site protocols All PWP supervisors have attended a PWP supervisor training course Regular case management and clinical skills supervision should be provided. students must be able to access the required number of practice based learning days, and these should not be used for routine clinical work. Services should have availability of adequate equipment for routine audio and video recording of sessions by PWP students Roles in PWP training of NHS education commissioners, university training courses, IAPT service placement providers and BPS as accreditation body
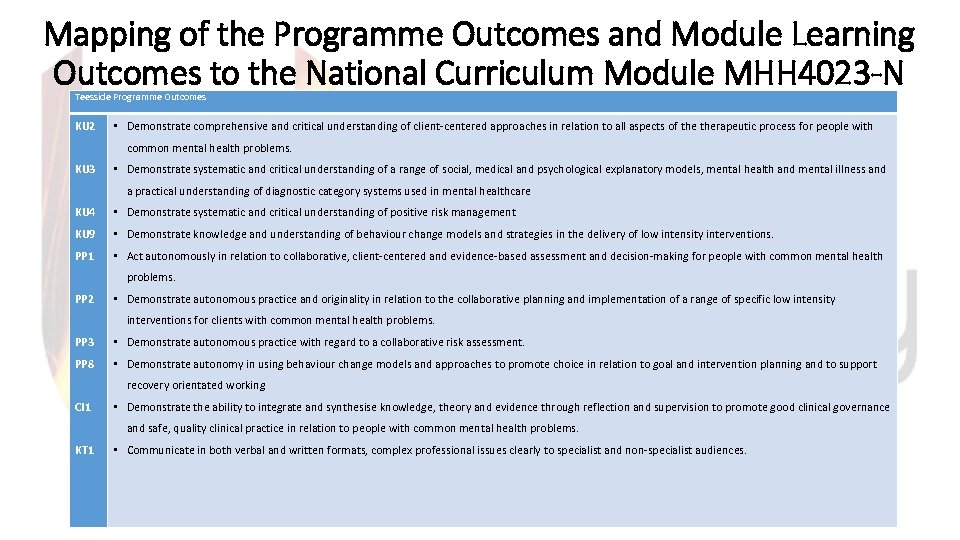 Mapping of the Programme Outcomes and Module Learning Outcomes to the National Curriculum Module MHH 4023 -N Teesside Programme Outcomes KU 2 • Demonstrate comprehensive and critical understanding of client-centered approaches in relation to all aspects of therapeutic process for people with KU 3 common mental health problems. • Demonstrate systematic and critical understanding of a range of social, medical and psychological explanatory models, mental health and mental illness and a practical understanding of diagnostic category systems used in mental healthcare KU 4 • Demonstrate systematic and critical understanding of positive risk management KU 9 • Demonstrate knowledge and understanding of behaviour change models and strategies in the delivery of low intensity interventions. PP 1 • Act autonomously in relation to collaborative, client-centered and evidence-based assessment and decision-making for people with common mental health PP 2 problems. • Demonstrate autonomous practice and originality in relation to the collaborative planning and implementation of a range of specific low intensity interventions for clients with common mental health problems. PP 3 • Demonstrate autonomous practice with regard to a collaborative risk assessment. PP 8 • Demonstrate autonomy in using behaviour change models and approaches to promote choice in relation to goal and intervention planning and to support CI 1 recovery orientated working • Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. KT 1 • Communicate in both verbal and written formats, complex professional issues clearly to specialist and non-specialist audiences.
Mapping of the Programme Outcomes and Module Learning Outcomes to the National Curriculum Module MHH 4023 -N Teesside Programme Outcomes KU 2 • Demonstrate comprehensive and critical understanding of client-centered approaches in relation to all aspects of therapeutic process for people with KU 3 common mental health problems. • Demonstrate systematic and critical understanding of a range of social, medical and psychological explanatory models, mental health and mental illness and a practical understanding of diagnostic category systems used in mental healthcare KU 4 • Demonstrate systematic and critical understanding of positive risk management KU 9 • Demonstrate knowledge and understanding of behaviour change models and strategies in the delivery of low intensity interventions. PP 1 • Act autonomously in relation to collaborative, client-centered and evidence-based assessment and decision-making for people with common mental health PP 2 problems. • Demonstrate autonomous practice and originality in relation to the collaborative planning and implementation of a range of specific low intensity interventions for clients with common mental health problems. PP 3 • Demonstrate autonomous practice with regard to a collaborative risk assessment. PP 8 • Demonstrate autonomy in using behaviour change models and approaches to promote choice in relation to goal and intervention planning and to support CI 1 recovery orientated working • Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. KT 1 • Communicate in both verbal and written formats, complex professional issues clearly to specialist and non-specialist audiences.
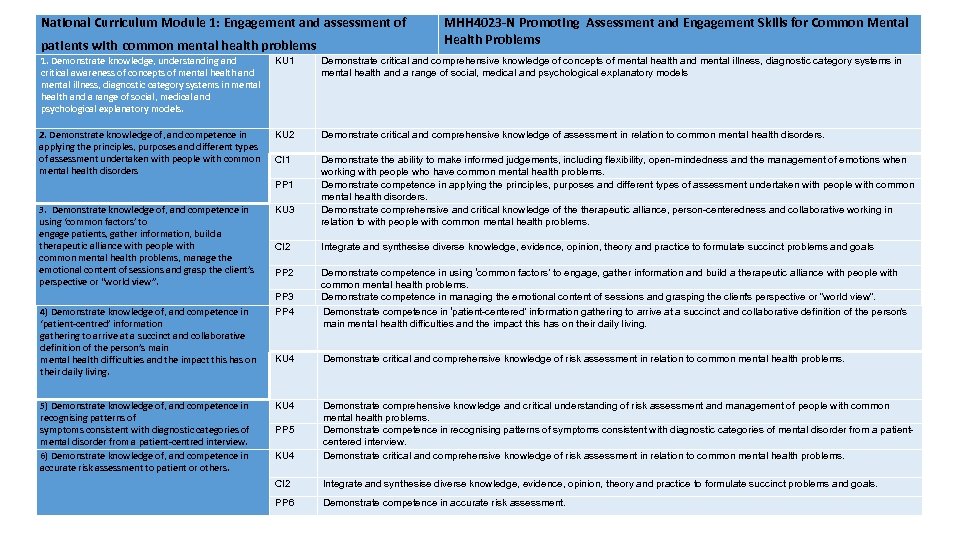 National Curriculum Module 1: Engagement and assessment of MHH 4023 -N Promoting Assessment and Engagement Skills for Common Mental Health Problems patients with common mental health problems 1. Demonstrate knowledge, understanding and KU 1 Demonstrate critical and comprehensive knowledge of concepts of mental health and mental illness, diagnostic category systems in critical awareness of concepts of mental health and mental illness, diagnostic category systems in mental health and a range of social, medical and psychological explanatory models Demonstrate critical and comprehensive knowledge of assessment in relation to common mental health disorders. Demonstrate the ability to make informed judgements, including flexibility, open-mindedness and the management of emotions when working with people who have common mental health problems. Demonstrate competence in applying the principles, purposes and different types of assessment undertaken with people with common mental health disorders. Demonstrate comprehensive and critical knowledge of therapeutic alliance, person-centeredness and collaborative working in relation to with people with common mental health problems. 2. Demonstrate knowledge of, and competence in applying the principles, purposes and different types of assessment undertaken with people with common mental health disorders 3. Demonstrate knowledge of, and competence in using ‘common factors’ to engage patients, gather information, build a therapeutic alliance with people with common mental health problems, manage the emotional content of sessions and grasp the client’s perspective or “world view”. KU 2 4) Demonstrate knowledge of, and competence in ‘patient-centred’ information gathering to arrive at a succinct and collaborative definition of the person’s main mental health difficulties and the impact this has on their daily living. PP 4 Demonstrate competence in ‘patient-centered’ information gathering to arrive at a succinct and collaborative definition of the person ’s main mental health difficulties and the impact this has on their daily living. KU 4 Demonstrate critical and comprehensive knowledge of risk assessment in relation to common mental health problems. 5) Demonstrate knowledge of, and competence in recognising patterns of symptoms consistent with diagnostic categories of mental disorder from a patient-centred interview. 6) Demonstrate knowledge of, and competence in accurate risk assessment to patient or others. KU 4 Demonstrate comprehensive knowledge and critical understanding of risk assessment and management of people with common mental health problems. Demonstrate competence in recognising patterns of symptoms consistent with diagnostic categories of mental disorder from a patientcentered interview. Demonstrate critical and comprehensive knowledge of risk assessment in relation to common mental health problems. CI 2 Integrate and synthesise diverse knowledge, evidence, opinion, theory and practice to formulate succinct problems and goals. PP 6 Demonstrate competence in accurate risk assessment. CI 1 PP 1 KU 3 CI 2 Integrate and synthesise diverse knowledge, evidence, opinion, theory and practice to formulate succinct problems and goals. PP 2 Demonstrate competence in using ‘common factors’ to engage, gather information and build a therapeutic alliance with people with common mental health problems. Demonstrate competence in managing the emotional content of sessions and grasping the clients perspective or “world view”. ’ PP 3 PP 5
