Tubulointerstitial Disorders.pptx
- Количество слайдов: 28
Tubulointerstitial Diseases Jennifer Anderson PA-C
The Goal of the Kidney • Key role - remove metabolic wastes from blood, maintain normal electrolyte and p. H blood composition – the kidneys produce erythropoietin • If renal function declines - urea, phosphate, creatinine, potassium accumulation, decreased RBC production
Nephron • Primary renal functional unit • About 1 million nephrons per kidney • Each nephron contains: – Glomerulus- filtering system • Proteins and large cells stay in the blood, fluid and small molecules are forced out into the tubule – Tubule- sends filtered blood back to the body and removes the waste
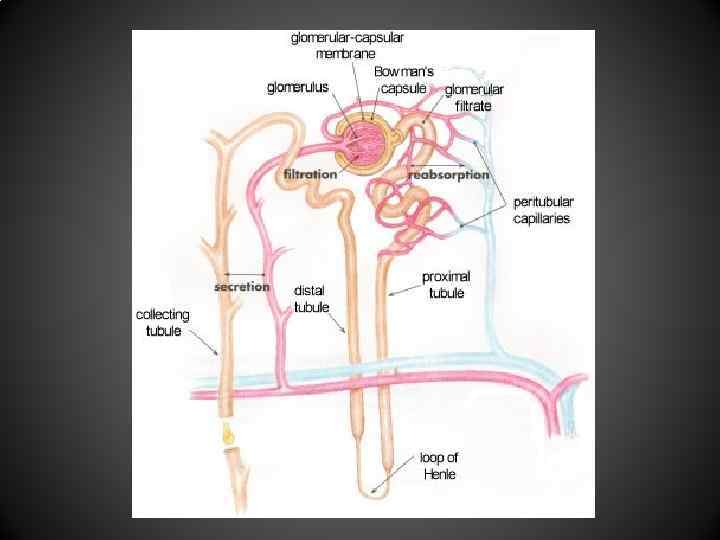
Renal Tubule • Receives the glomerular filtrate and reabsorbs or secretes substances based on the body’s needs • controlled by selective permeability of different areas of the tubule (H 2 O, Na, urea) and by response of distal tubule to hormones (aldosterone, antidiuretic & parathyroid hormones) • Then passes on to the collecting ducts for urine excretion
Renal Tubule • Reabsorption - movement of fluids & solutes from tubular lumen to peritubular capillary plasma (urine to blood) • Secretion - movements of substances from peritubular capillary plasma to tubular lumen (blood to urine)
Renal Disease Work-up • Duration of Disease – Acute Kidney Injury (aka acute renal failure) • Worsening of kidney function over hours to days • Retention of nitrogenous waste and creatinine – Called azotemia – Chronic Kidney Disease • Loss of kidney function over months to years
Acute Kidney Injury • AKA acute renal failure • Often reversible • Results in an inability to excrete nitrogenous wastes, maintain acid-base balance and fluid and electrolyte balance • Typically we look at serum Cr. – acutely elevated • Can also be determined by decreased urine output
AKI-Symptoms • Often none and highly dependent upon the cause of the renal insufficiency • Uremia (elevated urea) – nausea, vomiting, malaise and altered mental status • Altered volume status depending on the cause – Hypovolemia or hypervolemia and symptoms that would be associated with each • Electrolyte abnormalities
Acute Kidney Injury • Divided into three major categories of causes – Prerenal – Intrinsic – Postrenal • Today, we are discussing one type of intrinsic cause – Tubulointerstitial disorders
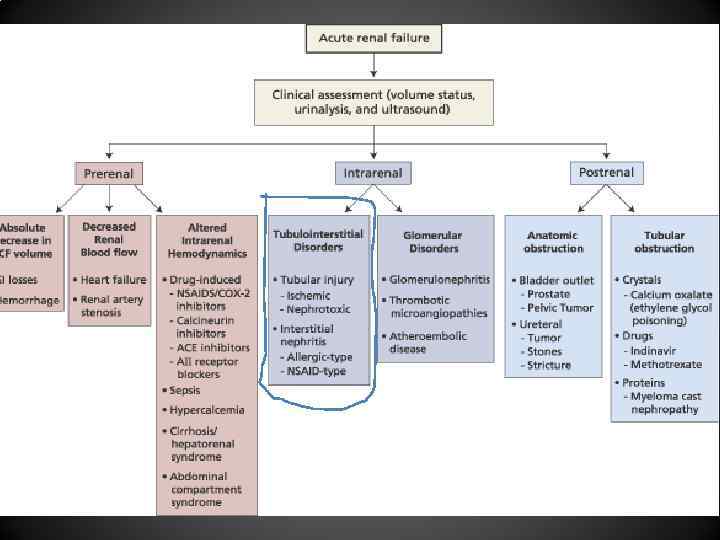
AKI - Intrinsic • Up to 50% of cases of AKI • Tubulointerstitial Disorders, vascular disorders and Glomerular disorders within the kidney • Considered after pre-renal and post-renal causes are ruled out
Acute Tubular Necrosis(ATN) • AKI due to tubular damage • 85% of intrinsic AKI’s • 2 causes – Ischemia – Nephrotoxin exposure
ATN • Progresses through 3 phases – Initiation • Acute increase in BUN and Cr with decreases in renal function – Maintenance • Sustained period of decreased renal function • Typically 1 -2 weeks – Recovery • Tubular function is restored • Often have an initial increase in urine volume (post-ATN diuresis) • BUN and Cr typically return to pre-ATN levels
Ischemic ATN • Prolonged low kidney perfusion causes ischemia and tubular damage • Occurs most commonly in hypotension – Volume depletion (oliguria) – Shock – Sepsis – Surgical procedures that involve long periods of hypoperfusion
Nephrotoxic ATN Caused by exposure to both exogenous nephrotoxins and endogenous nephrotoxins • Predisposing factors include underlying kidney damage, advanced age, volume depletion and exposure to concurrent nephrotoxic substances • Exogenous – Aminoglycosides and many other antibiotics – Radiographic contrast media (contrast nephropathy) • Endogenous – Heme, uric acid – Myoglobin from rhabdomyolysis – Multiple Myeloma (Bence Jones Proteins)
