6e6ba06c0f2c5a58bf010bd8eed08655.ppt
- Количество слайдов: 38
TUBERCULOSIS DIAGNOSIS TREATMENT ACTION GROUP TB/HIV ADVOCACY TOOLKIT NOVEMBER 2017 With thanks to Adam Almeida and Andolyn Medina
TOPICS TO BE COVERED • Fundamentals: what is “diagnosis”? • Active TB Diagnosis • • Screening • Tools for diagnosis: microbiological confirmation • Tools for diagnosis: LAM • Diagnosing active TB in special populations Latent TB Infection • • Tools for diagnosis The Main Points
FUNDAMENTALS: WHAT IS DIAGNOSIS?
WHAT IS DIAGNOSIS? • Diagnosis is the evaluation of a health outcome (e. g. , active TB disease or latent TB infection), using a method or tool to measure, identify, or analyze conditions of the body • in vitro diagnostics use samples taken from the human body– most TB diagnostics are in vitro • in vivo diagnostics are conducted in the body—the tuberculin skin test used for diagnosing latent TB infection is an in vivo diagnostic • Diagnostic tests detect changes in our bodies that indicate an unhealthy state or look for the source of disease • TB diagnostics are used to: • identify latent TB infection • find active TB disease • provide information about drug resistance (what drugs will work best for treatment) FUNDAMENTALS
TB DIAGNOSTIC VOCABULARY • Sensitivity: refers to the proportion of people with a disease that are correctly identified by a diagnostic tool as having the condition • Specificity: refers to the proportion of people without a disease that are correctly identified by a diagnostic tool as not having the condition • False Positive: a test that incorrectly shows someone as having the health outcome of interest (TB, TB infection, drug resistance) when they do not • This shows that a test has low specificity • False Negative: a test that incorrectly shows someone as not having the health outcome of interest (TB, TB infection, drug resistance) when they do • This shows that a test has low sensitivity FUNDAMENTALS
TB DIAGNOSTIC VOCABULARY • Media: the substances (solid or liquid) containing nutrients that allow TB bacteria to be grown in a laboratory setting • Culture: the process of growing TB bacteria on a substance that provides nutrients (food) to allow the TB to grow • Drug susceptibility testing (DST): a test to detect drug resistance– that is, a test to see which drugs will work best against a particular strain of TB • Gold standard: the best way to do something FUNDAMENTALS
ACTIVE TB DIAGNOSIS