National Curriculum Module 1: Engagement and assessment of MHH 4023 -N Promoting Assessment and Engagement Skills for Common Mental Health Problems patients with common mental health problems 1. Demonstrate knowledge, understanding and KU 1 Demonstrate critical and comprehensive knowledge of concepts of mental health and mental illness, diagnostic category systems in critical awareness of concepts of mental health and mental illness, diagnostic category systems in mental health and a range of social, medical and psychological explanatory models Demonstrate critical and comprehensive knowledge of assessment in relation to common mental health disorders. Demonstrate the ability to make informed judgements, including flexibility, open-mindedness and the management of emotions when working with people who have common mental health problems. Demonstrate competence in applying the principles, purposes and different types of assessment undertaken with people with common mental health disorders. Demonstrate comprehensive and critical knowledge of therapeutic alliance, person-centeredness and collaborative working in relation to with people with common mental health problems. 2. Demonstrate knowledge of, and competence in applying the principles, purposes and different types of assessment undertaken with people with common mental health disorders 3. Demonstrate knowledge of, and competence in using ‘common factors’ to engage patients, gather information, build a therapeutic alliance with people with common mental health problems, manage the emotional content of sessions and grasp the client’s perspective or “world view”. KU 2 4) Demonstrate knowledge of, and competence in ‘patient-centred’ information gathering to arrive at a succinct and collaborative definition of the person’s main mental health difficulties and the impact this has on their daily living. PP 4 Demonstrate competence in ‘patient-centered’ information gathering to arrive at a succinct and collaborative definition of the person ’s main mental health difficulties and the impact this has on their daily living. KU 4 Demonstrate critical and comprehensive knowledge of risk assessment in relation to common mental health problems. 5) Demonstrate knowledge of, and competence in recognising patterns of symptoms consistent with diagnostic categories of mental disorder from a patient-centred interview. 6) Demonstrate knowledge of, and competence in accurate risk assessment to patient or others. KU 4 Demonstrate comprehensive knowledge and critical understanding of risk assessment and management of people with common mental health problems. Demonstrate competence in recognising patterns of symptoms consistent with diagnostic categories of mental disorder from a patientcentered interview. Demonstrate critical and comprehensive knowledge of risk assessment in relation to common mental health problems. CI 2 Integrate and synthesise diverse knowledge, evidence, opinion, theory and practice to formulate succinct problems and goals. PP 6 Demonstrate competence in accurate risk assessment. CI 1 PP 1 KU 3 CI 2 Integrate and synthesise diverse knowledge, evidence, opinion, theory and practice to formulate succinct problems and goals. PP 2 Demonstrate competence in using ‘common factors’ to engage, gather information and build a therapeutic alliance with people with common mental health problems. Demonstrate competence in managing the emotional content of sessions and grasping the clients perspective or “world view”. ’ PP 3 PP 5
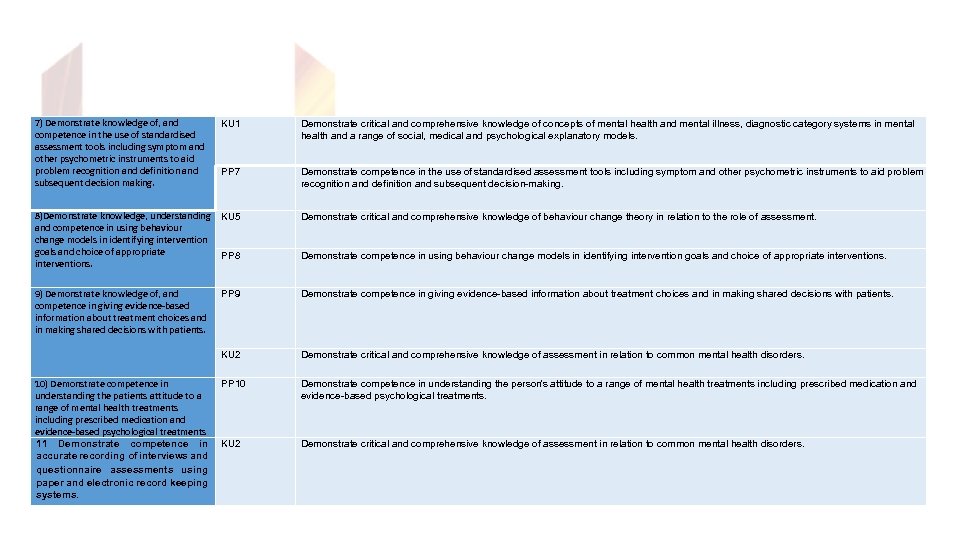 7) Demonstrate knowledge of, and competence in the use of standardised assessment tools including symptom and other psychometric instruments to aid problem recognition and definition and subsequent decision making. KU 1 Demonstrate critical and comprehensive knowledge of concepts of mental health and mental illness, diagnostic category systems in mental health and a range of social, medical and psychological explanatory models. PP 7 Demonstrate competence in the use of standardised assessment tools including symptom and other psychometric instruments to aid problem recognition and definition and subsequent decision-making. 8)Demonstrate knowledge, understanding KU 5 and competence in using behaviour change models in identifying intervention goals and choice of appropriate PP 8 interventions. Demonstrate critical and comprehensive knowledge of behaviour change theory in relation to the role of assessment. 9) Demonstrate knowledge of, and competence in giving evidence-based information about treatment choices and in making shared decisions with patients. PP 9 Demonstrate competence in giving evidence-based information about treatment choices and in making shared decisions with patients. KU 2 Demonstrate critical and comprehensive knowledge of assessment in relation to common mental health disorders. PP 10 Demonstrate competence in understanding the person’s attitude to a range of mental health treatments including prescribed medication and evidence-based psychological treatments. KU 2 Demonstrate critical and comprehensive knowledge of assessment in relation to common mental health disorders. 10) Demonstrate competence in understanding the patients attitude to a range of mental health treatments including prescribed medication and evidence-based psychological treatments 11 Demonstrate competence in accurate recording of interviews and questionnaire assessments using paper and electronic record keeping systems. Demonstrate competence in using behaviour change models in identifying intervention goals and choice of appropriate interventions.
