Tuberculosis case detecting Lecturer Grib Helen Main



- Размер: 3.5 Mегабайта
- Количество слайдов: 36
Описание презентации Tuberculosis case detecting Lecturer Grib Helen Main по слайдам
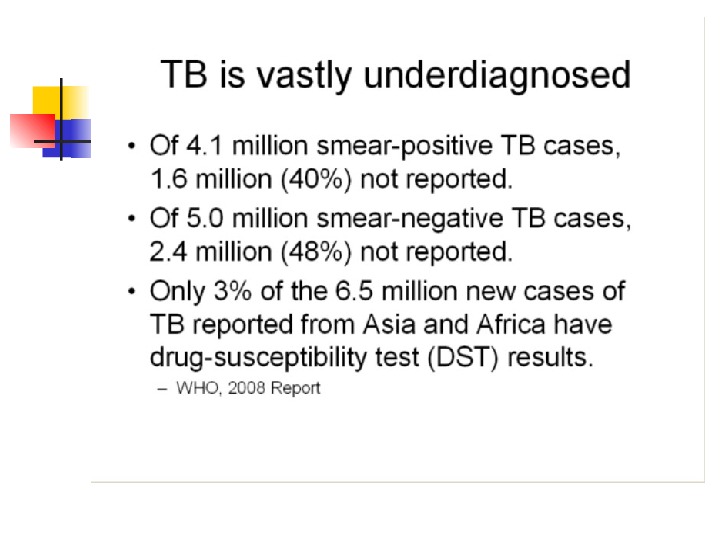
 Tuberculosis case detecting Lecturer Grib Helen
Tuberculosis case detecting Lecturer Grib Helen
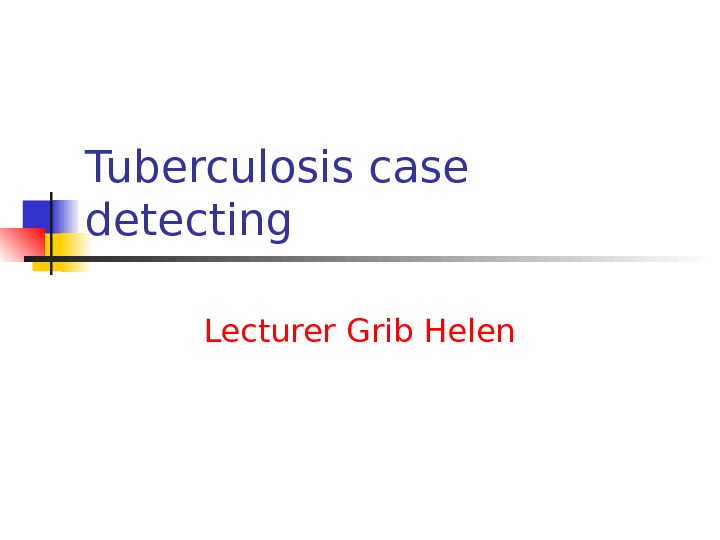
 Main ways of the new cases revealing Passive Obligate diagnostical minimum (clinical, radiological examination, direct smear microscopy) Active Screening X-ray examination for adults Screening Mantoux test for children
Main ways of the new cases revealing Passive Obligate diagnostical minimum (clinical, radiological examination, direct smear microscopy) Active Screening X-ray examination for adults Screening Mantoux test for children
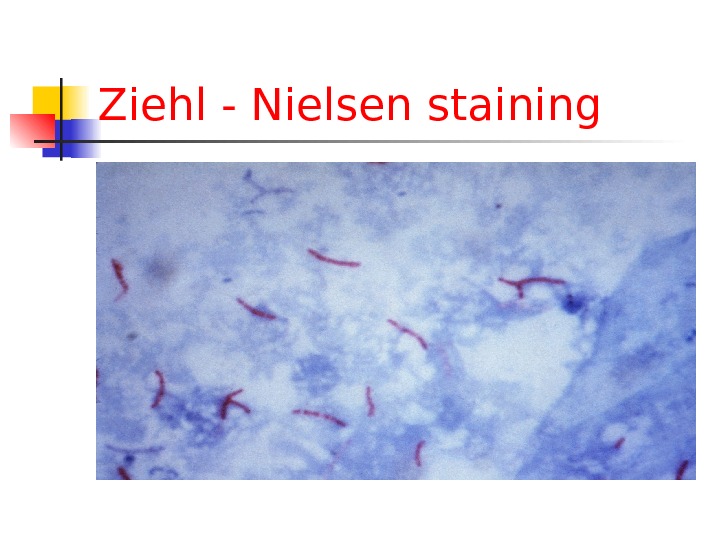
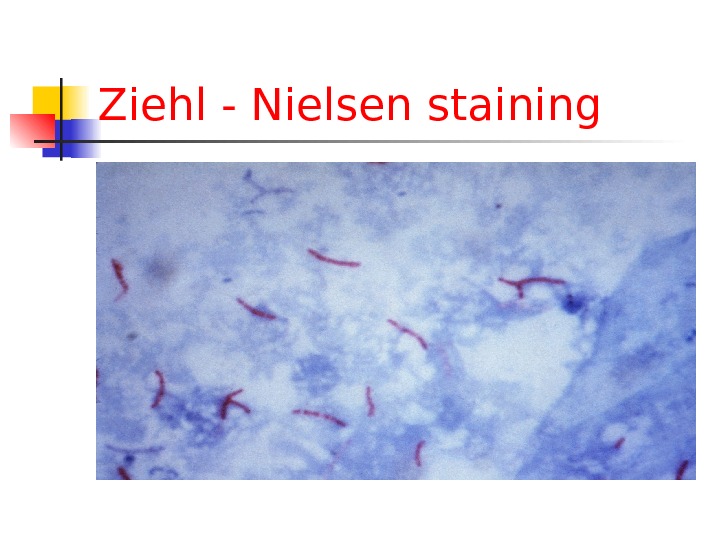 Ziehl — Nielsen staining
Ziehl — Nielsen staining
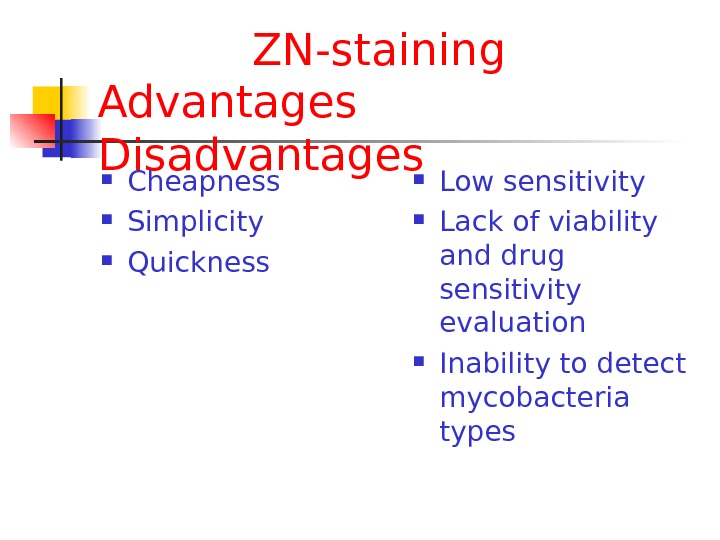
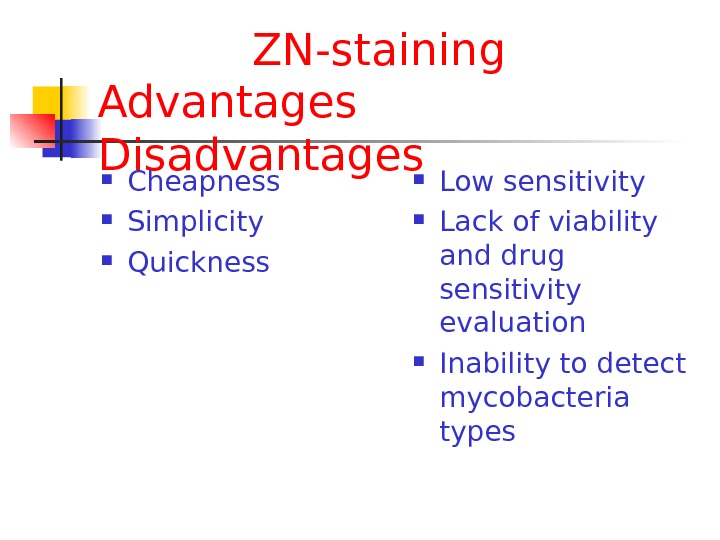 ZN-staining Advantages Disadvantages Cheapness Simplicity Quickness Low sensitivity Lack of viability and drug sensitivity evaluation Inability to detect mycobacteria types
