40840f26c18ac5a20206e21099d6a1c0.ppt
- Количество слайдов: 57
TUMOURS OF THE CENTRAL NERVOUS SYSTEM FM Brett MD. , FRCPath
At the end of this lecture you should be able to: 1. Give basic classification of CNS tumours 2. Understand how patients present 3. Know the common tumours in children and adults 4. Know what is meant by paraneoplastic syndromes 5. Know that concept of benign and malignant meaningless when applied to CNS tumours
CLASSIFICATION OF CNS TUMOURS 1. Intrinsic tumours – account for virtually all tumours in children and 60% of primary CNS tumours in adults 2. Extrinsic tumours – arising from cranial and spinal nerves and dura. 3. Tumours arising from adjacent structures i. e pituitary gland metastatic tumours.
The pathologist and CNS neoplasms Clinical details of importance ~ ~ Age Sex F/X Site of neoplasm
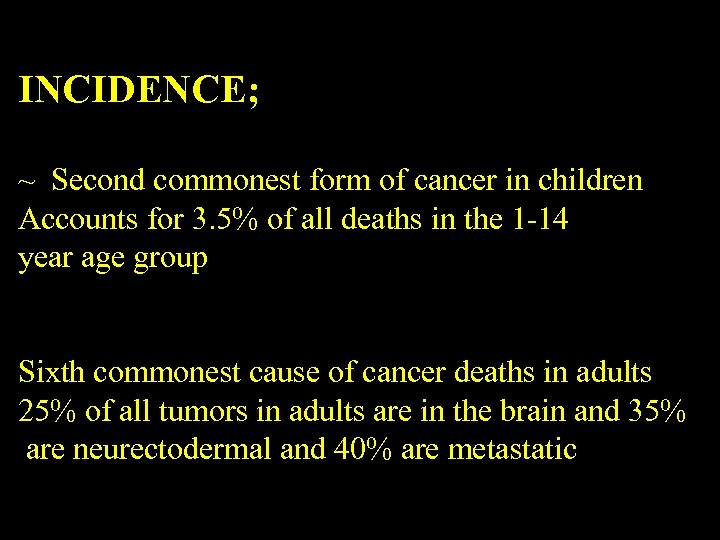
INCIDENCE; ~ Second commonest form of cancer in children Accounts for 3. 5% of all deaths in the 1 -14 year age group Sixth commonest cause of cancer deaths in adults 25% of all tumors in adults are in the brain and 35% are neurectodermal and 40% are metastatic