7) Demonstrate knowledge of, and competence in the use of standardised assessment tools including symptom and other psychometric instruments to aid problem recognition and definition and subsequent decision making. KU 1 Demonstrate critical and comprehensive knowledge of concepts of mental health and mental illness, diagnostic category systems in mental health and a range of social, medical and psychological explanatory models. PP 7 Demonstrate competence in the use of standardised assessment tools including symptom and other psychometric instruments to aid problem recognition and definition and subsequent decision-making. 8)Demonstrate knowledge, understanding KU 5 and competence in using behaviour change models in identifying intervention goals and choice of appropriate PP 8 interventions. Demonstrate critical and comprehensive knowledge of behaviour change theory in relation to the role of assessment. 9) Demonstrate knowledge of, and competence in giving evidence-based information about treatment choices and in making shared decisions with patients. PP 9 Demonstrate competence in giving evidence-based information about treatment choices and in making shared decisions with patients. KU 2 Demonstrate critical and comprehensive knowledge of assessment in relation to common mental health disorders. PP 10 Demonstrate competence in understanding the person’s attitude to a range of mental health treatments including prescribed medication and evidence-based psychological treatments. KU 2 Demonstrate critical and comprehensive knowledge of assessment in relation to common mental health disorders. 10) Demonstrate competence in understanding the patients attitude to a range of mental health treatments including prescribed medication and evidence-based psychological treatments 11 Demonstrate competence in accurate recording of interviews and questionnaire assessments using paper and electronic record keeping systems. Demonstrate competence in using behaviour change models in identifying intervention goals and choice of appropriate interventions.
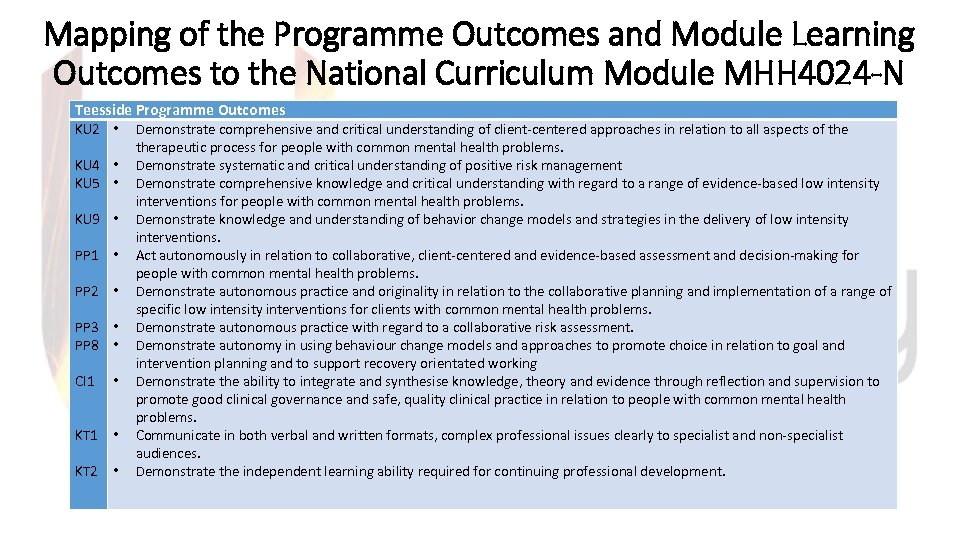 Mapping of the Programme Outcomes and Module Learning Outcomes to the National Curriculum Module MHH 4024 -N Teesside Programme Outcomes KU 2 • Demonstrate comprehensive and critical understanding of client-centered approaches in relation to all aspects of the KU 4 • KU 5 • KU 9 • PP 1 PP 2 PP 3 PP 8 CI 1 • KT 2 • • • therapeutic process for people with common mental health problems. Demonstrate systematic and critical understanding of positive risk management Demonstrate comprehensive knowledge and critical understanding with regard to a range of evidence-based low intensity interventions for people with common mental health problems. Demonstrate knowledge and understanding of behavior change models and strategies in the delivery of low intensity interventions. Act autonomously in relation to collaborative, client-centered and evidence-based assessment and decision-making for people with common mental health problems. Demonstrate autonomous practice and originality in relation to the collaborative planning and implementation of a range of specific low intensity interventions for clients with common mental health problems. Demonstrate autonomous practice with regard to a collaborative risk assessment. Demonstrate autonomy in using behaviour change models and approaches to promote choice in relation to goal and intervention planning and to support recovery orientated working Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. Communicate in both verbal and written formats, complex professional issues clearly to specialist and non-specialist audiences. Demonstrate the independent learning ability required for continuing professional development.
Mapping of the Programme Outcomes and Module Learning Outcomes to the National Curriculum Module MHH 4024 -N Teesside Programme Outcomes KU 2 • Demonstrate comprehensive and critical understanding of client-centered approaches in relation to all aspects of the KU 4 • KU 5 • KU 9 • PP 1 PP 2 PP 3 PP 8 CI 1 • KT 2 • • • therapeutic process for people with common mental health problems. Demonstrate systematic and critical understanding of positive risk management Demonstrate comprehensive knowledge and critical understanding with regard to a range of evidence-based low intensity interventions for people with common mental health problems. Demonstrate knowledge and understanding of behavior change models and strategies in the delivery of low intensity interventions. Act autonomously in relation to collaborative, client-centered and evidence-based assessment and decision-making for people with common mental health problems. Demonstrate autonomous practice and originality in relation to the collaborative planning and implementation of a range of specific low intensity interventions for clients with common mental health problems. Demonstrate autonomous practice with regard to a collaborative risk assessment. Demonstrate autonomy in using behaviour change models and approaches to promote choice in relation to goal and intervention planning and to support recovery orientated working Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. Communicate in both verbal and written formats, complex professional issues clearly to specialist and non-specialist audiences. Demonstrate the independent learning ability required for continuing professional development.
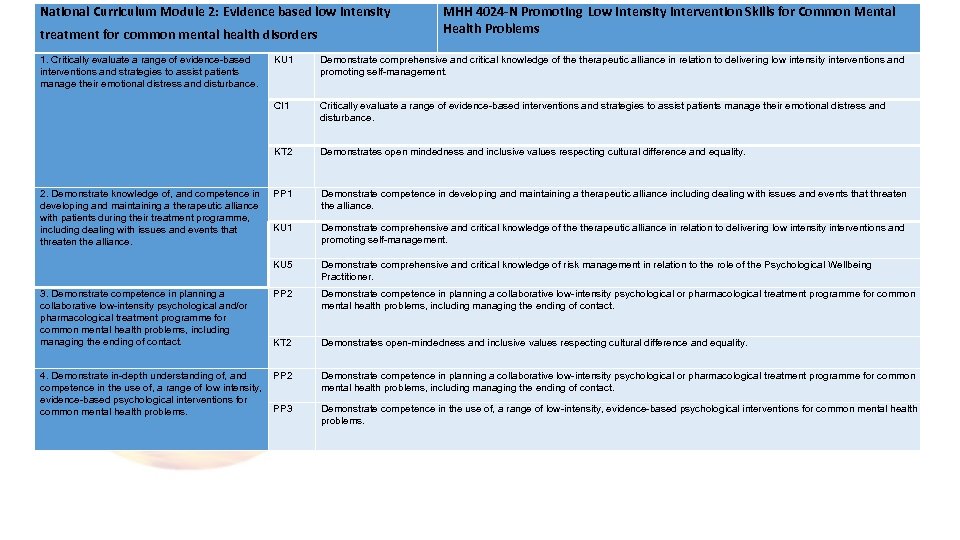 National Curriculum Module 2: Evidence based low intensity treatment for common mental health disorders 1. Critically evaluate a range of evidence-based interventions and strategies to assist patients manage their emotional distress and disturbance. MHH 4024 -N Promoting Low Intensity Intervention Skills for Common Mental Health Problems CI 1 Critically evaluate a range of evidence-based interventions and strategies to assist patients manage their emotional distress and disturbance. Demonstrates open mindedness and inclusive values respecting cultural difference and equality. PP 1 Demonstrate competence in developing and maintaining a therapeutic alliance including dealing with issues and events that threaten the alliance. KU 1 Demonstrate comprehensive and critical knowledge of therapeutic alliance in relation to delivering low intensity interventions and promoting self-management. KU 5 3. Demonstrate competence in planning a collaborative low-intensity psychological and/or pharmacological treatment programme for common mental health problems, including managing the ending of contact. Demonstrate comprehensive and critical knowledge of therapeutic alliance in relation to delivering low intensity interventions and promoting self-management. KT 2 2. Demonstrate knowledge of, and competence in developing and maintaining a therapeutic alliance with patients during their treatment programme, including dealing with issues and events that threaten the alliance. KU 1 Demonstrate comprehensive and critical knowledge of risk management in relation to the role of the Psychological Wellbeing Practitioner. PP 2 Demonstrate competence in planning a collaborative low-intensity psychological or pharmacological treatment programme for common mental health problems, including managing the ending of contact. KT 2 Demonstrates open-mindedness and inclusive values respecting cultural difference and equality. 4. Demonstrate in-depth understanding of, and PP 2 competence in the use of, a range of low intensity, evidence-based psychological interventions for PP 3 common mental health problems. Demonstrate competence in planning a collaborative low-intensity psychological or pharmacological treatment programme for common mental health problems, including managing the ending of contact. Demonstrate competence in the use of, a range of low-intensity, evidence-based psychological interventions for common mental health problems.