ZN-staining Advantages Disadvantages Cheapness Simplicity Quickness Low sensitivity Lack of viability and drug sensitivity evaluation Inability to detect mycobacteria types
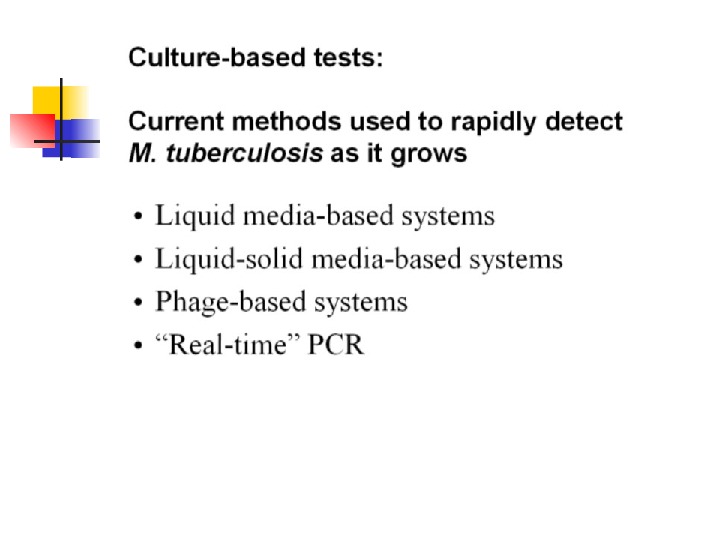
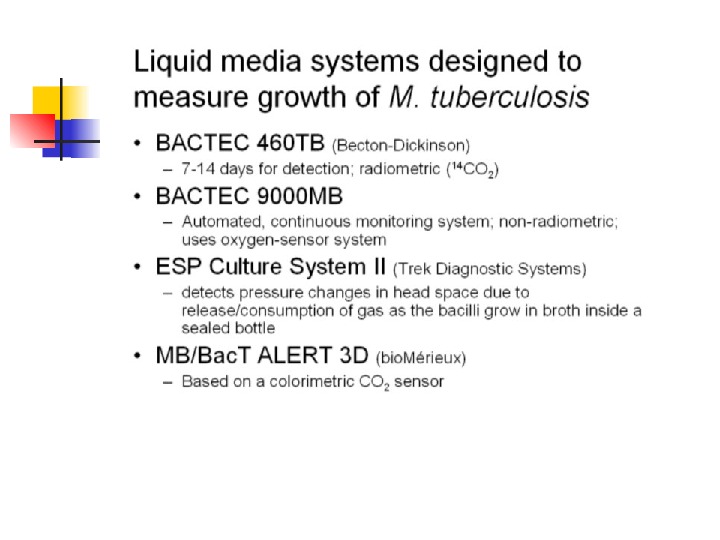
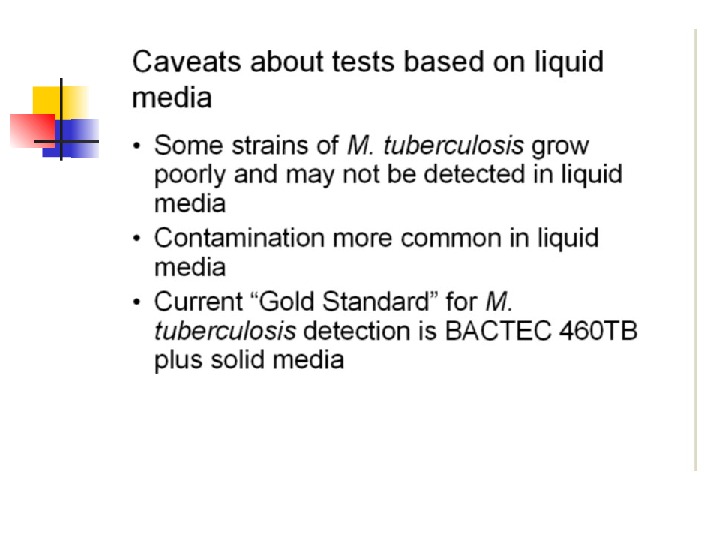
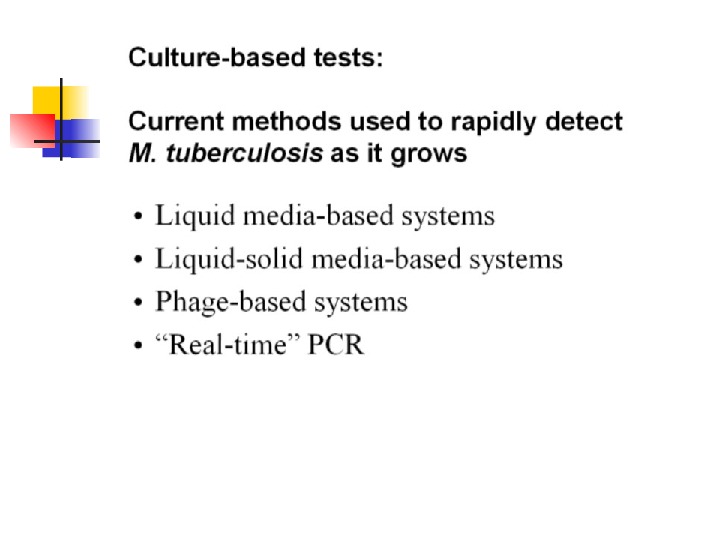
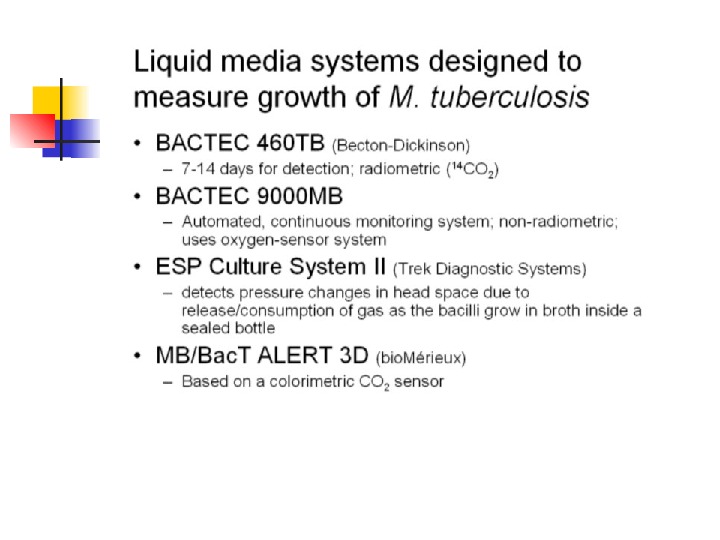
 Cultural test Lewenstein-Yensen Middlebrook set BACTEC set
Cultural test Lewenstein-Yensen Middlebrook set BACTEC set
 Culture
Culture
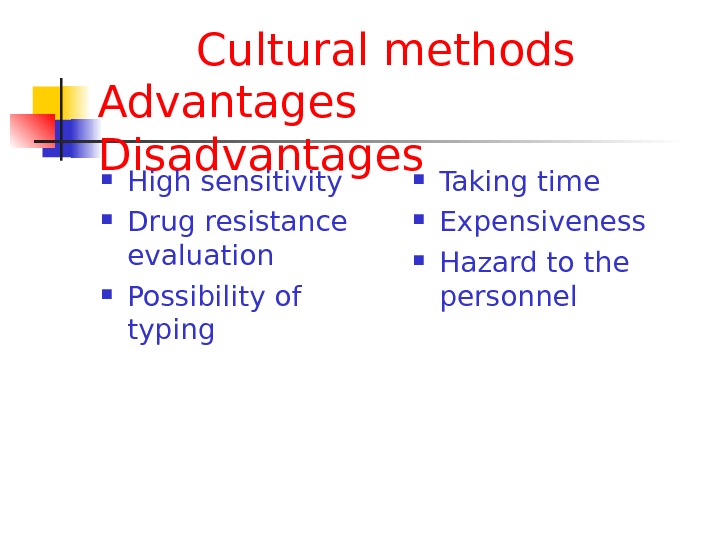
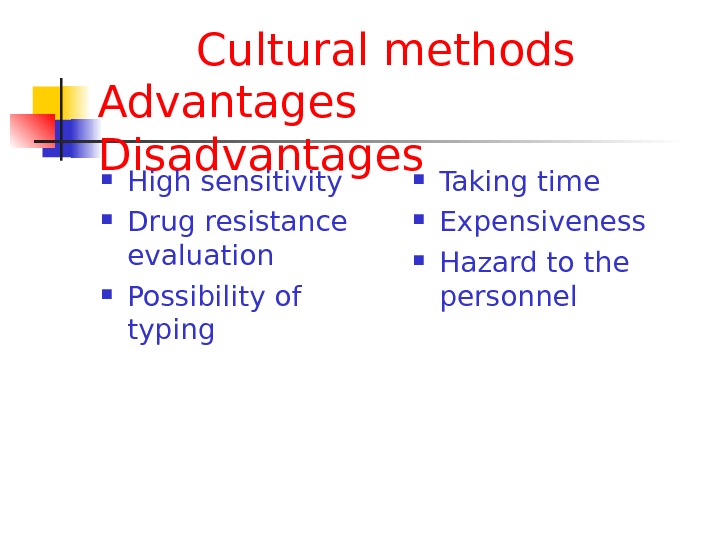 Cultural methods Advantages Disadvantages High sensitivity Drug resistance evaluation Possibility of typing Taking time Expensiveness Hazard to the personnel
Cultural methods Advantages Disadvantages High sensitivity Drug resistance evaluation Possibility of typing Taking time Expensiveness Hazard to the personnel
