tuber.pptx
- Количество слайдов: 58
TUBERCULOSIS Ø Tuberculosis is a common disease prevalent through out the world. ØIt is a chronic specific inflammatory infectious disease caused by Mycobacterium tuberculosis in humans. ØTuberculosis usually attacks the lungs but it can also affect any parts of the body. ØPhysicians in ancient Greece called this illness as “Phthisis” reflecting its wasting character. 1
ETIOLOGY OF TB • Myco. tuberculosis – most common cause • Other than tuberculosis- includes – M. avium intracellulare – M. kansasi – M. scrofulaceum – M. ulcerans – M. marinum – M. fortuitum – M. chelonei
SITES INVOLVED • PULMONARY TB- 85% of all TB cases • EXTRAPULMONARY SITES. » LYMPH NODE » GENITO-URINARY TRACT » BONES & JOINTS » MENINGES » INTESTINE » SKIN
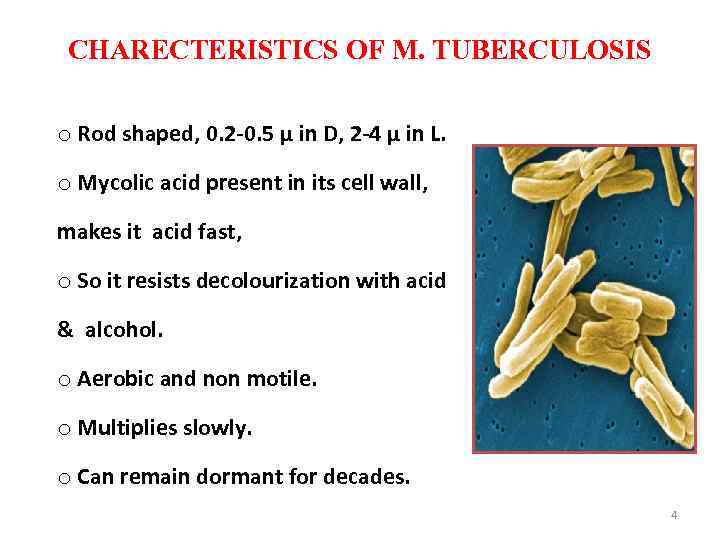
CHARECTERISTICS OF M. TUBERCULOSIS o Rod shaped, 0. 2 -0. 5 µ in D, 2 -4 µ in L. o Mycolic acid present in its cell wall, makes it acid fast, o So it resists decolourization with acid & alcohol. o Aerobic and non motile. o Multiplies slowly. o Can remain dormant for decades. 4
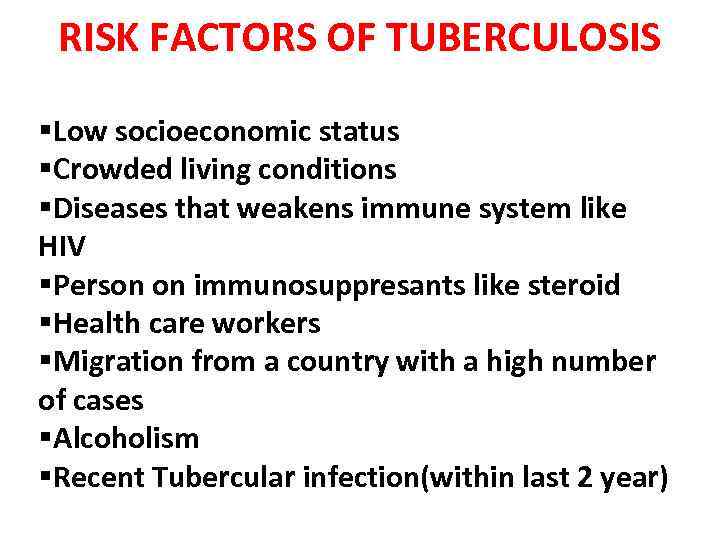
RISK FACTORS OF TUBERCULOSIS §Low socioeconomic status §Crowded living conditions §Diseases that weakens immune system like HIV §Person on immunosuppresants like steroid §Health care workers §Migration from a country with a high number of cases §Alcoholism §Recent Tubercular infection(within last 2 year)
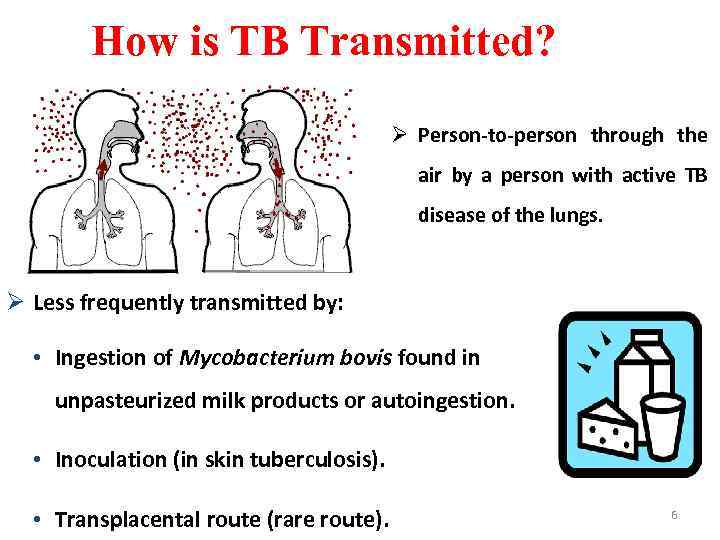
How is TB Transmitted? Ø Person-to-person through the air by a person with active TB disease of the lungs. Ø Less frequently transmitted by: • Ingestion of Mycobacterium bovis found in unpasteurized milk products or autoingestion. • Inoculation (in skin tuberculosis). • Transplacental route (rare route). 6
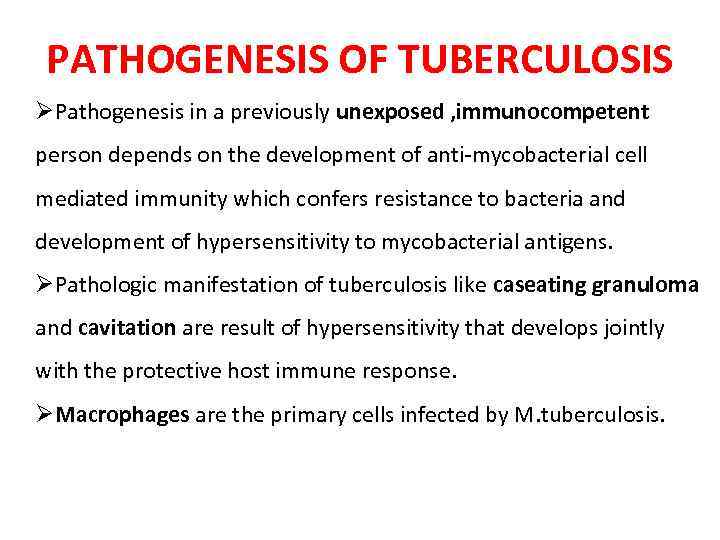
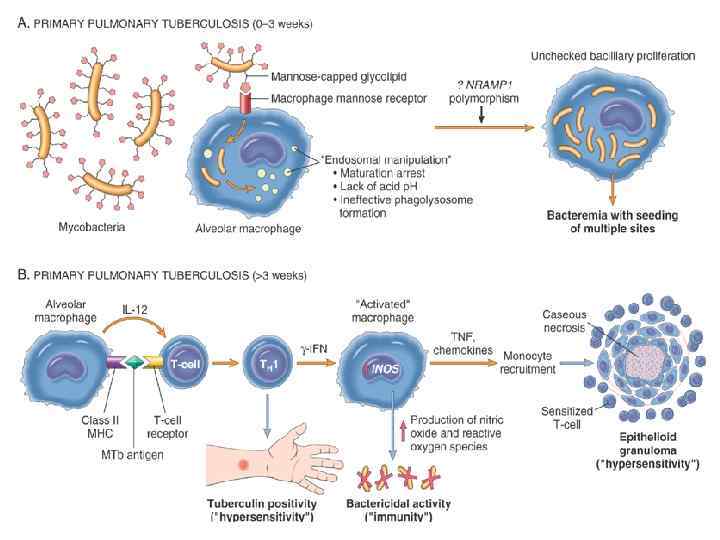
PATHOGENESIS OF TUBERCULOSIS ØPathogenesis in a previously unexposed , immunocompetent person depends on the development of anti-mycobacterial cell mediated immunity which confers resistance to bacteria and development of hypersensitivity to mycobacterial antigens. ØPathologic manifestation of tuberculosis like caseating granuloma and cavitation are result of hypersensitivity that develops jointly with the protective host immune response. ØMacrophages are the primary cells infected by M. tuberculosis.