National Curriculum Module 2: Evidence based low intensity treatment for common mental health disorders 1. Critically evaluate a range of evidence-based interventions and strategies to assist patients manage their emotional distress and disturbance. MHH 4024 -N Promoting Low Intensity Intervention Skills for Common Mental Health Problems CI 1 Critically evaluate a range of evidence-based interventions and strategies to assist patients manage their emotional distress and disturbance. Demonstrates open mindedness and inclusive values respecting cultural difference and equality. PP 1 Demonstrate competence in developing and maintaining a therapeutic alliance including dealing with issues and events that threaten the alliance. KU 1 Demonstrate comprehensive and critical knowledge of therapeutic alliance in relation to delivering low intensity interventions and promoting self-management. KU 5 3. Demonstrate competence in planning a collaborative low-intensity psychological and/or pharmacological treatment programme for common mental health problems, including managing the ending of contact. Demonstrate comprehensive and critical knowledge of therapeutic alliance in relation to delivering low intensity interventions and promoting self-management. KT 2 2. Demonstrate knowledge of, and competence in developing and maintaining a therapeutic alliance with patients during their treatment programme, including dealing with issues and events that threaten the alliance. KU 1 Demonstrate comprehensive and critical knowledge of risk management in relation to the role of the Psychological Wellbeing Practitioner. PP 2 Demonstrate competence in planning a collaborative low-intensity psychological or pharmacological treatment programme for common mental health problems, including managing the ending of contact. KT 2 Demonstrates open-mindedness and inclusive values respecting cultural difference and equality. 4. Demonstrate in-depth understanding of, and PP 2 competence in the use of, a range of low intensity, evidence-based psychological interventions for PP 3 common mental health problems. Demonstrate competence in planning a collaborative low-intensity psychological or pharmacological treatment programme for common mental health problems, including managing the ending of contact. Demonstrate competence in the use of, a range of low-intensity, evidence-based psychological interventions for common mental health problems.
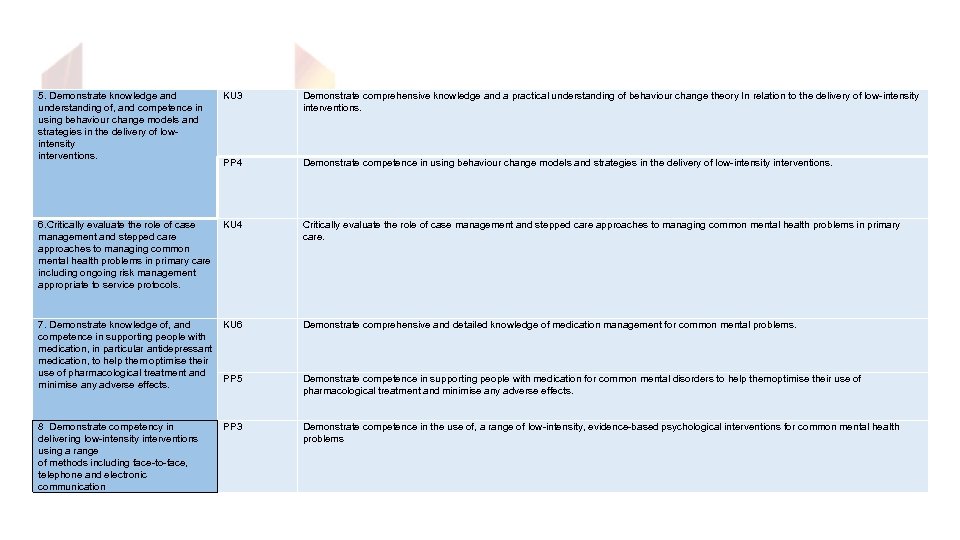 5. Demonstrate knowledge and understanding of, and competence in using behaviour change models and strategies in the delivery of lowintensity interventions. KU 3 Demonstrate comprehensive knowledge and a practical understanding of behaviour change theory In relation to the delivery of low-intensity interventions. PP 4 Demonstrate competence in using behaviour change models and strategies in the delivery of low-intensity interventions. 6. Critically evaluate the role of case KU 4 management and stepped care approaches to managing common mental health problems in primary care including ongoing risk management appropriate to service protocols. Critically evaluate the role of case management and stepped care approaches to managing common mental health problems in primary care. 7. Demonstrate knowledge of, and KU 6 competence in supporting people with medication, in particular antidepressant medication, to help them optimise their use of pharmacological treatment and PP 5 minimise any adverse effects. 8 Demonstrate competency in PP 3 delivering low-intensity interventions using a range of methods including face-to-face, telephone and electronic communication Demonstrate comprehensive and detailed knowledge of medication management for common mental problems. Demonstrate competence in supporting people with medication for common mental disorders to help them ptimise their use of o pharmacological treatment and minimise any adverse effects. Demonstrate competence in the use of, a range of low-intensity, evidence-based psychological interventions for common mental health problems
5. Demonstrate knowledge and understanding of, and competence in using behaviour change models and strategies in the delivery of lowintensity interventions. KU 3 Demonstrate comprehensive knowledge and a practical understanding of behaviour change theory In relation to the delivery of low-intensity interventions. PP 4 Demonstrate competence in using behaviour change models and strategies in the delivery of low-intensity interventions. 6. Critically evaluate the role of case KU 4 management and stepped care approaches to managing common mental health problems in primary care including ongoing risk management appropriate to service protocols. Critically evaluate the role of case management and stepped care approaches to managing common mental health problems in primary care. 7. Demonstrate knowledge of, and KU 6 competence in supporting people with medication, in particular antidepressant medication, to help them optimise their use of pharmacological treatment and PP 5 minimise any adverse effects. 8 Demonstrate competency in PP 3 delivering low-intensity interventions using a range of methods including face-to-face, telephone and electronic communication Demonstrate comprehensive and detailed knowledge of medication management for common mental problems. Demonstrate competence in supporting people with medication for common mental disorders to help them ptimise their use of o pharmacological treatment and minimise any adverse effects. Demonstrate competence in the use of, a range of low-intensity, evidence-based psychological interventions for common mental health problems
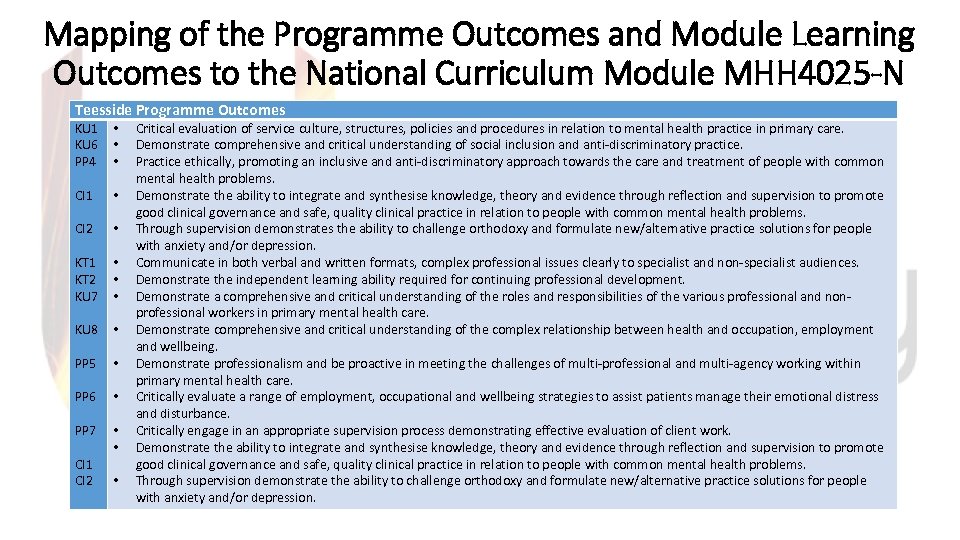 Mapping of the Programme Outcomes and Module Learning Outcomes to the National Curriculum Module MHH 4025 -N Teesside Programme Outcomes KU 1 KU 6 PP 4 CI 1 CI 2 KT 1 KT 2 KU 7 KU 8 PP 5 PP 6 PP 7 CI 1 CI 2 • • • • Critical evaluation of service culture, structures, policies and procedures in relation to mental health practice in primary care. Demonstrate comprehensive and critical understanding of social inclusion and anti-discriminatory practice. Practice ethically, promoting an inclusive and anti-discriminatory approach towards the care and treatment of people with common mental health problems. Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. Through supervision demonstrates the ability to challenge orthodoxy and formulate new/alternative practice solutions for people with anxiety and/or depression. Communicate in both verbal and written formats, complex professional issues clearly to specialist and non-specialist audiences. Demonstrate the independent learning ability required for continuing professional development. Demonstrate a comprehensive and critical understanding of the roles and responsibilities of the various professional and nonprofessional workers in primary mental health care. Demonstrate comprehensive and critical understanding of the complex relationship between health and occupation, employment and wellbeing. Demonstrate professionalism and be proactive in meeting the challenges of multi-professional and multi-agency working within primary mental health care. Critically evaluate a range of employment, occupational and wellbeing strategies to assist patients manage their emotional distress and disturbance. Critically engage in an appropriate supervision process demonstrating effective evaluation of client work. Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. Through supervision demonstrate the ability to challenge orthodoxy and formulate new/alternative practice solutions for people with anxiety and/or depression.