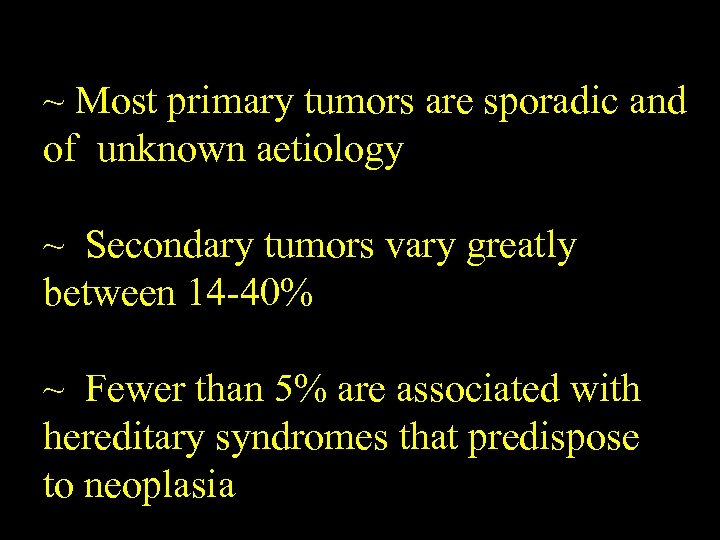
~ Most primary tumors are sporadic and of unknown aetiology ~ Secondary tumors vary greatly between 14 -40% ~ Fewer than 5% are associated with hereditary syndromes that predispose to neoplasia
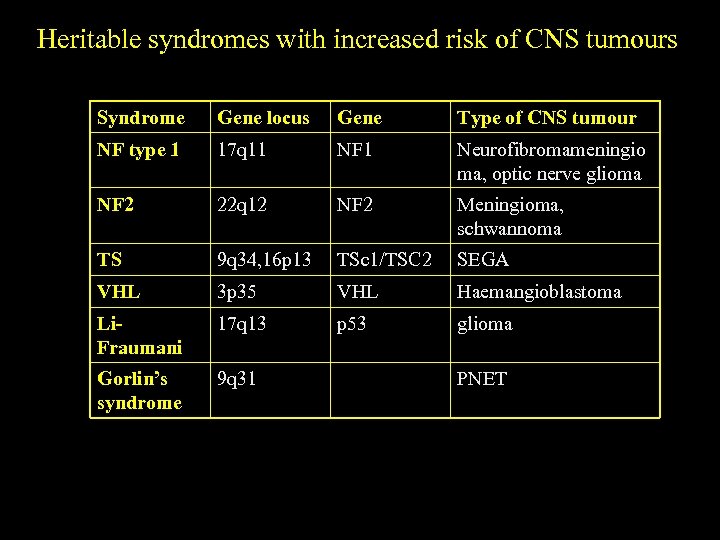
Heritable syndromes with increased risk of CNS tumours Syndrome Gene locus Gene Type of CNS tumour NF type 1 17 q 11 NF 1 Neurofibromameningio ma, optic nerve glioma NF 2 22 q 12 NF 2 Meningioma, schwannoma TS 9 q 34, 16 p 13 TSc 1/TSC 2 SEGA VHL 3 p 35 VHL Haemangioblastoma Li. Fraumani 17 q 13 p 53 glioma Gorlin’s syndrome 9 q 31 PNET
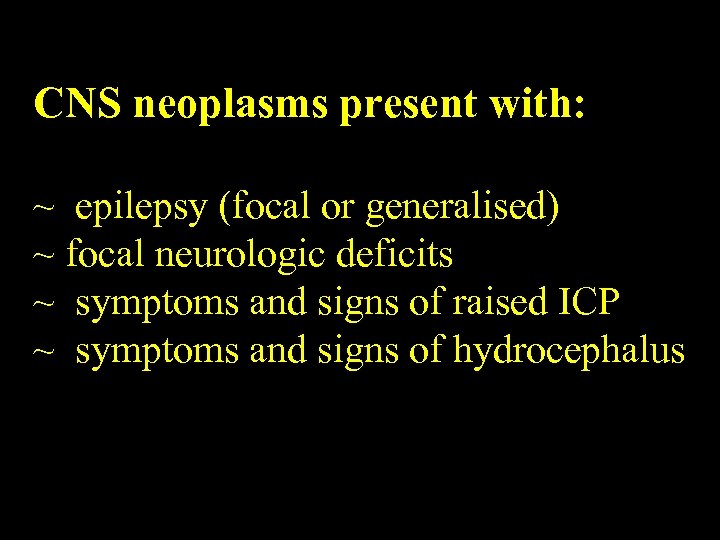
CNS neoplasms present with: ~ epilepsy (focal or generalised) ~ focal neurologic deficits ~ symptoms and signs of raised ICP ~ symptoms and signs of hydrocephalus
Sites of cerebral tumors SSites of cerebral tumors ADULTS Supratentorial tumors account for 90% Therefore increased incidence of epilepsy and decreased incidence of headache Posterior fossa tumours cause headache and vomiting as early features
