Case detecting 2013.ppt
- Количество слайдов: 36
Tuberculosis case detecting Lecturer Grib Helen
Main ways of the new cases revealing Passive Obligate diagnostical minimum (clinical, radiological examination, direct smear microscopy) n Active Screening X-ray examination for adults Screening Mantoux test for children n


Ziehl - Nielsen staining
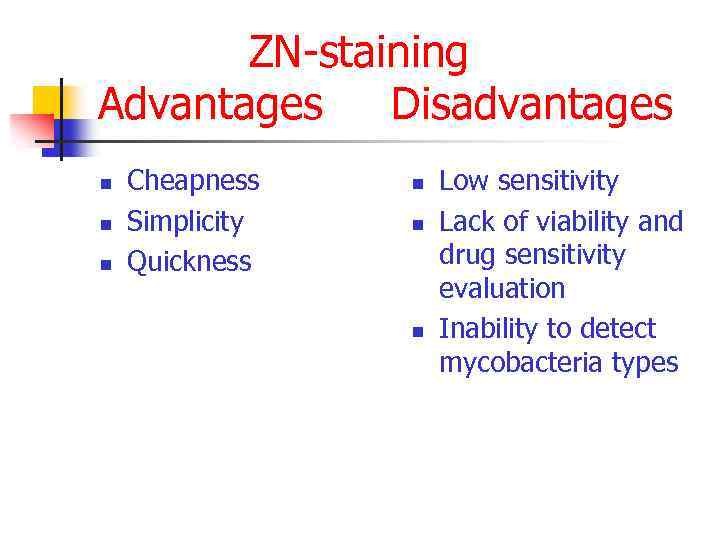
ZN-staining Advantages Disadvantages n n n Cheapness Simplicity Quickness n n n Low sensitivity Lack of viability and drug sensitivity evaluation Inability to detect mycobacteria types
Cultural test n n n Lewenstein-Yensen Middlebrook set BACTEC set

Culture
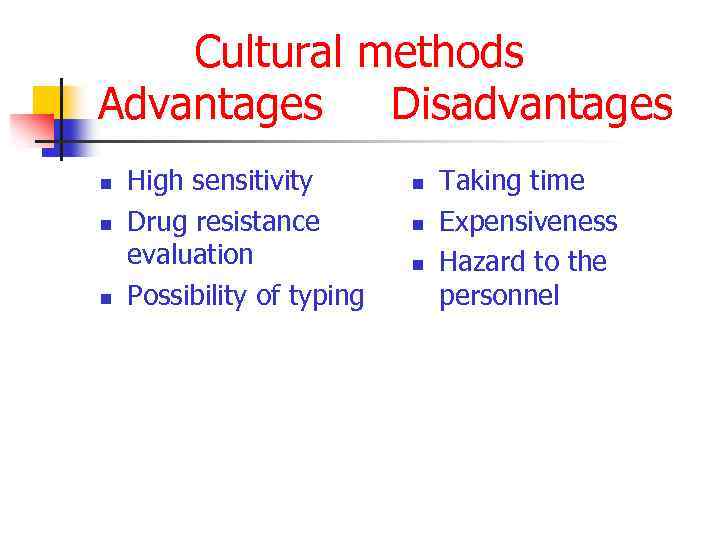
Cultural methods Advantages Disadvantages n n n High sensitivity Drug resistance evaluation Possibility of typing n n n Taking time Expensiveness Hazard to the personnel

Xpert MTB/RIF Test The new rapid TB test known as Xpert MTB/RIF is a fully automated diagnostic molecular test. It has the potential to revolutionize and transform TB care and control. The test: • simultaneously detects TB and rifampicin drug resistance • provides accurate results in less than two hours so that patients can be offered proper treatment on the same day • has minimal bio-safety requirements, training, and can be housed in non-conventional laboratories
WHY IS MDR-TB & TB/HIV DIFFICULT TO DIAGNOSE? The most widely used method to detect TB is the 125 year-old sputum smear microscopy test, which has a number of drawbacks, including low sensitivity (especially in HIV-positive individuals and children) and inability to determine drug-resistance.