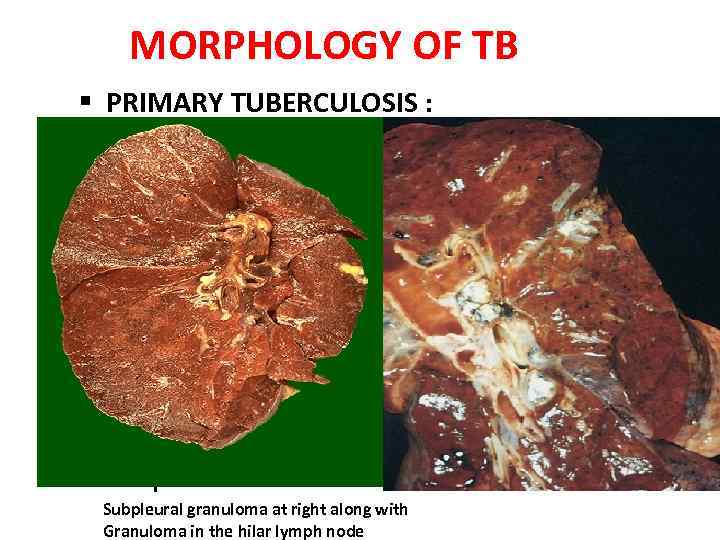
MORPHOLOGY OF TB § PRIMARY TUBERCULOSIS : • Form of disease that develops in a previously unexposed person. • Almost always begins in lungs. • Inhaled bacilli implant in the distal airspaces of lower part of upper lobe or upper part of lower lobe. • 1 -1. 5 cm area of grey white inflammation with consoldation develops, called as ghon focus which often caseates. • Tubercle bacilli drains to the regional lymph node which also often undergo caseous necrosis. • Parenchymal lung lesion + Nodal involvement= Ghon’s complex. Subpleural granuloma at right along with Granuloma in the hilar lymph node
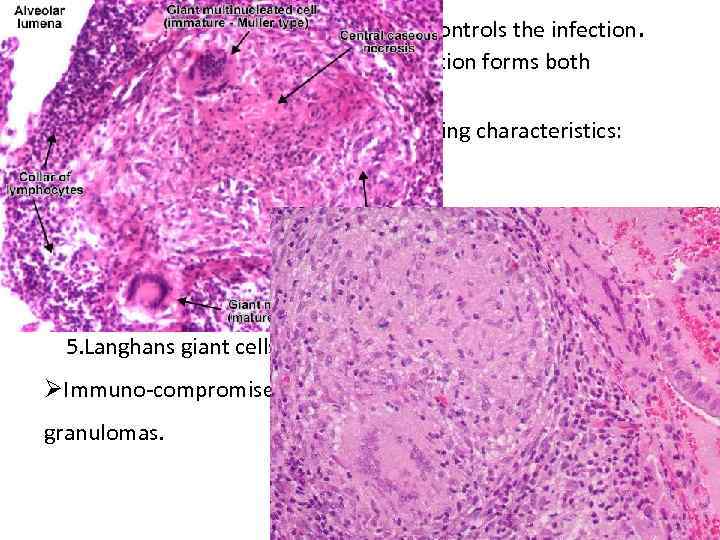
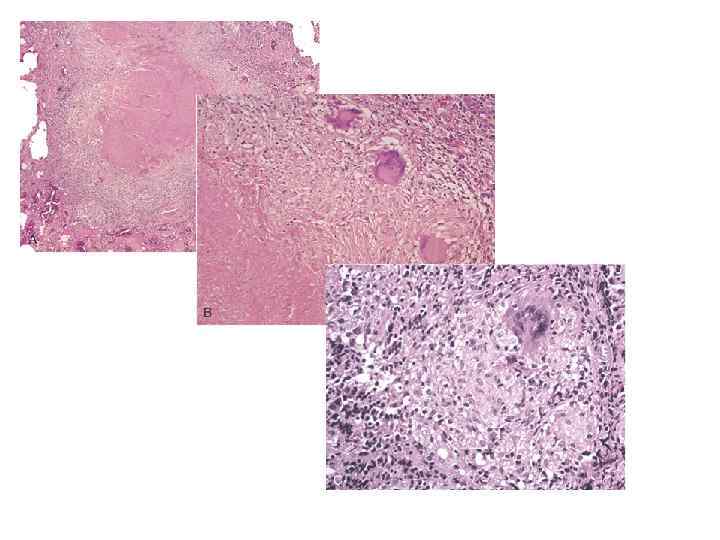
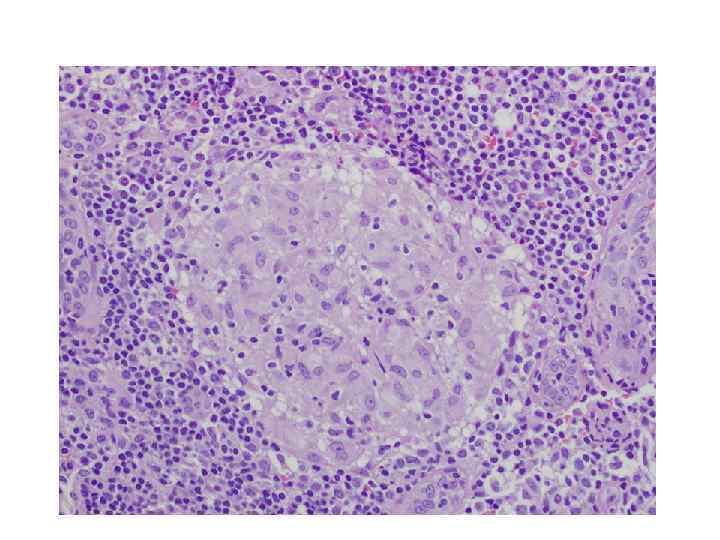
ØIn 95% cases cell mediated immunity controls the infection. Histologically: Granulomatous inflammation forms both caseating and non caseating tubercles. ØTuberculous Granuloma has the following characteristics: 1. Rounded outlines 2. Central caseous necrosis 3. Transformed macrophages called epithelioid cells 4. Lymphocytes, plasma cells, and fibroblasts 5. Langhans giant cells ØImmuno-compromised persons do not form the characteristic granulomas.
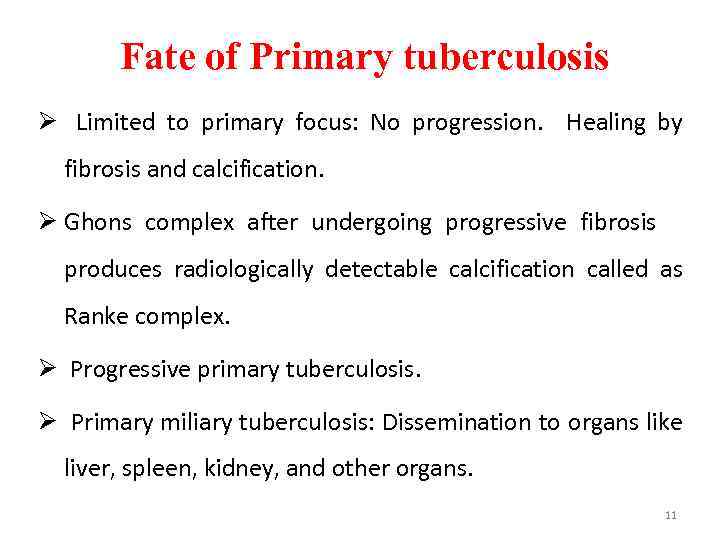
Fate of Primary tuberculosis Ø Limited to primary focus: No progression. Healing by fibrosis and calcification. Ø Ghons complex after undergoing progressive fibrosis produces radiologically detectable calcification called as Ranke complex. Ø Progressive primary tuberculosis. Ø Primary miliary tuberculosis: Dissemination to organs like liver, spleen, kidney, and other organs. 11
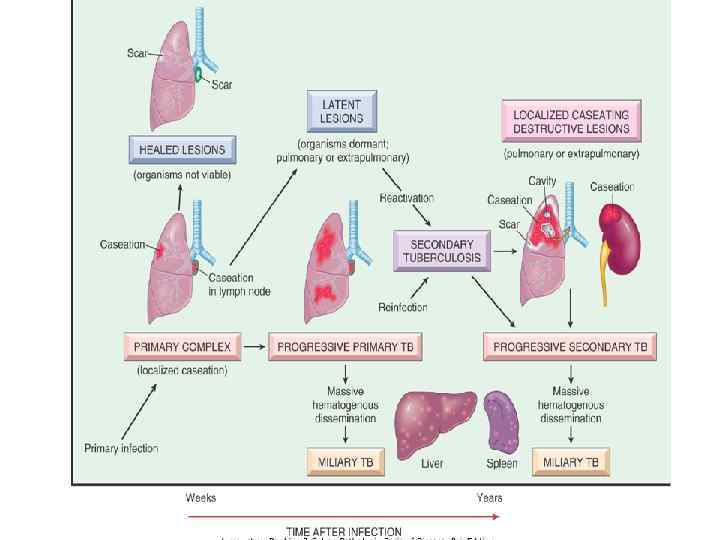
PROGRESSIVE PRIMARY TUBERCULOSIS • Occasional local progression, despite hypersensitivity (more common in younger patients). • can be cavitary. • can have endo-bronchial spread. • similar in appearance to adult type reactivation disease. • 2/3 rd of cases progress to death in the untreated condition.