WHAT IS SCREENING? • Screening is used to detect possible cases of TB among vulnerable populations at high risk for contracting the disease • Screening tools are typically not very specific, but they are sensitive • This means that false positives are common, but false negatives are rare • Screening is used to rule out active cases of TB or to continue on with microbiological testing • Not everyone needs to be tested for TB, efforts should be focused on high-risk groups (outlined in the next slide) • The two main screening tools for TB are symptom screening and chest X-ray SCREENING
SYMPTOM SCREENING Symptom screening can be performed in groups at high risk for contracting TB High-risk for TB: • People with close contact with someone with TB • People with HIV • Workers exposed to crystalline silica dust Symptoms of TB: • Cough • Hemoptysis (coughing up blood) • Fever • Night sweats • Weight loss Advantages • Helps people seek healthcare • Allows the diagnostic process to start • Inexpensive Disadvantages • Inconclusive (not a final answer) • Occurs when disease has already progressed • Not useful for extrapulmonary TB (TB outside the lungs) • Potential to increase number of false positives Source: http: //www. who. int/tb/publications/tbscreenin g_factsheet. pdf? ua=1 SCREENING
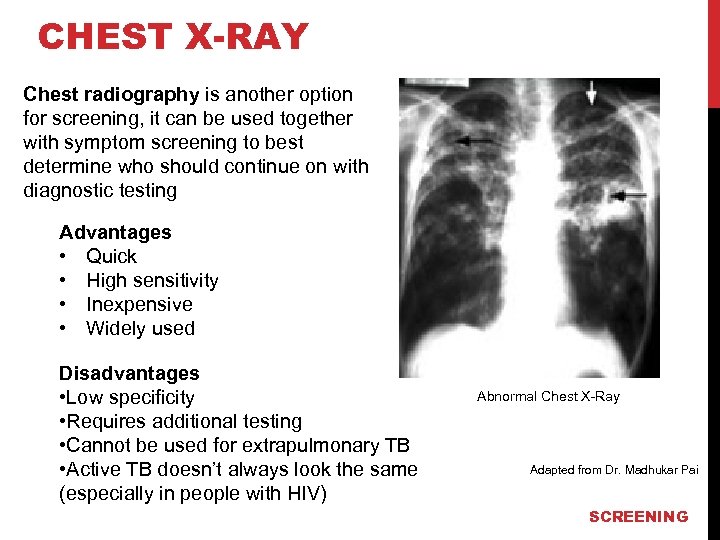
CHEST X-RAY Chest radiography is another option for screening, it can be used together with symptom screening to best determine who should continue on with diagnostic testing Advantages • Quick • High sensitivity • Inexpensive • Widely used Disadvantages • Low specificity • Requires additional testing • Cannot be used for extrapulmonary TB • Active TB doesn’t always look the same (especially in people with HIV) Abnormal Chest X-Ray Adapted from Dr. Madhukar Pai SCREENING
DIAGNOSTIC TECHNIQUES Microbiological confirmation means diagnosing TB by detecting the presence of M. tuberculosis (MTB), the bacterium or bug that causes TB • Microbiological confirmation is the preferred way to diagnose active TB There are three types of microbiological tests for TB: 1) See the bug • Sputum smear microscopy 2) Multiply the bug (multiply genetic information from MTB) • Nucleic Acid Amplification Test (NAAT)* • Xpert MTB/RIF ULTRA • Line Probe Assays 3) Grow the bug • Solid culture • Liquid culture (MGIT, MODS, Bac. T/ALERT 3 D) Concept courtesy of Dr. Madhukar Pai *NOTE: TB LAMP, not to be confused with LAM (which is covered later in this deck) is omitted due to limited utility as compared to Xpert MTB/RIF Ultra DIAGNOSTIC TOOLS
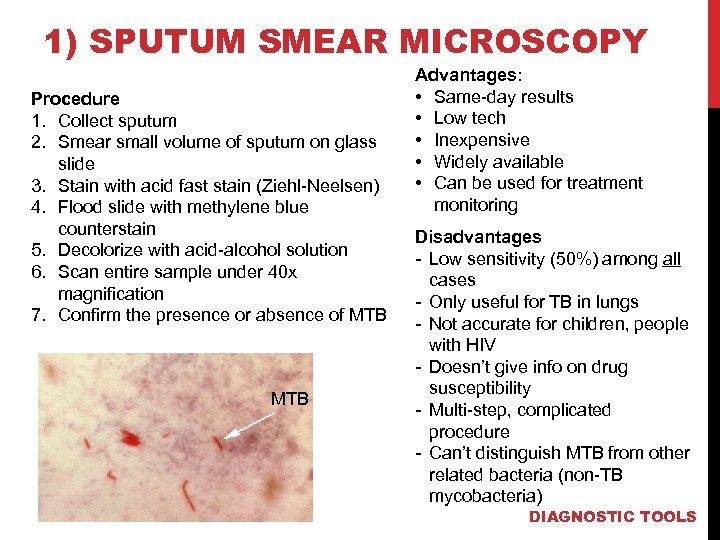