WHY IS MDR-TB & TB/HIV DIFFICULT TO DIAGNOSE? Conventional diagnosis of drug-resistant TB relies on bacterial culture and drug susceptibility testing, a slow and cumbersome process. During this time patients may be inappropriately treated, drug-resistant strains may continue to spread, and resistance may become amplified.
WHY IS MDR-TB & TB/HIV DIFFICULT TO DIAGNOSE? In contrast, the new Xpert MTB/RIF test is rapid, fully-automated and therefore not as susceptible to human error. It provides a highly accurate diagnosis in a single test that identifies both the presence of TB and rifampicin-resistant TB. This means people can be offered the proper treatment immediately
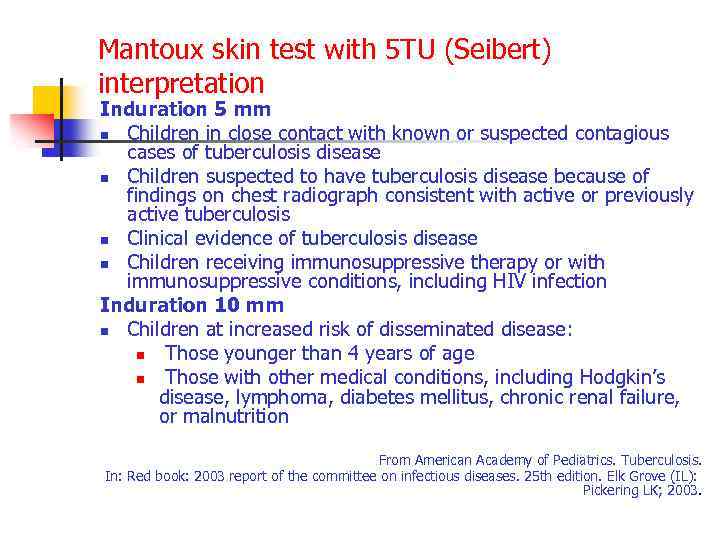
Mantoux skin test with 5 TU (Seibert) interpretation Induration 5 mm n Children in close contact with known or suspected contagious cases of tuberculosis disease n Children suspected to have tuberculosis disease because of findings on chest radiograph consistent with active or previously active tuberculosis n Clinical evidence of tuberculosis disease n Children receiving immunosuppressive therapy or with immunosuppressive conditions, including HIV infection Induration 10 mm n Children at increased risk of disseminated disease: n Those younger than 4 years of age n Those with other medical conditions, including Hodgkin’s disease, lymphoma, diabetes mellitus, chronic renal failure, or malnutrition From American Academy of Pediatrics. Tuberculosis. In: Red book: 2003 report of the committee on infectious diseases. 25 th edition. Elk Grove (IL): Pickering LK; 2003.