Mapping of the Programme Outcomes and Module Learning Outcomes to the National Curriculum Module MHH 4025 -N Teesside Programme Outcomes KU 1 KU 6 PP 4 CI 1 CI 2 KT 1 KT 2 KU 7 KU 8 PP 5 PP 6 PP 7 CI 1 CI 2 • • • • Critical evaluation of service culture, structures, policies and procedures in relation to mental health practice in primary care. Demonstrate comprehensive and critical understanding of social inclusion and anti-discriminatory practice. Practice ethically, promoting an inclusive and anti-discriminatory approach towards the care and treatment of people with common mental health problems. Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. Through supervision demonstrates the ability to challenge orthodoxy and formulate new/alternative practice solutions for people with anxiety and/or depression. Communicate in both verbal and written formats, complex professional issues clearly to specialist and non-specialist audiences. Demonstrate the independent learning ability required for continuing professional development. Demonstrate a comprehensive and critical understanding of the roles and responsibilities of the various professional and nonprofessional workers in primary mental health care. Demonstrate comprehensive and critical understanding of the complex relationship between health and occupation, employment and wellbeing. Demonstrate professionalism and be proactive in meeting the challenges of multi-professional and multi-agency working within primary mental health care. Critically evaluate a range of employment, occupational and wellbeing strategies to assist patients manage their emotional distress and disturbance. Critically engage in an appropriate supervision process demonstrating effective evaluation of client work. Demonstrate the ability to integrate and synthesise knowledge, theory and evidence through reflection and supervision to promote good clinical governance and safe, quality clinical practice in relation to people with common mental health problems. Through supervision demonstrate the ability to challenge orthodoxy and formulate new/alternative practice solutions for people with anxiety and/or depression.
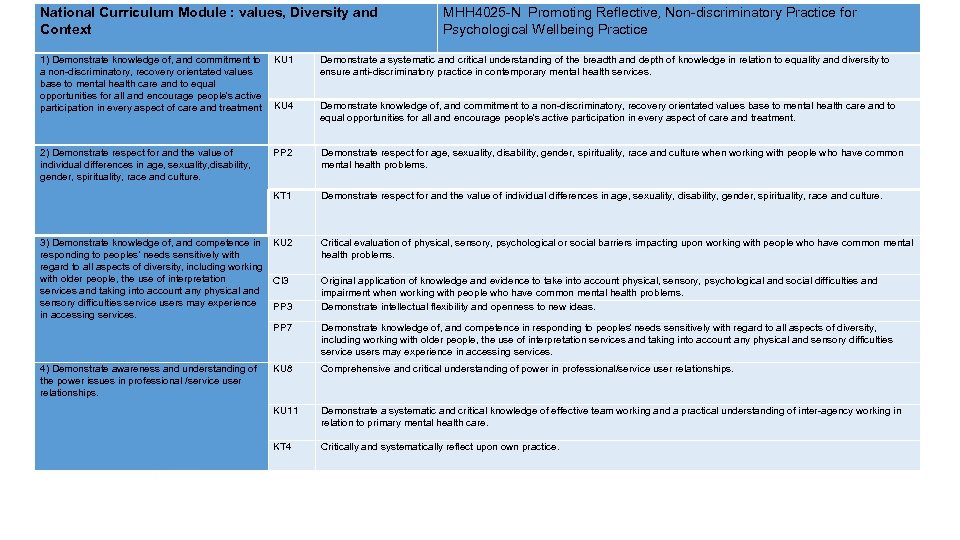 National Curriculum Module : values, Diversity and Context MHH 4025 -N Promoting Reflective, Non-discriminatory Practice for Psychological Wellbeing Practice 1) Demonstrate knowledge of, and commitment to KU 1 a non-discriminatory, recovery orientated values base to mental health care and to equal opportunities for all and encourage people’s active participation in every aspect of care and treatment KU 4 Demonstrate a systematic and critical understanding of the breadth and depth of knowledge in relation to equality and diversity to ensure anti-discriminatory practice in contemporary mental health services. 2) Demonstrate respect for and the value of individual differences in age, sexuality, disability, gender, spirituality, race and culture. PP 2 Demonstrate respect for age, sexuality, disability, gender, spirituality, race and culture when working with people who have common mental health problems. KT 1 Demonstrate respect for and the value of individual differences in age, sexuality, disability, gender, spirituality, race and culture. 3) Demonstrate knowledge of, and competence in responding to peoples’ needs sensitively with regard to all aspects of diversity, including working with older people, the use of interpretation services and taking into account any physical and sensory difficulties service users may experience in accessing services. KU 2 Critical evaluation of physical, sensory, psychological or social barriers impacting upon working with people who have common mental health problems. CI 3 PP 3 Original application of knowledge and evidence to take into account physical, sensory, psychological and social difficulties and impairment when working with people who have common mental health problems. Demonstrate intellectual flexibility and openness to new ideas. PP 7 Demonstrate knowledge of, and competence in responding to peoples ’ needs sensitively with regard to all aspects of diversity, including working with older people, the use of interpretation services and taking into account any physical and sensory difficulties service users may experience in accessing services. 4) Demonstrate awareness and understanding of the power issues in professional /service user relationships. KU 8 Comprehensive and critical understanding of power in professional/service user relationships. KU 11 KT 4 Demonstrate a systematic and critical knowledge of effective team working and a practical understanding of inter-agency working in relation to primary mental health care. Demonstrate knowledge of, and commitment to a non-discriminatory, recovery orientated values base to mental health care and to equal opportunities for all and encourage people’s active participation in every aspect of care and treatment. Critically and systematically reflect upon own practice.