CHILDREN Cerebellum Pons Optic nerve/chiasm SUPRATENTORIAL TUMORS ARE RARE Therefore Headache, vomiting, visual disturbances common Epilepsy - unusual
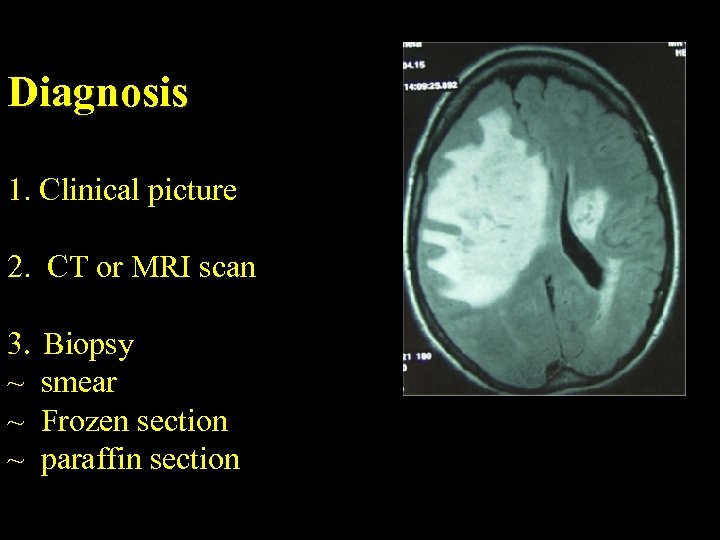
Diagnosis 1. Clinical picture 2. CT or MRI scan 3. Biopsy ~ smear ~ Frozen section ~ paraffin section
Factors in the aetiology of CNS neoplasms 1. Sex – gliomas commoner in males meningiomas commoner in females 2. Exposure to ionizing radiation implicated in the genesis of ~ meningiomas ~ gliomas ~ nerve sheath tumors 3. Primary CNS lymphoma – is associated with immunodeficiency 4. Nitroso compounds cause CNS neoplasms in animals 5. No convincing evidence has linked CNS neoplasms with trauma, occupation, diet, electromagnetic fields
Prognostic factors in CNS tumors ~ Patient characteristics ~ Tumour characteristics
Patient characteristics ~ Age ~ General physical characteristics ~ Extent of surgical resection
Tumour characteristics ~ Specimen procurement ~ Phenotypic analysis ~ Proliferative capacity
EFFECTS OF TUMOUR 1. 2. 3. 4. Local destruction of neural tissue Oedema Distortion of neural tissue Raised ICP