SECONDARY PULMONARY TUBERCULOSIS Ø Infection of an individual who has been previously infected or sensitized is called Secondary or Post Primary tuberculosis. Ø It can be due to reactivation or reinfection. Ø Occurs most commonly in the apex region of the lung. Ø 1 - 2 cm area of consolidation of lung develops. Ø May in time develop a small area of central caseaous necrosis and peripheral fibrosis. Ø Occurs by hematogenous spread of infection from Primary Complex to the apex and other parts of the affected lung. 14
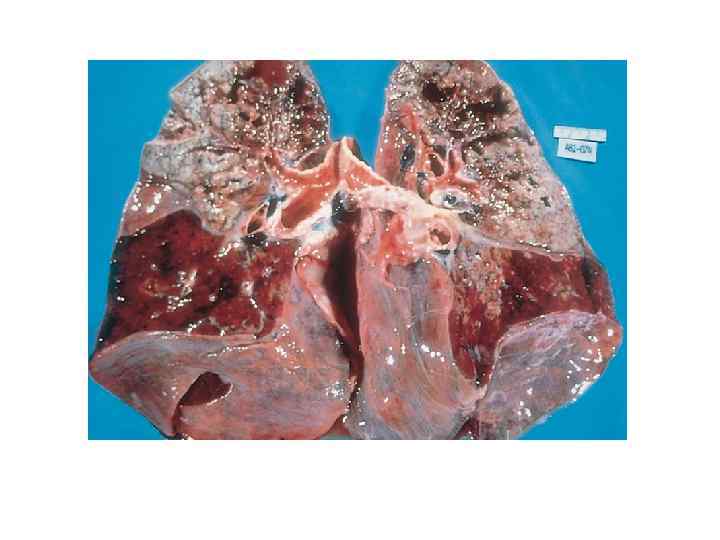
FATE OF SEC. PULMONARY TUBERCULOSIS 1 The lesion may heal with fibrous scarring and calcification. 2 The lesions may coalesce together to form large area of tuberculous pneumonia and produce progressive secondary pulmonary tuberculosis producing pulmonary & extra pulmonary lesions: Ø Tuberculous caseous pneumonia Ø Fibrocaseous tuberculosis Ø Miliary tuberculosis 15
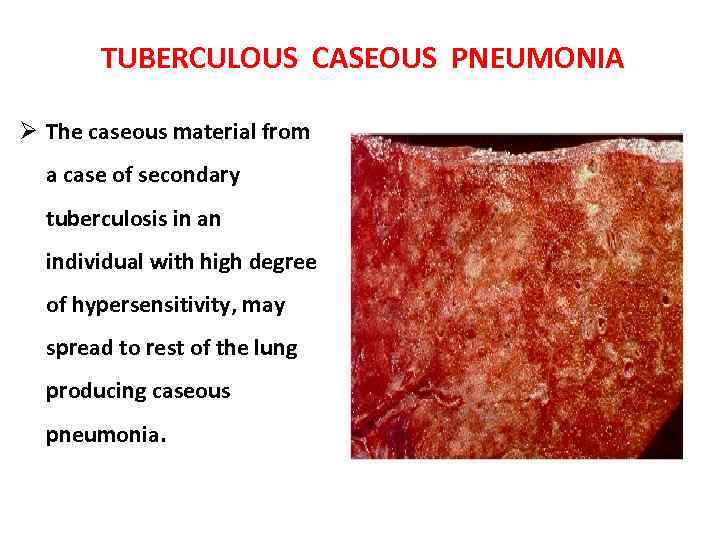
TUBERCULOUS CASEOUS PNEUMONIA Ø The caseous material from a case of secondary tuberculosis in an individual with high degree of hypersensitivity, may spread to rest of the lung producing caseous pneumonia. 16
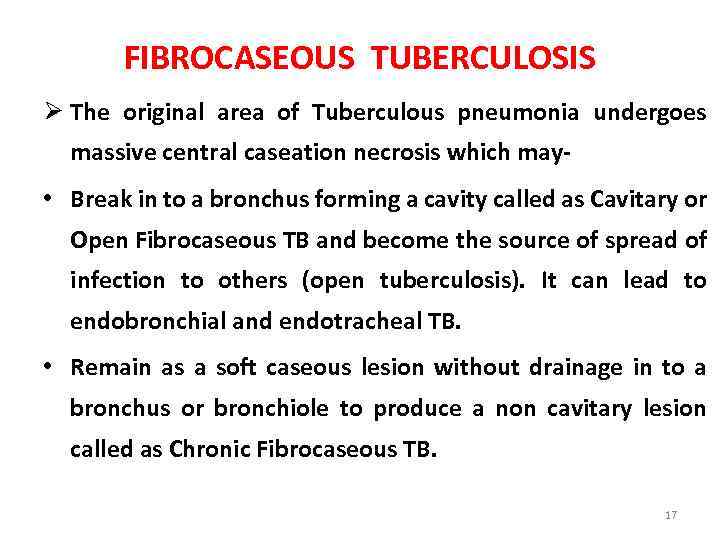
FIBROCASEOUS TUBERCULOSIS Ø The original area of Tuberculous pneumonia undergoes massive central caseation necrosis which may- • Break in to a bronchus forming a cavity called as Cavitary or Open Fibrocaseous TB and become the source of spread of infection to others (open tuberculosis). It can lead to endobronchial and endotracheal TB. • Remain as a soft caseous lesion without drainage in to a bronchus or bronchiole to produce a non cavitary lesion called as Chronic Fibrocaseous TB. 17
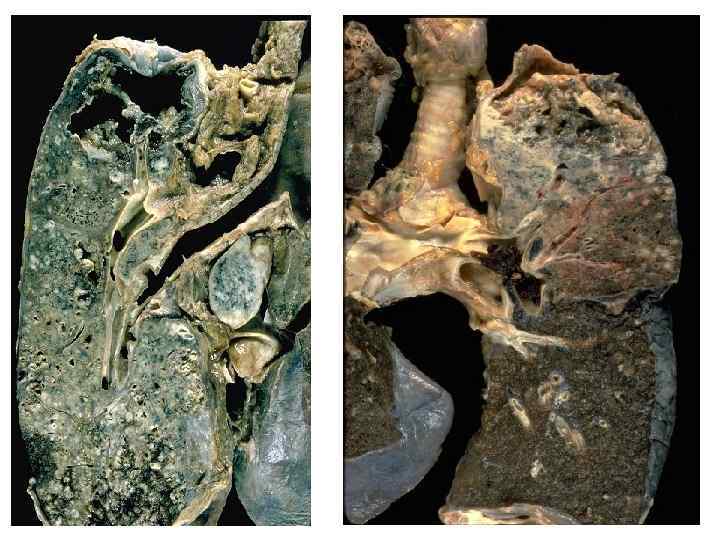
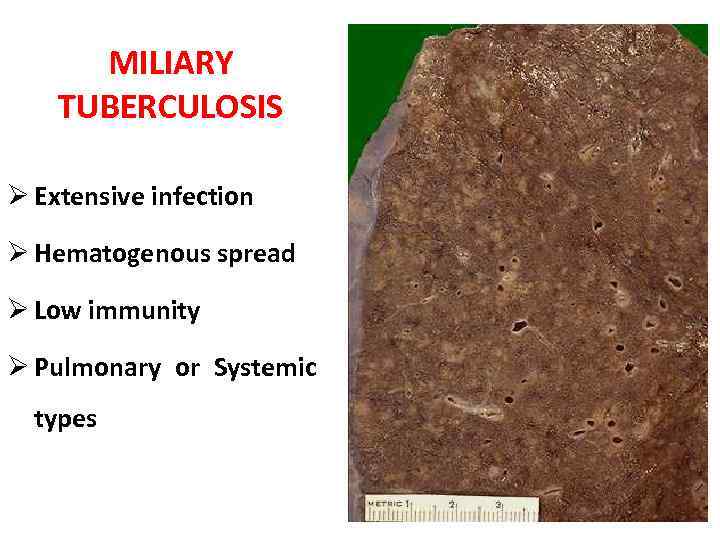
MILIARY TUBERCULOSIS Ø Extensive infection Ø Hematogenous spread Ø Low immunity Ø Pulmonary or Systemic types 19
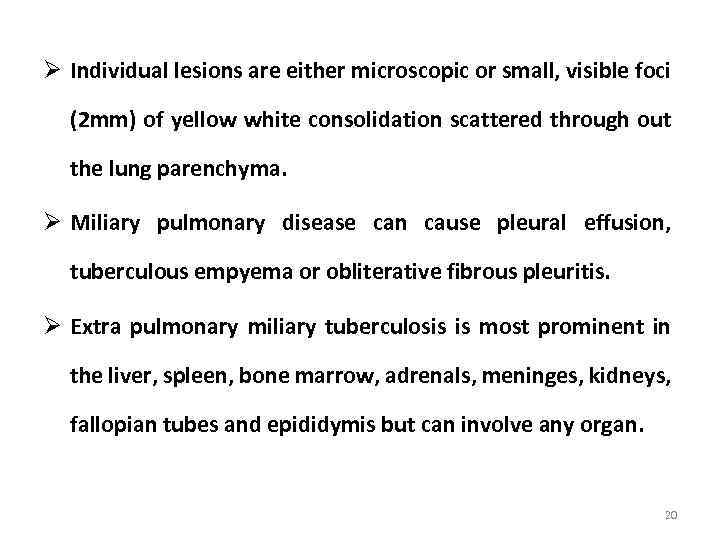
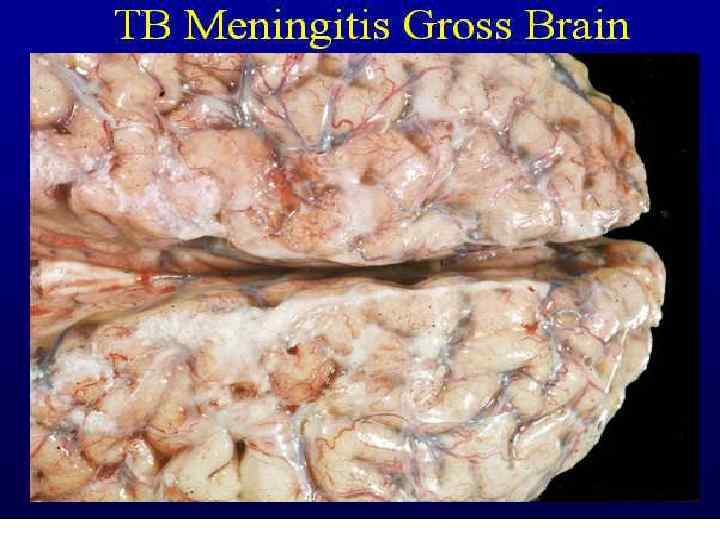