1) SPUTUM SMEAR MICROSCOPY Procedure 1. Collect sputum 2. Smear small volume of sputum on glass slide 3. Stain with acid fast stain (Ziehl-Neelsen) 4. Flood slide with methylene blue counterstain 5. Decolorize with acid-alcohol solution 6. Scan entire sample under 40 x magnification 7. Confirm the presence or absence of MTB Advantages: • Same-day results • Low tech • Inexpensive • Widely available • Can be used for treatment monitoring Disadvantages - Low sensitivity (50%) among all cases - Only useful for TB in lungs - Not accurate for children, people with HIV - Doesn’t give info on drug susceptibility - Multi-step, complicated procedure - Can’t distinguish MTB from other related bacteria (non-TB mycobacteria) DIAGNOSTIC TOOLS
Optimization Of Microscopy The WHO recommends the following strategies to improve microscopy: • Use fluorescence staining • Use light-emitting diode (LED) microscope • Inexpensive, battery-operated light source can be used These additions make bacteria easier to detect, offering about 10% increase in sensitivity and making smear 25% faster compared to conventional microscopy BUT even still, smear is less sensitive and specific than Xpert MTB/RIF ULTRA, and gives no information on drug resistance Image source: Health Biz Informa DIAGNOSTIC TOOLS
2) NUCLEIC ACID AMPLIFICATION TESTS • Nucleic acid amplification testing (NAAT) searches the genetic information in the tests sample to find the presence of MTB • It can analyze two different kinds of genetic information: DNA and RNA • NAAT is able to analyze genetic mutations that cause drug resistance as well, allowing the test to determine which treatment would be most effective • NAAT is a fast testing method because the genetic information is extracted and amplified, rather than waiting for the bacteria to grow DIAGNOSTIC TOOLS
GENEXPERT Gene. Xpert system is a cartridge-based test to detect MTB and resistance to the drug rifampicin • The cartridge is called “Xpert MTB/RIF ULTRA” • The new Ultra cartridge is more sensitive than the previous Xpert MTB/RIF cartrdige, especially in people with HIV, people with extrapulmonary TB, and children • The system analyzes a sample by extracting MTB genetic information, multiplying it, and reading its genetic code • The WHO recommends Gene. Xpert as the initial test for all adults and children in need of TB evaluation • In the future… • A small, portable machine with only one module (can only run one test at a time) called Omni is coming out in 2018 • A cartridge in development may be able to detect resistance to more drugs (isoniazid, fluoroquinolones, and the second-line injectables) http: //apps. who. int/iris/bitstream/10665/254792/1/WHO-HTM-TB-2017. 04 -eng. pdf DIAGNOSTIC TOOLS