Grading of Gliomas (WHO) Grade 1 – 1 V – based on presence of pleomorphism, mitoses, vascular proliferation and necrosis Median Overall Survival AA – 3 -5 years OS GBM – 1 year Secondary GBM – younger patients with pre-existing lower grade glioma Primary – 60 -70
Primary GBM – high frequency of RGFR amplification -p 16 loss -Secondary GBM – TP 53 mutations
Oligodendroglioma ~ Concurrent deletion of 1 p and 19 q In AO – good response to DXT and chemo ~ Criteria for anaplasia – nuclear pleomorphism, mitotic activity, endothelial vascular hyperplasia and necrosis ~ For anaplasia 2 features – one of which frequent mitoses or VEH
Predictive Markers in Malignant Gliomas ~ 1 p 19 q loss in AO associated with enhanced chemosensitivity and longer overall survival ~ MGMT status in GBM inc responsivness to temezolamide ~ EGFR – inc in GBM
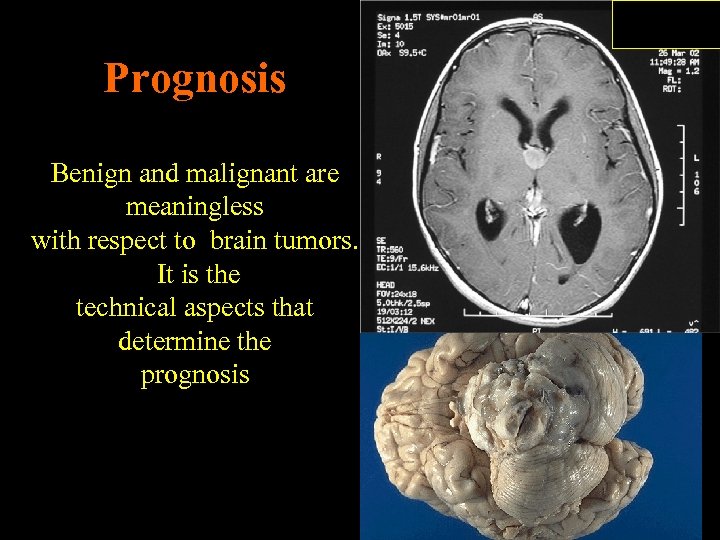
Prognosis Benign and malignant are meaningless with respect to brain tumors. It is the technical aspects that determine the prognosis
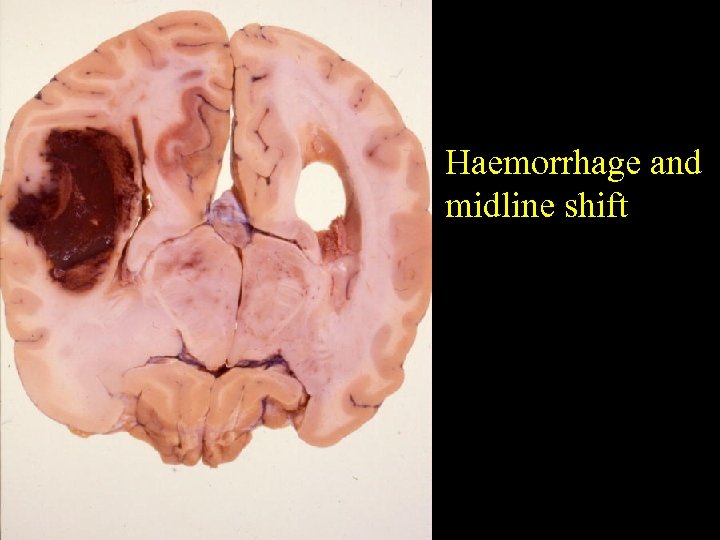
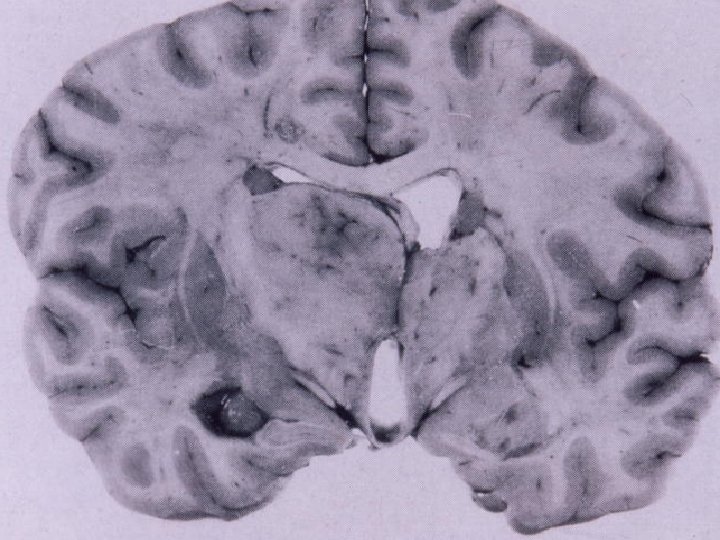
Haemorrhage and midline shift
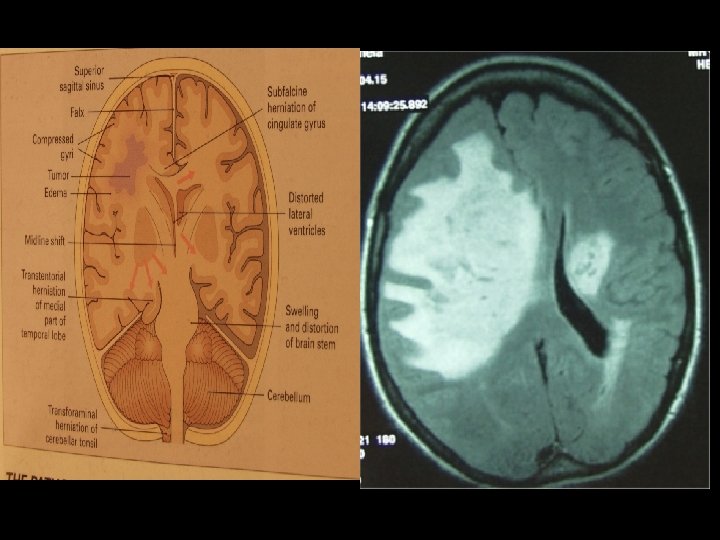
