82716ab136d70c4e76fd45528aba6e34.ppt
- Количество слайдов: 62
 Tumor Cytogenetics Vundavalli Murty Department of Pathology & Cell Biology & Institute for Cancer Genetics Sept 18, 2017
Tumor Cytogenetics Vundavalli Murty Department of Pathology & Cell Biology & Institute for Cancer Genetics Sept 18, 2017
 Reference Material 1. Cancer Cytogenetics: Text Book: Heim S and Mitelman F, 2015 2. Recurrent Chromosome Aberrations in Cancer Web site http: //cgap. nci. nih. gov/Chromosomes/Recurrent. Aberrations 3. Atlas of Genetics and Cytogenetics in Oncology and Haematology Web site: http: //atlasgeneticsoncology. org// 15 March 2018 Page 2
Reference Material 1. Cancer Cytogenetics: Text Book: Heim S and Mitelman F, 2015 2. Recurrent Chromosome Aberrations in Cancer Web site http: //cgap. nci. nih. gov/Chromosomes/Recurrent. Aberrations 3. Atlas of Genetics and Cytogenetics in Oncology and Haematology Web site: http: //atlasgeneticsoncology. org// 15 March 2018 Page 2
 Overview - Chromosomes in human tumors are widely abnormal: David von Hansemann 1890: nuclear and mitotic abnormalities in tumors Boveri 1914: Chromosome abnormalities play a central role in transformaton - Controversy: Early 1950 s Whether the chromosome changes are primary events or merely secondary phenomena? - Changed view: Recurring chromosome aberrations associated with leukemia, lymphoma, sarcoma, carcinoma Proto-oncogenes identified at the breakpoints Experimental evidence for these genes in transformation Targeted drugs that inhibit gene product: e. g. STI 571 for BCR-ABL 15 March 2018 Page 3
Overview - Chromosomes in human tumors are widely abnormal: David von Hansemann 1890: nuclear and mitotic abnormalities in tumors Boveri 1914: Chromosome abnormalities play a central role in transformaton - Controversy: Early 1950 s Whether the chromosome changes are primary events or merely secondary phenomena? - Changed view: Recurring chromosome aberrations associated with leukemia, lymphoma, sarcoma, carcinoma Proto-oncogenes identified at the breakpoints Experimental evidence for these genes in transformation Targeted drugs that inhibit gene product: e. g. STI 571 for BCR-ABL 15 March 2018 Page 3
 Methods of Chromosome Preparations • Actively dividing cells can be arrested at metaphase or prometaphase stages using mitotic arresting agegns (eg. Colcemid) • Direct preparations or short-term cultures to represent in vivo conditions • • Hypotonic treatment & fixation A variety of methods: Giemsa-banding FISH (Fluorescence in situ hybridization) Probes to detect translocations, inversions, deletions, amplification • Chromosomal CGH, SKY, array CGH, Microarray 15 March 2018 Page 4
Methods of Chromosome Preparations • Actively dividing cells can be arrested at metaphase or prometaphase stages using mitotic arresting agegns (eg. Colcemid) • Direct preparations or short-term cultures to represent in vivo conditions • • Hypotonic treatment & fixation A variety of methods: Giemsa-banding FISH (Fluorescence in situ hybridization) Probes to detect translocations, inversions, deletions, amplification • Chromosomal CGH, SKY, array CGH, Microarray 15 March 2018 Page 4
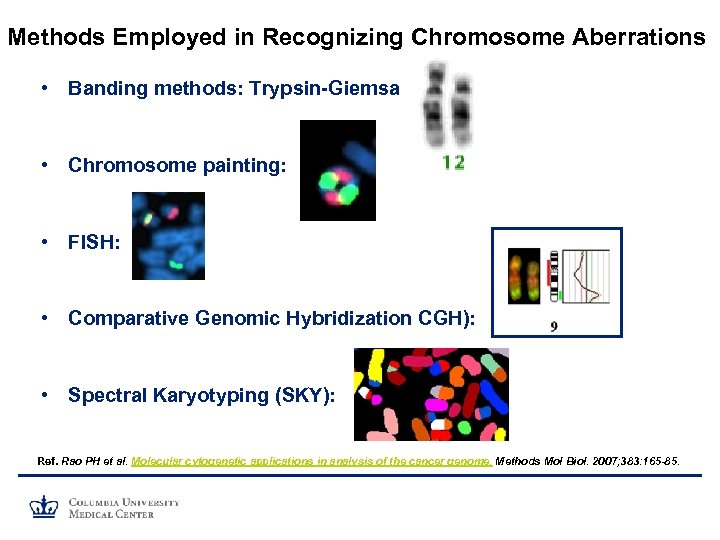 Methods Employed in Recognizing Chromosome Aberrations • Banding methods: Trypsin-Giemsa • Chromosome painting: • FISH: • Comparative Genomic Hybridization CGH): • Spectral Karyotyping (SKY): Ref. Rao PH et al. Molecular cytogenetic applications in analysis of the cancer genome. Methods Mol Biol. 2007; 383: 165 -85.
Methods Employed in Recognizing Chromosome Aberrations • Banding methods: Trypsin-Giemsa • Chromosome painting: • FISH: • Comparative Genomic Hybridization CGH): • Spectral Karyotyping (SKY): Ref. Rao PH et al. Molecular cytogenetic applications in analysis of the cancer genome. Methods Mol Biol. 2007; 383: 165 -85.
 15 March 2018 Page 6
15 March 2018 Page 6
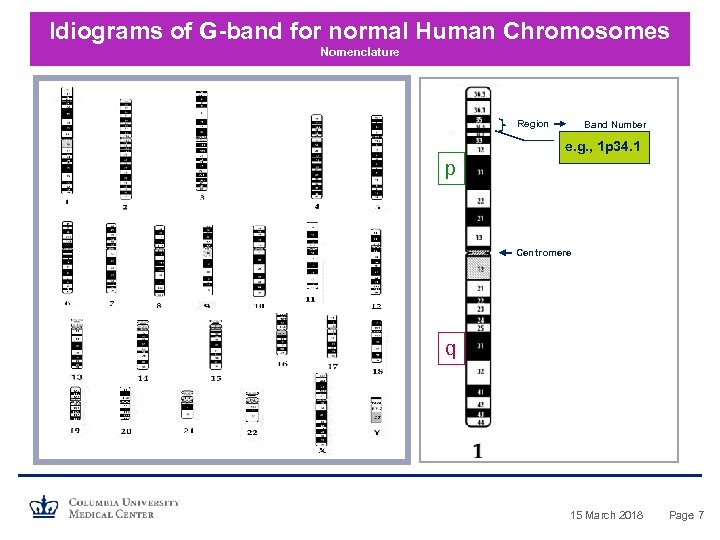 Idiograms of G-band for normal Human Chromosomes Nomenclature Region Band Number e. g. , 1 p 34. 1 p Centromere q 15 March 2018 Page 7
Idiograms of G-band for normal Human Chromosomes Nomenclature Region Band Number e. g. , 1 p 34. 1 p Centromere q 15 March 2018 Page 7
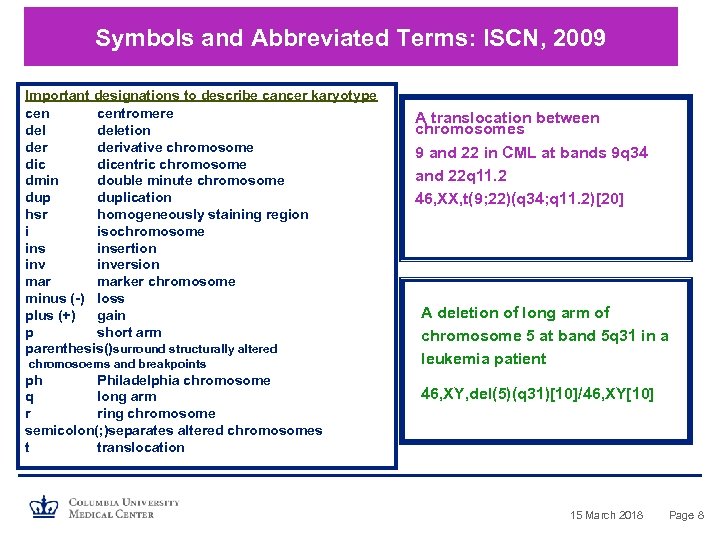 Symbols and Abbreviated Terms: ISCN, 2009 Important designations to describe cancer karyotype centromere deletion derivative chromosome dicentric chromosome dmin double minute chromosome duplication hsr homogeneously staining region i isochromosome insertion inversion marker chromosome minus (-) loss plus (+) gain p short arm parenthesis()surround structurally altered chromosoems and breakpoints ph Philadelphia chromosome q long arm r ring chromosome semicolon(; )separates altered chromosomes t translocation A translocation between chromosomes 9 and 22 in CML at bands 9 q 34 and 22 q 11. 2 46, XX, t(9; 22)(q 34; q 11. 2)[20] A deletion of long arm of chromosome 5 at band 5 q 31 in a leukemia patient 46, XY, del(5)(q 31)[10]/46, XY[10] 15 March 2018 Page 8