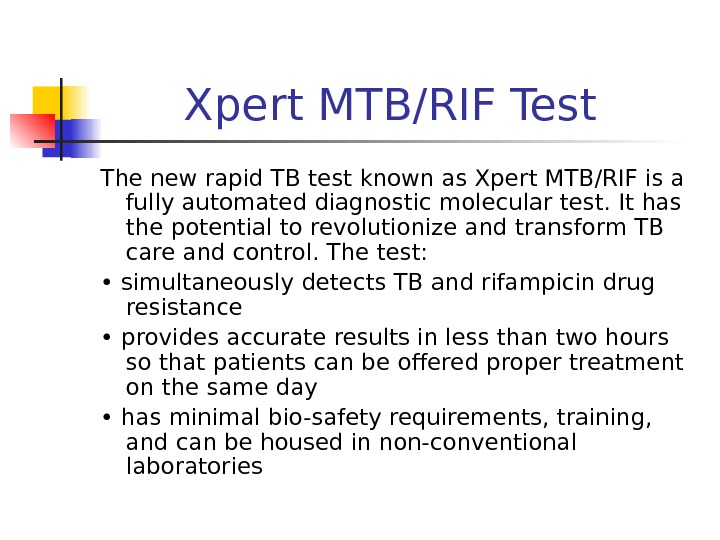 Xpert MTB/RIF Test The new rapid TB test known as Xpert MTB/RIF is a fully automated diagnostic molecular test. It has the potential to revolutionize and transform TB care and control. The test: • simultaneously detects TB and rifampicin drug resistance • provides accurate results in less than two hours so that patients can be offered proper treatment on the same day • has minimal bio-safety requirements, training, and can be housed in non-conventional laboratories
Xpert MTB/RIF Test The new rapid TB test known as Xpert MTB/RIF is a fully automated diagnostic molecular test. It has the potential to revolutionize and transform TB care and control. The test: • simultaneously detects TB and rifampicin drug resistance • provides accurate results in less than two hours so that patients can be offered proper treatment on the same day • has minimal bio-safety requirements, training, and can be housed in non-conventional laboratories
 WHY IS MDR-TB & TB/HIV DIFFICULT TO DIAGNOSE? The most widely used method to detect TB is the 125 year-old sputum smear microscopy test, which has a number of drawbacks, including low sensitivity (especially in HIV-positive individuals and children) and inability to determine drug-resistance.