Ø Individual lesions are either microscopic or small, visible foci (2 mm) of yellow white consolidation scattered through out the lung parenchyma. Ø Miliary pulmonary disease can cause pleural effusion, tuberculous empyema or obliterative fibrous pleuritis. Ø Extra pulmonary miliary tuberculosis is most prominent in the liver, spleen, bone marrow, adrenals, meninges, kidneys, fallopian tubes and epididymis but can involve any organ. 20
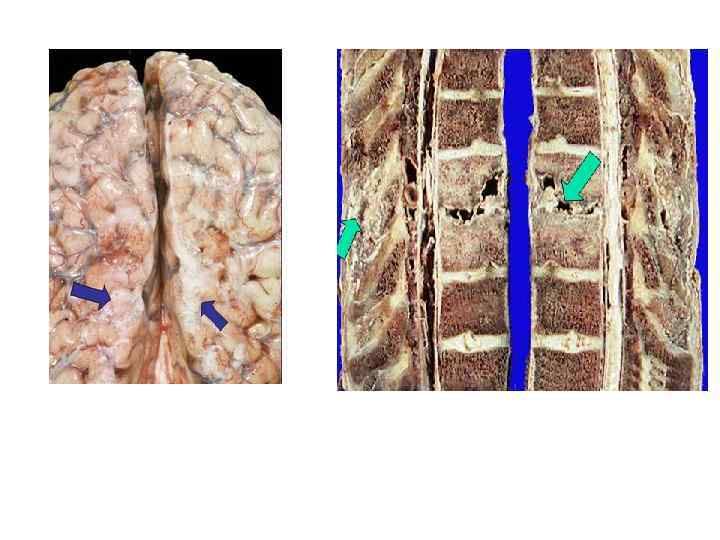
EXTRA PULMONARY TUBERCULOSIS Ø In tissues or organs seeded hematogenously. Ø Commonly involved organs include the : • Intestinal tuberculosis • Meninges (Tuberculous meningitis) • Kidneys (Renal tuberculosis) • Adrenals (Addison disease) • Bones (Osteomyelitis) • Vertebrae (Pott disease) • Fallopian tubes (Salpingitis) 21
INTESTINAL TUBERCULOSIS Occurs in three forms: 1. Primary intestinal tuberculosis : Used to occur by ingestion of unpasteurised cow’s milk infected with Mycobacterium bovis. But now a days most cases are due to M. tuberculosis. Most commonly ileocaecal region is involved. M/E: Ghon’s focus in the intestinal mucosa as occurs elsewhere in primary tuberculous infection. Subsequently, mesentric lymph nodes are affected which show typical tuberculous granulomatous inflammatory reaction with caseation necrosis. 22
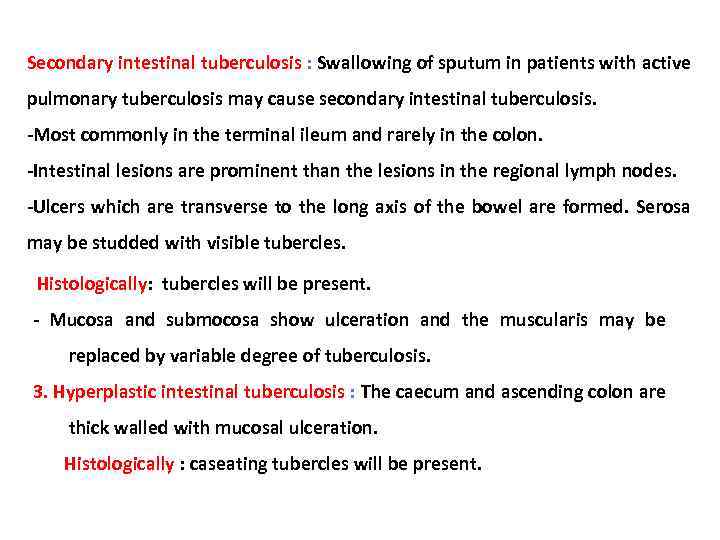
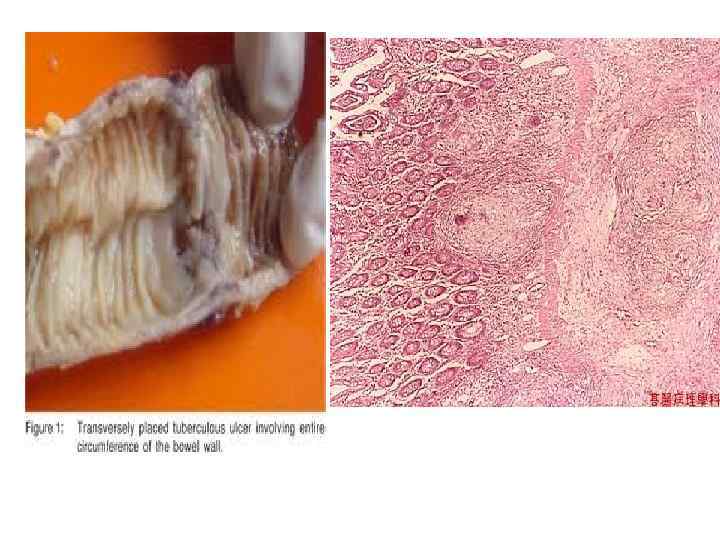
Secondary intestinal tuberculosis : Swallowing of sputum in patients with active pulmonary tuberculosis may cause secondary intestinal tuberculosis. -Most commonly in the terminal ileum and rarely in the colon. -Intestinal lesions are prominent than the lesions in the regional lymph nodes. -Ulcers which are transverse to the long axis of the bowel are formed. Serosa may be studded with visible tubercles. Histologically: tubercles will be present. - Mucosa and submocosa show ulceration and the muscularis may be replaced by variable degree of tuberculosis. 3. Hyperplastic intestinal tuberculosis : The caecum and ascending colon are thick walled with mucosal ulceration. Histologically : caseating tubercles will be present.