Symbols and Abbreviated Terms: ISCN, 2009 Important designations to describe cancer karyotype centromere deletion derivative chromosome dicentric chromosome dmin double minute chromosome duplication hsr homogeneously staining region i isochromosome insertion inversion marker chromosome minus (-) loss plus (+) gain p short arm parenthesis()surround structurally altered chromosoems and breakpoints ph Philadelphia chromosome q long arm r ring chromosome semicolon(; )separates altered chromosomes t translocation A translocation between chromosomes 9 and 22 in CML at bands 9 q 34 and 22 q 11. 2 46, XX, t(9; 22)(q 34; q 11. 2)[20] A deletion of long arm of chromosome 5 at band 5 q 31 in a leukemia patient 46, XY, del(5)(q 31)[10]/46, XY[10] 15 March 2018 Page 8
 Types & Consequences of Major chromosome changes • Ploidy (e. g. , haploid, triploid, tetraploid): Unclear • Aneuploidy (e. g. , tri-, tetra-, monosomy): Increased or decreased expression of set of genes • Reciprocal or non-reciprocal translocations (inversions): Overexpression/fusion gene • Deletions: Loss of expression • Duplications and Amplifications: Increased gene expression • Insertions: Loss or gain of function of genes Ref. Mitelman, F et al. , The impact of translocations and gene fusions on cancer causation. Nat. Rev. Cancer 7, 233– 245 (2007). 15 March 2018 Page 9
Types & Consequences of Major chromosome changes • Ploidy (e. g. , haploid, triploid, tetraploid): Unclear • Aneuploidy (e. g. , tri-, tetra-, monosomy): Increased or decreased expression of set of genes • Reciprocal or non-reciprocal translocations (inversions): Overexpression/fusion gene • Deletions: Loss of expression • Duplications and Amplifications: Increased gene expression • Insertions: Loss or gain of function of genes Ref. Mitelman, F et al. , The impact of translocations and gene fusions on cancer causation. Nat. Rev. Cancer 7, 233– 245 (2007). 15 March 2018 Page 9
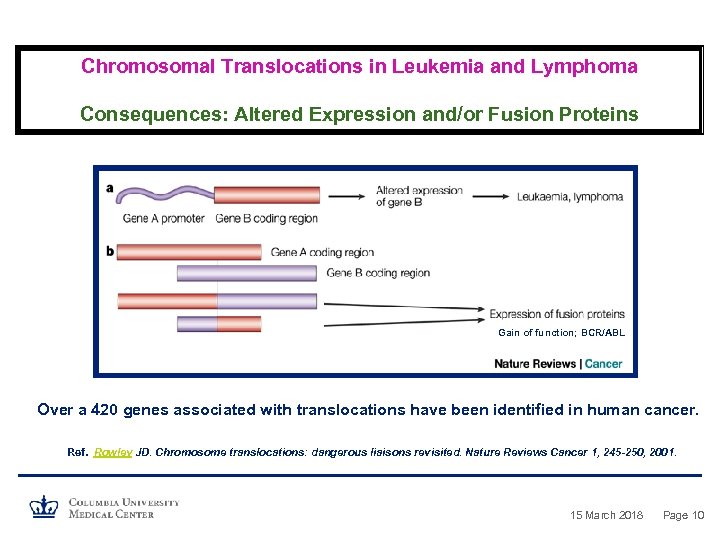 Chromosomal Translocations in Leukemia and Lymphoma Consequences: Altered Expression and/or Fusion Proteins Gain of function; BCR/ABL Over a 420 genes associated with translocations have been identified in human cancer. Ref. Rowley JD. Chromosome translocations: dangerous liaisons revisited. Nature Reviews Cancer 1, 245 -250, 2001. 15 March 2018 Page 10
Chromosomal Translocations in Leukemia and Lymphoma Consequences: Altered Expression and/or Fusion Proteins Gain of function; BCR/ABL Over a 420 genes associated with translocations have been identified in human cancer. Ref. Rowley JD. Chromosome translocations: dangerous liaisons revisited. Nature Reviews Cancer 1, 245 -250, 2001. 15 March 2018 Page 10
 Cancer is a Genetic (Chromosomal) Disease -Tumor cells exhibit non-random chromosome abnormalities -Recurrent in specific types of malignancies -Have been used as diagnostic and prognostic markers -Have lead to the understanding of biology of cancer
Cancer is a Genetic (Chromosomal) Disease -Tumor cells exhibit non-random chromosome abnormalities -Recurrent in specific types of malignancies -Have been used as diagnostic and prognostic markers -Have lead to the understanding of biology of cancer
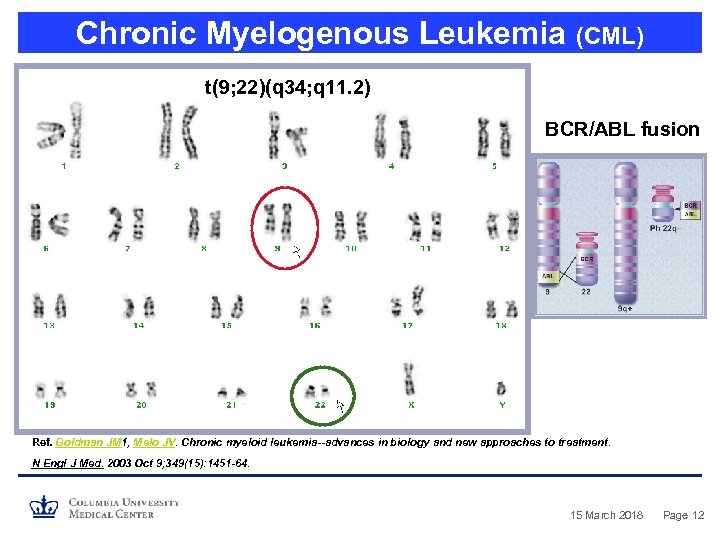 Chronic Myelogenous Leukemia (CML) t(9; 22)(q 34; q 11. 2) BCR/ABL fusion Ref. Goldman JM 1, Melo JV. Chronic myeloid leukemia--advances in biology and new approaches to treatment. N Engl J Med. 2003 Oct 9; 349(15): 1451 -64. 15 March 2018 Page 12
Chronic Myelogenous Leukemia (CML) t(9; 22)(q 34; q 11. 2) BCR/ABL fusion Ref. Goldman JM 1, Melo JV. Chronic myeloid leukemia--advances in biology and new approaches to treatment. N Engl J Med. 2003 Oct 9; 349(15): 1451 -64. 15 March 2018 Page 12
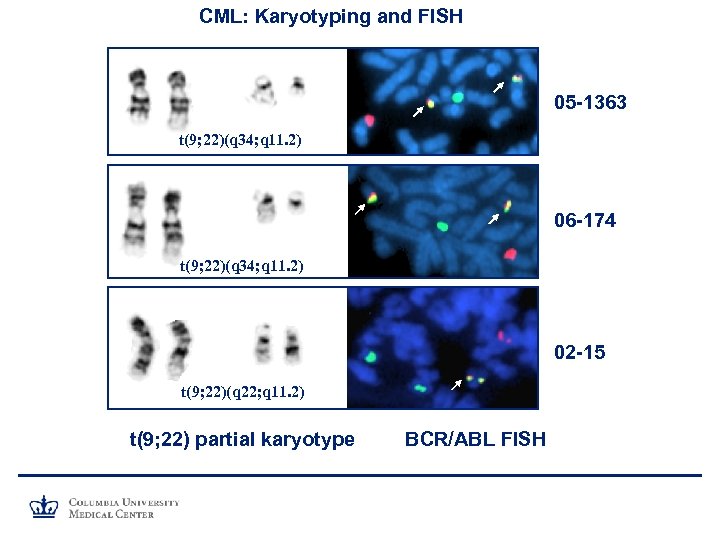 CML: Karyotyping and FISH 05 -1363 t(9; 22)(q 34; q 11. 2) 06 -174 t(9; 22)(q 34; q 11. 2) 02 -15 t(9; 22)(q 22; q 11. 2) t(9; 22) partial karyotype BCR/ABL FISH
CML: Karyotyping and FISH 05 -1363 t(9; 22)(q 34; q 11. 2) 06 -174 t(9; 22)(q 34; q 11. 2) 02 -15 t(9; 22)(q 22; q 11. 2) t(9; 22) partial karyotype BCR/ABL FISH
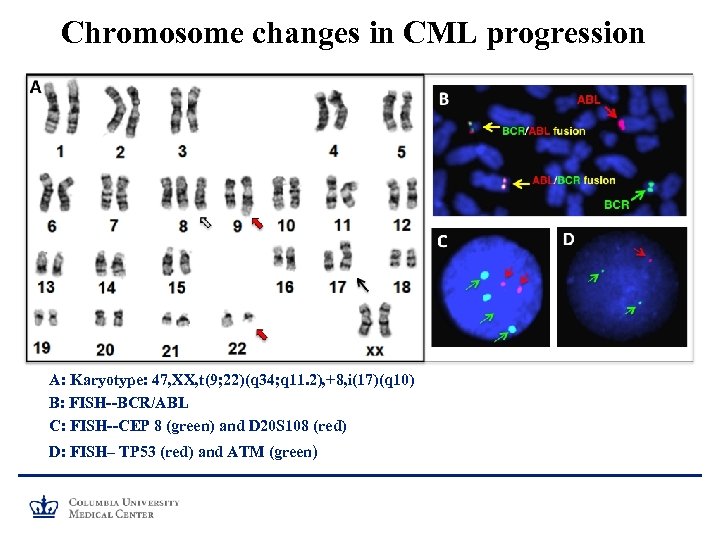 Chromosome changes in CML progression A: Karyotype: 47, XX, t(9; 22)(q 34; q 11. 2), +8, i(17)(q 10) B: FISH--BCR/ABL C: FISH--CEP 8 (green) and D 20 S 108 (red) D: FISH– TP 53 (red) and ATM (green)
Chromosome changes in CML progression A: Karyotype: 47, XX, t(9; 22)(q 34; q 11. 2), +8, i(17)(q 10) B: FISH--BCR/ABL C: FISH--CEP 8 (green) and D 20 S 108 (red) D: FISH– TP 53 (red) and ATM (green)
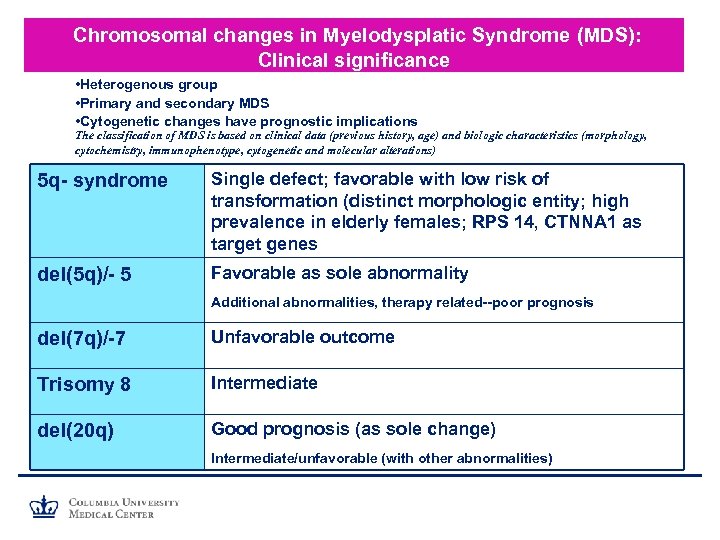 Chromosomal changes in Myelodysplatic Syndrome (MDS): Clinical significance • Heterogenous group • Primary and secondary MDS • Cytogenetic changes have prognostic implications The classification of MDS is based on clinical data (previous history, age) and biologic characteristics (morphology, cytochemistry, immunophenotype, cytogenetic and molecular alterations) 5 q- syndrome Single defect; favorable with low risk of transformation (distinct morphologic entity; high prevalence in elderly females; RPS 14, CTNNA 1 as target genes del(5 q)/- 5 Favorable as sole abnormality Additional abnormalities, therapy related--poor prognosis del(7 q)/-7 Unfavorable outcome Trisomy 8 Intermediate del(20 q) Good prognosis (as sole change) Intermediate/unfavorable (with other abnormalities)