National Curriculum Module : values, Diversity and Context MHH 4025 -N Promoting Reflective, Non-discriminatory Practice for Psychological Wellbeing Practice 1) Demonstrate knowledge of, and commitment to KU 1 a non-discriminatory, recovery orientated values base to mental health care and to equal opportunities for all and encourage people’s active participation in every aspect of care and treatment KU 4 Demonstrate a systematic and critical understanding of the breadth and depth of knowledge in relation to equality and diversity to ensure anti-discriminatory practice in contemporary mental health services. 2) Demonstrate respect for and the value of individual differences in age, sexuality, disability, gender, spirituality, race and culture. PP 2 Demonstrate respect for age, sexuality, disability, gender, spirituality, race and culture when working with people who have common mental health problems. KT 1 Demonstrate respect for and the value of individual differences in age, sexuality, disability, gender, spirituality, race and culture. 3) Demonstrate knowledge of, and competence in responding to peoples’ needs sensitively with regard to all aspects of diversity, including working with older people, the use of interpretation services and taking into account any physical and sensory difficulties service users may experience in accessing services. KU 2 Critical evaluation of physical, sensory, psychological or social barriers impacting upon working with people who have common mental health problems. CI 3 PP 3 Original application of knowledge and evidence to take into account physical, sensory, psychological and social difficulties and impairment when working with people who have common mental health problems. Demonstrate intellectual flexibility and openness to new ideas. PP 7 Demonstrate knowledge of, and competence in responding to peoples ’ needs sensitively with regard to all aspects of diversity, including working with older people, the use of interpretation services and taking into account any physical and sensory difficulties service users may experience in accessing services. 4) Demonstrate awareness and understanding of the power issues in professional /service user relationships. KU 8 Comprehensive and critical understanding of power in professional/service user relationships. KU 11 KT 4 Demonstrate a systematic and critical knowledge of effective team working and a practical understanding of inter-agency working in relation to primary mental health care. Demonstrate knowledge of, and commitment to a non-discriminatory, recovery orientated values base to mental health care and to equal opportunities for all and encourage people’s active participation in every aspect of care and treatment. Critically and systematically reflect upon own practice.
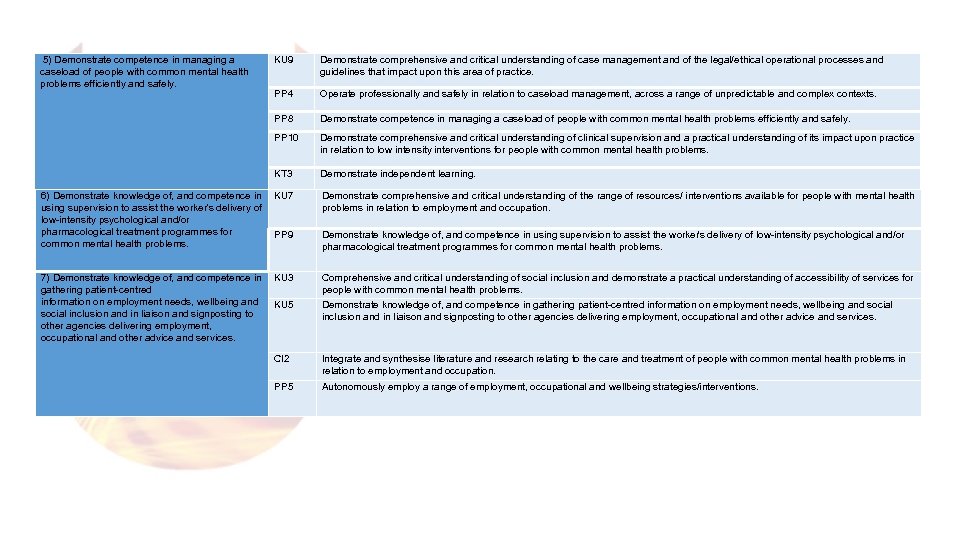 5) Demonstrate competence in managing a caseload of people with common mental health problems efficiently and safely. KU 9 Demonstrate comprehensive and critical understanding of case management and of the legal/ethical operational processes and guidelines that impact upon this area of practice. PP 4 PP 8 Operate professionally and safely in relation to caseload management, across a range of unpredictable and complex contexts. PP 10 Demonstrate comprehensive and critical understanding of clinical supervision and a practical understanding of its impact upon practice in relation to low intensity interventions for people with common mental health problems. KT 3 Demonstrate independent learning. Demonstrate competence in managing a caseload of people with common mental health problems efficiently and safely. 6) Demonstrate knowledge of, and competence in KU 7 using supervision to assist the worker’s delivery of low-intensity psychological and/or pharmacological treatment programmes for PP 9 common mental health problems. Demonstrate comprehensive and critical understanding of the range of resources/ interventions available for people with mental health problems in relation to employment and occupation. 7) Demonstrate knowledge of, and competence in gathering patient-centred information on employment needs, wellbeing and social inclusion and in liaison and signposting to other agencies delivering employment, occupational and other advice and services. KU 3 Comprehensive and critical understanding of social inclusion and demonstrate a practical understanding of accessibility of services for people with common mental health problems. KU 5 Demonstrate knowledge of, and competence in gathering patient-centred information on employment needs, wellbeing and social inclusion and in liaison and signposting to other agencies delivering employment, occupational and other advice and services. CI 2 Integrate and synthesise literature and research relating to the care and treatment of people with common mental health problems in relation to employment and occupation. PP 5 Autonomously employ a range of employment, occupational and wellbeing strategies/interventions. Demonstrate knowledge of, and competence in using supervision to assist the worker ’s delivery of low-intensity psychological and/or pharmacological treatment programmes for common mental health problems.
5) Demonstrate competence in managing a caseload of people with common mental health problems efficiently and safely. KU 9 Demonstrate comprehensive and critical understanding of case management and of the legal/ethical operational processes and guidelines that impact upon this area of practice. PP 4 PP 8 Operate professionally and safely in relation to caseload management, across a range of unpredictable and complex contexts. PP 10 Demonstrate comprehensive and critical understanding of clinical supervision and a practical understanding of its impact upon practice in relation to low intensity interventions for people with common mental health problems. KT 3 Demonstrate independent learning. Demonstrate competence in managing a caseload of people with common mental health problems efficiently and safely. 6) Demonstrate knowledge of, and competence in KU 7 using supervision to assist the worker’s delivery of low-intensity psychological and/or pharmacological treatment programmes for PP 9 common mental health problems. Demonstrate comprehensive and critical understanding of the range of resources/ interventions available for people with mental health problems in relation to employment and occupation. 7) Demonstrate knowledge of, and competence in gathering patient-centred information on employment needs, wellbeing and social inclusion and in liaison and signposting to other agencies delivering employment, occupational and other advice and services. KU 3 Comprehensive and critical understanding of social inclusion and demonstrate a practical understanding of accessibility of services for people with common mental health problems. KU 5 Demonstrate knowledge of, and competence in gathering patient-centred information on employment needs, wellbeing and social inclusion and in liaison and signposting to other agencies delivering employment, occupational and other advice and services. CI 2 Integrate and synthesise literature and research relating to the care and treatment of people with common mental health problems in relation to employment and occupation. PP 5 Autonomously employ a range of employment, occupational and wellbeing strategies/interventions. Demonstrate knowledge of, and competence in using supervision to assist the worker ’s delivery of low-intensity psychological and/or pharmacological treatment programmes for common mental health problems.