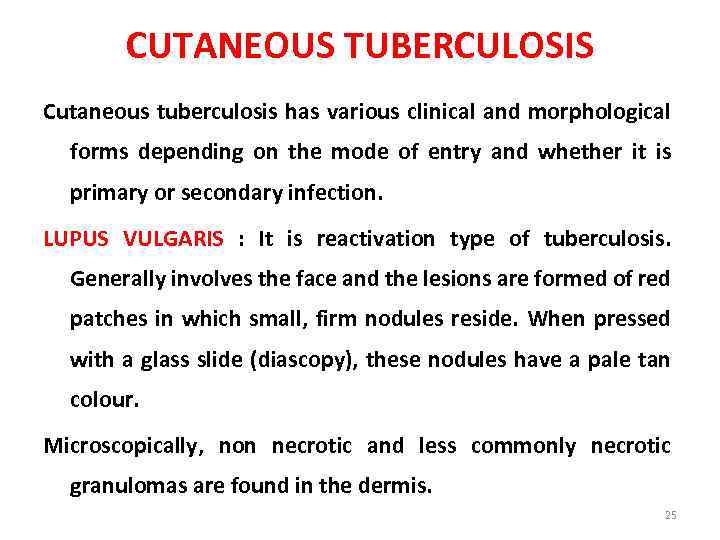
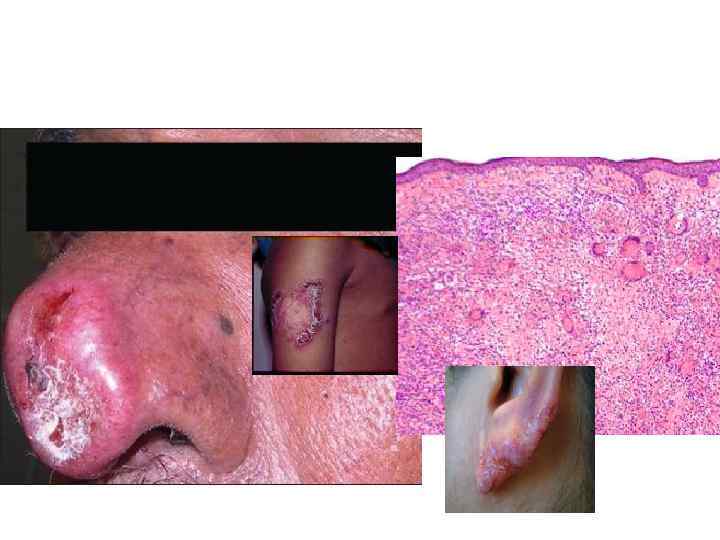
CUTANEOUS TUBERCULOSIS Cutaneous tuberculosis has various clinical and morphological forms depending on the mode of entry and whether it is primary or secondary infection. LUPUS VULGARIS : It is reactivation type of tuberculosis. Generally involves the face and the lesions are formed of red patches in which small, firm nodules reside. When pressed with a glass slide (diascopy), these nodules have a pale tan colour. Microscopically, non necrotic and less commonly necrotic granulomas are found in the dermis. 25

LUPUS VULGARIS
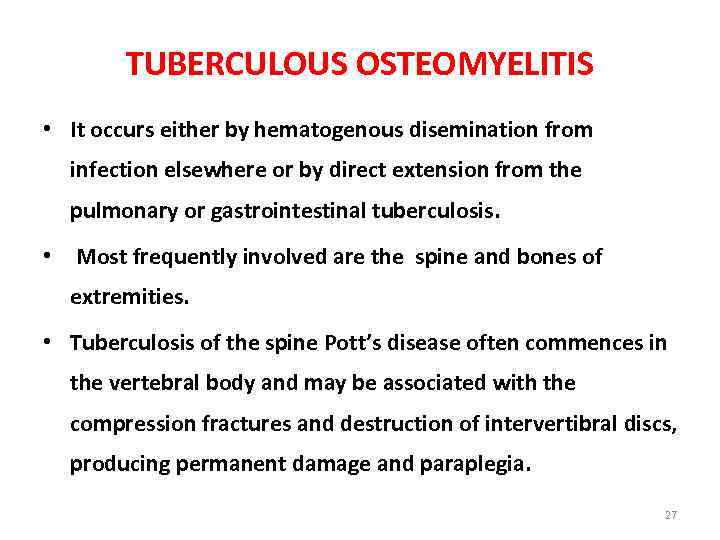
TUBERCULOUS OSTEOMYELITIS • It occurs either by hematogenous disemination from infection elsewhere or by direct extension from the pulmonary or gastrointestinal tuberculosis. • Most frequently involved are the spine and bones of extremities. • Tuberculosis of the spine Pott’s disease often commences in the vertebral body and may be associated with the compression fractures and destruction of intervertibral discs, producing permanent damage and paraplegia. 27
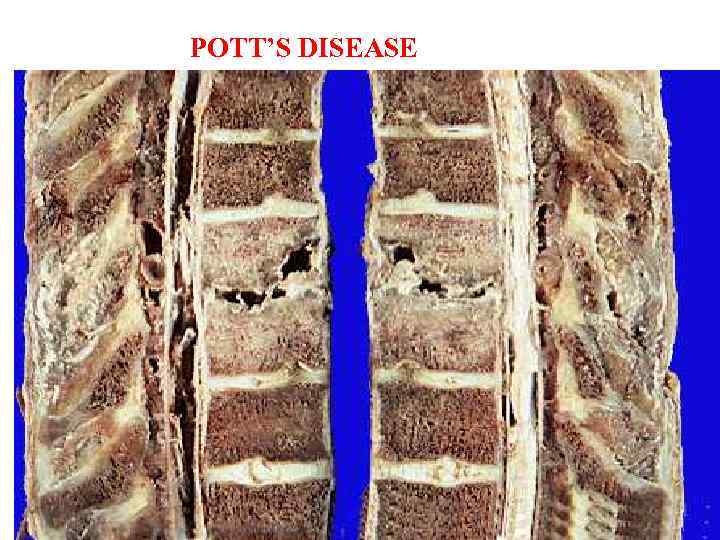
POTT’S DISEASE
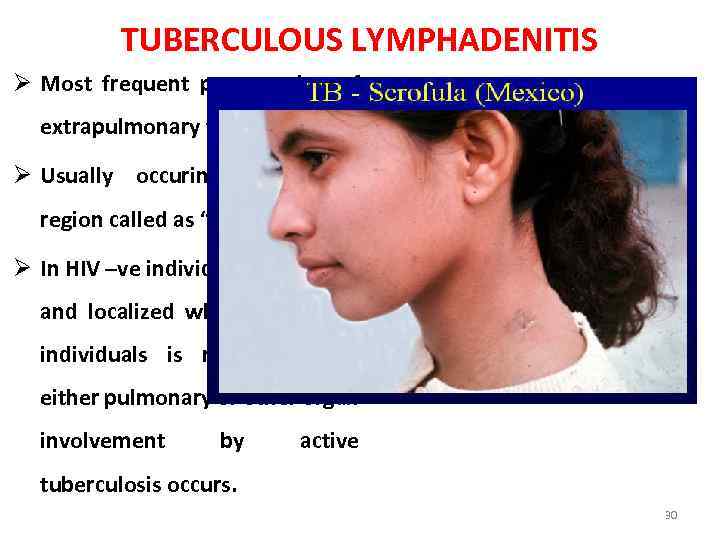
TUBERCULOUS LYMPHADENITIS Ø Most frequent presentation of extrapulmonary tuberculosis. Ø Usually occuring in cervical region called as “Scrofula”. Ø In HIV –ve individuals is unifocal and localized while in HIV +ve individuals is multifocal and either pulmonary or other organ involvement by active tuberculosis occurs. 30
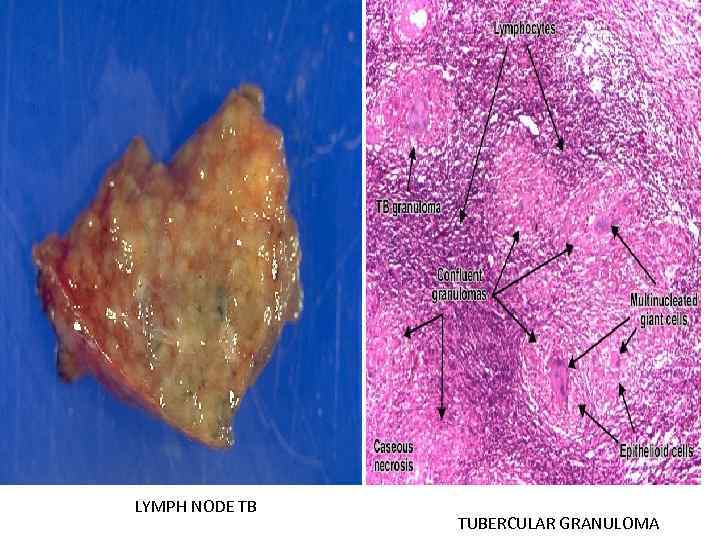
LYMPH NODE TB TUBERCULAR GRANULOMA
CLINICAL FEATURES Common symptoms of pulmonary tuberculosis are- Ø Productive cough 3 weeks or longer Ø Shortness of breath Ø Chest pain Ø Hemoptysis Ø fever/Night sweats Ø Unexplained weight loss Ø Fatigue 32