Chromosomal changes in Myelodysplatic Syndrome (MDS): Clinical significance • Heterogenous group • Primary and secondary MDS • Cytogenetic changes have prognostic implications The classification of MDS is based on clinical data (previous history, age) and biologic characteristics (morphology, cytochemistry, immunophenotype, cytogenetic and molecular alterations) 5 q- syndrome Single defect; favorable with low risk of transformation (distinct morphologic entity; high prevalence in elderly females; RPS 14, CTNNA 1 as target genes del(5 q)/- 5 Favorable as sole abnormality Additional abnormalities, therapy related--poor prognosis del(7 q)/-7 Unfavorable outcome Trisomy 8 Intermediate del(20 q) Good prognosis (as sole change) Intermediate/unfavorable (with other abnormalities)
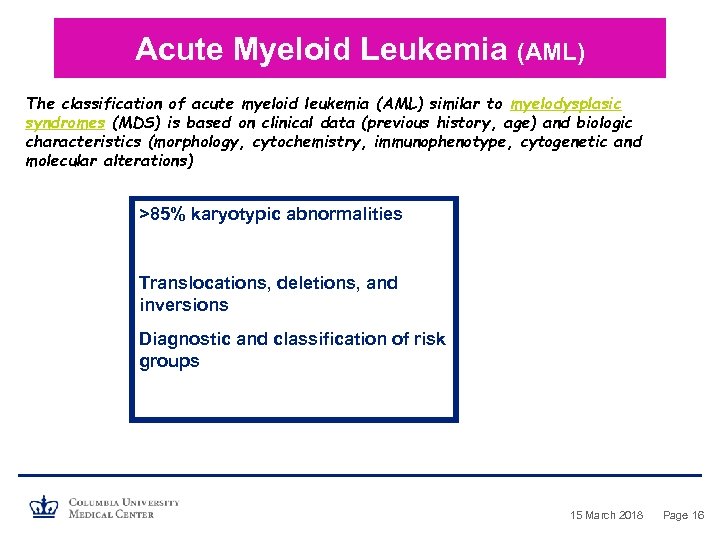 Acute Myeloid Leukemia (AML) The classification of acute myeloid leukemia (AML) similar to myelodysplasic syndromes (MDS) is based on clinical data (previous history, age) and biologic characteristics (morphology, cytochemistry, immunophenotype, cytogenetic and molecular alterations) >85% karyotypic abnormalities Translocations, deletions, and inversions Diagnostic and classification of risk groups 15 March 2018 Page 16
Acute Myeloid Leukemia (AML) The classification of acute myeloid leukemia (AML) similar to myelodysplasic syndromes (MDS) is based on clinical data (previous history, age) and biologic characteristics (morphology, cytochemistry, immunophenotype, cytogenetic and molecular alterations) >85% karyotypic abnormalities Translocations, deletions, and inversions Diagnostic and classification of risk groups 15 March 2018 Page 16
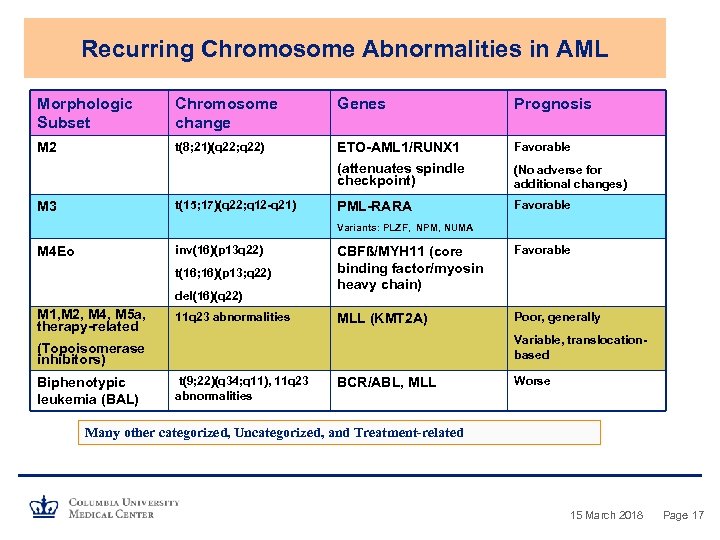 Recurring Chromosome Abnormalities in AML Morphologic Subset Chromosome change Genes Prognosis M 2 t(8; 21)(q 22; q 22) ETO-AML 1/RUNX 1 Favorable (attenuates spindle checkpoint) (No adverse for additional changes) PML-RARA Favorable t(15; 17)(q 22; q 12 -q 21) M 3 Variants: PLZF, NPM, NUMA inv(16)(p 13 q 22) M 4 Eo t(16; 16)(p 13; q 22) del(16)(q 22) M 1, M 2, M 4, M 5 a, therapy-related 11 q 23 abnormalities CBFß/MYH 11 (core binding factor/myosin heavy chain) Favorable MLL (KMT 2 A) Poor, generally Variable, translocationbased (Topoisomerase inhibitors) Biphenotypic leukemia (BAL) t(9; 22)(q 34; q 11), 11 q 23 abnormalities BCR/ABL, MLL Worse Many other categorized, Uncategorized, and Treatment-related 15 March 2018 Page 17
Recurring Chromosome Abnormalities in AML Morphologic Subset Chromosome change Genes Prognosis M 2 t(8; 21)(q 22; q 22) ETO-AML 1/RUNX 1 Favorable (attenuates spindle checkpoint) (No adverse for additional changes) PML-RARA Favorable t(15; 17)(q 22; q 12 -q 21) M 3 Variants: PLZF, NPM, NUMA inv(16)(p 13 q 22) M 4 Eo t(16; 16)(p 13; q 22) del(16)(q 22) M 1, M 2, M 4, M 5 a, therapy-related 11 q 23 abnormalities CBFß/MYH 11 (core binding factor/myosin heavy chain) Favorable MLL (KMT 2 A) Poor, generally Variable, translocationbased (Topoisomerase inhibitors) Biphenotypic leukemia (BAL) t(9; 22)(q 34; q 11), 11 q 23 abnormalities BCR/ABL, MLL Worse Many other categorized, Uncategorized, and Treatment-related 15 March 2018 Page 17
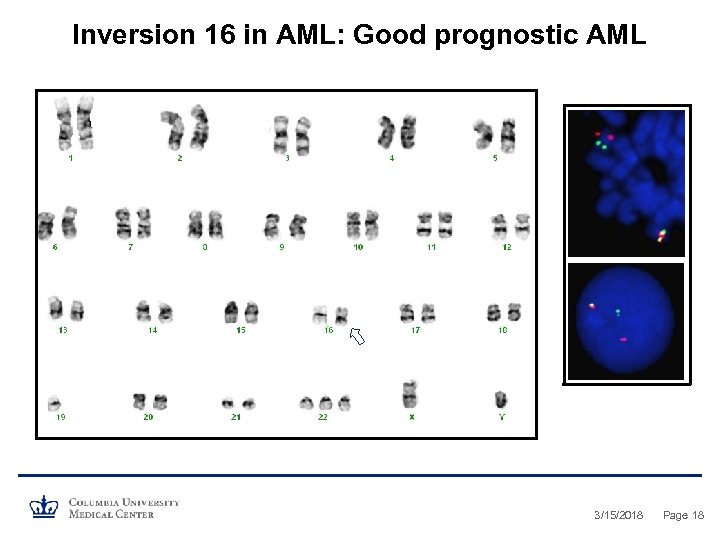 Inversion 16 in AML: Good prognostic AML 3/15/2018 Page 18
Inversion 16 in AML: Good prognostic AML 3/15/2018 Page 18
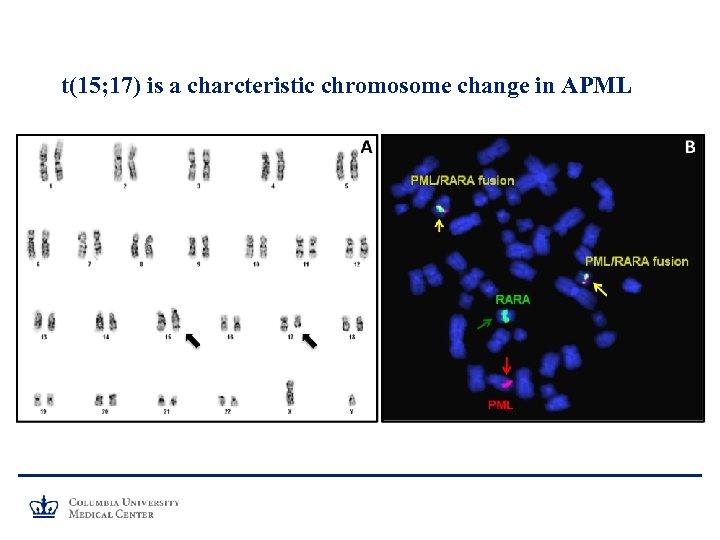 t(15; 17) is a charcteristic chromosome change in APML
t(15; 17) is a charcteristic chromosome change in APML
 Therapy Related MDS and AML
Therapy Related MDS and AML
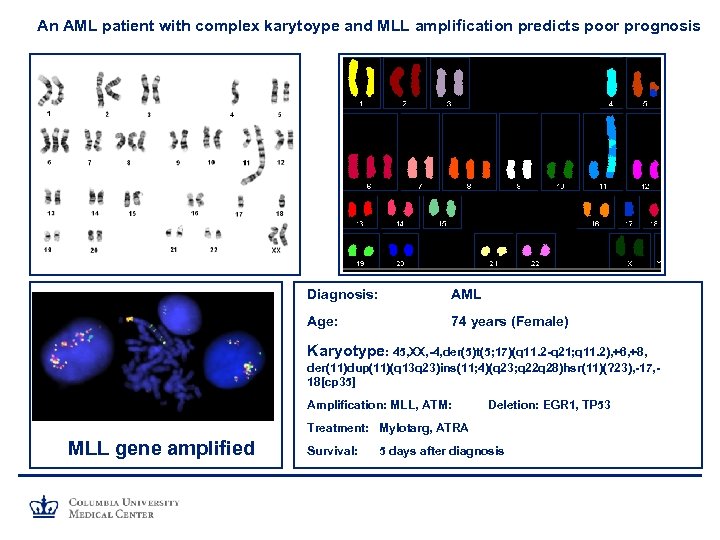 An AML patient with complex karytoype and MLL amplification predicts poor prognosis Diagnosis: AML Age: 74 years (Female) Karyotype: 45, XX, -4, der(5)t(5; 17)(q 11. 2 -q 21; q 11. 2), +6, +8, der(11)dup(11)(q 13 q 23)ins(11; 4)(q 23; q 22 q 28)hsr(11)(? 23), -17, 18[cp 35] Amplification: MLL, ATM: Deletion: EGR 1, TP 53 Treatment: Mylotarg, ATRA MLL gene amplified Survival: 5 days after diagnosis
An AML patient with complex karytoype and MLL amplification predicts poor prognosis Diagnosis: AML Age: 74 years (Female) Karyotype: 45, XX, -4, der(5)t(5; 17)(q 11. 2 -q 21; q 11. 2), +6, +8, der(11)dup(11)(q 13 q 23)ins(11; 4)(q 23; q 22 q 28)hsr(11)(? 23), -17, 18[cp 35] Amplification: MLL, ATM: Deletion: EGR 1, TP 53 Treatment: Mylotarg, ATRA MLL gene amplified Survival: 5 days after diagnosis
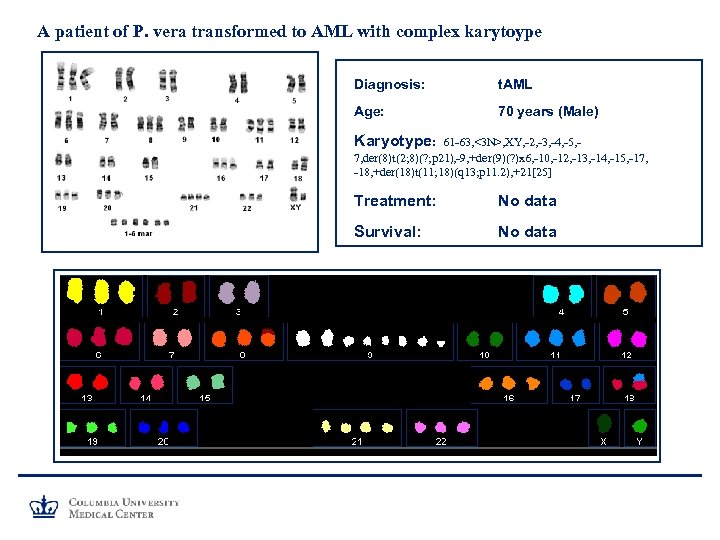 A patient of P. vera transformed to AML with complex karytoype Diagnosis: t. AML Age: 70 years (Male) Karyotype: 61 -63, <3 N>, XY, -2, -3, -4, -5, 7, der(8)t(2; 8)(? ; p 21), -9, +der(9)(? )x 6, -10, -12, -13, -14, -15, -17, -18, +der(18)t(11; 18)(q 13; p 11. 2), +21[25] Treatment: No data Survival: No data
A patient of P. vera transformed to AML with complex karytoype Diagnosis: t. AML Age: 70 years (Male) Karyotype: 61 -63, <3 N>, XY, -2, -3, -4, -5, 7, der(8)t(2; 8)(? ; p 21), -9, +der(9)(? )x 6, -10, -12, -13, -14, -15, -17, -18, +der(18)t(11; 18)(q 13; p 11. 2), +21[25] Treatment: No data Survival: No data
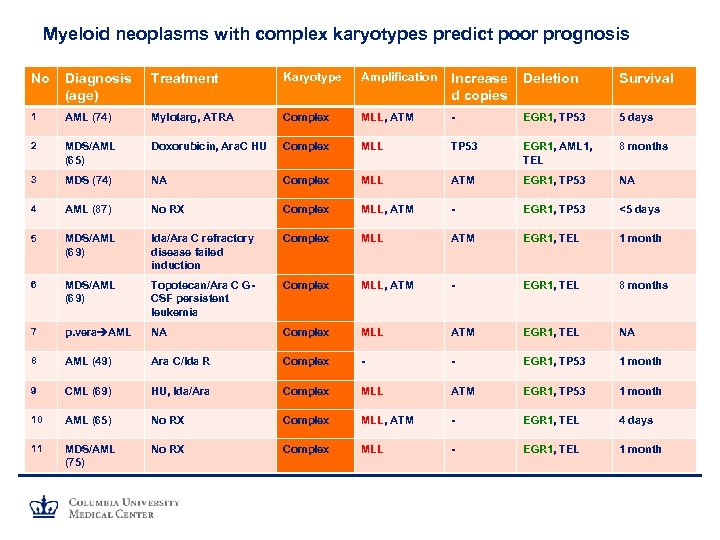 Myeloid neoplasms with complex karyotypes predict poor prognosis No Diagnosis (age) Treatment Karyotype Amplification Increase d copies Deletion Survival 1 AML (74) Mylotarg, ATRA Complex MLL, ATM - EGR 1, TP 53 5 days 2 MDS/AML (65) Doxorubicin, Ara. C HU Complex MLL TP 53 EGR 1, AML 1, TEL 8 months 3 MDS (74) NA Complex MLL ATM EGR 1, TP 53 NA 4 AML (87) No RX Complex MLL, ATM - EGR 1, TP 53 <5 days 5 MDS/AML (69) Ida/Ara C refractory disease failed induction Complex MLL ATM EGR 1, TEL 1 month 6 MDS/AML (69) Topotecan/Ara C GCSF persistent leukemia Complex MLL, ATM - EGR 1, TEL 8 months 7 p. vera AML NA Complex MLL ATM EGR 1, TEL NA 8 AML (49) Ara C/Ida R Complex - - EGR 1, TP 53 1 month 9 CML (69) HU, Ida/Ara Complex MLL ATM EGR 1, TP 53 1 month 10 AML (65) No RX Complex MLL, ATM - EGR 1, TEL 4 days 11 MDS/AML (75) No RX Complex MLL - EGR 1, TEL 1 month