WHY IS MDR-TB & TB/HIV DIFFICULT TO DIAGNOSE? The most widely used method to detect TB is the 125 year-old sputum smear microscopy test, which has a number of drawbacks, including low sensitivity (especially in HIV-positive individuals and children) and inability to determine drug-resistance.
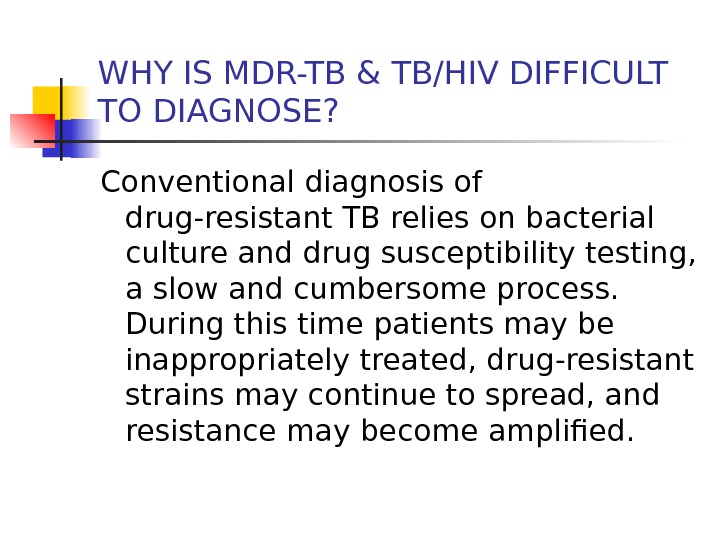 WHY IS MDR-TB & TB/HIV DIFFICULT TO DIAGNOSE? Conventional diagnosis of drug-resistant TB relies on bacterial culture and drug susceptibility testing, a slow and cumbersome process. During this time patients may be inappropriately treated, drug-resistant strains may continue to spread, and resistance may become amplified.
WHY IS MDR-TB & TB/HIV DIFFICULT TO DIAGNOSE? Conventional diagnosis of drug-resistant TB relies on bacterial culture and drug susceptibility testing, a slow and cumbersome process. During this time patients may be inappropriately treated, drug-resistant strains may continue to spread, and resistance may become amplified.