Raised ICP ~ As neoplasm grows – contents of the skull are compressed ~ Within the skull brain occupies 1400 mls CSF 100 -200 mls and blood 100 -150 mls ~ Displacement of CSF and blood compensate initially for mass effect ~ Then ICP rises quickly mass effect compression vascular insufficiency
IC ICP Herniations ~ Subfalcine herniation ~ Tentorial herniation ~ Tonsillar herniation
FALSE LOCALISING SIGNS ~ Occulomotor nerve compression ~ Abducens nerve compressed against the petrous ligament ~ Ipsilateral hemiparesis – from compression of the cerebral peduncle against the tentorium ~ PCA infarction from compression of the artery against the tentorium
Under the age of 16, 75% occur In the posterior fossa ~ Pilocytic astrocytoma ~ Ependymoma ~ Medulloblastoma

Medulloblastoma Childhood Male predominance
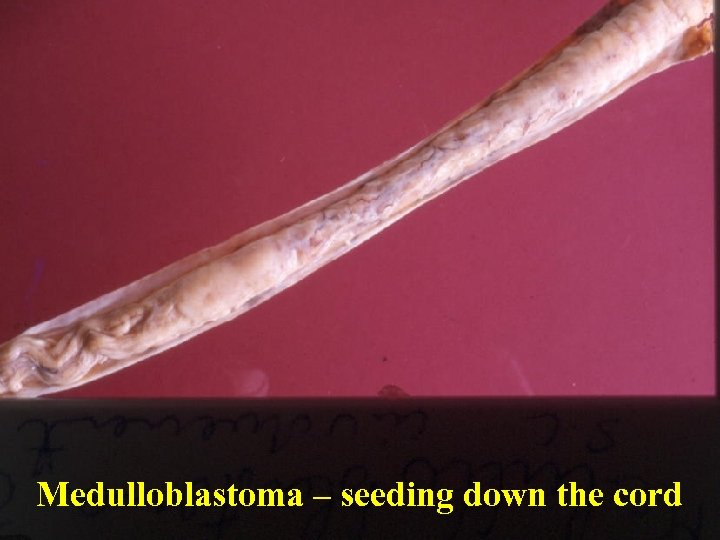
Medulloblastoma – seeding down the cord
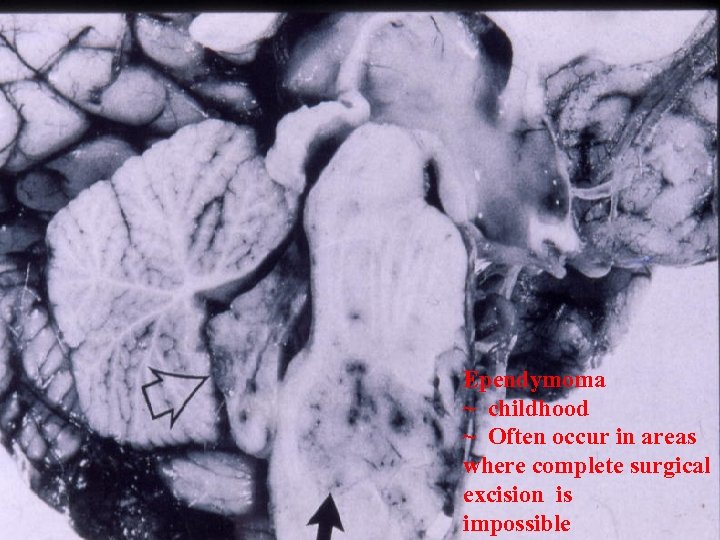
Ependymoma ~ childhood ~ Often occur in areas where complete surgical excision is impossible
Neuroectodermal tumours Prognosis depends on a. Site b. histology
Meningiomas ~ Older adults usually female ~ Increased incidence in Von Recklinhausen disease ~ Association between meningiomas and breast cancer