Myeloid neoplasms with complex karyotypes predict poor prognosis No Diagnosis (age) Treatment Karyotype Amplification Increase d copies Deletion Survival 1 AML (74) Mylotarg, ATRA Complex MLL, ATM - EGR 1, TP 53 5 days 2 MDS/AML (65) Doxorubicin, Ara. C HU Complex MLL TP 53 EGR 1, AML 1, TEL 8 months 3 MDS (74) NA Complex MLL ATM EGR 1, TP 53 NA 4 AML (87) No RX Complex MLL, ATM - EGR 1, TP 53 <5 days 5 MDS/AML (69) Ida/Ara C refractory disease failed induction Complex MLL ATM EGR 1, TEL 1 month 6 MDS/AML (69) Topotecan/Ara C GCSF persistent leukemia Complex MLL, ATM - EGR 1, TEL 8 months 7 p. vera AML NA Complex MLL ATM EGR 1, TEL NA 8 AML (49) Ara C/Ida R Complex - - EGR 1, TP 53 1 month 9 CML (69) HU, Ida/Ara Complex MLL ATM EGR 1, TP 53 1 month 10 AML (65) No RX Complex MLL, ATM - EGR 1, TEL 4 days 11 MDS/AML (75) No RX Complex MLL - EGR 1, TEL 1 month
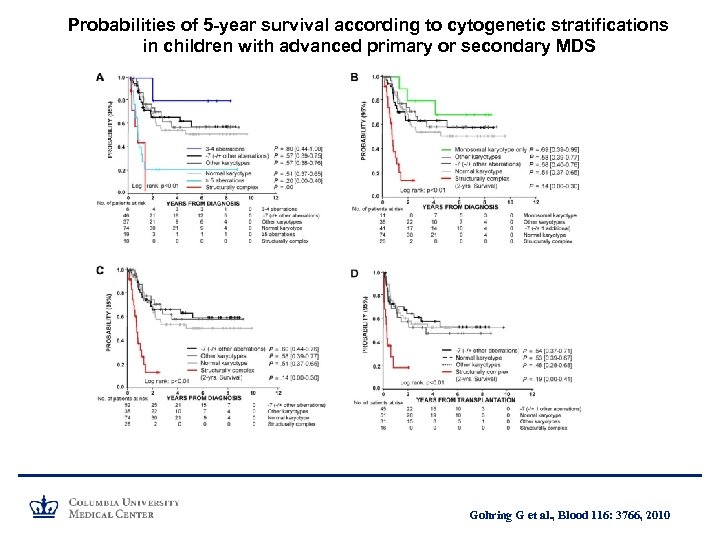 Probabilities of 5 -year survival according to cytogenetic stratifications in children with advanced primary or secondary MDS Gohring G et al. , Blood 116: 3766, 2010
Probabilities of 5 -year survival according to cytogenetic stratifications in children with advanced primary or secondary MDS Gohring G et al. , Blood 116: 3766, 2010
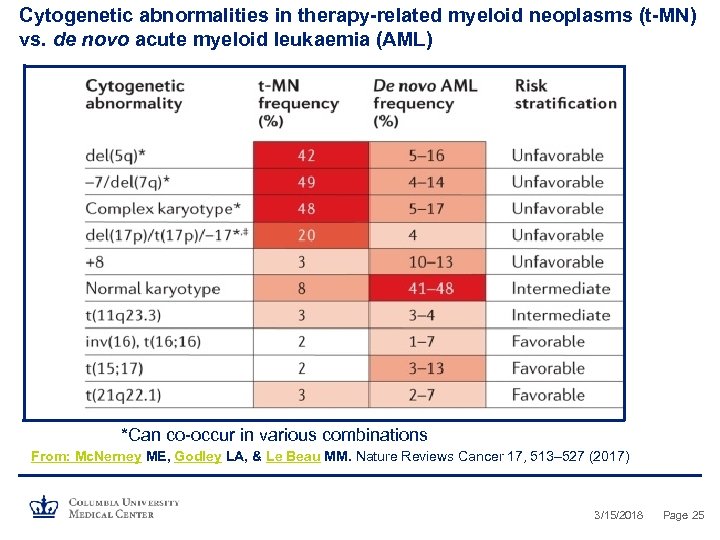 Cytogenetic abnormalities in therapy-related myeloid neoplasms (t-MN) vs. de novo acute myeloid leukaemia (AML) *Can co-occur in various combinations From: Mc. Nerney ME, Godley LA, & Le Beau MM. Nature Reviews Cancer 17, 513– 527 (2017) 3/15/2018 Page 25
Cytogenetic abnormalities in therapy-related myeloid neoplasms (t-MN) vs. de novo acute myeloid leukaemia (AML) *Can co-occur in various combinations From: Mc. Nerney ME, Godley LA, & Le Beau MM. Nature Reviews Cancer 17, 513– 527 (2017) 3/15/2018 Page 25
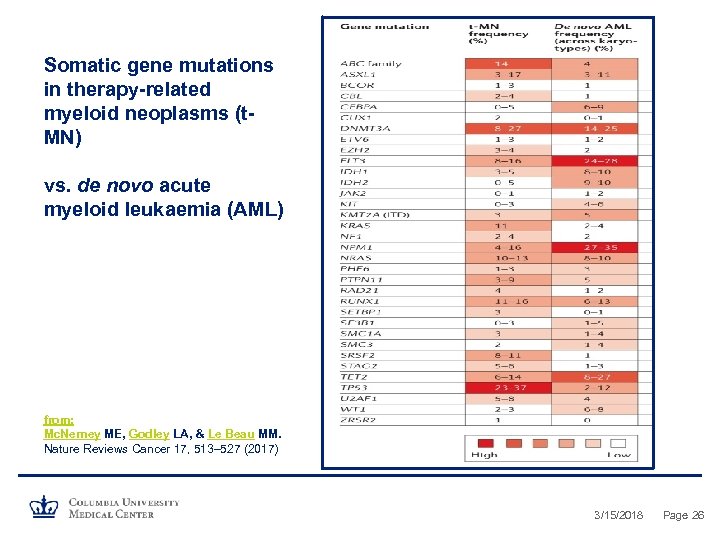 Somatic gene mutations in therapy-related myeloid neoplasms (t. MN) vs. de novo acute myeloid leukaemia (AML) from: Mc. Nerney ME, Godley LA, & Le Beau MM. Nature Reviews Cancer 17, 513– 527 (2017) 3/15/2018 Page 26
Somatic gene mutations in therapy-related myeloid neoplasms (t. MN) vs. de novo acute myeloid leukaemia (AML) from: Mc. Nerney ME, Godley LA, & Le Beau MM. Nature Reviews Cancer 17, 513– 527 (2017) 3/15/2018 Page 26
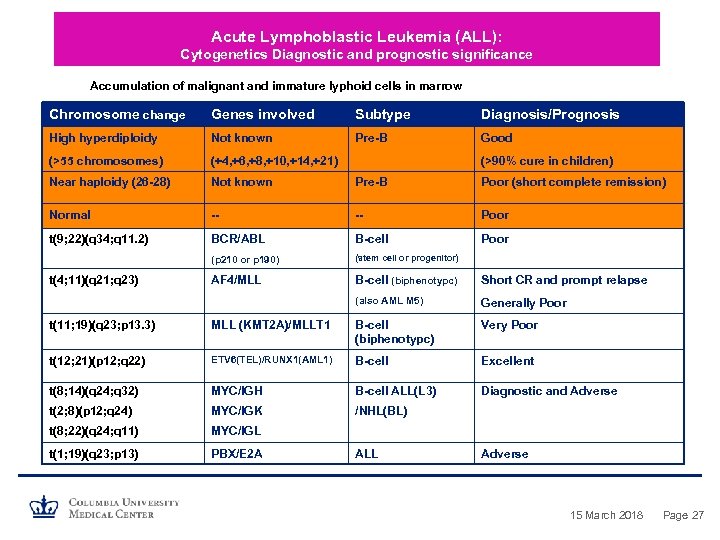 Acute Lymphoblastic Leukemia (ALL): Cytogenetics Diagnostic and prognostic significance Accumulation of malignant and immature lyphoid cells in marrow Chromosome change Genes involved Subtype Diagnosis/Prognosis High hyperdiploidy Not known Pre-B Good (>55 chromosomes) (+4, +6, +8, +10, +14, +21) Near haploidy (26 -28) Not known Pre-B Poor (short complete remission) Normal -- -- Poor t(9; 22)(q 34; q 11. 2) BCR/ABL B-cell Poor (p 210 or p 190) (stem cell or progenitor) AF 4/MLL B-cell (biphenotypc) Short CR and prompt relapse (also AML M 5) Generally Poor t(4; 11)(q 21; q 23) (>90% cure in children) t(11; 19)(q 23; p 13. 3) MLL (KMT 2 A)/MLLT 1 B-cell (biphenotypc) Very Poor t(12; 21)(p 12; q 22) ETV 6(TEL)/RUNX 1(AML 1) B-cell Excellent t(8; 14)(q 24; q 32) MYC/IGH B-cell ALL(L 3) Diagnostic and Adverse t(2; 8)(p 12; q 24) MYC/IGK /NHL(BL) t(8; 22)(q 24; q 11) MYC/IGL t(1; 19)(q 23; p 13) PBX/E 2 A ALL Adverse 15 March 2018 Page 27
Acute Lymphoblastic Leukemia (ALL): Cytogenetics Diagnostic and prognostic significance Accumulation of malignant and immature lyphoid cells in marrow Chromosome change Genes involved Subtype Diagnosis/Prognosis High hyperdiploidy Not known Pre-B Good (>55 chromosomes) (+4, +6, +8, +10, +14, +21) Near haploidy (26 -28) Not known Pre-B Poor (short complete remission) Normal -- -- Poor t(9; 22)(q 34; q 11. 2) BCR/ABL B-cell Poor (p 210 or p 190) (stem cell or progenitor) AF 4/MLL B-cell (biphenotypc) Short CR and prompt relapse (also AML M 5) Generally Poor t(4; 11)(q 21; q 23) (>90% cure in children) t(11; 19)(q 23; p 13. 3) MLL (KMT 2 A)/MLLT 1 B-cell (biphenotypc) Very Poor t(12; 21)(p 12; q 22) ETV 6(TEL)/RUNX 1(AML 1) B-cell Excellent t(8; 14)(q 24; q 32) MYC/IGH B-cell ALL(L 3) Diagnostic and Adverse t(2; 8)(p 12; q 24) MYC/IGK /NHL(BL) t(8; 22)(q 24; q 11) MYC/IGL t(1; 19)(q 23; p 13) PBX/E 2 A ALL Adverse 15 March 2018 Page 27
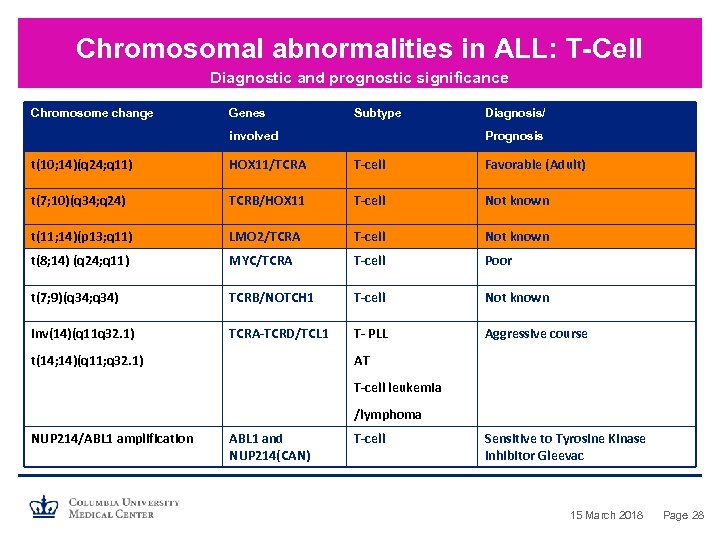 Chromosomal abnormalities in ALL: T-Cell Diagnostic and prognostic significance Chromosome change Genes Subtype involved Diagnosis/ Prognosis t(10; 14)(q 24; q 11) HOX 11/TCRA T-cell Favorable (Adult) t(7; 10)(q 34; q 24) TCRB/HOX 11 T-cell Not known t(11; 14)(p 13; q 11) LMO 2/TCRA T-cell Not known t(8; 14) (q 24; q 11) MYC/TCRA T-cell Poor t(7; 9)(q 34; q 34) TCRB/NOTCH 1 T-cell Not known inv(14)(q 11 q 32. 1) TCRA-TCRD/TCL 1 T- PLL Aggressive course t(14; 14)(q 11; q 32. 1) AT T-cell leukemia /lymphoma NUP 214/ABL 1 amplification ABL 1 and NUP 214(CAN) T-cell Sensitive to Tyrosine Kinase inhibitor Gleevac 15 March 2018 Page 28