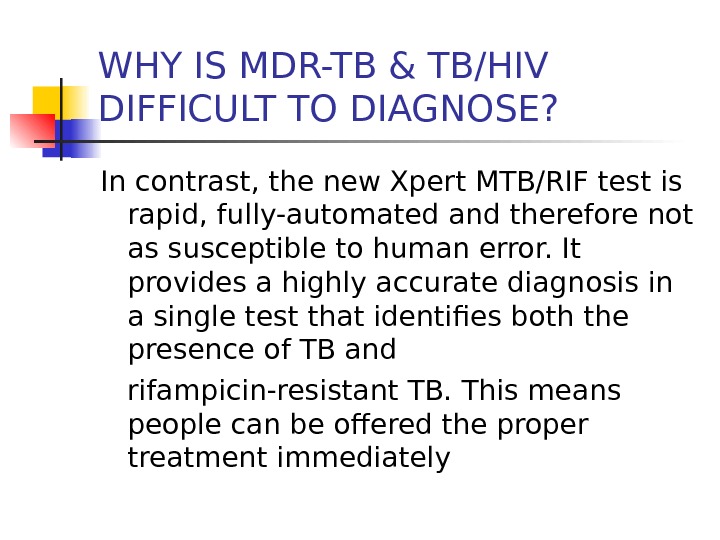 WHY IS MDR-TB & TB/HIV DIFFICULT TO DIAGNOSE? In contrast, the new Xpert MTB/RIF test is rapid, fully-automated and therefore not as susceptible to human error. It provides a highly accurate diagnosis in a single test that identifies both the presence of TB and rifampicin-resistant TB. This means people can be offered the proper treatment immediately
WHY IS MDR-TB & TB/HIV DIFFICULT TO DIAGNOSE? In contrast, the new Xpert MTB/RIF test is rapid, fully-automated and therefore not as susceptible to human error. It provides a highly accurate diagnosis in a single test that identifies both the presence of TB and rifampicin-resistant TB. This means people can be offered the proper treatment immediately
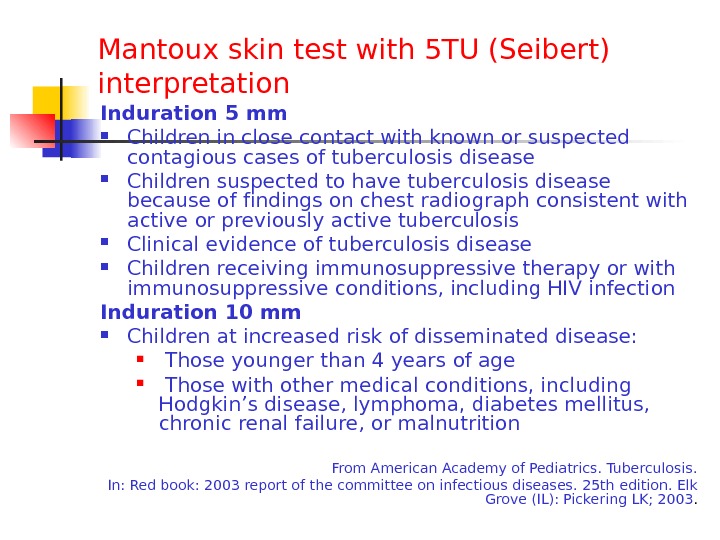
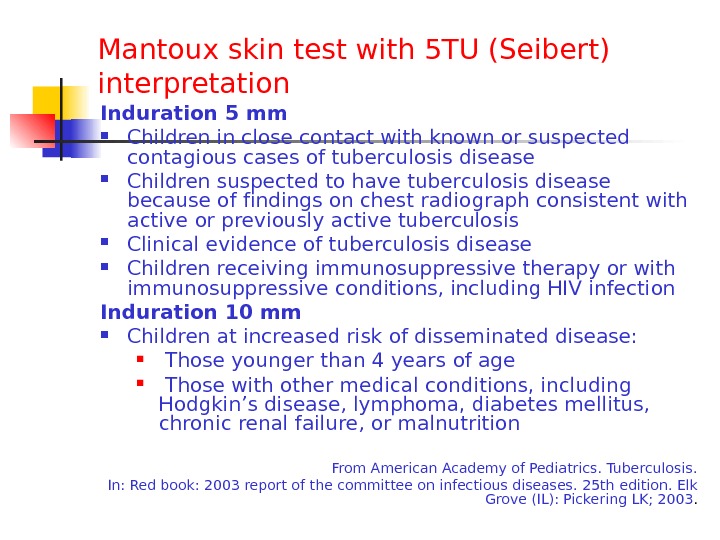 Mantoux skin test with 5 TU (Seibert) interpretation Induration 5 mm Children in close contact with known or suspected contagious cases of tuberculosis disease Children suspected to have tuberculosis disease because of f indings on chest radiograph consistent with active or previously active tuberculosis Clinical evidence of tuberculosis disease Children receiving immunosuppressive therapy or with immunosuppressive conditions, including HIV infection Induration 10 mm Children at increased risk of disseminated disease: Those younger than 4 years of age Those with other medical conditions, including Hodgkin’s disease, lymphoma, diabetes mellitus, chronic renal failure, or malnutrition From American Academy of Pediatrics. Tuberculosis. In: Red book: 2003 report of the committee on infectious diseases. 25 th edition. Elk Grove (IL): Pickering LK; 2003.
Mantoux skin test with 5 TU (Seibert) interpretation Induration 5 mm Children in close contact with known or suspected contagious cases of tuberculosis disease Children suspected to have tuberculosis disease because of f indings on chest radiograph consistent with active or previously active tuberculosis Clinical evidence of tuberculosis disease Children receiving immunosuppressive therapy or with immunosuppressive conditions, including HIV infection Induration 10 mm Children at increased risk of disseminated disease: Those younger than 4 years of age Those with other medical conditions, including Hodgkin’s disease, lymphoma, diabetes mellitus, chronic renal failure, or malnutrition From American Academy of Pediatrics. Tuberculosis. In: Red book: 2003 report of the committee on infectious diseases. 25 th edition. Elk Grove (IL): Pickering LK; 2003.