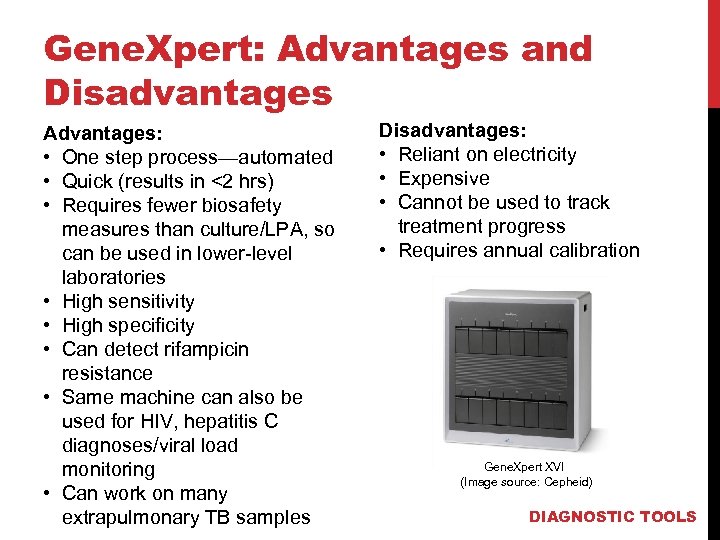
Gene. Xpert: Advantages and Disadvantages Advantages: • One step process—automated • Quick (results in <2 hrs) • Requires fewer biosafety measures than culture/LPA, so can be used in lower-level laboratories • High sensitivity • High specificity • Can detect rifampicin resistance • Same machine can also be used for HIV, hepatitis C diagnoses/viral load monitoring • Can work on many extrapulmonary TB samples Disadvantages: • Reliant on electricity • Expensive • Cannot be used to track treatment progress • Requires annual calibration Gene. Xpert XVI (Image source: Cepheid) DIAGNOSTIC TOOLS
Line Probe Assay Line probe assays (LPAs) are another genetic or molecular test • They can detect presence of MTB • First-line LPAs can detect rifampicin and isoniazid resistance (MDR -TB) • Second-line LPAs can be used to detect resistance to the secondline injectable drugs and fluoroquinolones • LPAs are very important for quickly guiding treatment decisions: § To detect resistance to isoniazid, which has worse health outcomes and is not detected by Gene. Xpert § To determine which people with MDR-TB can take the shortened regimen DIAGNOSTIC TOOLS
Line Probe ASSAy Advantages: • Can perform multiple tests at once • Quick (results in under 48 hrs) • Accurate • Only rapid test to give information about isoniazid resistance • Necessary for guiding treatment decisions Disadvantages: • Cannot fully replace other methods, like conventional cultures • Not as fast as Xpert • Expensive • Requires well-trained staff in a professional laboratory • Has high biosafety requirements (can only be used in certain labs) DIAGNOSTIC TOOLS
3) CULTURE • Culture is considered the gold standard, meaning the most accurate test, for TB • Culture is the growth of bacteria in vitro (in a controlled environment outside of the body) on a medium (substance providing nutrients) • The number of colony forming units (CFU)—MTB bacterial cells that can grow—can then be counted, either visually or by automated detection • Culture positive: presence of any MTB CFUs • Culture negative: no CFU detected after 42 days Advantages: • High sensitivity • High specificity • Ability to perform drug susceptibility testing (called “phenotypic testing”) • Can assess treatment progress Disadvantages: • Requires trained staff • Automated liquid culture is expensive (but getting more affordable) • Solid culture takes longer DIAGNOSTIC TOOLS