ATN • • Laboratory findings include: Elevated BUN and Cr Brown urine Muddy brown casts – Sloughed off dead cells block the tubules which contributes to the lack of filtration
ATN Treatment • Maintain Euvolemia • Careful with IVF – want to avoid volume overload because the kidney isn’t functioning well • Diuresis has been the mainstay of treatment in order to augment the kidney function. Effective? • Monitor electrolytes and make corrections as needed • Nutritional support • Dose all renally eliminated drugs appropriately based on the estimated degree of renal impairment • Temporary dialysis
ATN • Prognosis – outcome is better in nonoliguric cases • Most patients recover their renal function after days to weeks • Some cases of ATN can lead to permanent loss of function (CKD)
Acute Interstitial Nephritis • Interstitial (the spaces around the tubules) inflammatory response with edema and possible cellular damage • Cell-mediated immune reaction – Acute infiltration of the renal interstitium with eosinophils, plasma cells, t-lymphocytes and monocytes
Acute Interstitial Nephritis • Causes – Drugs (70% of cases) – hypersensitivity reaction • NSAIDS • ABX – PCN, cephalosporins, sulfa • Can be seen with almost all medications – Infectious diseases • Pyelonephritis, Strep, rocky mountain spotted fever, legionella, CMV – Autoimmune disorders – can cause this, but more commonly lead to glomerulonephritis • SLE, Sjogren syndrome, sarcoidosis
AIN • s/s include fever (80%), arthralgias and a possible transient maculopapular rash (20%) • If medication is the causes, usually occurs within 10 days of starting • Laboratory findings: – UA reveals pyuria (primarily eosinophils), WBC casts, proteinuria (<1 -2 g/day), elevated ESR
Acute Interstitial Nephritis • Treatment – prognosis overall good – Worse prognosis in pts. with prolonged oliguria and advanced age – can progress to chronic kidney disease or even ESRD – Supportive measures – Removal/treatment of causative agent – If persists, can try short course of corticosteroids
Chronic Tubulointerstitial Diseases • Chronic disease can be caused by the same things that cause acute disease (post ATN, autoimmune disorders) if the insult is not reversed in a timely fashion – Chronic insults lead to interstitial fibrosis and tubular atrophy • Acute is most commonly caused by drugs, chronic is most commonly caused by obstructive uropathy (prolonged obstruction of the urinary tract)
Additional Causes of Chronic Tubulointerstitial Disease – Obstructive uropathy – most common • Prostate disease • Ureteral calculus, cancer – Reflux nephropathy – congenital incompetence of the vesicoureteral sphincter. Urine passes retrograde from the bladder to the kidneys during urination – Analgesic nephropathy – NSAIDS (>1 gram/day x 3 years) – Heavy Metal Exposure – lead is filtered by the glomerulus and accumulates in the tubule • Welders, people who drink moonshine distilled in automobile radiators
Chronic Tubulointerstitial Diseases • Clinical findings – Polyuria – damaged tubules cannot concentrate urine – Sterile pyuria – Hyperkalemia – Proteinuria (<1 -2 g/day) – Broad waxy casts – Other findings based on the cause • Hydroureter or hydronephrosis in obstructive uropathy
Chronic Tubulointerstitial Diseases • Treatment: – Remove the offending agent (NSAIDS, heavy metals) – No antibiotics (inflammation not infection) – Chelation therapy if heavy metal related – Medical management • May need potassium and phosphorus restriction • Sodium, calcium, bicarbonate supplements – Relieve obstruction if present
Tubulointerstitial Disorders.pptx