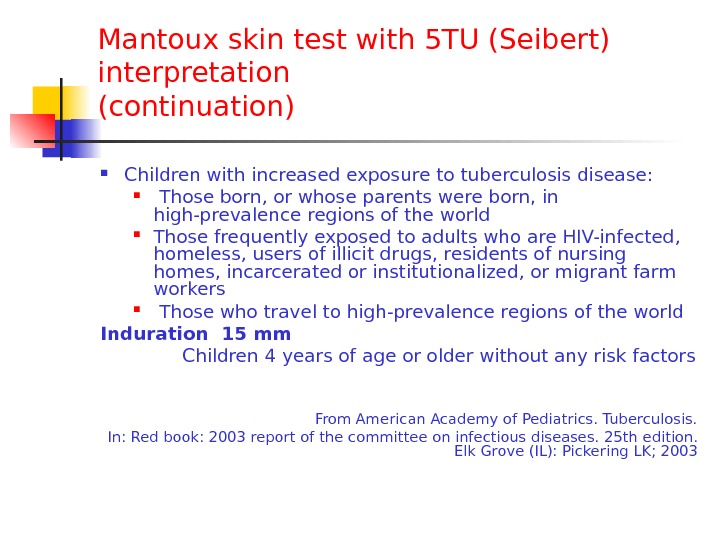
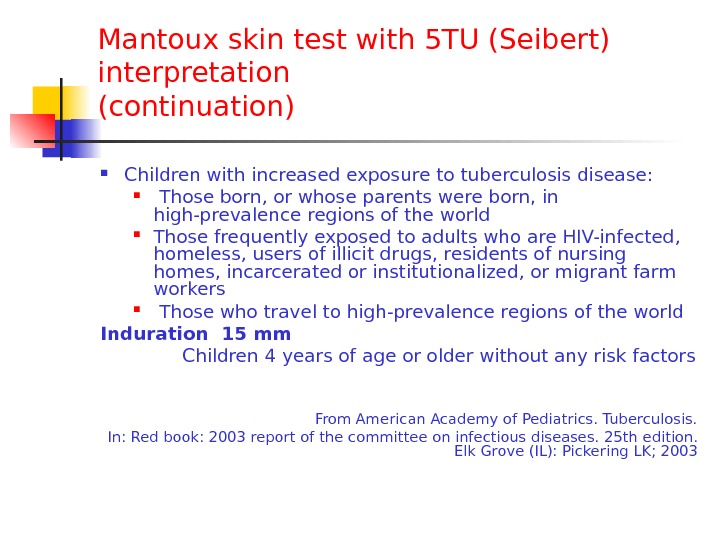 Mantoux skin test with 5 TU (Seibert) interpretation ( continuation ) Children with increased exposure to tuberculosis disease: Those born, or whose parents were born, in high-prevalence regions of the world Those frequently exposed to adults who are HIV-infected, homeless, users of illicit drugs, residents of nursing homes, incarcerated or institutionalized, or migrant farm workers Those who travel to high-prevalence regions of the world Induration 15 mm Children 4 years of age or older without any risk factors From American Academy of Pediatrics. Tuberculosis. In: Red book: 2003 report of the committee on infectious diseases. 25 th edition. Elk Grove (IL): Pickering LK;
Mantoux skin test with 5 TU (Seibert) interpretation ( continuation ) Children with increased exposure to tuberculosis disease: Those born, or whose parents were born, in high-prevalence regions of the world Those frequently exposed to adults who are HIV-infected, homeless, users of illicit drugs, residents of nursing homes, incarcerated or institutionalized, or migrant farm workers Those who travel to high-prevalence regions of the world Induration 15 mm Children 4 years of age or older without any risk factors From American Academy of Pediatrics. Tuberculosis. In: Red book: 2003 report of the committee on infectious diseases. 25 th edition. Elk Grove (IL): Pickering LK;
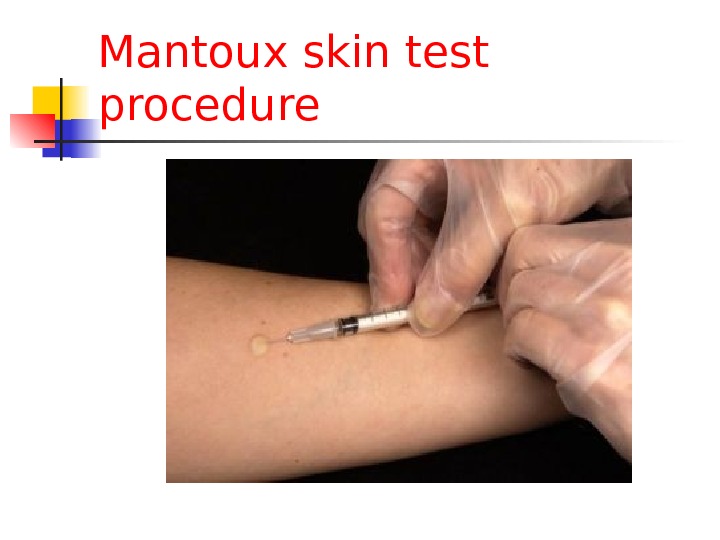