Meningioms Clinical presentation depends on: a) Site b) Rapidity of growth Prognosis – ~ benign (usually) ~ slowly growing ~ often can be completely excised
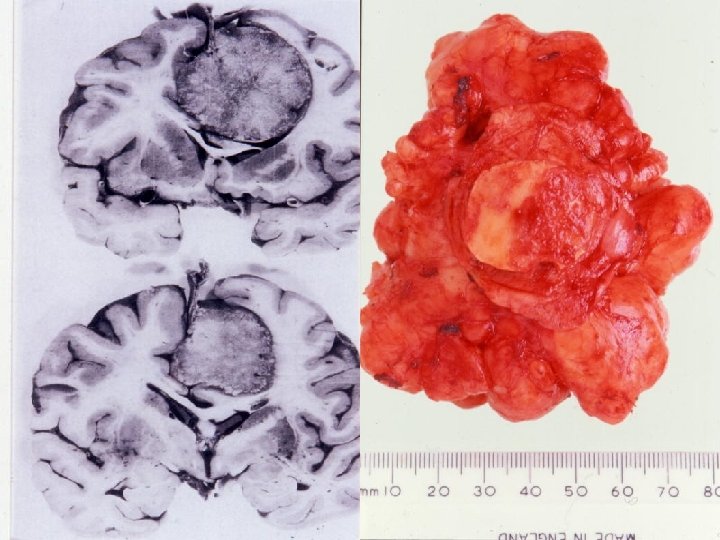
Meningioma arising from the falx cerebri

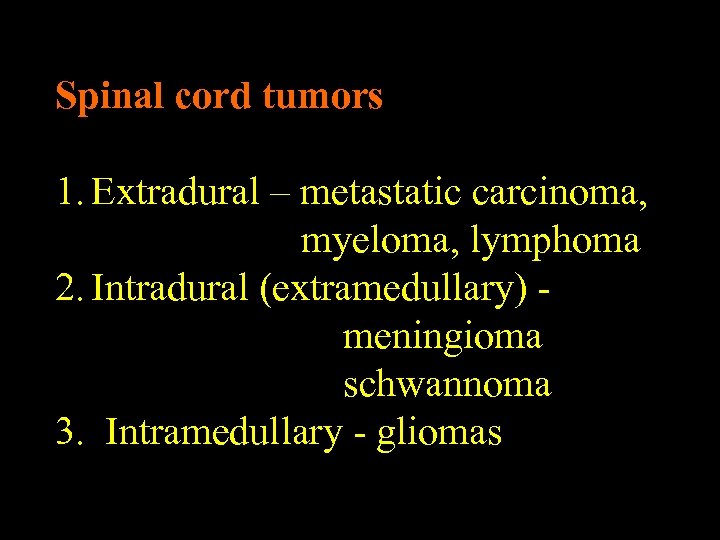
Spinal cord tumors 1. Extradural – metastatic carcinoma, myeloma, lymphoma 2. Intradural (extramedullary) meningioma schwannoma 3. Intramedullary - gliomas
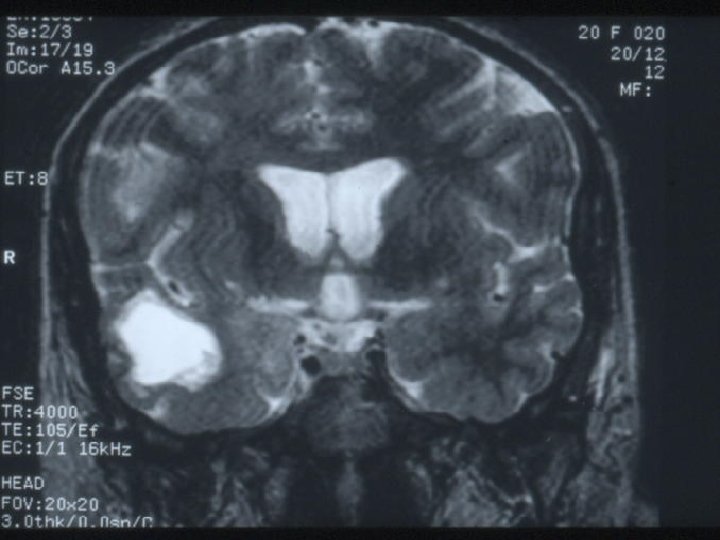
Metastatic tumours in Adults ~ Common ~ Over the age of 65 – commonest variety of intracerebral neoplasm ~ Mets in children uncommon but CNS well recognised site for relapse of ALL
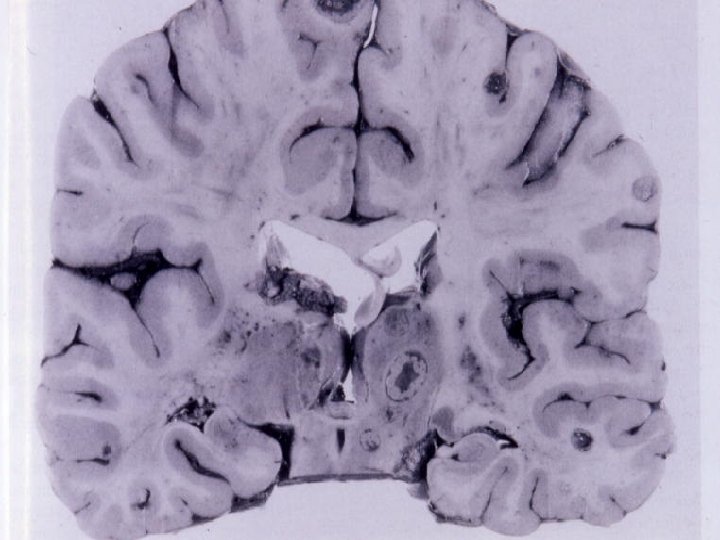

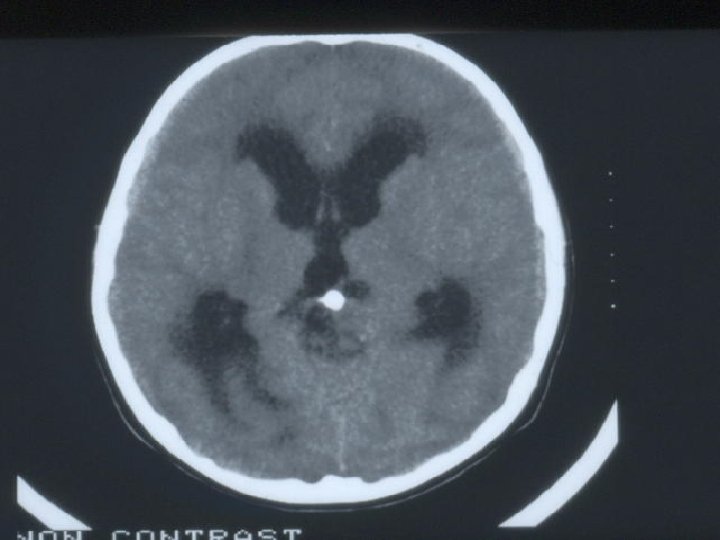
Case History ~ Patient transferred with a history of Headaches and drowsiness ~ Microcytic hypochromic anaemia, Thrombocytopenia ~ CT – hydrocephalus – no known cause ~ EVD inserted ~ IVH ~ RIP
E. O. N Admitted on 02/10/00 with stridor and Personality change Progressive deterioration Infective screen negative ? s. CJD ? ?