Chromosomal abnormalities in ALL: T-Cell Diagnostic and prognostic significance Chromosome change Genes Subtype involved Diagnosis/ Prognosis t(10; 14)(q 24; q 11) HOX 11/TCRA T-cell Favorable (Adult) t(7; 10)(q 34; q 24) TCRB/HOX 11 T-cell Not known t(11; 14)(p 13; q 11) LMO 2/TCRA T-cell Not known t(8; 14) (q 24; q 11) MYC/TCRA T-cell Poor t(7; 9)(q 34; q 34) TCRB/NOTCH 1 T-cell Not known inv(14)(q 11 q 32. 1) TCRA-TCRD/TCL 1 T- PLL Aggressive course t(14; 14)(q 11; q 32. 1) AT T-cell leukemia /lymphoma NUP 214/ABL 1 amplification ABL 1 and NUP 214(CAN) T-cell Sensitive to Tyrosine Kinase inhibitor Gleevac 15 March 2018 Page 28
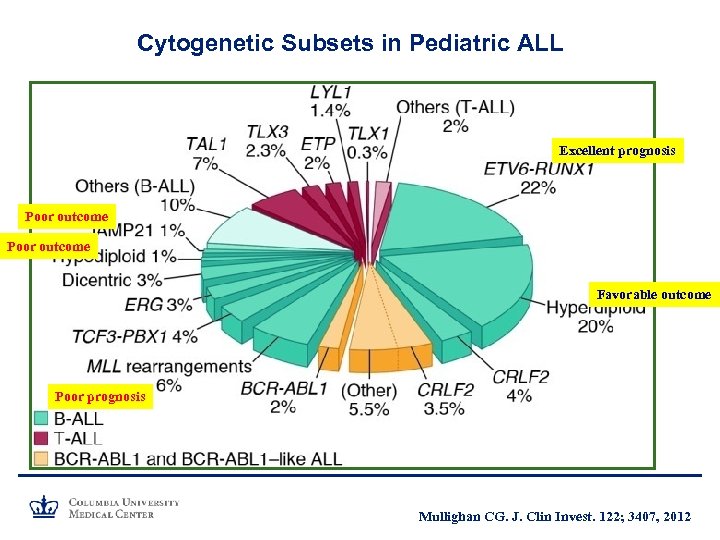 Cytogenetic Subsets in Pediatric ALL Excellent prognosis Poor outcome Favorable outcome Poor prognosis Mullighan CG. J. Clin Invest. 122; 3407, 2012
Cytogenetic Subsets in Pediatric ALL Excellent prognosis Poor outcome Favorable outcome Poor prognosis Mullighan CG. J. Clin Invest. 122; 3407, 2012
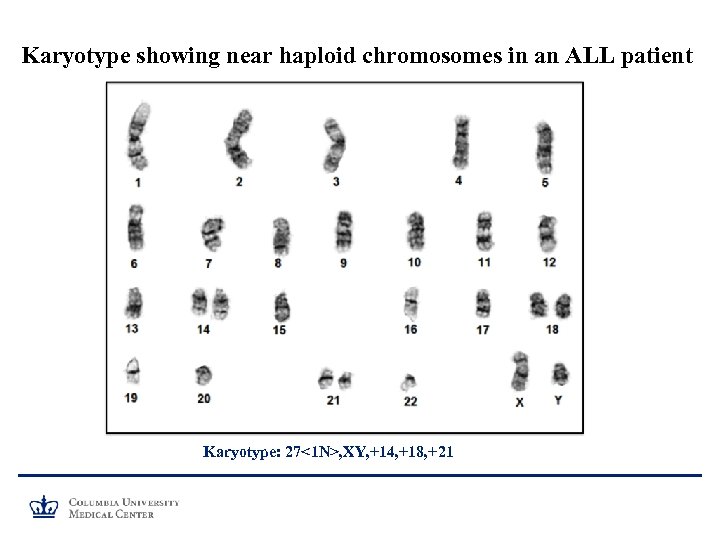 Karyotype showing near haploid chromosomes in an ALL patient Karyotype: 27<1 N>, XY, +14, +18, +21
Karyotype showing near haploid chromosomes in an ALL patient Karyotype: 27<1 N>, XY, +14, +18, +21
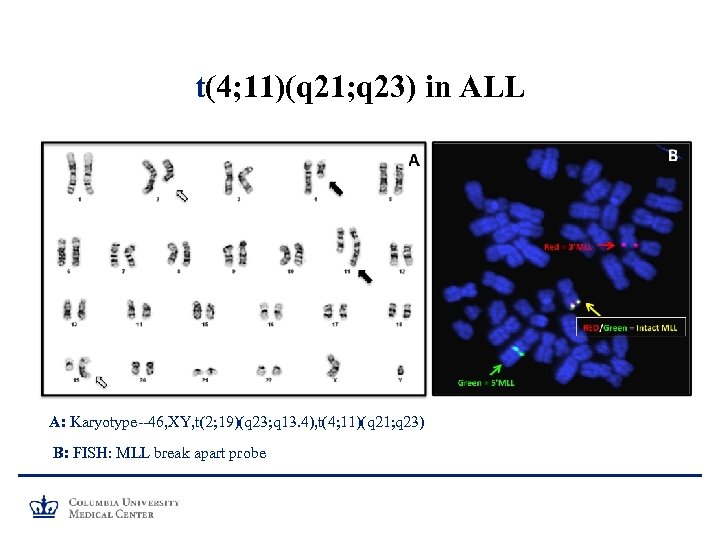 t(4; 11)(q 21; q 23) in ALL A: Karyotype--46, XY, t(2; 19)(q 23; q 13. 4), t(4; 11)(q 21; q 23) B: FISH: MLL break apart probe
t(4; 11)(q 21; q 23) in ALL A: Karyotype--46, XY, t(2; 19)(q 23; q 13. 4), t(4; 11)(q 21; q 23) B: FISH: MLL break apart probe
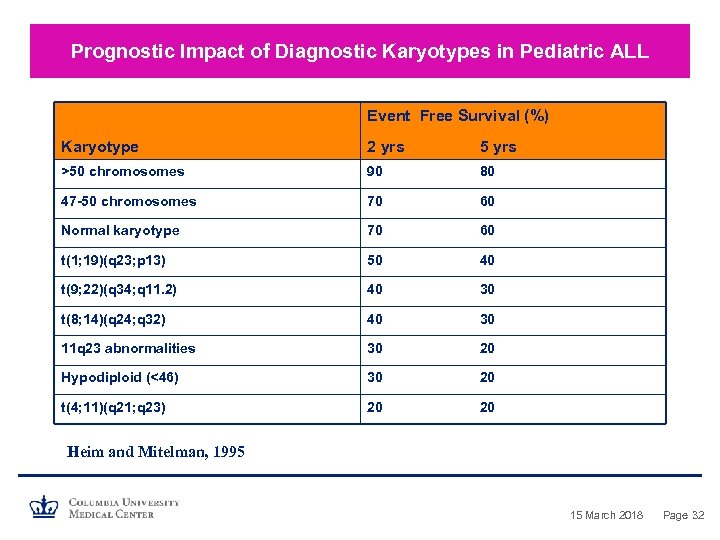 Prognostic Impact of Diagnostic Karyotypes in Pediatric ALL Event Free Survival (%) Karyotype 2 yrs 5 yrs >50 chromosomes 90 80 47 -50 chromosomes 70 60 Normal karyotype 70 60 t(1; 19)(q 23; p 13) 50 40 t(9; 22)(q 34; q 11. 2) 40 30 t(8; 14)(q 24; q 32) 40 30 11 q 23 abnormalities 30 20 Hypodiploid (<46) 30 20 t(4; 11)(q 21; q 23) 20 20 Heim and Mitelman, 1995 15 March 2018 Page 32
Prognostic Impact of Diagnostic Karyotypes in Pediatric ALL Event Free Survival (%) Karyotype 2 yrs 5 yrs >50 chromosomes 90 80 47 -50 chromosomes 70 60 Normal karyotype 70 60 t(1; 19)(q 23; p 13) 50 40 t(9; 22)(q 34; q 11. 2) 40 30 t(8; 14)(q 24; q 32) 40 30 11 q 23 abnormalities 30 20 Hypodiploid (<46) 30 20 t(4; 11)(q 21; q 23) 20 20 Heim and Mitelman, 1995 15 March 2018 Page 32
 Cytogenetics: Mature B- and T-Cell Lympoma
Cytogenetics: Mature B- and T-Cell Lympoma
 Chromosome Translocations: Lymphocyte Development • Translocations are considered to arise as errors during intragenic physiologic rearrangements that assemble productive copies of IG and TCR genes during normal Band T-cell development • Translocations tend to be specific for breakpoints and show a high degree of association with histologic subsets • Three Main Subsets of NHLs: -- B-Cell -- T-Cell/Natural Killer (NK) Cell -- Hodgkin’s Lymphoma (HL) • First description of karyotype in BL in 1963 (Jacobs et al. , 1963) • Identified as t(8; 14)(q 24; q 32) in 1972 (Manolov and Manolova, 1972) • t(8; 14) was shown that MYC rearranges with IGH (Dalla-Favera et al. , 1987) 15 March 2018 Page 34
Chromosome Translocations: Lymphocyte Development • Translocations are considered to arise as errors during intragenic physiologic rearrangements that assemble productive copies of IG and TCR genes during normal Band T-cell development • Translocations tend to be specific for breakpoints and show a high degree of association with histologic subsets • Three Main Subsets of NHLs: -- B-Cell -- T-Cell/Natural Killer (NK) Cell -- Hodgkin’s Lymphoma (HL) • First description of karyotype in BL in 1963 (Jacobs et al. , 1963) • Identified as t(8; 14)(q 24; q 32) in 1972 (Manolov and Manolova, 1972) • t(8; 14) was shown that MYC rearranges with IGH (Dalla-Favera et al. , 1987) 15 March 2018 Page 34
 Burkitt’s Lymphoma Primary Chromosome change: • --t(8; 14)(q 24; q 32) MYC/Ig. H • Variant translocations: • -- t(8; 22)(q 24; q 11) (MYC/Ig. L) • -- t(2; 8)(p 11; q 24) (Ig. K/MYC) • Duplication 1 q: progression 15 March 2018 Page 35
Burkitt’s Lymphoma Primary Chromosome change: • --t(8; 14)(q 24; q 32) MYC/Ig. H • Variant translocations: • -- t(8; 22)(q 24; q 11) (MYC/Ig. L) • -- t(2; 8)(p 11; q 24) (Ig. K/MYC) • Duplication 1 q: progression 15 March 2018 Page 35
 Follicular Lymphoma Primary Chromosome Change: t(14; 18)(q 32; q 21) (Ig. H/BCL 2)(>75%) variant translocations involving 18 q 21 break point (BCL 2) » 3 q 27 rearrangements (BCL 6) » 6 q 21 deletions t/der(1 q), +7, del(6 q), del(17 p): Progression/transformation t(14; 18) negative tumors do exist, which exhibit complex and heterogeneous breakpoints (3 q 27; 8 q 24, ect) 15 March 2018 Page 36
Follicular Lymphoma Primary Chromosome Change: t(14; 18)(q 32; q 21) (Ig. H/BCL 2)(>75%) variant translocations involving 18 q 21 break point (BCL 2) » 3 q 27 rearrangements (BCL 6) » 6 q 21 deletions t/der(1 q), +7, del(6 q), del(17 p): Progression/transformation t(14; 18) negative tumors do exist, which exhibit complex and heterogeneous breakpoints (3 q 27; 8 q 24, ect) 15 March 2018 Page 36
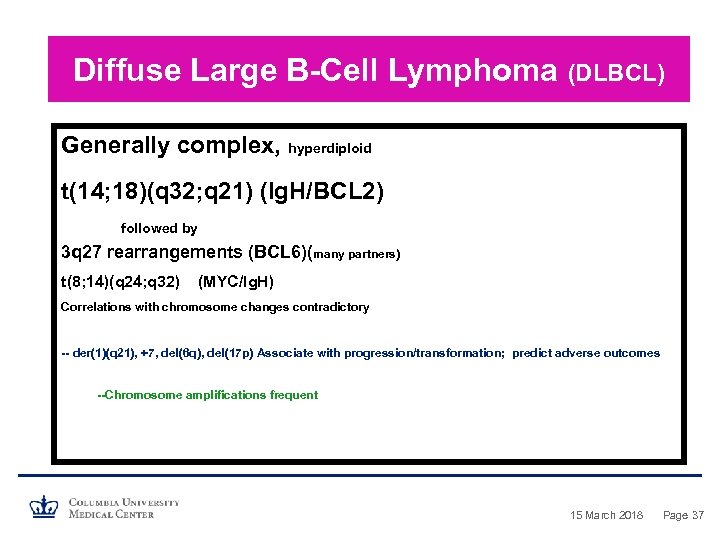 Diffuse Large B-Cell Lymphoma (DLBCL) Generally complex, hyperdiploid t(14; 18)(q 32; q 21) (Ig. H/BCL 2) followed by 3 q 27 rearrangements (BCL 6)(many partners) t(8; 14)(q 24; q 32) (MYC/Ig. H) Correlations with chromosome changes contradictory -- der(1)(q 21), +7, del(6 q), del(17 p) Associate with progression/transformation; predict adverse outcomes --Chromosome amplifications frequent 15 March 2018 Page 37