Ø Other clinical features depends on the site of involvement: • Tuberculous osteomyelitis especially in the spine (Pott’s disease) presents with pain on motion, localized tenderness, permanent compression fractures and neurological deficits secondary to spinal cord and nerve compression. • Adrenocortical insufficiency in cases of Tuberculous adrenalitis. • Tuberculous meningitis have symptoms of headache, malaise, mental confusion and vomiting while brain tuberculomas the symptoms are typical of space occupying lesions of the brain. • Renal tuberculosis presents with painless haematuria. • Tuberculous salpingitis presents with infertility. 33
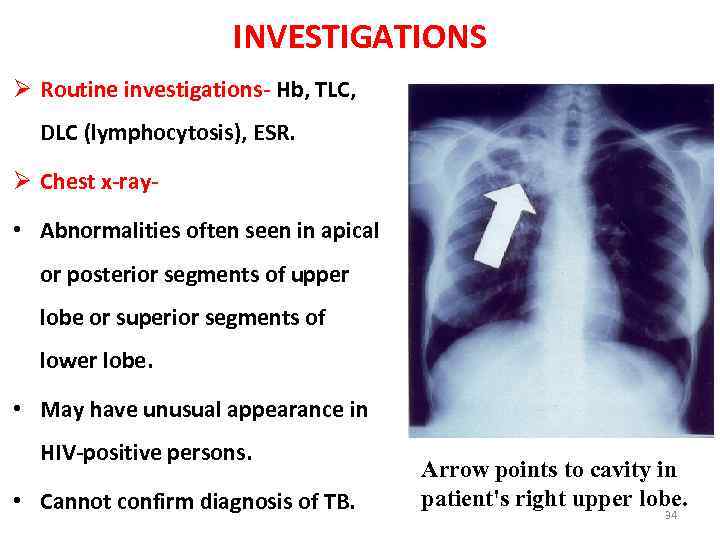
INVESTIGATIONS Ø Routine investigations- Hb, TLC, DLC (lymphocytosis), ESR. Ø Chest x-ray • Abnormalities often seen in apical or posterior segments of upper lobe or superior segments of lower lobe. • May have unusual appearance in HIV-positive persons. • Cannot confirm diagnosis of TB. Arrow points to cavity in patient's right upper lobe. 34
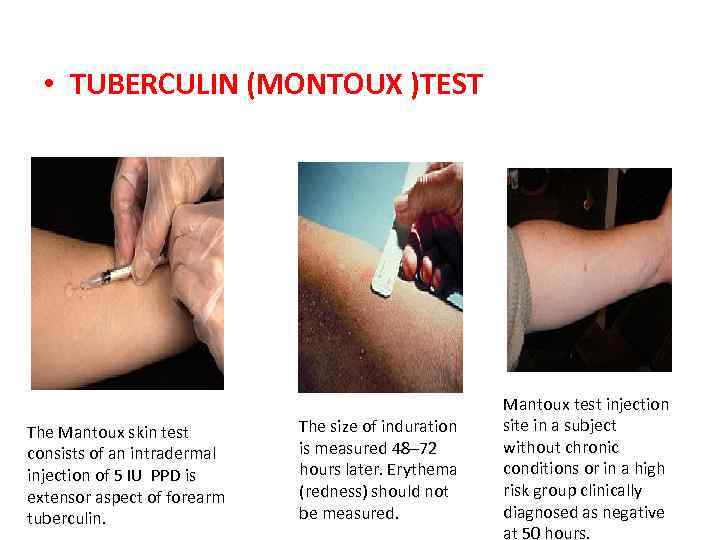
• TUBERCULIN (MONTOUX )TEST The Mantoux skin test consists of an intradermal injection of 5 IU PPD is extensor aspect of forearm tuberculin. The size of induration is measured 48– 72 hours later. Erythema (redness) should not be measured. Mantoux test injection site in a subject without chronic conditions or in a high risk group clinically diagnosed as negative at 50 hours.
§SPUTUM EXAMINATION – Sputum examination are essential to confirm TB §Best collected in morning before any meal. §Sputum examination on 3 days increase chances of detection. §Sputum can be collected from laryngeal swab or bronchial washing. §In small children, gastric lavage can be examined. §Smear should be prepared from thick dirty part of sputum & stained with Ziehl-Neelson technique.
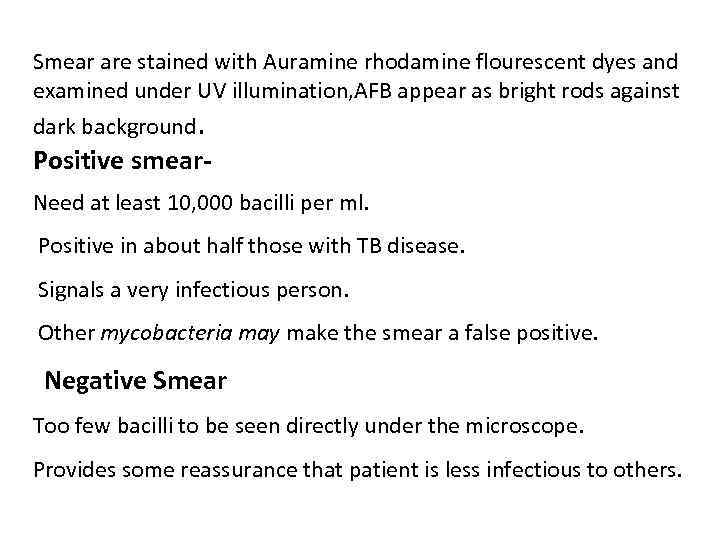
Smear are stained with Auramine rhodamine flourescent dyes and examined under UV illumination, AFB appear as bright rods against dark background. Positive smear. Need at least 10, 000 bacilli per ml. Positive in about half those with TB disease. Signals a very infectious person. Other mycobacteria may make the smear a false positive. Negative Smear Too few bacilli to be seen directly under the microscope. Provides some reassurance that patient is less infectious to others.