Investigations CSF – NAD MRI - ? EEG - NAD

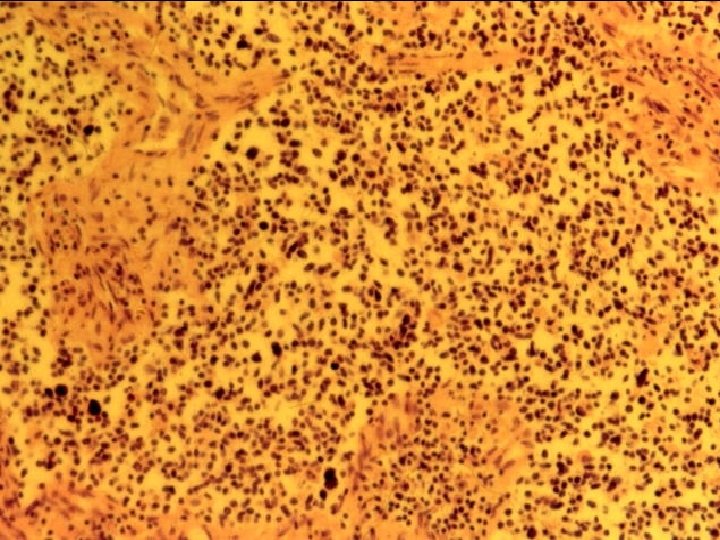
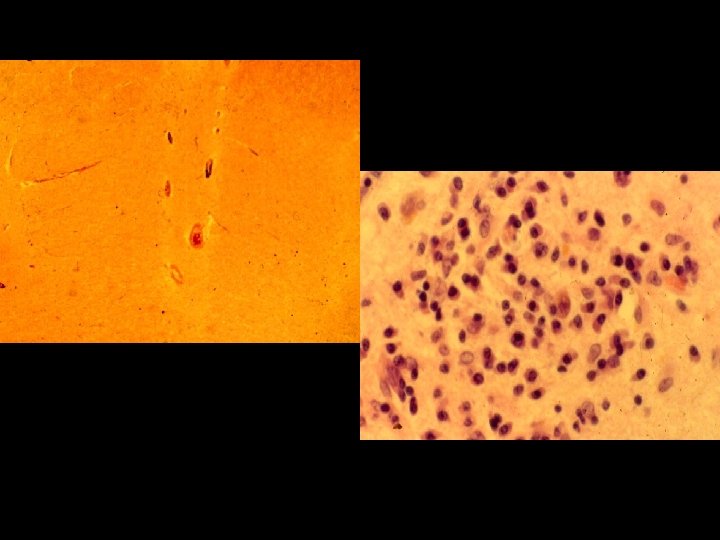
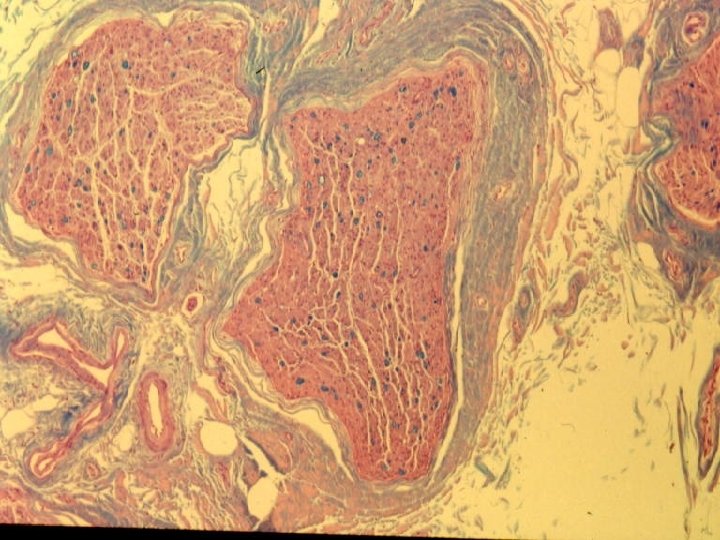
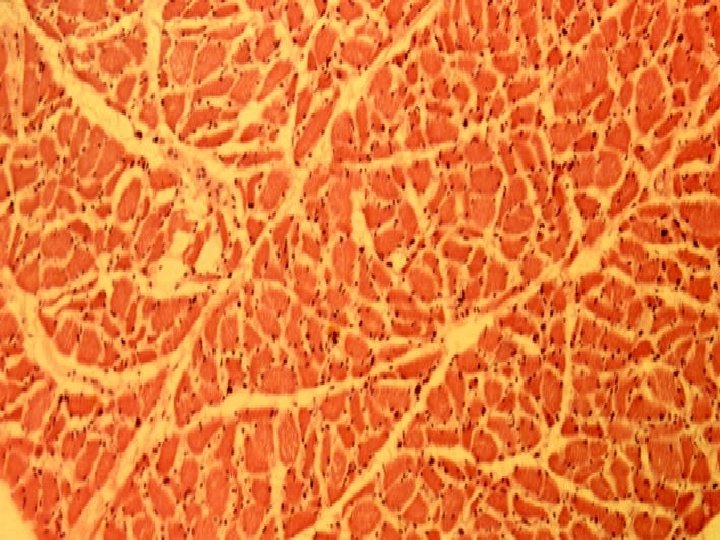
PM A 50/01 Paraneoplastic encephalomyelitis Tumour mass 8 x 6 x 4 cm, wt 120 gms Anterior, inferior and left lateral to the Thyroid
Paraneoplastic encephalomyelitis ~ neurological disorders of unknown cause associated with systemic malignancy ~ Subacute progressive course over mths – years ~ May precede follow or occur simultaneously with a systemic cancer
Include: 1. Encephalitis 2. Cerebellarr cortical degeneration 3. Myopathy 4. Peripheral neuropathy 5. Necrotising myelopathy
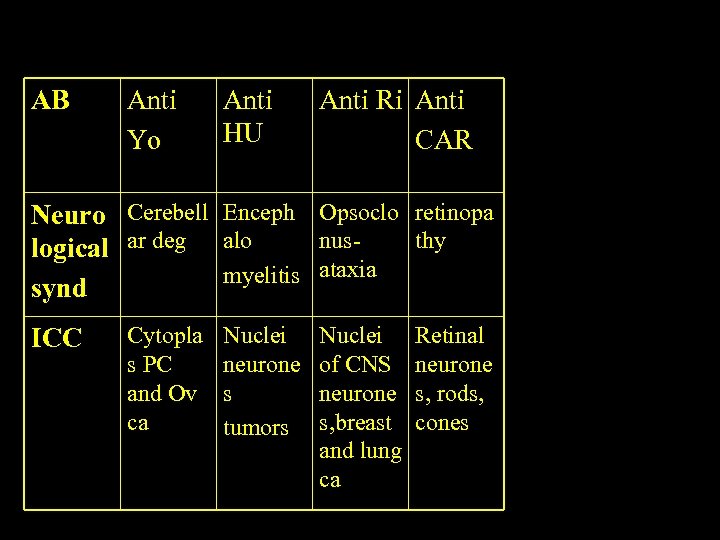
AB Anti Yo Anti HU Anti Ri Anti CAR Neuro Cerebell Enceph Opsoclo retinopa nusthy logical ar deg alo myelitis ataxia synd ICC Cytopla s PC and Ov ca Nuclei neurone s tumors Nuclei of CNS neurone s, breast and lung ca Retinal neurone s, rods, cones
Benign cystic lesions in the brain that may cause sudden death ~ colloid cyst of the third ventricle ~ Other cystic lesions

A 209/01
CONCLUSION 1. Brain tumours classified into intrinsic, extrinsic and spread from adjacent structures 2. Adults usually present with supratentorial tumours 3. Commonest primary tumour in adults gliomas. >65 metastatic tumours common 4. Paraneoplastic syndromes – non-metastatic complications of an underlying malignancy.
40840f26c18ac5a20206e21099d6a1c0.ppt