Diffuse Large B-Cell Lymphoma (DLBCL) Generally complex, hyperdiploid t(14; 18)(q 32; q 21) (Ig. H/BCL 2) followed by 3 q 27 rearrangements (BCL 6)(many partners) t(8; 14)(q 24; q 32) (MYC/Ig. H) Correlations with chromosome changes contradictory -- der(1)(q 21), +7, del(6 q), del(17 p) Associate with progression/transformation; predict adverse outcomes --Chromosome amplifications frequent 15 March 2018 Page 37
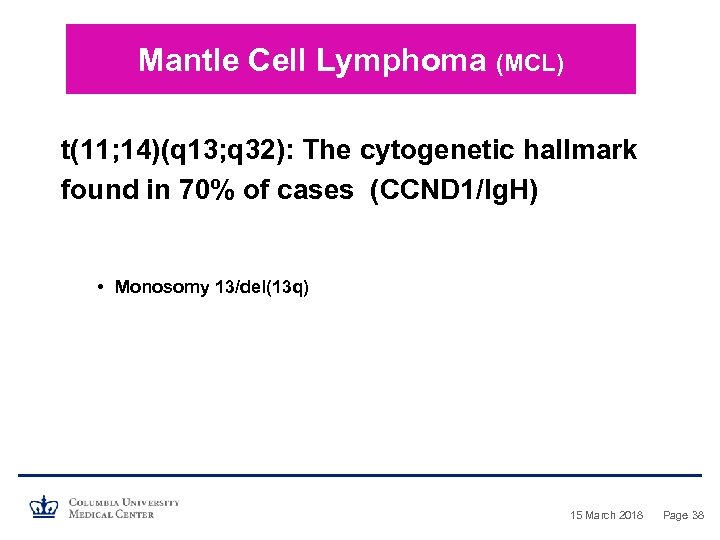 Mantle Cell Lymphoma (MCL) t(11; 14)(q 13; q 32): The cytogenetic hallmark found in 70% of cases (CCND 1/Ig. H) • Monosomy 13/del(13 q) 15 March 2018 Page 38
Mantle Cell Lymphoma (MCL) t(11; 14)(q 13; q 32): The cytogenetic hallmark found in 70% of cases (CCND 1/Ig. H) • Monosomy 13/del(13 q) 15 March 2018 Page 38
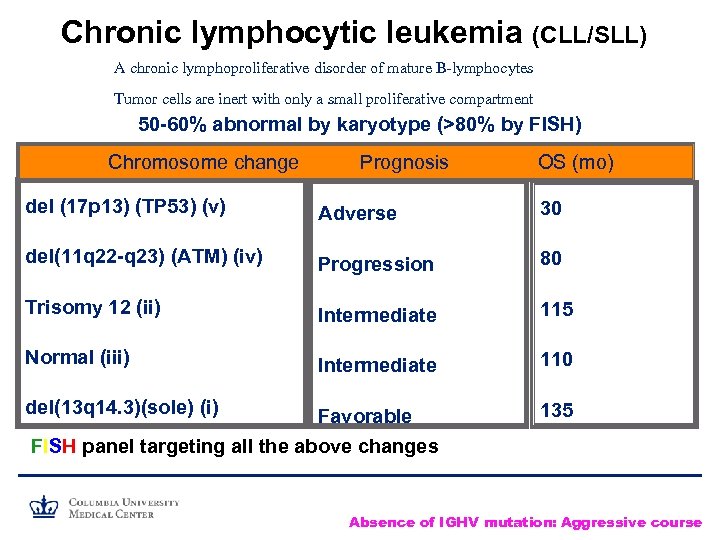 Chronic lymphocytic leukemia (CLL/SLL) A chronic lymphoproliferative disorder of mature B-lymphocytes Tumor cells are inert with only a small proliferative compartment 50 -60% abnormal by karyotype (>80% by FISH) Chromosome change Prognosis OS (mo) del (17 p 13) (TP 53) (v) Adverse 30 del(11 q 22 -q 23) (ATM) (iv) Progression 80 Trisomy 12 (ii) Intermediate 115 Normal (iii) Intermediate 110 del(13 q 14. 3)(sole) (i) Favorable 135 FISH panel targeting all the above changes Absence of IGHV mutation: Aggressive course
Chronic lymphocytic leukemia (CLL/SLL) A chronic lymphoproliferative disorder of mature B-lymphocytes Tumor cells are inert with only a small proliferative compartment 50 -60% abnormal by karyotype (>80% by FISH) Chromosome change Prognosis OS (mo) del (17 p 13) (TP 53) (v) Adverse 30 del(11 q 22 -q 23) (ATM) (iv) Progression 80 Trisomy 12 (ii) Intermediate 115 Normal (iii) Intermediate 110 del(13 q 14. 3)(sole) (i) Favorable 135 FISH panel targeting all the above changes Absence of IGHV mutation: Aggressive course
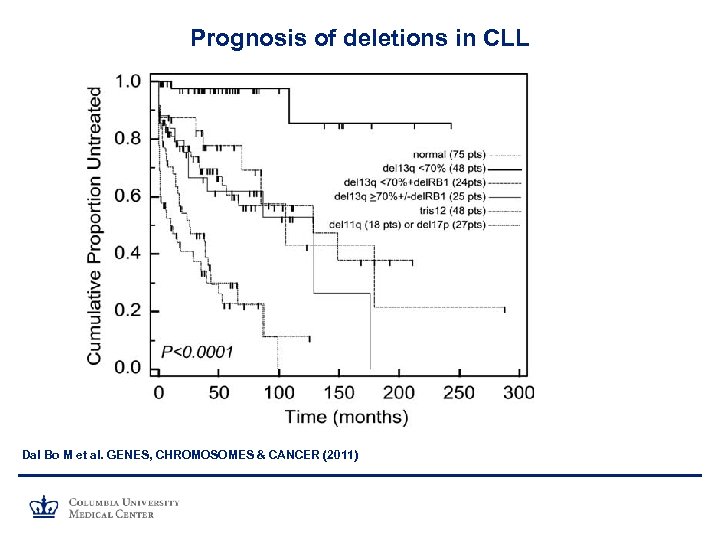 Prognosis of deletions in CLL Dal Bo M et al. GENES, CHROMOSOMES & CANCER (2011)
Prognosis of deletions in CLL Dal Bo M et al. GENES, CHROMOSOMES & CANCER (2011)
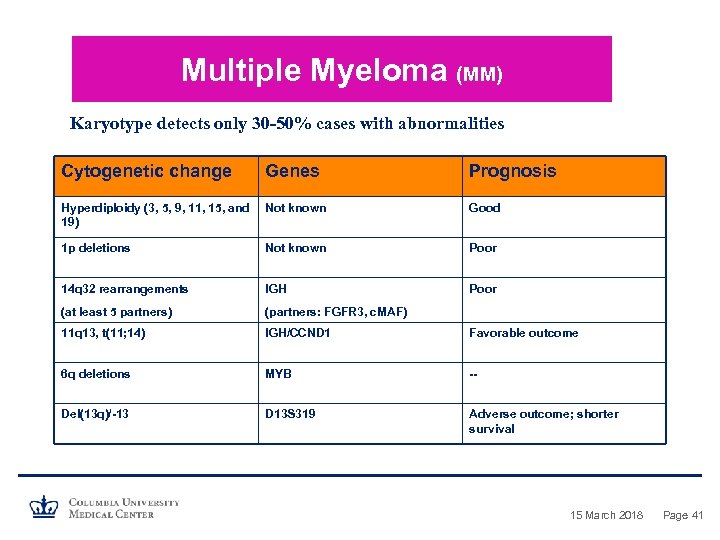 Multiple Myeloma (MM) Karyotype detects only 30 -50% cases with abnormalities Cytogenetic change Genes Prognosis Hyperdiploidy (3, 5, 9, 11, 15, and 19) Not known Good 1 p deletions Not known Poor 14 q 32 rearrangements IGH Poor (at least 5 partners) (partners: FGFR 3, c. MAF) 11 q 13, t(11; 14) IGH/CCND 1 Favorable outcome 6 q deletions MYB -- Del(13 q)/-13 D 13 S 319 Adverse outcome; shorter survival 15 March 2018 Page 41
Multiple Myeloma (MM) Karyotype detects only 30 -50% cases with abnormalities Cytogenetic change Genes Prognosis Hyperdiploidy (3, 5, 9, 11, 15, and 19) Not known Good 1 p deletions Not known Poor 14 q 32 rearrangements IGH Poor (at least 5 partners) (partners: FGFR 3, c. MAF) 11 q 13, t(11; 14) IGH/CCND 1 Favorable outcome 6 q deletions MYB -- Del(13 q)/-13 D 13 S 319 Adverse outcome; shorter survival 15 March 2018 Page 41
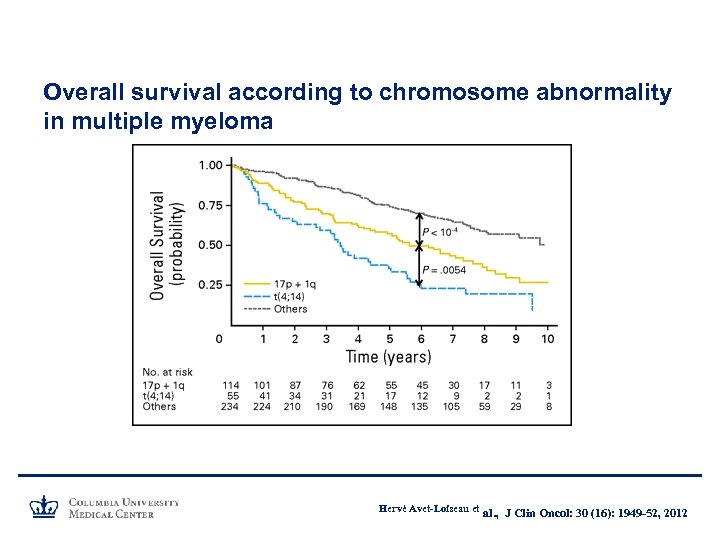 Overall survival according to chromosome abnormality in multiple myeloma Hervé Avet-Loiseau et al. , J Clin Oncol: 30 (16): 1949 -52, 2012
Overall survival according to chromosome abnormality in multiple myeloma Hervé Avet-Loiseau et al. , J Clin Oncol: 30 (16): 1949 -52, 2012
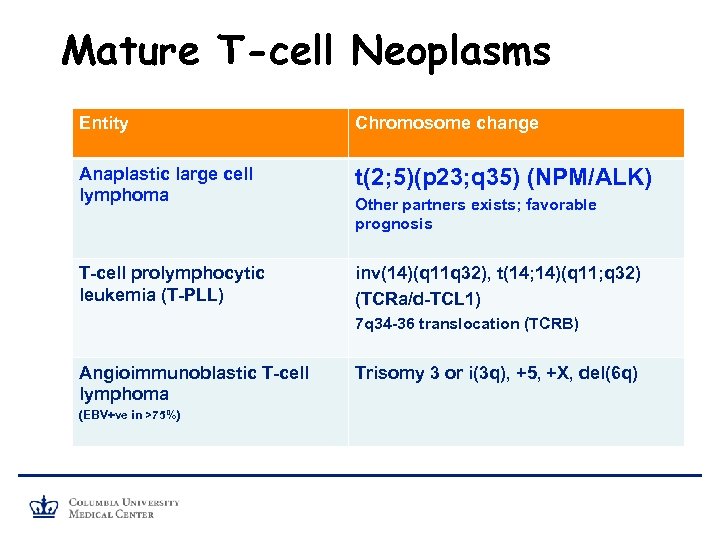 Mature T-cell Neoplasms Entity Chromosome change Anaplastic large cell lymphoma t(2; 5)(p 23; q 35) (NPM/ALK) T-cell prolymphocytic leukemia (T-PLL) inv(14)(q 11 q 32), t(14; 14)(q 11; q 32) (TCRa/d-TCL 1) Other partners exists; favorable prognosis 7 q 34 -36 translocation (TCRB) Angioimmunoblastic T-cell lymphoma (EBV+ve in >75%) Trisomy 3 or i(3 q), +5, +X, del(6 q)
Mature T-cell Neoplasms Entity Chromosome change Anaplastic large cell lymphoma t(2; 5)(p 23; q 35) (NPM/ALK) T-cell prolymphocytic leukemia (T-PLL) inv(14)(q 11 q 32), t(14; 14)(q 11; q 32) (TCRa/d-TCL 1) Other partners exists; favorable prognosis 7 q 34 -36 translocation (TCRB) Angioimmunoblastic T-cell lymphoma (EBV+ve in >75%) Trisomy 3 or i(3 q), +5, +X, del(6 q)
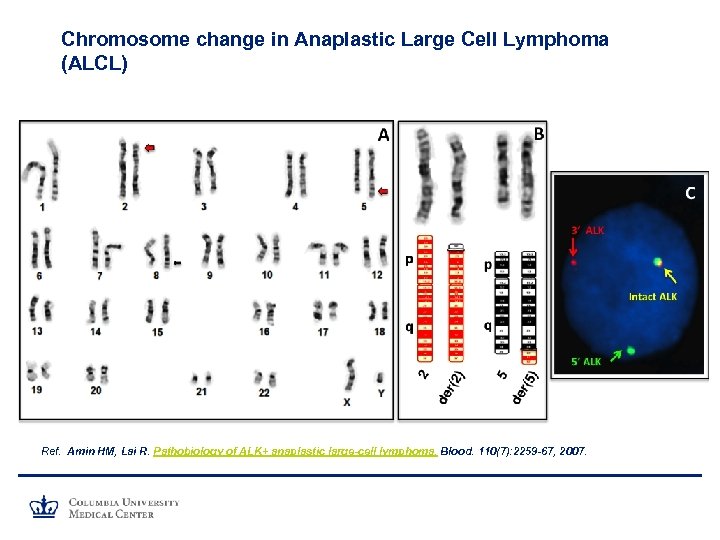 Chromosome change in Anaplastic Large Cell Lymphoma (ALCL) Ref. Amin HM, Lai R. Pathobiology of ALK+ anaplastic large-cell lymphoma. Blood. 110(7): 2259 -67, 2007.
Chromosome change in Anaplastic Large Cell Lymphoma (ALCL) Ref. Amin HM, Lai R. Pathobiology of ALK+ anaplastic large-cell lymphoma. Blood. 110(7): 2259 -67, 2007.
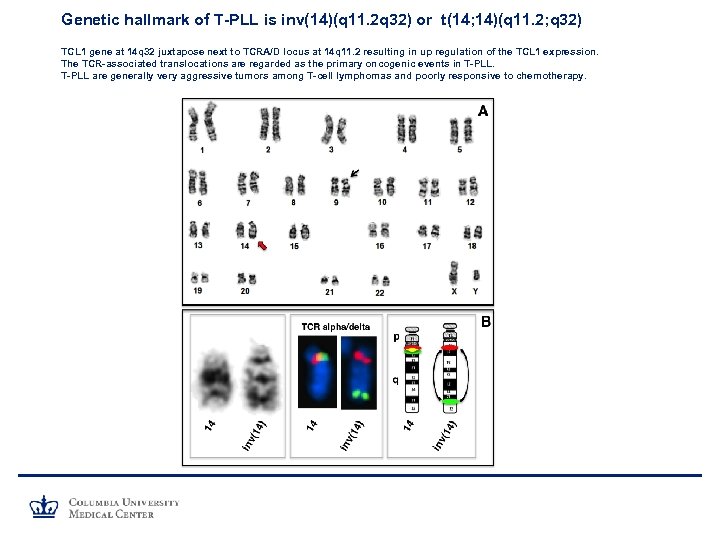 Genetic hallmark of T-PLL is inv(14)(q 11. 2 q 32) or t(14; 14)(q 11. 2; q 32) TCL 1 gene at 14 q 32 juxtapose next to TCRA/D locus at 14 q 11. 2 resulting in up regulation of the TCL 1 expression. The TCR-associated translocations are regarded as the primary oncogenic events in T-PLL are generally very aggressive tumors among T-cell lymphomas and poorly responsive to chemotherapy.
Genetic hallmark of T-PLL is inv(14)(q 11. 2 q 32) or t(14; 14)(q 11. 2; q 32) TCL 1 gene at 14 q 32 juxtapose next to TCRA/D locus at 14 q 11. 2 resulting in up regulation of the TCL 1 expression. The TCR-associated translocations are regarded as the primary oncogenic events in T-PLL are generally very aggressive tumors among T-cell lymphomas and poorly responsive to chemotherapy.