MODS • Microscopic observation drug susceptibility (MODS) is an inexpensive, non-commercial liquid culture option • It gives results within seven days • Due to its low cost, MODS is feasible in resource-limited areas • The WHO recommends MODS as a method of detection as countries move towards the roll-out of automated liquid culture methods DIAGNOSTIC TOOLS
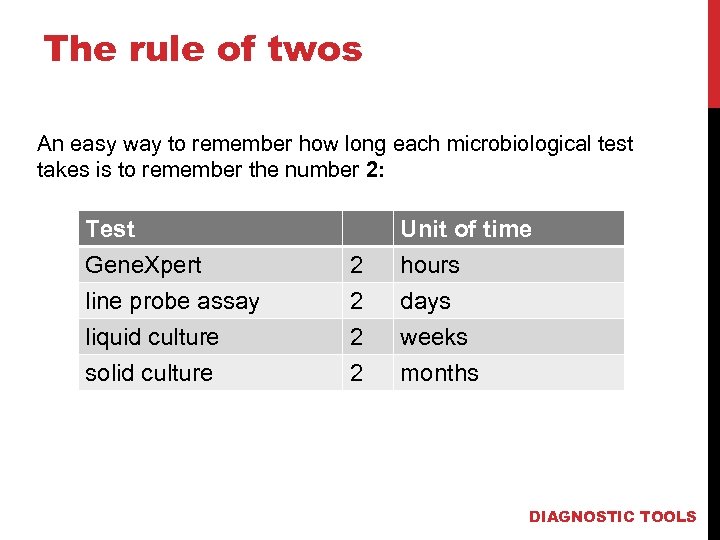
The rule of twos An easy way to remember how long each microbiological test takes is to remember the number 2: Test Gene. Xpert line probe assay liquid culture 2 2 2 Unit of time hours days weeks solid culture 2 months DIAGNOSTIC TOOLS
POINT-OF-CARE TESTING • Most microbiological tests for detecting MTB provide the clearest diagnosis of TB and allow drug susceptibility to be tested as well • However, these tests have many limitations: they can be expensive, lengthy, and require infrastructure, like laboratories and trained staff, to be in place to analyze the specimens. Most importantly, current microbiological tests do not provide information at the point-of-care level • The LAM test is a newly introduced diagnostic tool that provides point-of-care TB testing in some people with HIV DIAGNOSTIC TOOLS
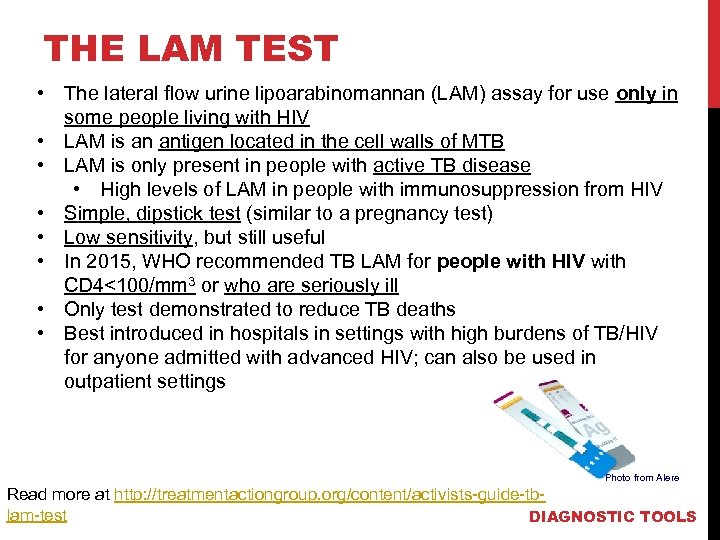
THE LAM TEST • The lateral flow urine lipoarabinomannan (LAM) assay for use only in some people living with HIV • LAM is an antigen located in the cell walls of MTB • LAM is only present in people with active TB disease • High levels of LAM in people with immunosuppression from HIV • Simple, dipstick test (similar to a pregnancy test) • Low sensitivity, but still useful • In 2015, WHO recommended TB LAM for people with HIV with CD 4<100/mm 3 or who are seriously ill • Only test demonstrated to reduce TB deaths • Best introduced in hospitals in settings with high burdens of TB/HIV for anyone admitted with advanced HIV; can also be used in outpatient settings Photo from Alere Read more at http: //treatmentactiongroup. org/content/activists-guide-tblam-test DIAGNOSTIC TOOLS