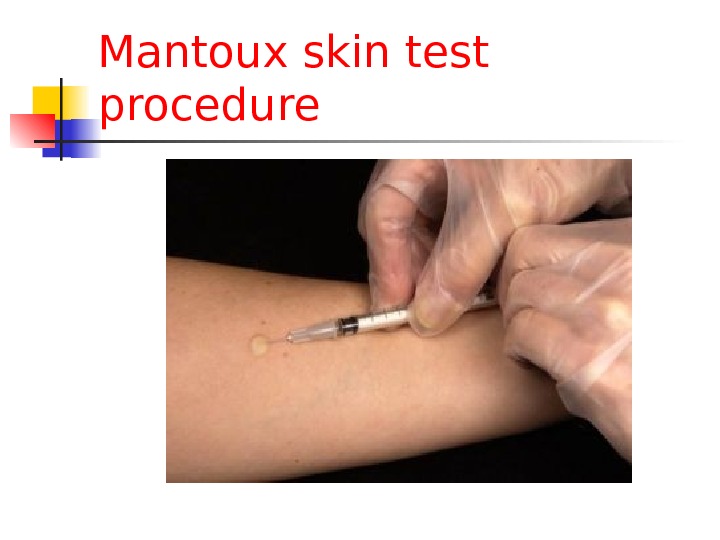 Mantoux skin test procedure
Mantoux skin test procedure
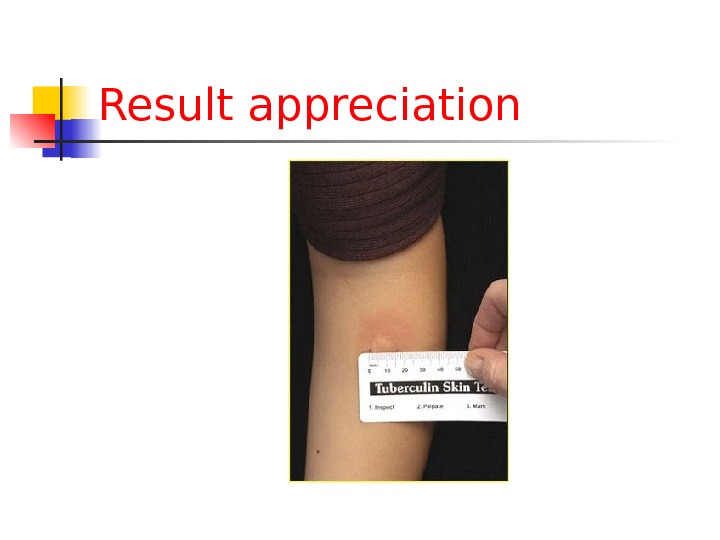
 Result appreciation
Result appreciation
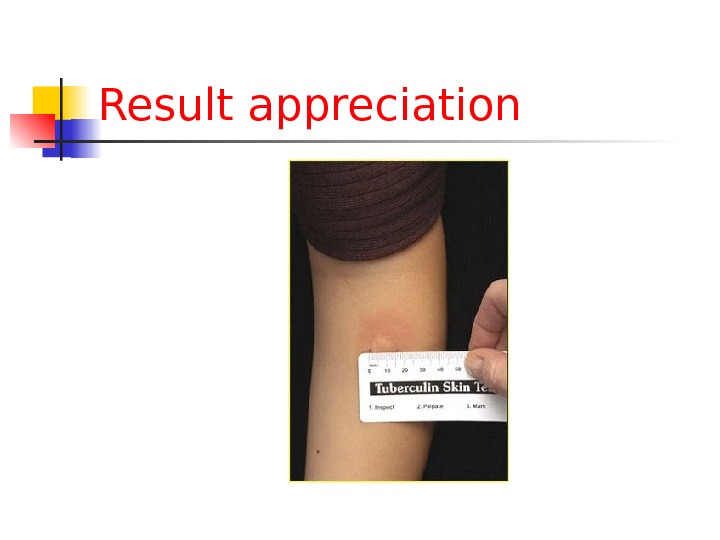 Result appreciation
Result appreciation
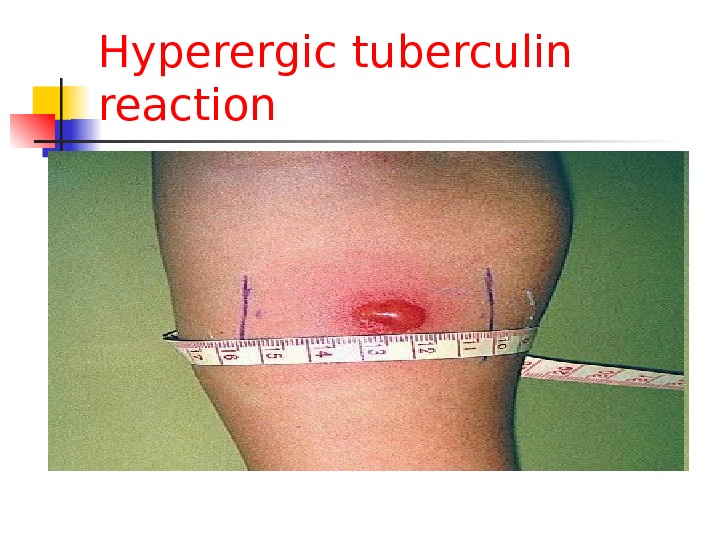
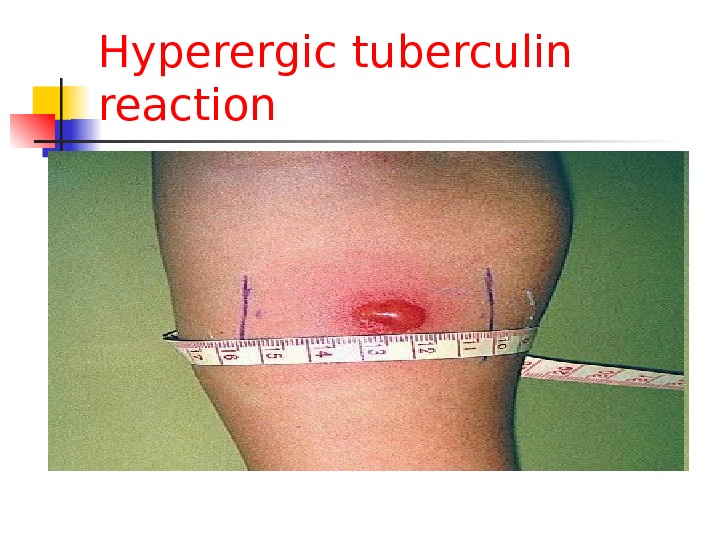 Hyperergic tuberculin reaction
Hyperergic tuberculin reaction
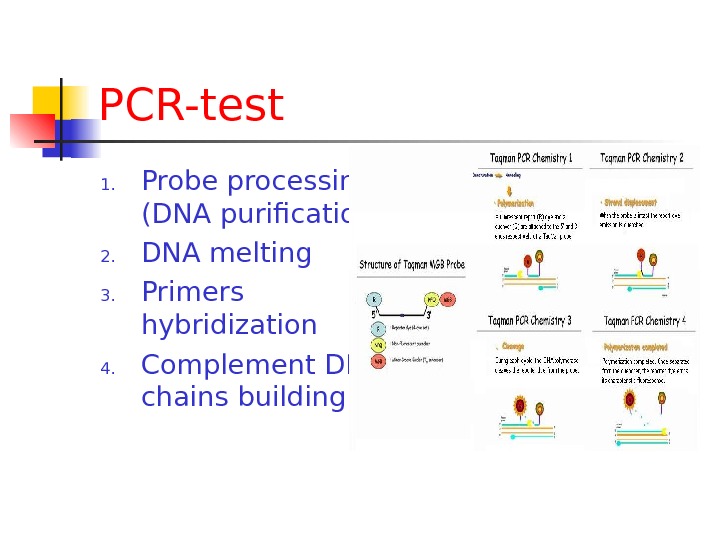
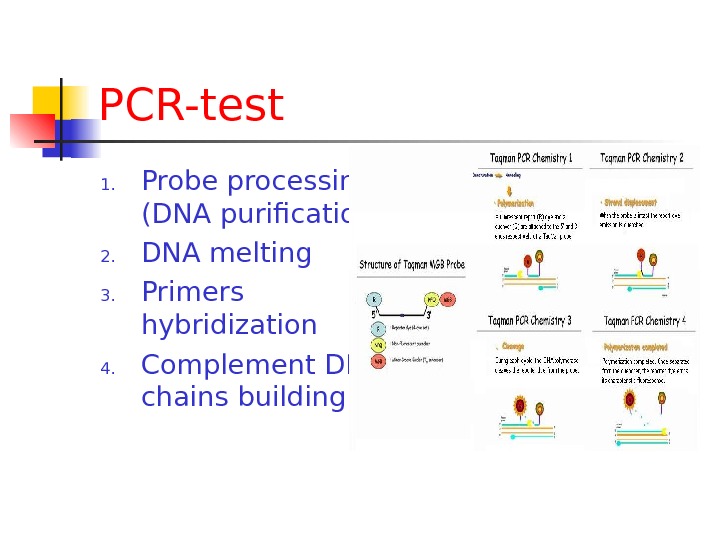 PCR-test 1. Probe processing (DNA purification) 2. DNA melting 3. Primers hybridization 4. Complement DNA chains building
PCR-test 1. Probe processing (DNA purification) 2. DNA melting 3. Primers hybridization 4. Complement DNA chains building
 Radiological examination: purposes Case detecting Differential diagnosis Treatment control
Radiological examination: purposes Case detecting Differential diagnosis Treatment control
 Radiological examination: main approaches Screening (fluoroscopy, roentgenoscopy) Additional examination – tomography Movement observing — radioscopy
Radiological examination: main approaches Screening (fluoroscopy, roentgenoscopy) Additional examination – tomography Movement observing — radioscopy
 Routine clinical examination Complaints: General: Fatigue, malaise, weakness, sweating, fever Local: Cough with mucous sputum, hemophtysis Chest pain Dyspnoe
Routine clinical examination Complaints: General: Fatigue, malaise, weakness, sweating, fever Local: Cough with mucous sputum, hemophtysis Chest pain Dyspnoe