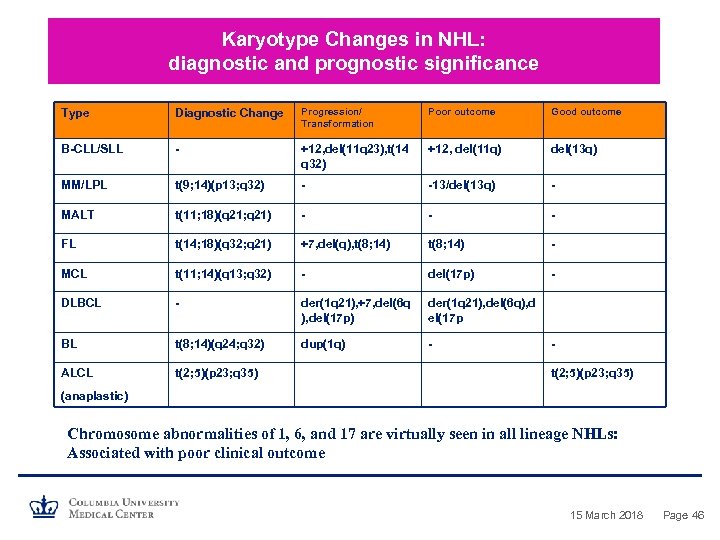 Karyotype Changes in NHL: diagnostic and prognostic significance Type Diagnostic Change Progression/ Transformation Poor outcome Good outcome B-CLL/SLL - +12, del(11 q 23), t(14 q 32) +12, del(11 q) del(13 q) MM/LPL t(9; 14)(p 13; q 32) - -13/del(13 q) - MALT t(11; 18)(q 21; q 21) - - - FL t(14; 18)(q 32; q 21) +7, del(q), t(8; 14) - MCL t(11; 14)(q 13; q 32) - del(17 p) - DLBCL - der(1 q 21), +7, del(6 q ), del(17 p) der(1 q 21), del(6 q), d el(17 p BL t(8; 14)(q 24; q 32) dup(1 q) - ALCL t(2; 5)(p 23; q 35) (anaplastic) Chromosome abnormalities of 1, 6, and 17 are virtually seen in all lineage NHLs: Associated with poor clinical outcome 15 March 2018 Page 46
Karyotype Changes in NHL: diagnostic and prognostic significance Type Diagnostic Change Progression/ Transformation Poor outcome Good outcome B-CLL/SLL - +12, del(11 q 23), t(14 q 32) +12, del(11 q) del(13 q) MM/LPL t(9; 14)(p 13; q 32) - -13/del(13 q) - MALT t(11; 18)(q 21; q 21) - - - FL t(14; 18)(q 32; q 21) +7, del(q), t(8; 14) - MCL t(11; 14)(q 13; q 32) - del(17 p) - DLBCL - der(1 q 21), +7, del(6 q ), del(17 p) der(1 q 21), del(6 q), d el(17 p BL t(8; 14)(q 24; q 32) dup(1 q) - ALCL t(2; 5)(p 23; q 35) (anaplastic) Chromosome abnormalities of 1, 6, and 17 are virtually seen in all lineage NHLs: Associated with poor clinical outcome 15 March 2018 Page 46
 Solid Tumor Cytogenetics
Solid Tumor Cytogenetics
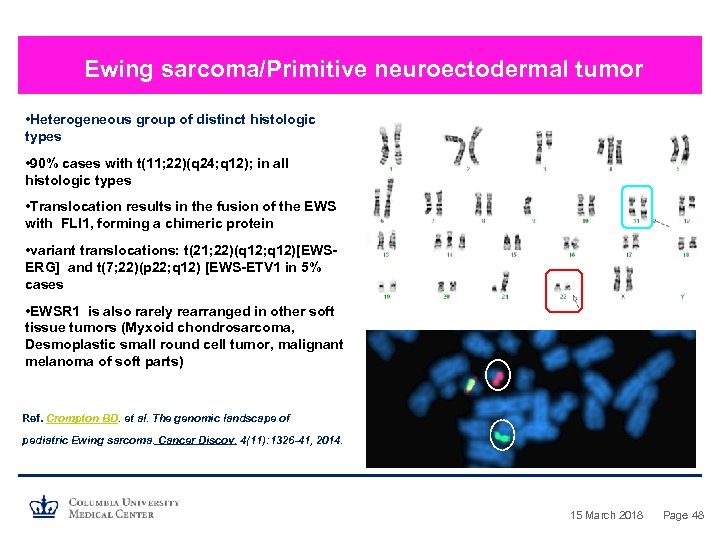 Ewing sarcoma/Primitive neuroectodermal tumor • Heterogeneous group of distinct histologic types • 90% cases with t(11; 22)(q 24; q 12); in all histologic types • Translocation results in the fusion of the EWS with FLI 1, forming a chimeric protein • variant translocations: t(21; 22)(q 12; q 12)[EWSERG] and t(7; 22)(p 22; q 12) [EWS-ETV 1 in 5% cases • EWSR 1 is also rarely rearranged in other soft tissue tumors (Myxoid chondrosarcoma, Desmoplastic small round cell tumor, malignant melanoma of soft parts) Ref. Crompton BD. et al. The genomic landscape of pediatric Ewing sarcoma. Cancer Discov. 4(11): 1326 -41, 2014. 15 March 2018 Page 48
Ewing sarcoma/Primitive neuroectodermal tumor • Heterogeneous group of distinct histologic types • 90% cases with t(11; 22)(q 24; q 12); in all histologic types • Translocation results in the fusion of the EWS with FLI 1, forming a chimeric protein • variant translocations: t(21; 22)(q 12; q 12)[EWSERG] and t(7; 22)(p 22; q 12) [EWS-ETV 1 in 5% cases • EWSR 1 is also rarely rearranged in other soft tissue tumors (Myxoid chondrosarcoma, Desmoplastic small round cell tumor, malignant melanoma of soft parts) Ref. Crompton BD. et al. The genomic landscape of pediatric Ewing sarcoma. Cancer Discov. 4(11): 1326 -41, 2014. 15 March 2018 Page 48
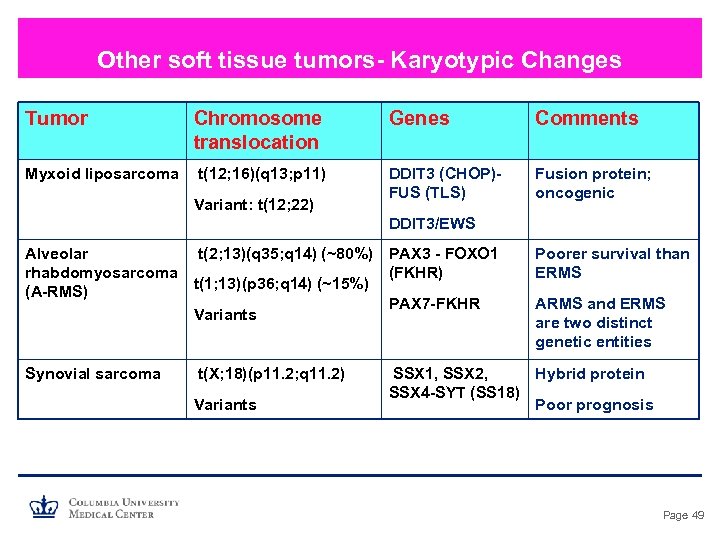 Other soft tissue tumors- Karyotypic Changes Tumor Chromosome translocation Myxoid liposarcoma t(12; 16)(q 13; p 11) Variant: t(12; 22) Genes Comments DDIT 3 (CHOP)FUS (TLS) Fusion protein; oncogenic DDIT 3/EWS Alveolar t(2; 13)(q 35; q 14) (~80%) PAX 3 - FOXO 1 rhabdomyosarcoma (FKHR) t(1; 13)(p 36; q 14) (~15%) (A-RMS) PAX 7 -FKHR Variants Synovial sarcoma t(X; 18)(p 11. 2; q 11. 2) Variants Poorer survival than ERMS ARMS and ERMS are two distinct genetic entities SSX 1, SSX 2, Hybrid protein SSX 4 -SYT (SS 18) Poor prognosis Page 49
Other soft tissue tumors- Karyotypic Changes Tumor Chromosome translocation Myxoid liposarcoma t(12; 16)(q 13; p 11) Variant: t(12; 22) Genes Comments DDIT 3 (CHOP)FUS (TLS) Fusion protein; oncogenic DDIT 3/EWS Alveolar t(2; 13)(q 35; q 14) (~80%) PAX 3 - FOXO 1 rhabdomyosarcoma (FKHR) t(1; 13)(p 36; q 14) (~15%) (A-RMS) PAX 7 -FKHR Variants Synovial sarcoma t(X; 18)(p 11. 2; q 11. 2) Variants Poorer survival than ERMS ARMS and ERMS are two distinct genetic entities SSX 1, SSX 2, Hybrid protein SSX 4 -SYT (SS 18) Poor prognosis Page 49
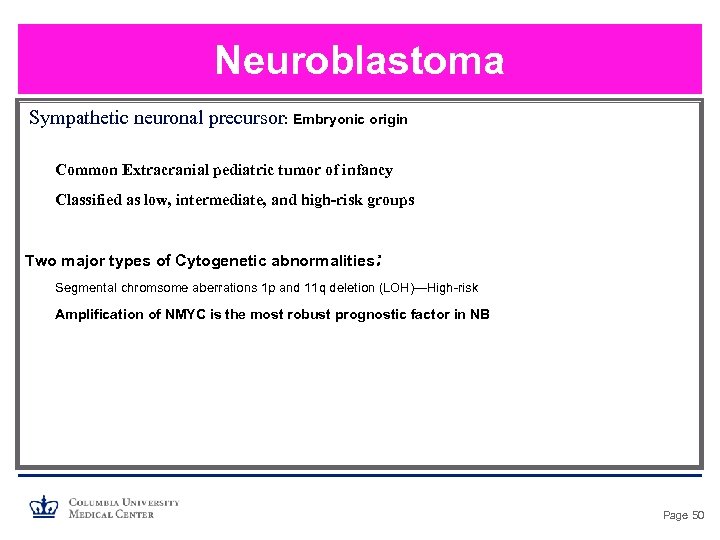 Neuroblastoma Sympathetic neuronal precursor: Embryonic origin Common Extracranial pediatric tumor of infancy Classified as low, intermediate, and high-risk groups Two major types of Cytogenetic abnormalities: Segmental chromsome aberrations 1 p and 11 q deletion (LOH)—High-risk Amplification of NMYC is the most robust prognostic factor in NB Page 50
Neuroblastoma Sympathetic neuronal precursor: Embryonic origin Common Extracranial pediatric tumor of infancy Classified as low, intermediate, and high-risk groups Two major types of Cytogenetic abnormalities: Segmental chromsome aberrations 1 p and 11 q deletion (LOH)—High-risk Amplification of NMYC is the most robust prognostic factor in NB Page 50
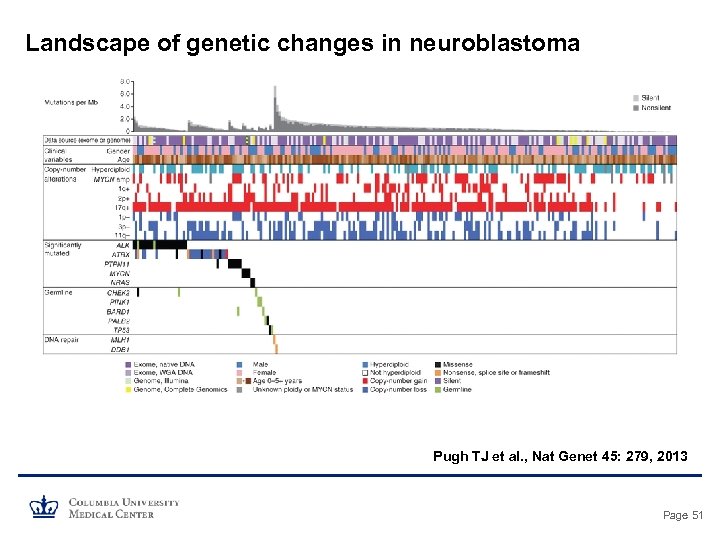 Landscape of genetic changes in neuroblastoma Pugh TJ et al. , Nat Genet 45: 279, 2013 Page 51
Landscape of genetic changes in neuroblastoma Pugh TJ et al. , Nat Genet 45: 279, 2013 Page 51
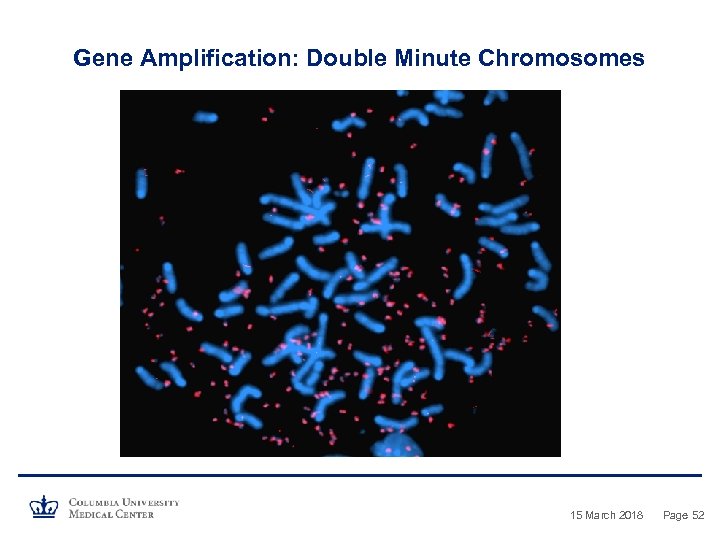 Gene Amplification: Double Minute Chromosomes 15 March 2018 Page 52
Gene Amplification: Double Minute Chromosomes 15 March 2018 Page 52
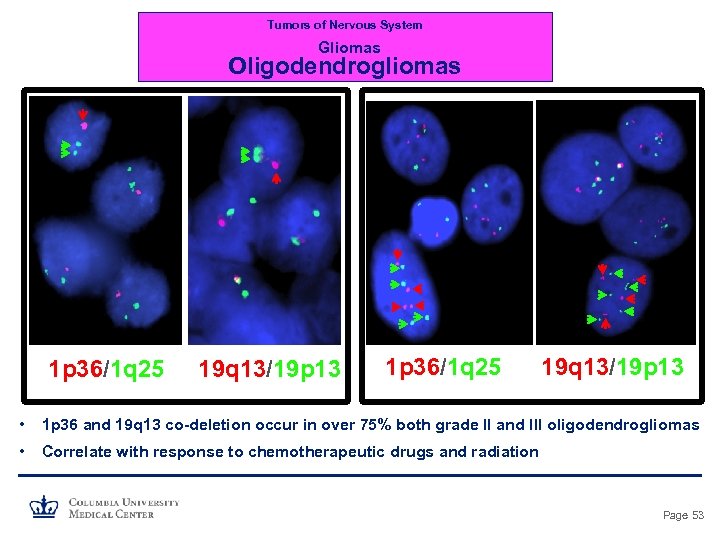 Tumors of Nervous System Gliomas Oligodendrogliomas 1 p 36/1 q 25 19 q 13/19 p 13 • 1 p 36 and 19 q 13 co-deletion occur in over 75% both grade II and III oligodendrogliomas • Correlate with response to chemotherapeutic drugs and radiation Page 53
Tumors of Nervous System Gliomas Oligodendrogliomas 1 p 36/1 q 25 19 q 13/19 p 13 • 1 p 36 and 19 q 13 co-deletion occur in over 75% both grade II and III oligodendrogliomas • Correlate with response to chemotherapeutic drugs and radiation Page 53