THE LAM TEST • If positive, treatment should be started immediately • If negative, follow up with another kind of test since sensitivity is not very high Advantages • Point-of-care test • Simple, very low-tech • Fast (25 minutes) • Inexpensive • Easy to collect and store urine • Detection in population that cannot use other diagnostic techniques • Does not require electricity or labs • Saves lives by allowing earlier treatment start* Disadvantages • Test must be followed up with other diagnostics • Low sensitivity • No info on drug resistance • Used in limited patient population • Cannot distinguish MTB from other non-TB mycobacteria *Peter, J. G. et al. (March 01, 2016). Effect on mortality of point-of-care, urine-based lipoarabinomannan testing to guide tuberculosis treatment initiation in HIV-positive hospital inpatients: a pragmatic, parallel-group, multicountry, open-label, randomised controlled trial. The Lancet, 387, 10024, 1187 -1197. Source: http: //www. who. int/tb/areas-ofwork/laboratory/policy_statement_lam_web. pdf DIAGNOSTIC TOOLS
Diagnosing Extrapulmonary TB • Most TB tests rely on sputum as the sample, but this will not work for TB outside the lungs (extrapulmonary TB) • Usually performed due to clinical suspicion • Sample taken from the suspected site of disease • Options: need to use a combination of tests • Smear: likely to be negative • Gene. Xpert: on tissue biopsies, gastric contents, pus, cerebrospinal fluid, and urine • Culture: helpful, but takes 2 -3 weeks • Biopsy: very helpful • If nothing works, treat TB based on clinical judgment even in absence of confirmation (empiric treatment) • No role for blood tests • Blood is not used in any active TB diagnosis Slide courtesy of Dr. Madhukar Pai DIAGNOSTIC TOOLS
DIAGNOSIS IN CHILDREN • Children are an especially vulnerable population for developing active TB • Diagnosing children comes with its own set of difficulties since: • Children have difficulty producing sputum samples • Children have lower levels of bacteria in the body • TB is often diagnosed in children without microbiological confirmation • Instead, a physician will use symptom screening, chest Xrays, or points of contact with infected individuals • For using microbiological diagnostic tests, Gene. Xpert is preferred SPECIAL POPULATIONS
Latent TB INFECTION DIAGNOSIS Goal: prevent active TB by giving preventive therapy • Options: • Tuberculin Skin Test (TST) • Also referred to as the Mantoux test • Uses purified protein derivative (PPD) • Interferon Gamma Release Assays (IGRAs) • TB Platinum • T Spot. TB Test • Quanti. FERON-TB Gold Plus • There is no “gold standard” for diagnosing latent TB infection • No test can predict who with latent TB infection will develop active TB disease • WHO recommends that TST be performed instead of IGRA in resource-poor settings, due to its cost and similar effectiveness • For people with HIV, do not need to diagnose LTBI to start preventive therapy, as long as active disease is ruled out DIAGNOSING TB INFECTION