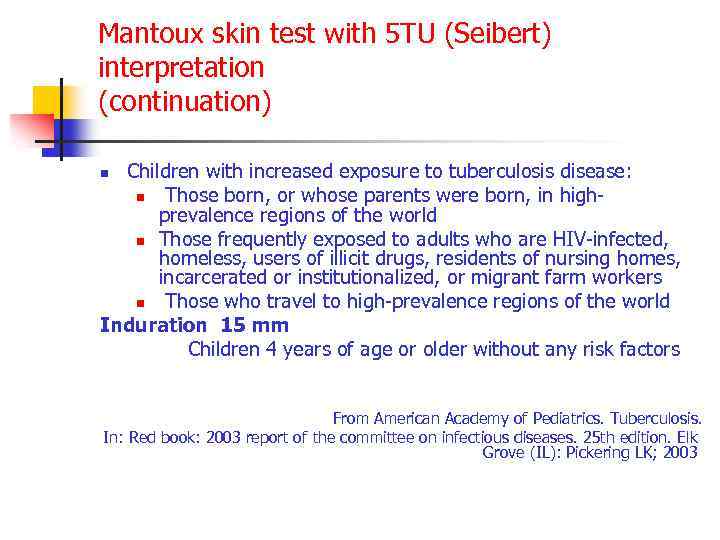
Mantoux skin test with 5 TU (Seibert) interpretation (continuation) Children with increased exposure to tuberculosis disease: n Those born, or whose parents were born, in highprevalence regions of the world n Those frequently exposed to adults who are HIV-infected, homeless, users of illicit drugs, residents of nursing homes, incarcerated or institutionalized, or migrant farm workers n Those who travel to high-prevalence regions of the world Induration 15 mm Children 4 years of age or older without any risk factors n From American Academy of Pediatrics. Tuberculosis. In: Red book: 2003 report of the committee on infectious diseases. 25 th edition. Elk Grove (IL): Pickering LK; 2003

Mantoux skin test procedure

Result appreciation
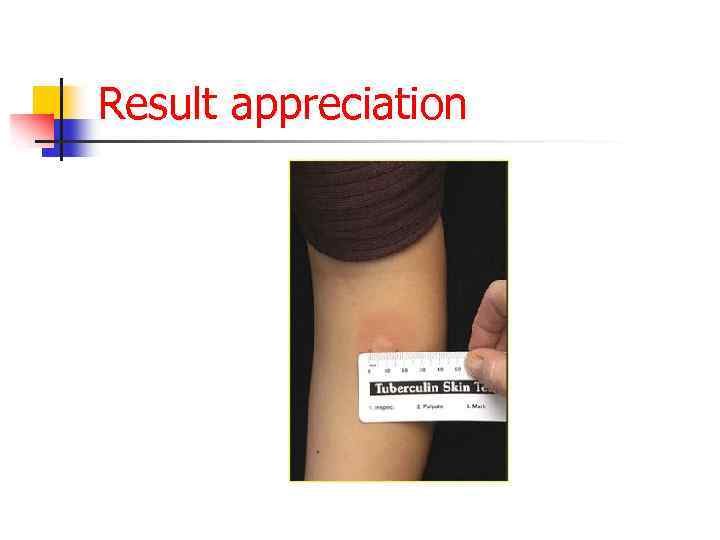
Result appreciation
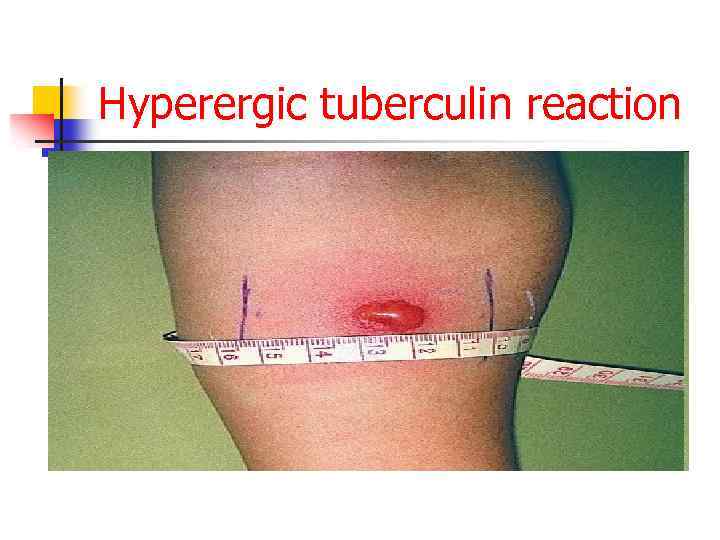
Hyperergic tuberculin reaction

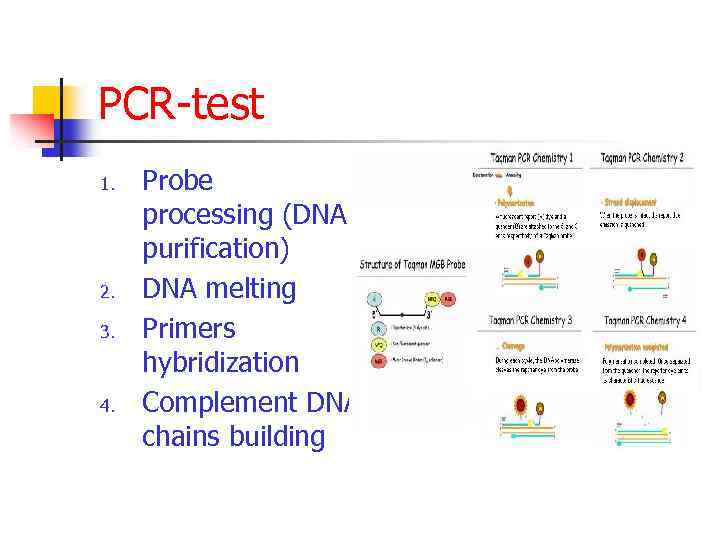
PCR-test 1. 2. 3. 4. Probe processing (DNA purification) DNA melting Primers hybridization Complement DNA chains building