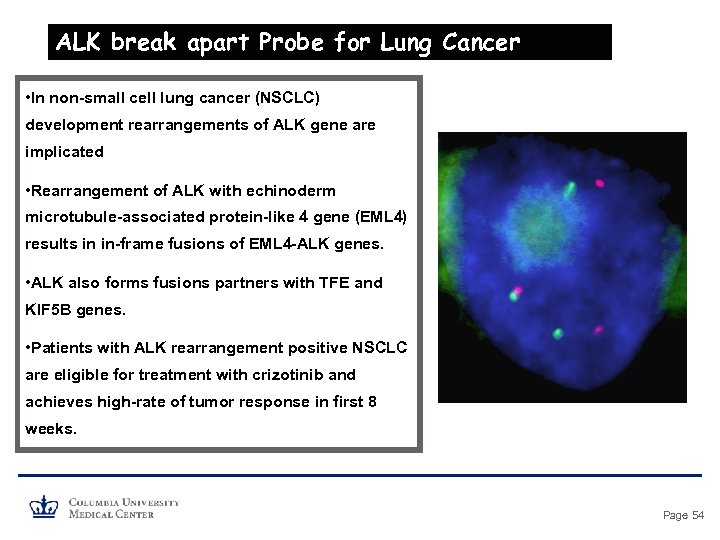 ALK break apart Probe for Lung Cancer • In non-small cell lung cancer (NSCLC) development rearrangements of ALK gene are implicated • Rearrangement of ALK with echinoderm microtubule-associated protein-like 4 gene (EML 4) results in in-frame fusions of EML 4 -ALK genes. • ALK also forms fusions partners with TFE and KIF 5 B genes. • Patients with ALK rearrangement positive NSCLC are eligible for treatment with crizotinib and achieves high-rate of tumor response in first 8 weeks. Page 54
ALK break apart Probe for Lung Cancer • In non-small cell lung cancer (NSCLC) development rearrangements of ALK gene are implicated • Rearrangement of ALK with echinoderm microtubule-associated protein-like 4 gene (EML 4) results in in-frame fusions of EML 4 -ALK genes. • ALK also forms fusions partners with TFE and KIF 5 B genes. • Patients with ALK rearrangement positive NSCLC are eligible for treatment with crizotinib and achieves high-rate of tumor response in first 8 weeks. Page 54
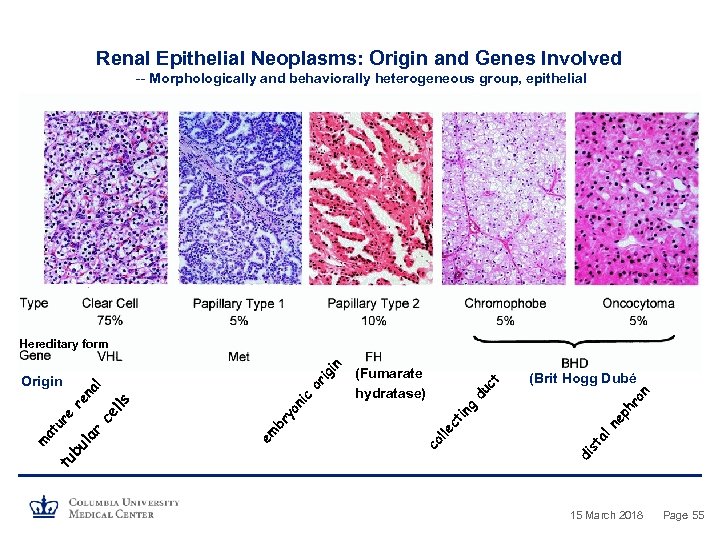 Renal Epithelial Neoplasms: Origin and Genes Involved -- Morphologically and behaviorally heterogeneous group, epithelial n ro t ne in ph g du c (Brit Hogg Dubé di st al ct lle c em br yo ni ls ce l (Fumarate hydratase) co or l na r la bu tu m at ur e re Origin ig in Hereditary form 15 March 2018 Page 55
Renal Epithelial Neoplasms: Origin and Genes Involved -- Morphologically and behaviorally heterogeneous group, epithelial n ro t ne in ph g du c (Brit Hogg Dubé di st al ct lle c em br yo ni ls ce l (Fumarate hydratase) co or l na r la bu tu m at ur e re Origin ig in Hereditary form 15 March 2018 Page 55
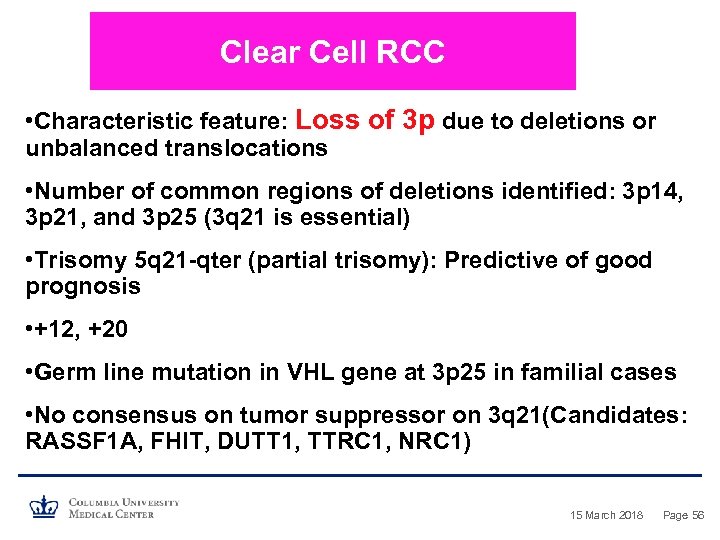 Clear Cell RCC • Characteristic feature: Loss of 3 p due to deletions or unbalanced translocations • Number of common regions of deletions identified: 3 p 14, 3 p 21, and 3 p 25 (3 q 21 is essential) • Trisomy 5 q 21 -qter (partial trisomy): Predictive of good prognosis • +12, +20 • Germ line mutation in VHL gene at 3 p 25 in familial cases • No consensus on tumor suppressor on 3 q 21(Candidates: RASSF 1 A, FHIT, DUTT 1, TTRC 1, NRC 1) 15 March 2018 Page 56
Clear Cell RCC • Characteristic feature: Loss of 3 p due to deletions or unbalanced translocations • Number of common regions of deletions identified: 3 p 14, 3 p 21, and 3 p 25 (3 q 21 is essential) • Trisomy 5 q 21 -qter (partial trisomy): Predictive of good prognosis • +12, +20 • Germ line mutation in VHL gene at 3 p 25 in familial cases • No consensus on tumor suppressor on 3 q 21(Candidates: RASSF 1 A, FHIT, DUTT 1, TTRC 1, NRC 1) 15 March 2018 Page 56
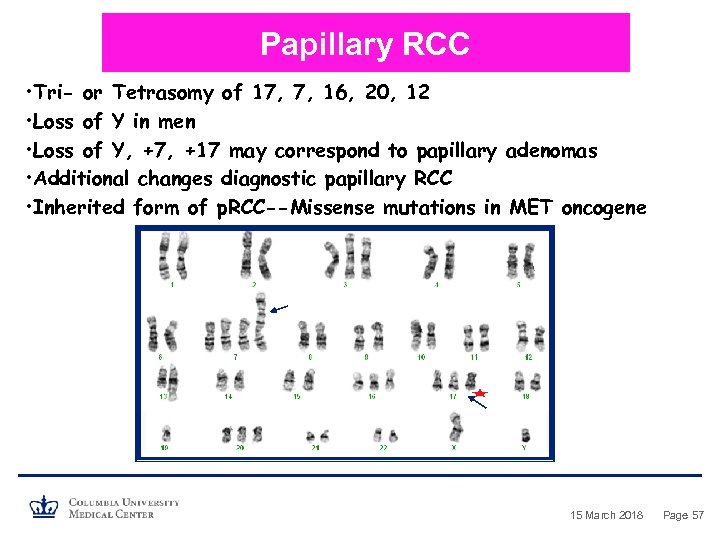 Papillary RCC • Tri- or Tetrasomy of 17, 7, 16, 20, 12 • Loss of Y in men • Loss of Y, +7, +17 may correspond to papillary adenomas • Additional changes diagnostic papillary RCC • Inherited form of p. RCC--Missense mutations in MET oncogene 15 March 2018 Page 57
Papillary RCC • Tri- or Tetrasomy of 17, 7, 16, 20, 12 • Loss of Y in men • Loss of Y, +7, +17 may correspond to papillary adenomas • Additional changes diagnostic papillary RCC • Inherited form of p. RCC--Missense mutations in MET oncogene 15 March 2018 Page 57
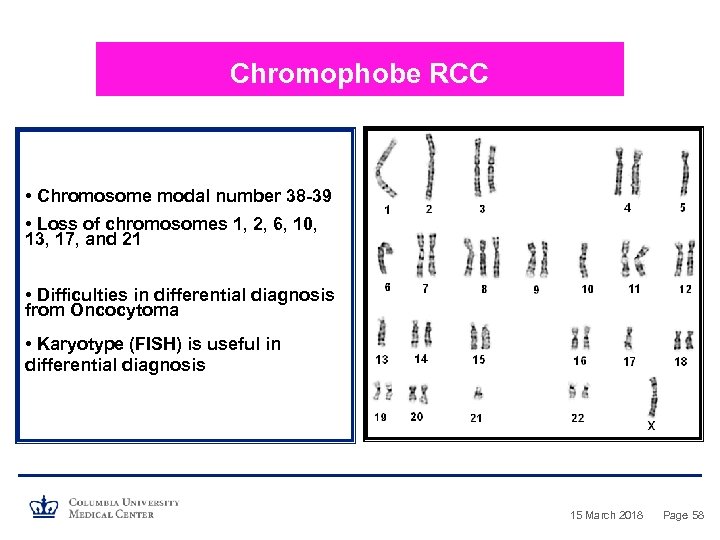 Chromophobe RCC • Chromosome modal number 38 -39 • Loss of chromosomes 1, 2, 6, 10, 13, 17, and 21 • Difficulties in differential diagnosis from Oncocytoma • Karyotype (FISH) is useful in differential diagnosis 15 March 2018 Page 58
Chromophobe RCC • Chromosome modal number 38 -39 • Loss of chromosomes 1, 2, 6, 10, 13, 17, and 21 • Difficulties in differential diagnosis from Oncocytoma • Karyotype (FISH) is useful in differential diagnosis 15 March 2018 Page 58
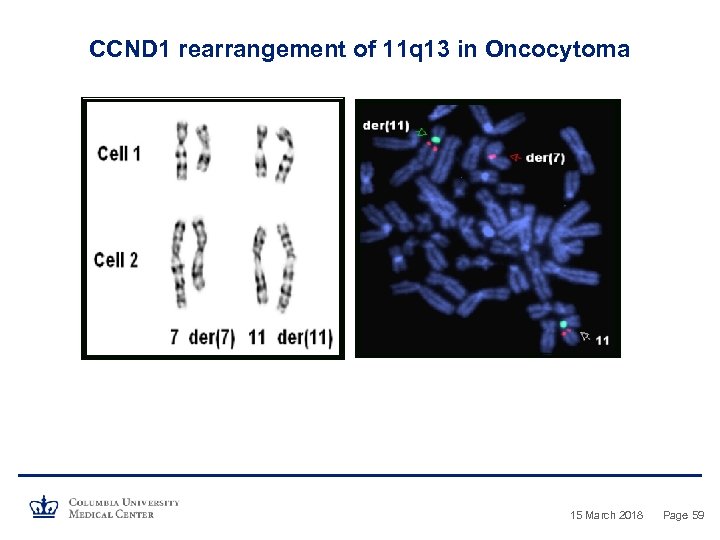 CCND 1 rearrangement of 11 q 13 in Oncocytoma 15 March 2018 Page 59
CCND 1 rearrangement of 11 q 13 in Oncocytoma 15 March 2018 Page 59
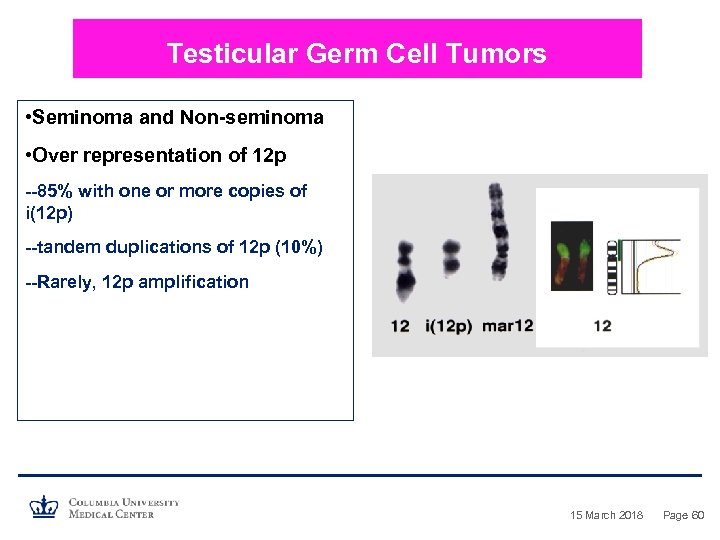 Testicular Germ Cell Tumors • Seminoma and Non-seminoma • Over representation of 12 p --85% with one or more copies of i(12 p) --tandem duplications of 12 p (10%) --Rarely, 12 p amplification 15 March 2018 Page 60
Testicular Germ Cell Tumors • Seminoma and Non-seminoma • Over representation of 12 p --85% with one or more copies of i(12 p) --tandem duplications of 12 p (10%) --Rarely, 12 p amplification 15 March 2018 Page 60
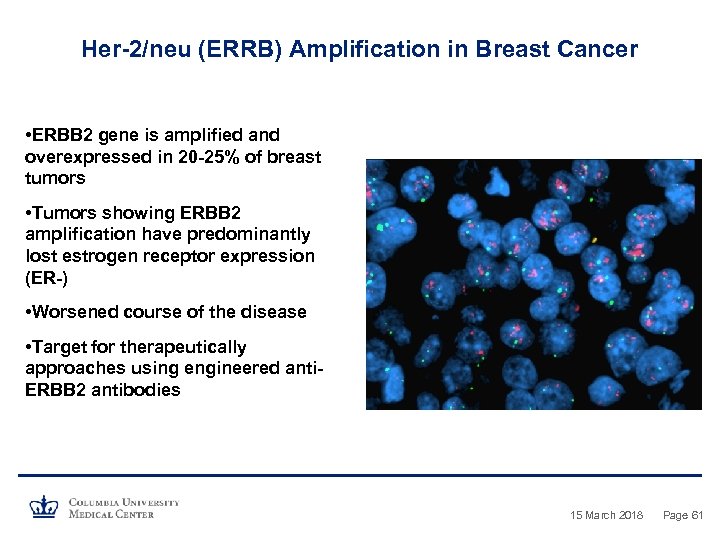 Her-2/neu (ERRB) Amplification in Breast Cancer • ERBB 2 gene is amplified and overexpressed in 20 -25% of breast tumors • Tumors showing ERBB 2 amplification have predominantly lost estrogen receptor expression (ER-) • Worsened course of the disease • Target for therapeutically approaches using engineered anti. ERBB 2 antibodies 15 March 2018 Page 61
Her-2/neu (ERRB) Amplification in Breast Cancer • ERBB 2 gene is amplified and overexpressed in 20 -25% of breast tumors • Tumors showing ERBB 2 amplification have predominantly lost estrogen receptor expression (ER-) • Worsened course of the disease • Target for therapeutically approaches using engineered anti. ERBB 2 antibodies 15 March 2018 Page 61
 Utilities of Tumor Cytogenetics • To Establish Malignant Clone (normal karyotype doesn’t rule out) • To Clarity/Establish Diagnosis • To Indicate Prognosis (some changes associated with poor response) • To Assist in Choice of Treatment Strategy • To Monitor Response to Treatment • To Establish Engraftment Status and Monitor Number of targeted therapies already exists against specific genetic changes that patient’s tumor uniquely possesses. 15 March 2018 Page 62
Utilities of Tumor Cytogenetics • To Establish Malignant Clone (normal karyotype doesn’t rule out) • To Clarity/Establish Diagnosis • To Indicate Prognosis (some changes associated with poor response) • To Assist in Choice of Treatment Strategy • To Monitor Response to Treatment • To Establish Engraftment Status and Monitor Number of targeted therapies already exists against specific genetic changes that patient’s tumor uniquely possesses. 15 March 2018 Page 62