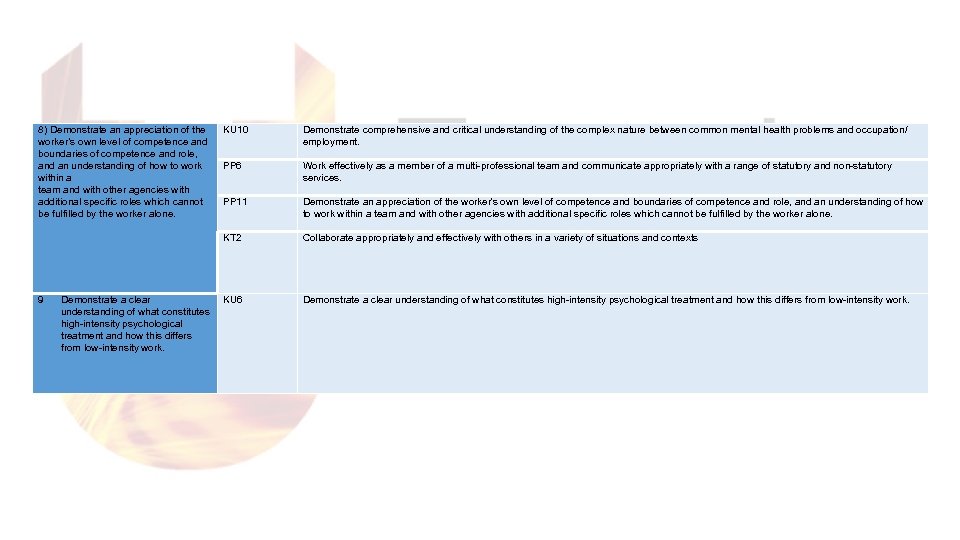 8) Demonstrate an appreciation of the worker’s own level of competence and boundaries of competence and role, and an understanding of how to work within a team and with other agencies with additional specific roles which cannot be fulfilled by the worker alone. Demonstrate a clear understanding of what constitutes high-intensity psychological treatment and how this differs from low-intensity work. Demonstrate comprehensive and critical understanding of the complex nature between common mental health problems and occupation/ employment. PP 11 Demonstrate an appreciation of the worker’s own level of competence and boundaries of competence and role, and an understanding of how to work within a team and with other agencies with additional specific roles which cannot be fulfilled by the worker alone. KT 2 9 KU 10 PP 6 Collaborate appropriately and effectively with others in a variety of situations and contexts KU 6 Demonstrate a clear understanding of what constitutes high-intensity psychological treatment and how this differs from low-intensity work. Work effectively as a member of a multi-professional team and communicate appropriately with a range of statutory and non-statutory services.
8) Demonstrate an appreciation of the worker’s own level of competence and boundaries of competence and role, and an understanding of how to work within a team and with other agencies with additional specific roles which cannot be fulfilled by the worker alone. Demonstrate a clear understanding of what constitutes high-intensity psychological treatment and how this differs from low-intensity work. Demonstrate comprehensive and critical understanding of the complex nature between common mental health problems and occupation/ employment. PP 11 Demonstrate an appreciation of the worker’s own level of competence and boundaries of competence and role, and an understanding of how to work within a team and with other agencies with additional specific roles which cannot be fulfilled by the worker alone. KT 2 9 KU 10 PP 6 Collaborate appropriately and effectively with others in a variety of situations and contexts KU 6 Demonstrate a clear understanding of what constitutes high-intensity psychological treatment and how this differs from low-intensity work. Work effectively as a member of a multi-professional team and communicate appropriately with a range of statutory and non-statutory services.
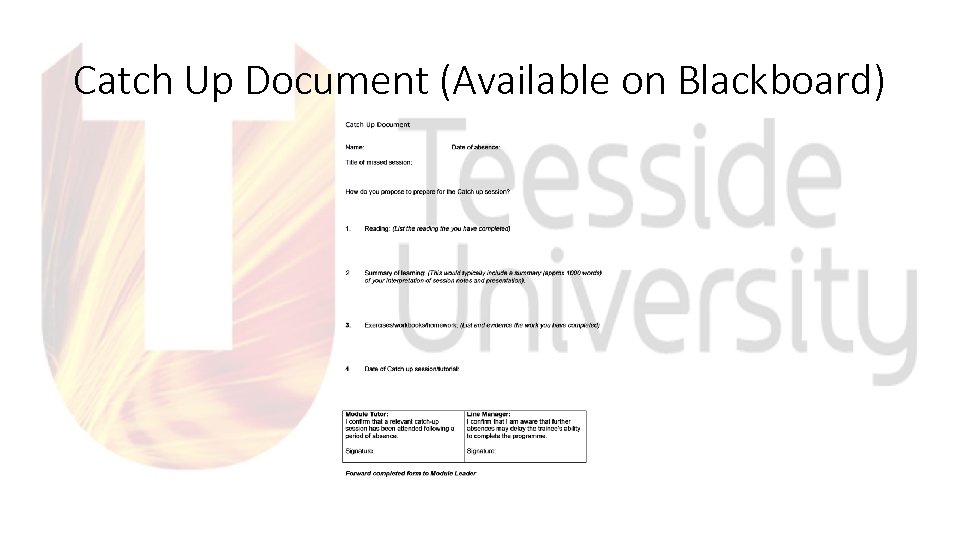 Catch Up Document (Available on Blackboard)
Catch Up Document (Available on Blackboard)
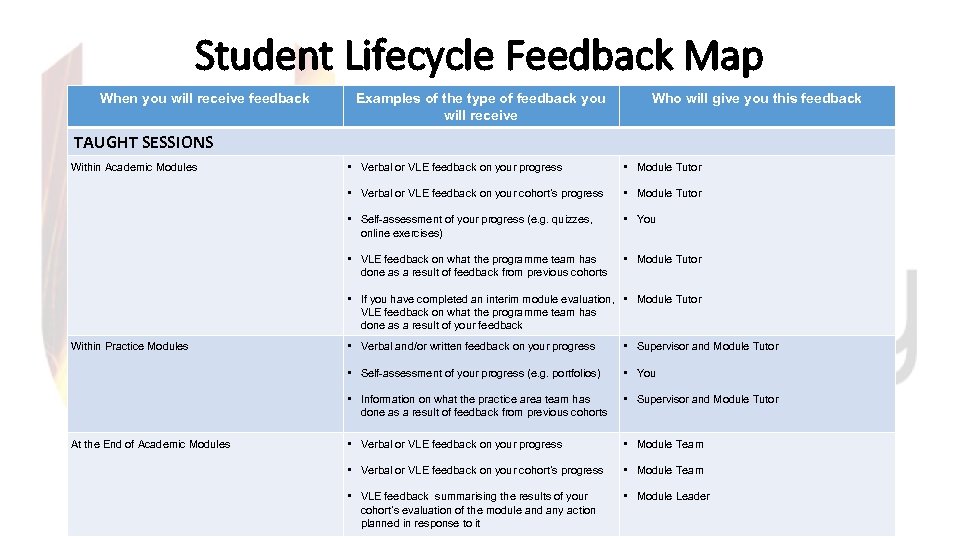 Student Lifecycle Feedback Map When you will receive feedback Examples of the type of feedback you will receive Who will give you this feedback TAUGHT SESSIONS • Verbal or VLE feedback on your progress • Module Tutor • Verbal or VLE feedback on your cohort’s progress • Module Tutor • Self-assessment of your progress (e. g. quizzes, online exercises) • You • VLE feedback on what the programme team has done as a result of feedback from previous cohorts Within Academic Modules • Module Tutor • If you have completed an interim module evaluation, • Module Tutor VLE feedback on what the programme team has done as a result of your feedback • Supervisor and Module Tutor • You • Information on what the practice area team has done as a result of feedback from previous cohorts At the End of Academic Modules • Verbal and/or written feedback on your progress • Self-assessment of your progress (e. g. portfolios) Within Practice Modules • Supervisor and Module Tutor • Verbal or VLE feedback on your progress • Module Team • Verbal or VLE feedback on your cohort’s progress • Module Team • VLE feedback summarising the results of your cohort’s evaluation of the module and any action planned in response to it • Module Leader
Student Lifecycle Feedback Map When you will receive feedback Examples of the type of feedback you will receive Who will give you this feedback TAUGHT SESSIONS • Verbal or VLE feedback on your progress • Module Tutor • Verbal or VLE feedback on your cohort’s progress • Module Tutor • Self-assessment of your progress (e. g. quizzes, online exercises) • You • VLE feedback on what the programme team has done as a result of feedback from previous cohorts Within Academic Modules • Module Tutor • If you have completed an interim module evaluation, • Module Tutor VLE feedback on what the programme team has done as a result of your feedback • Supervisor and Module Tutor • You • Information on what the practice area team has done as a result of feedback from previous cohorts At the End of Academic Modules • Verbal and/or written feedback on your progress • Self-assessment of your progress (e. g. portfolios) Within Practice Modules • Supervisor and Module Tutor • Verbal or VLE feedback on your progress • Module Team • Verbal or VLE feedback on your cohort’s progress • Module Team • VLE feedback summarising the results of your cohort’s evaluation of the module and any action planned in response to it • Module Leader