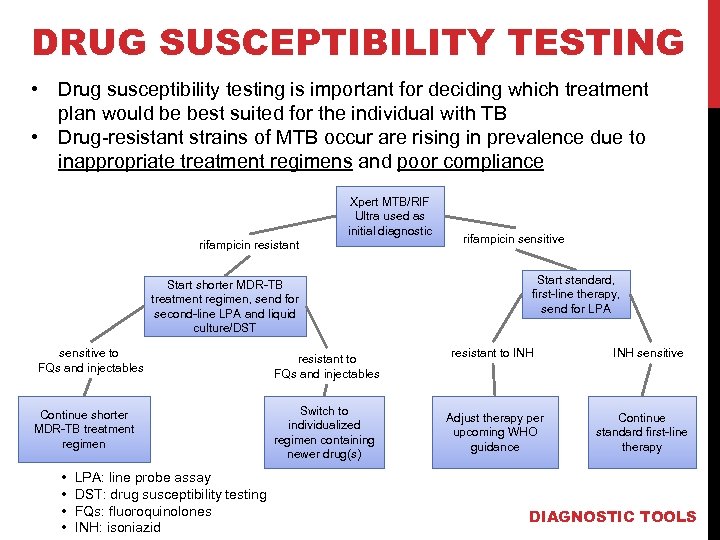
DRUG SUSCEPTIBILITY TESTING • Drug susceptibility testing is important for deciding which treatment plan would be best suited for the individual with TB • Drug-resistant strains of MTB occur are rising in prevalence due to inappropriate treatment regimens and poor compliance Xpert MTB/RIF Ultra used as initial diagnostic rifampicin resistant Start shorter MDR-TB treatment regimen, send for second-line LPA and liquid culture/DST sensitive to FQs and injectables Continue shorter MDR-TB treatment regimen • • LPA: line probe assay DST: drug susceptibility testing FQs: fluoroquinolones INH: isoniazid resistant to FQs and injectables Switch to individualized regimen containing newer drug(s) rifampicin sensitive Start standard, first-line therapy, send for LPA resistant to INH Adjust therapy per upcoming WHO guidance INH sensitive Continue standard first-line therapy DIAGNOSTIC TOOLS
TOOLS FOR DIAGNOSIS: TB INFECTION
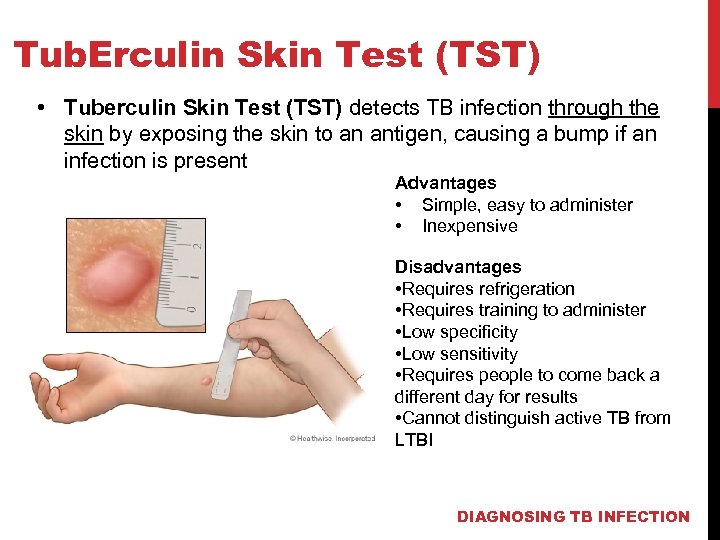
Tub. Erculin Skin Test (TST) • Tuberculin Skin Test (TST) detects TB infection through the skin by exposing the skin to an antigen, causing a bump if an infection is present Advantages • Simple, easy to administer • Inexpensive Disadvantages • Requires refrigeration • Requires training to administer • Low specificity • Low sensitivity • Requires people to come back a different day for results • Cannot distinguish active TB from LTBI DIAGNOSING TB INFECTION
Interferon Gamma Release Assays (IGRA) • IGRAs uses a blood sample to determine the body’s immune reactivity to MTB • White blood cells from people with MTB infection release interferon-gamma when they meet MTB antigens • Fresh blood samples are mixed with antigens and controls to compare reactions Advantages: • One-time test • Quick (results in 24 h) • Does not boost responses measured by subsequent tests • Prior BCG (bacille Calmette. Guérin) vaccination does not cause a false-positive result Source: http: //www. cdc. gov/tb/publications/factsheets/testing/igra. htm Disadvantages: • Expensive • Blood must be processed quickly after collection • Errors arise easily • Cannot distinguish active TB from LTBI • Limited data on use in children and people with HIV DIAGNOSING TB INFECTION

THE MAIN POINTS
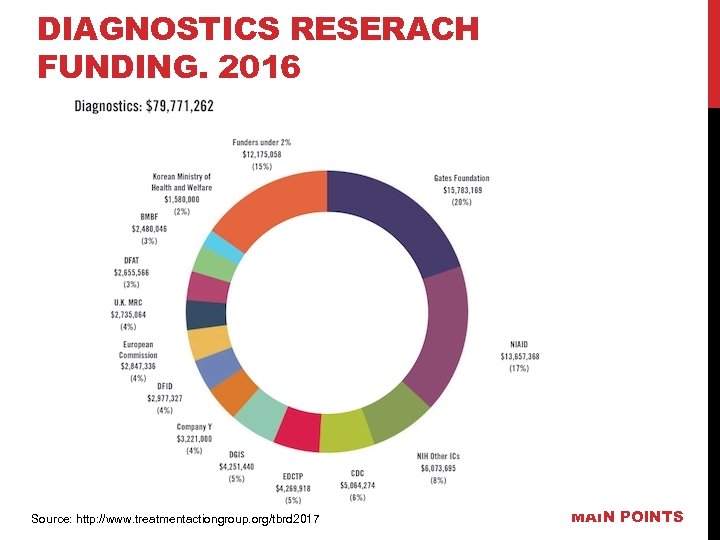
DIAGNOSTICS RESERACH FUNDING, 2016 Source: http: //www. treatmentactiongroup. org/tbrd 2017 MAIN POINTS