Radiological examination: purposes n n n Case detecting Differential diagnosis Treatment control
Radiological examination: main approaches n n n Screening (fluoroscopy, roentgenoscopy) Additional examination – tomography Movement observing - radioscopy
Routine clinical examination Complaints: General: n Fatigue, malaise, weakness, sweating, fever Local: n Cough with mucous sputum, hemophtysis n Chest pain n Dyspnoe
Routine clinical examination Anamnesis: Diseases onset: n Sudden n Insidious n Wavy
Respiratory tract examination n n Percussion: dull sound, tympanic sound Auscultation: weakened breathing, dry or moisture rales
Routine clinical examination Anamnesis: n Social and professional history At risk: n n Low income Profession: industry workers, miners, health care workers Family history: TB contact Personal history: diseases, substances abusing
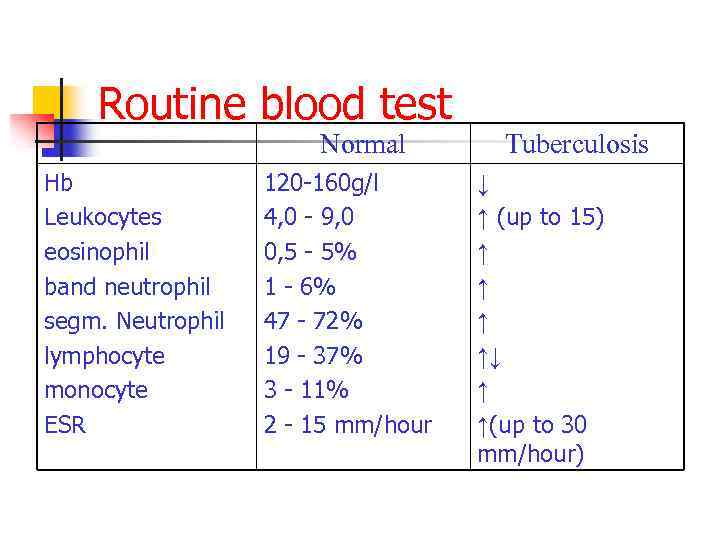
Routine blood test Normal Hb Leukocytes eosinophil band neutrophil segm. Neutrophil lymphocyte monocyte ESR 120 -160 g/l 4, 0 - 9, 0 0, 5 - 5% 1 - 6% 47 - 72% 19 - 37% 3 - 11% 2 - 15 mm/hour Tuberculosis ↓ ↑ (up to 15) ↑ ↑↓ ↑ ↑(up to 30 mm/hour)
Case detecting 2013.ppt