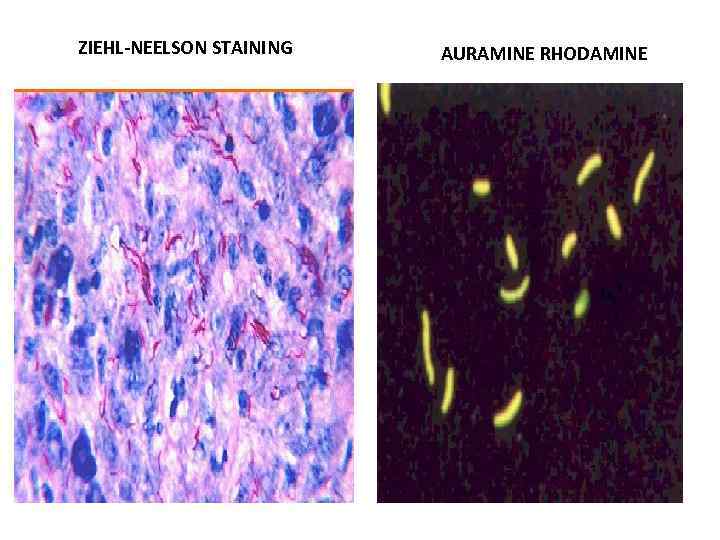
ZIEHL-NEELSON STAINING AURAMINE RHODAMINE
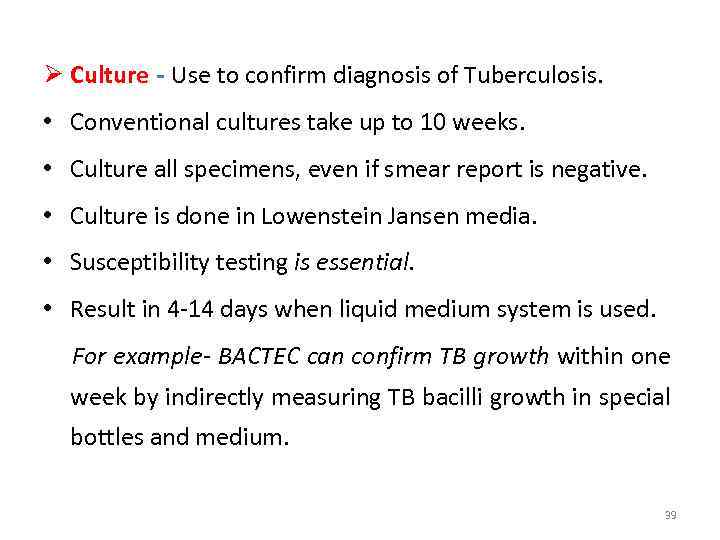
Ø Culture - Use to confirm diagnosis of Tuberculosis. • Conventional cultures take up to 10 weeks. • Culture all specimens, even if smear report is negative. • Culture is done in Lowenstein Jansen media. • Susceptibility testing is essential. • Result in 4 -14 days when liquid medium system is used. For example- BACTEC can confirm TB growth within one week by indirectly measuring TB bacilli growth in special bottles and medium. 39
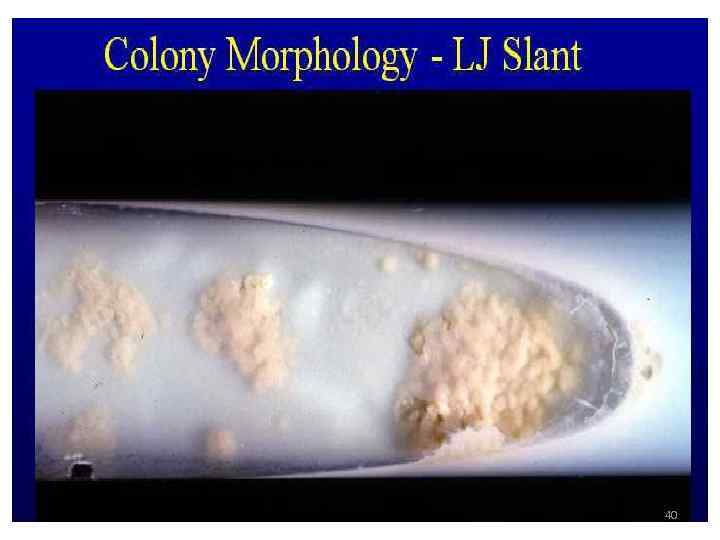
40
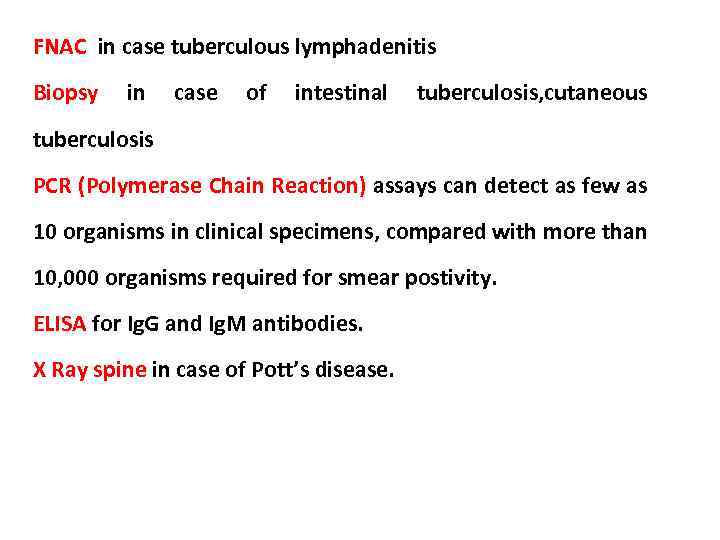
FNAC in case tuberculous lymphadenitis Biopsy in case of intestinal tuberculosis, cutaneous tuberculosis PCR (Polymerase Chain Reaction) assays can detect as few as 10 organisms in clinical specimens, compared with more than 10, 000 organisms required for smear postivity. ELISA for Ig. G and Ig. M antibodies. X Ray spine in case of Pott’s disease.
TREATING TB DISEASE (GENERAL PRINCIPLES) Ø Always treat with multiple drugs. Ø Never add a single drug to a failing regimen. Ø DOTS (Directly Observed Treatment Shortcourse) is