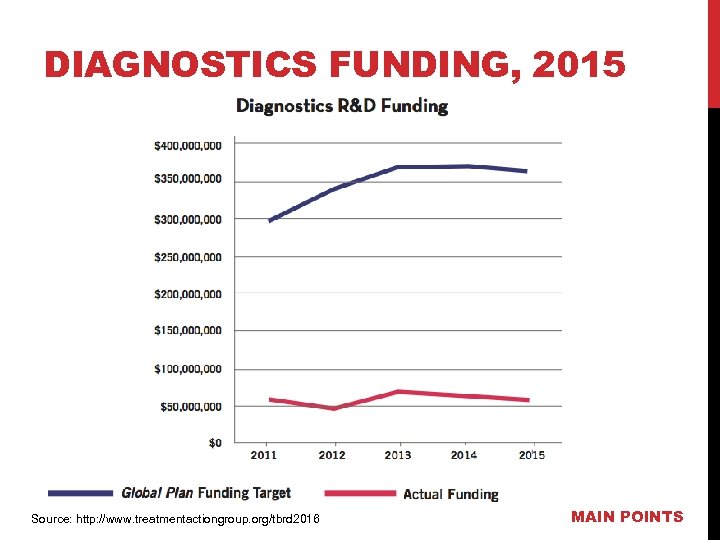
DIAGNOSTICS FUNDING, 2015 Source: http: //www. treatmentactiongroup. org/tbrd 2016 MAIN POINTS
Limitations in Diagnosis • TB screening and diagnosis requires a combination of different methods and techniques to accurately test people • There is no singlr TB test that can do it all • Most TB diagnostic tests are not appropriate for use as point-of-care tests in local settings where most TB patients are seen • Culture and LPA require high biosafety levels to protect the workers and get accurate results. • Majority of TB tests require electricity, equipment, and some degree of infrastructure • Most are costly for national governments to afford without donor support • We need more investment in TB research and development to develop better tests MAIN POINTS
How to know if a diagnostic is useful in your setting • Is the test sensitive and specific? • What kind of TB (e. g. , smear-negative TB, drug resistant TB, latent TB) and populations (e. g. , infants, people with HIV) is it useful for? • How long does the test take? • What does the test tell us (e. g. infection, disease)? • Does its use need a lot of technology and training? • What type of specimen does it need (e. g. sputum, urine)? • Does it need a high level of biosafety? (e. g. does it involve culturing the bacteria)? • What does it cost? • Has the test been studied objectively and endorsed by WHO? MAIN POINTS
MAIN MESSAGE— ALL COUNTRIES NEED: • Gene. Xpert MTB/RIF ULTRA as the initial test for ALL people needing testing for TB • Line Probe Assay (both first- and second-line) to quickly guide treatment decisions • Liquid culture (MGIT) for full drug susceptibility testing AND monitoring drug-resistant TB treatment • Smear microscopy for monitoring standard TB treatment, but Gene. Xpert is the preferred test for diagnosing TB In areas with high burdens of TB/HIV: • TB LAM (Determine TB LAM Ag) for quickly, easily finding TB in people very sick with HIV and starting them on TB treatment MAIN POINTS
ADDITIONAL RESOURCES Treatment Action Group (TAG) has created An Activist’s Guide to Tuberculosis Diagnostic Tools, which expands upon what has been outlined in these slide decks. To access: http: //www. treatmentactiongroup. org/site s/default/files/TB%20 Diagnostics%20 Gu ide. pdf TAG also issued An Activist's Guide to the TB LAM Test, available at: http: //treatmentactiongroup. org/conte nt/activists-guide-tb-lam-test MAIN POINTS
6e6ba06c0f2c5a58bf010bd8eed08655.ppt