 Routine clinical examination Anamnesis: Diseases onset: Sudden Insidious Wavy
Routine clinical examination Anamnesis: Diseases onset: Sudden Insidious Wavy
 Respiratory tract examination Percussion: dull sound, tympanic sound Auscultation: weakened breathing, dry or moisture rales
Respiratory tract examination Percussion: dull sound, tympanic sound Auscultation: weakened breathing, dry or moisture rales
 Routine clinical examination Anamnesis: Social and professional history At risk: Low income Profession: industry workers, miners, health care workers Family history: TB contact Personal history: diseases, substances abusing
Routine clinical examination Anamnesis: Social and professional history At risk: Low income Profession: industry workers, miners, health care workers Family history: TB contact Personal history: diseases, substances abusing
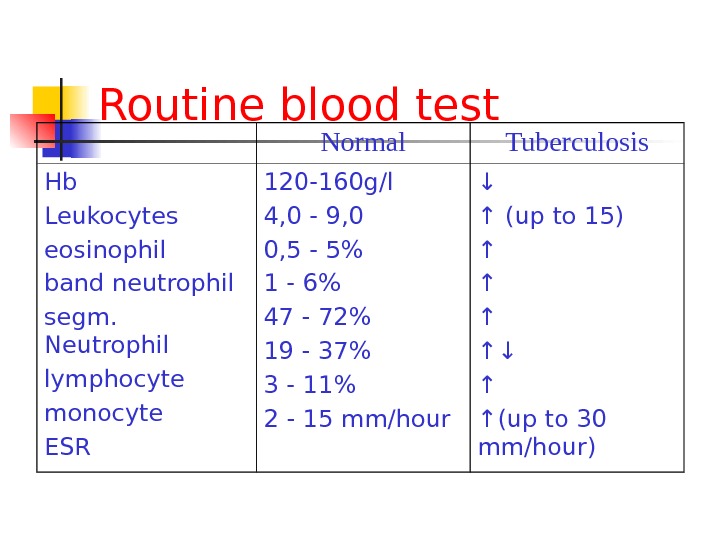
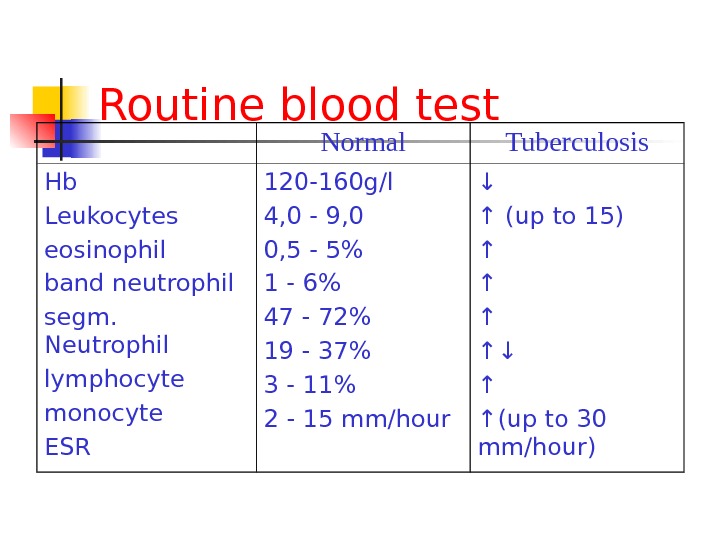 Routine blood test Normal Tuberculosis Hb Leukocytes eosinophil band neutrophil segm. Neutrophil lymphocyte monocyte ESR 120 -160 g/l 4, 0 — 9, 0 0, 5 — 5% 1 — 6% 47 — 72% 19 — 37% 3 — 11% 2 — 15 mm/hour ↓ ↑ (up to 15) ↑ ↑↓ ↑ ↑ (up to 30 mm/hour)
Routine blood test Normal Tuberculosis Hb Leukocytes eosinophil band neutrophil segm. Neutrophil lymphocyte monocyte ESR 120 -160 g/l 4, 0 — 9, 0 0, 5 — 5% 1 — 6% 47 — 72% 19 — 37% 3 — 11% 2 — 15 mm/hour ↓ ↑ (up to 15) ↑ ↑↓ ↑ ↑ (up to 30 mm/hour)