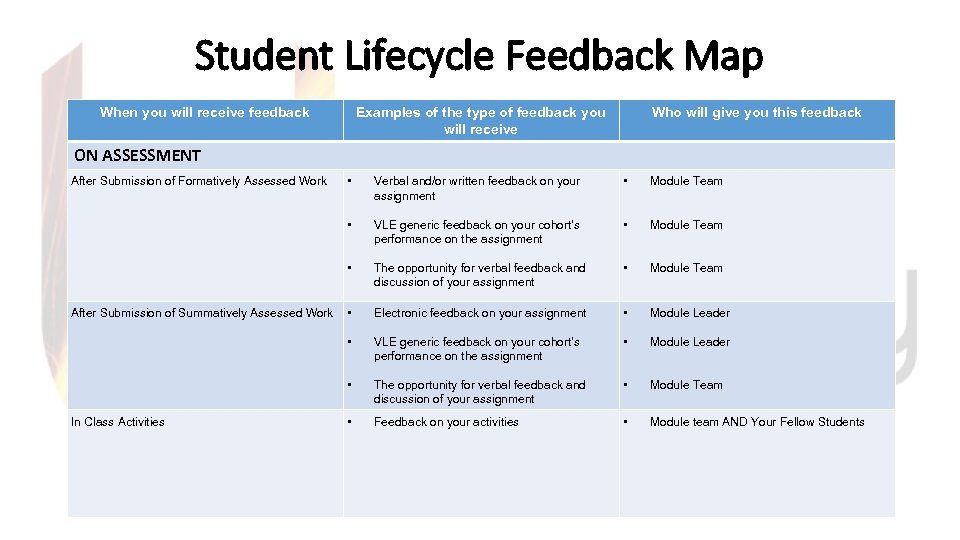 Student Lifecycle Feedback Map When you will receive feedback Examples of the type of feedback you will receive Who will give you this feedback ON ASSESSMENT • Module Team VLE generic feedback on your cohort’s performance on the assignment • Module Team The opportunity for verbal feedback and discussion of your assignment • Module Team • Electronic feedback on your assignment • Module Leader • VLE generic feedback on your cohort’s performance on the assignment • Module Leader • In Class Activities Verbal and/or written feedback on your assignment • After Submission of Summatively Assessed Work • • After Submission of Formatively Assessed Work The opportunity for verbal feedback and discussion of your assignment • Module Team • Feedback on your activities • Module team AND Your Fellow Students
Student Lifecycle Feedback Map When you will receive feedback Examples of the type of feedback you will receive Who will give you this feedback ON ASSESSMENT • Module Team VLE generic feedback on your cohort’s performance on the assignment • Module Team The opportunity for verbal feedback and discussion of your assignment • Module Team • Electronic feedback on your assignment • Module Leader • VLE generic feedback on your cohort’s performance on the assignment • Module Leader • In Class Activities Verbal and/or written feedback on your assignment • After Submission of Summatively Assessed Work • • After Submission of Formatively Assessed Work The opportunity for verbal feedback and discussion of your assignment • Module Team • Feedback on your activities • Module team AND Your Fellow Students
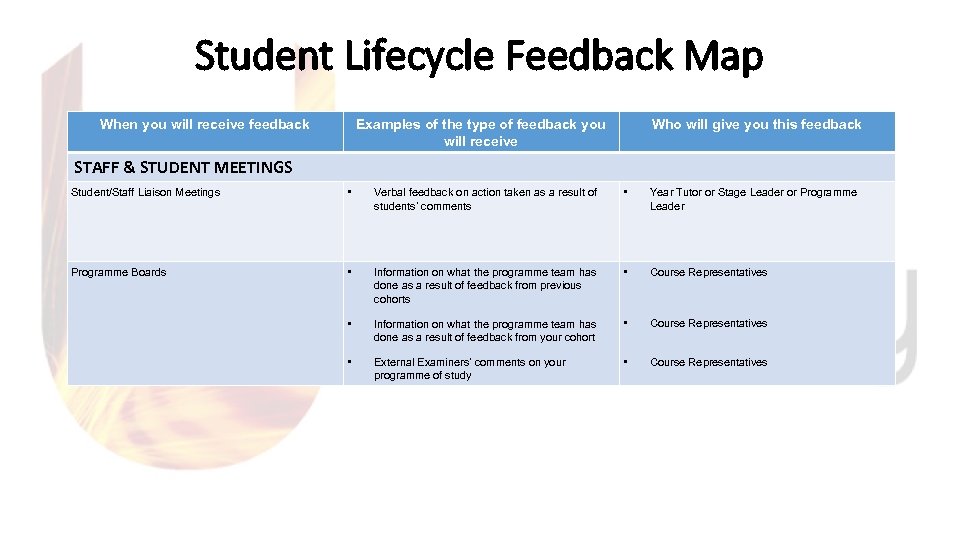 Student Lifecycle Feedback Map When you will receive feedback Examples of the type of feedback you will receive Who will give you this feedback STAFF & STUDENT MEETINGS Student/Staff Liaison Meetings • Verbal feedback on action taken as a result of students’ comments • Year Tutor or Stage Leader or Programme Leader Programme Boards • Information on what the programme team has done as a result of feedback from previous cohorts • Course Representatives • Information on what the programme team has done as a result of feedback from your cohort Course Representatives • External Examiners’ comments on your programme of study • • Course Representatives
Student Lifecycle Feedback Map When you will receive feedback Examples of the type of feedback you will receive Who will give you this feedback STAFF & STUDENT MEETINGS Student/Staff Liaison Meetings • Verbal feedback on action taken as a result of students’ comments • Year Tutor or Stage Leader or Programme Leader Programme Boards • Information on what the programme team has done as a result of feedback from previous cohorts • Course Representatives • Information on what the programme team has done as a result of feedback from your cohort Course Representatives • External Examiners’ comments on your programme of study • • Course Representatives
 References • Department of Health (2015) Improving Access to Psychological Therapies Implementation Plan: Curriculum for Low Intensity Therapy Workers. London: HMSO. • Department of Health (2015) Psychological Wellbeing Practitioner Best Practice Guide. London: HMSO • Richards, D and Whyte, M. (2011) Reach Out Student Materials. 2 nd ed. RETHINK. • Richards, D. A. , Chellingsworth, M. , Hope, R. , Turpin, G. and Whyte, M. (2010). Reach Out National Programme Supervisor Materials to Support the Delivery of Training for Psychological Wellbeing Practitioners Delivering Low Intensity Interventions http: //www. iapt. nhs. uk/workforce/low-intensity/
References • Department of Health (2015) Improving Access to Psychological Therapies Implementation Plan: Curriculum for Low Intensity Therapy Workers. London: HMSO. • Department of Health (2015) Psychological Wellbeing Practitioner Best Practice Guide. London: HMSO • Richards, D and Whyte, M. (2011) Reach Out Student Materials. 2 nd ed. RETHINK. • Richards, D. A. , Chellingsworth, M. , Hope, R. , Turpin, G. and Whyte, M. (2010). Reach Out National Programme Supervisor Materials to Support the Delivery of Training for Psychological Wellbeing Practitioners Delivering Low Intensity Interventions http: //www. iapt. nhs. uk/workforce/low-intensity/