given. Ø Treatment course depends on the categories of the patient. Ø Usually 6 months, sometimes 9 months. Ø Four drugs for two months. Isoniazid – Rifampicin – Ethambutol - Pyrazinamide Ø Two drugs for four or seven months. Isoniazid - Rifampicin 42
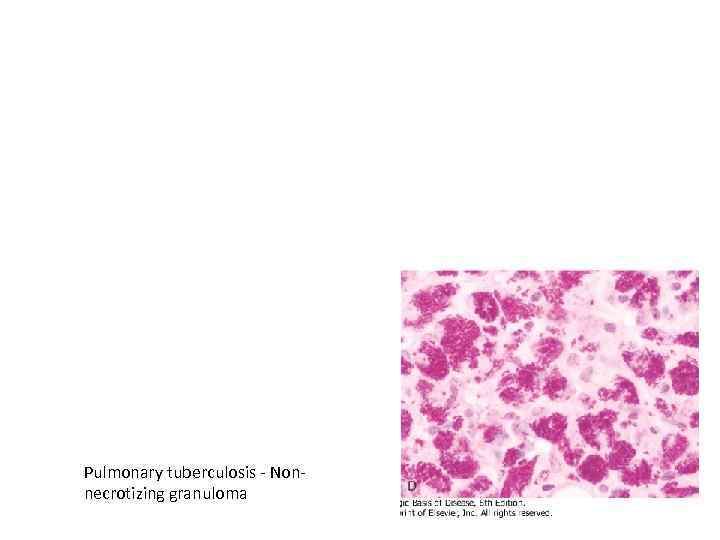
Pulmonary tuberculosis - Nonnecrotizing granuloma
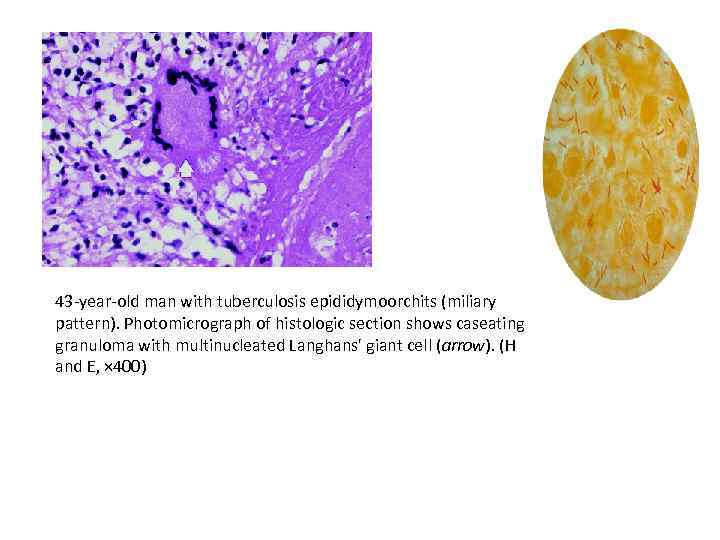
43 -year-old man with tuberculosis epididymoorchits (miliary pattern). Photomicrograph of histologic section shows caseating granuloma with multinucleated Langhans' giant cell (arrow). (H and E, × 400)
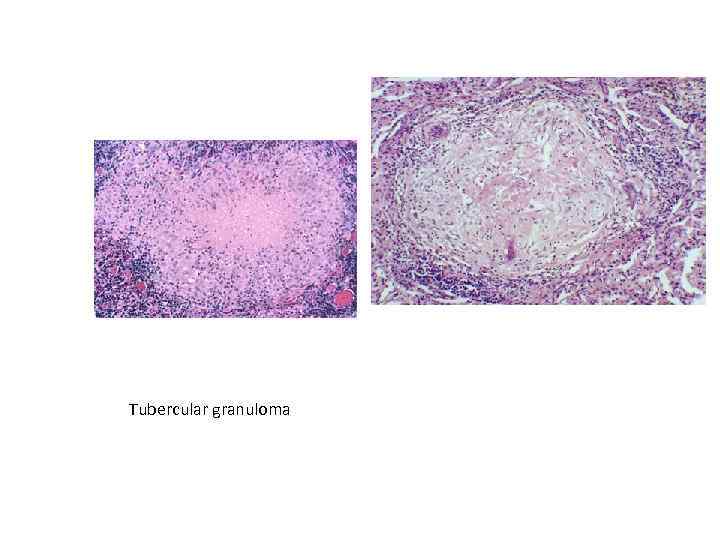
Tubercular granuloma

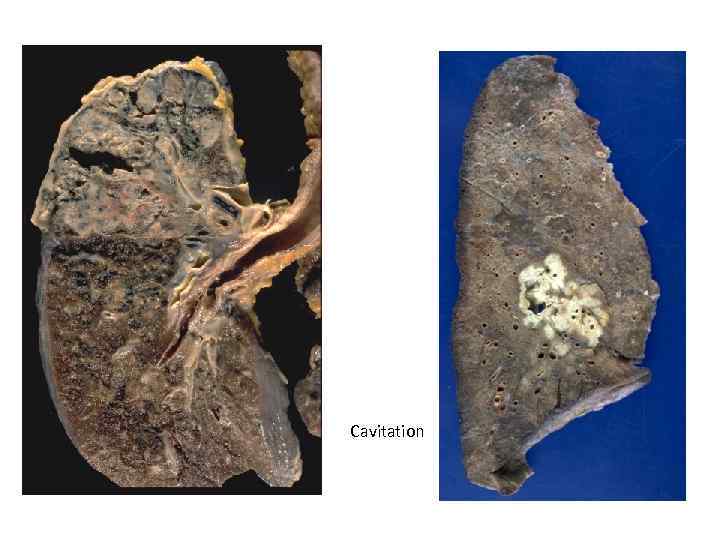
Cavitation
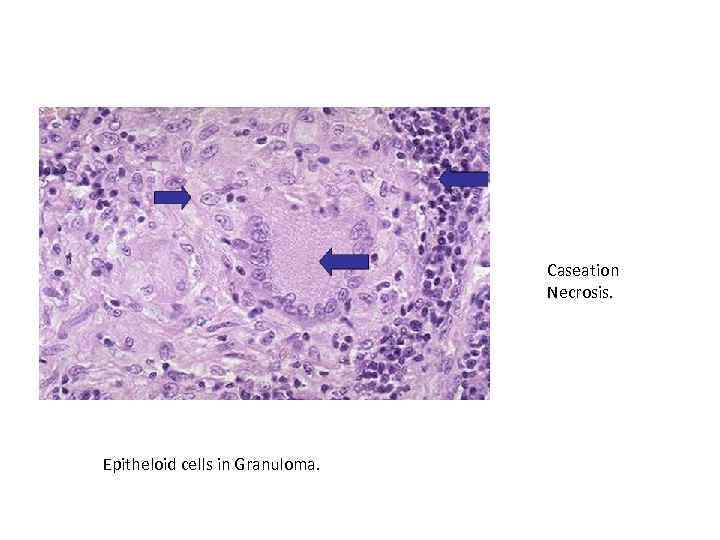
Caseation Necrosis. Epitheloid cells in Granuloma.
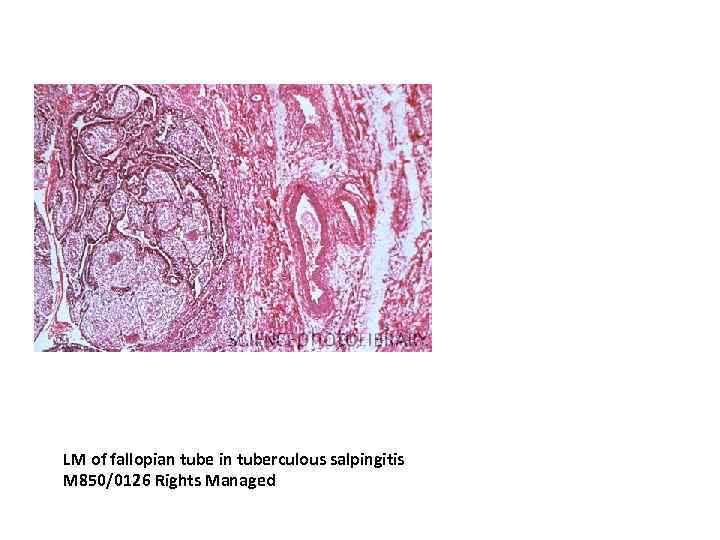
LM of fallopian tube in tuberculous salpingitis M 850/0126 Rights Managed
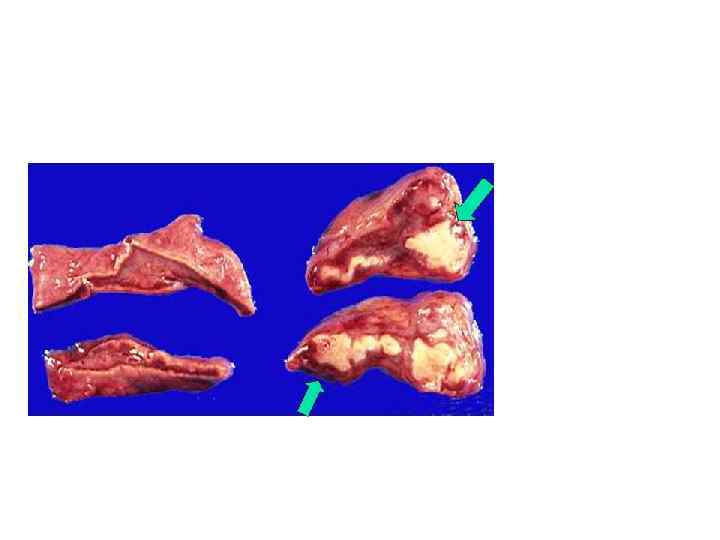
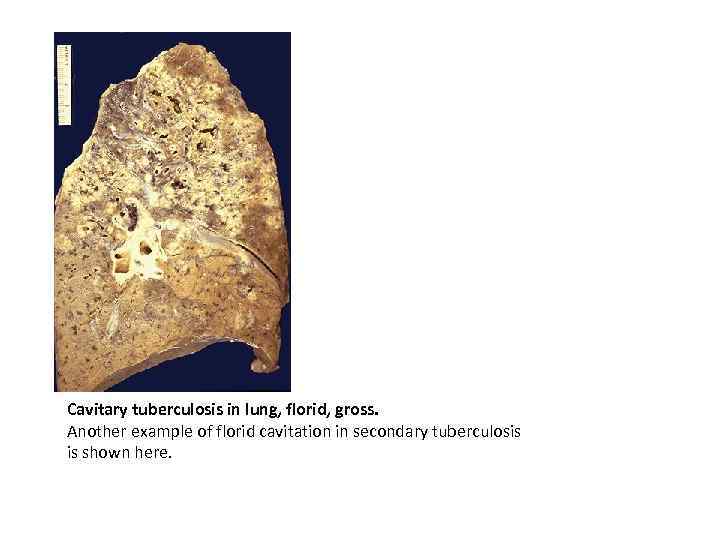
Cavitary tuberculosis in lung, florid, gross. Another example of florid cavitation in secondary tuberculosis is shown here.
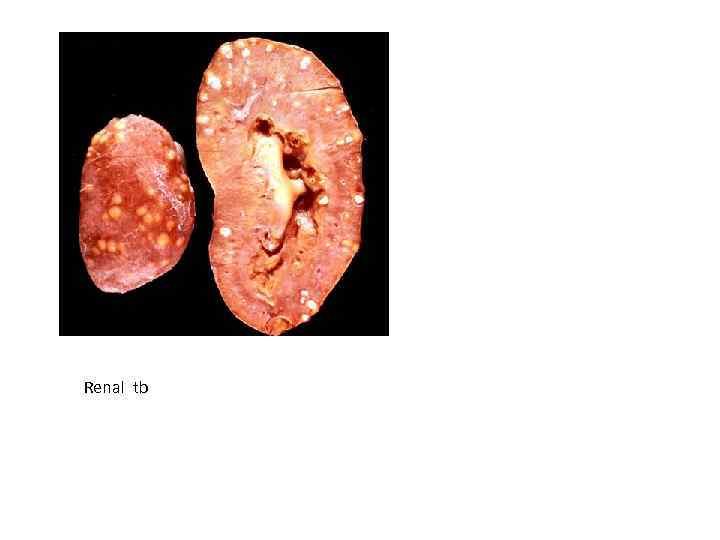
Renal tb

tuber.pptx